Mon, Feb 2, 2026
Volume 11, Issue 4 (Autumn 2025)
Caspian J Neurol Sci 2025, 11(4): 295-305 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alimohamadi N, Khafri S, Dehghan Nayeri N, Nadali J, Khorvash F, Alijanpour S, et al . The Caspian Nursing Process Project: A Structured Nursing Approach to New-onset Constipation After Stroke. Caspian J Neurol Sci 2025; 11 (4) :295-305
URL: http://cjns.gums.ac.ir/article-1-790-en.html
URL: http://cjns.gums.ac.ir/article-1-790-en.html
Nasrollah Alimohamadi1 

 , Soraya Khafri2
, Soraya Khafri2 

 , Nahid Dehghan Nayeri3
, Nahid Dehghan Nayeri3 

 , Javad Nadali4
, Javad Nadali4 

 , Fariborz Khorvash5
, Fariborz Khorvash5 

 , Shayan Alijanpour *6
, Shayan Alijanpour *6 

 , Seyedeh Fatemeh Hosseini Aghamolki7
, Seyedeh Fatemeh Hosseini Aghamolki7 

 , Anahita Divani8
, Anahita Divani8 




 , Soraya Khafri2
, Soraya Khafri2 

 , Nahid Dehghan Nayeri3
, Nahid Dehghan Nayeri3 

 , Javad Nadali4
, Javad Nadali4 

 , Fariborz Khorvash5
, Fariborz Khorvash5 

 , Shayan Alijanpour *6
, Shayan Alijanpour *6 

 , Seyedeh Fatemeh Hosseini Aghamolki7
, Seyedeh Fatemeh Hosseini Aghamolki7 

 , Anahita Divani8
, Anahita Divani8 


1- Nursing and Midwifery Care Research Center, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Biostatistics and Epidemiology, Babol University of Medical Sciences, Babol, Iran.
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
4- Student Research Committee, School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran.
5- Isfahan Neurosciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
6- Department of Nursing, School of Nursing and Midwifery, Babol University of Medical Sciences, Babol, Iran. ,sh.alijanpour@mubabol.ac.ir
7- Department of Emergency, Yahyanezhad Hospital, Babol University of Medical Sciences, Babol, Iran.
8- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Biostatistics and Epidemiology, Babol University of Medical Sciences, Babol, Iran.
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
4- Student Research Committee, School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran.
5- Isfahan Neurosciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
6- Department of Nursing, School of Nursing and Midwifery, Babol University of Medical Sciences, Babol, Iran. ,
7- Department of Emergency, Yahyanezhad Hospital, Babol University of Medical Sciences, Babol, Iran.
8- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1314 kb]
(482 Downloads)
| Abstract (HTML) (419 Views)
Full-Text: (279 Views)
Introduction
According to the World Health Organization (WHO), stroke affects about 15 million people globally each year [1]. Several studies indicate that as many as 96% of patients hospitalized for stroke experience medical or neurological complications during their hospital stay, which significantly increases the mortality rate [2]. Although the primary effects of stroke are neurological in nature, the organ systems that can be affected continue to increase and include the gastrointestinal tract, particularly in cases of constipation [3]. According to Alijanpour et al., new-onset constipation is secondary constipation arising from multiple factors after a cerebrovascular accident, occurring in patients who had no prior signs or symptoms of constipation before the stroke [4]. A systematic review and meta-analysis showed that the incidence of constipation in the acute stage is 36% to 54% [5]. The risks of this complication ranged from 16% to 66% [4]. Patients who developed new-onset constipation during hospitalization had longer hospital stays, which negatively impacted their QoL and social activities. The multifactorial etiology of post-stroke constipation encompasses reduced mobility, dietary modifications, medication side effects (e.g. opioids, anticholinergics), and neurogenic disruptions in colonic motility regulation [6]. Evidence-based interventions include early mobilization, reducing anticholinergic medications, giving stool softeners, and personalized hydration and fiber plans. Nurse-led bowel management programs show effectiveness in improving evacuation outcomes, focusing on proactive monitoring and patient-centered education [4]. Constipation, as defined by the North American Nursing Diagnosis Association (NANDA-I), places nurses in a prime position to provide comprehensive care for affected patients [7, 8]. According to the NANDA, nursing’s roles in managing constipation include using non-medical methods, like diet changes, lifestyle modifications, and exercise to improve bowel movements and well-being [4].
Recent research has highlighted the importance of structured nursing interventions in managing new-onset constipation after stroke. However, there remains a significant gap in the literature regarding the development and implementation of comprehensive nursing programs based on the nursing process for this specific condition. While studies have demonstrated the effectiveness of individual interventions, such as early mobilization and dietary modifications, there is a lack of standardized, process-oriented nursing protocols that address the multifaceted nature of post-stroke constipation management [4, 9]. Yet, there remains uncertainty about the extent of the nurse’s role in addressing constipation, and clear guidelines are lacking [7, 10]. Managing constipation can be complex, often seen as minor. However, it can seriously affect well-being and may hide more serious health issues [11].
This gap underscores the necessity for developing evidence-based nursing programs that incorporate assessment, diagnosis, planning, implementation, and evaluation stages of the nursing process. This study aimed to develop and validate a comprehensive nursing plan for managing new-onset constipation in acute stroke patients using the RAND/UCLA appropriateness method and the Delphi technique. This approach will synthesize expert opinion and available evidence to create a consensus-based, clinically relevant protocol. By utilizing these rigorous methodologies, we sought to establish a standardized nursing approach that can be widely implemented in stroke care units, potentially improving patient outcomes and quality of life (QoL).
Materials and Methods
This multi-method study is part of a larger research project (Caspian nursing process project (CNP2)), which was conducted with the combination of Delphi and RAND methods (RAM) in three phases [12]. The first phase was a protocol study [4], the second was the development of the care plan for new-onset constipation, and the third phase was an intervention with a care plan, which was defined in the second phase [4]. This study is the result of the second phase and involved several steps:
1. Searching for scientific sources
2. Formal content validity
3. RAM and Delphi methods
4. Results and changes made at the Delphi stage
5. The panel of experts
Research design
1. Searching for scientific sources: The preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline was used in this study [13]. A literature search across ScienceDirect, Cochrane Library, Medline, Scopus, PubMed, and Google Scholar with keywords and MeSH terms, including “stroke”, “constipation”, “bowel management”, “bowel strategy”, “post stroke constipation”, and “new-onset constipation” was conducted. The EndNote software, version 9 (Clarivate Analytics; Philadelphia, PA, USA) was used to remove duplicates. Original articles, studies published in English, and full-text manuscripts were enrolled. All included studies were conducted on humans. We also excluded studies where the diagnostic criteria of constipation were unclear. Sixty-eight articles from 2009 to 2019 were identified. Then, two authors screened potentially eligible studies in terms of the title and abstract according to the checklist, and 11 articles were selected. Any disagreements were resolved by discussions among the two reviewers or by consultations with the third reviewer.
In addition to database searching, hand searching targeted several specialized sites: World Gastroenterology Organization (WGO) [14], American Gastroenterology Association (AGA) [15], and the British Institute of Health and Care Excellence (NICE) [16]. This search yielded six guidelines related to constipation management. These guidelines were appraised using AGREE II (the appraisal of guidelines for research & evaluation), and three guidelines were approved. Finally, 14 articles and guidelines were included in the study.
After the data were gathered in the last step, the primary nursing care plan was defined according to the nursing process and reviewed by the research team. It was then sent for face and content validity.
2. Face and content validity: Face and content validity of the primary nursing care plan were obtained from the supervisor and the advisor of the current study, along with 5 faculty members of the Isfahan School of Nursing and Midwifery. Then, a draft of the nursing care plan was revised and sent for RAM and Delphi steps.
3. RAM and Delphi methods: The RAM includes priority, usefulness, applicability, conceptualization, and who is authorized to provide service. A set of evidence-based recommendations for the new-onset constipation care plan was developed from credible sources and articles, organized according to the nursing process, and presented in four tables: Assessment, goals and outcomes, nursing diagnoses, interventions, and evaluation. Twenty two authorities from different professions of Isfahan, Tehran and Babol University of Medical Sciences were enrolled, including 11 nurses (50%), 4 neurologists (18.2%), 2 fellows in intensive care (9.1%), 2 internal medicine specialists (9.1%), 1 surgeon (4.5%), 1 nutrition specialist (4.5%), and 1 emergency medicine specialist (4.5%). Using the Delphi method to gather expert perspectives, a written care plan aligned with the nursing process was completed. The draft of this care plan was delivered to the experts for review, with a request to evaluate it using a 5-point Likert scale and to provide any further care or advice in the form of proposals. The ratings used a 1-to-5 scale across four domains (priority, benefit, applicability, and concept) for each recommendation, followed by comments on the recommendations in the relevant column.
4. Results and changes made at the Delphi stage: In this stage, the results obtained from the participant survey indicated that each item with 70% agreement and above was retained, while items with <70% agreement were reconsidered.
5. The panel of experts: Due to a consensus of over 70% in the last stage, the panel of experts was deemed unnecessary. After these steps, we prepared this care plan in the nursing process structure. The results of each step were published in the last study. In this paper, we presented the Caspian care plan for new-onset constipation after stroke, which was developed using a scientific method.
Results
CNP
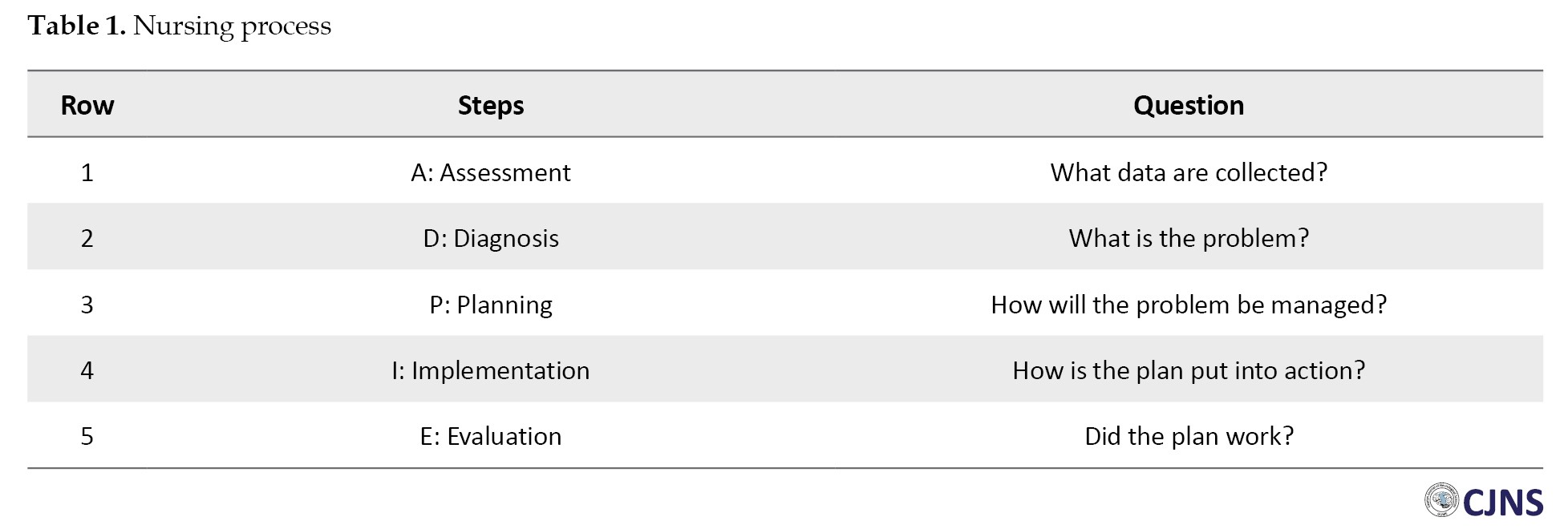
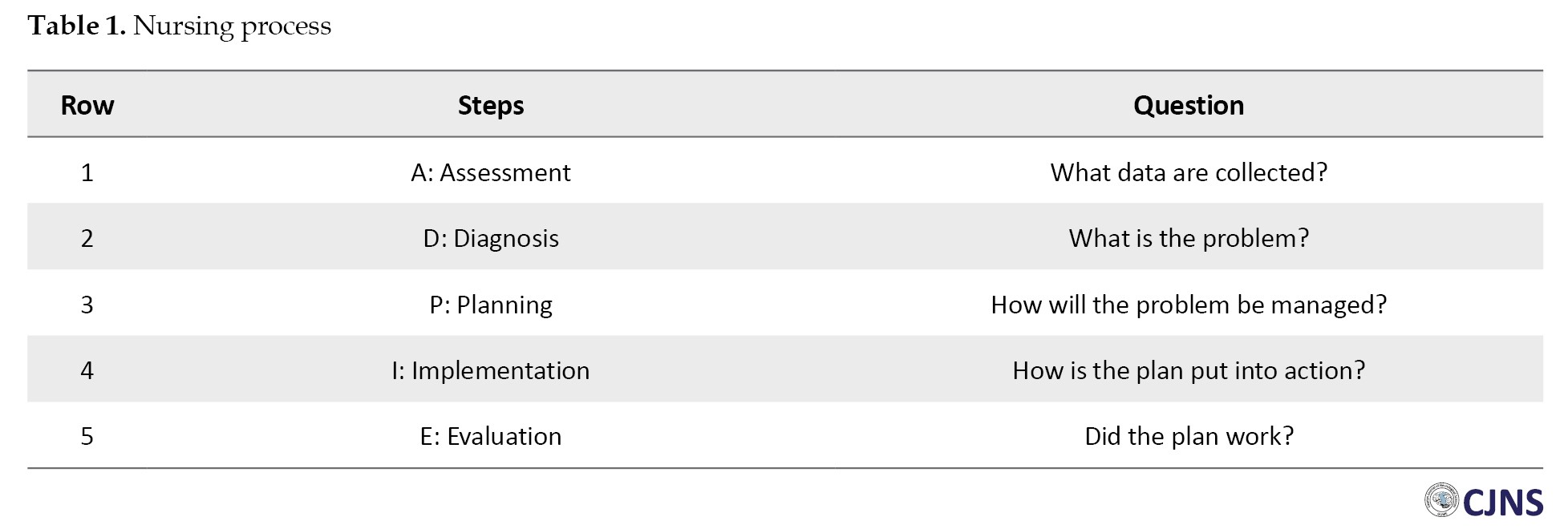
The nursing process is a goal-directed framework that guides and organizes nursing care. It involves five major steps (ADPIE), which are shown in Table 1.
Assessment
Focused constipation assessment: When performing a comprehensive evaluation of a client’s constipation, it is important to gather both subjective and objective information.
History: Frequently occurring symptoms associated with the abdomen and specific to gastrointestinal disorders encompass indigestion, nausea, vomiting, hematemesis, abdominal pain, dysphagia and odynophagia, alterations in bowel function, constipation or diarrhea, and jaundice [17].
A-chief complaint: Some typical indications of constipation include abdominal discomfort, tenderness, palpable muscle resistance, loss of appetite, borborygmi, reduced stool frequency or volume, abdominal distension, fatigue, and hard, formed stools [18].
B-signs and symptoms (SOCRATES): This includes site, onset, character, radiation (if the symptom is pain or discomfort), alleviating factors, timing, exacerbating factors, and severity [19].
C-present illness: It is important to inquire about the frequency and consistency of bowel movements (using the Bristol stool scale), any discomfort during bowel movements, the presence of blood or black, tarry stool (melena), stool color (white or gray stools indicating potential liver or gallbladder disease), and any associated symptoms, such as jaundice or icteric sclera.
D-past history: In this step, we asked about drug and treatment history, social history, and family history of patients.
E-review of systems (ROS): This involves evaluating nutrition (including inadequate fiber consumption, anorexia, and insufficient food and fluid intake), as well as considering lifestyle, behavior, and environmental factors (such as lack of privacy and assistance during toileting), cultural influences, and other factors (such as inactivity, age, depression, and sedation) [20].
F-physical examination: Ensure that the patient is comfortable before proceeding with the examination by following the sequence of “look, listen, and feel” [17].
Inspection: In cases of constipation, this may involve examining the contour of the abdomen (rounded, protuberant, scaphoid, flat), skin characteristics (lesions, hernias, scars, striae [silver or purple], tattoos, ecchymosis, hair distribution), and distension (generalized distension of the abdomen can be caused by one of the five Fs: Fluid [ascites], fetus, feces, fat, flatus). Also, we assessed the umbilicus (for Cullen’s sign) and other factors (such as gravid uterus, nodules, ascites, peristalsis, movement, aortic pulsations, and vein visibility) [21].
Auscultation: This method is used to listen to the sounds of the body. We used the diaphragm for bowel sounds and the bell for vascular sounds, bruits, friction rubs, and venous hums. We listened for clicks/gurgles, known as “borborygmi,” which typically occur 5-35 times per minute and are usually more active after a meal. The absence of bowel sounds should be established only after 3 minutes of continuous listening.
If there is an absence of bowel sounds, it is recommended to conduct a thorough assessment by listening for a duration of five minutes to confirm their absence [22].
Percussion: To perform percussion, one should place two fingers over a specific area and tap on them with the fingertips of the other hand [21]. When percussing the abdomen, the predominant sound should be tympany. In the supine position, air tends to accumulate at the top of the abdomen, resulting in a drum-like sound characteristic of tympany. Dullness, on the other hand, is commonly observed over solid organs or masses, such as the liver, spleen, or a distended bladder [23].
Palpation: Important indicators include ‘guarding’, in which the patient instinctively shields their abdomen, suggesting pain, and ‘rebound tenderness’, characterized by a painful response following deep palpation and hand removal [21].
G-scale for collection of data: We suggest using the Rome criteria IV, which is widely accepted as an international standard in research, to describe post-stroke constipation.
The following criteria are involved in the diagnosis and treatment of constipation, of which at least two must be satisfied:
Experiencing strain during a minimum of 25% of bowel movements.
Passing lumpy or hard stools in at least 25% of bowel movements.
A feeling of incomplete bowel emptying occurs in at least 25% of instances.
Sensing an obstruction or blockage in the anorectal area during at least 25% of defecations [24]. These symptoms must have been present after the stroke. However, a specific instrument for the evaluation of new-onset stroke constipation was not found.
The Bristol stool scale serves as a useful instrument for monitoring colon transit, particularly in cases where bowel frequency and stool consistency are not in concordance. Additionally, abdominal radiography can provide supplementary information to healthcare professionals [25].
H-paraclinical test: Routine testing may not always be necessary. Nevertheless, in instances of clinical suspicion, it is crucial to assess calcium levels and thyroid function. Extensive investigations are warranted for severe symptoms, abrupt alterations in bowel habits, presence of blood in the stool, or, in the case of older adults, taking into account their health status and stage of disease.
Nursing diagnosis
To reach a diagnosis from nursing assessment, nurses need to follow these steps [26-28]:
Data collection or assessment: In this initial stage of the nursing process, you collect information from the patient that is both objective and subjective, including vital signs, medical history, physical examination, and psychosocial assessment.
Data analysis and organization: This second step involves analyzing and interpreting the collected data, identifying patient strengths and limitations, and prioritizing the patient’s needs.
Formulating your nursing diagnoses: This is the third step, where you use the data analysis and the NANDA-I taxonomy to select the most appropriate nursing diagnosis.
Setting priorities: This is the fourth step, where you rank the nursing diagnoses according to their urgency and importance. You can use various frameworks to guide your prioritization, such as Maslow’s hierarchy of needs, ABCDE, or clinical judgment.
Establishing client goals and desired outcomes: This is the fifth step, where you set realistic and measurable goals for the patient based on the nursing diagnosis. The goals should be specific, measurable, attainable, relevant, and time-bound (SMART).
The nurse will assess the gathered information to ascertain the patient’s status and requirements. This procedure encompasses the analysis of data, identification of health concerns, potential risks, and strengths, as well as the formulation of diagnostic statements regarding actual or potential health issues. In some cases, multiple diagnoses may be assigned to a single patient. The utilization of clinical judgment in formulating nursing diagnoses is instrumental in the planning and execution of patient care, including the identification of key nursing diagnoses associated with constipation [27]:
Constipation associated with water and electrolyte disturbance following a stroke.
Constipation associated with inadequate fiber intake following a stroke.
Constipation associated with low physical activity following a stroke.
Constipation associated with taking multiple medications following a stroke.
Constipation due to drug side effects after a stroke.
Constipation associated with nerve damage following a stroke.
Lack of knowledge about constipation management following a stroke.
Planning
The planning phase involves the formulation of goals and outcomes that have a direct impact on patient care, in accordance with evidence-based practice (evidence-based practice) guidelines [27].
Prevention of bowel dysfunction.
Increased awareness of bowel care needs.
Steady state in water and electrolytes.
Placement in types 3 or 4 of the Bristol criteria.
No evidence of constipation according to the Rome IV criteria.
Implementation
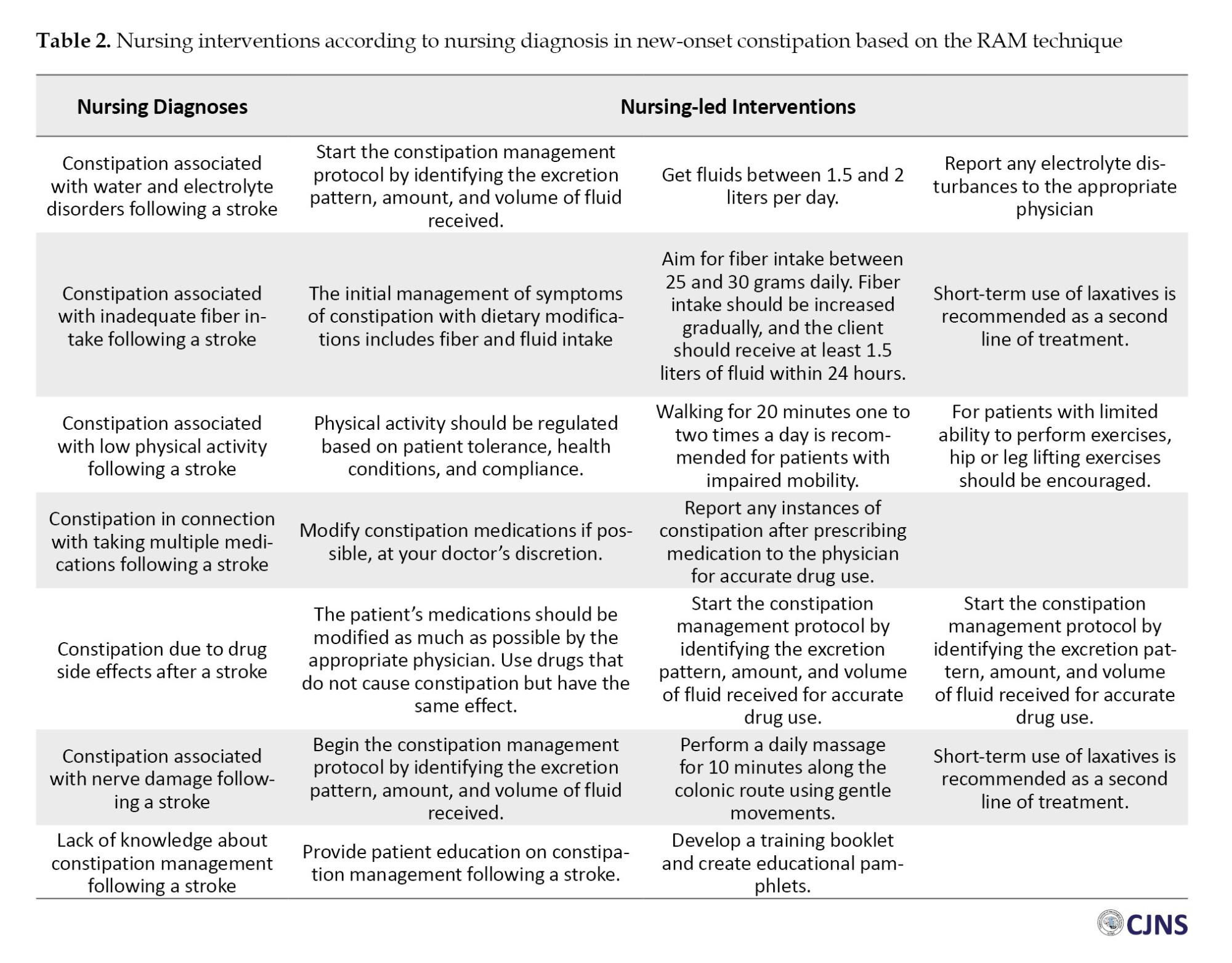
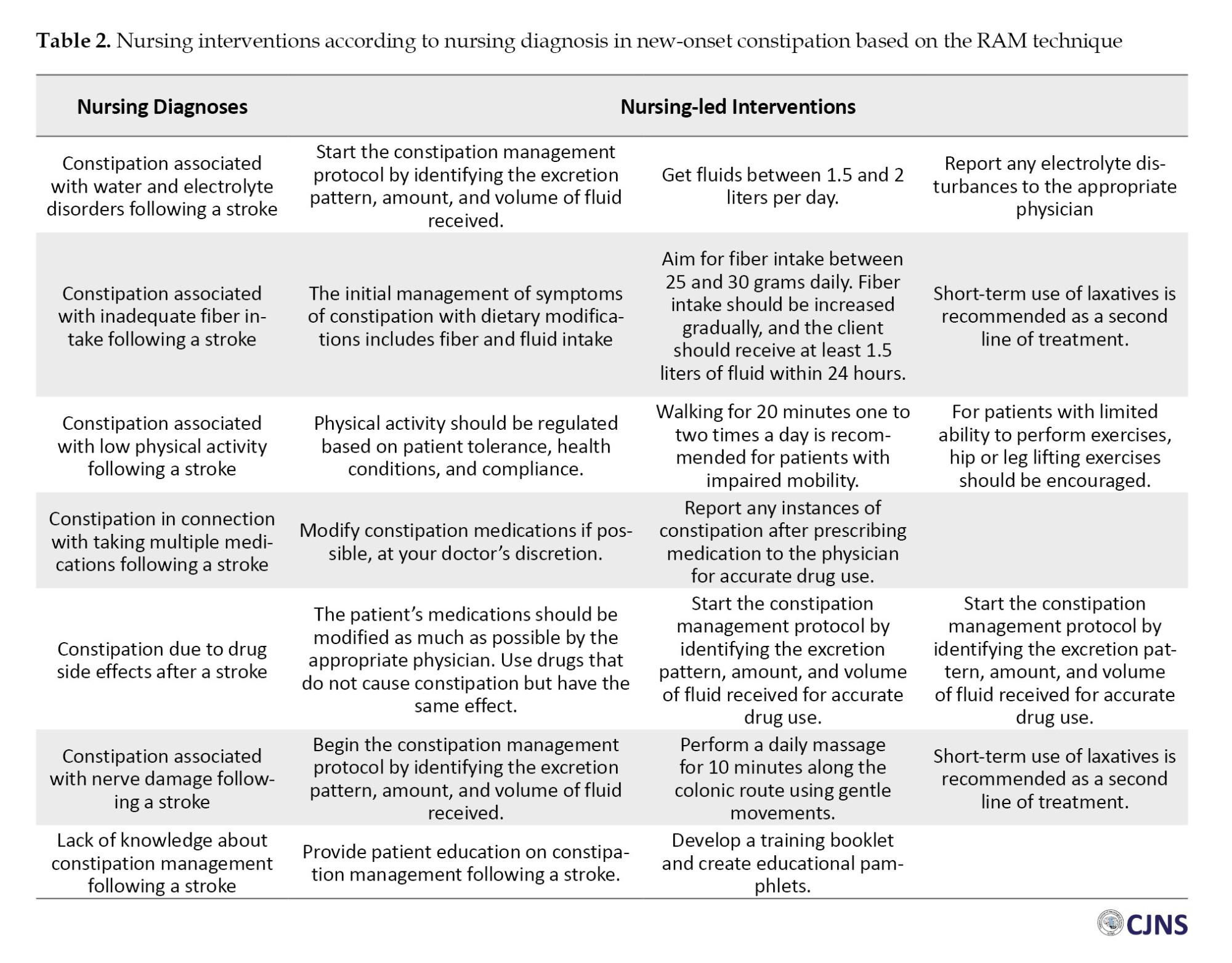
Nursing-led interventions generally include seven items, including physical activity and exercise, modified drug regimen, diet, fiber therapy, abdominal massage therapy, patient training, and patient follow-up. The practice nurse should inquire about fluid and dietary fiber intake, activity levels, and all medications the person is taking, including prescribed and nonprescription drugs [29, 30]. The intervention was performed according to each nursing diagnosis (Table 2).
Physical activity and exercise: For individuals who engage in regular physical activity, walking is the most prevalent form of exercise. However, some participants are unable to engage in physical activity due to various reasons, such as permanent immobility caused by conditions, like paraplegia, arthritis, or emphysema, temporary immobility during hospitalization or recovery, adverse weather conditions, safety concerns when exercising alone, or the risk of sustaining injuries, such as fractured limbs, during physical activity.
Modified drug regimen: Therapeutic drugs associated with constipating effects that were included in the care plan were replaced by a neurologist, if appropriate. If the drug was not available, the number and types of constipation were recorded in a questionnaire.
Diet: Participants consume various vegetables, including hot ones or salads, to prevent constipation. Prunes or prune juice are commonly used as effective laxatives. Some find liquorice sticks helpful, while others use pepitos or sorbitol-containing sweets [31]. Recently, herbal medicine [30, 32] and acupoint herbal patching [33] have also been recommended to treat post-stroke constipation.
Fiber therapy: Dietary fiber can help with mild to moderate constipation, but not severe cases. It is recommended to consume 20-35 grams daily from sources, like whole wheat bread, unrefined cereals, citrus fruits, and vegetables. However, insoluble fiber, like cereal bran, can cause gas, bloating, and delay gastric emptying, reducing appetite. It is best to start with low doses of fiber supplements and gradually increase to 20-25 grams per day, while also increasing water intake [34].
Abdominal message therapy: Massage therapy, based on various studies, was performed ten minutes daily [30]. Abdominal massage, according to the study by Alijanpour et al., can be performed using longitudinal, transverse, and rotational movements of the colon [4]. Moreover, acupressure and moxibustion [35], as well as acupoint embedding therapy, which is a therapeutic technique applied at specific acupuncture points, are recommended to treat post-stroke constipation [36].
Patient training: At discharge, provide the patient with a booklet addressing new-onset stroke constipation, emphasizing self-care practices and self-efficacy [30]. Also, in coordination with a neurologist, the patient should receive practical training in massage therapy, learn to work with the Bristol tool to determine the consistency of stools after discharge, and understand how to contact the treatment team by telephone or social media. Educational content for patients and partners should include familiarity with the food pyramid, food groups, weight control methods, lifestyle changes, drug side effects, laxative foods, constipated foods, high-fiber foods, constipation medications, water intake, physical activity, stress reduction, and how to use herbal laxatives correctly. Moreover, a study suggests that structured bowel programs and nurse-led interventions in bowel care have a significant effect on improving bowel evacuations [30].
Patient follow-up: After discharge, patients should be followed for four weeks in two steps: Communicating with the treatment team and evaluating how training and counseling influenced outcomes.
Patient relationship with care team
Communication with the treatment team should include asking questions or raising complaints from the patients or their companions, patient consultations with a physician or research nurse in case of need, and scheduling appointments between the patient and the treatment team to discuss alternatives if necessary. This connection should be made through virtual networks.
Evaluation of the effect of education and counseling on patient constipation
After one month of training and counseling, the Bristol scale should be used to evaluate stool consistency. The score ranges from 1 (diarrhea) to 7 (constipation), and the Rome IV criteria should be applied, which include general and specialized criteria. Patients should meet all general criteria and two special criteria to be considered as having constipation. The patient should receive the necessary training in using these criteria at discharge. The booklet will also provide the necessary criteria and explanations for each criterion.
Evaluation of the care plan at discharge
The assessment of the care plan at the time of discharge, which includes several crucial components, is the next phase in our process:
– Evaluation of the client’s response and the need for ongoing interventions.
– Evaluation of the client’s awareness of intestinal care.
– Evaluation of the care performed according to the Bristol scale.
– Evaluation of the care performed according to the Rome IV criteria.
– Evaluation of disability in daily activities according to the Barthel index.
Discussion
This study aimed to develop a care plan for managing new-onset constipation following a stroke. The Registered Nurses’ Association of Ontario (RNAO) Guidelines highlight the importance of a focused initial assessment for constipation, including bowel habits, dietary fiber intake, and medication review, aligning with the user’s emphasis on history-taking and the review of systems (ROS) [37]. StatPearls recommends using the Bristol stool scale and Rome IV criteria [38], which is consistent with the user’s methodology, but adds that abdominal radiography or colonic transit studies may be necessary for refractory cases. Nursing standard focuses on the role of lifestyle factors (e.g. inactivity, low fluid intake) in the assessment, mirroring the user’s focus on diet and activity levels [39]. The user’s assessment aligns with evidence-based tools (Rome IV, Bristol scale) and the holistic evaluation of lifestyle factors. However, recent studies prioritize interprofessional collaboration during assessments (e.g. involving dietitians for dietary reviews), a component that is less emphasized in the user’s framework [37].
The study utilized the NANDA-I taxonomy to formulate diagnoses (e.g. constipation related to low fiber intake) and prioritized using Maslow’s hierarchy or clinical judgment. The nursing diagnosis guide lists similar NANDA-I diagnoses but highlights risk diagnoses (e.g. risk for chronic functional constipation) for preventive care, which the user’s study partially addresses [40]. Also, the National Council of State Boards of Nursing (NCSBN) clinical judgment model (2025) shifts the focus from rigid diagnoses to clinical reasoning, prioritizing hypotheses, like “analyze cues” over formal NANDA labels. While the user’s study adheres to traditional NANDA-I taxonomy, newer models, like the NCJMM (NCSBN clinical judgment measurement model), advocate for dynamic, context-driven reasoning, reducing reliance on standardized diagnoses. This suggests a potential gap in the user’s approach regarding adaptability to evolving clinical judgment frameworks.
Planning includes preventing bowel dysfunction and achieving Bristol scale type 3/4 stools, aligned with SMART criteria [40]. The RNAO guidelines (2020) recommend individualized bowel protocols that combine fiber intake, hydration, and physical activity (30–60 minutes, 3 times per week) [37]. Simplenursing (2022) advocates for patient-specific plans anchored in lifestyle modifications (e.g. prune juice for laxation), similar to the user’s dietary and exercise interventions. Both the user and recent studies emphasize evidence-based, patient-centered goals. However, the RNAO guidelines explicitly stress the importance of interprofessional care plans (e.g. involving physiotherapists for mobility), which the user’s study could integrate more thoroughly.
Interventions include dietary fiber, abdominal massage, patient education, and follow-up. Herbal therapies (e.g. acupressure) are mentioned but lack robust evidence. StatPearls supports fiber therapy and laxatives but cautions against insoluble fiber in severe cases, mirroring the user’s recommendations [38]. The RNAO guidelines promote psyllium supplements and structured bowel programs, validating the user’s focus on fiber and education [37]. Nursing Standard questions the efficacy of abdominal massage, citing limited evidence, which contrasts with the user’s inclusion of massage therapy [39]. The user’s interventions align with mainstream strategies (fiber, hydration) but incorporate less validated methods (e.g. herbal medicine). Recent research [37]highlights the need for multicomponent approaches (e.g. combining diet with physical activity), which the user’s study addresses but could expand with interprofessional strategies.
This study used the Bristol scale, Rome IV criteria, and Barthel index to assess outcomes post-discharge [40]. The RNAO guidelines advocate for ongoing monitoring of fluid intake and fiber adherence, which the user’s follow-up protocol addresses [37]. Both the user and recent studies prioritize objective metrics (e.g. Bristol scale). However, newer frameworks emphasize patient-reported outcomes (e.g. QoL), which could enhance the user’s evaluation phase.
The strengths of this study were a comprehensive assessment using the Rome IV criteria and Bristol scale, holistic interventions combining diet, exercise, and education, and an emphasis on patient-centered, multicomponent interventions. The limitation was that this care plan relied on subjective patient reporting (e.g. SOCRATES, Bristol scale) without objective biomarkers (e.g. colonic transit studies).
Conclusion
This study established a systematic care plan based on scientific methods and the nursing process, developed by experts in the field. It describes a structured nursing approach for new-onset stroke constipation, incorporating validated tools, such as the Rome IV criteria and Bristol scale, along with comprehensive interventions, including diet, exercise, and education. This care framework can be employed for new-onset constipation and emphasizes the integration of interprofessional teams into the care process. Further research is recommended to evaluate the effectiveness of this plan and to create customized protocols for various populations, such as the elderly and chronic pain patients.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was submitted to the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20181008041273N1). this study was approved by the Vice Chancellor in Research and the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (Code: IR.MUI.RESEARCH.REC.1397.320). Participation in this research was not obligatory, and the purpose of the study was explained to all participants, and informed written consent was obtained from the participants, who were assured that all information would be kept confidential and that their names and comments would be provided only to the research team. The research findings would be shared with the participants if requested.
Funding
This study was extracted from the master’s thesis of Shayan Alijanpour, approved by the Department of Critical Nursing, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran (Grand No.: 397514).
Authors contributions
Conceptualization: Shayan Alijanpour, Nahid Dehghan Nayeri, and Soraya Khafri; Methodology: Nasrollah Alimohamadi and Fariborz Khorvash; Investigation: Javad Nadali, Shayan Alijanpour, Seyedeh Fatemeh Hosseini Aghamolki, and Anahita Divani; Writing the original draft: Javad Nadali and Shayan Alijanpour; Review, and editing: Nahid Dehghan Nayeri, Soraya Khafri; Supervision: Nasrollah Alimohamadi, Nahid Dehghan Nayeri, Soraya Khafri, Seyedeh Fatemeh Hosseini Aghamolki, and Anahita Divani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge Alijan Ahmadi Ahangar, Payam Saadat (Mobility Impairments Research Center, Babol), Mohsen Shahriari (Isfahan Faculty of Nursing and Midwifery), and Saeed Abbasi (Head of ICU2, Alzahra Hospital, Isfahan), for their support and collaboration, which made this work feasible.
References
According to the World Health Organization (WHO), stroke affects about 15 million people globally each year [1]. Several studies indicate that as many as 96% of patients hospitalized for stroke experience medical or neurological complications during their hospital stay, which significantly increases the mortality rate [2]. Although the primary effects of stroke are neurological in nature, the organ systems that can be affected continue to increase and include the gastrointestinal tract, particularly in cases of constipation [3]. According to Alijanpour et al., new-onset constipation is secondary constipation arising from multiple factors after a cerebrovascular accident, occurring in patients who had no prior signs or symptoms of constipation before the stroke [4]. A systematic review and meta-analysis showed that the incidence of constipation in the acute stage is 36% to 54% [5]. The risks of this complication ranged from 16% to 66% [4]. Patients who developed new-onset constipation during hospitalization had longer hospital stays, which negatively impacted their QoL and social activities. The multifactorial etiology of post-stroke constipation encompasses reduced mobility, dietary modifications, medication side effects (e.g. opioids, anticholinergics), and neurogenic disruptions in colonic motility regulation [6]. Evidence-based interventions include early mobilization, reducing anticholinergic medications, giving stool softeners, and personalized hydration and fiber plans. Nurse-led bowel management programs show effectiveness in improving evacuation outcomes, focusing on proactive monitoring and patient-centered education [4]. Constipation, as defined by the North American Nursing Diagnosis Association (NANDA-I), places nurses in a prime position to provide comprehensive care for affected patients [7, 8]. According to the NANDA, nursing’s roles in managing constipation include using non-medical methods, like diet changes, lifestyle modifications, and exercise to improve bowel movements and well-being [4].
Recent research has highlighted the importance of structured nursing interventions in managing new-onset constipation after stroke. However, there remains a significant gap in the literature regarding the development and implementation of comprehensive nursing programs based on the nursing process for this specific condition. While studies have demonstrated the effectiveness of individual interventions, such as early mobilization and dietary modifications, there is a lack of standardized, process-oriented nursing protocols that address the multifaceted nature of post-stroke constipation management [4, 9]. Yet, there remains uncertainty about the extent of the nurse’s role in addressing constipation, and clear guidelines are lacking [7, 10]. Managing constipation can be complex, often seen as minor. However, it can seriously affect well-being and may hide more serious health issues [11].
This gap underscores the necessity for developing evidence-based nursing programs that incorporate assessment, diagnosis, planning, implementation, and evaluation stages of the nursing process. This study aimed to develop and validate a comprehensive nursing plan for managing new-onset constipation in acute stroke patients using the RAND/UCLA appropriateness method and the Delphi technique. This approach will synthesize expert opinion and available evidence to create a consensus-based, clinically relevant protocol. By utilizing these rigorous methodologies, we sought to establish a standardized nursing approach that can be widely implemented in stroke care units, potentially improving patient outcomes and quality of life (QoL).
Materials and Methods
This multi-method study is part of a larger research project (Caspian nursing process project (CNP2)), which was conducted with the combination of Delphi and RAND methods (RAM) in three phases [12]. The first phase was a protocol study [4], the second was the development of the care plan for new-onset constipation, and the third phase was an intervention with a care plan, which was defined in the second phase [4]. This study is the result of the second phase and involved several steps:
1. Searching for scientific sources
2. Formal content validity
3. RAM and Delphi methods
4. Results and changes made at the Delphi stage
5. The panel of experts
Research design
1. Searching for scientific sources: The preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline was used in this study [13]. A literature search across ScienceDirect, Cochrane Library, Medline, Scopus, PubMed, and Google Scholar with keywords and MeSH terms, including “stroke”, “constipation”, “bowel management”, “bowel strategy”, “post stroke constipation”, and “new-onset constipation” was conducted. The EndNote software, version 9 (Clarivate Analytics; Philadelphia, PA, USA) was used to remove duplicates. Original articles, studies published in English, and full-text manuscripts were enrolled. All included studies were conducted on humans. We also excluded studies where the diagnostic criteria of constipation were unclear. Sixty-eight articles from 2009 to 2019 were identified. Then, two authors screened potentially eligible studies in terms of the title and abstract according to the checklist, and 11 articles were selected. Any disagreements were resolved by discussions among the two reviewers or by consultations with the third reviewer.
In addition to database searching, hand searching targeted several specialized sites: World Gastroenterology Organization (WGO) [14], American Gastroenterology Association (AGA) [15], and the British Institute of Health and Care Excellence (NICE) [16]. This search yielded six guidelines related to constipation management. These guidelines were appraised using AGREE II (the appraisal of guidelines for research & evaluation), and three guidelines were approved. Finally, 14 articles and guidelines were included in the study.
After the data were gathered in the last step, the primary nursing care plan was defined according to the nursing process and reviewed by the research team. It was then sent for face and content validity.
2. Face and content validity: Face and content validity of the primary nursing care plan were obtained from the supervisor and the advisor of the current study, along with 5 faculty members of the Isfahan School of Nursing and Midwifery. Then, a draft of the nursing care plan was revised and sent for RAM and Delphi steps.
3. RAM and Delphi methods: The RAM includes priority, usefulness, applicability, conceptualization, and who is authorized to provide service. A set of evidence-based recommendations for the new-onset constipation care plan was developed from credible sources and articles, organized according to the nursing process, and presented in four tables: Assessment, goals and outcomes, nursing diagnoses, interventions, and evaluation. Twenty two authorities from different professions of Isfahan, Tehran and Babol University of Medical Sciences were enrolled, including 11 nurses (50%), 4 neurologists (18.2%), 2 fellows in intensive care (9.1%), 2 internal medicine specialists (9.1%), 1 surgeon (4.5%), 1 nutrition specialist (4.5%), and 1 emergency medicine specialist (4.5%). Using the Delphi method to gather expert perspectives, a written care plan aligned with the nursing process was completed. The draft of this care plan was delivered to the experts for review, with a request to evaluate it using a 5-point Likert scale and to provide any further care or advice in the form of proposals. The ratings used a 1-to-5 scale across four domains (priority, benefit, applicability, and concept) for each recommendation, followed by comments on the recommendations in the relevant column.
4. Results and changes made at the Delphi stage: In this stage, the results obtained from the participant survey indicated that each item with 70% agreement and above was retained, while items with <70% agreement were reconsidered.
5. The panel of experts: Due to a consensus of over 70% in the last stage, the panel of experts was deemed unnecessary. After these steps, we prepared this care plan in the nursing process structure. The results of each step were published in the last study. In this paper, we presented the Caspian care plan for new-onset constipation after stroke, which was developed using a scientific method.
Results
CNP
The nursing process is a goal-directed framework that guides and organizes nursing care. It involves five major steps (ADPIE), which are shown in Table 1.
Assessment
Focused constipation assessment: When performing a comprehensive evaluation of a client’s constipation, it is important to gather both subjective and objective information.
History: Frequently occurring symptoms associated with the abdomen and specific to gastrointestinal disorders encompass indigestion, nausea, vomiting, hematemesis, abdominal pain, dysphagia and odynophagia, alterations in bowel function, constipation or diarrhea, and jaundice [17].
A-chief complaint: Some typical indications of constipation include abdominal discomfort, tenderness, palpable muscle resistance, loss of appetite, borborygmi, reduced stool frequency or volume, abdominal distension, fatigue, and hard, formed stools [18].
B-signs and symptoms (SOCRATES): This includes site, onset, character, radiation (if the symptom is pain or discomfort), alleviating factors, timing, exacerbating factors, and severity [19].
C-present illness: It is important to inquire about the frequency and consistency of bowel movements (using the Bristol stool scale), any discomfort during bowel movements, the presence of blood or black, tarry stool (melena), stool color (white or gray stools indicating potential liver or gallbladder disease), and any associated symptoms, such as jaundice or icteric sclera.
D-past history: In this step, we asked about drug and treatment history, social history, and family history of patients.
E-review of systems (ROS): This involves evaluating nutrition (including inadequate fiber consumption, anorexia, and insufficient food and fluid intake), as well as considering lifestyle, behavior, and environmental factors (such as lack of privacy and assistance during toileting), cultural influences, and other factors (such as inactivity, age, depression, and sedation) [20].
F-physical examination: Ensure that the patient is comfortable before proceeding with the examination by following the sequence of “look, listen, and feel” [17].
Inspection: In cases of constipation, this may involve examining the contour of the abdomen (rounded, protuberant, scaphoid, flat), skin characteristics (lesions, hernias, scars, striae [silver or purple], tattoos, ecchymosis, hair distribution), and distension (generalized distension of the abdomen can be caused by one of the five Fs: Fluid [ascites], fetus, feces, fat, flatus). Also, we assessed the umbilicus (for Cullen’s sign) and other factors (such as gravid uterus, nodules, ascites, peristalsis, movement, aortic pulsations, and vein visibility) [21].
Auscultation: This method is used to listen to the sounds of the body. We used the diaphragm for bowel sounds and the bell for vascular sounds, bruits, friction rubs, and venous hums. We listened for clicks/gurgles, known as “borborygmi,” which typically occur 5-35 times per minute and are usually more active after a meal. The absence of bowel sounds should be established only after 3 minutes of continuous listening.
If there is an absence of bowel sounds, it is recommended to conduct a thorough assessment by listening for a duration of five minutes to confirm their absence [22].
Percussion: To perform percussion, one should place two fingers over a specific area and tap on them with the fingertips of the other hand [21]. When percussing the abdomen, the predominant sound should be tympany. In the supine position, air tends to accumulate at the top of the abdomen, resulting in a drum-like sound characteristic of tympany. Dullness, on the other hand, is commonly observed over solid organs or masses, such as the liver, spleen, or a distended bladder [23].
Palpation: Important indicators include ‘guarding’, in which the patient instinctively shields their abdomen, suggesting pain, and ‘rebound tenderness’, characterized by a painful response following deep palpation and hand removal [21].
G-scale for collection of data: We suggest using the Rome criteria IV, which is widely accepted as an international standard in research, to describe post-stroke constipation.
The following criteria are involved in the diagnosis and treatment of constipation, of which at least two must be satisfied:
Experiencing strain during a minimum of 25% of bowel movements.
Passing lumpy or hard stools in at least 25% of bowel movements.
A feeling of incomplete bowel emptying occurs in at least 25% of instances.
Sensing an obstruction or blockage in the anorectal area during at least 25% of defecations [24]. These symptoms must have been present after the stroke. However, a specific instrument for the evaluation of new-onset stroke constipation was not found.
The Bristol stool scale serves as a useful instrument for monitoring colon transit, particularly in cases where bowel frequency and stool consistency are not in concordance. Additionally, abdominal radiography can provide supplementary information to healthcare professionals [25].
H-paraclinical test: Routine testing may not always be necessary. Nevertheless, in instances of clinical suspicion, it is crucial to assess calcium levels and thyroid function. Extensive investigations are warranted for severe symptoms, abrupt alterations in bowel habits, presence of blood in the stool, or, in the case of older adults, taking into account their health status and stage of disease.
Nursing diagnosis
To reach a diagnosis from nursing assessment, nurses need to follow these steps [26-28]:
Data collection or assessment: In this initial stage of the nursing process, you collect information from the patient that is both objective and subjective, including vital signs, medical history, physical examination, and psychosocial assessment.
Data analysis and organization: This second step involves analyzing and interpreting the collected data, identifying patient strengths and limitations, and prioritizing the patient’s needs.
Formulating your nursing diagnoses: This is the third step, where you use the data analysis and the NANDA-I taxonomy to select the most appropriate nursing diagnosis.
Setting priorities: This is the fourth step, where you rank the nursing diagnoses according to their urgency and importance. You can use various frameworks to guide your prioritization, such as Maslow’s hierarchy of needs, ABCDE, or clinical judgment.
Establishing client goals and desired outcomes: This is the fifth step, where you set realistic and measurable goals for the patient based on the nursing diagnosis. The goals should be specific, measurable, attainable, relevant, and time-bound (SMART).
The nurse will assess the gathered information to ascertain the patient’s status and requirements. This procedure encompasses the analysis of data, identification of health concerns, potential risks, and strengths, as well as the formulation of diagnostic statements regarding actual or potential health issues. In some cases, multiple diagnoses may be assigned to a single patient. The utilization of clinical judgment in formulating nursing diagnoses is instrumental in the planning and execution of patient care, including the identification of key nursing diagnoses associated with constipation [27]:
Constipation associated with water and electrolyte disturbance following a stroke.
Constipation associated with inadequate fiber intake following a stroke.
Constipation associated with low physical activity following a stroke.
Constipation associated with taking multiple medications following a stroke.
Constipation due to drug side effects after a stroke.
Constipation associated with nerve damage following a stroke.
Lack of knowledge about constipation management following a stroke.
Planning
The planning phase involves the formulation of goals and outcomes that have a direct impact on patient care, in accordance with evidence-based practice (evidence-based practice) guidelines [27].
Prevention of bowel dysfunction.
Increased awareness of bowel care needs.
Steady state in water and electrolytes.
Placement in types 3 or 4 of the Bristol criteria.
No evidence of constipation according to the Rome IV criteria.
Implementation
Nursing-led interventions generally include seven items, including physical activity and exercise, modified drug regimen, diet, fiber therapy, abdominal massage therapy, patient training, and patient follow-up. The practice nurse should inquire about fluid and dietary fiber intake, activity levels, and all medications the person is taking, including prescribed and nonprescription drugs [29, 30]. The intervention was performed according to each nursing diagnosis (Table 2).
Physical activity and exercise: For individuals who engage in regular physical activity, walking is the most prevalent form of exercise. However, some participants are unable to engage in physical activity due to various reasons, such as permanent immobility caused by conditions, like paraplegia, arthritis, or emphysema, temporary immobility during hospitalization or recovery, adverse weather conditions, safety concerns when exercising alone, or the risk of sustaining injuries, such as fractured limbs, during physical activity.
Modified drug regimen: Therapeutic drugs associated with constipating effects that were included in the care plan were replaced by a neurologist, if appropriate. If the drug was not available, the number and types of constipation were recorded in a questionnaire.
Diet: Participants consume various vegetables, including hot ones or salads, to prevent constipation. Prunes or prune juice are commonly used as effective laxatives. Some find liquorice sticks helpful, while others use pepitos or sorbitol-containing sweets [31]. Recently, herbal medicine [30, 32] and acupoint herbal patching [33] have also been recommended to treat post-stroke constipation.
Fiber therapy: Dietary fiber can help with mild to moderate constipation, but not severe cases. It is recommended to consume 20-35 grams daily from sources, like whole wheat bread, unrefined cereals, citrus fruits, and vegetables. However, insoluble fiber, like cereal bran, can cause gas, bloating, and delay gastric emptying, reducing appetite. It is best to start with low doses of fiber supplements and gradually increase to 20-25 grams per day, while also increasing water intake [34].
Abdominal message therapy: Massage therapy, based on various studies, was performed ten minutes daily [30]. Abdominal massage, according to the study by Alijanpour et al., can be performed using longitudinal, transverse, and rotational movements of the colon [4]. Moreover, acupressure and moxibustion [35], as well as acupoint embedding therapy, which is a therapeutic technique applied at specific acupuncture points, are recommended to treat post-stroke constipation [36].
Patient training: At discharge, provide the patient with a booklet addressing new-onset stroke constipation, emphasizing self-care practices and self-efficacy [30]. Also, in coordination with a neurologist, the patient should receive practical training in massage therapy, learn to work with the Bristol tool to determine the consistency of stools after discharge, and understand how to contact the treatment team by telephone or social media. Educational content for patients and partners should include familiarity with the food pyramid, food groups, weight control methods, lifestyle changes, drug side effects, laxative foods, constipated foods, high-fiber foods, constipation medications, water intake, physical activity, stress reduction, and how to use herbal laxatives correctly. Moreover, a study suggests that structured bowel programs and nurse-led interventions in bowel care have a significant effect on improving bowel evacuations [30].
Patient follow-up: After discharge, patients should be followed for four weeks in two steps: Communicating with the treatment team and evaluating how training and counseling influenced outcomes.
Patient relationship with care team
Communication with the treatment team should include asking questions or raising complaints from the patients or their companions, patient consultations with a physician or research nurse in case of need, and scheduling appointments between the patient and the treatment team to discuss alternatives if necessary. This connection should be made through virtual networks.
Evaluation of the effect of education and counseling on patient constipation
After one month of training and counseling, the Bristol scale should be used to evaluate stool consistency. The score ranges from 1 (diarrhea) to 7 (constipation), and the Rome IV criteria should be applied, which include general and specialized criteria. Patients should meet all general criteria and two special criteria to be considered as having constipation. The patient should receive the necessary training in using these criteria at discharge. The booklet will also provide the necessary criteria and explanations for each criterion.
Evaluation of the care plan at discharge
The assessment of the care plan at the time of discharge, which includes several crucial components, is the next phase in our process:
– Evaluation of the client’s response and the need for ongoing interventions.
– Evaluation of the client’s awareness of intestinal care.
– Evaluation of the care performed according to the Bristol scale.
– Evaluation of the care performed according to the Rome IV criteria.
– Evaluation of disability in daily activities according to the Barthel index.
Discussion
This study aimed to develop a care plan for managing new-onset constipation following a stroke. The Registered Nurses’ Association of Ontario (RNAO) Guidelines highlight the importance of a focused initial assessment for constipation, including bowel habits, dietary fiber intake, and medication review, aligning with the user’s emphasis on history-taking and the review of systems (ROS) [37]. StatPearls recommends using the Bristol stool scale and Rome IV criteria [38], which is consistent with the user’s methodology, but adds that abdominal radiography or colonic transit studies may be necessary for refractory cases. Nursing standard focuses on the role of lifestyle factors (e.g. inactivity, low fluid intake) in the assessment, mirroring the user’s focus on diet and activity levels [39]. The user’s assessment aligns with evidence-based tools (Rome IV, Bristol scale) and the holistic evaluation of lifestyle factors. However, recent studies prioritize interprofessional collaboration during assessments (e.g. involving dietitians for dietary reviews), a component that is less emphasized in the user’s framework [37].
The study utilized the NANDA-I taxonomy to formulate diagnoses (e.g. constipation related to low fiber intake) and prioritized using Maslow’s hierarchy or clinical judgment. The nursing diagnosis guide lists similar NANDA-I diagnoses but highlights risk diagnoses (e.g. risk for chronic functional constipation) for preventive care, which the user’s study partially addresses [40]. Also, the National Council of State Boards of Nursing (NCSBN) clinical judgment model (2025) shifts the focus from rigid diagnoses to clinical reasoning, prioritizing hypotheses, like “analyze cues” over formal NANDA labels. While the user’s study adheres to traditional NANDA-I taxonomy, newer models, like the NCJMM (NCSBN clinical judgment measurement model), advocate for dynamic, context-driven reasoning, reducing reliance on standardized diagnoses. This suggests a potential gap in the user’s approach regarding adaptability to evolving clinical judgment frameworks.
Planning includes preventing bowel dysfunction and achieving Bristol scale type 3/4 stools, aligned with SMART criteria [40]. The RNAO guidelines (2020) recommend individualized bowel protocols that combine fiber intake, hydration, and physical activity (30–60 minutes, 3 times per week) [37]. Simplenursing (2022) advocates for patient-specific plans anchored in lifestyle modifications (e.g. prune juice for laxation), similar to the user’s dietary and exercise interventions. Both the user and recent studies emphasize evidence-based, patient-centered goals. However, the RNAO guidelines explicitly stress the importance of interprofessional care plans (e.g. involving physiotherapists for mobility), which the user’s study could integrate more thoroughly.
Interventions include dietary fiber, abdominal massage, patient education, and follow-up. Herbal therapies (e.g. acupressure) are mentioned but lack robust evidence. StatPearls supports fiber therapy and laxatives but cautions against insoluble fiber in severe cases, mirroring the user’s recommendations [38]. The RNAO guidelines promote psyllium supplements and structured bowel programs, validating the user’s focus on fiber and education [37]. Nursing Standard questions the efficacy of abdominal massage, citing limited evidence, which contrasts with the user’s inclusion of massage therapy [39]. The user’s interventions align with mainstream strategies (fiber, hydration) but incorporate less validated methods (e.g. herbal medicine). Recent research [37]highlights the need for multicomponent approaches (e.g. combining diet with physical activity), which the user’s study addresses but could expand with interprofessional strategies.
This study used the Bristol scale, Rome IV criteria, and Barthel index to assess outcomes post-discharge [40]. The RNAO guidelines advocate for ongoing monitoring of fluid intake and fiber adherence, which the user’s follow-up protocol addresses [37]. Both the user and recent studies prioritize objective metrics (e.g. Bristol scale). However, newer frameworks emphasize patient-reported outcomes (e.g. QoL), which could enhance the user’s evaluation phase.
The strengths of this study were a comprehensive assessment using the Rome IV criteria and Bristol scale, holistic interventions combining diet, exercise, and education, and an emphasis on patient-centered, multicomponent interventions. The limitation was that this care plan relied on subjective patient reporting (e.g. SOCRATES, Bristol scale) without objective biomarkers (e.g. colonic transit studies).
Conclusion
This study established a systematic care plan based on scientific methods and the nursing process, developed by experts in the field. It describes a structured nursing approach for new-onset stroke constipation, incorporating validated tools, such as the Rome IV criteria and Bristol scale, along with comprehensive interventions, including diet, exercise, and education. This care framework can be employed for new-onset constipation and emphasizes the integration of interprofessional teams into the care process. Further research is recommended to evaluate the effectiveness of this plan and to create customized protocols for various populations, such as the elderly and chronic pain patients.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was submitted to the Iranian Registry of Clinical Trials (IRCT), Tehran, Iran (Code: IRCT20181008041273N1). this study was approved by the Vice Chancellor in Research and the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (Code: IR.MUI.RESEARCH.REC.1397.320). Participation in this research was not obligatory, and the purpose of the study was explained to all participants, and informed written consent was obtained from the participants, who were assured that all information would be kept confidential and that their names and comments would be provided only to the research team. The research findings would be shared with the participants if requested.
Funding
This study was extracted from the master’s thesis of Shayan Alijanpour, approved by the Department of Critical Nursing, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran (Grand No.: 397514).
Authors contributions
Conceptualization: Shayan Alijanpour, Nahid Dehghan Nayeri, and Soraya Khafri; Methodology: Nasrollah Alimohamadi and Fariborz Khorvash; Investigation: Javad Nadali, Shayan Alijanpour, Seyedeh Fatemeh Hosseini Aghamolki, and Anahita Divani; Writing the original draft: Javad Nadali and Shayan Alijanpour; Review, and editing: Nahid Dehghan Nayeri, Soraya Khafri; Supervision: Nasrollah Alimohamadi, Nahid Dehghan Nayeri, Soraya Khafri, Seyedeh Fatemeh Hosseini Aghamolki, and Anahita Divani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully acknowledge Alijan Ahmadi Ahangar, Payam Saadat (Mobility Impairments Research Center, Babol), Mohsen Shahriari (Isfahan Faculty of Nursing and Midwifery), and Saeed Abbasi (Head of ICU2, Alzahra Hospital, Isfahan), for their support and collaboration, which made this work feasible.
References
- Hall RF. Mixed methods: In search of a paradigm. In: Le T, Le Q. Conducting research in a changing challenging world. New York: Nova Science Pub Inc; 2013. [Link]
- Janus-Laszuk B, Mirowska-Guzel D, Sarzynska-Dlugosz I, Czlonkowska A. Effect of medical complications on the after-stroke rehabilitation outcome. NeuroRehabilitation. 2017; 40(2):223-32. [DOI:10.3233/NRE-161407] [PMID]
- Macom RV, Brown CM. Gastrointestinal dysfunction and dysbiosis in ischemic stroke: Opportunities for therapeutic intervention. Pharmaceuticals (Basel). 2025; 18(3):320. [DOI:10.3390/ph18030320] [PMID]
- Alijanpour S, Alimohamadi N, Khafri S, Rokni MA, Khorvash F. Caspian nursing process: Impactions on new-onset constipations in admission, discharge, and follow-up of acute stroke patients. Iran J Nurs Midwifery Res. 2022; 27(6):509-16. [DOI:10.4103/ijnmr.ijnmr_90_21] [PMID]
- Li J, Yuan M, Liu Y, Zhao Y, Wang J, Guo W. Incidence of constipation in stroke patients: A systematic review and meta-analysis. Medicine (Baltimore). 2017; 96(25):e7225. [DOI:10.1097/MD.0000000000007225] [PMID]
- Kumar S, Chou SH, Smith CJ, Nallaparaju A, Laurido-Soto OJ, Leonard AD, et al. Addressing systemic complications of acute stroke: A scientific statement from the American Heart Association. Stroke. 2025; 56(1):e15-e29. [DOI:10.1161/STR.0000000000000477]
- Herdman TH, Kamitsuru S. Nursing diagnoses 2018-2020: Definitions and classification. New York, US: Thieme Medical Publishers; 2017. [Link]
- Alijanpour S, Aslani Z, Alimohammadi N, Taleghani F. Empowerment of nurses: A key to stroke patients' satisfactions. Iran J Nurs Midwifery Res. 2020; 25(3):237-41. [DOI:10.4103/ijnmr.IJNMR_121_17] [PMID]
- Alijanpour S, Alimohamadi N, Khafri S, Khorvash F. New-onset constipation after stroke: Caspian nursing process projects. J Holistic Nurs Midwifery. 2022; 32(1):29-39. [DOI:10.32598/jhnm.32.1.2117]
- Withell B. A protocol for treating acute constipation in the community setting. Br J Community Nurs. 2000; 5(3):110, 112, 114-7. [DOI:10.12968/bjcn.2000.5.3.7419] [PMID]
- Takaoka M, Igarashi A, Futami A, Yamamoto-Mitani N. Management of constipation in long-term care hospitals and its ward manager and organization factors. BMC Nurs. 2020; 19:5. [DOI:10.1186/s12912-020-0398-z] [PMID]
- Alijanpour S, Bahramnezhad F, Mowla A, Shafiee Sabet M, Dehghan Nayeri N. Updated protocol for stroke code management in prehospital settings: The Iranian comprehensive stroke code management program (ICSCM phase II). Arch Acad Emerg Med. 2025; 13(1):e43. [DOI: 10.22037/aaemj.v13i1.2633] [PMID]
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010; 8(5):336-41. [DOI:10.1016/j.ijsu.2010.02.007] [PMID]
- Lindberg G, Hamid SS, Malfertheiner P, Thomsen OO, Fernandez LB, Garisch J, et al. World gastroenterology Organisation global guideline: Constipation--a global perspective. J Clin Gastroenterol. 2011; 45(6):483-7. [DOI:10.1097/MCG.0b013e31820fb914] [PMID]
- American Gastroenterological Association; Bharucha AE, Dorn SD, Lembo A, Pressman A. American gastroenterological association medical position statement on constipation. Gastroenterology. 2013; 144(1):211-7. [DOI:10.1053/j.gastro.2012.10.029] [PMID]
- Murthy L, Richardson J, Rowark S, Wasielewska A. NICE public health guidance update. J Public Health (Oxf). 2017; 39(3):647-9. [DOI:10.1093/pubmed/fdx095] [PMID]
- Bickley L, Szilagyi PG. Bates’ guide to physical examination and history-taking. Philadelphia: Wolters Kluwer Health; 2012. [Link]
- Ackley BJ, Ladwig GB, Msn R, Makic MBF, Martinez-Kratz M, Zanotti M. Nursing diagnosis handbook e-book: An evidence-based guide to planning care. Missouri: Mosby; 2019. [Link]
- Talley NJ, O’Connor S. Clinical examination: A systematic guide to physical diagnosis. London: Chatswood: Elsevier Churchill Livingstone; 2010. [Link]
- Day A. The nurse’s role in managing constipation. Nurs Stand. 2001; 16(8):41-4. [DOI:10.7748/ns2001.11.16.8.41.c3116] [PMID]
- Murry T, Carrau RL, Chan K. Clinical management of swallowing disorders. San Diego: Plural Publishing, Incorporated; 2020. [Link]
- Cole C, Hill O, Saunders R. Jarvis's Physical Examination and Health Assessment: Pocket Companion. Australia: Elsevier Health Sciences; 2012. [Link]
- Maryniak K, Constantine L. RN.com’s Aassessment series: Focused endocrine assessment. San Diego: AMN Heathcare Education Service; 2004. [Link]
- Sobrado CW, Neto IJFC, Pinto RA, Sobrado LF, Nahas SC, Cecconello I. Diagnosis and treatment of constipation: A clinical update based on the Rome IV criteria. Journal of Coloproctology. 2018; 38(2):137-44. [DOI:10.1016/j.jcol.2018.02.003]
- Song KH. Practical methods to assess chronic constipation. J Neurogastroenterol Motil. 2015; 21(3):307-8. [DOI:10.5056/jnm15100] [PMID]
- Toney-Butler TJ, Thayer JM. Nursing Process. 2023 Apr 10. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. [PMID]
- Herdman TH, Kamitsuru S, Lopes C,. NANDA international nursing diagnoses: Definitions & classification, 2021-2023. Teningen: Thieme; 2021. [Link]
- Shahzeydi A, Farzi S, Tarrahi MJ, Sabouhi F, Babaei S, Yazdannik A. The effect of the clinical supervision model on nursing internship students' nursing process-based performance: An experimental study. BMC Nurs. 2024; 23(1):166. [DOI:10.1186/s12912-024-01840-0] [PMID]
- Nazarko L. Constipation: A guide to assessment and treatment. Indep Nurse. 2017; 2017(10):26-9. [DOI:10.12968/indn.2017.10.26]
- Pinto CFCS, Oliveira PDCM, Fernandes OMFSO, Padilha JMDSC, Machado PAP, Ribeiro ALA, et al. Nonpharmacological clinical effective interventions in constipation: A systematic review. J Nurs Scholarsh. 2020; 52(3):261-9. [DOI:10.1111/jnu.12555] [PMID]
- Annells M, Koch T. Constipation and the preached trio: Diet, fluid intake, exercise. Int J Nurs Stud. 2003; 40(8):843-52. [DOI:10.1016/S0020-7489(03)00075-0] [PMID]
- Wang X, Zhou M, Kang K, Yang R. Clinical observation on Xiao Cheng Qi Tang combined with external application therapy in treating constipation of stroke patients. Xibu Zhongyiyao. 2012; 25(5):10-2. [Link]
- Yuan Y, Gao Y, Ding Z, Qiao Y, Xu S, Tang Z, et al. The effectiveness of acupoint herbal patching for constipation after stroke: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2022; 101(7):e28843. [DOI:10.1097/MD.0000000000028843] [PMID]
- Portalatin M, Winstead N. Medical management of constipation. Clin Colon Rectal Surg. 2012; 25(1):12-9. [DOI:10.1055/s-0032-1301754] [PMID]
- Kim B, Jo HG, Lee D. Integrative traditional Korean medicine treatment for elderly post-stroke functional constipation: A CARE-compliant case report. Explore (NY). 2021; 17(3):270-3. [DOI:10.1016/j.explore.2020.09.004] [PMID]
- Du J, Liu H, Xu J, Lu CM, Zhou JF, Wu PH, et al. [Post-stroke constipation treated with acupoint embedding therapy: A multi-center randomized controlled trial (Chinese)]. Zhongguo Zhen Jiu. 2020; 40(5):493-7. [DOI:10.13703/j.0255-2930.20190507-k0004] [PMID]
- Registered Nurses’ Association of Ontario. A proactive approach to bladder and bowel management in adults. Toronto: Registered Nurses’ Association of Ontario; 2020. [Link]
- Diaz S, Bittar K, Hashmi MF, Mendez MG. Constipation. Treasure Island: StatPearls Publishing; 2023. [Link]
- Andrews A, St Aubyn B. Assessment, diagnosis and management of constipation. Nurs Stand. 2020; 35(9):59-65.[DOI:10.7748/ns.2020.e11512] [PMID]
- Matt V. Nursing diagnosis guide: All you need to know to master diagnosing [Internet]. 2020 [Updated 2025 October 4]. Available from: 2020. [Link]
Type of Study: Research |
Subject:
Special
Received: 2025/05/1 | Accepted: 2025/09/16 | Published: 2025/10/26
Received: 2025/05/1 | Accepted: 2025/09/16 | Published: 2025/10/26
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


