Fri, Jan 30, 2026
Volume 11, Issue 1 (Winter 2025)
Caspian J Neurol Sci 2025, 11(1): 58-66 |
Back to browse issues page
Ethics code: IR.GUMS.REC.1400.424
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahdavi F, Fallah-Arzpeima S, Reihanian Z, Asadi K, Zaresharifi N, Zare R, et al . The Impact of COVID-19 on Clinical Outcomes in Patients With Traumatic Brain Injury. Caspian J Neurol Sci 2025; 11 (1) :58-66
URL: http://cjns.gums.ac.ir/article-1-767-en.html
URL: http://cjns.gums.ac.ir/article-1-767-en.html
Farnaz Mahdavi1 

 , Sima Fallah-Arzpeima2
, Sima Fallah-Arzpeima2 

 , Zoheir Reihanian *3
, Zoheir Reihanian *3 

 , Khatereh Asadi4
, Khatereh Asadi4 

 , Nooshin Zaresharifi5
, Nooshin Zaresharifi5 

 , Roghaye Zare6
, Roghaye Zare6 

 , Mohammad Ali Yazdanipour7
, Mohammad Ali Yazdanipour7 

 , Masoud Shabani Chobe7
, Masoud Shabani Chobe7 




 , Sima Fallah-Arzpeima2
, Sima Fallah-Arzpeima2 

 , Zoheir Reihanian *3
, Zoheir Reihanian *3 

 , Khatereh Asadi4
, Khatereh Asadi4 

 , Nooshin Zaresharifi5
, Nooshin Zaresharifi5 

 , Roghaye Zare6
, Roghaye Zare6 

 , Mohammad Ali Yazdanipour7
, Mohammad Ali Yazdanipour7 

 , Masoud Shabani Chobe7
, Masoud Shabani Chobe7 


1- School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Radiology, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Neurosurgery, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,zoheir.reihanian@gmail.com
4- Biotechnology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
5- Department of Pathology, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
6- Trauma Institute, Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran.
7- Trauma Institute, Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Radiology, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Neurosurgery, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran. ,
4- Biotechnology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
5- Department of Pathology, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
6- Trauma Institute, Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran.
7- Trauma Institute, Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 1304 kb]
(343 Downloads)
| Abstract (HTML) (972 Views)
Full-Text: (212 Views)
Introduction
Traumatic brain injury (TBI) is a leading cause of emergency department visits and a major contributor to mortality and morbidity worldwide [1, 2]. TBI is a significant socioeconomic issue that burdens healthcare systems and affects individuals’ lives [1-3]. The incidence of severe consequences, such as intracranial hemorrhages, is mainly associated with TBIs following road traffic accidents rather than other types of traumatic injuries [3]. In addition to the initial brain damage, some avoidable secondary processes, such as progressive hemorrhagic injury (PHI) following intracranial bleeding, can deteriorate the general condition [4]. Hence, risk factors related to PHI should be addressed [4]. Evidence of a direct association exists between PHI and several risk factors, including a high D-dimer level, thrombocytopenia, leukocytosis, and prolonged prothrombin time (PT) [1, 4, 5]. Therefore, it seems rational to accept that coagulation disorders may contribute to poor prognosis in patients with TBI. Moreover, there is a correlation between higher mortality rates after TBIs and comorbidities such as hematologic malignancies and coagulation disorders [4, 6-8].
Coronavirus disease 2019 (COVID-19) emerged as a new infectious disease outbreaking in late December 2019. The disease originated in China and rapidly spread globally [9]. Therefore, in March 2020, the World Health Organization (WHO) declared that the COVID-19 outbreak became a pandemic and a primary global concern [10].
COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), an RNA virus [11]. Due to the virus’s high mutation rate, many subtypes have emerged that can impact symptoms’ incidence and severity. SARS-CoV-2 can lead to high morbidity and mortality rates, which can simultaneously affect various body organs, including the respiratory, cardiovascular, gastrointestinal, central nervous and hematopoietic systems [11, 12]. Although initially manifesting as a respiratory tract infection, subsequent data noted that it should be considered a systemic disease [11]. COVID-19 can impact the hematopoietic system remarkably, often associated with a hypercoagulability state [11]. Main hematologic findings include lymphocytopenia, thrombocytopenia, elevated D-dimer, and prolonged PT [11]. Also, a high rate of arterial and venous thromboembolisms at the first 24 hours of admission is reported among several COVID-19 patients [13, 14].
Angiotensin-converting enzyme 2 (ACE2) is an essential component of the renin-angiotensin-aldosterone system, which plays a crucial role in maintaining homeostasis [15]. It is a pro-inflammatory agent and vasoconstrictor, expressed in almost all organs [16]. ACE2 in lung pneumocytes type 2 can act as a receptor for SARS-CoV-2 [17]. This attachment inhibits ACE2 and facilitates virus entry into cells, followed by boosting cell infection [15, 16]. ACE2 receptors are also present in cerebrovascular endothelial cells, which regulate various brain functions, including autoregulation of cerebral perfusion [15]. Thus, COVID-19 can disrupt autoregulation in CNS and peripheral nervous system [16, 18-23]. Several researchers investigated the most common cranial hemorrhagic patterns both before and after the COVID-19 era, consisting of SDH, SAH and brain contusions, together with falling, which is the most frequent head trauma mechanism [13, 24].
Considering the effects of COVID-19 on various organs, especially the CNS and hematologic system, we aimed to assess the impact of COVID-19 infection on mortality and the average cerebral hemorrhage volume (ACHV) in patients with TBI.
Materials and Methods
In this comparative cross-sectional study, we included hospitalized patients with TBI who presented to our trauma center. They were categorized into two groups: 33 confirmed COVID-19 patients and 95 uninfected patients. All 33 COVID-19 patients were diagnosed before their hospitalization for TBI, with most confirmed through PCR testing. These patients were identified during the 19-month COVID-19 pandemic (commencing in March 2020 and culminating in September 2021). The patient’s clinical data were collected by reviewing their medical records, registered files in the hospital information system and the imaging modalities in the picture archiving and communication system.
We collected documented data based on a checklist including demographic information of patient’s age, gender, and underlying diseases, hypertension as blood pressure above 140/90 mm Hg, diabetes based on American Diabetes Association criteria, history of ischemic heart disease based on past medical history, other clinical information (smoking, mechanism of trauma, severity of brain injury, neurological defects and CT scan findings) and risk factors of intracranial complications (anticoagulant drug use, reduced level of consciousness and also type of treatment, suffering from Covid-19 and duration of hospitalization). There are two methods to estimate the intracerebral hemorrhage volume: ABC/2 and computer-assisted planimetric analysis. ABC/2 is a simple and reliable technique using A=maximum diameter of hemorrhage (in cm), B=width to A and C=the number of slices multiplied by slice thickness. This accurate method allows physicians to assess the intracerebral hemorrhage volume and predict patient outcomes in a short time.
Statistical analysis
Statistical analyses were done using IBM SPSS software, version 25.0 (SPSS, Inc., Chicago, IL, USA). Categorical variables were reported as frequencies and percentages, while continuous variables were summarized using means and standard deviations. Continuous variables were compared between COVID-19 and non-COVID-19 groups using the independent t test or Mann-Whitney U test. The categorical variables were analyzed using the chi-square or Fisher exact test. Univariate linear and logistic regression was used to investigate the relationship between COVID-19, demographic and clinical factors with ACHV, and mortality in TBI patients. All variables with a P<0.25 in the univariate models were entered into the multiple linear and logistic models. The significance level in all tests was set at P<0.05 and the tests were considered two domains.
Results
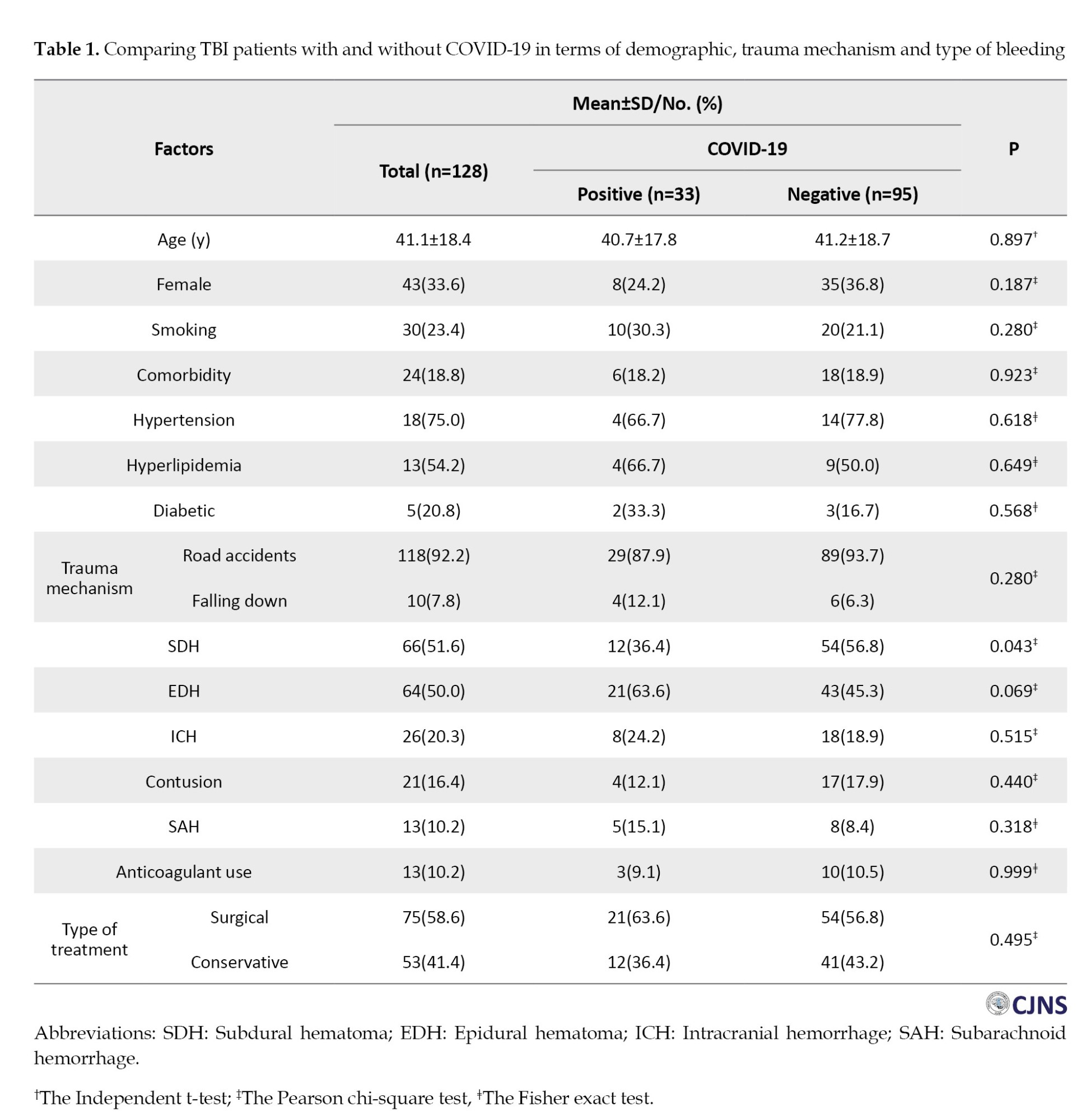
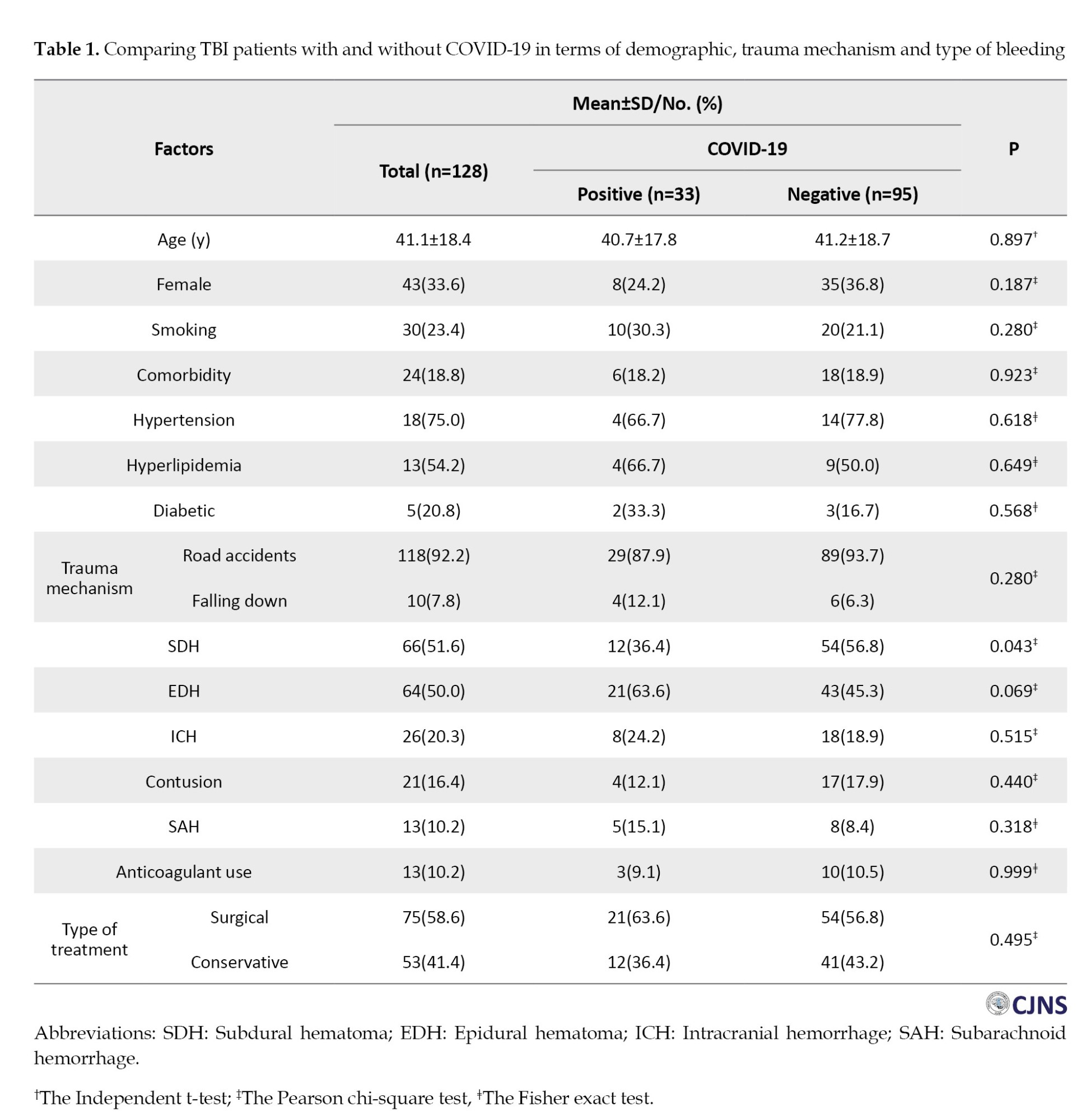
Demographic features, including age, gender, smoking status, and comorbidities, were evenly balanced between the two study groups (P>0.05). The reason for head trauma in most of the studied samples (92.2%) was road accidents. There was no significant statistical relationship between trauma mechanisms and COVID-19. The most common types of brain lesions were subdural hematoma (SDH) (51.6%), epidural hematoma (EDH) (50.0%), intracranial hemorrhage (ICH) (20.3%), contusion (16.4%) and subarachnoid hemorrhage (SAH) (10.2%). Among different types of brain lesions, SDH had a significant relationship with contracting COVID-19 in patients with TBI (P=0.043). The frequency of SDH lesions in people with COVID-19 was considerably lower than in people without COVID-19 (36.4% vs 56.8%). Among patients, 13(10.2%) were on anticoagulants, with no significant differences between the groups. Most patients underwent surgery; no significant differences were observed between the two groups (Table 1).
The mean Glasgow Coma Scale (GCS) of hospitalized patients with COVID-19 (8.1±3.3) was not significantly different from that of patients without COVID-19 (8.5±3.6) (P=0.528). Of 128 admitted patients, 66(51.6 %) had mild, 41(32.0 %) moderate and 21(16.4%) severe head injuries. There was no significant statistical difference between the two groups in this aspect. There was no statistically significant difference in the ACHV between the two groups (21.4±16.3 vs 21.3±18.3; P=0.758). Fifty-four patients (42.2%) died, with 15(45.4%) in the COVID-19 group and 39(41.1%) in the other. There was no statistically significant difference in this outcome between the two groups. Other clinical outcomes examined in both study groups showed no significant differences. The results are presented in Table 2.
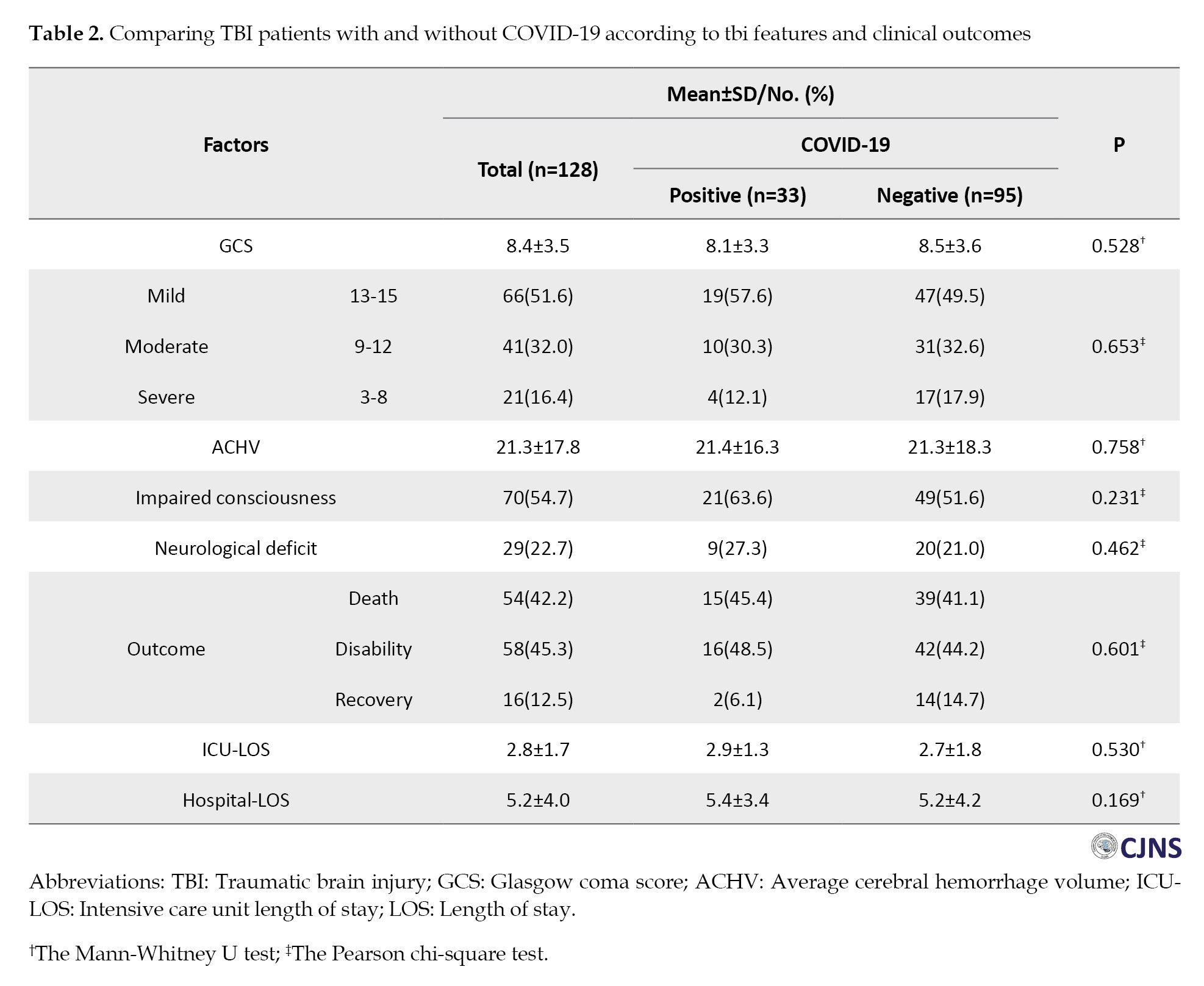
Table 3 shows no statistically significant difference in ACHV between COVID-19 and non-COVID-19, separated by smoking and anticoagulant use.
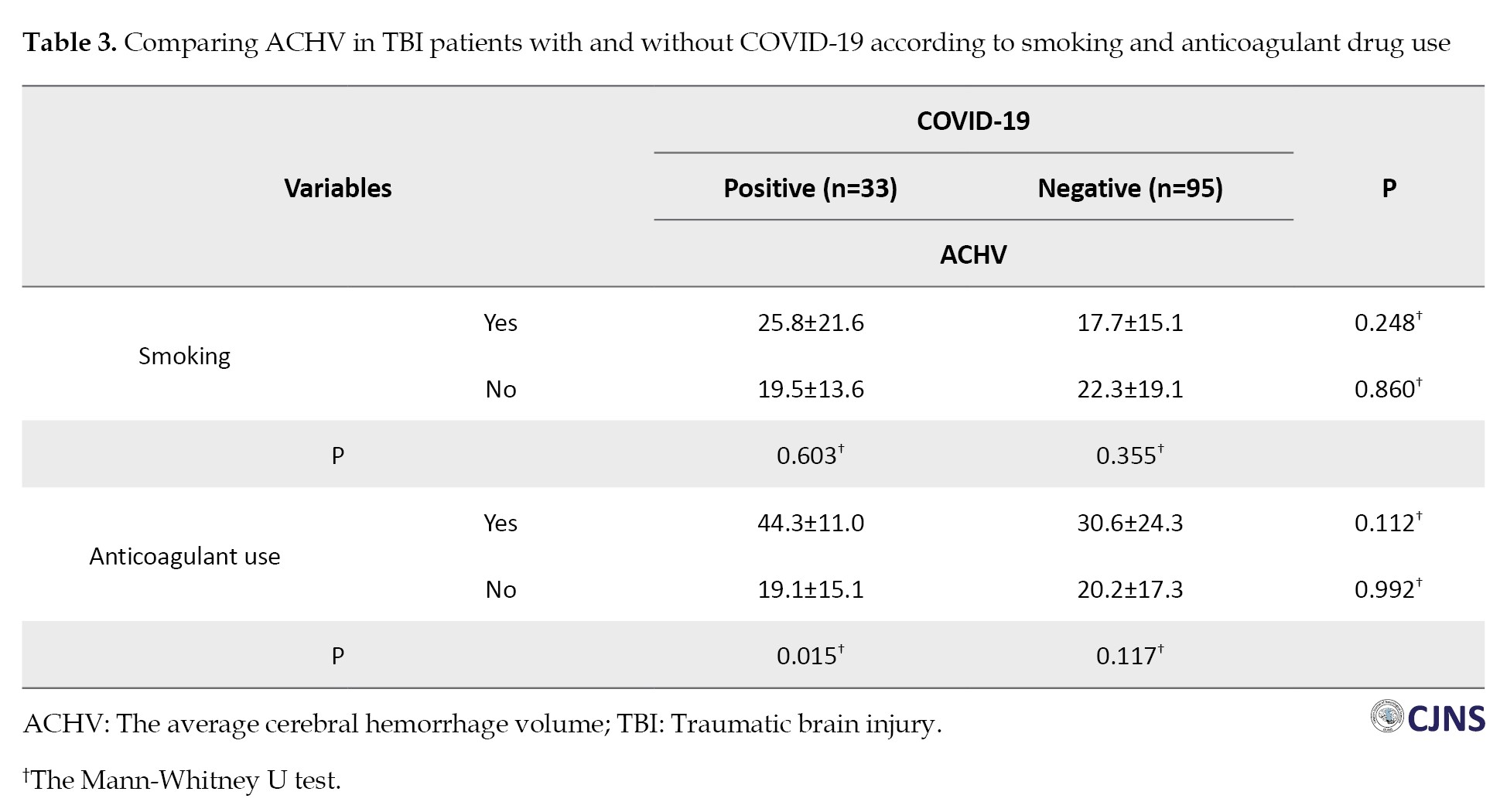
Only anticoagulant use was significantly associated with ACHV in COVID-19 patients. Among the COVID-19 patients, those who anticoagulant users experienced a higher ACHV than those who did not use medication (P=0.015).
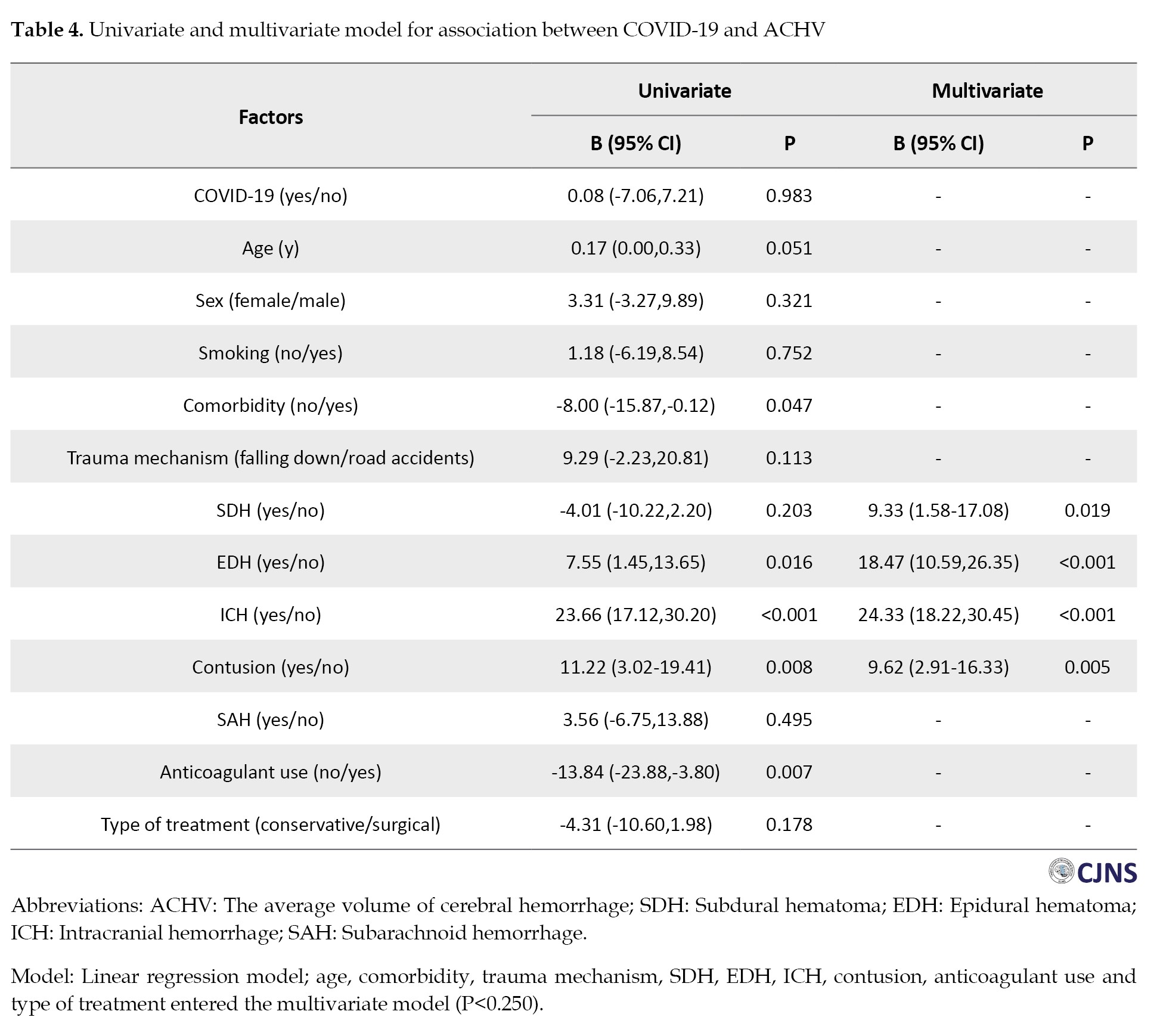
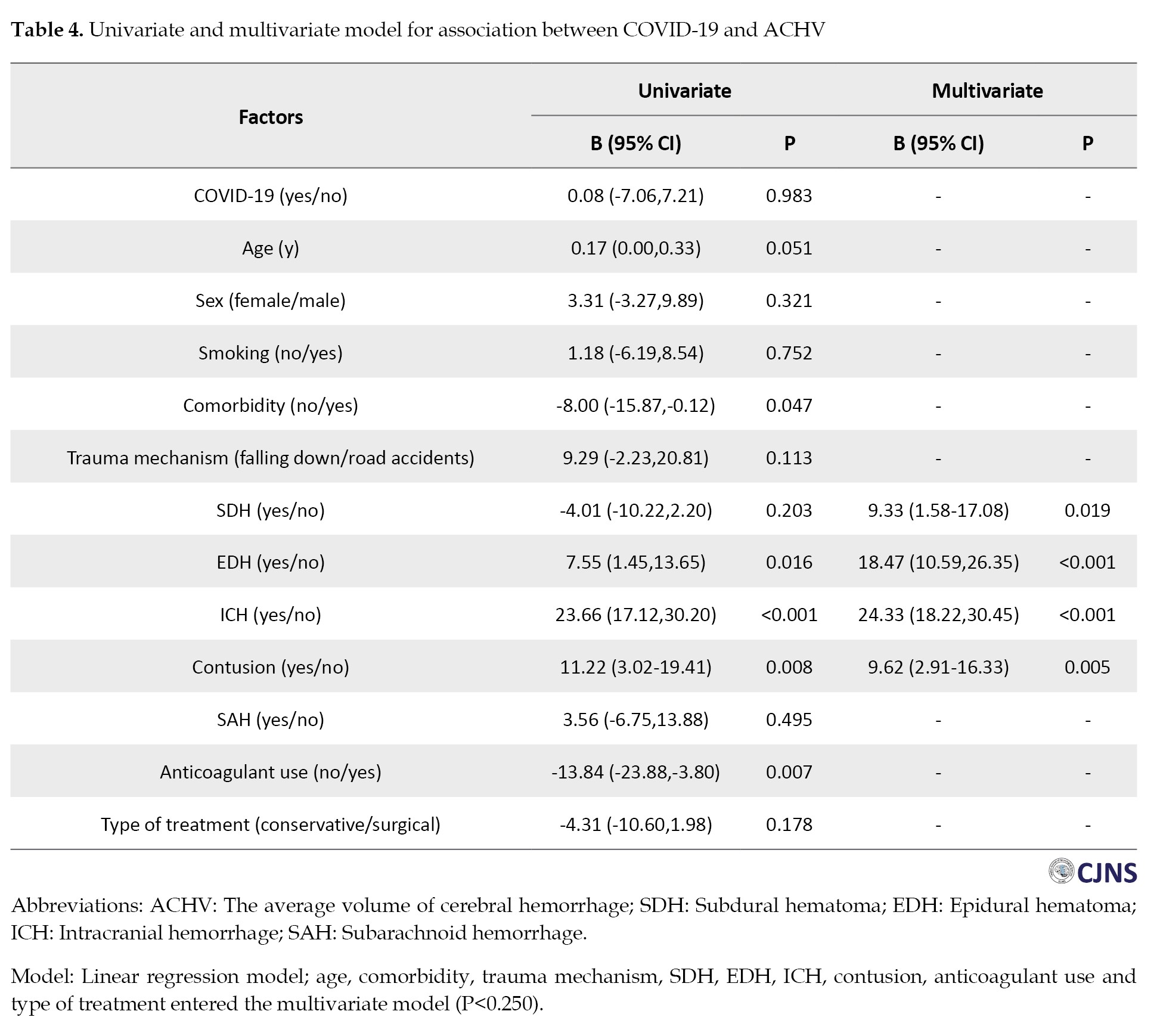
The univariate linear regression model showed no significant relationship between COVID-19 and ACHV (P=0.983). However, age, comorbidity, EDH, ICH, contusion, and anticoagulant use were all significantly related to ACHV. The multivariate linear regression model revealed that brain lesions, including SDH, EDH, ICH, and contusions, were significantly related to ACHV (Table 4).
The findings in Table 5 show that COVID-19 had no significant association with TBI patient mortality (P=0.695).
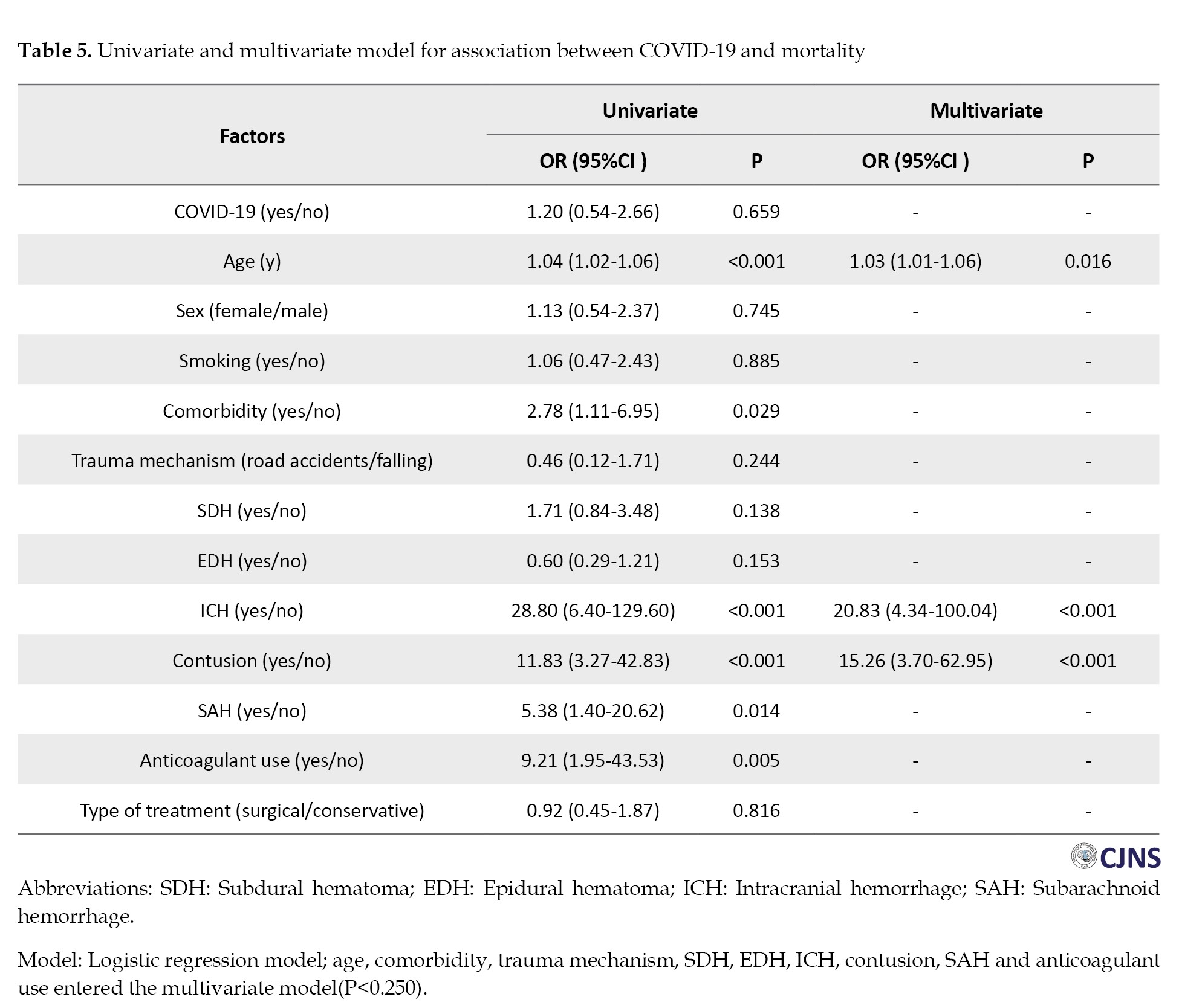
Age, comorbidity, ICH, contusion, SAH and anticoagulant use were all significantly related to mortality. Multivariate analysis indicated that older age, presence of ICH and contusions were significantly associated with mortality.
Discussion
Covid-19, a global pandemic, can affect several different systems in the body. Not only have there been reports of its effects on the hematological and neurological system [13, 14], but it also causes disorders in the function and self-regulation of cerebral vessels, followed by their rupture [16]. In this study, we examined the amount of bleeding and the clinical consequences between the two groups of with and without COVID-19 patients suffering from concussions and compared to check whether COVID-19 had a significant effect on the bleeding volume or their clinical outcome based on demographic characteristics.
Road accidents were the primary underlying phenomenon of trauma in our study, while in a similar study done by Lara-Reyna et al. in the later period of COVID-19, the major mechanism of head injury was reported to be falling. However, no significant correlation was discovered between patients’ clinical outcomes and COVID-19 infection in both groups [25].
Regarding the underlying disease, most subjects did not suffer from any underlying conditions. However, high blood pressure and hyperlipidemia were the most prevalent among the underlying diseases, but there was no difference between the two investigated groups.
There was no significant difference in smoking between the COVID-19 and non-COVID-19 groups. Another study also found no significant relationship between smoking and COVID-19 disease [26].
Also, no significant disparity was discovered in the average bleeding volume between the two mentioned groups.
The most prevalent type of brain lesion in our study was SDH, unlike other studies in which the largest subgroup caused by trauma was ICH [27]. Nevertheless, in our study, the frequency of SDH in the group with COVID-19 was noticeably lower than non-COVID-19.
The ACHV also had no significant difference between the two groups; in most patients, the bleeding volume was less than 20 mL. The hypothesis behind our study was that COVID-19 can increase the bleeding volume in the group with concussion injuries who suffer from COVID-19 due to its effect on hematological elements. However, there was no difference in bleeding in infected and non-infected patients. Nevertheless, among the group of COVID-19 patients, subjects who took anticoagulant medication experienced a higher average volume of bleeding than those who did not use medication. That outcome could result from a potential synergism formed between anticoagulant drugs and COVID-19 [4, 28, 29]. Since the effect of COVID-19 in reducing the platelet count and increasing PT and as leukopenia has been reported, it is probable that coupled with the use of anticoagulants, it can augment the platelets reduction and prolong PT, which leads to an increase in the frequency and volume of bleeding and has been witnessed in people who use anticoagulants such as aspirin. This point can strengthen the hypothesis of a synergistic effect of COVID-19 and the anticoagulant effect.
Several studies have revealed that patients with intracerebral bleeding risk factors are more prone to bleeding and its progression [4]. Among the mentioned risk factors are a high level of D-dimer, a low level of platelets, a high level of white blood cells, and an increase in PT [30]. Coagulation disorders increase the lesion size and the risk of progression after TBI, as the progression rate of intracerebral hemorrhage after TBI is commonly increased with coagulation disorders, and it has been suggested that higher levels of international normalized ratio and D-dimer and lower counts of platelets increase the size and intensifies the progression rate of the hemorrhage [4].
Conclusion
The study shows that TBI patients with COVID-19 on anticoagulants had higher ACHV levels than infected patients not on the therapy. However, among non-COVID patients, anticoagulants did not affect ACHV levels. This finding suggests that COVID-19 exacerbates coagulation abnormalities through an additive, synergistic effect, marking it as a key risk factor for worsening such conditions.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the Ethical Guidelines of the 2013 Declaration of Helsinki. The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.424).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian and Nooshin Zaresharifi; Methodology: Khatereh Asadi, Roghaye Zare and Mohammad Ali Yazdanipour; Investigation and resources: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian, and Nooshin Zaresharifi; Data collection: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian, Khatereh Asadi, and Masoud Shabani Chobe; Writing the original draft: Farnaz Mahdavi and Mohammad Ali Yazdanipour; Supervision: Sima Fallah-Arzpeima and Zoheir Reihanian; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge the assistance of the Neuroscience Research Center and Clinical Research Development Unit of Poursina Hospital.
References
Traumatic brain injury (TBI) is a leading cause of emergency department visits and a major contributor to mortality and morbidity worldwide [1, 2]. TBI is a significant socioeconomic issue that burdens healthcare systems and affects individuals’ lives [1-3]. The incidence of severe consequences, such as intracranial hemorrhages, is mainly associated with TBIs following road traffic accidents rather than other types of traumatic injuries [3]. In addition to the initial brain damage, some avoidable secondary processes, such as progressive hemorrhagic injury (PHI) following intracranial bleeding, can deteriorate the general condition [4]. Hence, risk factors related to PHI should be addressed [4]. Evidence of a direct association exists between PHI and several risk factors, including a high D-dimer level, thrombocytopenia, leukocytosis, and prolonged prothrombin time (PT) [1, 4, 5]. Therefore, it seems rational to accept that coagulation disorders may contribute to poor prognosis in patients with TBI. Moreover, there is a correlation between higher mortality rates after TBIs and comorbidities such as hematologic malignancies and coagulation disorders [4, 6-8].
Coronavirus disease 2019 (COVID-19) emerged as a new infectious disease outbreaking in late December 2019. The disease originated in China and rapidly spread globally [9]. Therefore, in March 2020, the World Health Organization (WHO) declared that the COVID-19 outbreak became a pandemic and a primary global concern [10].
COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), an RNA virus [11]. Due to the virus’s high mutation rate, many subtypes have emerged that can impact symptoms’ incidence and severity. SARS-CoV-2 can lead to high morbidity and mortality rates, which can simultaneously affect various body organs, including the respiratory, cardiovascular, gastrointestinal, central nervous and hematopoietic systems [11, 12]. Although initially manifesting as a respiratory tract infection, subsequent data noted that it should be considered a systemic disease [11]. COVID-19 can impact the hematopoietic system remarkably, often associated with a hypercoagulability state [11]. Main hematologic findings include lymphocytopenia, thrombocytopenia, elevated D-dimer, and prolonged PT [11]. Also, a high rate of arterial and venous thromboembolisms at the first 24 hours of admission is reported among several COVID-19 patients [13, 14].
Angiotensin-converting enzyme 2 (ACE2) is an essential component of the renin-angiotensin-aldosterone system, which plays a crucial role in maintaining homeostasis [15]. It is a pro-inflammatory agent and vasoconstrictor, expressed in almost all organs [16]. ACE2 in lung pneumocytes type 2 can act as a receptor for SARS-CoV-2 [17]. This attachment inhibits ACE2 and facilitates virus entry into cells, followed by boosting cell infection [15, 16]. ACE2 receptors are also present in cerebrovascular endothelial cells, which regulate various brain functions, including autoregulation of cerebral perfusion [15]. Thus, COVID-19 can disrupt autoregulation in CNS and peripheral nervous system [16, 18-23]. Several researchers investigated the most common cranial hemorrhagic patterns both before and after the COVID-19 era, consisting of SDH, SAH and brain contusions, together with falling, which is the most frequent head trauma mechanism [13, 24].
Considering the effects of COVID-19 on various organs, especially the CNS and hematologic system, we aimed to assess the impact of COVID-19 infection on mortality and the average cerebral hemorrhage volume (ACHV) in patients with TBI.
Materials and Methods
In this comparative cross-sectional study, we included hospitalized patients with TBI who presented to our trauma center. They were categorized into two groups: 33 confirmed COVID-19 patients and 95 uninfected patients. All 33 COVID-19 patients were diagnosed before their hospitalization for TBI, with most confirmed through PCR testing. These patients were identified during the 19-month COVID-19 pandemic (commencing in March 2020 and culminating in September 2021). The patient’s clinical data were collected by reviewing their medical records, registered files in the hospital information system and the imaging modalities in the picture archiving and communication system.
We collected documented data based on a checklist including demographic information of patient’s age, gender, and underlying diseases, hypertension as blood pressure above 140/90 mm Hg, diabetes based on American Diabetes Association criteria, history of ischemic heart disease based on past medical history, other clinical information (smoking, mechanism of trauma, severity of brain injury, neurological defects and CT scan findings) and risk factors of intracranial complications (anticoagulant drug use, reduced level of consciousness and also type of treatment, suffering from Covid-19 and duration of hospitalization). There are two methods to estimate the intracerebral hemorrhage volume: ABC/2 and computer-assisted planimetric analysis. ABC/2 is a simple and reliable technique using A=maximum diameter of hemorrhage (in cm), B=width to A and C=the number of slices multiplied by slice thickness. This accurate method allows physicians to assess the intracerebral hemorrhage volume and predict patient outcomes in a short time.
Statistical analysis
Statistical analyses were done using IBM SPSS software, version 25.0 (SPSS, Inc., Chicago, IL, USA). Categorical variables were reported as frequencies and percentages, while continuous variables were summarized using means and standard deviations. Continuous variables were compared between COVID-19 and non-COVID-19 groups using the independent t test or Mann-Whitney U test. The categorical variables were analyzed using the chi-square or Fisher exact test. Univariate linear and logistic regression was used to investigate the relationship between COVID-19, demographic and clinical factors with ACHV, and mortality in TBI patients. All variables with a P<0.25 in the univariate models were entered into the multiple linear and logistic models. The significance level in all tests was set at P<0.05 and the tests were considered two domains.
Results
Demographic features, including age, gender, smoking status, and comorbidities, were evenly balanced between the two study groups (P>0.05). The reason for head trauma in most of the studied samples (92.2%) was road accidents. There was no significant statistical relationship between trauma mechanisms and COVID-19. The most common types of brain lesions were subdural hematoma (SDH) (51.6%), epidural hematoma (EDH) (50.0%), intracranial hemorrhage (ICH) (20.3%), contusion (16.4%) and subarachnoid hemorrhage (SAH) (10.2%). Among different types of brain lesions, SDH had a significant relationship with contracting COVID-19 in patients with TBI (P=0.043). The frequency of SDH lesions in people with COVID-19 was considerably lower than in people without COVID-19 (36.4% vs 56.8%). Among patients, 13(10.2%) were on anticoagulants, with no significant differences between the groups. Most patients underwent surgery; no significant differences were observed between the two groups (Table 1).
The mean Glasgow Coma Scale (GCS) of hospitalized patients with COVID-19 (8.1±3.3) was not significantly different from that of patients without COVID-19 (8.5±3.6) (P=0.528). Of 128 admitted patients, 66(51.6 %) had mild, 41(32.0 %) moderate and 21(16.4%) severe head injuries. There was no significant statistical difference between the two groups in this aspect. There was no statistically significant difference in the ACHV between the two groups (21.4±16.3 vs 21.3±18.3; P=0.758). Fifty-four patients (42.2%) died, with 15(45.4%) in the COVID-19 group and 39(41.1%) in the other. There was no statistically significant difference in this outcome between the two groups. Other clinical outcomes examined in both study groups showed no significant differences. The results are presented in Table 2.
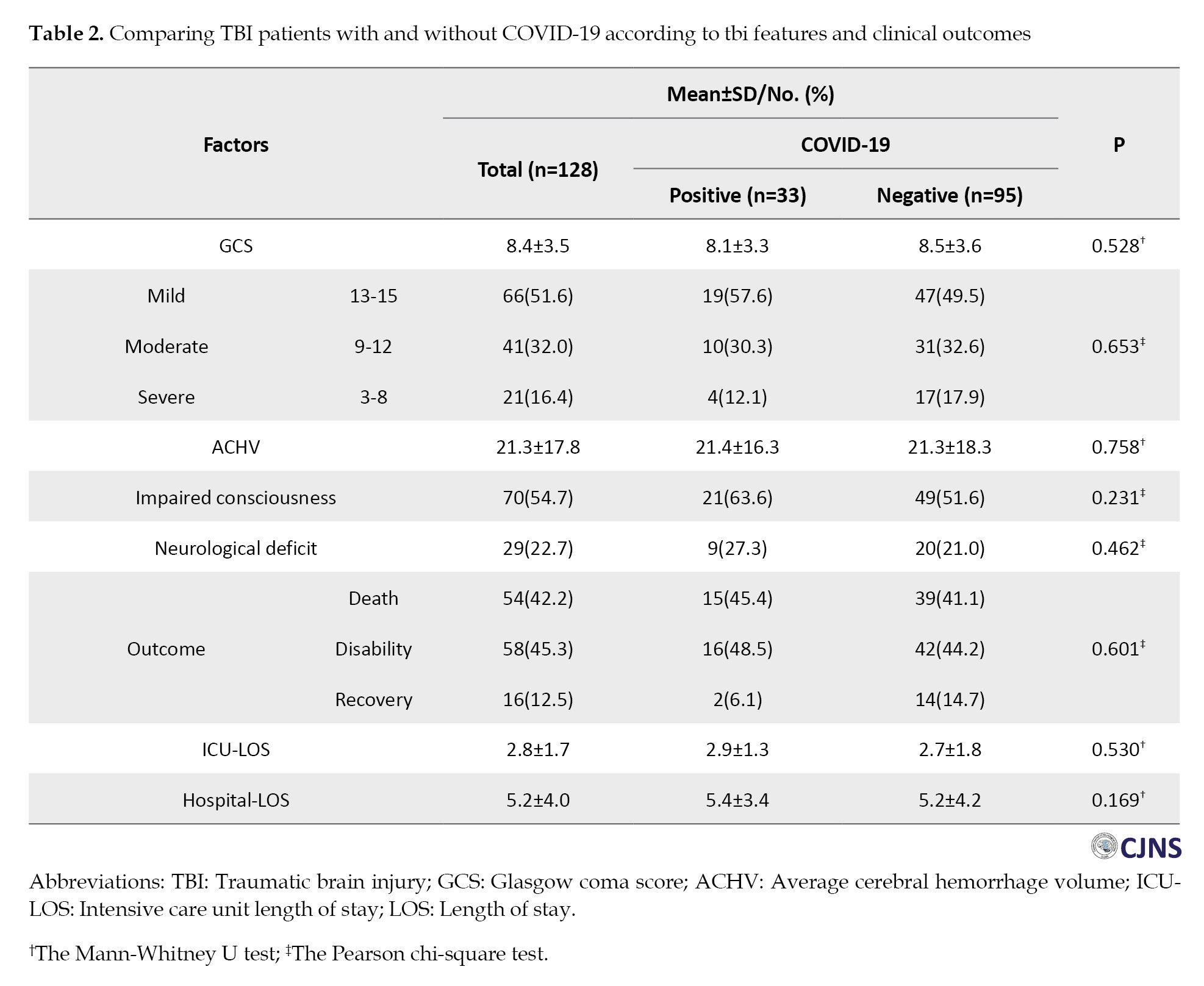
Table 3 shows no statistically significant difference in ACHV between COVID-19 and non-COVID-19, separated by smoking and anticoagulant use.
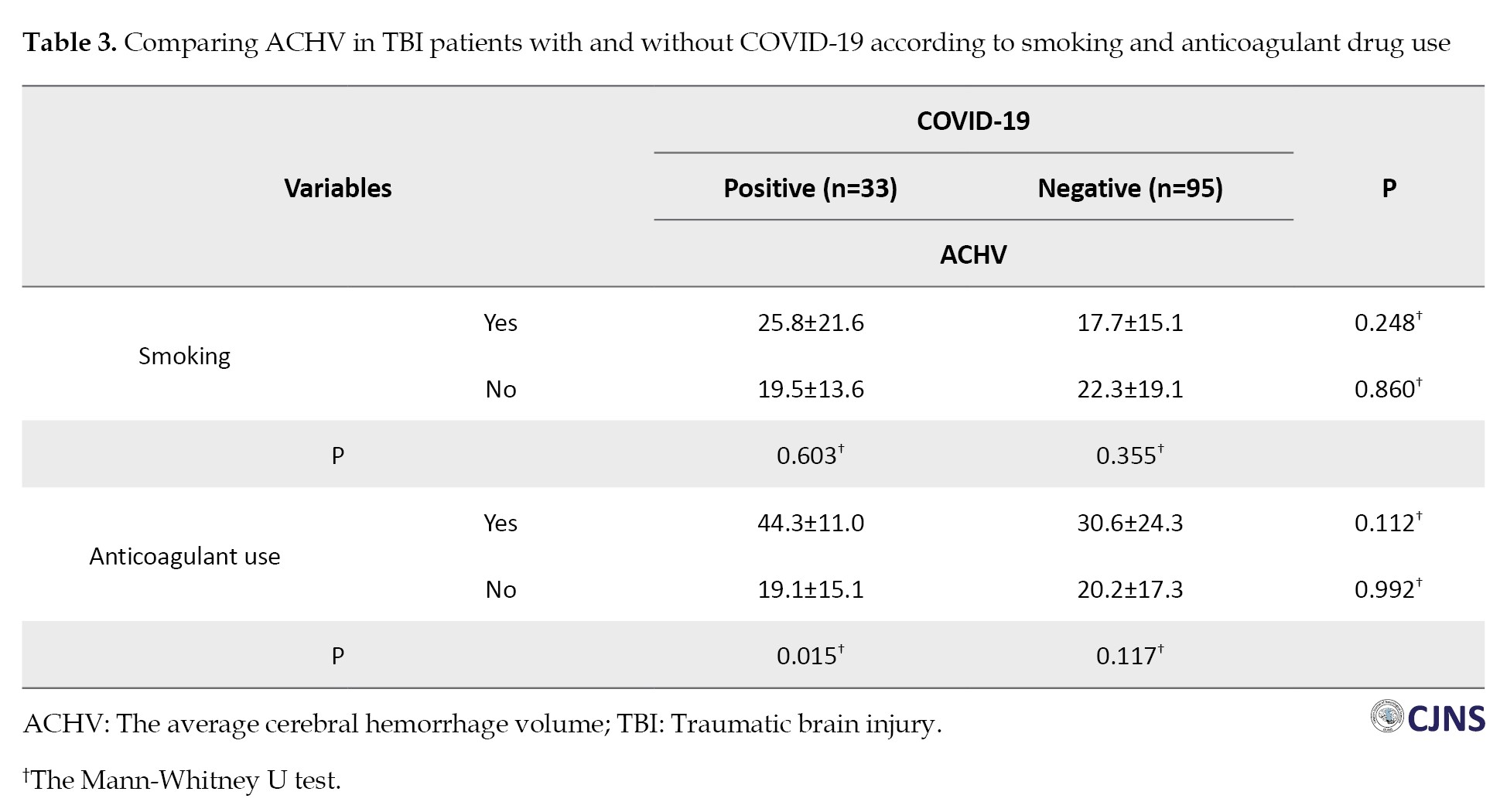
Only anticoagulant use was significantly associated with ACHV in COVID-19 patients. Among the COVID-19 patients, those who anticoagulant users experienced a higher ACHV than those who did not use medication (P=0.015).
The univariate linear regression model showed no significant relationship between COVID-19 and ACHV (P=0.983). However, age, comorbidity, EDH, ICH, contusion, and anticoagulant use were all significantly related to ACHV. The multivariate linear regression model revealed that brain lesions, including SDH, EDH, ICH, and contusions, were significantly related to ACHV (Table 4).
The findings in Table 5 show that COVID-19 had no significant association with TBI patient mortality (P=0.695).
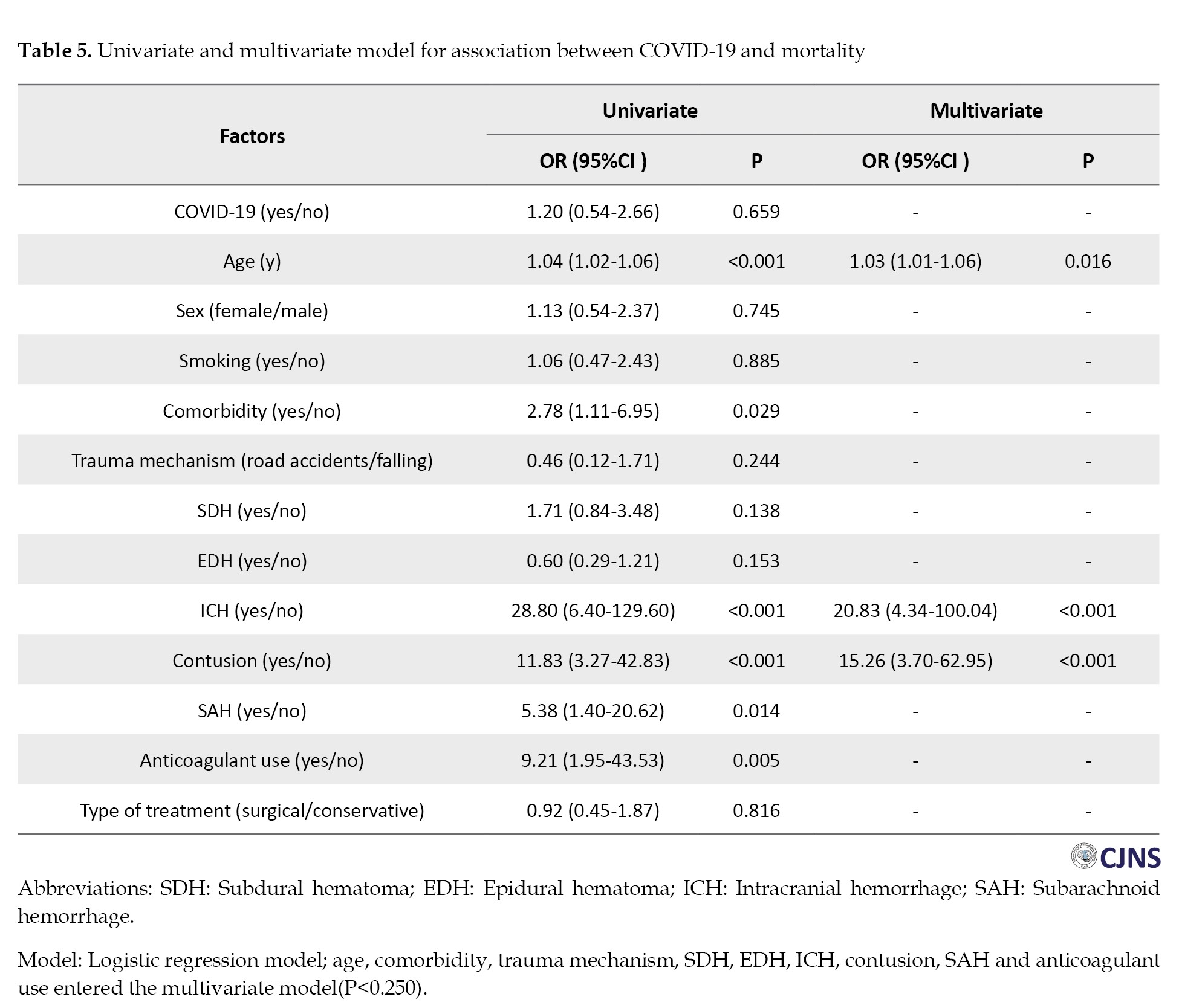
Age, comorbidity, ICH, contusion, SAH and anticoagulant use were all significantly related to mortality. Multivariate analysis indicated that older age, presence of ICH and contusions were significantly associated with mortality.
Discussion
Covid-19, a global pandemic, can affect several different systems in the body. Not only have there been reports of its effects on the hematological and neurological system [13, 14], but it also causes disorders in the function and self-regulation of cerebral vessels, followed by their rupture [16]. In this study, we examined the amount of bleeding and the clinical consequences between the two groups of with and without COVID-19 patients suffering from concussions and compared to check whether COVID-19 had a significant effect on the bleeding volume or their clinical outcome based on demographic characteristics.
Road accidents were the primary underlying phenomenon of trauma in our study, while in a similar study done by Lara-Reyna et al. in the later period of COVID-19, the major mechanism of head injury was reported to be falling. However, no significant correlation was discovered between patients’ clinical outcomes and COVID-19 infection in both groups [25].
Regarding the underlying disease, most subjects did not suffer from any underlying conditions. However, high blood pressure and hyperlipidemia were the most prevalent among the underlying diseases, but there was no difference between the two investigated groups.
There was no significant difference in smoking between the COVID-19 and non-COVID-19 groups. Another study also found no significant relationship between smoking and COVID-19 disease [26].
Also, no significant disparity was discovered in the average bleeding volume between the two mentioned groups.
The most prevalent type of brain lesion in our study was SDH, unlike other studies in which the largest subgroup caused by trauma was ICH [27]. Nevertheless, in our study, the frequency of SDH in the group with COVID-19 was noticeably lower than non-COVID-19.
The ACHV also had no significant difference between the two groups; in most patients, the bleeding volume was less than 20 mL. The hypothesis behind our study was that COVID-19 can increase the bleeding volume in the group with concussion injuries who suffer from COVID-19 due to its effect on hematological elements. However, there was no difference in bleeding in infected and non-infected patients. Nevertheless, among the group of COVID-19 patients, subjects who took anticoagulant medication experienced a higher average volume of bleeding than those who did not use medication. That outcome could result from a potential synergism formed between anticoagulant drugs and COVID-19 [4, 28, 29]. Since the effect of COVID-19 in reducing the platelet count and increasing PT and as leukopenia has been reported, it is probable that coupled with the use of anticoagulants, it can augment the platelets reduction and prolong PT, which leads to an increase in the frequency and volume of bleeding and has been witnessed in people who use anticoagulants such as aspirin. This point can strengthen the hypothesis of a synergistic effect of COVID-19 and the anticoagulant effect.
Several studies have revealed that patients with intracerebral bleeding risk factors are more prone to bleeding and its progression [4]. Among the mentioned risk factors are a high level of D-dimer, a low level of platelets, a high level of white blood cells, and an increase in PT [30]. Coagulation disorders increase the lesion size and the risk of progression after TBI, as the progression rate of intracerebral hemorrhage after TBI is commonly increased with coagulation disorders, and it has been suggested that higher levels of international normalized ratio and D-dimer and lower counts of platelets increase the size and intensifies the progression rate of the hemorrhage [4].
Conclusion
The study shows that TBI patients with COVID-19 on anticoagulants had higher ACHV levels than infected patients not on the therapy. However, among non-COVID patients, anticoagulants did not affect ACHV levels. This finding suggests that COVID-19 exacerbates coagulation abnormalities through an additive, synergistic effect, marking it as a key risk factor for worsening such conditions.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the Ethical Guidelines of the 2013 Declaration of Helsinki. The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.424).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian and Nooshin Zaresharifi; Methodology: Khatereh Asadi, Roghaye Zare and Mohammad Ali Yazdanipour; Investigation and resources: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian, and Nooshin Zaresharifi; Data collection: Farnaz Mahdavi, Sima Fallah-Arzpeima, Zoheir Reihanian, Khatereh Asadi, and Masoud Shabani Chobe; Writing the original draft: Farnaz Mahdavi and Mohammad Ali Yazdanipour; Supervision: Sima Fallah-Arzpeima and Zoheir Reihanian; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors acknowledge the assistance of the Neuroscience Research Center and Clinical Research Development Unit of Poursina Hospital.
References
- Santing JAL, van den Brand CL, Jellema K. Traumatic brain injury during the SARS-CoV-2 pandemic. Neurotrauma Rep. 2020; 1(1):5-7. [DOI:10.1089/neur.2020.0001] [PMID]
- Kim JJ, Gean AD. Imaging for the diagnosis and management of traumatic brain injury. Neurotherapeutics. 2011; 8(1):39-53. [DOI:10.1007/s13311-010-0003-3] [PMID]
- Finnie JW, Blumbergs PC. Traumatic brain injury. Vet Pathol. 2002; 39(6):679-89. [DOI:10.1354/vp.39-6-679] [PMID]
- Zhang D, Gong S, Jin H, Wang J, Sheng P, Zou W, et al Coagulation parameters and risk of progressive hemorrhagic injury after traumatic brain injury: A systematic review and meta-analysis. Biomed Res Int. 2015 ;2015:261825. [DOI:10.1155/2015/261825] [PMID]
- Aghayari Sheikh Neshin S, Basirjafari S, Saberi A, Shahhosseini B, Zarei M. Liver abnormality may develop cerebral vein thrombosis in COVID-19. J Neurol Sci. 2020; 417:117076. [DOI:10.1016/j.jns.2020.117076] [PMID]
- Bonville DJ, Ata A, Jahraus CB, Arnold-Lloyd T, Salem L, Rosati C, et al. Impact of preinjury warfarin and antiplatelet agents on outcomes of trauma patients. Surgery. 2011; 150(4):861-8. [DOI:10.1016/j.surg.2011.07.070] [PMID]
- Gupta G, Wadhwa C, Garg R, Dhaiya RS, Kaushal RK. Impact of coagulation profile on outcome of head injury. J Clin Diagn Res. 2016; 10(1):PC04-6. [DOI:10.7860/JCDR/2016/14638.7029] [PMID]
- Epstein DS, Mitra B, O'Reilly G, Rosenfeld JV, Cameron PA. Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: A systematic review and meta-analysis. Injury. 2014; 45(5):819-24. [DOI:10.1016/j.injury.2014.01.011] [PMID]
- Shi Y, Wang G, Cai XP, Deng JW, Zheng L, Zhu HH, et al. An overview of COVID-19. J Zhejiang Univ Sci B. 2020; 21(5):343-60. [DOI:10.1631/jzus.B2000083] [PMID]
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020; 91(1):157-60. [DOI: 10.23750/abm.v91i1.9397] [PMID]
- Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020; 95(7):834-47. [DOI:10.1002/ajh.25829] [PMID]
- Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020; 45(8):100618. [DOI:10.1016/j.cpcardiol.2020.100618] [PMID]
- Joob B, Wiwanitkit V. Hemorrhagic problem among the patients with COVID-19: Clinical summary of 41 thai infected patients. Clin Appl Thromb Hemost. 2020; 26:1076029620918308. [DOI:10.1177/1076029620918308] [PMID]
- Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020; 191:9-14. [DOI:10.1016/j.thromres.2020.04.024] [PMID]
- Bhalla V, Blish CA, South AM. A historical perspective on ACE2 in the COVID-19 era. J Hum Hypertens. 2021; 35(10):935-9. [DOI:10.1038/s41371-020-00459-3] [PMID]
- Sharifi-Razavi A, Karimi N, Rouhani N. COVID-19 and intracerebral haemorrhage: Causative or coincidental? New Microbes New Infect. 2020; 35:100669 [DOI:10.1016/j.nmni.2020.100669] [PMID]
- Agbuduwe C, Basu S. Haematological manifestations of COVID-19: From cytopenia to coagulopathy. Eur J Haematol. 2020; 105(5):540-6. [DOI:10.1111/ejh.13491] [PMID]
- Moaddabi Y, Farhang N, Mousavi AF, Neshin SAS, Lomer NB, Saberi A. Electrocardiogram and echocardiogram patterns among ischemic stroke patients during COVID-19 pandemic. Rom J Neurol. 2023; 22(4):286 [DOI:10.37897/RJN.2023.4.5]
- Atefi A, Ghanaatpisheh A, Ghasemi A, Haghshenas H, Eyvani K, Bakhshi A, et al. Correction: Meningitis after COVID-19 vaccination, A systematic review of case reports and case series. BMC Infect Dis. 2024; 24(1):1244. [DOI:10.1186/s12879-024-10087-8] [PMID]
- Saberi A, Ghayeghran A, Hatamian H, Hosseini-Nejad M, Bakhshayesh Eghbali B. COVID-19-associated myelitis, para/post infectious or infectious myelitis: A case report from the north of Iran. Caspian J Neurol Sci. 2020; 6(2):132-8 [DOI:10.32598/CJNS.6.21.1]
- Bakhshayesh Eghbali B, Saberi A, Jalali Emam SZ, Fallah-Arzpayma S, Zare R, Ramezani S, et al. Changes in seizure frequency and characteristics during COVID-19 pandemic: A hospital-based study. Caspian J Neurol Sci. 2023; 9(3):154-61 [DOI:10.32598/CJNS.9.34.425.1]
- Ghayeghran A, Ghahramani E, Saberi A, Hatamian H, Homaie Rad E, Ghorbani Shirkouhi S, et al. COVID-19 infection and seropositivity in multiple sclerosis patients in Guilan in 2021. Caspian J Neurol Sci. 2023; 9(1):39-49. [DOI:10.32598/CJNS.9.32.8.29]
- Besharati A, Saberi A, Ghorbani Shirkouhi S, Ashraf A, Hatamian H, Eslami Kenarsari H, et al. Guillain-barré syndrome during the COVID-19 pandemic and pre-pandemic periods. Caspian J Neurol Sci. 2022; 8(1):33-8 [DOI:10.32598/CJNS.8.28.213.2]
- Goyal N, Swain SK, Gupta K, Chaturvedi J, Arora RK, Sharma SK. "Locked up inside home" - Head injury patterns during coronavirus disease of 2019 pandemic. Surg Neurol Int. 2020; 11:395. [DOI:10.25259/SNI_675_2020] [PMID]
- Lara-Reyna J, Yaeger KA, Rossitto CP, Camara D, Wedderburn R, Ghatan S, et al. Staying home"-early changes in patterns of neurotrauma in New York city during the COVID-19 pandemic. World Neurosurg. 2020; 143:e344-50. [DOI:10.1016/j.wneu.2020.07.155] [PMID]
- Gallus S, Lugo A, Gorini G. No double-edged sword and no doubt about the relation between smoking and COVID-19 severity. Eur J Intern Med. 2020; 77:33-5. [DOI:10.1016/j.ejim.2020.06.014] [PMID]
- Shin SS, Marsh EB, Ali H, Nyquist PA, Hanley DF, Ziai WC. Comparison of traumatic intracranial hemorrhage expansion and outcomes among patients on direct oral anticoagulants versus vitamin k antagonists. Neurocrit Care. 2020; 32(2):407-18. [DOI:10.1007/s12028-019-00898-y] [PMID]
- Khalili H, Derakhshan N, Niakan A, Ghaffarpasand F, Salehi M, Eshraghian H, et al. Effects of oral glibenclamide on brain contusion volume and functional outcome of patients with moderate and severe traumatic brain injuries: A randomized double-blind placebo-controlled clinical trial. World Neurosurg. 2017; 101:130-6. [DOI:10.1016/j.wneu.2017.01.103] [PMID]
- Huttner HB, Steiner T, Hartmann M, Köhrmann M, Juettler E, Mueller S, et al. Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke. 2006; 37(2):404-8. [DOI:10.1161/01.STR.0000198806.67472.5c] [PMID]
- Simadibrata DM, Lubis AM. D-dimer levels on admission and all-cause mortality risk in COVID-19 patients: A meta-analysis. Epidemiol Infect. 2020; 148:e202. [DOI:10.1017/S0950268820002022] [PMID]
Type of Study: Research |
Subject:
General
Received: 2024/06/19 | Accepted: 2024/09/26 | Published: 2025/01/1
Received: 2024/06/19 | Accepted: 2024/09/26 | Published: 2025/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |