Thu, Jan 29, 2026
Volume 11, Issue 3 (Summer 2025)
Caspian J Neurol Sci 2025, 11(3): 245-255 |
Back to browse issues page
Ethics code: IR.IAU.SRB.REC.1403.187
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shafiee S, Arabsheybani N, Saadat S. The Mediating Role of Eating Behavior in the Relationship Between Rumination and Sleep Quality in University Students. Caspian J Neurol Sci 2025; 11 (3) :245-255
URL: http://cjns.gums.ac.ir/article-1-782-en.html
URL: http://cjns.gums.ac.ir/article-1-782-en.html
1- Department of Psychology, Faculty of Literature, Humanities and Social Sciences, Science and Research Branch (SR.C), Islamic Azad University, Tehran, Iran
2- Neuroscience Research Center, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,Sajjadsaadat69@gmail.com
2- Neuroscience Research Center, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 1699 kb]
(640 Downloads)
| Abstract (HTML) (607 Views)
Full-Text: (250 Views)
Introduction
Sleep is an important and global process [1]. Also, it is a natural and physiological state controlled by a neuro-biological process, which is necessary and crucial for human health [2]. The most important predictor of sleep is the quality of sleep, which means the problem and difficulty in falling asleep, staying asleep, the number of times you make up during sleep [3], and the degree of satisfaction and relaxation after waking up [4].
Sleep quality is generally used in sleep medicine. It includes a set of sleep measures, especially total sleep time (TST), sleep onset latency (SOL), sleep maintenance, total wake time (TWT), sleep efficiency (SE), and sleep problems like spontaneous arousal or apnea [5]. Low sleep quality hurts a person’s physical health, such as type 2 diabetes, chronic pain, and blood pressure [1]. In addition, low-quality sleep causes negative effects such as obesity and poor-quality diet [6].
People spend almost one-third of their lives sleeping. Sleep is an inherent physiological process controlled by homeostasis and circadian rhythms. It plays an essential role in maintaining general physical and mental health, but the exact function of sleep is not well understood [7]. Also, many individuals have sleep problems such as restless legs syndrome, insomnia, and sleep apnea [3]. On the other hand, the importance of sleep in college students is very important; college students need quality sleep to improve their academic functioning, emotional state, and problem-solving. Students do not care about the quality of their sleep and lack motivation for its high quality [8].
A review of previous studies suggests that rumination is important in reducing sleep quality. It is defined as a type of cognition that continuously focuses on a specific topic. For instance, thinking about the past or special emotions [9]. Rumination is related to some psychological problems, such as depressive mood, poor general sleep quality, increased sleep latency, sleep disturbances, eating disorders like bulimia and binge eating, binge drinking, anxiety, and obsessive-compulsive disorder or posttraumatic stress disorder (PTSD) [10].
People who ruminate a lot focus on their distress, which makes them feel more negative. This negative mood prevents constructive problem-solving because the person focuses on unpleasant feelings [11]. On the other hand, suppressing rumination may be a coping strategy, but research has shown that suppressing these thoughts increases intrusive thoughts [12]. Furthermore, research has demonstrated that psychosomatic symptoms, such as stomach and intestinal complaints, headaches, and chronic diseases, such as obesity, high blood pressure, diabetes, and cardiovascular illness, are impacted by rumination [13].
As a maladaptive response, rumination causes excessive negative thoughts before sleep, which causes autonomic arousal and emotional distress [14]. Individuals with high rumination traits are prone to experiencing repetitive and unproductive thoughts during the day and also face increased emotional and cognitive arousal at bedtime. They also experience more intrusive thoughts during the pre-sleep period, undermining their sleep quality [15, 16].
A review of previous studies also suggests that eating behavior plays an important role in reducing sleep quality; eating behavior is a complex process that involves the food environment and physiological factors [17]. Eating behavior includes food choice, motivation, eating style, diet, and eating problems, such as obesity, feeding disorders, and eating disorders. Individuals and how much they eat affect their health [18].
One of the common disorders in adolescent girls is obesity, which is caused by disordered eating behavior [18]. In other words, women are more prone to eating disorders [19]. Furthermore, college students have a different lifestyle and diet than other people; they often prefer to use quick and easy meals. Therefore, fast food consumption is high among them. In addition, most students ignore the recommendations of eating habits and skip many meals [20].
The relationship between sleep quality and eating behavior is bidirectional, with poor eating habits or maladaptive eating behavior being associated with an increased prevalence of sleep disorders and mental disorders such as depression and anxiety, and poor sleep quality being associated with an increase in problems related to eating behaviors [21, 22]. A well-rested person with good sleep quality is likelier to have healthier eating behaviors due to improved cognitive function, reduced cravings, and better impulse control. In addition, high-quality sleep can lead to the regulation of hormones such as ghrelin and leptin, which play a role in appetite control [23-25].
On the other hand, individuals with higher rumination traits may use eating as an emotional regulation strategy to cope with negative emotions resulting from repeated negative thinking. As a result, this strategy may become a habit, especially in an uncomfortable situation [26, 27]. From all previous studies, it can be inferred that high levels of rumination play an important role in reducing the quality of sleep in students due to increased unhealthy eating behavior. At the same time, this hypothesis has not been tested in previous studies.
Promoting and supporting healthy eating habits and adaptive eating behaviors among students is essential for educational institutions, as these habits can have a long-term impact on their health, academic success, and sleep quality. The significant issue in the present study is the placement of eating behavior as a mediating variable, which has theoretical support. In other words, mental rumination can lead to different outcomes due to its effect on eating behavior. This study will study the quality of sleep, which indicates a person’s overall view of his sleep status as an outcome.
For this reason, research in this field is important. At first, it seems that this research makes it possible to understand the psychological mechanisms affecting the quality of students’ sleep. This understanding is important for mental health professionals and counselors in providing effective student treatment interventions. Understanding the effect of eating behavior and mental rumination on sleep quality can lead to developing strategies to promote general well-being in students. Overall, it seems that understanding the complex relationships between research variables can significantly add to theoretical knowledge and practical applications in the fields of psychology and counseling, and the findings may contribute to the development of effective treatment approaches, interventions, and educational programs aimed at improving the well-being and sleep quality of students.
Materials and Methods
The present study was cross-sectional using structural equation modeling. In this study, information is collected using self-report questionnaires. Then, the linear relationship between the exogenous and mediator variables and the endogenous variable will be examined. Afterward, the extent to which the eating behavior variable can mediate the relationship between rumination and sleep quality in students will be examined. The statistical population consisted of all Islamic Azad University, Science and Research Branch students studying in Tehran City, Iran, in 2024. According to Kline’s (p.105, 28) recommendation, a sample size of approximately 200 participants is sufficient for an adequate model fit in structural equation modeling. However, considering the potential for sample attrition, the sample size was increased to 250 participants. The sampling method was convenience sampling. The questionnaires were distributed among the Science and Research Branch students of Azad University from March to June 2024. Informed consent was obtained from the participants, and there was an emphasis on maintaining the confidentiality of the collected information. The inclusion criterion was between 18 and 45 years of age. The exclusion criteria included unwillingness to complete the questionnaires, incomplete or distorted responses, a history of psychiatric disorders, receiving psychotherapy services, experiencing psychological trauma, or undergoing treatment for a specific physical illness — all within the past six months.
Study tools
Pittsburgh sleep quality index (PSQI)
The PSQI questionnaire measured the quality of people’s sleep in 19 items. This questionnaire has 7 subscales: Subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medications, and daily functioning disorders. Each component’s minimum and maximum scores range from 0 (no problem) to 3 (very serious problem). A high score on each element or total score indicates poor sleep quality. In the original version of this questionnaire, the Cronbach α coefficient was 0.83 [28]. Also, the Cronbach α coefficient in the Iranian sample was 0.86 [29]. In the present study, internal consistency was calculated as 0.82 using Cronbach’s α.
Ruminative response scale (RRS)
The RRS questionnaire has 22 questions. Participants rate the answers on a scale of 1 (almost never respond this way) to 4 (almost always respond this way). This questionnaire also has three components: Expressing, thinking, and depression. The lower score in this questionnaire is 22, and the upper limit of the score is 88. Higher scores on this questionnaire indicate higher rumination. The Cronbach α coefficient for this scale was 0.90, and the test re-test correlation coefficient was 0.067 over two years [30]. In the Iranian sample, the Cronbach α coefficient for this scale was 0.86 [31]. In the present study, internal consistency was calculated as 0.77 using the Cronbach α.
Dutch eating behavior questionnaire (DEBQ)
Van Strien et al. developed the DEBQ in 1986. It consists of 33 items and identifies three eating patterns: External, restrained, and emotional. Restrained eating refers to deliberately restricting food intake to control or reduce body weight, often through conscious dieting efforts. Emotional eating involves eating in response to emotional states such as anxiety, sadness, loneliness, or anger [32]. External eating is characterized by eating in response to external food-related cues such as the sight, smell, or presence of food, regardless of internal hunger. These eating styles can be considered maladaptive [33]. Emotional eating includes 13 items, external eating consists of 10 items, and restrained eating contains 10 items [32]. The responses are in the form of a 5-point rating, with the lowest rating being the lowest score and the highest rating being the highest (never=1, rarely=2, sometimes=3, often=4, very often=5) [32]. The minimum score for emotional eating is 13, and the maximum is 65. The minimum score for restrained and external eating is 10 and 50. Higher scores on each component indicate a greater extent of that eating behavior pattern. Arhire et al. [34] found that the Cronbach α coefficient was 0.95 for emotional, 0.85 for external, and 0.91 for restrained eating. The Persian version of the DEBQ demonstrated good internal consistency, as indicated by Cronbach α coefficients ranging from 0.77 to 0.83. Also, the construct validity was examined using confirmatory factor analysis. Its 3-factor structure was confirmed (comparative fit index [CFI]=0.91, normed fit index [NFI]=0.9, standardized root mean square residual [SRMR]=0.072, The root mean square error of approximation [RMSEA]=0.082) [35]. In the present study, internal consistency was calculated as 0.77 for external, 0.79 for restrained, and 0.81 for emotional eating using Cronbach α values.
Data analysis
SPSS and AMOS software version 24 were used to analyze the data. The research data analysis method was structural equation modeling. The fit of the research model was examined based on maximum likelihood estimation. The fit indices of χ2/df, Tucker-Lewis Index (TLI), CFI, incremental fit index (IFI), NFI, relative fit index (RFI), and RMSEA were reported. Also, to examine the direct and indirect effects, the bootstrap test with 5000 repetitions was used.
Results
Two hundred fifty students participated in this study, and information about the participants includes age, gender, and level of education. The mean age of the participants was 29.39, with the lowest age being 18 and the highest age being 41. The standard deviation was 6.85. One hundred twenty-eight women (51.2%) and 122 men (48.8%) participated in this study. Also, 28(11.2%) of them had an associate degree, 105(42%) had a bachelor’s degree, 87(34.8%) had a master’s degree, and 30(12%) had a PhD. In Table 1, the descriptive findings of the research variables and the normality of the data distribution are presented by skewness and kurtosis statistics.
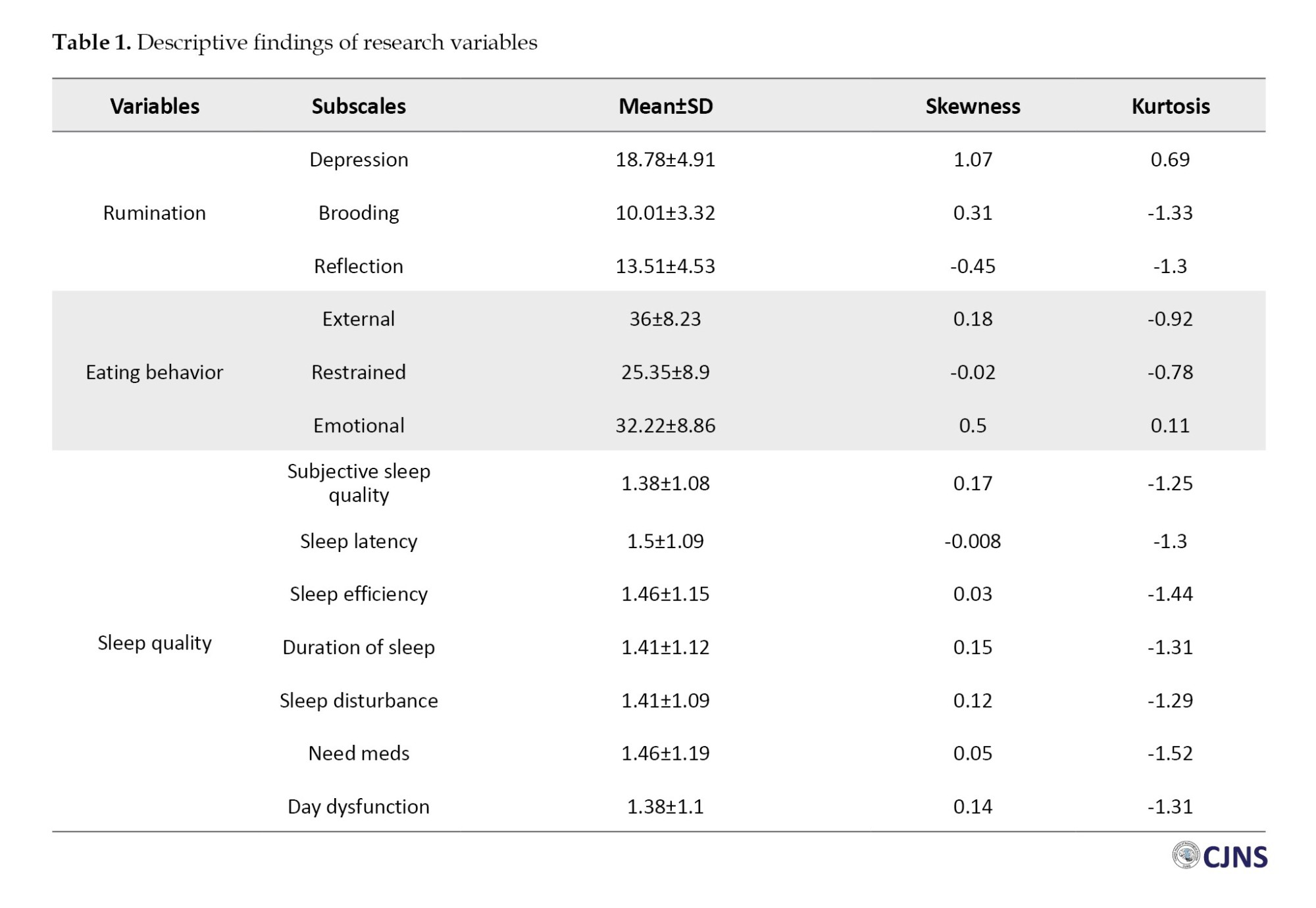
Table 1 shows the average scores of the research variables. In addition, the results of the examination of the skewness and kurtosis statistics have shown that they are all in the range of -2 to -2; based on these statistics, the research data has a normal distribution. Based on this, the use of parametric tests is allowed. The results of the Pearson correlation test are presented below.
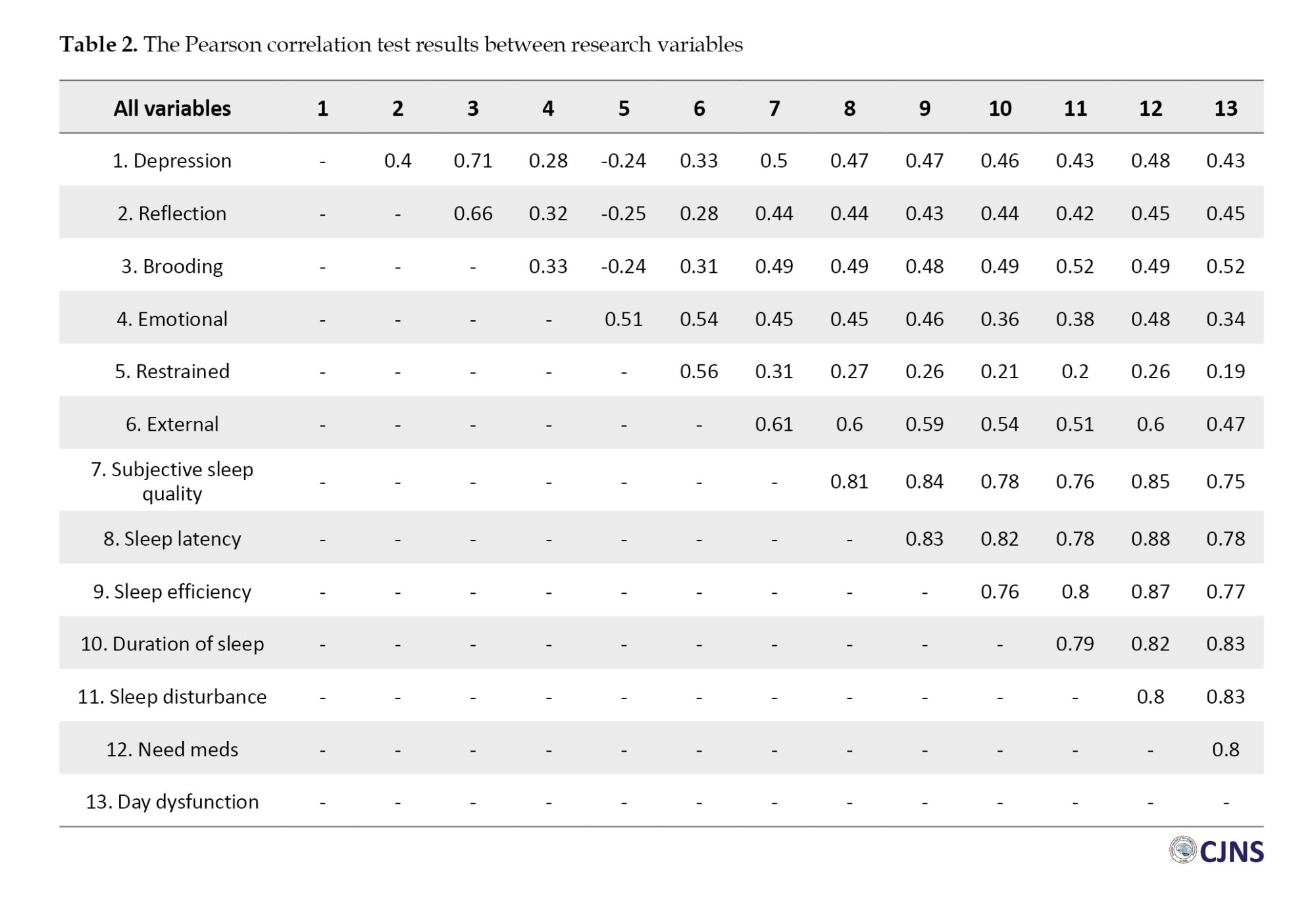
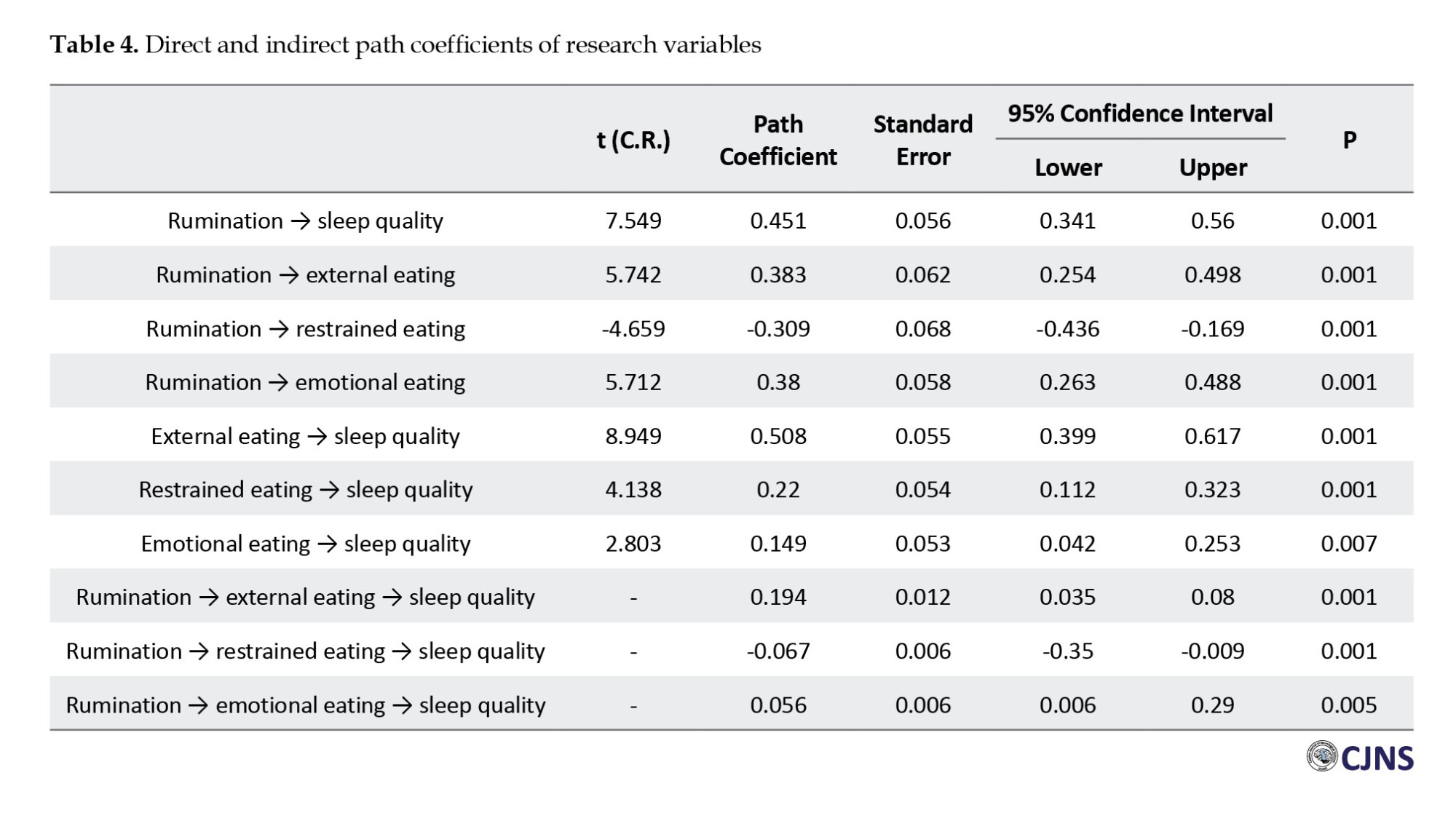
Table 2 shows a significant correlation between rumination, sleep quality, and eating behavior (P<0.05). The following presents autocorrelation results in the residuals and multicollinearity (collinearity) between predictor changes. Based on this, the autocorrelation value in the residuals was reported to be favorable using Durbin-Watson’s test (1.794) as it was in the range of 1.5 to 2.5. Also, there was no multicollinearity (collinearity) between pre-interval variables, and the tolerance value was calculated between 0.32 and 0.61. In addition, the variance inflation index was lower than 5, indicating the VIF index’s acceptable limit.
Structural equation modeling and bootstrap testing were used to test this hypothesis, and the results are presented below. Figure 1 shows the structural equation model in the standard mode.
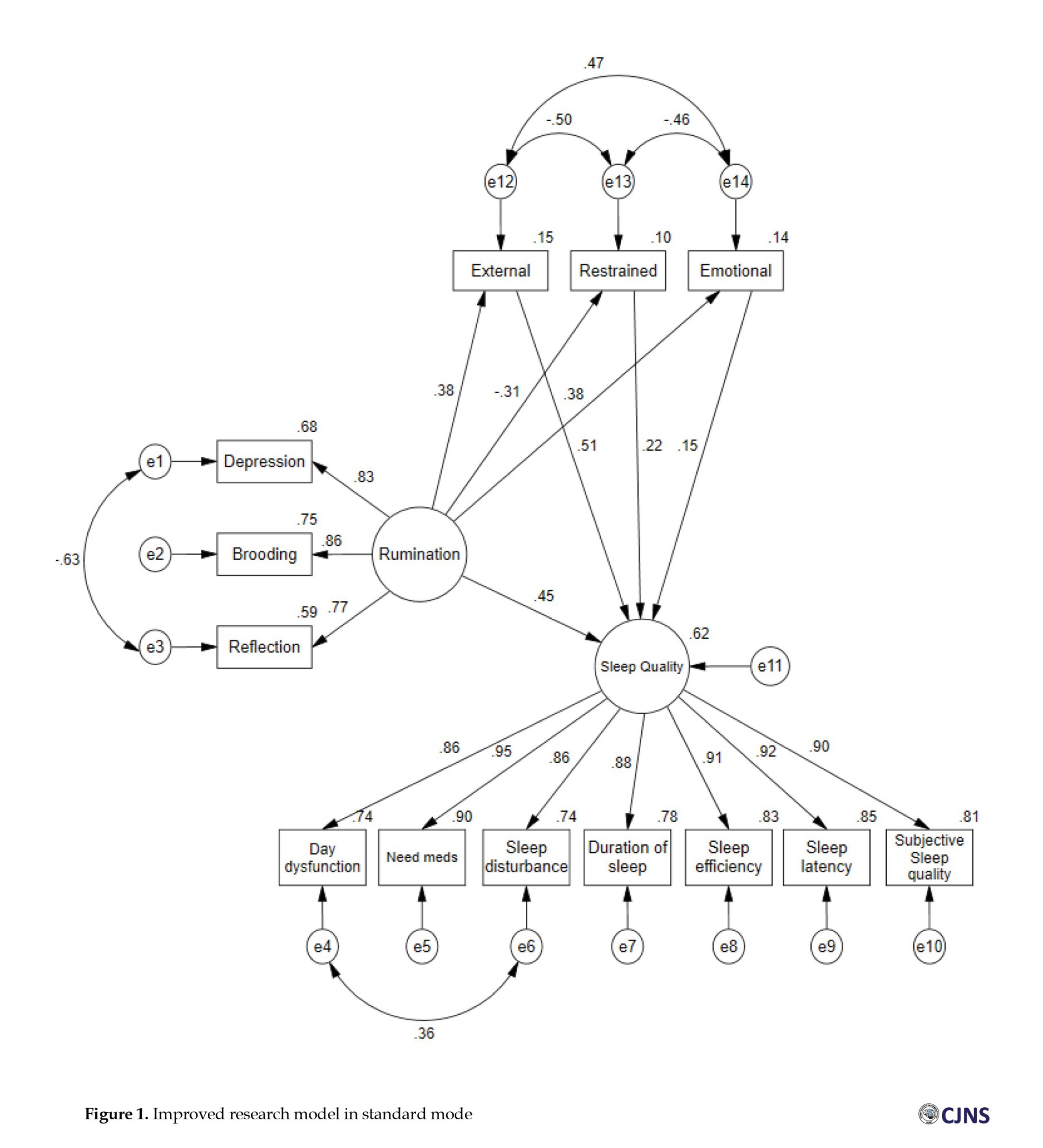
The results of Figure 1 show that the improved research model predicted 62% of the sleep quality in 250 participants. The fit indices of the proposed and modified model are presented in Table 3.
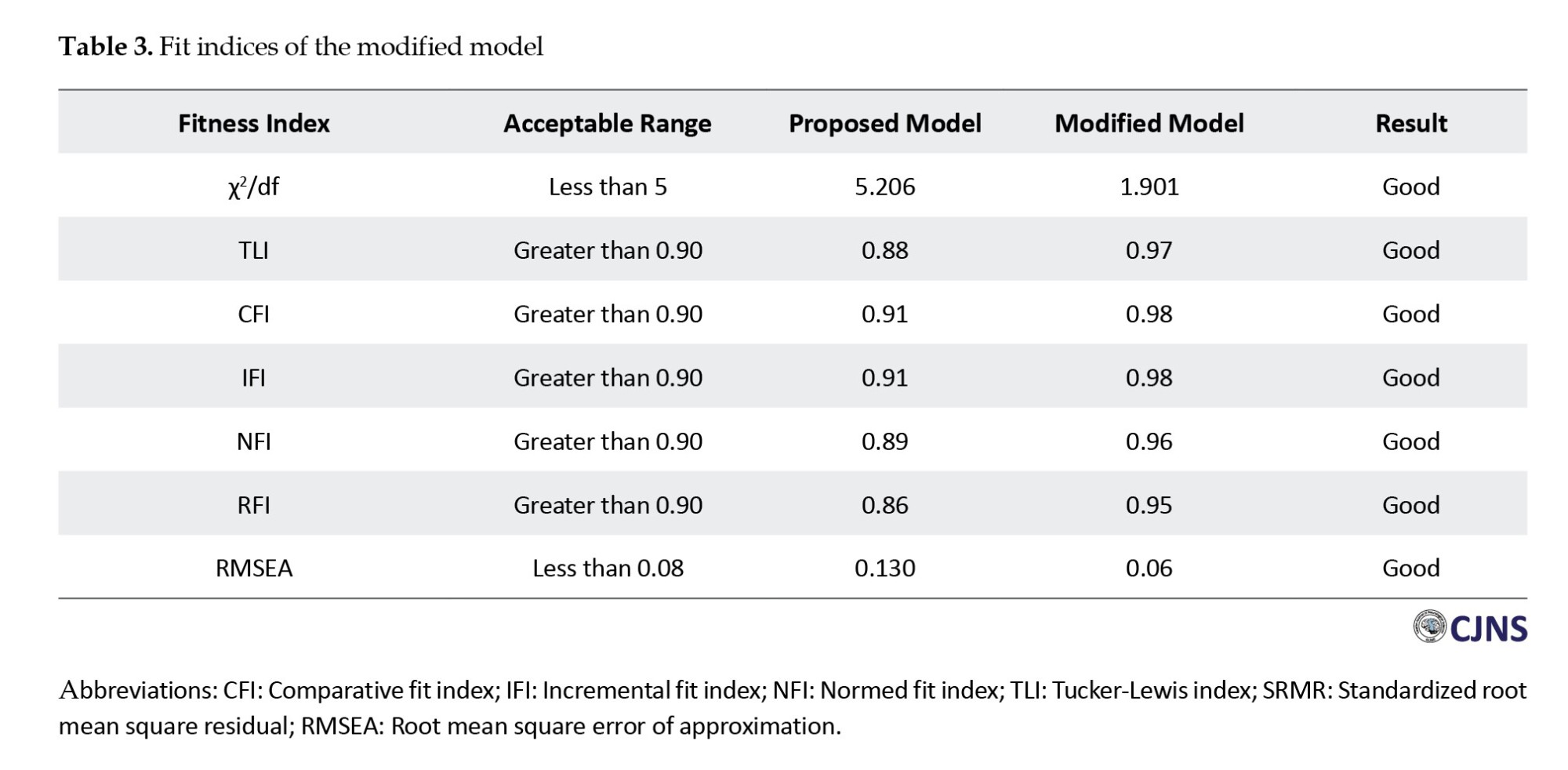
Table 3 shows that the modified model fits the data well. The χ²/df was 1.901, below the recommended threshold of 3, indicating an acceptable fit [36]. The TLI was 0.97, the CFI was 0.98, the IFI was 0.98, the NFI was 0.96, and the RFI was 0.95. These values exceed the commonly accepted cutoff of 0.90 [37, 38]. Furthermore, the RMSEA was 0.06, below the threshold of 0.08, indicating a good fit [38].
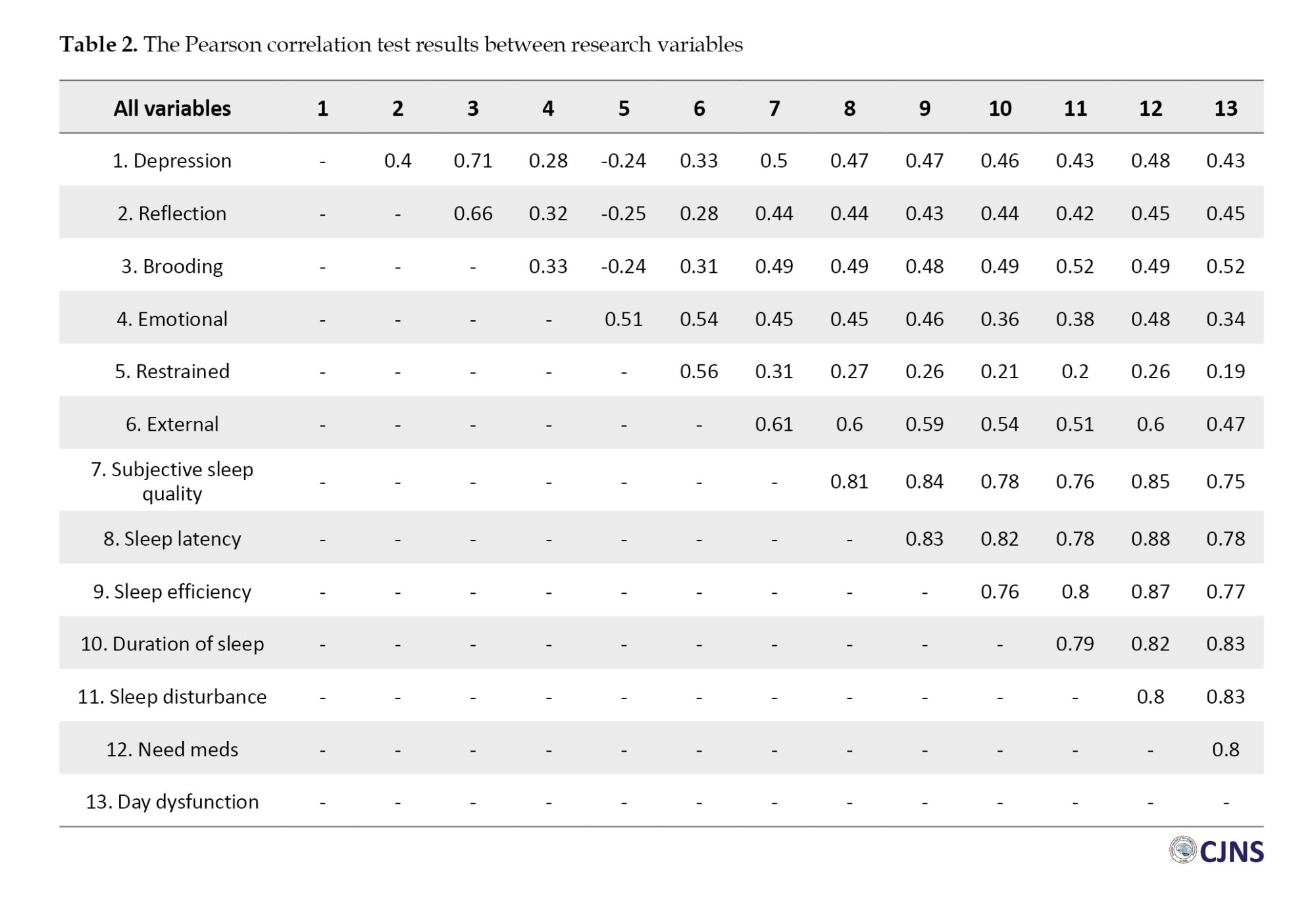
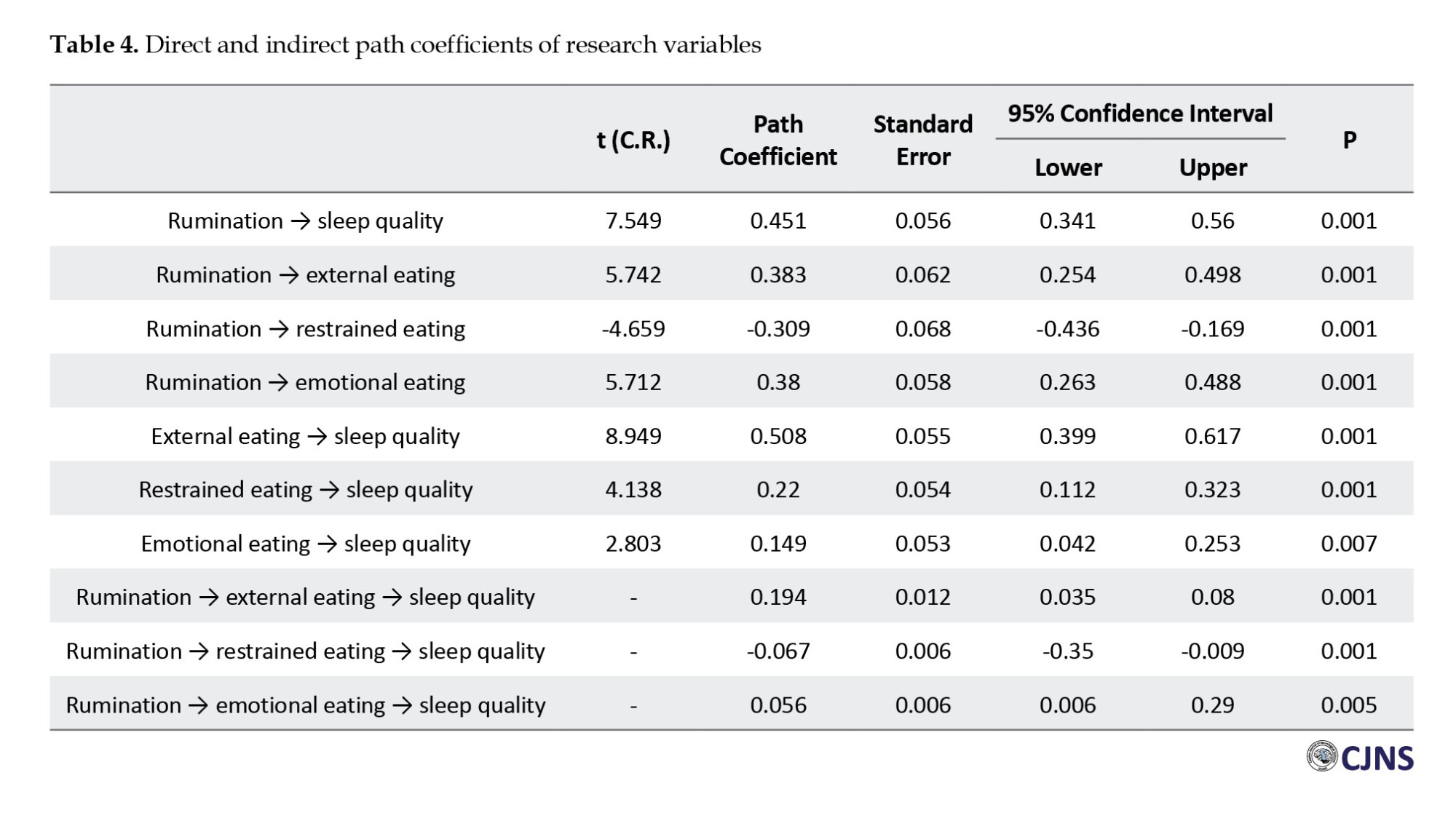
According to Table 4, rumination has a significant direct effect on sleep quality (β=0.451, P=0.001), external eating (β=0.383, P=0.001), restrained eating (β=-0.309, P=0.001), and emotional eating (β=0.380, P=0.001). Additionally, the paths from external eating (β=0.508, P=0.001), restrained eating (β=0.220, P=0.001), and emotional eating (β=0.149, P=0.007) to sleep quality were also significant. Furthermore, the indirect effects of rumination on sleep quality through external eating (β=0.194, P=0.001), restrained eating (β=-0.067, P=0.001), and emotional eating (β=0.056, P=0.005) were reported to be significant.
Discussion
Investigating sleep quality in students is important in today’s society because sleep quality affects students’ academic performance, mental health, and general well-being. The present study aimed to investigate the mediating role of eating behavior in the relationship between rumination and sleep quality in students. The first finding showed that rumination was directly associated with sleep quality, consistent with previous research. Rumination keeps people’s minds active and alert while they sleep, which is the opposite of the relaxation needed to initiate sleep [39]. Also, rumination can lead to maladaptive coping strategies. To manage their distress, people may engage in maladaptive behaviors, such as excessive screen time, substance use, or irregular sleep schedules, that are detrimental to quality sleep. These behaviors can exacerbate sleep problems and create a self-reinforcing cycle of poor sleep and increased rumination [40, 41]. In short, rumination increases physiological arousal, prolongs SOL, and causes frequent awakenings at night, disrupting the natural sleep cycle. Rumination also exacerbates conditions such as anxiety and depression, creating a vicious cycle of distress and poor sleep, all of which lead to reduced sleep quality.
The second finding indicated that external, emotional, and restrained eating behavior each directly impacted sleep quality, consistent with previous research. In explaining this finding, it can be said that quantity and quality of sleep affect eating behavior [42]. Eating behaviors and unhealthy food intake can also affect sleep quality through the gut-brain axis. The gut-brain axis plays a role in sleep regulation, and the gut microbiota influences the production of neurotransmitters and hormones involved in sleep. Foods that support a healthy gut microbiota, such as fiber-rich foods, prebiotics, and probiotics, can positively impact sleep quality [43]. In summary, eating behavior influences sleep quality through various mechanisms, including meal timing, diet’s nutritional content, the role of specific nutrients, hormonal regulation, and psychological factors.
The third finding showed that rumination directly and positively affected external and emotional eating behavior, consistent with previous research. In explaining these findings, it can be said rumination, which is often associated with negative emotions, can lead to unhealthy eating patterns and affect people’s overall well-being through various mechanisms [44]. Negative self-image is another mechanism through which rumination can influence eating behavior. Ruminating people may focus more on their perceived flaws and shortcomings, including weight and body shape [45]. In short, rumination perpetuates a cycle of negative reinforcement. When people start eating in response to rumination and negative emotions, they experience temporary relief. Over time, this pattern becomes ingrained, making it increasingly difficult to break the cycle of rumination and emotional eating. As a result, rumination profoundly influences eating behaviors through various psychological and physiological mechanisms. Conversely, the findings revealed a negative relationship between rumination and restrained eating behavior. That is, higher levels of rumination were linked to reduced self-control over eating. One possible explanation is that rumination heightens anxiety and impairs emotional self-regulation, which in turn weakens an individual’s ability to manage their eating habits. As a result, individuals who engage in frequent rumination may struggle to restrict their food intake, leading to lower levels of restrained eating.
The fourth finding indicated that eating behaviors mediate the relationship between rumination and sleep quality. Specifically, rumination is significantly linked to decreased sleep quality, suggesting that higher rumination increases the likelihood of poor sleep. Likewise, external and emotional eating is associated with worse sleep quality, highlighting these eating behaviors’ negative impact on sleep health. Restrained eating, while directly related to poorer sleep, shows a negative correlation with rumination, meaning individuals who ruminate more tend to engage less in restrained eating. These results can be theoretically understood through emotion regulation theories and cognitive-behavioral models of eating disorders [46, 47]. Rumination, recognized as an unsuccessful emotion regulation method, prolongs or heightens negative emotions such as anxiety and worry, which have been consistently associated with sleep problems in the literature.
The cognitive load imposed by rumination can lead to mental fatigue and make engaging in productive or relaxing activities more difficult. The emotional distress and cognitive overload caused by rumination often lead people to seek maladaptive coping mechanisms to manage their negative emotions. In other words, this constant mental engagement with negative thoughts can lead to a cycle of emotional dysregulation [48, 49]. One common maladaptive coping mechanism is emotional distress eating, in which individuals turn to food to relieve emotional distress. This form of eating is typically characterized by consuming convenient and readily available foods high in sugar, fat, and calories, providing temporary relief from emotional distress [50]. However, this relief is short-lived and can lead to a cycle of unhealthy eating habits. Meanwhile, maladaptive eating behaviors such as external and emotional eating are usually considered a strategy to escape negative emotions or respond to environmental food cues that do not solve emotional problems but weaken sleep quality by increasing psychological burden and disrupting the sleep-wake cycle.
Although restrained eating appears to partially mediate and lessen the negative impact of rumination on sleep, its direct association with poorer sleep suggests that this behavior may contribute to sleep disturbances over time by causing cognitive stress, dissatisfaction with eating control, and anxiety about dietary failure. Consequently, it can be inferred that the eating behaviors explored in this study predominantly have a harmful effect on sleep quality, with only restrained eating showing a limited indirect protective influence. This finding highlights the need for further experimental and theoretical research in future studies.
Despite the evidence that eating behavior mediates the relationship between rumination and sleep quality and fills a research gap in this area, our study has some limitations. First, this study was conducted only in Tehran, and future studies could lead to a larger sample size. The second limitation is its cross-sectional nature, which prevents causal inferences and an accurate understanding of the true nature of the relationships between the study variables. Also, due to the large size of the student population, convenience sampling was used in this study, which may limit the generalizability of the findings. This decision was due to constraints related to time, resources, and access to the entire target population. Future research will also be conducted to suggest some factors that affect sleep quality, such as socioeconomic status. In addition to self-report tools, other assessment methods, such as interviews, should also be considered to supplement the information to measure the research variables. Furthermore, it is recommended that future studies employ random or stratified sampling methods to enhance the external validity of the results.
Conclusion
The results of the present study have several practical applications, as they examine the mediating factor of eating behavior in the relationship between rumination and sleep quality. The results of these studies may be useful for conducting workshops for students. In addition, it can help therapists with diagnosis and treatment. Specifically, rumination is significantly and positively linked to decreased sleep quality. In other words, individuals who engage more in ruminative thinking are more prone to experiencing poor sleep.
Additionally, dysfunctional eating behaviors, including emotional and external eating, are also correlated with poorer sleep quality, highlighting their harmful effects on sleep health. Although restrained eating is directly associated with worse sleep, it differs from other maladaptive eating patterns by showing a negative correlation with rumination. Overall, the findings suggest that most eating behaviors studied here negatively impact sleep quality, with restrained eating potentially providing a limited indirect protective effect. Further research is needed to understand better these behaviors’ exact role in the interplay between emotions, eating, and sleep.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of the Science and Research Branch (SR.C), Islamic Azad University, Tehran, Iran (Code: IR.IAU.SRB.REC.1403.187).
Funding
This study was derived from the master’s thesis of Neda Arabsheybani, approved by the Department of Psychology, Faculty of Literature, Humanities and Social Sciences, Science and Research Branch (SR.C), Islamic Azad University, Tehran, Iran (Code: 162872735).
Authors contributions
Conceptualization, supervision, methodology, review and editing: Sajjad Saadat; Investigation: Shaghayegh Shafiee and Neda Arabsheybani; Resources, funding acquisition, and writing the original draft: Shaghayegh Shafiee and Neda Arabsheybani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to sincerely thank all students who participated in this study.
References
Sleep is an important and global process [1]. Also, it is a natural and physiological state controlled by a neuro-biological process, which is necessary and crucial for human health [2]. The most important predictor of sleep is the quality of sleep, which means the problem and difficulty in falling asleep, staying asleep, the number of times you make up during sleep [3], and the degree of satisfaction and relaxation after waking up [4].
Sleep quality is generally used in sleep medicine. It includes a set of sleep measures, especially total sleep time (TST), sleep onset latency (SOL), sleep maintenance, total wake time (TWT), sleep efficiency (SE), and sleep problems like spontaneous arousal or apnea [5]. Low sleep quality hurts a person’s physical health, such as type 2 diabetes, chronic pain, and blood pressure [1]. In addition, low-quality sleep causes negative effects such as obesity and poor-quality diet [6].
People spend almost one-third of their lives sleeping. Sleep is an inherent physiological process controlled by homeostasis and circadian rhythms. It plays an essential role in maintaining general physical and mental health, but the exact function of sleep is not well understood [7]. Also, many individuals have sleep problems such as restless legs syndrome, insomnia, and sleep apnea [3]. On the other hand, the importance of sleep in college students is very important; college students need quality sleep to improve their academic functioning, emotional state, and problem-solving. Students do not care about the quality of their sleep and lack motivation for its high quality [8].
A review of previous studies suggests that rumination is important in reducing sleep quality. It is defined as a type of cognition that continuously focuses on a specific topic. For instance, thinking about the past or special emotions [9]. Rumination is related to some psychological problems, such as depressive mood, poor general sleep quality, increased sleep latency, sleep disturbances, eating disorders like bulimia and binge eating, binge drinking, anxiety, and obsessive-compulsive disorder or posttraumatic stress disorder (PTSD) [10].
People who ruminate a lot focus on their distress, which makes them feel more negative. This negative mood prevents constructive problem-solving because the person focuses on unpleasant feelings [11]. On the other hand, suppressing rumination may be a coping strategy, but research has shown that suppressing these thoughts increases intrusive thoughts [12]. Furthermore, research has demonstrated that psychosomatic symptoms, such as stomach and intestinal complaints, headaches, and chronic diseases, such as obesity, high blood pressure, diabetes, and cardiovascular illness, are impacted by rumination [13].
As a maladaptive response, rumination causes excessive negative thoughts before sleep, which causes autonomic arousal and emotional distress [14]. Individuals with high rumination traits are prone to experiencing repetitive and unproductive thoughts during the day and also face increased emotional and cognitive arousal at bedtime. They also experience more intrusive thoughts during the pre-sleep period, undermining their sleep quality [15, 16].
A review of previous studies also suggests that eating behavior plays an important role in reducing sleep quality; eating behavior is a complex process that involves the food environment and physiological factors [17]. Eating behavior includes food choice, motivation, eating style, diet, and eating problems, such as obesity, feeding disorders, and eating disorders. Individuals and how much they eat affect their health [18].
One of the common disorders in adolescent girls is obesity, which is caused by disordered eating behavior [18]. In other words, women are more prone to eating disorders [19]. Furthermore, college students have a different lifestyle and diet than other people; they often prefer to use quick and easy meals. Therefore, fast food consumption is high among them. In addition, most students ignore the recommendations of eating habits and skip many meals [20].
The relationship between sleep quality and eating behavior is bidirectional, with poor eating habits or maladaptive eating behavior being associated with an increased prevalence of sleep disorders and mental disorders such as depression and anxiety, and poor sleep quality being associated with an increase in problems related to eating behaviors [21, 22]. A well-rested person with good sleep quality is likelier to have healthier eating behaviors due to improved cognitive function, reduced cravings, and better impulse control. In addition, high-quality sleep can lead to the regulation of hormones such as ghrelin and leptin, which play a role in appetite control [23-25].
On the other hand, individuals with higher rumination traits may use eating as an emotional regulation strategy to cope with negative emotions resulting from repeated negative thinking. As a result, this strategy may become a habit, especially in an uncomfortable situation [26, 27]. From all previous studies, it can be inferred that high levels of rumination play an important role in reducing the quality of sleep in students due to increased unhealthy eating behavior. At the same time, this hypothesis has not been tested in previous studies.
Promoting and supporting healthy eating habits and adaptive eating behaviors among students is essential for educational institutions, as these habits can have a long-term impact on their health, academic success, and sleep quality. The significant issue in the present study is the placement of eating behavior as a mediating variable, which has theoretical support. In other words, mental rumination can lead to different outcomes due to its effect on eating behavior. This study will study the quality of sleep, which indicates a person’s overall view of his sleep status as an outcome.
For this reason, research in this field is important. At first, it seems that this research makes it possible to understand the psychological mechanisms affecting the quality of students’ sleep. This understanding is important for mental health professionals and counselors in providing effective student treatment interventions. Understanding the effect of eating behavior and mental rumination on sleep quality can lead to developing strategies to promote general well-being in students. Overall, it seems that understanding the complex relationships between research variables can significantly add to theoretical knowledge and practical applications in the fields of psychology and counseling, and the findings may contribute to the development of effective treatment approaches, interventions, and educational programs aimed at improving the well-being and sleep quality of students.
Materials and Methods
The present study was cross-sectional using structural equation modeling. In this study, information is collected using self-report questionnaires. Then, the linear relationship between the exogenous and mediator variables and the endogenous variable will be examined. Afterward, the extent to which the eating behavior variable can mediate the relationship between rumination and sleep quality in students will be examined. The statistical population consisted of all Islamic Azad University, Science and Research Branch students studying in Tehran City, Iran, in 2024. According to Kline’s (p.105, 28) recommendation, a sample size of approximately 200 participants is sufficient for an adequate model fit in structural equation modeling. However, considering the potential for sample attrition, the sample size was increased to 250 participants. The sampling method was convenience sampling. The questionnaires were distributed among the Science and Research Branch students of Azad University from March to June 2024. Informed consent was obtained from the participants, and there was an emphasis on maintaining the confidentiality of the collected information. The inclusion criterion was between 18 and 45 years of age. The exclusion criteria included unwillingness to complete the questionnaires, incomplete or distorted responses, a history of psychiatric disorders, receiving psychotherapy services, experiencing psychological trauma, or undergoing treatment for a specific physical illness — all within the past six months.
Study tools
Pittsburgh sleep quality index (PSQI)
The PSQI questionnaire measured the quality of people’s sleep in 19 items. This questionnaire has 7 subscales: Subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medications, and daily functioning disorders. Each component’s minimum and maximum scores range from 0 (no problem) to 3 (very serious problem). A high score on each element or total score indicates poor sleep quality. In the original version of this questionnaire, the Cronbach α coefficient was 0.83 [28]. Also, the Cronbach α coefficient in the Iranian sample was 0.86 [29]. In the present study, internal consistency was calculated as 0.82 using Cronbach’s α.
Ruminative response scale (RRS)
The RRS questionnaire has 22 questions. Participants rate the answers on a scale of 1 (almost never respond this way) to 4 (almost always respond this way). This questionnaire also has three components: Expressing, thinking, and depression. The lower score in this questionnaire is 22, and the upper limit of the score is 88. Higher scores on this questionnaire indicate higher rumination. The Cronbach α coefficient for this scale was 0.90, and the test re-test correlation coefficient was 0.067 over two years [30]. In the Iranian sample, the Cronbach α coefficient for this scale was 0.86 [31]. In the present study, internal consistency was calculated as 0.77 using the Cronbach α.
Dutch eating behavior questionnaire (DEBQ)
Van Strien et al. developed the DEBQ in 1986. It consists of 33 items and identifies three eating patterns: External, restrained, and emotional. Restrained eating refers to deliberately restricting food intake to control or reduce body weight, often through conscious dieting efforts. Emotional eating involves eating in response to emotional states such as anxiety, sadness, loneliness, or anger [32]. External eating is characterized by eating in response to external food-related cues such as the sight, smell, or presence of food, regardless of internal hunger. These eating styles can be considered maladaptive [33]. Emotional eating includes 13 items, external eating consists of 10 items, and restrained eating contains 10 items [32]. The responses are in the form of a 5-point rating, with the lowest rating being the lowest score and the highest rating being the highest (never=1, rarely=2, sometimes=3, often=4, very often=5) [32]. The minimum score for emotional eating is 13, and the maximum is 65. The minimum score for restrained and external eating is 10 and 50. Higher scores on each component indicate a greater extent of that eating behavior pattern. Arhire et al. [34] found that the Cronbach α coefficient was 0.95 for emotional, 0.85 for external, and 0.91 for restrained eating. The Persian version of the DEBQ demonstrated good internal consistency, as indicated by Cronbach α coefficients ranging from 0.77 to 0.83. Also, the construct validity was examined using confirmatory factor analysis. Its 3-factor structure was confirmed (comparative fit index [CFI]=0.91, normed fit index [NFI]=0.9, standardized root mean square residual [SRMR]=0.072, The root mean square error of approximation [RMSEA]=0.082) [35]. In the present study, internal consistency was calculated as 0.77 for external, 0.79 for restrained, and 0.81 for emotional eating using Cronbach α values.
Data analysis
SPSS and AMOS software version 24 were used to analyze the data. The research data analysis method was structural equation modeling. The fit of the research model was examined based on maximum likelihood estimation. The fit indices of χ2/df, Tucker-Lewis Index (TLI), CFI, incremental fit index (IFI), NFI, relative fit index (RFI), and RMSEA were reported. Also, to examine the direct and indirect effects, the bootstrap test with 5000 repetitions was used.
Results
Two hundred fifty students participated in this study, and information about the participants includes age, gender, and level of education. The mean age of the participants was 29.39, with the lowest age being 18 and the highest age being 41. The standard deviation was 6.85. One hundred twenty-eight women (51.2%) and 122 men (48.8%) participated in this study. Also, 28(11.2%) of them had an associate degree, 105(42%) had a bachelor’s degree, 87(34.8%) had a master’s degree, and 30(12%) had a PhD. In Table 1, the descriptive findings of the research variables and the normality of the data distribution are presented by skewness and kurtosis statistics.
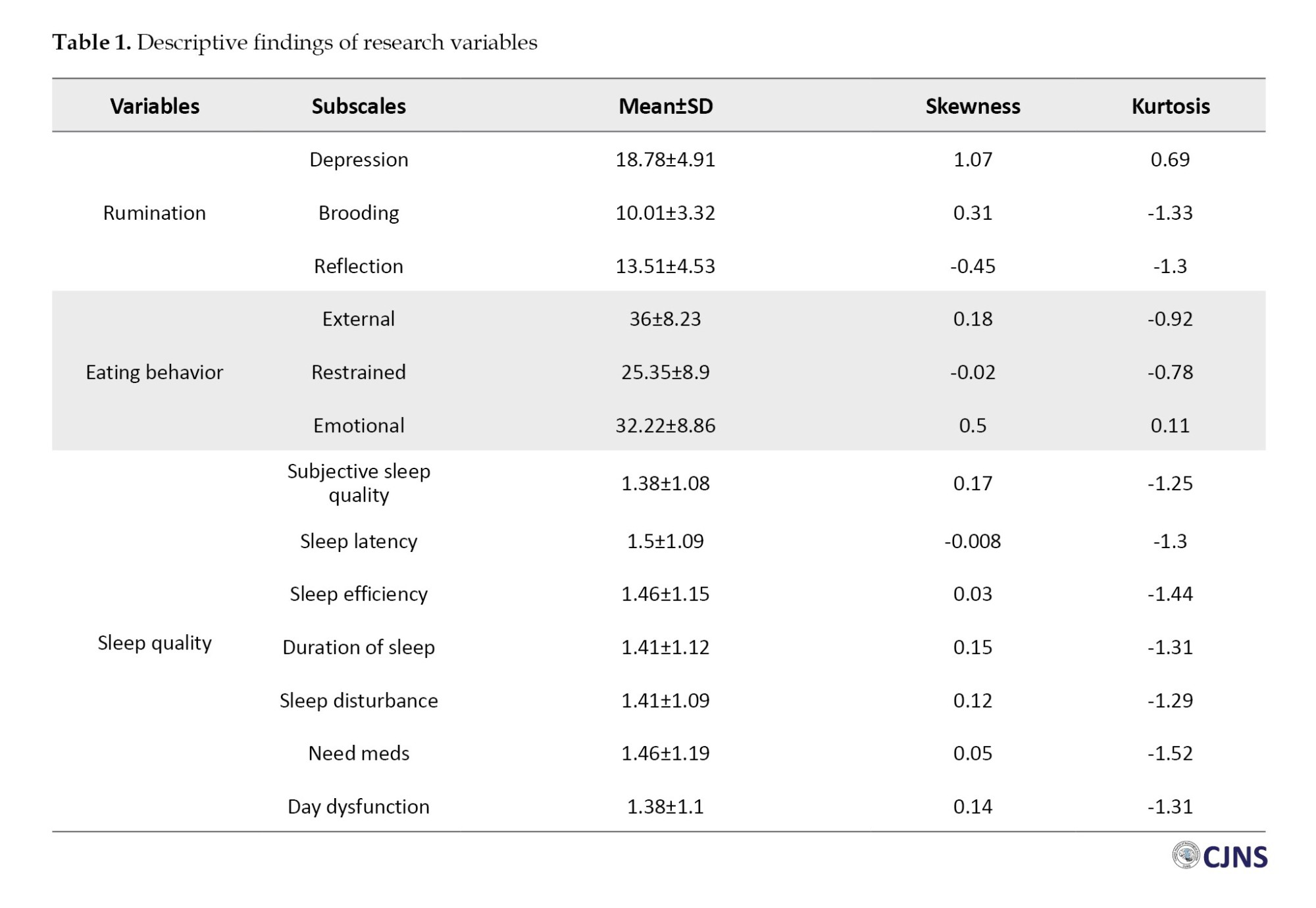
Table 1 shows the average scores of the research variables. In addition, the results of the examination of the skewness and kurtosis statistics have shown that they are all in the range of -2 to -2; based on these statistics, the research data has a normal distribution. Based on this, the use of parametric tests is allowed. The results of the Pearson correlation test are presented below.
Table 2 shows a significant correlation between rumination, sleep quality, and eating behavior (P<0.05). The following presents autocorrelation results in the residuals and multicollinearity (collinearity) between predictor changes. Based on this, the autocorrelation value in the residuals was reported to be favorable using Durbin-Watson’s test (1.794) as it was in the range of 1.5 to 2.5. Also, there was no multicollinearity (collinearity) between pre-interval variables, and the tolerance value was calculated between 0.32 and 0.61. In addition, the variance inflation index was lower than 5, indicating the VIF index’s acceptable limit.
Structural equation modeling and bootstrap testing were used to test this hypothesis, and the results are presented below. Figure 1 shows the structural equation model in the standard mode.
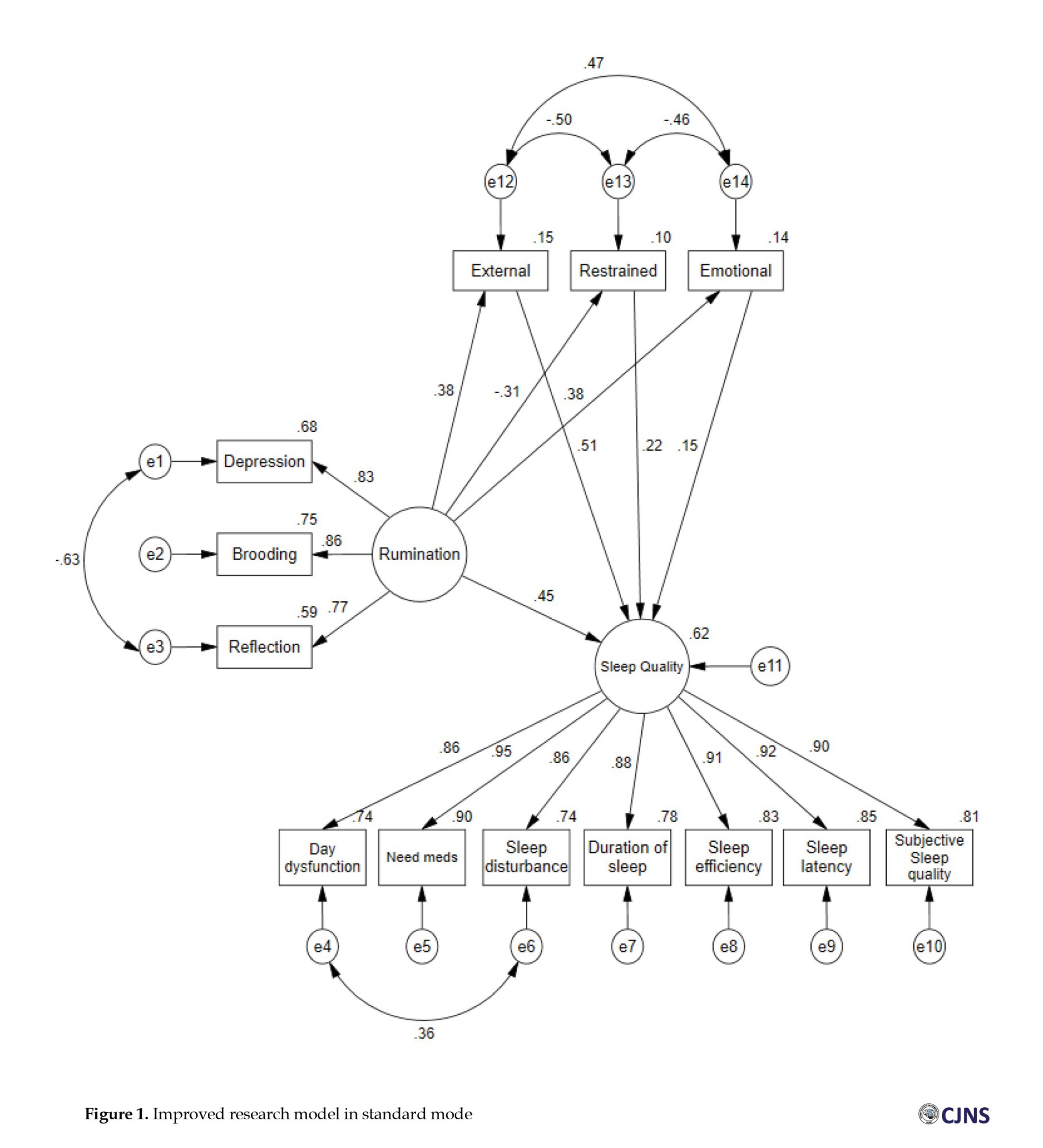
The results of Figure 1 show that the improved research model predicted 62% of the sleep quality in 250 participants. The fit indices of the proposed and modified model are presented in Table 3.
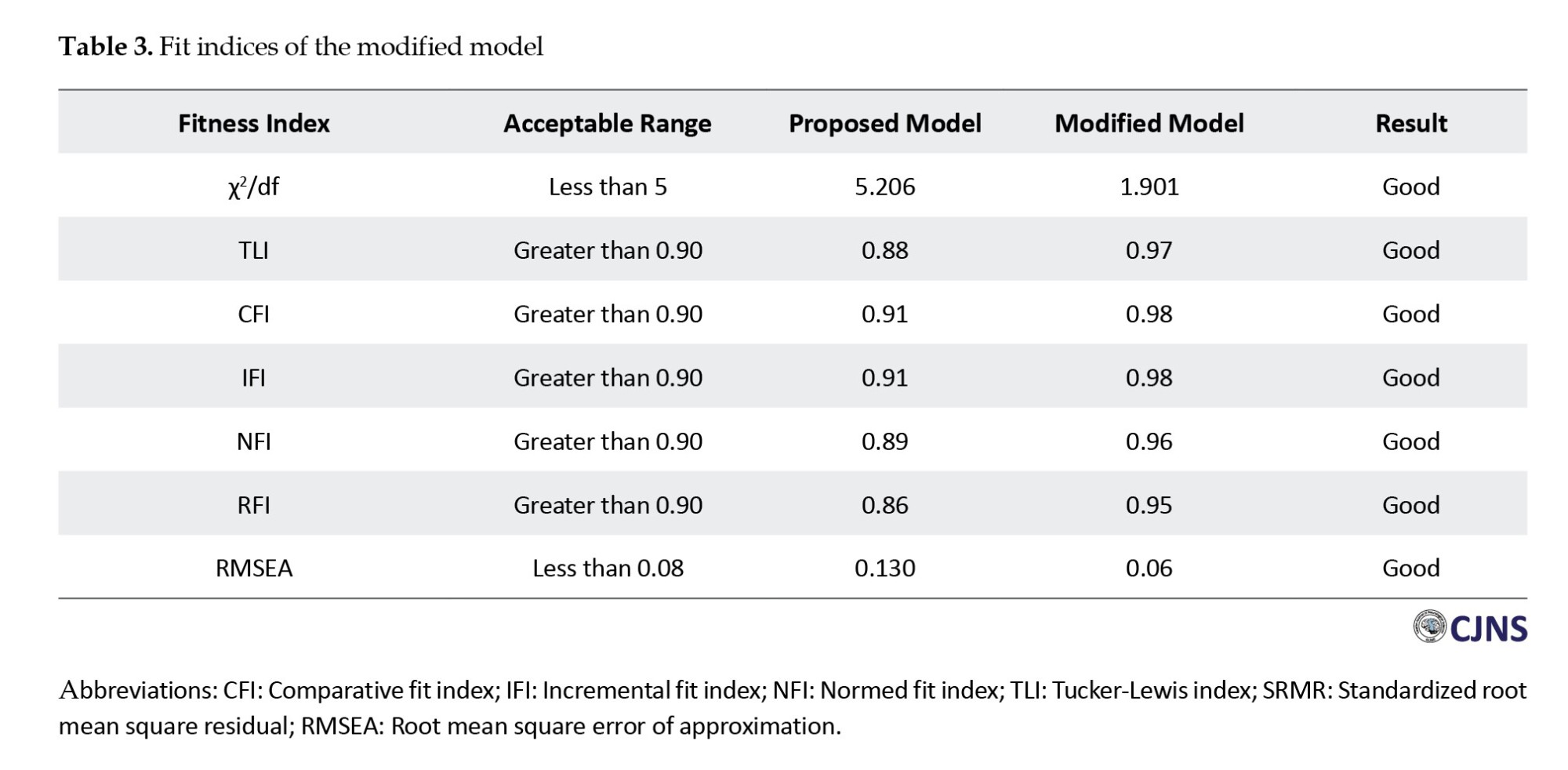
Table 3 shows that the modified model fits the data well. The χ²/df was 1.901, below the recommended threshold of 3, indicating an acceptable fit [36]. The TLI was 0.97, the CFI was 0.98, the IFI was 0.98, the NFI was 0.96, and the RFI was 0.95. These values exceed the commonly accepted cutoff of 0.90 [37, 38]. Furthermore, the RMSEA was 0.06, below the threshold of 0.08, indicating a good fit [38].
According to Table 4, rumination has a significant direct effect on sleep quality (β=0.451, P=0.001), external eating (β=0.383, P=0.001), restrained eating (β=-0.309, P=0.001), and emotional eating (β=0.380, P=0.001). Additionally, the paths from external eating (β=0.508, P=0.001), restrained eating (β=0.220, P=0.001), and emotional eating (β=0.149, P=0.007) to sleep quality were also significant. Furthermore, the indirect effects of rumination on sleep quality through external eating (β=0.194, P=0.001), restrained eating (β=-0.067, P=0.001), and emotional eating (β=0.056, P=0.005) were reported to be significant.
Discussion
Investigating sleep quality in students is important in today’s society because sleep quality affects students’ academic performance, mental health, and general well-being. The present study aimed to investigate the mediating role of eating behavior in the relationship between rumination and sleep quality in students. The first finding showed that rumination was directly associated with sleep quality, consistent with previous research. Rumination keeps people’s minds active and alert while they sleep, which is the opposite of the relaxation needed to initiate sleep [39]. Also, rumination can lead to maladaptive coping strategies. To manage their distress, people may engage in maladaptive behaviors, such as excessive screen time, substance use, or irregular sleep schedules, that are detrimental to quality sleep. These behaviors can exacerbate sleep problems and create a self-reinforcing cycle of poor sleep and increased rumination [40, 41]. In short, rumination increases physiological arousal, prolongs SOL, and causes frequent awakenings at night, disrupting the natural sleep cycle. Rumination also exacerbates conditions such as anxiety and depression, creating a vicious cycle of distress and poor sleep, all of which lead to reduced sleep quality.
The second finding indicated that external, emotional, and restrained eating behavior each directly impacted sleep quality, consistent with previous research. In explaining this finding, it can be said that quantity and quality of sleep affect eating behavior [42]. Eating behaviors and unhealthy food intake can also affect sleep quality through the gut-brain axis. The gut-brain axis plays a role in sleep regulation, and the gut microbiota influences the production of neurotransmitters and hormones involved in sleep. Foods that support a healthy gut microbiota, such as fiber-rich foods, prebiotics, and probiotics, can positively impact sleep quality [43]. In summary, eating behavior influences sleep quality through various mechanisms, including meal timing, diet’s nutritional content, the role of specific nutrients, hormonal regulation, and psychological factors.
The third finding showed that rumination directly and positively affected external and emotional eating behavior, consistent with previous research. In explaining these findings, it can be said rumination, which is often associated with negative emotions, can lead to unhealthy eating patterns and affect people’s overall well-being through various mechanisms [44]. Negative self-image is another mechanism through which rumination can influence eating behavior. Ruminating people may focus more on their perceived flaws and shortcomings, including weight and body shape [45]. In short, rumination perpetuates a cycle of negative reinforcement. When people start eating in response to rumination and negative emotions, they experience temporary relief. Over time, this pattern becomes ingrained, making it increasingly difficult to break the cycle of rumination and emotional eating. As a result, rumination profoundly influences eating behaviors through various psychological and physiological mechanisms. Conversely, the findings revealed a negative relationship between rumination and restrained eating behavior. That is, higher levels of rumination were linked to reduced self-control over eating. One possible explanation is that rumination heightens anxiety and impairs emotional self-regulation, which in turn weakens an individual’s ability to manage their eating habits. As a result, individuals who engage in frequent rumination may struggle to restrict their food intake, leading to lower levels of restrained eating.
The fourth finding indicated that eating behaviors mediate the relationship between rumination and sleep quality. Specifically, rumination is significantly linked to decreased sleep quality, suggesting that higher rumination increases the likelihood of poor sleep. Likewise, external and emotional eating is associated with worse sleep quality, highlighting these eating behaviors’ negative impact on sleep health. Restrained eating, while directly related to poorer sleep, shows a negative correlation with rumination, meaning individuals who ruminate more tend to engage less in restrained eating. These results can be theoretically understood through emotion regulation theories and cognitive-behavioral models of eating disorders [46, 47]. Rumination, recognized as an unsuccessful emotion regulation method, prolongs or heightens negative emotions such as anxiety and worry, which have been consistently associated with sleep problems in the literature.
The cognitive load imposed by rumination can lead to mental fatigue and make engaging in productive or relaxing activities more difficult. The emotional distress and cognitive overload caused by rumination often lead people to seek maladaptive coping mechanisms to manage their negative emotions. In other words, this constant mental engagement with negative thoughts can lead to a cycle of emotional dysregulation [48, 49]. One common maladaptive coping mechanism is emotional distress eating, in which individuals turn to food to relieve emotional distress. This form of eating is typically characterized by consuming convenient and readily available foods high in sugar, fat, and calories, providing temporary relief from emotional distress [50]. However, this relief is short-lived and can lead to a cycle of unhealthy eating habits. Meanwhile, maladaptive eating behaviors such as external and emotional eating are usually considered a strategy to escape negative emotions or respond to environmental food cues that do not solve emotional problems but weaken sleep quality by increasing psychological burden and disrupting the sleep-wake cycle.
Although restrained eating appears to partially mediate and lessen the negative impact of rumination on sleep, its direct association with poorer sleep suggests that this behavior may contribute to sleep disturbances over time by causing cognitive stress, dissatisfaction with eating control, and anxiety about dietary failure. Consequently, it can be inferred that the eating behaviors explored in this study predominantly have a harmful effect on sleep quality, with only restrained eating showing a limited indirect protective influence. This finding highlights the need for further experimental and theoretical research in future studies.
Despite the evidence that eating behavior mediates the relationship between rumination and sleep quality and fills a research gap in this area, our study has some limitations. First, this study was conducted only in Tehran, and future studies could lead to a larger sample size. The second limitation is its cross-sectional nature, which prevents causal inferences and an accurate understanding of the true nature of the relationships between the study variables. Also, due to the large size of the student population, convenience sampling was used in this study, which may limit the generalizability of the findings. This decision was due to constraints related to time, resources, and access to the entire target population. Future research will also be conducted to suggest some factors that affect sleep quality, such as socioeconomic status. In addition to self-report tools, other assessment methods, such as interviews, should also be considered to supplement the information to measure the research variables. Furthermore, it is recommended that future studies employ random or stratified sampling methods to enhance the external validity of the results.
Conclusion
The results of the present study have several practical applications, as they examine the mediating factor of eating behavior in the relationship between rumination and sleep quality. The results of these studies may be useful for conducting workshops for students. In addition, it can help therapists with diagnosis and treatment. Specifically, rumination is significantly and positively linked to decreased sleep quality. In other words, individuals who engage more in ruminative thinking are more prone to experiencing poor sleep.
Additionally, dysfunctional eating behaviors, including emotional and external eating, are also correlated with poorer sleep quality, highlighting their harmful effects on sleep health. Although restrained eating is directly associated with worse sleep, it differs from other maladaptive eating patterns by showing a negative correlation with rumination. Overall, the findings suggest that most eating behaviors studied here negatively impact sleep quality, with restrained eating potentially providing a limited indirect protective effect. Further research is needed to understand better these behaviors’ exact role in the interplay between emotions, eating, and sleep.
Ethical Considerations
Compliance with ethical guidelines
The present study was approved by the Ethics Committee of the Science and Research Branch (SR.C), Islamic Azad University, Tehran, Iran (Code: IR.IAU.SRB.REC.1403.187).
Funding
This study was derived from the master’s thesis of Neda Arabsheybani, approved by the Department of Psychology, Faculty of Literature, Humanities and Social Sciences, Science and Research Branch (SR.C), Islamic Azad University, Tehran, Iran (Code: 162872735).
Authors contributions
Conceptualization, supervision, methodology, review and editing: Sajjad Saadat; Investigation: Shaghayegh Shafiee and Neda Arabsheybani; Resources, funding acquisition, and writing the original draft: Shaghayegh Shafiee and Neda Arabsheybani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to sincerely thank all students who participated in this study.
References
- Clement-Carbonell V, Portilla-Tamarit I, Rubio-Aparicio M, Madrid-Valero JJ. Sleep quality, mental and physical health: a differential relationship. Int J Environ Res Public Health. 2021; 18(2):460. [DOI:10.3390/ijerph18020460.] [PMID] [PMCID]
- Sejbuk M, Mirończuk-Chodakowska I, Witkowska AM. Sleep quality: A narrative review on nutrition, stimulants, and physical activity as important factors. Nutrients. 2022; 14(9):1912. [DOI:10.3390/nu14091912.] [PMID] [PMCID]
- Alnawwar MA, Alraddadi MI, Algethmi RA, Salem GA, Salem MA, Alharbi AA. The effect of physical activity on sleep quality and sleep disorder: A systematic review. Cureus. 2023; 15(8):e43595. [DOI:10.7759/cureus.43595] [PMID] [PMCID]
- Denison HJ, Jameson KA, Sayer AA, Patel HP, Edwards MH, Arora T, et al. Poor sleep quality and physical performance in older adults. Sleep Health. 2021; 7(2):205-11. [DOI:10.1016/j.sleh.2020.10.002.] [PMID]
- Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: A review. Int J Environ Res Public Health. 2021; 18(3):1082. [DOI:10.3390/ijerph18031082.] [PMID] [PMCID]
- Grummon AH, Sokol RL, Lytle LA. Is late bedtime an overlooked sleep behaviour? Investigating associations between sleep timing, sleep duration and eating behaviours in adolescence and adulthood. Public Health Nutr. 2021; 24(7):1671-7. [DOI:10.1017/s1368980020002050.] [PMID] [PMCID]
- Cudney LE, Frey BN, McCabe RE, Green SM. Investigating the relationship between objective measures of sleep and self-report sleep quality in healthy adults: A review. J Clin Sleep Med. 2022; 18(3):927-36. [DOI:10.5664/jcsm.9708.] [PMID] [PMCID]
- Pham HT, Chuang HL, Kuo CP, Yeh TP, Liao WC. Electronic device use before bedtime and sleep quality among university students. Healthcare. 2021; 9(9):1091. [DOI:10.3390/healthcare9091091.] [PMID] [PMCID]
- Moulds ML, Bisby MA, Wild J, Bryant RA. Rumination in posttraumatic stress disorder: A systematic review. Clin Psychol Rev. 2020; 82:101910. [DOI:10.1016/j.cpr.2020.101910.] [PMID]
- Nowakowska-Domagała K, Juraś-Darowny M, Pietras T, Stecz P, Mokros Ł. Chronotype and poor sleep quality in young adults - a pilot study on the role of rumination. Sleep Med. 2022; 100:206-11. [DOI:10.1016/j.sleep.2022.08.012.] [PMID]
- Nagy LM, Shanahan ML, Seaford SP. Nonsuicidal self-injury and rumination: A meta-analysis. J Clin Psychol. 2023; 79(1):7-27. [DOI:10.1002/jclp.23394.] [PMID] [PMCID]
- Barba T, Buehler S, Kettner H, Radu C, Cunha BG, Nutt DJ, et al. Effects of psilocybin versus escitalopram on rumination and thought suppression in depression. BJPsych Open. 2022; 8(5):e163. [DOI:10.1192/bjo.2022.565.] [PMID] [PMCID]
- Nourian L Aghaei A, Ghorbani M. [Effectiveness of acceptance and commitment therapy on emotional eating among obese women (Persian)]. Knowledge Res Appl Psychol. 2017; 16(2):15-23. [Link]
- Takano K, Sakamoto S, Tanno Y. Ruminative self-focus in daily life: Associations with daily activities and depressive symptoms. Emotion. 2013; 13(4):657-67. [DOI:10.1037/a0031867] [PMID]
- Pillai V. Drake CL. Sleep and repetitive thought: the role of rumination and worry in sleep disturbance. In: babson ka, Feldner mt, editors. Sleep and affect: Assessment, theory, and clinical implications. London: Academic Press; 2015. [DOI:10.1016/B978-0-12-417188-6.00010-4.]
- Clancy F, Prestwich A, Caperon L, Tsipa A, O'Connor DB. The association between worry and rumination with sleep in non-clinical populations: A systematic review and meta-analysis. Health Psychol Rev. 2020; 14(4):427-48. [DOI:10.1080/17437199.2019.1700819.] [PMID]
- Gal AM, Iatcu CO, Popa AD, Arhire LI, Mihalache L, Gherasim A, et al. Understanding the interplay of dietary intake and eating behavior in type 2 diabetes. Nutrients. 2024; 16(6):771. [DOI:10.3390/nu16060771.] [PMID] [PMCID]
- lacaille l. Eating behavior. In: Gellman MD, editor. Encyclopedia of behavioral medicine. 2th ed. Cham: Springer; 2020. [DOI:10.1007/978-3-030-39903-0_1613]
- Ljubičić M, Matek Sarić M, Klarin I, Rumbak I, Colić Barić I, Ranilović J, et al. Emotions and food consumption: Emotional eating behavior in a European population. Foods. 2023; 12(4):872. [DOI:10.3390/foods12040872.] [PMID] [PMCID]
- Choi J. Impact of stress levels on eating behaviors among college students. Nutrients. 2020; 12(5):1241. [DOI:10.3390/nu12051241.] [PMID] [PMCID]
- Allison KC, Spaeth A, Hopkins CM. Sleep and eating disorders. Curr Psychiatry Rep. 2016; 18(10):92. [DOI:10.1007/s11920-016-0728-8.] [PMID]
- Goel NJ, Sadeh-Sharvit S, Trockel M, Flatt RE, Fitzsimmons-Craft EE, Balantekin KN, et al. Depression and anxiety mediate the relationship between insomnia and eating disorders in college women. J Am Coll Health. 2021; 69(8):976-81. [DOI:10.1080/07448481.2019.1710152.] [PMID] [PMCID]
- Gomes S, Ramalhete C, Ferreira I, Bicho M, Valente A. Sleep patterns, eating behavior and the risk of noncommunicable diseases. Nutrients. 2023; 15(11):2462. [DOI:10.3390/nu15112462.] [PMID] [PMCID]
- Peach HD, Gaultney JF. Sleep, impulse control, and sensation-seeking predict delinquent behavior in adolescents, emerging adults, and adults. J Adolesc Health. 2013; 53(2):293-9. [DOI:10.1016/j.jadohealth.2013.03.012.] [PMID]
- Vanderlind WM, Beevers CG, Sherman SM, Trujillo LT, McGeary JE, Matthews MD, et al. Sleep and sadness: Exploring the relation among sleep, cognitive control, and depressive symptoms in young adults. Sleep Med. 2014; 15(1):144-9. [DOI:10.1016/j.sleep.2013.10.006] [PMID] [PMCID]
- Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: A meta-analysis. Clin Psychol Rev. 2018; 61:9-23. [DOI:10.1016/j.cpr.2018.03.004.] [PMID] [PMCID]
- Rickerby N, Krug I, Fuller-Tyszkiewicz M, Forte E, Davenport R, Chayadi E, et al. Rumination across depression, anxiety, and eating disorders in adults: A meta-analytic review. Clin Psychol Sci Pract. 2022; 31(2):251-68. [DOI:10.1037/cps0000110]
- Buysse DJ, Reynolds 3rd CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Heydarei AR, Ehteshamzadeh P, Marashi M. [The relationship between insomnia severity, sleep quality, sleepiness, and health disorders with academic performance in girls (Persian)]. Women Cult Psychol. 2010; 1(4):65-76. [Link]
- Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. J Pers Soc Psychol. 1994; 67(1):92-104. [DOI:10.1037/0022-3514.67.1.92.] [PMID]
- Tanhaye Reshvanloo F, Torkamani M, Mirshahi S, Hajibakloo N, Kareshki H. [Validity and reliability assessment of the Persian version of the co-rumination questionnaire (Persian)]. J Clin Psychol. 2021; 13(1):79-87. [DOI:10.22075/jcp.2021.20312.1874.]
- Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986; 5(2):295-315. [DOI:10.1002/1098-108X(198602)5:2%3C295::AID-EAT2260050209%3E3.0.CO;2-T.]
- Canova L, Bobbio A, Benincà A, Manganelli AM. Italian validation of a short version of the Dutch eating behavior questionnaire: Psychometric properties and relationships with self-esteem, eating self-efficacy, and snacking habits in university students. Health Psychol Open. 2024; 11:20551029241262665. [DOI:10.1177/20551029241262665.] [PMID] [PMCID]
- Arhire LI, Niță O, Popa AD, Gal AM, Dumitrașcu O, Gherasim A, Mihalache L, et al. Validation of the Dutch eating behavior questionnaire in a Romanian adult population. Nutrients. 2021; 13(11):3890. [DOI:10.3390/nu13113890.] [PMID] [PMCID]
- Nejati V, Alipour F, Saeidpour S, Bodaghi E. Psychometric properties of Persian version of Dutch Eating Behavior Questionnaire. J Fundam Ment Health. 2018; 20(1):3-11. [DOI:10.22038/jfmh.2017.10033.]
- Whittaker TA, Schumacker RE. A beginner's guide to structural equation modeling. 5th ed. New York: Routledge; 2022. [DOI:10.4324/9781003044017]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980; 88(3):588-606. [DOI:10.1037/0033-2909.88.3.588.]
- Kline RB. Principles and practice of structural equation modeling. 5th ed. New York: Guilford publications; 2023. [Link]
- Yeh ZT, Wung SK, Lin CM. Pre-sleep arousal as a mediator of relationships among worry, rumination, and sleep quality. Int J Cogn Ther. 2015; 8(1):21-34. [DOI:10.1521/ijct.2015.8.1.21.]
- Tousignant OH, Taylor ND, Suvak MK, Fireman GD. Effects of rumination and worry on sleep. Behav Ther. 2019; 50(3):558-70. [DOI:10.1016/j.beth.2018.09.005.] [PMID]
- Kozusznik MW, Puig-Perez S, Kożusznik B, Pulopulos MM. The relationship between coping strategies and sleep problems: The role of depressive symptoms. Ann Behav Med. 2021; 55(3):253-65. [DOI:10.1093/abm/kaaa048.] [PMID] [PMCID]
- Lotfi M, Al-Hosseini MK, Jafarirad S. The relationship of sleep quality with eating behavior and food intake among male university students. J Sleep Med Disord. 2015; 2(5):1034. [Link]
- Tang M, Song X, Zhong W, Xie Y, Liu Y, Zhang X. Dietary fiber ameliorates sleep disturbance connected to the gut-brain axis. Food Funct. 2022; 13(23):12011-20. [DOI:10.1039/D2FO01178F.] [PMID]
- Kornacka M, Czepczor-Bernat K, Napieralski P, Brytek-Matera A. Rumination, mood, and maladaptive eating behaviors in overweight and healthy populations. Eat Weight Disord. 2021; 26(1):273-85. [DOI:10.1007/s40519-020-00857-z.] [PMID] [PMCID]
- Gordon KH, Holm-Denoma JM, Troop-Gordon W, Sand E. Rumination and body dissatisfaction interact to predict concurrent binge eating. Body Image. 2012; 9(3):352-7. [DOI:10.1016/j.bodyim.2012.04.001.] [PMID]
- Spoor ST, Bekker MH, Van Strien T, van Heck GL. Relations between negative affect, coping, and emotional eating. Appetite. 2007; 48(3):368-76. [DOI:10.1016/j.appet.2006.10.005.] [PMID]
- Vitousek KM, Brown KE. Cognitive‐behavioral theory of eating disorders. In: smolak l, levine mp, editors. The Wiley handbook of eating disorders. Hoboken: Wiley Blackwell; 2015. [DOI:10.1002/9781118574089.ch18.]
- Ehring T, Ehlers A. Does rumination mediate the relationship between emotion regulation ability and posttraumatic stress disorder? Eur J Psychotraumatol. 2014; 5. [DOI:10.3402/ejpt.v5.23547.] [PMID] [PMCID]
- Querstret D, Cropley M. Exploring the relationship between work-related rumination, sleep quality, and work-related fatigue. J Occup Health Psychol. 2012; 17(3):341-53. [DOI:10.1037/a0028552.] [PMID]
- Macht M, Simons G. Emotional eating. In: Nyklíček I, Vingerhoets A, Zeelenberg M, editors. Emotion regulation and well-being. New York: Springer; 2011. [DOI:10.1007/978-1-4419-6953-8_17.]
Type of Study: Research |
Subject:
General
Received: 2025/04/18 | Accepted: 2025/06/12 | Published: 2025/07/1
Received: 2025/04/18 | Accepted: 2025/06/12 | Published: 2025/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |