Tue, Dec 30, 2025
Volume 11, Issue 1 (Winter 2025)
Caspian J Neurol Sci 2025, 11(1): 67-76 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bakhshayesh Eghbali B, Hosseini-Nejad M, Saadat S, Babaee M, Eyvani K, Kohandel K et al . The Role of Sensory Processing Sensitivity and Self-management on Quality of Life in Multiple Sclerosis. Caspian J Neurol Sci 2025; 11 (1) :67-76
URL: http://cjns.gums.ac.ir/article-1-766-en.html
URL: http://cjns.gums.ac.ir/article-1-766-en.html
Babak Bakhshayesh Eghbali1 

 , Mozaffar Hosseini-Nejad *2
, Mozaffar Hosseini-Nejad *2 

 , Sajjad Saadat3
, Sajjad Saadat3 

 , Masoome Babaee3
, Masoome Babaee3 
 , Kimia Eyvani3
, Kimia Eyvani3 
 , Kosar Kohandel4
, Kosar Kohandel4 
 , Masoud Shabani Chobe3
, Masoud Shabani Chobe3 



 , Mozaffar Hosseini-Nejad *2
, Mozaffar Hosseini-Nejad *2 

 , Sajjad Saadat3
, Sajjad Saadat3 

 , Masoome Babaee3
, Masoome Babaee3 
 , Kimia Eyvani3
, Kimia Eyvani3 
 , Kosar Kohandel4
, Kosar Kohandel4 
 , Masoud Shabani Chobe3
, Masoud Shabani Chobe3 

1- Department of Neurology, Neuroscience Research Center, Trauma Institute, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Neurology, Neuroscience Research Center, Trauma Institute, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,hosseininezhadm@gmail.com
3- Trauma Institute, Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
4- Neuroscience Institute, Multiple Sclerosis Researcher Center, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Neurology, Neuroscience Research Center, Trauma Institute, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
3- Trauma Institute, Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
4- Neuroscience Institute, Multiple Sclerosis Researcher Center, Tehran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1347 kb]
(480 Downloads)
| Abstract (HTML) (818 Views)
Full-Text: (451 Views)
Introduction
Multiple sclerosis (MS) is a central nervous system (CNS) disorder with motor, sensory, cognitive and neuropsychiatric symptoms [1]. It is progressive, chronic and usually starts between the ages of 20 and 40. It is the second leading cause of non-traumatic disability in young people [2]. The prevalence and incidence of MS are rising in developing and developed countries. According to the reports, more than 400000 people in North America and about 2.5 million people worldwide have been affected by this disease. It is estimated that the prevalence of MS in Iran is 15-20 per 100000 population. On average, 5000 newly patients are diagnosed with this disease in Iran every year [2]. Although the exact cause of MS is unknown, some studies suggest that mitochondrial dysfunction, many genes, and environmental factors, such as exposure to ultraviolet B radiation, Epstein-Barr virus (EBV) infection, obesity and smoking, can affect this disease [3-7]. The most common type of this disease is relapsing-remitting MS (85-90%), and the majority of MS treatments are also focused on this type. It is noticeable that a small proportion of patients (10%) have primary progressive MS, and the treatment options for this condition are limited [8, 9]. MS compromises health-related quality of life (HRQOL). It is defined as the functional effect of a disease and its therapeutic outcome on the patient, as perceived by the patient [10].
Depression is known as the most important factor affecting the quality of life of Iranian MS patients [11]. The quality of life emphasizes various aspects of life, such as physical, emotional, cognitive and social [12, 13]. The main goal of treatment for chronic diseases such as MS is to optimize the patient’s quality of life [14]. In addition, identifying HRQOL factors can help maximize well-being and quality of life in MS patients. Physical and cognitive impairments, fatigue, comorbidities and emotional symptoms can predict HRQOL in people with MS [15-17]. Sensory processing is also another factor that may predict HRQOL in MS patients [18]. Sensory processing predicts how to respond to sensory information, including two components: neural threshold and self-regulation [19]. New evidence shows that the processing of sensory information in every person occurs in different ways, meaning that some persons are more sensitive to sensory information than others [20]. Neural threshold refers to the detection value of sensory stimuli, which ranges from hyposensitivity to hypersensitivity [21]. Self-regulation includes active and passive behaviors. Active strategies are responsible for dealing with available sensory information based on a person’s neural threshold, while passive strategies are not. For example, people with active hypersensitivity can try to minimize additional sensory input by controlling the environment [22].
Much evidence shows that people with self-regulation (those who have a deep understanding of their own emotions, can manage them effectively, and comprehend the emotions of others) are more successful and efficient in all areas of life. Emotion management includes monitoring flow, evaluating, and changing emotional experiences [20]. On the other hand, learning self-management by patients with chronic diseases is an important component of participation in their treatment [21]. Self-management is an active process of coping with illness through adherence to treatment and medication, participation in medical decisions, self-care, and maintaining social relationships and emotional balance [19]. Another definition of self-management is learning and participating in the skills necessary for an active life and a satisfactory mental state in living with a chronic disease [23].
Among patients with chronic disease, self-management enhances the quality of life, diminishing symptoms and treatment expenses [24]. Additional research suggests that self-management correlates with a broad spectrum of beneficial outcomes in the spheres of health and rehabilitation [25], such as improved self-regulation of disease symptoms [26], decreased rates of hospitalization [27] and alleviation of pain and anxiety [28]. Implementing self-management strategies that involve a more profound perception of the disease, acquiring relevant knowledge about appropriate dietary and nutritional guidelines and enhancing patient education and skills can significantly contribute to health maintenance and mitigating disease-related side effects [29].
Increasing self-management behaviors seems suitable for people with MS [21, 30-32]. This study investigates the association between HRQOL based on sensory processing sensitivity (SPS) and self-management in MS patients. Conducting this study and its results may provide a suitable solution for performing practical interventions and improving the quality of life in MS patients.
Materials and Methods
This cross-sectional-analytical study was conducted on MS patients registered in the nationwide MS registry of Iran (NMSRI), Guilan Province, from March 2020 to March 2021. The size of the studied population was 320 MS patients with relapsing-remitting MS (RRMS) type. The inclusion criteria were as follows: Patients diagnosed with MS by a neurologist based on revised McDonald criteria 2017 [33], aged between 20 and 55 years, RRMS type and their expanded disability status scale (EDSS) is <7. The exclusion criteria were as follows: Having other autoimmune diseases of the CNS or progressive MS (primary and secondary). Data were collected by three standard questionnaires and a general demographic information checklist. For this purpose, the first step was to upload the questionnaire and informed consent on the Porsline website. Then, a list of all active registered patients in NMSRI, Guilan, was prepared, and the survey link (completion guide, informed consent form, and questionnaire) was sent to them by a simple random method.
Study tools
MS self-management scale-revised (MSSM-R)
This MSSM-R includes 24 items in 5 subscales: Communication with health care providers, treatment adherence/coping with barriers, social/family support, information and knowledge about MS and health maintenance behavior. The scoring method of the questionnaire was based on a 5-point Likert scale (1=completely disagree, 2=somewhat disagree, 3=neither agree nor disagree, 4=somewhat agree, 5=completely agree). The higher the individual’s score, the higher the level of self-management is. The range of changes was between 24 and 120 [34]. This scale was translated into Farsi, and its psychometric properties were calculated by Saadat et al. The results showed that this scale has acceptable face and content validity. The results of confirmatory factor analysis showed that 24 items of the questionnaire have acceptable factor loadings in 5 subscales [35].
36-Item short form survey
The 36-item short-form survey (SF-36) or questionnaire has 36 items that evaluate 8 different areas of health: physical performance, role limitations due to physical health status and emotional problems, energy and vitality, emotional health, social performance, pain, and general health. The lowest score in this questionnaire is zero, and the highest is 100. A lower score means a lower quality of life; The closer the score is to 100, the higher the quality of life. In Montazeri et al.’s study, the Persian version of SF-36 subscales had standard reliability coefficients (0.77 to 0.9). So, it is a standard tool to measure HRQOL with required reliability and validity [36].
SPS questionnaire (SPSQ)
The SPSQ consists of 27 self-report questions that measure psychological reactivity to environmental stimuli. It consists of 3 subscales: Ease of stimulation, aesthetic sensitivity, and low sensory threshold and is answered based on a 7-point Likert scale so that the completely disagree option is given a score of 1 and the agree option is given a score of 7. The range of changes in this tool is between 27 and 189. Higher scores indicate better SPS; the validity and reliability of this questionnaire have been confirmed in an Iranian sample and its Cronbach alpha has been reported to be 0.78 [11].
Statistical analysis
Data analysis was performed in SPSS software, version 24. The data obtained were analyzed by the Independent t-test, one-way analysis of variance, the Pearson correlation coefficient and multiple linear regression. Also, a significance level of 0.05 was considered in this study.
Results
A total of 320 patients participated in this study in 2020. Individual characteristics of patients are given in Table 1.
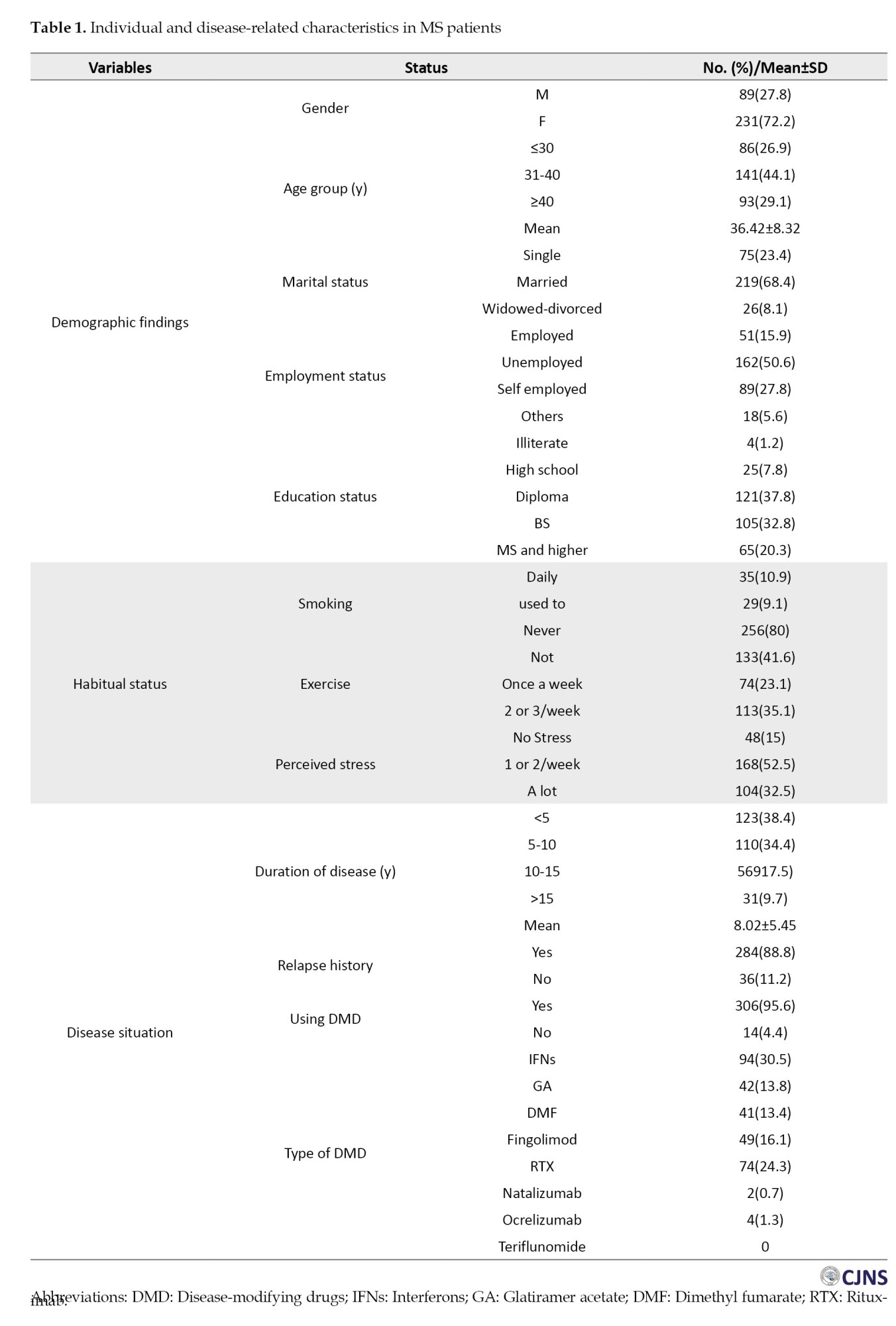
Table 2 reports the central tendency indices of the main research variables, the skewness and kurtosis indices, and the Pearson correlation coefficients between the variables.
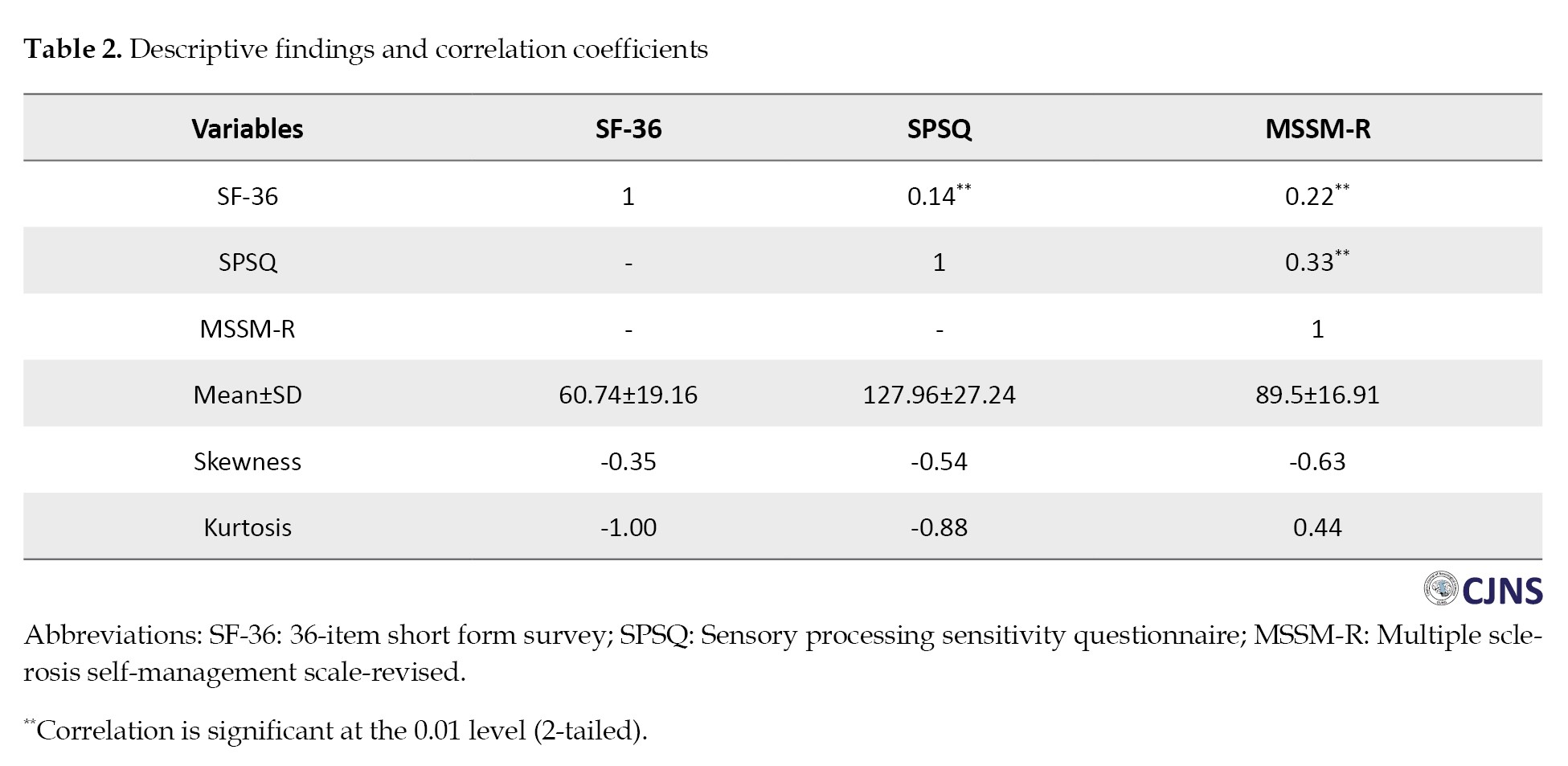
In Table 2, the results show that the skewness and kurtosis indices are in the range of ±2; accordingly, the data have a normal distribution. Also, the results of the Pearson correlation coefficient test showed that the quality of life in people with MS has a positive significant relationship with SPS (r=0.14) and self-management (r=0.22, P<0.05). Table 3 compares the scores of individuals on the SPSQ, MSSM-R and SF-36 based on demographic information.
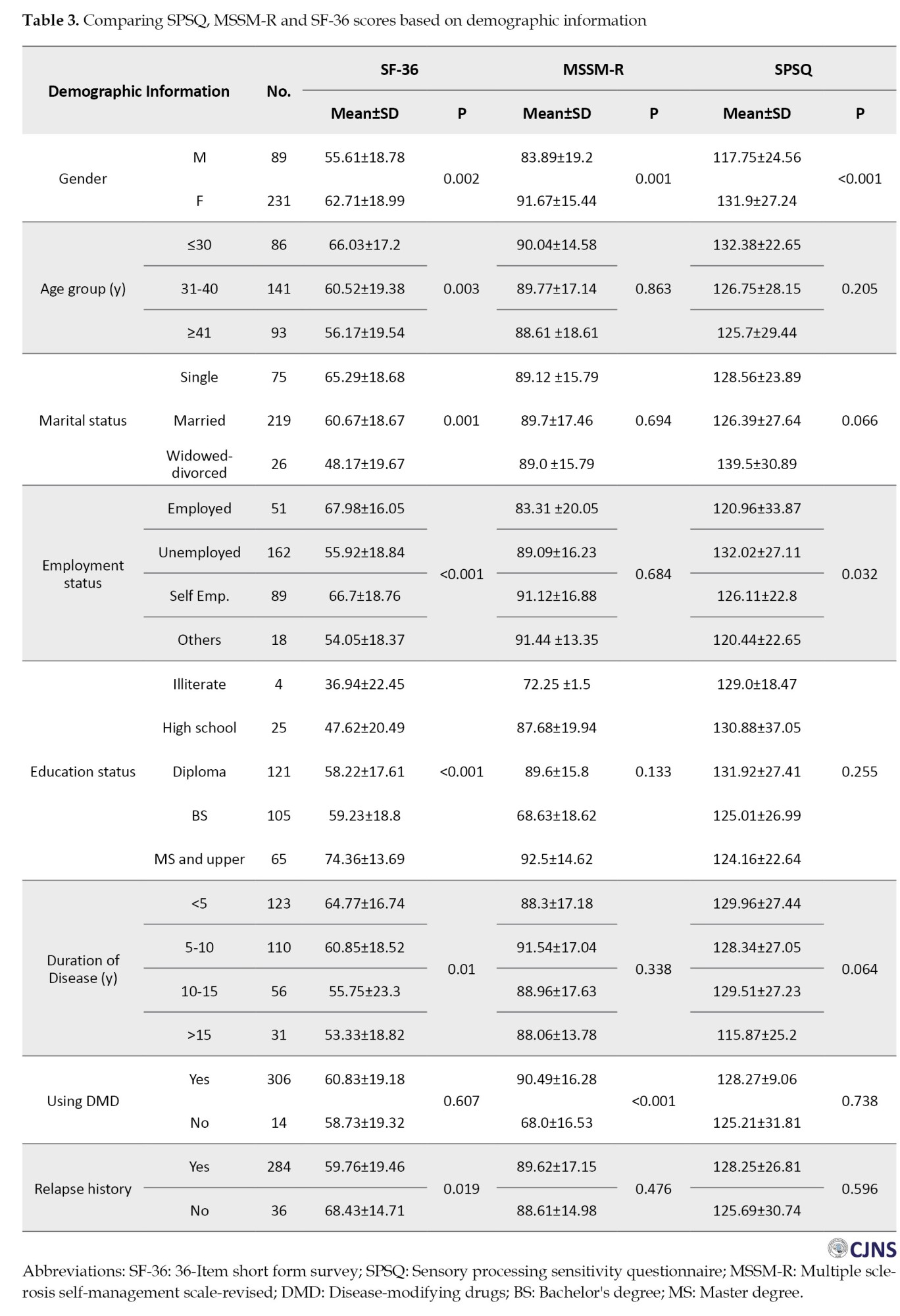
The findings in Table 3 show that the SF-36 score is significantly different according to gender, age group, marital status, education level, disease duration, and history of recurrence; also, the MSSM-R score was significantly different based on using DMD. Another finding shows that the SPSQ score is significantly different based on gender and employment status (P<0.05). The results of the regression model are presented in Table 4.
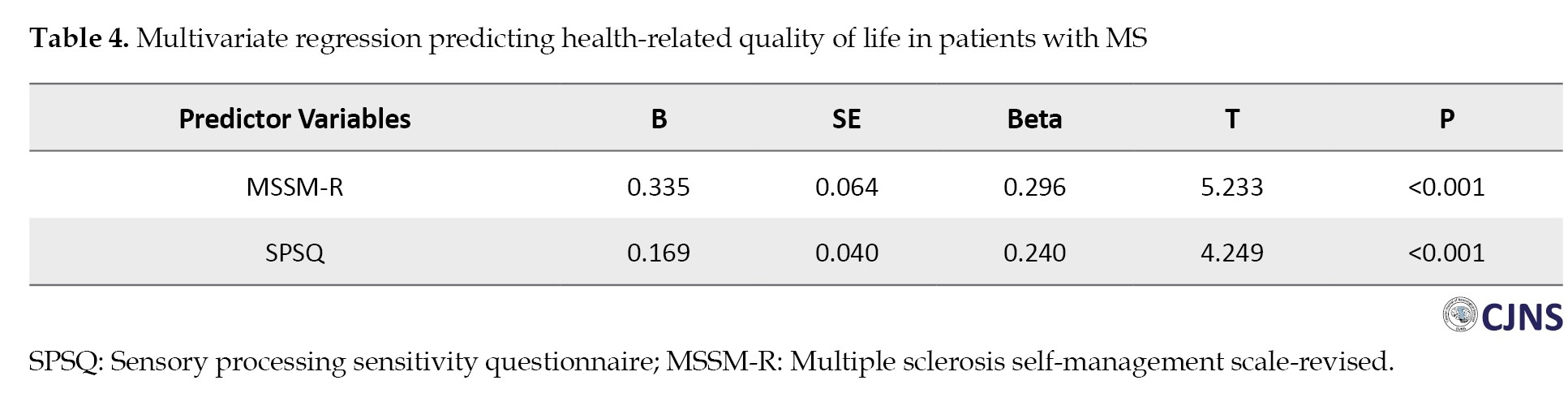
The stepwise multiple regression model results showed that MSSM-R and SPSQ, with beta coefficients of 0.296 and 0.240, respectively, significantly explained 12% of the variance in quality of life in people with MS.
Discussion
This study investigated the relationship between HRQOL and sensory processing and self-management in people with MS. The results showed that the majority of patients were female, married, homemakers, and in the age group of 31-40 years with a duration of illness less than 5 years and had a history of relapses and disease attacks. The findings showed that the SF-36 score significantly differed according to gender, age group, marital status, education level, disease duration, and history of recurrence. Also, the MSSM-R score was significantly different based on Using DMD. Another finding showed that the SPSQ score significantly differed based on gender and employment status. The results of multivariate regression showed that the quality of life-related to health can be predicted by sensory processing and self-management variables.
The influence of gender on MS has been evidenced across various dimensions of the condition, including a heightened vulnerability in women and more severe disease progression and outcomes in men [37]. In terms of the interplay between gender and age, the findings of this study indicated that 72.2% of the MS patients were female, with 44.1% falling within the age range of 31 to 40 years. Similar to the present study, Magyari and Sorensen reported this disease in women 3 times more than men, and the age of onset of the disease was between 20 and 40 years, although according to the reports, this disease can occur at any age [38]. This report is consistent with the results of other researchers [39-41]. In a way, it refers to the importance of the difference between the hormones of men and women, as well as the greater tendency of women than men to suffer from autoimmune diseases [42].
Numerous studies assessed the employment status of patients with MS [43-46]. In the current study, 50.6% of participants were homemakers and unemployed. In contrast, previous research indicated that 88% of individuals with MS had maintained a stable and or permanent job at some point in their lives, with a breakdown of 95% for men and 85% for women. Consistent with findings from other studies [44, 47], our research revealed that most unemployed patients were women with fewer years of education. This finding suggests that the lower employment rates among women at the onset of the disease may not solely be attributed to the clinical manifestations of MS but also to the greater challenges women face, regardless of age, in securing regular paid employment compared to men. Conversely, some studies have indicated a heightened risk of unemployment among men with MS [48, 49]. Other research has not found a significant correlation between gender and occupational status [43, 49].
The analytical findings of this study show that SPS and self-management are two important factors in predicting the quality of life of people with MS. This finding is consistent with previous studies [50, 51]. The importance of SPS and self-management in improving the quality of life of MS patients has been emphasized in previous studies. In explanation, it can be said that SPS and effective self-management strategies can significantly improve the quality of life of MS patients. People with strong sensory sensitivity attend more to sensory stimuli, which can help them recognize and respond more effectively to their body’s needs. This increased awareness allows for better management of MS-related symptoms, such as fatigue and pain [50]. Self-management also allows people to adjust their care routines according to their unique sensory processing patterns. This activity can include adjusting their environment to minimize overstimulation or fatigue improving daily functioning and overall quality of life [51]. Through self-management, people can develop effective coping strategies aligned with their sensory profiles. For example, those sensitive to sensory stimuli may benefit from creating quieter, more controlled environments to reduce sensory overload [51]. In summary, SPS and self-management strategies play an important role in improving the quality of life of people with MS. By cultivating greater awareness of their sensory experiences and implementing self-management techniques; individuals can better cope with the challenges posed by their condition, leading to improved emotional well-being and daily functioning.
One of the limitations of this study was the lack of a control group to compare with patients with MS to examine the variables. Another limitation was the online completion of information, which was used due to the coincidence of sampling with the COVID-19 pandemic to prevent patients from getting infected instead of being present on site. The number of questionnaires and the multiplicity of questions that people could answer could be a deterrent factor in providing correct answers. Before the collection, the necessary explanations were given to the eligible patients regarding the importance of the patients’ correct answers in expressing the results. Although the importance of data collection in person and through interviews cannot be ignored, the online method was accepted during sampling.
Conclusion
In summary, SPS and self-management are important factors in improving the quality of life of people with MS. Accordingly, empowerment interventions to improve psychological status and self-management of the quality of life of these people are recommended.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.542).
Funding
This article wasa extracted from Neurology specialty thesis of Masomeh Babaee, approved by Guilan University of Medical Sciences (Registration No.: 1244) and financially supported by Guilan University of Medical Sciences (Grant No.: 2756).
Authors contributions
Supervision: Mozaffar Hosseininezhad, Alia Saberi, and Sajjad Saadat; Funding administration and methodology: Babak Bakhshayesh Eghbali and Sajjad Saadat; Data analysis: Sajjad Saadat; Investigation: Masomeh Babaee, Kimia Eyvani and Kosar Kohandel; Conceptualization, writing the original draft, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate all the participants who helped us complete the questionnaires and also thank the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences.
References
Multiple sclerosis (MS) is a central nervous system (CNS) disorder with motor, sensory, cognitive and neuropsychiatric symptoms [1]. It is progressive, chronic and usually starts between the ages of 20 and 40. It is the second leading cause of non-traumatic disability in young people [2]. The prevalence and incidence of MS are rising in developing and developed countries. According to the reports, more than 400000 people in North America and about 2.5 million people worldwide have been affected by this disease. It is estimated that the prevalence of MS in Iran is 15-20 per 100000 population. On average, 5000 newly patients are diagnosed with this disease in Iran every year [2]. Although the exact cause of MS is unknown, some studies suggest that mitochondrial dysfunction, many genes, and environmental factors, such as exposure to ultraviolet B radiation, Epstein-Barr virus (EBV) infection, obesity and smoking, can affect this disease [3-7]. The most common type of this disease is relapsing-remitting MS (85-90%), and the majority of MS treatments are also focused on this type. It is noticeable that a small proportion of patients (10%) have primary progressive MS, and the treatment options for this condition are limited [8, 9]. MS compromises health-related quality of life (HRQOL). It is defined as the functional effect of a disease and its therapeutic outcome on the patient, as perceived by the patient [10].
Depression is known as the most important factor affecting the quality of life of Iranian MS patients [11]. The quality of life emphasizes various aspects of life, such as physical, emotional, cognitive and social [12, 13]. The main goal of treatment for chronic diseases such as MS is to optimize the patient’s quality of life [14]. In addition, identifying HRQOL factors can help maximize well-being and quality of life in MS patients. Physical and cognitive impairments, fatigue, comorbidities and emotional symptoms can predict HRQOL in people with MS [15-17]. Sensory processing is also another factor that may predict HRQOL in MS patients [18]. Sensory processing predicts how to respond to sensory information, including two components: neural threshold and self-regulation [19]. New evidence shows that the processing of sensory information in every person occurs in different ways, meaning that some persons are more sensitive to sensory information than others [20]. Neural threshold refers to the detection value of sensory stimuli, which ranges from hyposensitivity to hypersensitivity [21]. Self-regulation includes active and passive behaviors. Active strategies are responsible for dealing with available sensory information based on a person’s neural threshold, while passive strategies are not. For example, people with active hypersensitivity can try to minimize additional sensory input by controlling the environment [22].
Much evidence shows that people with self-regulation (those who have a deep understanding of their own emotions, can manage them effectively, and comprehend the emotions of others) are more successful and efficient in all areas of life. Emotion management includes monitoring flow, evaluating, and changing emotional experiences [20]. On the other hand, learning self-management by patients with chronic diseases is an important component of participation in their treatment [21]. Self-management is an active process of coping with illness through adherence to treatment and medication, participation in medical decisions, self-care, and maintaining social relationships and emotional balance [19]. Another definition of self-management is learning and participating in the skills necessary for an active life and a satisfactory mental state in living with a chronic disease [23].
Among patients with chronic disease, self-management enhances the quality of life, diminishing symptoms and treatment expenses [24]. Additional research suggests that self-management correlates with a broad spectrum of beneficial outcomes in the spheres of health and rehabilitation [25], such as improved self-regulation of disease symptoms [26], decreased rates of hospitalization [27] and alleviation of pain and anxiety [28]. Implementing self-management strategies that involve a more profound perception of the disease, acquiring relevant knowledge about appropriate dietary and nutritional guidelines and enhancing patient education and skills can significantly contribute to health maintenance and mitigating disease-related side effects [29].
Increasing self-management behaviors seems suitable for people with MS [21, 30-32]. This study investigates the association between HRQOL based on sensory processing sensitivity (SPS) and self-management in MS patients. Conducting this study and its results may provide a suitable solution for performing practical interventions and improving the quality of life in MS patients.
Materials and Methods
This cross-sectional-analytical study was conducted on MS patients registered in the nationwide MS registry of Iran (NMSRI), Guilan Province, from March 2020 to March 2021. The size of the studied population was 320 MS patients with relapsing-remitting MS (RRMS) type. The inclusion criteria were as follows: Patients diagnosed with MS by a neurologist based on revised McDonald criteria 2017 [33], aged between 20 and 55 years, RRMS type and their expanded disability status scale (EDSS) is <7. The exclusion criteria were as follows: Having other autoimmune diseases of the CNS or progressive MS (primary and secondary). Data were collected by three standard questionnaires and a general demographic information checklist. For this purpose, the first step was to upload the questionnaire and informed consent on the Porsline website. Then, a list of all active registered patients in NMSRI, Guilan, was prepared, and the survey link (completion guide, informed consent form, and questionnaire) was sent to them by a simple random method.
Study tools
MS self-management scale-revised (MSSM-R)
This MSSM-R includes 24 items in 5 subscales: Communication with health care providers, treatment adherence/coping with barriers, social/family support, information and knowledge about MS and health maintenance behavior. The scoring method of the questionnaire was based on a 5-point Likert scale (1=completely disagree, 2=somewhat disagree, 3=neither agree nor disagree, 4=somewhat agree, 5=completely agree). The higher the individual’s score, the higher the level of self-management is. The range of changes was between 24 and 120 [34]. This scale was translated into Farsi, and its psychometric properties were calculated by Saadat et al. The results showed that this scale has acceptable face and content validity. The results of confirmatory factor analysis showed that 24 items of the questionnaire have acceptable factor loadings in 5 subscales [35].
36-Item short form survey
The 36-item short-form survey (SF-36) or questionnaire has 36 items that evaluate 8 different areas of health: physical performance, role limitations due to physical health status and emotional problems, energy and vitality, emotional health, social performance, pain, and general health. The lowest score in this questionnaire is zero, and the highest is 100. A lower score means a lower quality of life; The closer the score is to 100, the higher the quality of life. In Montazeri et al.’s study, the Persian version of SF-36 subscales had standard reliability coefficients (0.77 to 0.9). So, it is a standard tool to measure HRQOL with required reliability and validity [36].
SPS questionnaire (SPSQ)
The SPSQ consists of 27 self-report questions that measure psychological reactivity to environmental stimuli. It consists of 3 subscales: Ease of stimulation, aesthetic sensitivity, and low sensory threshold and is answered based on a 7-point Likert scale so that the completely disagree option is given a score of 1 and the agree option is given a score of 7. The range of changes in this tool is between 27 and 189. Higher scores indicate better SPS; the validity and reliability of this questionnaire have been confirmed in an Iranian sample and its Cronbach alpha has been reported to be 0.78 [11].
Statistical analysis
Data analysis was performed in SPSS software, version 24. The data obtained were analyzed by the Independent t-test, one-way analysis of variance, the Pearson correlation coefficient and multiple linear regression. Also, a significance level of 0.05 was considered in this study.
Results
A total of 320 patients participated in this study in 2020. Individual characteristics of patients are given in Table 1.
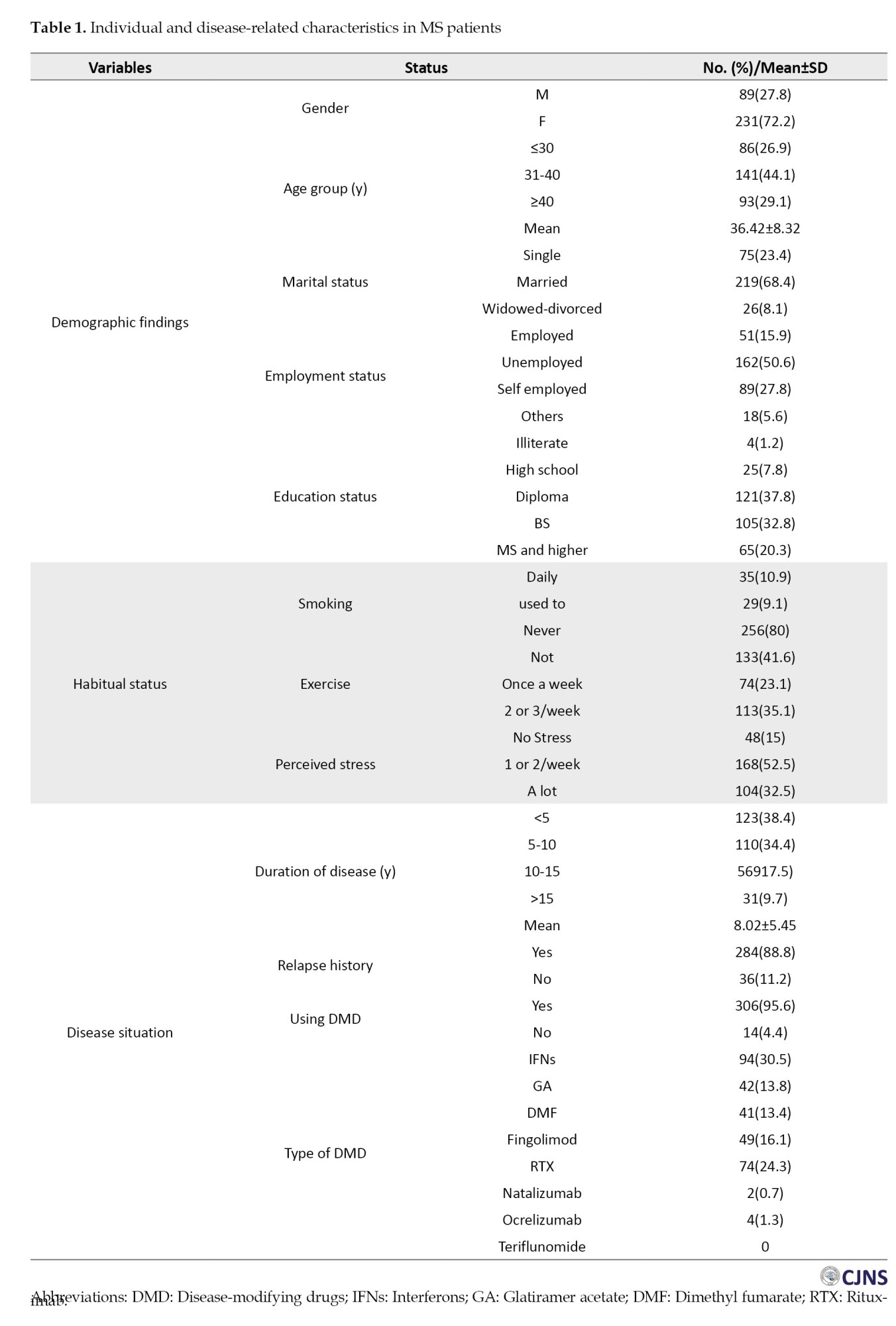
Table 2 reports the central tendency indices of the main research variables, the skewness and kurtosis indices, and the Pearson correlation coefficients between the variables.
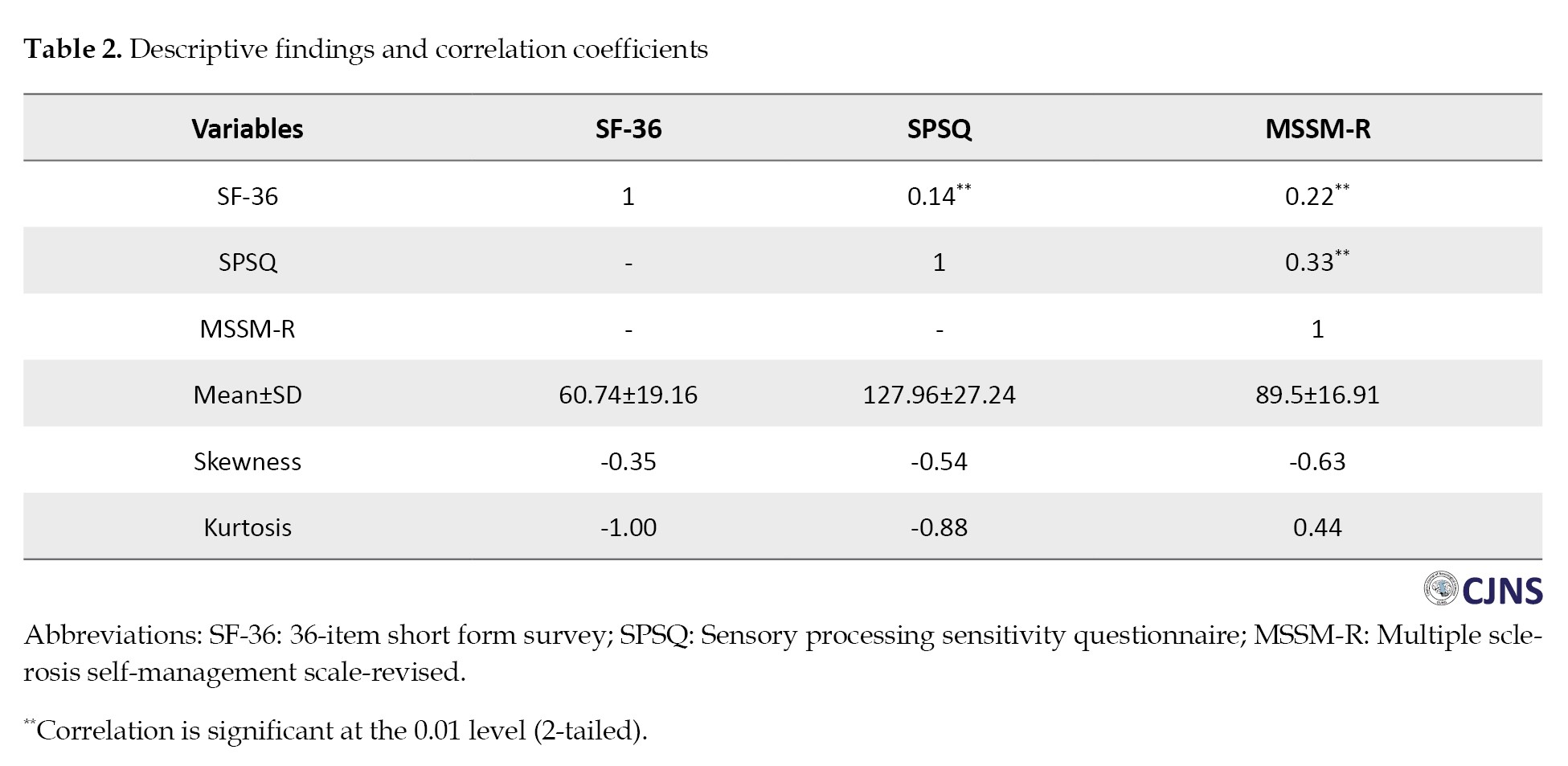
In Table 2, the results show that the skewness and kurtosis indices are in the range of ±2; accordingly, the data have a normal distribution. Also, the results of the Pearson correlation coefficient test showed that the quality of life in people with MS has a positive significant relationship with SPS (r=0.14) and self-management (r=0.22, P<0.05). Table 3 compares the scores of individuals on the SPSQ, MSSM-R and SF-36 based on demographic information.
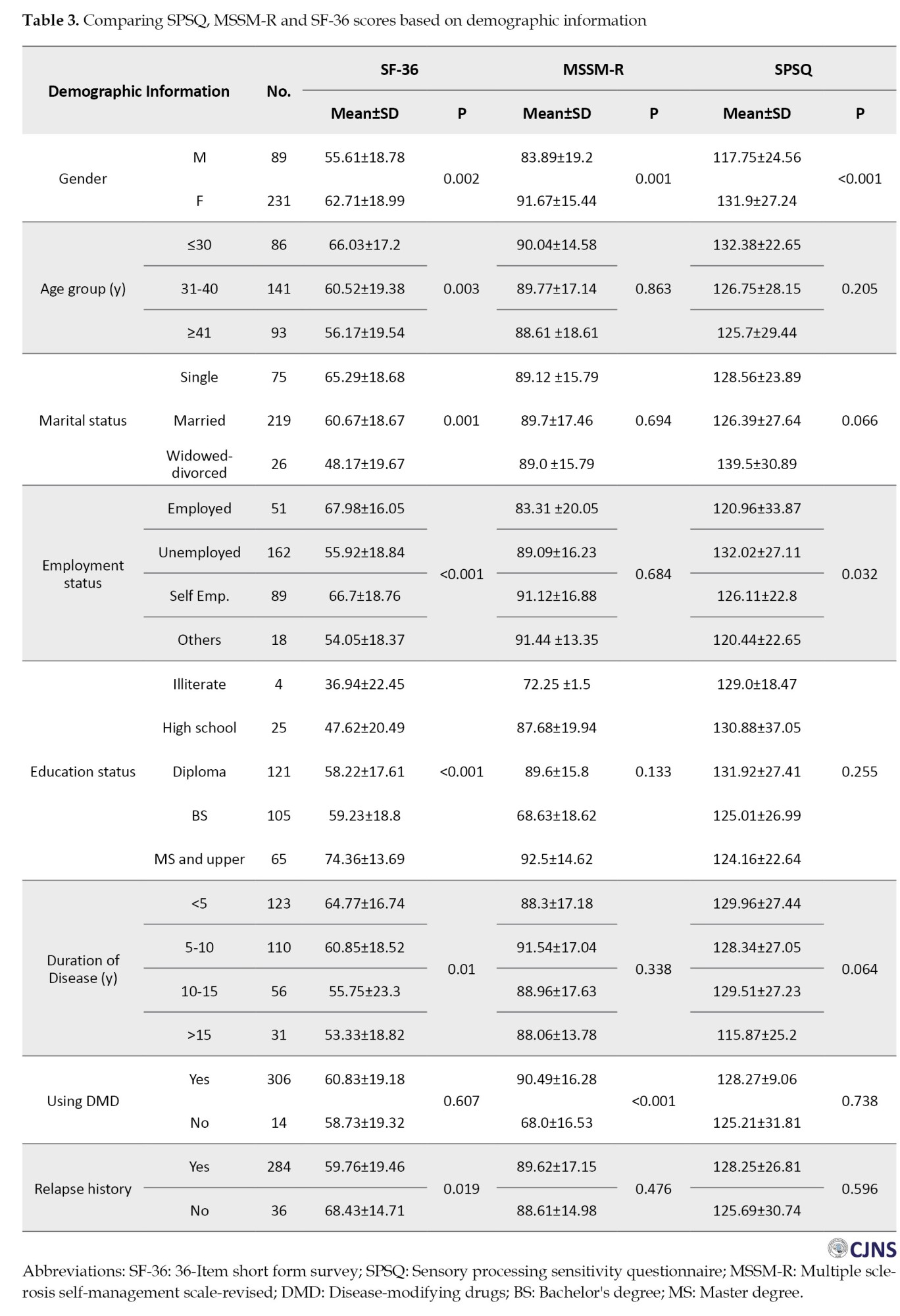
The findings in Table 3 show that the SF-36 score is significantly different according to gender, age group, marital status, education level, disease duration, and history of recurrence; also, the MSSM-R score was significantly different based on using DMD. Another finding shows that the SPSQ score is significantly different based on gender and employment status (P<0.05). The results of the regression model are presented in Table 4.
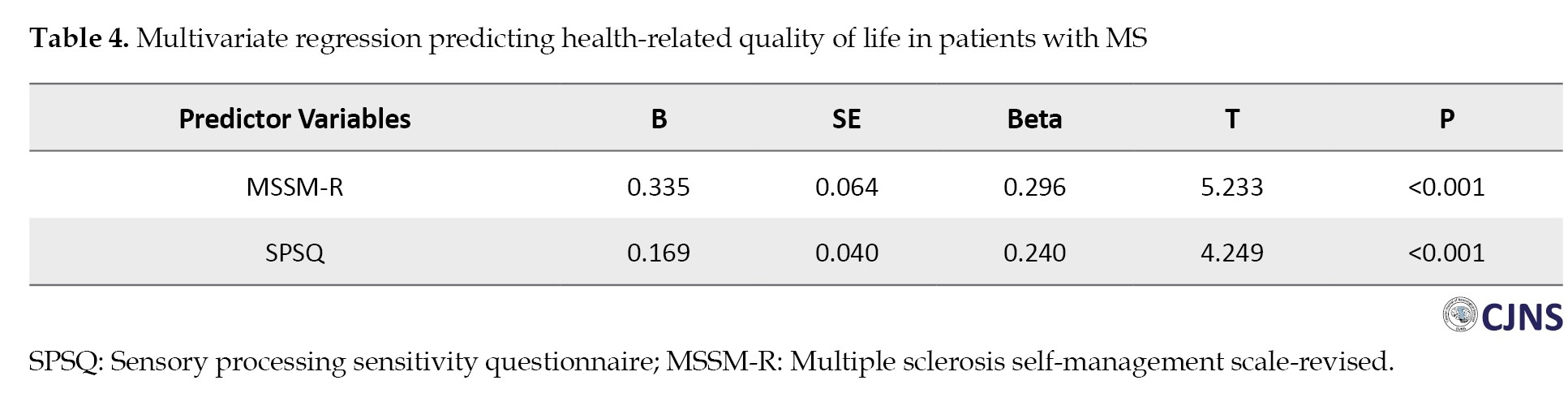
The stepwise multiple regression model results showed that MSSM-R and SPSQ, with beta coefficients of 0.296 and 0.240, respectively, significantly explained 12% of the variance in quality of life in people with MS.
Discussion
This study investigated the relationship between HRQOL and sensory processing and self-management in people with MS. The results showed that the majority of patients were female, married, homemakers, and in the age group of 31-40 years with a duration of illness less than 5 years and had a history of relapses and disease attacks. The findings showed that the SF-36 score significantly differed according to gender, age group, marital status, education level, disease duration, and history of recurrence. Also, the MSSM-R score was significantly different based on Using DMD. Another finding showed that the SPSQ score significantly differed based on gender and employment status. The results of multivariate regression showed that the quality of life-related to health can be predicted by sensory processing and self-management variables.
The influence of gender on MS has been evidenced across various dimensions of the condition, including a heightened vulnerability in women and more severe disease progression and outcomes in men [37]. In terms of the interplay between gender and age, the findings of this study indicated that 72.2% of the MS patients were female, with 44.1% falling within the age range of 31 to 40 years. Similar to the present study, Magyari and Sorensen reported this disease in women 3 times more than men, and the age of onset of the disease was between 20 and 40 years, although according to the reports, this disease can occur at any age [38]. This report is consistent with the results of other researchers [39-41]. In a way, it refers to the importance of the difference between the hormones of men and women, as well as the greater tendency of women than men to suffer from autoimmune diseases [42].
Numerous studies assessed the employment status of patients with MS [43-46]. In the current study, 50.6% of participants were homemakers and unemployed. In contrast, previous research indicated that 88% of individuals with MS had maintained a stable and or permanent job at some point in their lives, with a breakdown of 95% for men and 85% for women. Consistent with findings from other studies [44, 47], our research revealed that most unemployed patients were women with fewer years of education. This finding suggests that the lower employment rates among women at the onset of the disease may not solely be attributed to the clinical manifestations of MS but also to the greater challenges women face, regardless of age, in securing regular paid employment compared to men. Conversely, some studies have indicated a heightened risk of unemployment among men with MS [48, 49]. Other research has not found a significant correlation between gender and occupational status [43, 49].
The analytical findings of this study show that SPS and self-management are two important factors in predicting the quality of life of people with MS. This finding is consistent with previous studies [50, 51]. The importance of SPS and self-management in improving the quality of life of MS patients has been emphasized in previous studies. In explanation, it can be said that SPS and effective self-management strategies can significantly improve the quality of life of MS patients. People with strong sensory sensitivity attend more to sensory stimuli, which can help them recognize and respond more effectively to their body’s needs. This increased awareness allows for better management of MS-related symptoms, such as fatigue and pain [50]. Self-management also allows people to adjust their care routines according to their unique sensory processing patterns. This activity can include adjusting their environment to minimize overstimulation or fatigue improving daily functioning and overall quality of life [51]. Through self-management, people can develop effective coping strategies aligned with their sensory profiles. For example, those sensitive to sensory stimuli may benefit from creating quieter, more controlled environments to reduce sensory overload [51]. In summary, SPS and self-management strategies play an important role in improving the quality of life of people with MS. By cultivating greater awareness of their sensory experiences and implementing self-management techniques; individuals can better cope with the challenges posed by their condition, leading to improved emotional well-being and daily functioning.
One of the limitations of this study was the lack of a control group to compare with patients with MS to examine the variables. Another limitation was the online completion of information, which was used due to the coincidence of sampling with the COVID-19 pandemic to prevent patients from getting infected instead of being present on site. The number of questionnaires and the multiplicity of questions that people could answer could be a deterrent factor in providing correct answers. Before the collection, the necessary explanations were given to the eligible patients regarding the importance of the patients’ correct answers in expressing the results. Although the importance of data collection in person and through interviews cannot be ignored, the online method was accepted during sampling.
Conclusion
In summary, SPS and self-management are important factors in improving the quality of life of people with MS. Accordingly, empowerment interventions to improve psychological status and self-management of the quality of life of these people are recommended.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.542).
Funding
This article wasa extracted from Neurology specialty thesis of Masomeh Babaee, approved by Guilan University of Medical Sciences (Registration No.: 1244) and financially supported by Guilan University of Medical Sciences (Grant No.: 2756).
Authors contributions
Supervision: Mozaffar Hosseininezhad, Alia Saberi, and Sajjad Saadat; Funding administration and methodology: Babak Bakhshayesh Eghbali and Sajjad Saadat; Data analysis: Sajjad Saadat; Investigation: Masomeh Babaee, Kimia Eyvani and Kosar Kohandel; Conceptualization, writing the original draft, review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate all the participants who helped us complete the questionnaires and also thank the Clinical Research Development Unit of Poursina Hospital, Guilan University of Medical Sciences.
References
- Ropper AH, Samuels MA, Klein JP, Prasad S. Adams and victor’s principles of neurology. New York: McGraw Hill LLC; 2023. [Link]
- Goverover Y, Genova HM, Smith A, Lengenfelder J, Chiaravalloti ND. Changes in activity participation after multiple sclerosis diagnosis. Int J MS Care. 2020; 22(1):23-30. [DOI:10.7224/1537-2073.2018-036]
- Saberi A, Akhondzadeh S, Kazemi S. Infectious agents and different course of multiple sclerosis: A systematic review. Acta Neurol Belg. 2018; 118(3):361-77. [DOI:10.1007/s13760-018-0976-y] [PMID]
- Saberi A, Kazemi S. Mitochondrial dysfunction in multiple sclerosis: A systematic review. Acta Med Iran. 2019; 57(1):5-16. [DOI:10.18502/acta.v57i1.1748]
- Saadat S, Saberi A. Environmental risk factors in multiple sclerosis: A narrative review. J Guilan Univ of Med Sci. 2022; 31(2):166-79 [DOI:10.32598/JGUMS.31.2.1374.2]
- Bakhshi A, Saberi A, Norouzi N, Sedighi N. Association between multiple sclerosis and Helicobacter pylori in the acute and chronic phases of infection: A systematic review and meta-analysis. Ro J Neurol. 2023; 22(1):16-22. [DOI:10.37897/RJN.2023.1.2]
- Ghayeghran A, Ghahramani E, Saberi A, Hatamian H, Homaie Rad E, Ghorbani Shirkouhi S, et al. COVID-19 infection and seropositivity in multiple sclerosis patients in Guilan in 2021. Casp J Neurol Sci. 2023; 9(1):39-49. [DOI:10.32598/CJNS.9.32.8.29]
- Fallah Arzpeyma S, Janeshin S, Soofi Afshar N, Saberi A, Ghalyanchi Langroodi H, Ghaffari ME, et al. Brain MRI volumetric assessment of patients with multiple sclerosis: The volume of basal ganglia, thalamus, and posterior fossa. Basic Clin Neurosci. 2023; 14(6):741-52. [DOI:10.32598/bcn.2023.1324.4] [PMID]
- Lomer NB, Asalemi KA, Saberi A, Sarlak K. Predictors of multiple sclerosis progression: A systematic review of conventional magnetic resonance imaging studies. Plos One. 2024; 19(4):e0300415 [DOI:10.1371/journal.pone.0300415] [PMID]
- Ashing-Giwa KT. The contextual model of HRQoL: A paradigm for expanding the HRQoL framework. Qual Life Res. 2005; 14:297-307. [Link]
- Nedjat S, Montazeri A, Mohammad K, Majdzadeh R, Nabavi N, Nedjat F, et al. [Quality of life in multiple sclerosis compared to the healthy population in Tehran (Persian)]. Iran J Epidemiol. 2006; 2(3):19-24. [Link]
- Kesselring J, Mertin J. [Rehabilitation in multiple sclerosis (German)]. Schweiz Rundsch Med Prax. 1991 Oct 8;80(41):1120-3. [PMID]
- Motl RW, Snook EM. Physical activity, self-efficacy, and quality of life in multiple sclerosis. Ann Behav Med. 2008; 35(1):111-5. [DOI:10.1007/s12160-007-9006-7] [PMID]
- Drulovic J, Pekmezovic T, Matejic B, Mesaros S, Manigoda M, Dujmovic I, et al. Quality of life in patients with multiple sclerosis in Serbia. Acta Neurol Scand. 2007; 115(3):147-52. [DOI:10.1111/j.1600-0404.2006.00729.x] [PMID]
- Berrigan LI, Fisk JD, Patten SB, Tremlett H, Wolfson C, Warren S, et al. Health-related quality of life in multiple sclerosis: Direct and indirect effects of comorbidity. Neurology. 2016; 86(15):1417-24. [DOI:10.1212/WNL.0000000000002564] [PMID]
- Rezaei S, Saberi A, Hatamian H, Ghayeghran A, Khaksari Z, Mollahosein F. Adaptation and validation of the hamburg quality of life questionnaire in multiple sclerosis (HAQUAMS) for use in Iranian patients. Acta Neurol Taiwan. 2022; 31(1):24-35. [Link]
- Saberi A, Hatamian H, Ghayeghran A, Mola Hosseini F, Noroozi Guilandehi S, Rezaei S, et al. Comparing the quality of life in patients with multiple sclerosis consuming fingolimod and cinnovex. Casp J Neurol Sci. 2019; 5(4):151-60. [DOI:10.32598/CJNS.5.19.151]
- Colbeck M. Sensory processing, cognitive fatigue, and quality of life in multiple sclerosis: Traitement de l'information sensorielle, fatigue cognitive et qualité de vie des personnes atteintes de sclérose en plaques. Can J Occup Ther. 2018; 85(2):169-75. [DOI:10.1177/0008417417727298] [PMID]
- Brown C, Dunn W. Adolescent/adult sensory profile. San Antonio: Psychological Corporation; 2002. [Link]
- Bar-Shalita T, Cermak SA. Atypical sensory modulation and psychological distress in the general population. Am J Occup Ther. 2016; 70(4):7004250010. [DOI:10.5014/ajot.2016.018648] [PMID]
- Kantarci O, Wingerchuk D. Epidemiology and natural history of multiple sclerosis: New insights. Curr Opin Neurol. 2006; 19(3):248-54. [DOI:10.1097/01.wco.0000227033.47458.82] [PMID]
- Wilski M, Tasiemski T, Kocur P. Demographic, socioeconomic and clinical correlates of self-management in multiple sclerosis. Disabil Rehabil. 2015; 37(21):1970-5. [DOI:10.3109/09638288.2014.993435] [PMID]
- Lorig K. Self-management of chronic illness: A model for the future. Generations. 1993; 17(3):11-4. [Link]
- Holman H, Lorig K. Patient self-management: A key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004; 119(3):239-43. [DOI:10.1016/j.phr.2004.04.002] [PMID]
- Bishop M, Frain MP, Tschopp MK. Self-management, perceived control, and subjective quality of life in multiple sclerosis: An exploratory study. Rehab Couns Bull. 2008; 52(1):45-56. [DOI:10.1177/0034355208320000]
- Jordan JE, Osborne RH. Chronic disease self-management education programs: Challenges ahead. Med J Aust. 2007; 186(2):84-7. [DOI:10.5694/j.1326-5377.2007.tb00807.x] [PMID]
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002; 288(19):2469-75. [DOI:10.1001/jama.288.19.2469] [PMID]
- Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: Towards an explanatory model. J Behav Med. 2003; 26(1):1-18. [DOI:10.1207/S15324796ABM2601_01] [PMID]
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004; 364(9444):1523-37. [DOI:10.1016/S0140-6736(04)17277-2] [PMID]
- Chwastiak LA, Gibbons LE, Ehde DM, Sullivan M, Bowen JD, Bombardier CH, et al. Fatigue and psychiatric illness in a large community sample of persons with multiple sclerosis. J Psychosom Res. 2005; 59(5):291-8. [DOI:10.1016/j.jpsychores.2005.06.001] [PMID]
- Ehde DM, Osborne TL, Hanley MA, Jensen MP, Kraft GH. The scope and nature of pain in persons with multiple sclerosis. Mult Scler. 2006; 12(5):629-38. [DOI:10.1177/1352458506071346] [PMID]
- Eghbali BB, Saadat S, Hasanzadeh K, Pourramzani A, Khatami SS, Saberi A, et al. Relationship between self-compassion and psychological well-being with the mediating role of resilience in people with multiple sclerosis. Postep Psychiatr Neurol. 2022; 31(2):43-51. [DOI:10.5114/ppn.2022.117999] [PMID]
- Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018; 17(2):162-73. [DOI:10.1016/S1474-4422(17)30470-2] [PMID]
- Bishop M, Frain MP. The multiple sclerosis self-management scale: Revision and psychometric analysis. Rehabil Psychol. 2011; 56(2):150-9. [DOI:10.1037/a0023679] [PMID]
- Saadat S, Kalantari M, Kajbaf MB, Hosseininezhad M. [Psychological status of multiple sclerosis patients: A qualitative study (Persian)]. J Health Syst Res. 2020; 15(4):296-303. [DOI:10.48305/hsr.2020.15.4.106]
- Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short form health survey (SF-36): Translation and validation study of the Iranian version. Qual Life Res. 2005; 14(3):875-82. [DOI:10.1007/s11136-004-1014-5] [PMID]
- Harbo HF, Gold R, Tintoré M. Sex and gender issues in multiple sclerosis. Ther Adv Neurol Disord. 2013; 6(4):237-48. [DOI:10.1177/1756285613488434] [PMID]
- Magyari M, Sorensen PS. The changing course of multiple sclerosis: Rising incidence, change in geographic distribution, disease course, and prognosis. Curr Opin Neurol. 2019; 32(3):320-6. [DOI:10.1097/WCO.0000000000000695] [PMID]
- Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult Scler. 2020; 26(14):1816-21. [DOI:10.1177/1352458520970841] [PMID]
- Kingwell E, Marriott JJ, Jetté N, Pringsheim T, Makhani N, Morrow SA, et al. Incidence and prevalence of multiple sclerosis in Europe: A systematic review. BMC Neurol. 2013; 13:128. [DOI:10.1186/1471-2377-13-128] [PMID]
- Saadatnia M, Etemadifar M, Maghzi AH. Multiple sclerosis in Isfahan, Iran. Int Rev Neurobiol. 2007; 79:357-75. [DOI:10.1016/S0074-7742(07)79016-5] [PMID]
- Avila M, Bansal A, Culberson J, Peiris AN. The role of sex hormones in multiple sclerosis. Eur Neurol. 2018; 80(1-2):93-99. [DOI:10.1159/000494262] [PMID]
- Moore P, Harding KE, Clarkson H, Pickersgill TP, Wardle M, Robertson NP. Demographic and clinical factors associated with changes in employment in multiple sclerosis. Mult Scler. 2013; 19(12):1647-54. [DOI:10.1177/1352458513481396] [PMID]
- Pompeii LA, Moon SD, McCrory DC. Measures of physical and cognitive function and work status among individuals with multiple sclerosis: A review of the literature. J Occup Rehabil. 2005; 15(1):69-84. [DOI:10.1007/s10926-005-0875-y] [PMID]
- Renner A, Baetge SJ, Filser M, Penner IK. Working ability in individuals with different disease courses of multiple sclerosis: Factors beyond physical impairment. Mult Scler Relat Disord. 2020; 46:102559. [DOI:10.1016/j.msard.2020.102559] [PMID]
- Messmer Uccelli M, Specchia C, Battaglia MA, Miller DM. Factors that influence the employment status of people with multiple sclerosis: A multi-national study. J Neurol. 2009; 256(12):1989-96. [DOI:10.1007/s00415-009-5225-0] [PMID]
- Raggi A, Covelli V, Schiavolin S, Scaratti C, Leonardi M, Willems M. Work-related problems in multiple sclerosis: A literature review on its associates and determinants. Disabil Rehabil. 2016; 38(10):936-44. [DOI:10.3109/09638288.2015.1070295] [PMID]
- Larocca N, Kalb R, Scheinberg L, Kendall P. Factors associated with unemployment of patients with multiple sclerosis. J Chronic Dis. 1985; 38(2):203-10. [DOI:10.1016/0021-9681(85)90093-1] [PMID]
- Hammond SR, McLeod JG, Macaskill P, English DR. Multiple sclerosis in Australia: Socioeconomic factors. J Neurol Neurosurg Psychiatry. 1996; 61(3):311-3. [DOI:10.1136/jnnp.61.3.311] [PMID]
- Rosso M, Chitnis T. Association between cigarette smoking and multiple sclerosis: A review. JAMA Neurol. 2020; 77(2):245-53. [DOI:10.1001/jamaneurol.2019.4271] [PMID]
- Degelman ML, Herman KM. Smoking and multiple sclerosis: A systematic review and meta-analysis using the Bradford Hill criteria for causation. Mult Scler Relat Disord. 2017; 17:207-16. [DOI:10.1016/j.msard.2017.07.020] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2024/02/25 | Accepted: 2024/05/26 | Published: 2025/01/1
Received: 2024/02/25 | Accepted: 2024/05/26 | Published: 2025/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |