Fri, Jan 30, 2026
Volume 11, Issue 4 (Autumn 2025)
Caspian J Neurol Sci 2025, 11(4): 286-294 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Imantalab V, Sedighinejad A, Ghanadi Karimi N, Kanafi Vahed L, Zargarnataj S S, Gholipour M et al . Effects of Preoperative Quetiapine on Postoperative Delirium in Coronary Artery Bypass Graft Surgery Patients: A Randomized Double-blind Controlled Trial. Caspian J Neurol Sci 2025; 11 (4) :286-294
URL: http://cjns.gums.ac.ir/article-1-791-en.html
URL: http://cjns.gums.ac.ir/article-1-791-en.html
Vali Imantalab1 

 , Abbas Sedighinejad *2
, Abbas Sedighinejad *2 

 , Narjes Ghanadi Karimi1
, Narjes Ghanadi Karimi1 
 , Leila Kanafi Vahed3
, Leila Kanafi Vahed3 

 , Seyed Sadegh Zargarnataj4
, Seyed Sadegh Zargarnataj4 

 , Mahboobe Gholipour4
, Mahboobe Gholipour4 

 , Gelareh Biazar1
, Gelareh Biazar1 




 , Abbas Sedighinejad *2
, Abbas Sedighinejad *2 

 , Narjes Ghanadi Karimi1
, Narjes Ghanadi Karimi1 
 , Leila Kanafi Vahed3
, Leila Kanafi Vahed3 

 , Seyed Sadegh Zargarnataj4
, Seyed Sadegh Zargarnataj4 

 , Mahboobe Gholipour4
, Mahboobe Gholipour4 

 , Gelareh Biazar1
, Gelareh Biazar1 


1- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,a_sedighinejad@yahoo.com
3- Department of Community Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Cardiology, Healthy Heart Research Center, School of Medicine, Heshmat Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Anesthesiology, Anesthesiology Research Center, Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Department of Community Medicine, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Cardiology, Healthy Heart Research Center, School of Medicine, Heshmat Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 1278 kb]
(439 Downloads)
| Abstract (HTML) (393 Views)
References
Full-Text: (195 Views)
Introduction
Delirium is an acute medical condition characterized by acute disturbance of the level of consciousness and cognitive function occurring within the first three days after surgery, and is the most commonly seen psychiatric disorder in the intensive care unit (ICU) [1]. The occurrence of POD is associated with considerable adverse effects, such as prolonged lengths of stay in hospital, longer mechanical ventilation, impaired recovery, long-term cognitive dysfunction, and higher readmission and mortality rates [2-4]. Cardiac surgeries are at higher risk of developing POD due to several known risk factors, such as advanced age, perioperative medications, atrial fibrillation, pre-existing cognitive impairment, congestive heart failure, and negative effects of cardiopulmonary bypass (CPB) [5, 6].
Given the prevalence and costs of POD in cardiac surgeries, the prevention and management of this disorder are crucial. Studies have focused on this topic with different types of interventions, including pharmacological options such as cholinesterase inhibitors, antipsychotics, and analgesics [7, 8], as well as non-pharmacological interventions such as cognitive engagement, early mobilization, and optimization of environmental factors in the ICU [9]. Quetiapine, as an atypical antipsychotic, works by changing the activity of certain natural substances in the brain. It was introduced in 1985 and received approval for medical use in 1997. In 2022, it was the most commonly prescribed antipsychotic in the USA [10, 11]. The aim of this study was to investigate the effectiveness of quetiapine in preventing postoperative delirium in patients undergoing coronary artery bypass graft (CABG) surgery.
Materials and Methods
This prospective, double -blind clinical trial was conducted at Dr. Heshmat Hospital from December 2023 to November 2024. This cardiac center is located in Northern Iran and admits all types of cardiac surgeries. Screening of the patients for eligibility was performed after approval by the Institutional Ethical Committee of Guilan University of Medical Sciences (GUMS), and the research was registered at the Iranian Registry of Clinical Trials (IRCT). First, the purpose of the study was explained to the patients, and informed consent was obtained.
Inclusion criteria were patients of both genders, aged between 35-70, scheduled for CABG surgery, with the ASA classes of II and III.
Exclusion criteria included patients undergoing emergency surgery, those with any mental disorder, renal failure, chronic liver disease (child classification classes B and C), prolonged postoperative intubation, re-exploration, or any contraindication to quetiapine.
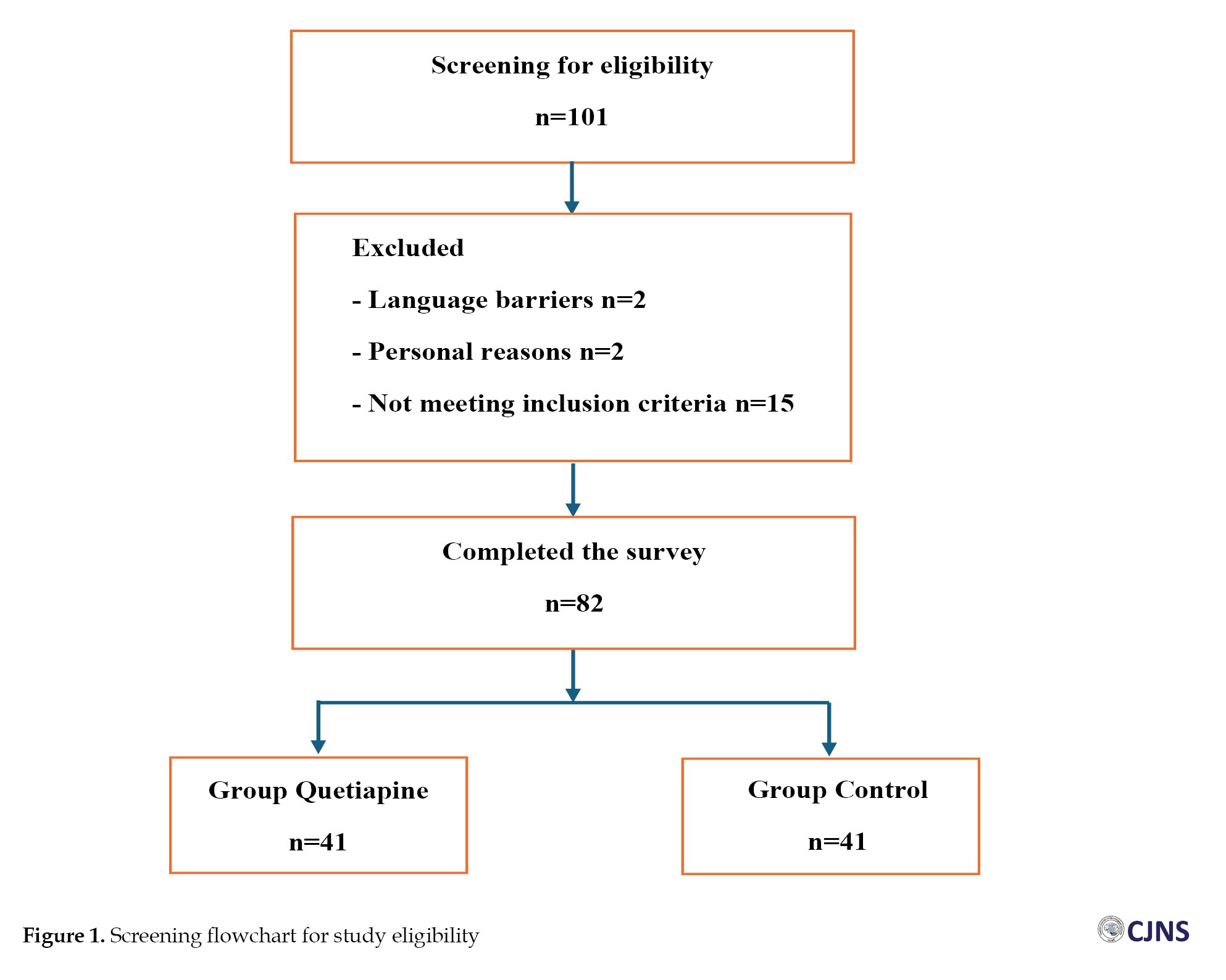
In total, 101 CABG patients were screened for eligibility, and 19 individuals did not meet the inclusion criteria. Finally, data from 82 cases were analyzed (Figure 1).
Delirium is an acute medical condition characterized by acute disturbance of the level of consciousness and cognitive function occurring within the first three days after surgery, and is the most commonly seen psychiatric disorder in the intensive care unit (ICU) [1]. The occurrence of POD is associated with considerable adverse effects, such as prolonged lengths of stay in hospital, longer mechanical ventilation, impaired recovery, long-term cognitive dysfunction, and higher readmission and mortality rates [2-4]. Cardiac surgeries are at higher risk of developing POD due to several known risk factors, such as advanced age, perioperative medications, atrial fibrillation, pre-existing cognitive impairment, congestive heart failure, and negative effects of cardiopulmonary bypass (CPB) [5, 6].
Given the prevalence and costs of POD in cardiac surgeries, the prevention and management of this disorder are crucial. Studies have focused on this topic with different types of interventions, including pharmacological options such as cholinesterase inhibitors, antipsychotics, and analgesics [7, 8], as well as non-pharmacological interventions such as cognitive engagement, early mobilization, and optimization of environmental factors in the ICU [9]. Quetiapine, as an atypical antipsychotic, works by changing the activity of certain natural substances in the brain. It was introduced in 1985 and received approval for medical use in 1997. In 2022, it was the most commonly prescribed antipsychotic in the USA [10, 11]. The aim of this study was to investigate the effectiveness of quetiapine in preventing postoperative delirium in patients undergoing coronary artery bypass graft (CABG) surgery.
Materials and Methods
This prospective, double -blind clinical trial was conducted at Dr. Heshmat Hospital from December 2023 to November 2024. This cardiac center is located in Northern Iran and admits all types of cardiac surgeries. Screening of the patients for eligibility was performed after approval by the Institutional Ethical Committee of Guilan University of Medical Sciences (GUMS), and the research was registered at the Iranian Registry of Clinical Trials (IRCT). First, the purpose of the study was explained to the patients, and informed consent was obtained.
Inclusion criteria were patients of both genders, aged between 35-70, scheduled for CABG surgery, with the ASA classes of II and III.
Exclusion criteria included patients undergoing emergency surgery, those with any mental disorder, renal failure, chronic liver disease (child classification classes B and C), prolonged postoperative intubation, re-exploration, or any contraindication to quetiapine.
In total, 101 CABG patients were screened for eligibility, and 19 individuals did not meet the inclusion criteria. Finally, data from 82 cases were analyzed (Figure 1).
The patients were randomly divided into two groups: the quetiapine group (n=41) and the control group (n=41). The same method of anesthesia and surgery was followed for all patients in both groups, using computer-generated numbers. The patients, surgeon, and the anesthesiologist not involved in the study, who filled out the questionnaires, were blinded.
Patients in group Q received 12.5 mg quetiapine (25 mg tablets manufactured by Fatek Shimi Pars Company - Iran) the morning of surgery and every 12 hours for 48 hours postoperatively. In this study, delirium was assessed using the confusion assessment method (CAM) for the ICU. The CAM-ICU assessment tool has a sensitivity between 95% and 100% and a specificity between 89% and 93% [12]. This questionnaire had four basic items: 1- Acute change in mental status, 2- Inattention, 3- Thought disorder, 4- Change in level of consciousness [13]. Postoperative delirium was assessed from the time the patient was admitted to the ICU until discharge from the unit. If the patient developed severe agitation, haloperidol 1-5 mg was administered. During the study, patients were assessed for possible side effects, such as long QT interval, hypotension, and elevated liver enzymes [14].
Statistical analysis: The collected data were analyzed by SPSS software, version 21 using the chi-square test, Fisher’s exact test, t-test, and repeated measures ANOVA. The parametric data were described as Mean±SD, and the nonparametric data were presented as median (range). A P<0.05 was considered significant.
Results
A total of 82 eligible CABG patients were enrolled in the study, with a mean age of 58.46±4.59 years in the quetiapine group and 57.97±5.01 years in the control group, as well as a mean BMI of 26.92±4.48 kg/m² in the quetiapine group and 27.61±4.04 kg/m² in the control group. More demographic details are shown in Table 1.

No significant difference was observed in terms of the demographic data and surgical characteristics of the individuals.
There was no association between patients’ co-morbidities (P=0.675), ASA class (P=0.154), age (P=0.648), BMI (P=0.468), and the occurrence of POD (Tables 1 and 2).

Medication status was compared between the two groups (Table 3).

The overall incidence of POD in the studied patients was 7.3%, with two cases in the intervention group (4.87%) and four patients in the control group (9.75%) developing POD. None of our patients showed serious adverse events, and no patients dropped out of the survey.
Discussion
Delirium is a mental state characterized by acute momentary deterioration of mental abilities, caused by a disruption in the regulation of neuronal activity. POD is a common complication of cardiac surgery [3, 15]. A recent meta-analysis showed that the incidence of POD in cardiac surgery was 32%, which is higher than in other types of surgeries. According to the available literature, a wide range of incidence rates for POD after cardiac surgery, from 2.8 to 63.8%, has been reported [16]. Studies have shown that, following surgery-related stress responses, the levels of inflammatory mediators such as IL-6 and CRP increase, leading to systemic and neurological inflammatory responses that can ultimately predispose individuals to postoperative delirium. The severity of surgical stress facilitates this process, particularly in patients with preoperative cerebral infarction and poor pain control [16-18]. This indicates the important role of anesthesia management in appropriately controlling pain and inflammatory reactions. So far, several interventions have been performed in cardiac surgery to control inflammatory reactions, with varying degrees of success [19-22].
Studies indicate that effective measures for reducing POD begin with careful preoperative assessments [23]. The choice of anesthesia method and selected drugs also affects the outcomes. For example, a study conducted in 2024 found that total intravenous anesthesia (TIVA) using propofol was associated with a lower incidence of delirium compared to sevoflurane-based anesthesia [24-26]. Additionally, a study by Suenaga et al. in 2025 showed that patients who underwent transcatheter aortic valve implantation (TAVI) surgery and developed delirium had a higher mortality rate and more adverse outcomes [27]. Lagonigro et al. also reported in 2025 an association between hyperglycemia—caused by stress responses in cardiac surgery, particularly in diabetic patients—and an increased incidence of POD [28]. Esfahanian et al. evaluated the effect of music on POD in CABG. In contrast to this study, a significant difference was observed between the case and control groups, with 3% in the case group compared to 12% in the control group [29]. Gonçalves et al., in their study on cardiac surgery patients in 2025, reported a prevalence of 18.3% for delirium, identifying age, gender, and inflammatory responses as predisposing factors [30]. A recent study reported that 40% of CABG patients developed POD, with female gender, perioperative anxiety and stress, surgery duration exceeding seven hours, and older age being predisposing factors [13]. Huang et al. demonstrated an association between POD and the patient’s gastrointestinal status concerning the presence of opportunistic pathogens [31].
Given the importance of the issue, both pharmacologic and non-pharmacologic interventions have been investigated [29]. This study is the first to examine the effect of quetiapine on post-CABG delirium, a drug previously used in CABG surgery with no significant adverse effects [7, 29, 32]. The primary outcome of this study indicated that the overall incidence of POD in CABG was 7.3%, which is lower than reported in similar studies [7, 32]. The results showed no significant difference between the intervention and control groups regarding complications, the incidence of POD, demographic characteristics, comorbidities, or medications. None of the variables studied—including literacy level, place of residence, employment status, comorbidities, age, BMI, and medications—were associated with the incidence of delirium. Although the number of delirium cases was higher in men than in women (4 patients compared to 1 patient), it is noteworthy that five of these six cases involved older patients and that this complication occurred more frequently among those taking medications. These findings align with several other studies [33]. The observed side effects related to quetiapine were minimal and manageable. The results indicated that the use of quetiapine did not significantly reduce the incidence of POD in patients undergoing CABG surgery when compared to the control group. There are some points worth mentioning. First, no similar study has been conducted to evaluate the effects of quetiapine on POD in CABG patients; only limited studies exist for other conditions [34, 35]. Therefore, meaningful comparisons with existing results were not possible.
Additionally, the mean age of CABG patients in this study was lower than in other studies, which partly justifies the lower incidence of POD, consistent with previous studies identifying older age as one of the most significant risk factors for delirium [15, 29, 36-38]. As mentioned, the results of studies are not consistent. It should be noted that the development of POD in CABG patients could be influenced by several factors. Patient population characteristics, such as age, gender, ASA class, habits, nutrition status, pre- operative mental state, and mood disorders, such as depression, as well as study methodology the assessment tool, who fills out the questionnaire, the level of accuracy, and the intervals between visits are all among the influential factors [13, 39-42]. Additionally, some studies report that other states of postoperative cognitive impairment might be considered delirium [18].
Overall, the findings of this study suggest that while quetiapine is widely used for various medical conditions, its effectiveness in preventing POD in CABG patients may be limited by this prescribing pattern. The overall low rate of POD in both groups could indicate that other factors, such as surgical and anesthesia techniques, as well as postoperative care and management of these patients, may play a more significant role in influencing delirium outcomes than pharmacological intervention alone [43]. The lack of significant difference in POD incidence between the quetiapine and control groups aligns with some previous studies that have also reported minimal benefits from antipsychotic medications in preventing delirium in surgical patients. However, the small sample size, the specific patient population, and other limitations of this study should be considered. Future studies should explore alternative strategies for preventing delirium. Furthermore, investigating different dosages or timing of quetiapine administration may yield better results. This comprehensive approach will help delineate strategies for preventing POD and improving outcomes for CABG surgery patients.
Conclusion
In conclusion while quetiapine had a favorable safety profile, this study did not find a significant benefit in preventing postoperative delirium in patients undergoing CABG surgery. Further well-planned clinical trials with other doses of the drug, larger sample sizes, and diverse patient populations are needed to better understand the role of quetiapine in the prevention of POD.
Limitations
The relatively short follow-up period post-surgery may not detect all cases of POD, and the assessment method (CAM-ICU) may not identify all cases of delirium, particularly those with less severe symptoms. The degree of pre-operative anxiety was not assessed, which is influential and should be considered one of the limitations of this study. Additionally, the study was conducted at a single center, which may limit the external validity of the findings.
Ethical Considerations
Compliance with ethical guidelines
This study protocol was approved by the Research Ethics Committee of the Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1402.242), and the research was registered at the Iranian Registry of Clinical Trials (IRCT) Tehran, Iran (Code: IRCT20130525013456N7). Moreover, informed consent was obtained from the patients who agreed to participate.
Funding
This study was extracted from the General Medical Doctorate thesis of Narjes Ghanadi Karimi, approved by the School of Medicine, Guilan University of Medical Sciences, Rasht, Iran (Grant No.: 4920).
Authors contributions
Conceptualization and study design: Abbas Sedighinejad and Vali Imantalab; Analysis and interpretation of data: Leila Kanafivahed; Provision of study materials or patients: Seyed Sadegh Zargarnataj, Mahboobe Gholipour, and Narjes Ghanadi Karimi; Writing the original draft: Narjes Ghanadi Karimi; Review and editing: Gelareh Biazar; Final approval: Abbas Sedighinejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Anesthesiology Research Center, Guilan University of Medical Sciences, Rasht, Iran, with special thanks to the staff of the Cardiac Surgery ICU at Dr. Heshmat Hospital, Rasht, Iran.
Patients in group Q received 12.5 mg quetiapine (25 mg tablets manufactured by Fatek Shimi Pars Company - Iran) the morning of surgery and every 12 hours for 48 hours postoperatively. In this study, delirium was assessed using the confusion assessment method (CAM) for the ICU. The CAM-ICU assessment tool has a sensitivity between 95% and 100% and a specificity between 89% and 93% [12]. This questionnaire had four basic items: 1- Acute change in mental status, 2- Inattention, 3- Thought disorder, 4- Change in level of consciousness [13]. Postoperative delirium was assessed from the time the patient was admitted to the ICU until discharge from the unit. If the patient developed severe agitation, haloperidol 1-5 mg was administered. During the study, patients were assessed for possible side effects, such as long QT interval, hypotension, and elevated liver enzymes [14].
Statistical analysis: The collected data were analyzed by SPSS software, version 21 using the chi-square test, Fisher’s exact test, t-test, and repeated measures ANOVA. The parametric data were described as Mean±SD, and the nonparametric data were presented as median (range). A P<0.05 was considered significant.
Results
A total of 82 eligible CABG patients were enrolled in the study, with a mean age of 58.46±4.59 years in the quetiapine group and 57.97±5.01 years in the control group, as well as a mean BMI of 26.92±4.48 kg/m² in the quetiapine group and 27.61±4.04 kg/m² in the control group. More demographic details are shown in Table 1.

No significant difference was observed in terms of the demographic data and surgical characteristics of the individuals.
There was no association between patients’ co-morbidities (P=0.675), ASA class (P=0.154), age (P=0.648), BMI (P=0.468), and the occurrence of POD (Tables 1 and 2).

Medication status was compared between the two groups (Table 3).

The overall incidence of POD in the studied patients was 7.3%, with two cases in the intervention group (4.87%) and four patients in the control group (9.75%) developing POD. None of our patients showed serious adverse events, and no patients dropped out of the survey.
Discussion
Delirium is a mental state characterized by acute momentary deterioration of mental abilities, caused by a disruption in the regulation of neuronal activity. POD is a common complication of cardiac surgery [3, 15]. A recent meta-analysis showed that the incidence of POD in cardiac surgery was 32%, which is higher than in other types of surgeries. According to the available literature, a wide range of incidence rates for POD after cardiac surgery, from 2.8 to 63.8%, has been reported [16]. Studies have shown that, following surgery-related stress responses, the levels of inflammatory mediators such as IL-6 and CRP increase, leading to systemic and neurological inflammatory responses that can ultimately predispose individuals to postoperative delirium. The severity of surgical stress facilitates this process, particularly in patients with preoperative cerebral infarction and poor pain control [16-18]. This indicates the important role of anesthesia management in appropriately controlling pain and inflammatory reactions. So far, several interventions have been performed in cardiac surgery to control inflammatory reactions, with varying degrees of success [19-22].
Studies indicate that effective measures for reducing POD begin with careful preoperative assessments [23]. The choice of anesthesia method and selected drugs also affects the outcomes. For example, a study conducted in 2024 found that total intravenous anesthesia (TIVA) using propofol was associated with a lower incidence of delirium compared to sevoflurane-based anesthesia [24-26]. Additionally, a study by Suenaga et al. in 2025 showed that patients who underwent transcatheter aortic valve implantation (TAVI) surgery and developed delirium had a higher mortality rate and more adverse outcomes [27]. Lagonigro et al. also reported in 2025 an association between hyperglycemia—caused by stress responses in cardiac surgery, particularly in diabetic patients—and an increased incidence of POD [28]. Esfahanian et al. evaluated the effect of music on POD in CABG. In contrast to this study, a significant difference was observed between the case and control groups, with 3% in the case group compared to 12% in the control group [29]. Gonçalves et al., in their study on cardiac surgery patients in 2025, reported a prevalence of 18.3% for delirium, identifying age, gender, and inflammatory responses as predisposing factors [30]. A recent study reported that 40% of CABG patients developed POD, with female gender, perioperative anxiety and stress, surgery duration exceeding seven hours, and older age being predisposing factors [13]. Huang et al. demonstrated an association between POD and the patient’s gastrointestinal status concerning the presence of opportunistic pathogens [31].
Given the importance of the issue, both pharmacologic and non-pharmacologic interventions have been investigated [29]. This study is the first to examine the effect of quetiapine on post-CABG delirium, a drug previously used in CABG surgery with no significant adverse effects [7, 29, 32]. The primary outcome of this study indicated that the overall incidence of POD in CABG was 7.3%, which is lower than reported in similar studies [7, 32]. The results showed no significant difference between the intervention and control groups regarding complications, the incidence of POD, demographic characteristics, comorbidities, or medications. None of the variables studied—including literacy level, place of residence, employment status, comorbidities, age, BMI, and medications—were associated with the incidence of delirium. Although the number of delirium cases was higher in men than in women (4 patients compared to 1 patient), it is noteworthy that five of these six cases involved older patients and that this complication occurred more frequently among those taking medications. These findings align with several other studies [33]. The observed side effects related to quetiapine were minimal and manageable. The results indicated that the use of quetiapine did not significantly reduce the incidence of POD in patients undergoing CABG surgery when compared to the control group. There are some points worth mentioning. First, no similar study has been conducted to evaluate the effects of quetiapine on POD in CABG patients; only limited studies exist for other conditions [34, 35]. Therefore, meaningful comparisons with existing results were not possible.
Additionally, the mean age of CABG patients in this study was lower than in other studies, which partly justifies the lower incidence of POD, consistent with previous studies identifying older age as one of the most significant risk factors for delirium [15, 29, 36-38]. As mentioned, the results of studies are not consistent. It should be noted that the development of POD in CABG patients could be influenced by several factors. Patient population characteristics, such as age, gender, ASA class, habits, nutrition status, pre- operative mental state, and mood disorders, such as depression, as well as study methodology the assessment tool, who fills out the questionnaire, the level of accuracy, and the intervals between visits are all among the influential factors [13, 39-42]. Additionally, some studies report that other states of postoperative cognitive impairment might be considered delirium [18].
Overall, the findings of this study suggest that while quetiapine is widely used for various medical conditions, its effectiveness in preventing POD in CABG patients may be limited by this prescribing pattern. The overall low rate of POD in both groups could indicate that other factors, such as surgical and anesthesia techniques, as well as postoperative care and management of these patients, may play a more significant role in influencing delirium outcomes than pharmacological intervention alone [43]. The lack of significant difference in POD incidence between the quetiapine and control groups aligns with some previous studies that have also reported minimal benefits from antipsychotic medications in preventing delirium in surgical patients. However, the small sample size, the specific patient population, and other limitations of this study should be considered. Future studies should explore alternative strategies for preventing delirium. Furthermore, investigating different dosages or timing of quetiapine administration may yield better results. This comprehensive approach will help delineate strategies for preventing POD and improving outcomes for CABG surgery patients.
Conclusion
In conclusion while quetiapine had a favorable safety profile, this study did not find a significant benefit in preventing postoperative delirium in patients undergoing CABG surgery. Further well-planned clinical trials with other doses of the drug, larger sample sizes, and diverse patient populations are needed to better understand the role of quetiapine in the prevention of POD.
Limitations
The relatively short follow-up period post-surgery may not detect all cases of POD, and the assessment method (CAM-ICU) may not identify all cases of delirium, particularly those with less severe symptoms. The degree of pre-operative anxiety was not assessed, which is influential and should be considered one of the limitations of this study. Additionally, the study was conducted at a single center, which may limit the external validity of the findings.
Ethical Considerations
Compliance with ethical guidelines
This study protocol was approved by the Research Ethics Committee of the Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1402.242), and the research was registered at the Iranian Registry of Clinical Trials (IRCT) Tehran, Iran (Code: IRCT20130525013456N7). Moreover, informed consent was obtained from the patients who agreed to participate.
Funding
This study was extracted from the General Medical Doctorate thesis of Narjes Ghanadi Karimi, approved by the School of Medicine, Guilan University of Medical Sciences, Rasht, Iran (Grant No.: 4920).
Authors contributions
Conceptualization and study design: Abbas Sedighinejad and Vali Imantalab; Analysis and interpretation of data: Leila Kanafivahed; Provision of study materials or patients: Seyed Sadegh Zargarnataj, Mahboobe Gholipour, and Narjes Ghanadi Karimi; Writing the original draft: Narjes Ghanadi Karimi; Review and editing: Gelareh Biazar; Final approval: Abbas Sedighinejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the Anesthesiology Research Center, Guilan University of Medical Sciences, Rasht, Iran, with special thanks to the staff of the Cardiac Surgery ICU at Dr. Heshmat Hospital, Rasht, Iran.
References
- Tilouche N, Hassen MF, Ali HBS, Jaoued O, Gharbi R, El Atrous SS. Delirium in the intensive care unit: Incidence, risk factors, and impact on outcome. Indian J Crit Care Med. 2018; 22(3):144-9. [DOI:10.4103/ijccm.IJCCM_244_17] [PMID]
- Martin BJ, Buth KJ, Arora RC, Baskett RJ. Delirium as a predictor of sepsis in post-coronary artery bypass grafting patients: A retrospective cohort study. Crit Care. 2010; n14(5):R171. [DOI:10.1186/cc9273] [PMID]
- Mattimore D, Fischl A, Christophides A, Cuenca J, Davidson S, Jin Z, et al. Delirium after cardiac surgery-A narrative review. Brain Sci. 2023;1 3(12):1682. [DOI:10.3390/brainsci13121682] [PMID]
- Kotfis K, Szylińska A, Listewnik M, Strzelbicka M, Brykczyński M, Rotter I, et al. Early delirium after cardiac surgery: An analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018; 13:1061-70. [DOI:10.2147/CIA.S166909] [PMID]
- Ely EW, Stephens RK, Jackson JC, Thomason JW, Truman B, Gordon S, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: A survey of 912 healthcare professionals. Crit Care Med. 2004; 32(1):106-12. [DOI:10.1097/01.CCM.0000098033.94737.84] [PMID]
- Saller T, V Dossow V, Hofmann-Kiefer K. [Knowledge and implementation of the S3 guideline on delirium management in Germany (German)]. Anaesthesist. 2016; 65(10):755-62. [DOI:10.1007/s00101-016-0218-8] [PMID]
- Alshaya AI, Gilmore JF, Nashett RM, Kovacevic MP, Dube KM, Assiri IM, et al. Cardiac safety of clonidine and quetiapine in post-cardiac surgery intensive care unit patients. J Pharm Pract. 2023; 36(2):309-14. [DOI:10.1177/08971900211044687] [PMID]
- Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016; 3(3):CD005563. [PMID]
- Cottuli de Cothi E, Perry R, Kota R, Walker-Smith T, Barnes JD, Pufulete M, et al. Pharmacological and non-pharmacological interventions to prevent delirium after cardiac surgery: A protocol for a systematic review and meta-analysis. BMJ Open. 2023; 13(12):e076919. [DOI:10.1136/bmjopen-2023-076919] [PMID]
- DAILYMED. Label: SEROQUEL- quetiapine tablet, film coated. [Internet]. 2024 [Updated 2025 September 29]. Available from: [Link]
- Drugs.com. QUEtiapine (Monograph) [Internet] 2017. [Updated 2025 September 29]. Available from: [Link]
- Tomasi CD, Grandi C, Salluh J, Soares M, Giombelli VR, Cascaes S, et al. Comparison of CAM-ICU and ICDSC for the detection of delirium in critically ill patients focusing on relevant clinical outcomes. J Crit Care. 2012; 27(2):212-7. [DOI:10.1016/j.jcrc.2011.05.015] [PMID]
- Oldham MA, Kukla B, Walsh P, Lee HB. Sex differences in delirium after coronary artery bypass graft surgery and perioperative neuropsychiatric conditions: A secondary analysis of a cohort study. J Geriatr Psychiatry Neurol. 2024; 37(6):473-81.[DOI:10.1177/08919887241246226] [PMID]
- Cleveland Clinic. Quetiapine (Seroquel): Uses & side effects. Ohio: Cleveland Clinic; 2025. [Link]
- Mahrose R, ElSerwi H, Maurice A, Elsersi M. Postoperative delirium after coronary artery bypass graft surgery: Dexmedetomidine infusion alone or with the addition of oral melatonin. Egypt J Anaest. 2021; 37(1):62-8. [DOI:10.1080/11101849.2021.1885956]
- Igwe EO, Nealon J, O'Shaughnessy P, Bowden A, Chang HR, Ho MH, et al. Incidence of postoperative delirium in older adults undergoing surgical procedures: A systematic literature review and meta-analysis. Worldviews Evid Based Nurs. 2023; 20(3):220-37. [DOI:10.1111/wvn.12649] [PMID]
- Noah AM, Almghairbi D, Evley R, Moppett IK. Preoperative inflammatory mediators and postoperative delirium: Systematic review and meta-analysis. Br J Anaesth. 2021; 127(3):424-34. [DOI:10.1016/j.bja.2021.04.033] [PMID]
- Greaves D, Psaltis PJ, Ross TJ, Davis D, Smith AE, Boord MS, et al. Cognitive outcomes following coronary artery bypass grafting: A systematic review and meta-analysis of 91,829 patients. Int J Cardiol. 2019; 289:43-9. [DOI:10.1016/j.ijcard.2019.04.065] [PMID]
- Makiabadi E, Nakhaeizadeh R, Soleimani M, Nasrollahzadeh J. Effects of perioperative vitamin E and zinc co-supplementation on systemic inflammation and length of stay following coronary artery bypass graft surgery: A randomized controlled trial. Eur J Clin Nutr. 2024; 78(2):120-7. [DOI:10.1038/s41430-023-01356-x] [PMID]
- Banerjee D, Feng J, Sellke FW. Strategies to attenuate maladaptive inflammatory response associated with cardiopulmonary bypass. Front Surg. 2024; 11:1224068. [DOI:10.3389/fsurg.2024.1224068] [PMID]
- Squiccimarro E, Stasi A, Lorusso R, Paparella D. Narrative review of the systemic inflammatory reaction to cardiac surgery and cardiopulmonary bypass. Artif Organs. 2022; 46(4):568-577. [DOI:10.1111/aor.14171] [PMID]
- Sarhan AM, Awad AK, Alassiri AK, Abd-Alkhaleq MS, Al-Asmar R, Gonnah AR. Efficacy of selenium on patients undergoing cardiac surgery: A meta-analysis of randomized controlled trials. J Cardiothorac Surg. 2024; 19(1):264. [DOI:10.1186/s13019-024-02761-4] [PMID]
- Zhao BS, Zhai WQ, Ren M, Zhang Z, Han JG. Systemic Immune Inflammatory Index (SII) and systemic inflammatory response index (SIRI) as predictors of postoperative delirium in patients undergoing off-pump coronary artery bypass grafting (OPCABG) with cerebral infarction. BMC Surg. 2024; 24(1):338. [DOI:10.1186/s12893-024-02598-7] [PMID]
- Zhao N, Qin R, Liu B, Zhang D. Sevoflurane versus propofol on immediate postoperative cognitive dysfunction in patients undergoing cardiac surgery under cardiopulmonary bypass: A comparative analysis. J Cardiothorac Surg. 2025; 20(1):54. [DOI:10.1186/s13019-024-03327-0] [PMID]
- Maroufi SS, Kiaei MM, Aligholizadeh M, Saei A, Sangi S, Akbarpour P. The effect of ketamine administration on the incidence of delirium after coronary artery bypass graft surgery: A scoping review. J Cell Mol Anesth. 2024; 9(3): e147124. [DOI:10.5812/jcma-147124]
- Varsha AV, Unnikrishnan KP, Saravana Babu MS, Raman SP, Koshy T. Comparison of propofol-based total intravenous anesthesia versus volatile anesthesia with sevoflurane for postoperative delirium in adult coronary artery bypass grafting surgery: A prospective randomized single-blinded study. J Cardiothorac Vasc Anesth. 2024; 38(9):1932-40. [DOI:10.1053/j.jvca.2024.05.027] [PMID]
- Suenaga T, Ishizu K, Shirai S, Yoshida S, Wakugawa H, Miyahara K, et ak. Association between delirium severity and prognosis following Transcatheter aortic valve implantation. J Cardiol. 2025; 86(1):38-47. [DOI:10.1016/j.jjcc.2025.01.004] [PMID]
- Lagonigro E, Pansini A, Mone P, Guerra G, Komici K, Fantini C. The role of stress hyperglycemia on delirium onset. J Clin Med. 2025; 14(2):407. [DOI:10.3390/jcm14020407] [PMID]
- Esfahanian F, Mirmohammadsadeghi A, Gholami H, Neshat S, Mansouri M, Sadeghi M, et al. Using music for the prevention of delirium in patients after coronary artery bypass graft surgery: A randomized clinical trial. J Cardiothorac Vasc Anesth. 2022; 36(12):4341-6. [DOI:10.1053/j.jvca.2022.09.007] [PMID]
- Gonçalves MCB, Khera T, Otu HH, Narayanan S, Dillon ST, Shanker A, et al. Multivariable Predictive Model of Postoperative Delirium in Cardiac Surgery Patients: Proteomic and demographic contributions. Anesth Analg. 2025; 140(2):476-87. [DOI:10.1213/ANE.0000000000007293] [PMID]
- Huang P, Di L, Cui S, Wang X, Cao T, Jiang S, et al. Postoperative delirium after cardiac surgery associated with perioperative gut microbiota dysbiosis: Evidence from human and antibiotic-treated mouse model. Anaesth Crit Care Pain Med. 2025; 44(2):101484. [DOI:10.1016/j.accpm.2025.101484] [PMID]
- Mirmohammadsadeghi A, Nariman I, Chitsaz A. Post-Coronary Artery Bypass Graft Surgery Insomnia: Quetiapine vs Alprazolam. Iran Heart J. 2021; 22(3):74-80. [Link]
- Singh M, Spence J, Shah K, Duncan AE, Kimmaliardjuk D, Sessler DI, et al. Intraoperative high and low blood pressures are not associated with delirium after cardiac surgery: A retrospective cohort study. J Clin Anesth. 2025; 100:111686. [DOI:10.1016/j.jclinane.2024.111686] [PMID]
- Almeida F, Albuquerque E, Murta I. Delirium Induced by Quetiapine and the Potential Role of Norquetiapine. Front Neurosci. 2019; 13:886. [DOI:10.3389/fnins.2019.00886] [PMID]
- Hawkins SB, Bucklin M, Muzyk AJ. Quetiapine for the treatment of delirium. J Hosp Med. 2013; 8(4):215-20. [DOI:10.1002/jhm.2019] [PMID]
- Singh A, Garg V, Mehta Y, Bhan A, Trehan N. Perioperative dexmedetomidine reduces delirium after coronary artery bypass graft surgery: A prospective, single-blind, observational study. Ann Card Anaesth. 2022; 25(4):490-7. [DOI:10.4103/aca.aca_45_21] [PMID]
- Shi C, Jin J, Qiao L, Li T, Ma J, Ma Z. Effect of perioperative administration of dexmedetomidine on delirium after cardiac surgery in elderly patients: a double-blinded, multi-center, randomized study. Clin Interv Aging. 2019; 14:571-5. [DOI:10.2147/CIA.S194476] [PMID]
- Han Y, Tian Y, Wu J, Zhu X, Wang W, Zeng Z, et al. Melatonin and its analogs for prevention of post-cardiac surgery delirium: A systematic review and meta-analysis. Front Cardiovasc Med. 2022; 9:888211. [DOI:10.3389/fcvm.2022.888211] [PMID]
- Li J, Meng D, Chang C, Fu B, Xie C, Wu Z, et al. Risk factors for delirium after coronary artery bypass grafting in elderly patients. Ann Transl Med. 2021; 9(22):1666. [DOI:10.21037/atm-21-5160] [PMID]
- Velayati A, Vahdat Shariatpanahi M, Shahbazi E, Vahdat Shariatpanahi Z. Association between preoperative nutritional status and postoperative delirium in individuals with coronary artery bypass graft surgery: A prospective cohort study. Nutrition. 2019; 66:227-32. [DOI:10.1016/j.nut.2019.06.006] [PMID]
- Velayati A, Vahdat Shariatpanahi M, Dehghan S, Zayeri F, Vahdat Shariatpanahi Z. Vitamin D and postoperative delirium after coronary artery bypass grafting: A prospective cohort study. J Cardiothorac Vasc Anesth. 2020; 34(7):1774-9. [DOI:10.1053/j.jvca.2020.02.008] [PMID]
- Greaves D, Psaltis PJ, Davis DHJ, Ross TJ, Ghezzi ES, Lampit A, et al. Risk factors for delirium and cognitive decline following coronary artery bypass grafting surgery: A systematic review and meta-analysis. J Am Heart Assoc. 2020; 9(22):e017275. [DOI:10.1161/JAHA.120.017275] [PMID]
- Tao R, Wang XW, Pang LJ, Cheng J, Wang YM, Gao GQ, et al. Pharmacologic prevention of postoperative delirium after on-pump cardiac surgery: A meta-analysis of randomized trials. Medicine (Baltimore). 2018; 97(43):e12771. [DOI:10.1097/MD.0000000000012771] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2025/05/28 | Accepted: 2025/08/17 | Published: 2025/10/26
Received: 2025/05/28 | Accepted: 2025/08/17 | Published: 2025/10/26
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |