Fri, Jan 30, 2026
Volume 10, Issue 4 (Autumn 2024)
Caspian J Neurol Sci 2024, 10(4): 341-346 |
Back to browse issues page
Ethics code: 1400.533
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sedighinejad A, Zavarmousavi S M, Soltanipour S, Naderi Nabi B, Safari moghadam F, Shahrokhi Rad R et al . The Impact of Delivery Mode on the Development of Behavioral Disorders in Children. Caspian J Neurol Sci 2024; 10 (4) :341-346
URL: http://cjns.gums.ac.ir/article-1-731-en.html
URL: http://cjns.gums.ac.ir/article-1-731-en.html
Abbas Sedighinejad1 

 , Seyedeh Maryam Zavarmousavi2
, Seyedeh Maryam Zavarmousavi2 

 , Soheil Soltanipour3
, Soheil Soltanipour3 

 , Bahram Naderi Nabi1
, Bahram Naderi Nabi1 

 , Fatemeh Safari moghadam4
, Fatemeh Safari moghadam4 

 , Reyhaneh Shahrokhi Rad *5
, Reyhaneh Shahrokhi Rad *5 

 , Gelareh Biazar1
, Gelareh Biazar1 




 , Seyedeh Maryam Zavarmousavi2
, Seyedeh Maryam Zavarmousavi2 

 , Soheil Soltanipour3
, Soheil Soltanipour3 

 , Bahram Naderi Nabi1
, Bahram Naderi Nabi1 

 , Fatemeh Safari moghadam4
, Fatemeh Safari moghadam4 

 , Reyhaneh Shahrokhi Rad *5
, Reyhaneh Shahrokhi Rad *5 

 , Gelareh Biazar1
, Gelareh Biazar1 


1- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Psychiatry, School of Medicine, Kavosh Cognitive Behavior Sciences and Addiction Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Community Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,shahrokhireyhaneh@yahoo.com
2- Department of Psychiatry, School of Medicine, Kavosh Cognitive Behavior Sciences and Addiction Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Community Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 963 kb]
(416 Downloads)
| Abstract (HTML) (1068 Views)
Full-Text: (319 Views)
Introduction
Families of children with behavioral disorders face many out of ordinary challenges that may result from the child’s conditions or adverse reactions and stigma from society. Social arrangements often do not consider their needs and interests [1]. Studies have shown that the treatment of behavioral disorders in children is challenging and not consistently successful [2]. Decades of research have demonstrated multiple risk factors for behavioral disorders beyond genetics [3]. Nagata et al. showed a strong association between social media, screen time and new-onset behavior disorders [4]. Another study emphasizes the critical importance of the time of exposure and the vulnerability of the developing brain to anesthetics [5]. Lähdepuro et al. demonstrated that behavioral disorders in children were related to adverse maternal mental health during pregnancy [6]. Madigan et al. [7] Robinson et al. [8] and Van den Bergh et al. [9] reported similar results. This evidence suggests that exposure of the developing brain to environmental factors may program the brain differently and increase the risk of behavioral disorders [9, 10, 11].
Recently, the association between early general anesthesia (GA) exposure and behavioral disorders has been widely discussed. Studies demonstrate that children who were born by cesarian section (CS) under GA are at higher risk of autism spectrum disorder (ASD), emphasizing GA-related neurotoxicity [12, 13]. Experimental studies have also supported this hypothesis [14, 15]. Furthermore, studies have demonstrated other problems besides behavioral disorders, including maternal postpartum mood disorders [16], infants’ skin and gastrointestinal issues [17], and neurocognitive development in children [18]. Despite the alarms about the issue of GA-related neurotoxicity in developing brains and FDA recommendation [19], the subject has not been thoroughly investigated in Iran [20].
Considering the problems that the family and child with behavioral disorder are dealing with, as well as the financial burden of these children on society and given the contradictory results of the related studies [21], this research was designed. Behavioral disorders are multifactorial, and some predisposing factors are preventable, while others, such as season of birth, gender and genetics, are not. The mode of delivery and the type of anesthesia are among the factors that can be selected to some extent [22, 23]. In this study, we investigated the issue of behavioral disorders from the aspect of fetal exposure to anesthetic agents according to the mode of delivery.
Materials and Methods
This study was performed in academic psychiatric clinics, Shafa and Besat, Rasht City, Iran, affiliated with Guilan University of Medical Sciences (GUMS) from February 2022 to May 2024. The study was approved by the University Research Ethics Committee. First, the medical student of the research project screened the medical files of children to identify and sort out those with ASD, attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder diagnoses.
Through telephone interviews, the purpose of the study was explained to the parents, and if they agreed to participate, they were included in this research. Due to the genetic background of these diseases, a healthy sibling was also included in the study as a control group for each case. Afterward, a checklist containing questions about the type of delivery, including normal vaginal delivery (NVD), CS under GA or spinal anesthesia (SA), painless labor, and neonate birth status (term/preterm), was completed by the responsible medical student.
The inclusion criteria comprised children aged 5-18 diagnosed with ASD, ADHD, or oppositional defiant disorder based on the diagnosis of a pediatric psychiatry specialist. The diagnosis was performed according to DSM-5 criteria.
The exclusion criteria comprised the unwillingness of parents to participate in the research or lacking healthy siblings in the family.
Statistical analysis
The data were entered into SPSS software, version 21. Mean±SD were used to describe the data. If the data were normally distributed, the independent t-test. The equivalent non-parametric test was used in non-normal distribution. The chi-square test or Fisher exact was used for frequency comparisons between the case and control groups. Finally, logistic regression analysis was used. Statistical significance was determined as P<0.05.
Results
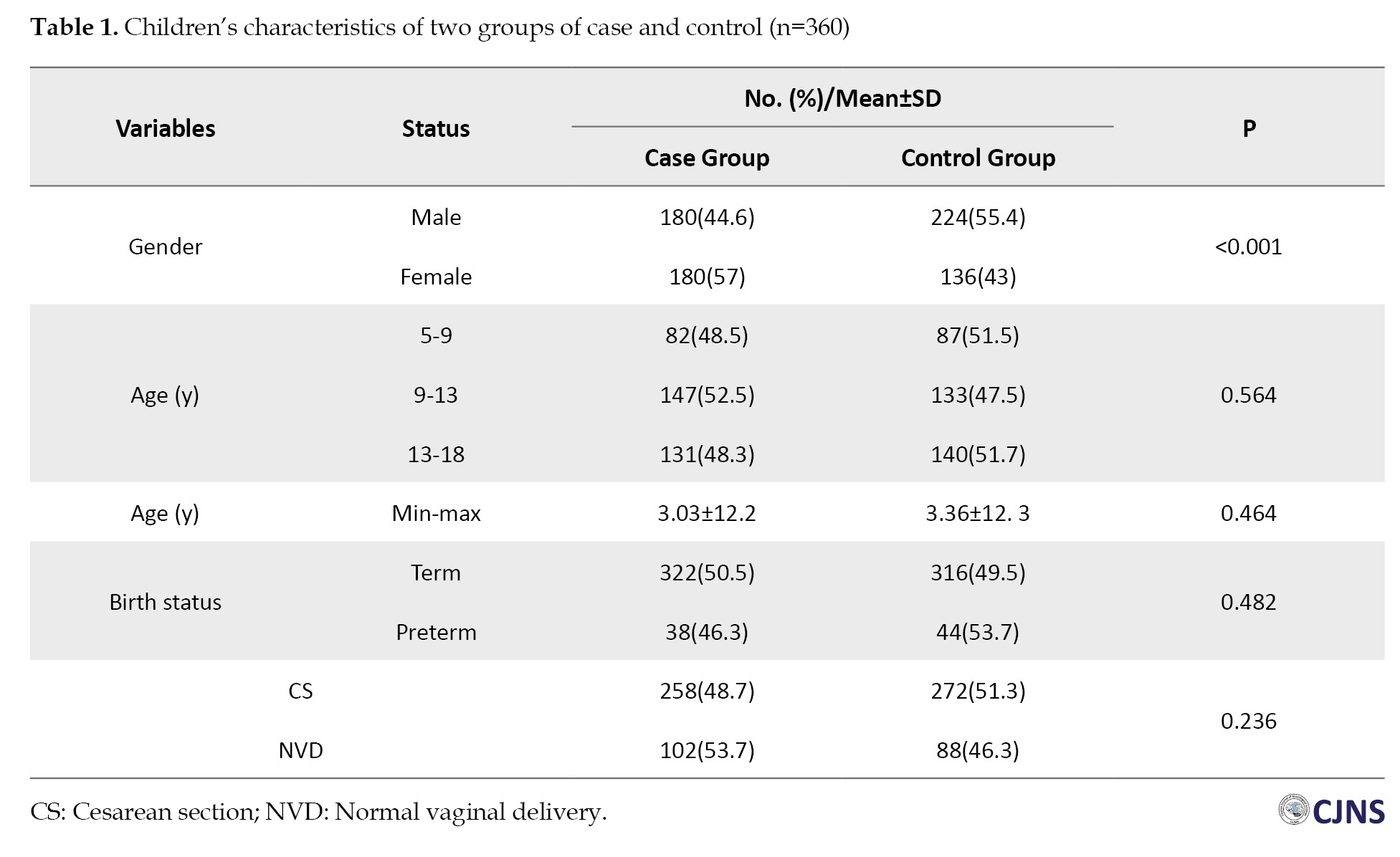
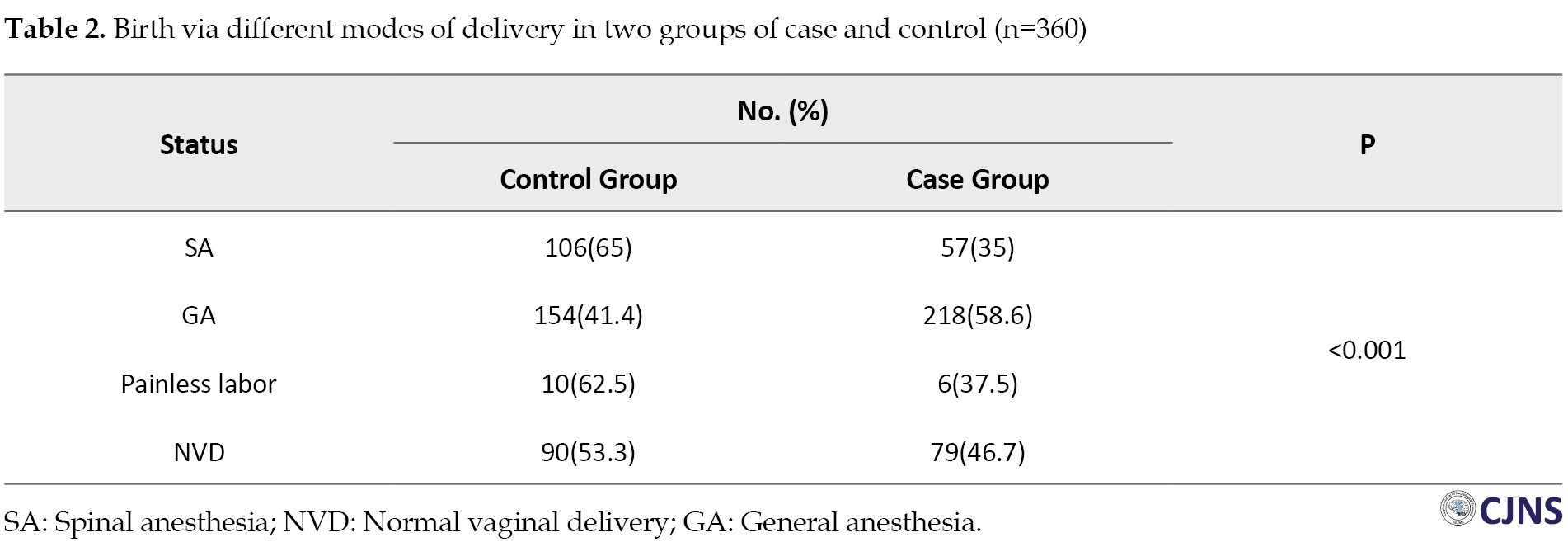
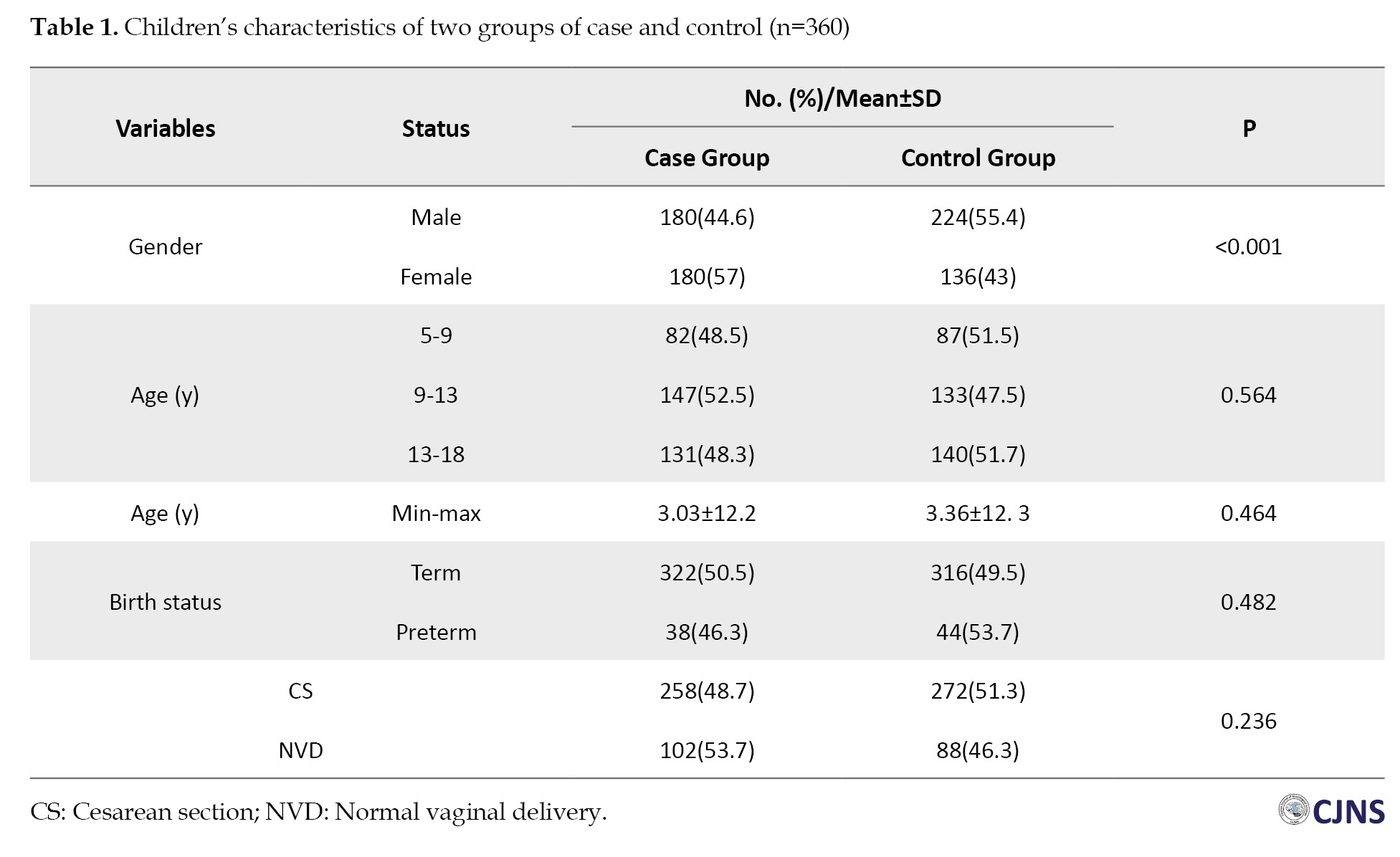
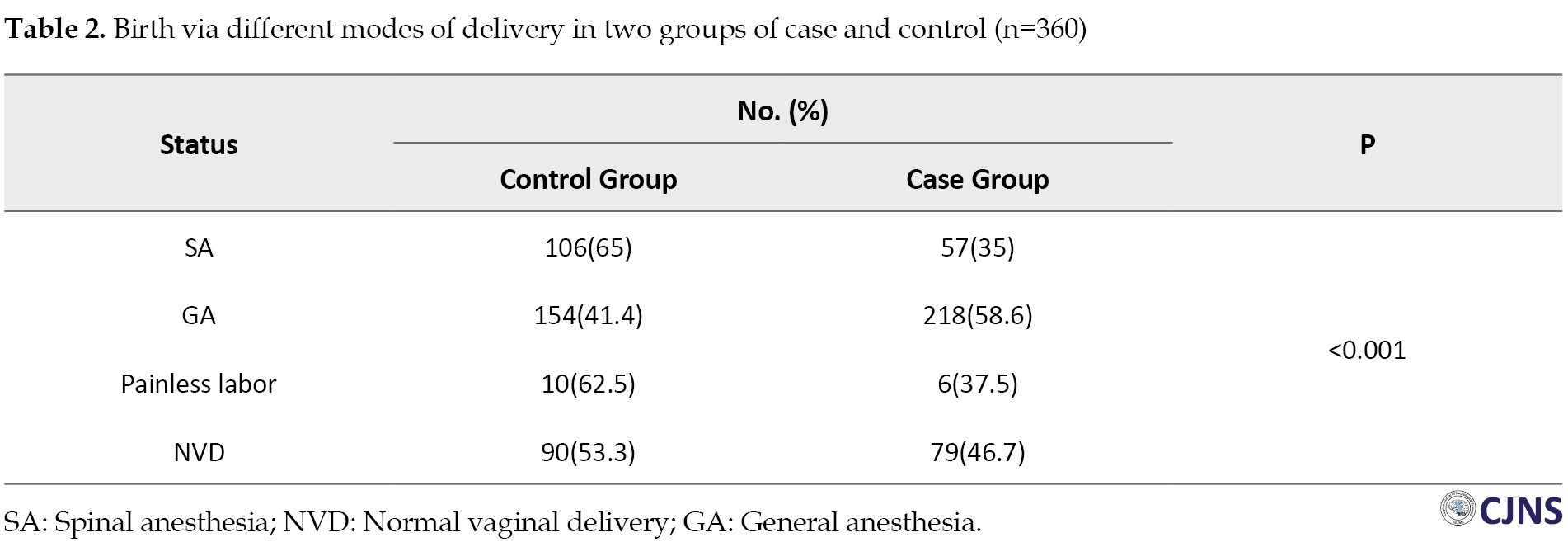
Finally, the data from 720 children (360 cases and 360 controls) with a mean age of 12.21±3.20 years were analyzed. Comparing the two groups, no significant difference was observed in terms of birth status (term or preterm) (P=0.482), age (P=0.464), and mode of delivery (P=0.236). However, a significant difference was detected regarding gender (P=0.001) and type of anesthesia (P=0.0001). Thus, delivery under GA was positively associated with behavioral disorders compared to other modes of delivery, including NVD or CS under SA (Tables 1 and 2).
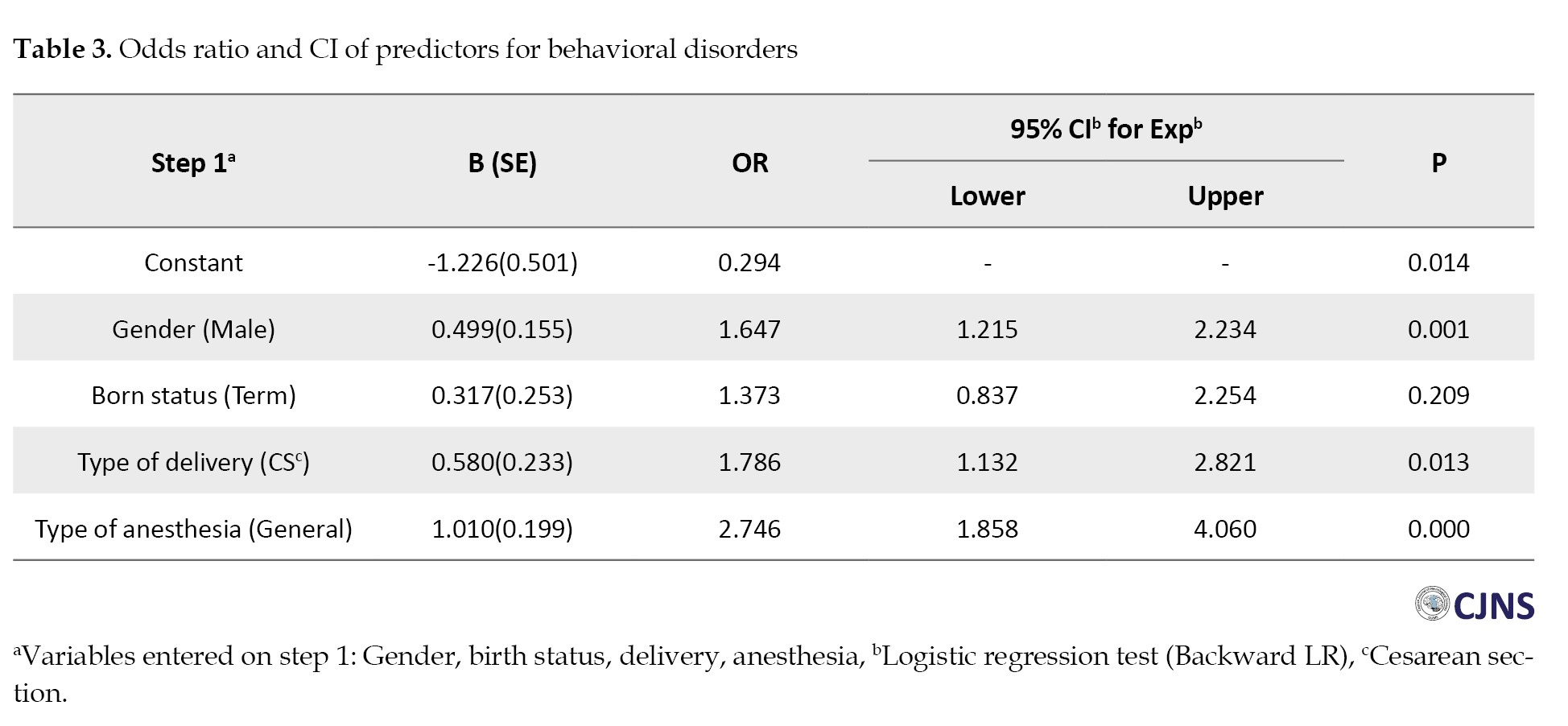
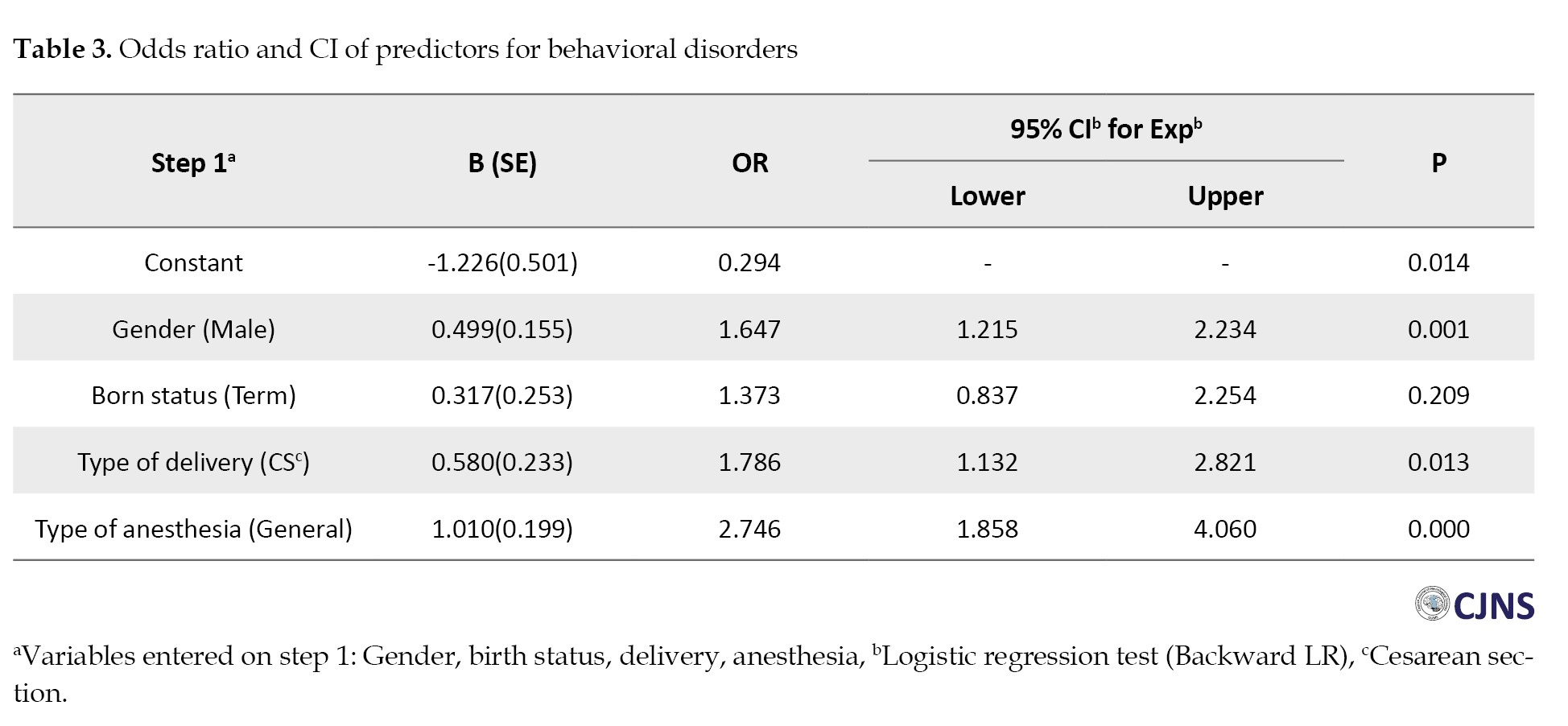
To control the confounding variables and obtain the odds ratio of each investigated factor, the 4-mode of delivery variables was converted into two modes, including two groups of receiving anesthesia or not, and then entered into the model along with other variables. The logistic regression model revealed that male gender, exposure to GA and CS were significantly associated with the development of behavioral disorders with odds ratios of 1.64, 1.78, and 2.74, respectively (Table 3).
Discussion
We found that more behavioral disorders were reported when GA was chosen for CS and boys also showed more vulnerability. Previously, we conducted a study to investigate the relationship between ADHD and early exposure of the developing brain to anesthetics. Similarly, boys were significantly more affected than girls [24]. A recent meta-analysis reported that compared to children born via NVD, children born by CS showed an increased risk of ASD and ADHD [25]. Chien L-N et al. compared the effect of CS under GA and regional anesthesia (RA) and NVD in developing ASD. They showed that ASD was significantly more common among children who underwent CS under GA than RA. However, there was no difference between CS by RA and NVD. This finding is a self-confirmation of the harmfulness of anesthetic drugs in the early stages of life [13]. This study also supported the study conducted by Samuel, who found that birth via CS under GA was associated with the development of ASD. Emphasizing the hypothesis that early brain exposure to anesthetic agents could be harmful [26]. In a contrasting study, Maher et al. examined the association between mode of delivery and behavioral disorders in children aged between 3 and 17 years at six time points. They reported that the delivery mode did not significantly impact behavioral problems [23]. Grisbrook et al. and Künzel found no associations between delivery mode and behavioral disorders [16, 27]. As mentioned, there is a discrepancy among human studies. Conducting human studies creates some challenges. It is difficult to match the studied groups in terms of genetics, socioeconomic status and the type and dose of anesthetics, all of which are among the influential factors. Also, differences in the methodology and design of the studies should be considered. As in the Wen-Ru-Ko study, only children referred to health assessment centers were investigated [28]. In Sprung’s study, the information was based on samples collected from all over the country [29]. Furthermore, how the behavioral disorders diagnosed is also important, which could be done by neurologists, psychiatrics, or pediatricians. Therefore, there is a possibility that all diagnostic criteria were not strictly followed. In the current study, the diagnosis was made by an expert pediatric psychiatrist. Another issue that arises is to what extent behavioral disorders can be attributed to anesthetic drugs. So that, a child who needs surgery and GA at a young age may suffer from co-morbidities and gets sick in general. Studies have shown that any systemic inflammation can affect the developing brain. Therefore, surgery itself can also cause systemic inflammatory and stress responses. In general, it is believed that behavioral disorders cannot be attributed only to neurotoxicity caused by anesthetic drugs [30, 31].
Conclusion
The study found a significant association between anesthesia exposure during delivery and later behavioral disorders. The male gender seemed to be more vulnerable to this process. This research confirmed the studies that emphasized the possibility of neurotoxicity of anesthetic drugs in the developing brain. Considering the limited number of research studies and many confounding factors in forming behavioral disorders, conducting well-planned prospective cohort studies is recommended.
Study limitations
Due to the nature of a retrospective study, we acknowledge some limitations. Valid information about influential factors such as birth hypoxia, Apgar score, jaundice, and birth weight was not provided. Furthermore, parental forgetfulness should be considered.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.533).
Funding
The paper was extracted from the PhD dissertation of Fatemeh Safari Moghadam, approved by Research Council of Gilan University of Medical Sciences (Code: 1400092211).
Authors contributions
Conceptualization and study design: Abbas Sedighinejad and Reyhaneh Shahrokhi Rad; Data Analysis and interpretation: Soheil Soltanipour and Bahram Naderi Nabi; Data collection: Fatemeh Safari Moghadam and Seyedeh Maryam Zavarmousavi; Statistical analysis: Soheil Soltanipour; Critical revision: Gelareh Biazar; Final approval: Abbas Sedighinejad and Reyhaneh Shahrokhi Rad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors sincerely express their gratitude for the valuable support of the esteemed Vice President of Research and Technology at Guilan University of Medical Sciences, Mahin Tayefeh Ashrafieh, and Zahra Khosnoudi, experts at the Anesthesia Research Center. The authors also want to thank all the parents who participated in this study.
References
Families of children with behavioral disorders face many out of ordinary challenges that may result from the child’s conditions or adverse reactions and stigma from society. Social arrangements often do not consider their needs and interests [1]. Studies have shown that the treatment of behavioral disorders in children is challenging and not consistently successful [2]. Decades of research have demonstrated multiple risk factors for behavioral disorders beyond genetics [3]. Nagata et al. showed a strong association between social media, screen time and new-onset behavior disorders [4]. Another study emphasizes the critical importance of the time of exposure and the vulnerability of the developing brain to anesthetics [5]. Lähdepuro et al. demonstrated that behavioral disorders in children were related to adverse maternal mental health during pregnancy [6]. Madigan et al. [7] Robinson et al. [8] and Van den Bergh et al. [9] reported similar results. This evidence suggests that exposure of the developing brain to environmental factors may program the brain differently and increase the risk of behavioral disorders [9, 10, 11].
Recently, the association between early general anesthesia (GA) exposure and behavioral disorders has been widely discussed. Studies demonstrate that children who were born by cesarian section (CS) under GA are at higher risk of autism spectrum disorder (ASD), emphasizing GA-related neurotoxicity [12, 13]. Experimental studies have also supported this hypothesis [14, 15]. Furthermore, studies have demonstrated other problems besides behavioral disorders, including maternal postpartum mood disorders [16], infants’ skin and gastrointestinal issues [17], and neurocognitive development in children [18]. Despite the alarms about the issue of GA-related neurotoxicity in developing brains and FDA recommendation [19], the subject has not been thoroughly investigated in Iran [20].
Considering the problems that the family and child with behavioral disorder are dealing with, as well as the financial burden of these children on society and given the contradictory results of the related studies [21], this research was designed. Behavioral disorders are multifactorial, and some predisposing factors are preventable, while others, such as season of birth, gender and genetics, are not. The mode of delivery and the type of anesthesia are among the factors that can be selected to some extent [22, 23]. In this study, we investigated the issue of behavioral disorders from the aspect of fetal exposure to anesthetic agents according to the mode of delivery.
Materials and Methods
This study was performed in academic psychiatric clinics, Shafa and Besat, Rasht City, Iran, affiliated with Guilan University of Medical Sciences (GUMS) from February 2022 to May 2024. The study was approved by the University Research Ethics Committee. First, the medical student of the research project screened the medical files of children to identify and sort out those with ASD, attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder diagnoses.
Through telephone interviews, the purpose of the study was explained to the parents, and if they agreed to participate, they were included in this research. Due to the genetic background of these diseases, a healthy sibling was also included in the study as a control group for each case. Afterward, a checklist containing questions about the type of delivery, including normal vaginal delivery (NVD), CS under GA or spinal anesthesia (SA), painless labor, and neonate birth status (term/preterm), was completed by the responsible medical student.
The inclusion criteria comprised children aged 5-18 diagnosed with ASD, ADHD, or oppositional defiant disorder based on the diagnosis of a pediatric psychiatry specialist. The diagnosis was performed according to DSM-5 criteria.
The exclusion criteria comprised the unwillingness of parents to participate in the research or lacking healthy siblings in the family.
Statistical analysis
The data were entered into SPSS software, version 21. Mean±SD were used to describe the data. If the data were normally distributed, the independent t-test. The equivalent non-parametric test was used in non-normal distribution. The chi-square test or Fisher exact was used for frequency comparisons between the case and control groups. Finally, logistic regression analysis was used. Statistical significance was determined as P<0.05.
Results
Finally, the data from 720 children (360 cases and 360 controls) with a mean age of 12.21±3.20 years were analyzed. Comparing the two groups, no significant difference was observed in terms of birth status (term or preterm) (P=0.482), age (P=0.464), and mode of delivery (P=0.236). However, a significant difference was detected regarding gender (P=0.001) and type of anesthesia (P=0.0001). Thus, delivery under GA was positively associated with behavioral disorders compared to other modes of delivery, including NVD or CS under SA (Tables 1 and 2).
To control the confounding variables and obtain the odds ratio of each investigated factor, the 4-mode of delivery variables was converted into two modes, including two groups of receiving anesthesia or not, and then entered into the model along with other variables. The logistic regression model revealed that male gender, exposure to GA and CS were significantly associated with the development of behavioral disorders with odds ratios of 1.64, 1.78, and 2.74, respectively (Table 3).
Discussion
We found that more behavioral disorders were reported when GA was chosen for CS and boys also showed more vulnerability. Previously, we conducted a study to investigate the relationship between ADHD and early exposure of the developing brain to anesthetics. Similarly, boys were significantly more affected than girls [24]. A recent meta-analysis reported that compared to children born via NVD, children born by CS showed an increased risk of ASD and ADHD [25]. Chien L-N et al. compared the effect of CS under GA and regional anesthesia (RA) and NVD in developing ASD. They showed that ASD was significantly more common among children who underwent CS under GA than RA. However, there was no difference between CS by RA and NVD. This finding is a self-confirmation of the harmfulness of anesthetic drugs in the early stages of life [13]. This study also supported the study conducted by Samuel, who found that birth via CS under GA was associated with the development of ASD. Emphasizing the hypothesis that early brain exposure to anesthetic agents could be harmful [26]. In a contrasting study, Maher et al. examined the association between mode of delivery and behavioral disorders in children aged between 3 and 17 years at six time points. They reported that the delivery mode did not significantly impact behavioral problems [23]. Grisbrook et al. and Künzel found no associations between delivery mode and behavioral disorders [16, 27]. As mentioned, there is a discrepancy among human studies. Conducting human studies creates some challenges. It is difficult to match the studied groups in terms of genetics, socioeconomic status and the type and dose of anesthetics, all of which are among the influential factors. Also, differences in the methodology and design of the studies should be considered. As in the Wen-Ru-Ko study, only children referred to health assessment centers were investigated [28]. In Sprung’s study, the information was based on samples collected from all over the country [29]. Furthermore, how the behavioral disorders diagnosed is also important, which could be done by neurologists, psychiatrics, or pediatricians. Therefore, there is a possibility that all diagnostic criteria were not strictly followed. In the current study, the diagnosis was made by an expert pediatric psychiatrist. Another issue that arises is to what extent behavioral disorders can be attributed to anesthetic drugs. So that, a child who needs surgery and GA at a young age may suffer from co-morbidities and gets sick in general. Studies have shown that any systemic inflammation can affect the developing brain. Therefore, surgery itself can also cause systemic inflammatory and stress responses. In general, it is believed that behavioral disorders cannot be attributed only to neurotoxicity caused by anesthetic drugs [30, 31].
Conclusion
The study found a significant association between anesthesia exposure during delivery and later behavioral disorders. The male gender seemed to be more vulnerable to this process. This research confirmed the studies that emphasized the possibility of neurotoxicity of anesthetic drugs in the developing brain. Considering the limited number of research studies and many confounding factors in forming behavioral disorders, conducting well-planned prospective cohort studies is recommended.
Study limitations
Due to the nature of a retrospective study, we acknowledge some limitations. Valid information about influential factors such as birth hypoxia, Apgar score, jaundice, and birth weight was not provided. Furthermore, parental forgetfulness should be considered.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.533).
Funding
The paper was extracted from the PhD dissertation of Fatemeh Safari Moghadam, approved by Research Council of Gilan University of Medical Sciences (Code: 1400092211).
Authors contributions
Conceptualization and study design: Abbas Sedighinejad and Reyhaneh Shahrokhi Rad; Data Analysis and interpretation: Soheil Soltanipour and Bahram Naderi Nabi; Data collection: Fatemeh Safari Moghadam and Seyedeh Maryam Zavarmousavi; Statistical analysis: Soheil Soltanipour; Critical revision: Gelareh Biazar; Final approval: Abbas Sedighinejad and Reyhaneh Shahrokhi Rad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors sincerely express their gratitude for the valuable support of the esteemed Vice President of Research and Technology at Guilan University of Medical Sciences, Mahin Tayefeh Ashrafieh, and Zahra Khosnoudi, experts at the Anesthesia Research Center. The authors also want to thank all the parents who participated in this study.
References
- McConnell D, Savage A, Breitkreuz R. Resilience in families raising children with disabilities and behavior problems. Res Dev Disabil. 2014; 35(4):833-48. [DOI:10.1016/j.ridd.2014.01.015]
- Perlstein S, Fair M, Hong E, Waller R. Treatment of childhood disruptive behavior disorders and callous-unemotional traits: A systematic review and two multilevel meta-analyses. J Child Psychol Psychiatry. 2023; 64(9):1372-87. [DOI:10.1111/jcpp.13774]
- Tortella-Feliu M, Fullana MA, Pérez-Vigil A, Torres X, Chamorro J, Littarelli SA, et al. Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neurosci Biobehav Rev. 2019; 107:154-65. [DOI:10.1016/j.neubiorev.2019.09.013]
- Nagata JM, Chu J, Ganson KT, Murray SB, Iyer P, Gabriel KP, et al. Contemporary screen time modalities and disruptive behavior disorders in children: A prospective cohort study. J Child Psychol Psychiatry. 2023; 64(1):125-35. [DOI:10.1111/jcpp.13673]
- Liu W, Wu X, Huang K, Yan S, Ma L, Cao H, et al. Early childhood screen time as a predictor of emotional and behavioral problems in children at 4 years: A birth cohort study in China. Environment Health Prev Med. 2021;26:1-9. [DOI:10.1186/s12199-020-00926-w]
- Lähdepuro A, Lahti-Pulkkinen M, Pyhälä R, Tuovinen S, Lahti J, Heinonen K, et al. Positive maternal mental health during pregnancy and mental and behavioral disorders in children: A prospective pregnancy cohort study. J Child Psychol Psychiatry. 2023; 64(5):807-16. [DOI:10.1111/jcpp.13625]
- Madigan S, Oatley H, Racine N, Fearon RP, Schumacher L, Akbari E, et al. A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J Am Acad Child Adolesc Psychiatry. 2018; 57(9):645-57. [DOI:10.1016/j.jaac.2018.06.012]
- Robinson R, Lahti-Pulkkinen M, Heinonen K, Reynolds RM, Räikkönen K. Fetal programming of neuropsychiatric disorders by maternal pregnancy depression: A systematic mini review. Pediatr Res. 2019; 85(2):134-45. [DOI:10.1038/s41390-018-0173-y]
- Van den Bergh BR, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2020; 117:26-64. [DOI:10.1016/j.neubiorev.2017.07.003]
- Maitre L, Julvez J, López-Vicente M, Warembourg C, Tamayo-Uria I, Philippat C, et al. Early-life environmental exposure determinants of child behavior in Europe: A longitudinal, population-based study. Environ Int. 2021; 153:106523. [DOI:10.1016/j.envint.2021.106523]
- O’Donnell KJ, Meaney MJ. Fetal origins of mental health: the developmental origins of health and disease hypothesis. Am J Psychiatry. 2017; 174(4):319-28. [DOI:10.1176/appi.ajp.2016.16020138]
- Curran EA, Cryan JF, Kenny LC, Dinan TG, Kearney PM, Khashan AS. Obstetrical mode of delivery and childhood behavior and psychological development in a British cohort. J Autism Dev Disord. 2016; 46(2):603-14. [DOI:10.1007/s10803-015-2616-1]
- Chien LN, Lin HC, Shao YHJ, Chiou ST, Chiou HY. Risk of autism associated with general anesthesia during cesarean delivery: A population-based birth-cohort analysis. J Autism Dev Disor. 2015; 45:932-42. [DOI:10.1007/s10803-014-2247-y]
- Zachariassen LF, Sørensen DB, Krych L, Hansen AK, Hansen CHF. Effects of delivery mode on behavior in mouse offspring. Physiol Behav. 2021; 230:113285. [DOI:10.1016/j.physbeh.2020.113285]
- Morais LH, Golubeva AV, Moloney GM, Moya-Pérez A, Ventura-Silva AP, Arboleya S, et al. Enduring behavioral effects induced by birth by caesarean section in the mouse. Curr Biol. 2020; 30(19):3761-74. [DOI:10.1016/j.cub.2020.07.044]
- Grisbrook MA, Dewey D, Cuthbert C, McDonald S, Ntanda H, Letourneau N. The Association between cesarean section delivery and child behavior: Is it mediated by maternal post-traumatic stress disorder and maternal postpartum depression? Behav Sci. 2024; 14(1):61. [DOI:10.3390/bs14010061]
- Ziętek M, Szczuko M, Machałowski T. Gastrointestinal disorders and atopic dermatitis in infants in the first year of life according to ROME IV criteria-A possible association with the mode of delivery and early life nutrition. J Clin Med. 2024; 13(4):927. [DOI:10.3390/jcm13040927]
- Lupu VV, Miron I, Răileanu AA, Jechel E, Cianga AL, Buga AML, et al. Impact of cesarean delivery on childhood neurocognitive development. BRAIN Broad Artif Intell Neurosci. 2024; 15(1):141-8. [DOI:10.18662/brain/15.1/541]
- Pinyavat T, Saraiya NR, Chen J, Ferrari LR, Goffman D, Imahiyerobo TA, et al. Anesthesia exposure in children: practitioners respond to the 2016 FDA drug safety communication. J Neurosurg Anesthesiol. 2019; 31(1):129-33. [DOI:10.1097/ANA.0000000000000545]
- Sedighinejad A, Soltanipour S, Rimaz S, Biazar G, Chaibakhsh Y, Kouhi MB. General anesthesia-related neurotoxicity in the developing brain and current knowledge and practice of physicians at Guilan academic hospitals. Anesthesiol Pain Med. 2019;9(4):e92366. [DOI:10.5812/aapm.92366]
- Useinovic N, Jevtovic-Todorovic V. Controversies in anesthesia-induced developmental neurotoxicity. Best Pract Res Clin Anaesthesiol. 2023; 37(1):28-39. [DOI:10.1016/j.bpa.2023.03.004]
- Asano R, Tsuchiya KJ, Harada T, Kugizaki Y, Nakahara R, Nakayasu C, et al. Season of birth predicts emotional and behavioral regulation in 18-month-old infants: Hamamatsu birth cohort for mothers and children (hBc study). Front Public Health. 2016; 4:152. [DOI:10.3389/fpubh.2016.00152]
- Maher GM, Khashan AS, McCarthy FP. Obstetrical mode of delivery and behavioural outcomes in childhood and adolescence: Findings from the millennium cohort study. Soc Psychiatry Psychiatr Epidemiol. 2022; 57(8):1697-709. [DOI:10.1007/s00127-022-02233-x]
- Sedighnejad A, Soltanipour S, Saberi A, Kousha M, Bidabadi E, Biazar G, et al. Risk of attention deficit hyper activity disorder after early exposure to general anesthesia; A case control study. Iran J Pediatr. 2020; 30(3):e99976. [DOI:10.5812/ijp.99976]
- Zhang T, Sidorchuk A, Sevilla-Cermeño L, Vilaplana-Pérez A, Chang Z, Larsson H, et al. Association of cesarean delivery with risk of neurodevelopmental and psychiatric disorders in the offspring: A systematic review and meta-analysis. JAMA Netw Open. 2019; 2(8):e1910236-e. [DOI:10.1001/jamanetworkopen.2019.10236]
- Huberman Samuel M, Meiri G, Dinstein I, Flusser H, Michaelovski A, Bashiri A, et al. Exposure to general anesthesia may contribute to the association between cesarean delivery and autism spectrum disorder. J Autism Dev Disord. 2019; 49(8):3127-35. [DOI:10.1007/s10803-019-04034-9]
- Künzel RG. Association between obstetric mode of delivery and emotional and behavioural problems in children and adolescents: the children of the 90s health study. Soc Psychiatry Psychiatric Epidemiol. 2024; 1-2. [DOI:10.1007/s00127-024-02698-y]
- Ko WR, Liaw YP, Huang JY, Zhao DH, Chang HC, Ko PC, et al. Exposure to general anesthesia in early life and the risk of attention deficit/hyperactivity disorder development: A nationwide, retrospective matched-cohort study. Pediatr Anesth. 2014; 24(7):741-8. [DOI:10.1111/pan.12371]
- Sprung J, Flick RP, Katusic SK, Colligan RC, Barbaresi WJ, Bojanić K, et al. Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc. 2012; 87(2):120-9. [DOI:10.1016/j.mayocp.2011.11.008]
- Lopatina OL, Panina YA, Malinovskaya NA, Salmina AB. Early life stress and brain plasticity: From molecular alterations to aberrant memory and behavior. Rev Neurosci. 2021; 32(2):131-42. [DOI:10.1515/revneuro-2020-0077]
- Nolvi S, Merz EC, Kataja E-L, Parsons CE. Prenatal stress and the developing brain: Postnatal environments promoting resilience. Biol Psychiatry. 2023; 93(10):942-52. [DOI:10.1016/j.biopsych.2022.11.023]
Type of Study: Research |
Subject:
Special
Received: 2024/07/24 | Accepted: 2024/09/28 | Published: 2024/10/1
Received: 2024/07/24 | Accepted: 2024/09/28 | Published: 2024/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |