Mon, Dec 29, 2025
Volume 11, Issue 1 (Winter 2025)
Caspian J Neurol Sci 2025, 11(1): 77-86 |
Back to browse issues page
Ethics code: IR.GUMS.REC.1399.508
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseininezhad M, Saadat S, Younesi Rostami F, Zare R, Bonyad A, Qanbary Joopish M, et al . The Feasibility of Telephone-delivered Self-management Intervention in Multiple Sclerosis. Caspian J Neurol Sci 2025; 11 (1) :77-86
URL: http://cjns.gums.ac.ir/article-1-765-en.html
URL: http://cjns.gums.ac.ir/article-1-765-en.html
Mozaffar Hosseininezhad1 

 , Sajjad Saadat2
, Sajjad Saadat2 

 , Fatemeh Younesi Rostami1
, Fatemeh Younesi Rostami1 

 , Roghaye Zare3
, Roghaye Zare3 

 , Ali Bonyad4
, Ali Bonyad4 

 , Masoumeh Qanbary Joopish5
, Masoumeh Qanbary Joopish5 

 , Alia Saberi *6
, Alia Saberi *6 

 , Fateme Shafaee2
, Fateme Shafaee2 




 , Sajjad Saadat2
, Sajjad Saadat2 

 , Fatemeh Younesi Rostami1
, Fatemeh Younesi Rostami1 

 , Roghaye Zare3
, Roghaye Zare3 

 , Ali Bonyad4
, Ali Bonyad4 

 , Masoumeh Qanbary Joopish5
, Masoumeh Qanbary Joopish5 

 , Alia Saberi *6
, Alia Saberi *6 

 , Fateme Shafaee2
, Fateme Shafaee2 


1- Neuroscience Research Center, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Guilan, Iran.
2- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Neuroscience Research Center, Trauma Institute, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Faculty of Medicine, Guilan University of Medical Science, Rasht, Iran.
5- Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran.
6- Neuroscience Research Center, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Guilan, Iran. ,Alia.saberi1@gmail.com
2- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Neuroscience Research Center, Trauma Institute, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Faculty of Medicine, Guilan University of Medical Science, Rasht, Iran.
5- Department of Psychology, Tonekabon Branch, Islamic Azad University, Tonekabon, Iran.
6- Neuroscience Research Center, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Guilan, Iran. ,
Full-Text [PDF 1590 kb]
(466 Downloads)
| Abstract (HTML) (857 Views)
Full-Text: (353 Views)
Introduction
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system which is chronic and degenerative. It affects approximately 2 million people worldwide [1] and is the second leading cause of non-traumatic disability in young people [2]. MS typically emerges in adults aged 20-40, with patients having a regular life expectancy [3]. It is more prevalent in women, especially in the white population. Key symptoms include cognitive and movement issues, sensory deficits, visual problems, balance impairments, fatigue, and pain [4, 5]. MS patients face daily physical, mental, and emotional challenges [1, 5]. Psychological issues like anxiety and mood disorders are common [6, 7], leading to significant disability in some cases [8]. Consequently, it impacts the quality of life [9]. While incurable, lifelong symptom management is crucial, requiring active self-management for treatment adherence, decision-making, self-care, and well-being [10-14].
Self-management in chronic diseases involves acquiring skills to lead a fulfilling life despite illness challenges, leading to improved quality of life, symptom reduction, and cost savings [11]. These strategies enhance understanding, knowledge, diet and well-being, benefiting health outcomes [15, 16]. There is significant evidence of health benefits after self-management interventions in chronic and long-term diseases such as diabetes, arthritis, and heart diseases [17, 18]. Individuals with chronic illnesses take charge of treatment adherence, exercise, social engagement, and healthcare choices, highlighting its pivotal role in addressing the condition and its secondary effects [17-19].
Telephone-based interventions improve the quality of life in people with MS by promoting physical activities like walking and exercise, leading to enhanced mental and physical performance [20, 21]. Research into the effectiveness and design of telephone interventions is vital due to knowledge gaps. While some studies indicate that interventions focusing on physical activity and self-management can moderately enhance healthy behaviors and quality of life, a lack of comprehensive understanding persists. Despite its acknowledged importance in chronic disease management, the limited research on self-management among people with MS accentuates the need for this research. Addressing these gaps can bridge evidence divides and potentially provide impactful strategies for promoting healthy behaviors, especially among MS patients.
Materials and Methods
This quasi-experimental study involved 20 MS patients selected from registered patients in the nationwide MS registry of Iran (NMSRI), Guilan, in 2020. Individuals were selected through a public call using judgmental sampling. The sample size was calculated based on the factor repeated measure approach’s formula with a 95% confidence level, 85% power and 0.33 effect size. According to the previous study [22] information, the G*Power software, version 3.1.9.4 calculated the sample size as 20. The study employed a pre-test-post-test with a two-month follow-up design. Inclusion criteria were MS diagnosis per McDonald’s 2017 criteria, age 20-55 and willingness to participate. The exclusion criteria were incomplete training and disagreement to participate in the study. A pre-test was taken before the intervention, and then training was implemented online and via telephone. The post-test was conducted immediately after the intervention and two months later using an online survey.
Study intervention
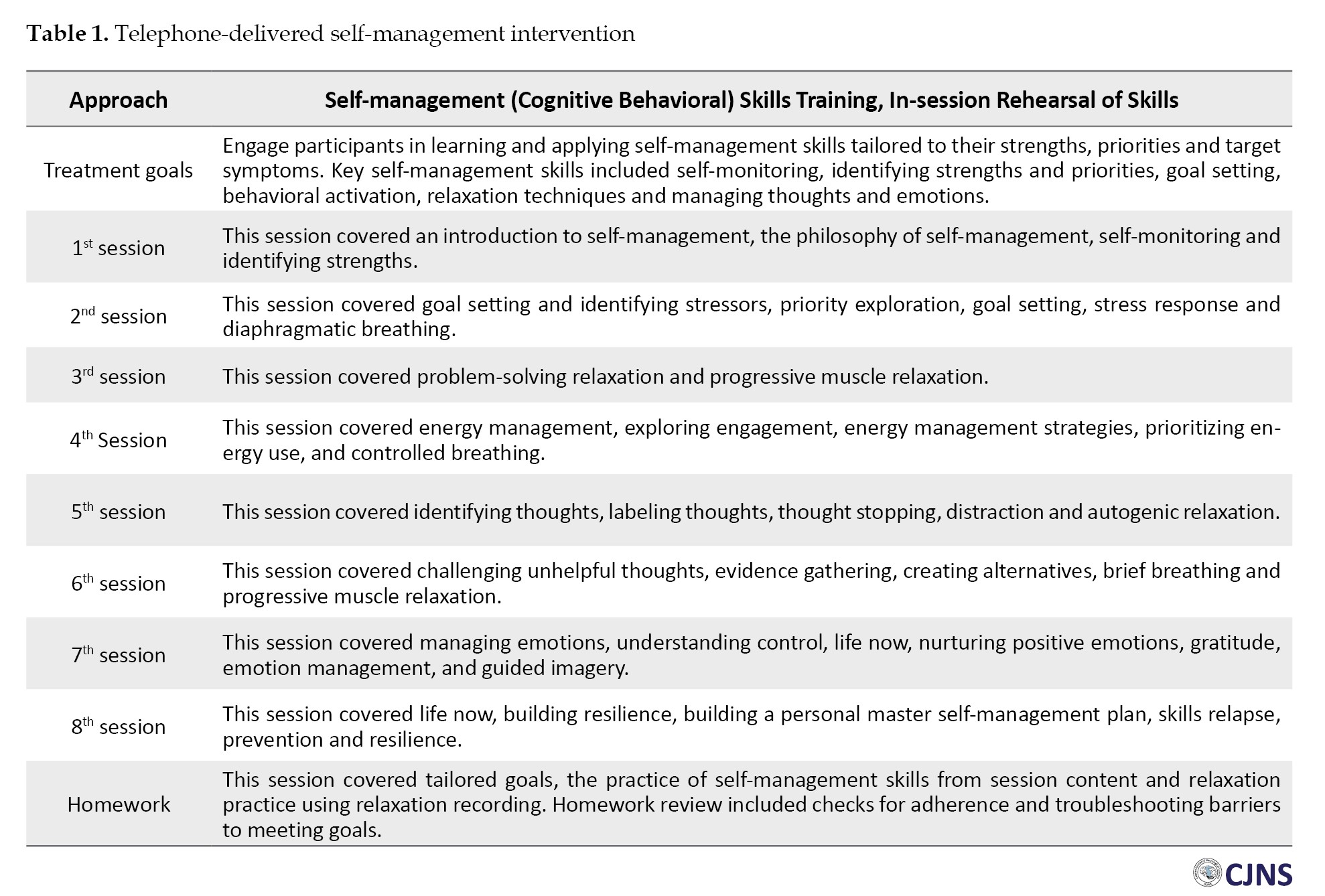
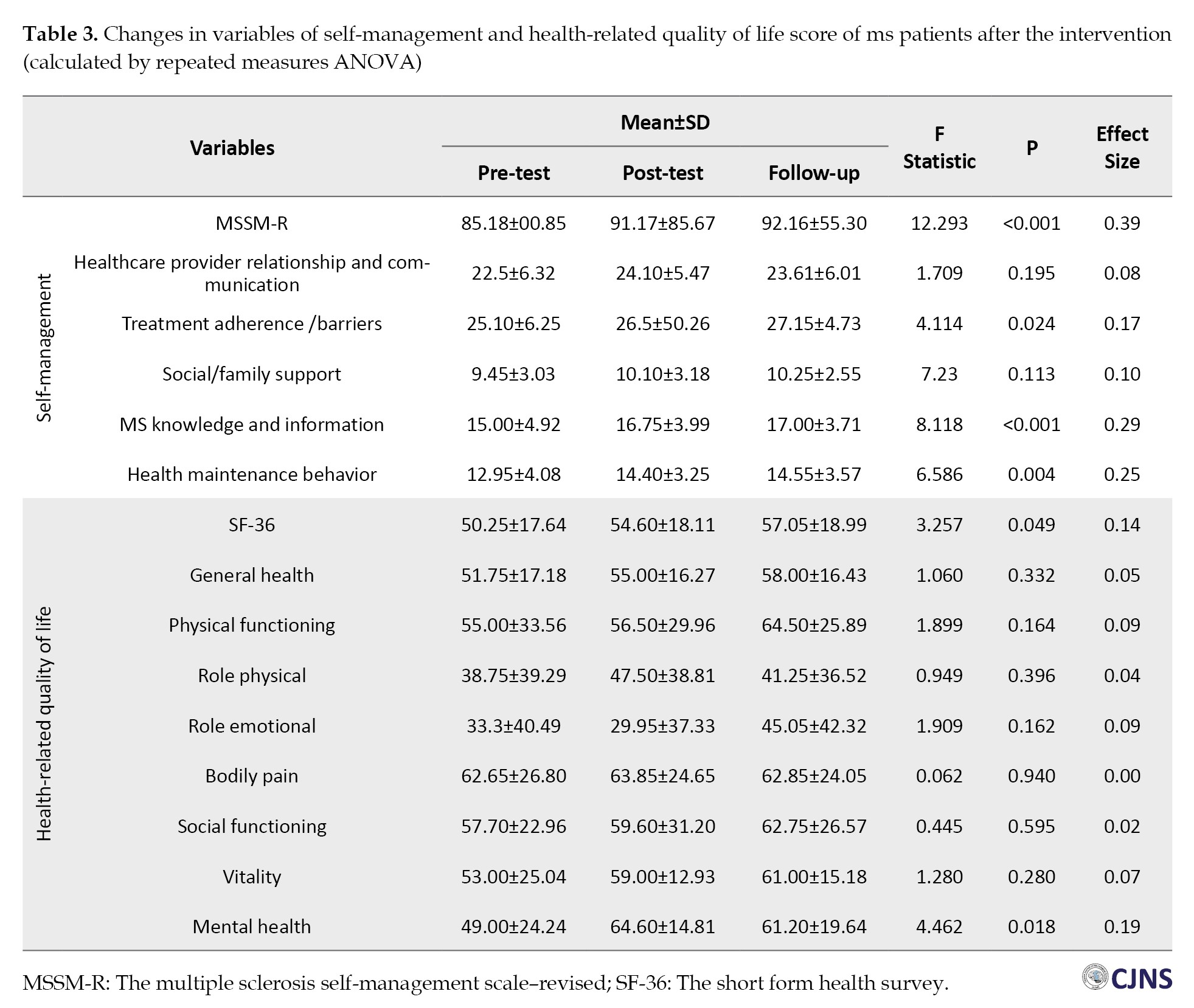
The educational program was a telephone-delivered self-management intervention and a standard intervention developed by Ehde et al. [23], including 8 weekly sessions of 45 to 60 minutes by phone with MS patients in a group setting. Self-management intervention is over the phone (audio, video and educational files and phone calls), including evidence-based cognitive-behavioral and psychological strategies to help participants manage pain, depression, and fatigue in everyday life. The therapist communicated with the participants on a scheduled basis to discuss the educational implications with them. Also, the academic content of each session was provided to the participants in the form of an electronic booklet, audio, and educational videos so that they could refer to them if they wanted to understand more about the training. Training sessions aimed at familiarizing self-management, goal setting, identifying stressful factors, problem-solving and relaxation training, energy management, working with thoughts, emotion management, and building resilience (Table 1).
Study tools
The MS self-management scale–revised (MSSM-R)
Bishop and Frein developed this self-report tool and has 24 items and 5 subscales: Healthcare provider relationship and communication, treatment adherence/barriers (TA/B), social/family support (S/FS) (three items: 6, 10, 13), MS knowledge and information (MSKI) and health maintenance behavior (HMB). The scoring method of the questionnaire was based on a 5-point Likert scale (completely disagree=1 to completely agree=5). The higher score indicates a high level of self-management; questions 21, 23 and 24 are scored in reverse. The range of changes in this tool is between 24 and 120 [24]. The psychometric assessment of the Persian-translated version of this scale was done by Saadat et al. The results showed that this scale has acceptable face and content validity. The confirmatory factor analysis showed that 24 items had acceptable factor loadings in 5 subscales. The internal consistency results of this scale were calculated by the Cronbach α method and the test-re-test reliability for the test subscales was reported between 0.70 and 0.89 [15].
The short form health survey (SF-36)
This questionnaire aims to assess the physical and mental health state. It has 36 items that evaluate 8 different subscales of health (physical functioning [PF], role physical [RP], bodily pain [BP], general health [GH], vitality [VT], social functioning [SF], role emotional [RE] and mental health [MH]). A lower score means a lower quality of life. In a study, the internal consistency of the first version of this questionnaire was between 0.72 and 0.94 with the Cronbach α [25]. Also, in Iran, Motamed et al. in Shiraz checked its reliability and estimated the Cronbach’s α of the Persian questionnaire to be 0.87 [26].
Statistical analysis
Data were analyzed using IBM SPSS software, version 26. Data were reported by frequency (percentage) or Mean±SD. The Shapiro-Wilk test was used to determine the normality of the distribution. A repeated measure analysis examined the changes in the variables from the pre-test to the follow-up.
Results
Initially, 60 patients referred to the MS Society of Guilan, Iran, participated in this study. Data gathering and intervention continued to reach the determined sample size. Finally, 20 patients completed the sessions, post-test, and follow-up evaluation. The descriptive findings of the study are reported in Table 2.
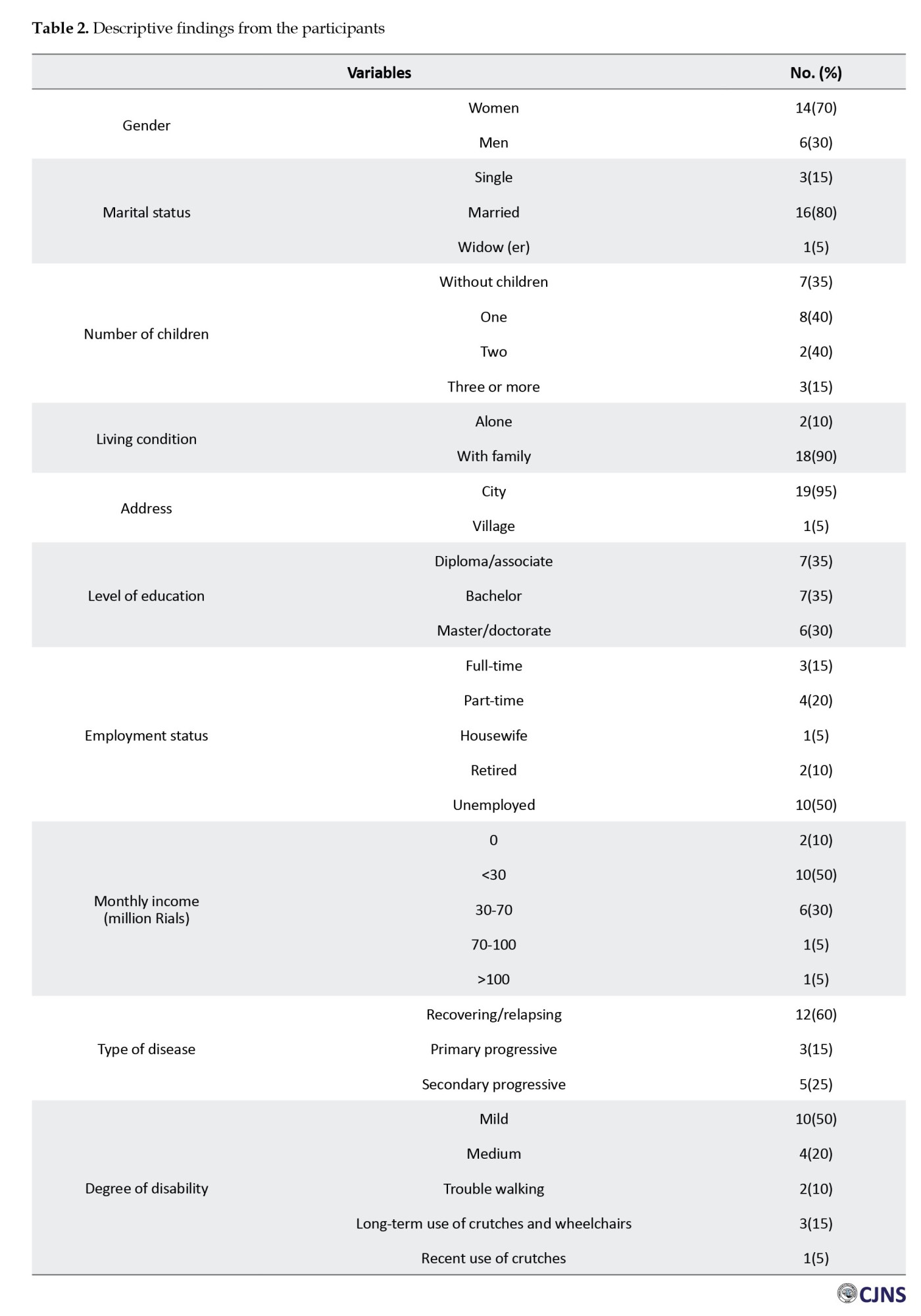
In this study, 20 individuals with MS participated until the end of the intervention and cooperated in various assessment stages. Their demographic information is presented in Table 2.
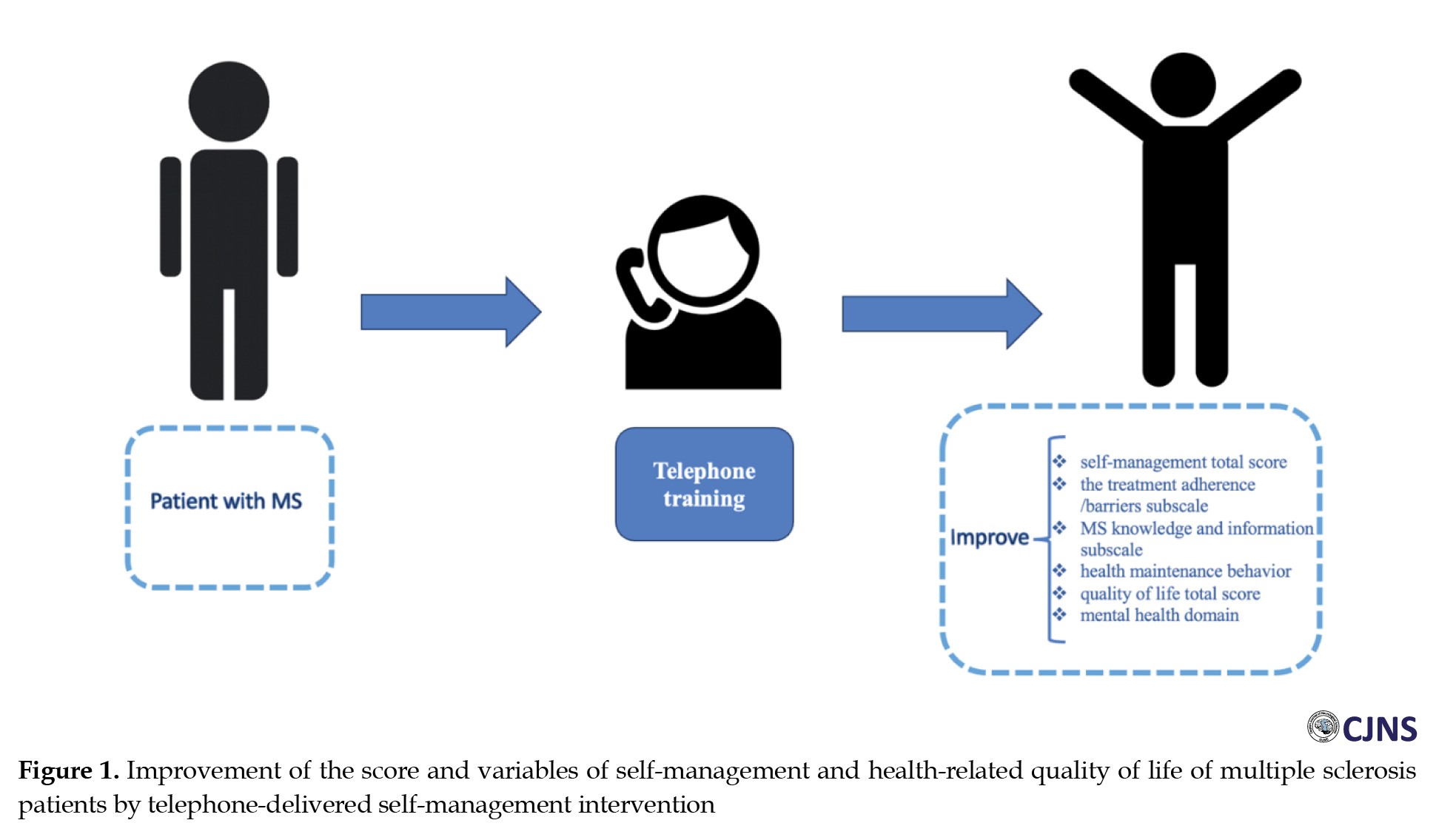
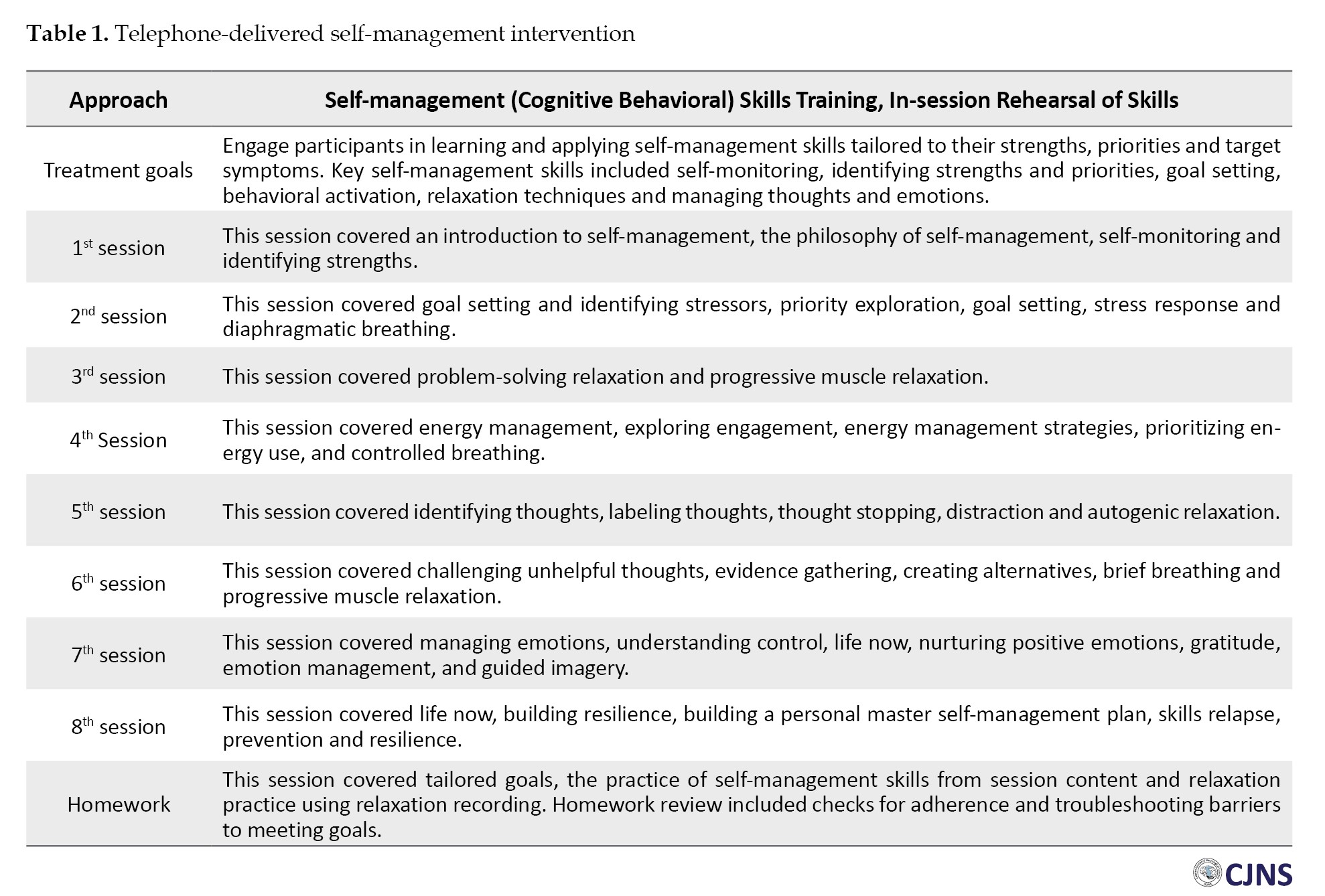
The Shapiro-Wilk test showed that the assumption of normality of all variables was established. Therefore, the repeated measures analysis of variance (ANOVA) is used to assess the variable’s change over time. The results in Table 3 showed that the intervention affects the self-management total score (P<0.001, F=12.29), TA/B (P=0.024, F=4.11), MSKI (P<0.001, F=8.11) and HMB (P=0.004, F=6.58).
It also influenced the quality-of-life total score (P=0.049, F=3.25) and mental health subscale (P=0.018, F=4.46). However, in other variables, there was no significant effect over time (Table 3, Figure 1). Table 4 presents the pairwise comparison of the three times assessments.
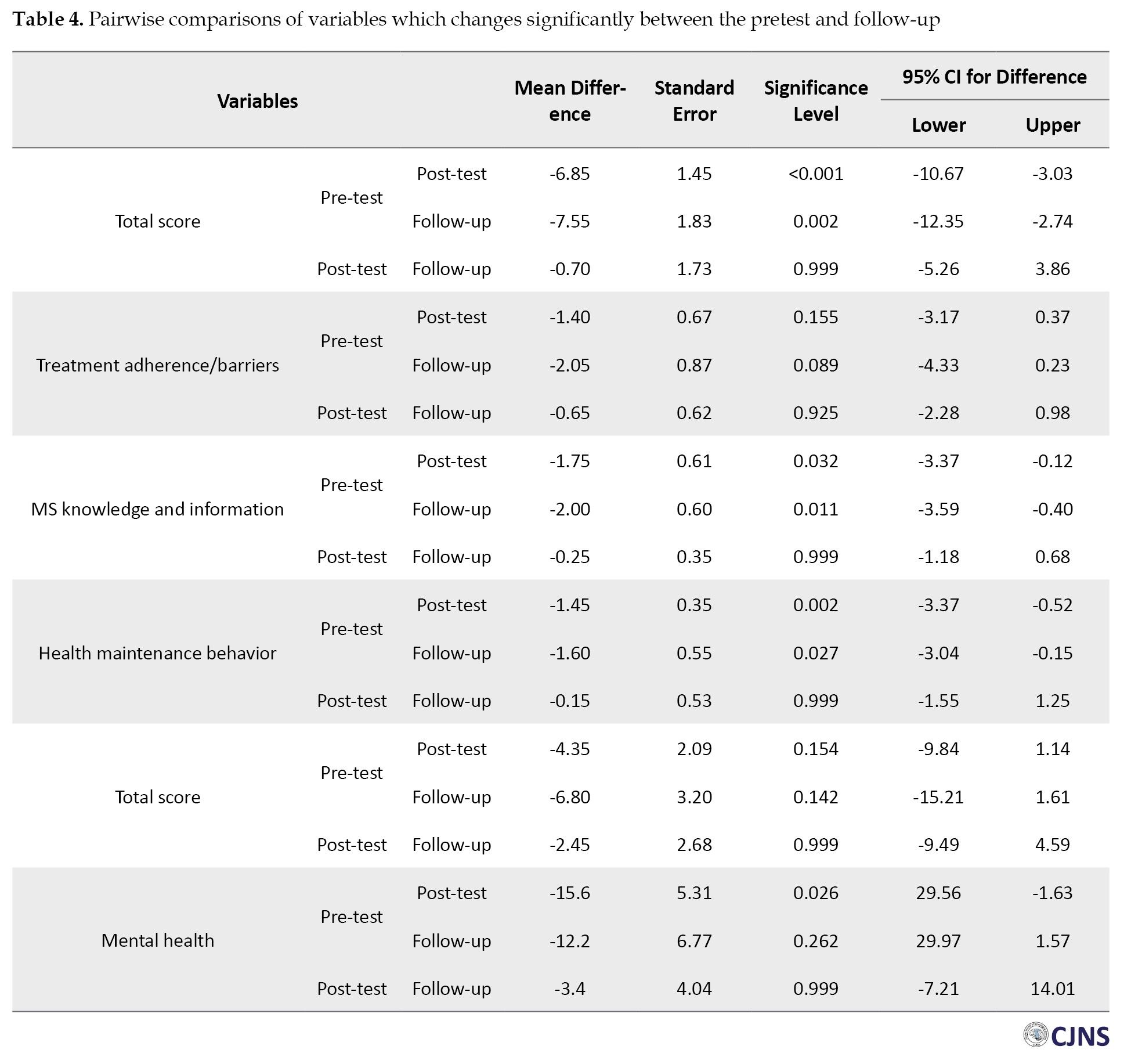
The results showed a significant increase in the self-management total score from the pre-test to the post-test (mean difference = 6.85, P=0.001), and it was stable from the post-test to the follow-up (mean difference=0.70, P=0.999). The “MSKI” subscale (mean difference=1.75, P=0.032) and “HMB” subscale (mean difference=1.45, P=0.002) increased significantly between pre-test and post-test and they were stable from the post-test to follow-up by the mean difference=0.250 (P=0.999) and mean difference=0.150 (P=0.999), respectively.
In the quality-of-life total score and all its subscales except the mental health subscale, there were no significant changes between the pre-test, the post-test, and the follow-up. There was a considerable increase in the “mental health” subscale between the pre-test and the post-test (mean difference=15.6, P=0.026). While it decreased after the post-test, the changes between the post-test and the follow-up were not statistically significant (Table 4).
Discussion
This study aims to determine the feasibility of telephone-delivered self-management intervention in patients with MS. The importance of our results is the significant impact of our intervention in increasing the total self-management score of MS patients. Our study’s results align with those of other studies, such as the double-blind study conducted by Bombardier et al. According to their study, motivational telephone interviews for 30 minutes a day for 6 months significantly increased the lifestyle indices (including physical and mental health improvements, etc.) [27].
According to the present study’s results, there was no significant positive or negative relationship between the healthcare provider relationship and communication in the pre-test, post-test and follow-up stages. In Deibel et al.’s study, MS participants felt that having more information and a strong relationship with healthcare professionals as tools of self-management skills are needed to address their physical and psychosocial challenges [28].
Regarding treatment adherence/barriers, the mean scores of the post-test and follow-up increased significantly in relation to the pre-test. This means that our intervention significantly increases patients’ treatment adherence. Our study’s results align with the study of Graziano et al. In their study, 82 patients with MS were investigated, and interventions were conducted in behavioral therapy sessions. Finally, after 6 months, treatment adherence was observed in these patients, demonstrating that psychotherapy sessions effectively increased treatment adherence/barrier [29].
No significant difference was observed in the average score of the social/family support area in our examined patients after the intervention. One of the reasons for this difference can be considered the poor socioeconomic status of patients and their families. However, Baharian et al.’s study showed that social support is related to self-management in MS patients. This concept should be applied in clinical practice when targeting and designing education, support, and care for MS patients. This notion can be used when designing education, support, and care for patients with MS in clinical practice [30].
Our study’s mean score of patients’ MSKI increased significantly from the pre-test to the post-test and follow-up. In this respect, our study aligns with many previous studies, including the study of Plow et al. [13] and Bombardier et al. [27]. This outcome illustrates the lack of patients’ knowledge about their illness and the benefit of a healthcare provider’s education and information provision to patients.
The present study’s mean score of health-maintaining behaviors increased positively and significantly from the pre-test to the post-test and follow-up. The results of Plow et al.’s study are consistent with the results of our research. According to the results of this study, after training by the therapist for 6 months, performing sports activities in patients as a HMB has had a positive and significant effect [13]. In addition, Bombardier et al. concluded in their study that there was an inverse and significant relationship between motivational interviews and reducing alcohol consumption in patients [27].
In the present study, the mean score of the total quality of life showed a positive and significant increase. These results align with the studies of Bombardier et al. and Finlayson et al. According to the results mentioned in the study of Finlayson et al. there is a significant relationship between motivational interviewing and controlling the level of fatigue and patients’ quality of life [1 , 31]. In the study by Proctor et al. telephone-based psychotherapy positively improves depression, fatigue, quality of life, MS symptoms, physical activity, and medication adherence in the short-term [32]. Also, in a study by Moss-Morris et al. Internet-based cognitive behavioral therapy self-management is a promising, acceptable and cost-effective approach for treating MS fatigue and improving broader outcomes such as distress [33].
According to the results of our study, the average score in the physical performance area did not increase significantly. This issue is inconsistent with the results of past studies. The study conducted by Plow et al. demonstrated that group conference calls followed by appropriate phone calls have a small statistically significant effect on promoting physical activity and reducing fatigue in MS patients [13]. The reason for this difference could be the small sample size of the present study compared to other studies [23, 34] and perhaps the length of the questions in the questionnaire was associated with the decrease in accuracy of answering the questions by the patients. As fatigue is a non-specific symptom and affects various dimensions of patients’ daily lives, it should be addressed through a comprehensive approach that targets both patient behaviors and their emotional and mental attitudes toward fatigue. However, the clinical correlation of treatment effects, specifically the relationship with patients’ daily functioning, has been unclear and likely requires longer-term interventions exceeding 6 months. According to the results of this investigation, the average score of the bodily pain subscale increased in the post-test group compared to the pre-test, but it decreased in the follow-up. Overall, these changes were not significant. This study is comparable to Ehde et al.’s in lowering the average score of bodily pain [35]. The average range of vitality scores among patients in this study has increased over time. However, this increase was not significant. It is in line with many studies, such as the study of Ehde et al. and Graziano et al. In both mentioned above studies, cognitive-behavioral therapy caused a significant reduction in depression scores [29, 35]. Also, the results of our study indicate a positive and significant increase in the mental health score. This result aligns with other studies, such as Ehde et al.’s and Turner et al.’s studies [35, 36].
Conclusion
In this study, telephone-delivered self-management intervention in patients with MS has positive effectiveness in many areas under investigation. The mean score in self-management, treatment adherence/barriers, knowledge and information about the disease, HMBs, quality of life, vitality and mental health increased significantly in the follow-up compared to the pre-test. Therefore, this intervention can be used to improve the quality of life of these patients. The follow-up of patients during and after the treatment period is of particular importance.
Study limitations
Despite the registration of many patients with MS in the Rasht MS Association, only a small number of patients are connected with this association. So, the weak point of our study is its small sample size. Therefore, it is recommended that further studies be conducted on a broader scale and with a larger sample size.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.508).
Funding
This research was extracted from post-doctoral thesis of Fatemeh Younesi Rostami, approved by Guilan University of Medical Sciences (Registration No.: 1257).
Authors contributions
Conceptualization: Mozaffar Hosseininezhad and Sajjad Saadat; Methodology: Sajjad Saadat and Roghaye Zare; Investigation: Fatemeh Younesi Rostami, Masoumeh Qanbary Joopish and Alia Saberi; Writing the original draft: Ali Bonyad; Writing, review and editing: Alia Saberi; Supervision: Mozaffar Hosseininezhad, Sajjad Saadat and Alia Saberi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank Poursina Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran, for cooperating in this project.
References
Multiple sclerosis (MS) is an autoimmune disease of the central nervous system which is chronic and degenerative. It affects approximately 2 million people worldwide [1] and is the second leading cause of non-traumatic disability in young people [2]. MS typically emerges in adults aged 20-40, with patients having a regular life expectancy [3]. It is more prevalent in women, especially in the white population. Key symptoms include cognitive and movement issues, sensory deficits, visual problems, balance impairments, fatigue, and pain [4, 5]. MS patients face daily physical, mental, and emotional challenges [1, 5]. Psychological issues like anxiety and mood disorders are common [6, 7], leading to significant disability in some cases [8]. Consequently, it impacts the quality of life [9]. While incurable, lifelong symptom management is crucial, requiring active self-management for treatment adherence, decision-making, self-care, and well-being [10-14].
Self-management in chronic diseases involves acquiring skills to lead a fulfilling life despite illness challenges, leading to improved quality of life, symptom reduction, and cost savings [11]. These strategies enhance understanding, knowledge, diet and well-being, benefiting health outcomes [15, 16]. There is significant evidence of health benefits after self-management interventions in chronic and long-term diseases such as diabetes, arthritis, and heart diseases [17, 18]. Individuals with chronic illnesses take charge of treatment adherence, exercise, social engagement, and healthcare choices, highlighting its pivotal role in addressing the condition and its secondary effects [17-19].
Telephone-based interventions improve the quality of life in people with MS by promoting physical activities like walking and exercise, leading to enhanced mental and physical performance [20, 21]. Research into the effectiveness and design of telephone interventions is vital due to knowledge gaps. While some studies indicate that interventions focusing on physical activity and self-management can moderately enhance healthy behaviors and quality of life, a lack of comprehensive understanding persists. Despite its acknowledged importance in chronic disease management, the limited research on self-management among people with MS accentuates the need for this research. Addressing these gaps can bridge evidence divides and potentially provide impactful strategies for promoting healthy behaviors, especially among MS patients.
Materials and Methods
This quasi-experimental study involved 20 MS patients selected from registered patients in the nationwide MS registry of Iran (NMSRI), Guilan, in 2020. Individuals were selected through a public call using judgmental sampling. The sample size was calculated based on the factor repeated measure approach’s formula with a 95% confidence level, 85% power and 0.33 effect size. According to the previous study [22] information, the G*Power software, version 3.1.9.4 calculated the sample size as 20. The study employed a pre-test-post-test with a two-month follow-up design. Inclusion criteria were MS diagnosis per McDonald’s 2017 criteria, age 20-55 and willingness to participate. The exclusion criteria were incomplete training and disagreement to participate in the study. A pre-test was taken before the intervention, and then training was implemented online and via telephone. The post-test was conducted immediately after the intervention and two months later using an online survey.
Study intervention
The educational program was a telephone-delivered self-management intervention and a standard intervention developed by Ehde et al. [23], including 8 weekly sessions of 45 to 60 minutes by phone with MS patients in a group setting. Self-management intervention is over the phone (audio, video and educational files and phone calls), including evidence-based cognitive-behavioral and psychological strategies to help participants manage pain, depression, and fatigue in everyday life. The therapist communicated with the participants on a scheduled basis to discuss the educational implications with them. Also, the academic content of each session was provided to the participants in the form of an electronic booklet, audio, and educational videos so that they could refer to them if they wanted to understand more about the training. Training sessions aimed at familiarizing self-management, goal setting, identifying stressful factors, problem-solving and relaxation training, energy management, working with thoughts, emotion management, and building resilience (Table 1).
Study tools
The MS self-management scale–revised (MSSM-R)
Bishop and Frein developed this self-report tool and has 24 items and 5 subscales: Healthcare provider relationship and communication, treatment adherence/barriers (TA/B), social/family support (S/FS) (three items: 6, 10, 13), MS knowledge and information (MSKI) and health maintenance behavior (HMB). The scoring method of the questionnaire was based on a 5-point Likert scale (completely disagree=1 to completely agree=5). The higher score indicates a high level of self-management; questions 21, 23 and 24 are scored in reverse. The range of changes in this tool is between 24 and 120 [24]. The psychometric assessment of the Persian-translated version of this scale was done by Saadat et al. The results showed that this scale has acceptable face and content validity. The confirmatory factor analysis showed that 24 items had acceptable factor loadings in 5 subscales. The internal consistency results of this scale were calculated by the Cronbach α method and the test-re-test reliability for the test subscales was reported between 0.70 and 0.89 [15].
The short form health survey (SF-36)
This questionnaire aims to assess the physical and mental health state. It has 36 items that evaluate 8 different subscales of health (physical functioning [PF], role physical [RP], bodily pain [BP], general health [GH], vitality [VT], social functioning [SF], role emotional [RE] and mental health [MH]). A lower score means a lower quality of life. In a study, the internal consistency of the first version of this questionnaire was between 0.72 and 0.94 with the Cronbach α [25]. Also, in Iran, Motamed et al. in Shiraz checked its reliability and estimated the Cronbach’s α of the Persian questionnaire to be 0.87 [26].
Statistical analysis
Data were analyzed using IBM SPSS software, version 26. Data were reported by frequency (percentage) or Mean±SD. The Shapiro-Wilk test was used to determine the normality of the distribution. A repeated measure analysis examined the changes in the variables from the pre-test to the follow-up.
Results
Initially, 60 patients referred to the MS Society of Guilan, Iran, participated in this study. Data gathering and intervention continued to reach the determined sample size. Finally, 20 patients completed the sessions, post-test, and follow-up evaluation. The descriptive findings of the study are reported in Table 2.
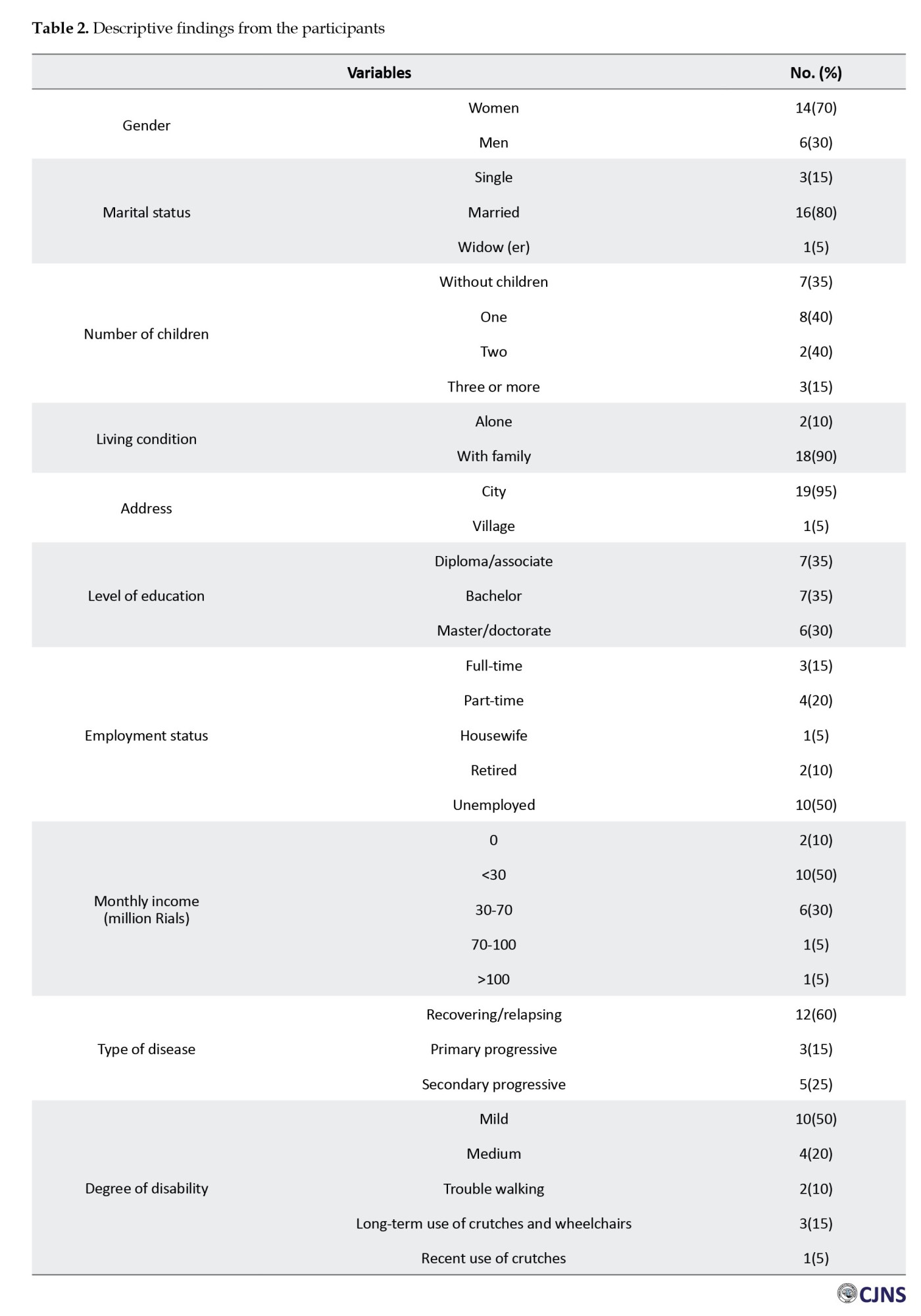
In this study, 20 individuals with MS participated until the end of the intervention and cooperated in various assessment stages. Their demographic information is presented in Table 2.
The Shapiro-Wilk test showed that the assumption of normality of all variables was established. Therefore, the repeated measures analysis of variance (ANOVA) is used to assess the variable’s change over time. The results in Table 3 showed that the intervention affects the self-management total score (P<0.001, F=12.29), TA/B (P=0.024, F=4.11), MSKI (P<0.001, F=8.11) and HMB (P=0.004, F=6.58).
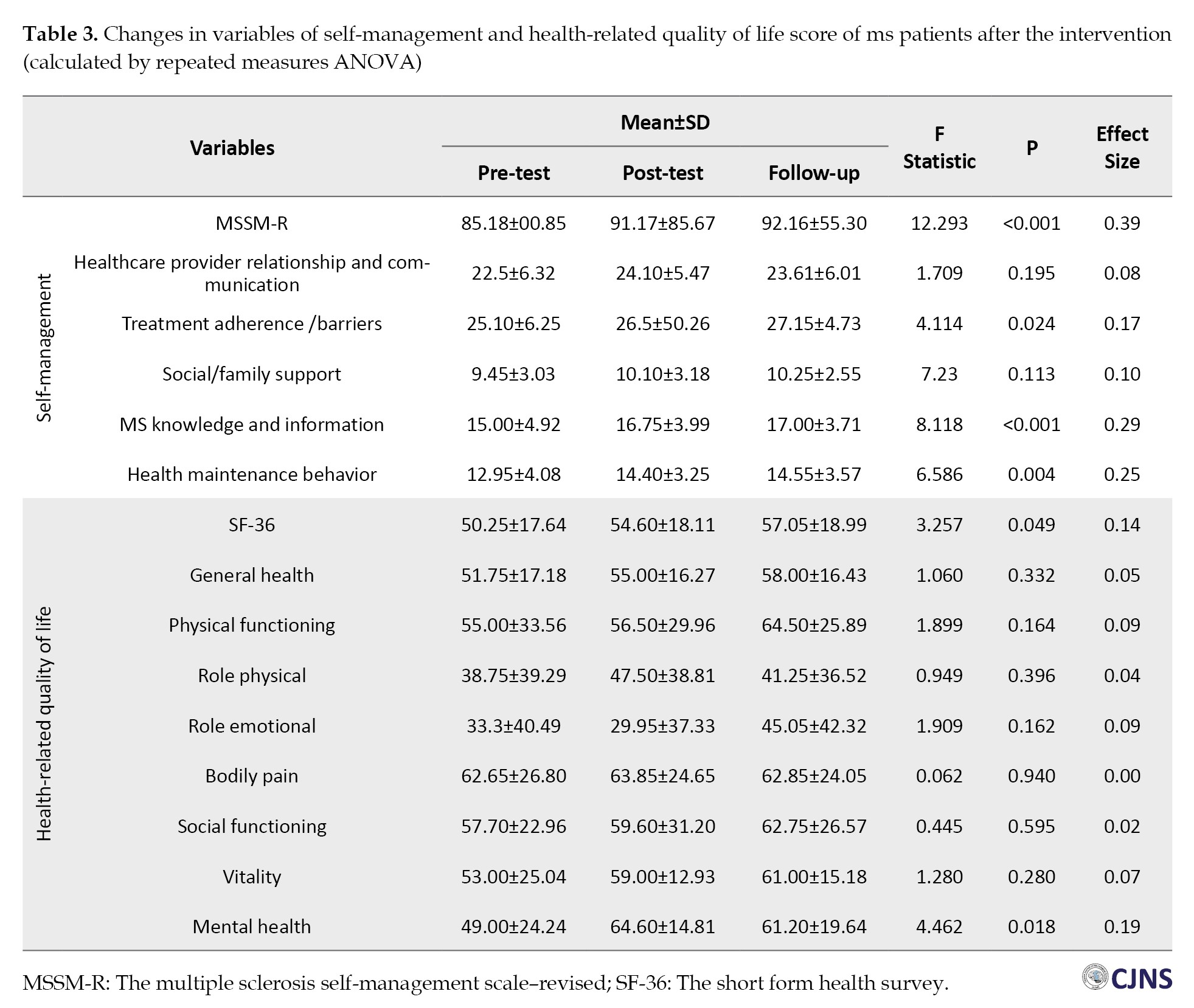
It also influenced the quality-of-life total score (P=0.049, F=3.25) and mental health subscale (P=0.018, F=4.46). However, in other variables, there was no significant effect over time (Table 3, Figure 1). Table 4 presents the pairwise comparison of the three times assessments.
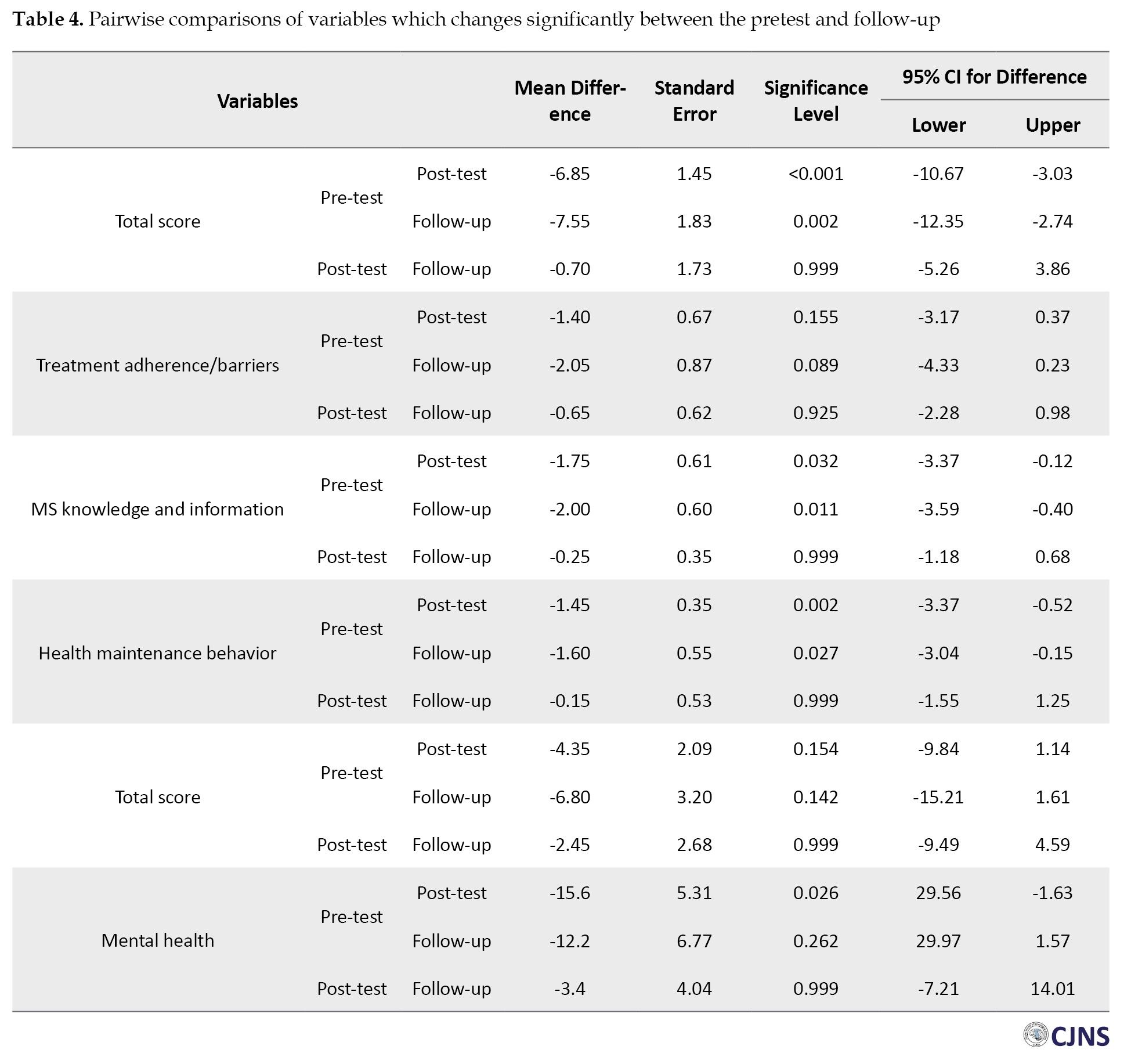
The results showed a significant increase in the self-management total score from the pre-test to the post-test (mean difference = 6.85, P=0.001), and it was stable from the post-test to the follow-up (mean difference=0.70, P=0.999). The “MSKI” subscale (mean difference=1.75, P=0.032) and “HMB” subscale (mean difference=1.45, P=0.002) increased significantly between pre-test and post-test and they were stable from the post-test to follow-up by the mean difference=0.250 (P=0.999) and mean difference=0.150 (P=0.999), respectively.
In the quality-of-life total score and all its subscales except the mental health subscale, there were no significant changes between the pre-test, the post-test, and the follow-up. There was a considerable increase in the “mental health” subscale between the pre-test and the post-test (mean difference=15.6, P=0.026). While it decreased after the post-test, the changes between the post-test and the follow-up were not statistically significant (Table 4).
Discussion
This study aims to determine the feasibility of telephone-delivered self-management intervention in patients with MS. The importance of our results is the significant impact of our intervention in increasing the total self-management score of MS patients. Our study’s results align with those of other studies, such as the double-blind study conducted by Bombardier et al. According to their study, motivational telephone interviews for 30 minutes a day for 6 months significantly increased the lifestyle indices (including physical and mental health improvements, etc.) [27].
According to the present study’s results, there was no significant positive or negative relationship between the healthcare provider relationship and communication in the pre-test, post-test and follow-up stages. In Deibel et al.’s study, MS participants felt that having more information and a strong relationship with healthcare professionals as tools of self-management skills are needed to address their physical and psychosocial challenges [28].
Regarding treatment adherence/barriers, the mean scores of the post-test and follow-up increased significantly in relation to the pre-test. This means that our intervention significantly increases patients’ treatment adherence. Our study’s results align with the study of Graziano et al. In their study, 82 patients with MS were investigated, and interventions were conducted in behavioral therapy sessions. Finally, after 6 months, treatment adherence was observed in these patients, demonstrating that psychotherapy sessions effectively increased treatment adherence/barrier [29].
No significant difference was observed in the average score of the social/family support area in our examined patients after the intervention. One of the reasons for this difference can be considered the poor socioeconomic status of patients and their families. However, Baharian et al.’s study showed that social support is related to self-management in MS patients. This concept should be applied in clinical practice when targeting and designing education, support, and care for MS patients. This notion can be used when designing education, support, and care for patients with MS in clinical practice [30].
Our study’s mean score of patients’ MSKI increased significantly from the pre-test to the post-test and follow-up. In this respect, our study aligns with many previous studies, including the study of Plow et al. [13] and Bombardier et al. [27]. This outcome illustrates the lack of patients’ knowledge about their illness and the benefit of a healthcare provider’s education and information provision to patients.
The present study’s mean score of health-maintaining behaviors increased positively and significantly from the pre-test to the post-test and follow-up. The results of Plow et al.’s study are consistent with the results of our research. According to the results of this study, after training by the therapist for 6 months, performing sports activities in patients as a HMB has had a positive and significant effect [13]. In addition, Bombardier et al. concluded in their study that there was an inverse and significant relationship between motivational interviews and reducing alcohol consumption in patients [27].
In the present study, the mean score of the total quality of life showed a positive and significant increase. These results align with the studies of Bombardier et al. and Finlayson et al. According to the results mentioned in the study of Finlayson et al. there is a significant relationship between motivational interviewing and controlling the level of fatigue and patients’ quality of life [1 , 31]. In the study by Proctor et al. telephone-based psychotherapy positively improves depression, fatigue, quality of life, MS symptoms, physical activity, and medication adherence in the short-term [32]. Also, in a study by Moss-Morris et al. Internet-based cognitive behavioral therapy self-management is a promising, acceptable and cost-effective approach for treating MS fatigue and improving broader outcomes such as distress [33].
According to the results of our study, the average score in the physical performance area did not increase significantly. This issue is inconsistent with the results of past studies. The study conducted by Plow et al. demonstrated that group conference calls followed by appropriate phone calls have a small statistically significant effect on promoting physical activity and reducing fatigue in MS patients [13]. The reason for this difference could be the small sample size of the present study compared to other studies [23, 34] and perhaps the length of the questions in the questionnaire was associated with the decrease in accuracy of answering the questions by the patients. As fatigue is a non-specific symptom and affects various dimensions of patients’ daily lives, it should be addressed through a comprehensive approach that targets both patient behaviors and their emotional and mental attitudes toward fatigue. However, the clinical correlation of treatment effects, specifically the relationship with patients’ daily functioning, has been unclear and likely requires longer-term interventions exceeding 6 months. According to the results of this investigation, the average score of the bodily pain subscale increased in the post-test group compared to the pre-test, but it decreased in the follow-up. Overall, these changes were not significant. This study is comparable to Ehde et al.’s in lowering the average score of bodily pain [35]. The average range of vitality scores among patients in this study has increased over time. However, this increase was not significant. It is in line with many studies, such as the study of Ehde et al. and Graziano et al. In both mentioned above studies, cognitive-behavioral therapy caused a significant reduction in depression scores [29, 35]. Also, the results of our study indicate a positive and significant increase in the mental health score. This result aligns with other studies, such as Ehde et al.’s and Turner et al.’s studies [35, 36].
Conclusion
In this study, telephone-delivered self-management intervention in patients with MS has positive effectiveness in many areas under investigation. The mean score in self-management, treatment adherence/barriers, knowledge and information about the disease, HMBs, quality of life, vitality and mental health increased significantly in the follow-up compared to the pre-test. Therefore, this intervention can be used to improve the quality of life of these patients. The follow-up of patients during and after the treatment period is of particular importance.
Study limitations
Despite the registration of many patients with MS in the Rasht MS Association, only a small number of patients are connected with this association. So, the weak point of our study is its small sample size. Therefore, it is recommended that further studies be conducted on a broader scale and with a larger sample size.
Ethical Considerations
Compliance with ethical guidelines
The research was approved by the Research Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.508).
Funding
This research was extracted from post-doctoral thesis of Fatemeh Younesi Rostami, approved by Guilan University of Medical Sciences (Registration No.: 1257).
Authors contributions
Conceptualization: Mozaffar Hosseininezhad and Sajjad Saadat; Methodology: Sajjad Saadat and Roghaye Zare; Investigation: Fatemeh Younesi Rostami, Masoumeh Qanbary Joopish and Alia Saberi; Writing the original draft: Ali Bonyad; Writing, review and editing: Alia Saberi; Supervision: Mozaffar Hosseininezhad, Sajjad Saadat and Alia Saberi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank Poursina Clinical Research Development Unit, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran, for cooperating in this project.
References
- Kidd T, Carey N, Mold F, Westwood S, Miklaucich M, Konstantara E, et al. A systematic review of the effectiveness of self-management interventions in people with multiple sclerosis at improving depression, anxiety and quality of life. Plos One. 2017; 12(10):e0185931. [DOI:10.1371/journal.pone.0185931] [PMID]
- Hapfelmeier A, Gasperi C, Donnachie E, Hemmer B. A large case-control study on vaccination as risk factor for multiple sclerosis. Neurology. 2019; 93(9):e908-16. [DOI:10.1212/WNL.0000000000008012] [PMID]
- Dehghani Bidgoli T, Mahdian H, Shakiba A. The effectiveness of emotion regulation training and acceptance and commitment therapy (ACT) on psychological pain in patients with multiple sclerosis (MS). J Res Psychopathol. 2022; 3(7):35-46. [DOI:10.22098/jrp.2022.10367.1068]
- Saberi A, Ashkan M, Hatamian H, Ashraf A, Rad EH, Bakhshi A,et al. Migraine headache in multiple sclerosis. is more frequent among MS patients?. Romann J Neurol. 2023; 22(1):54-7. [DOI:10.37897/RJN.2023.1.9]
- Saberi A, Hatamian HR, Nemati S, Banan R. Hearing statement in multiple sclerosis: A case control study using auditory brainstem responses and otoacoustic emissions. Acta Med Iran. 2012; 50(10):679-83. [PMID]
- Salhofer-Polanyi S, Friedrich F, Löffler S, Rommer PS, Gleiss A, Engelmaier R, et al. Health-related quality of life in multiple sclerosis: Temperament outweighs EDSS. BMC Psychiatry. 2018; 18(1):143. [DOI:10.1186/s12888-018-1719-6] [PMID]
- Nazari N, Sadeghi M, Ghadampour E, Mirzaeefar D. Transdiagnostic treatment of emotional disorders in people with multiple sclerosis: Randomized controlled trial. BMC Psychol. 2020; 8(1):114. [DOI:10.1186/s40359-020-00480-8] [PMID]
- Kamm CP, Uitdehaag BM, Polman CH. Multiple sclerosis: Current knowledge and future outlook. Eur Neurol. 2014; 72(3-4):132-41. [DOI:10.1159/000360528] [PMID]
- Wilski M, Gabryelski J, Brola W, Tomasz T. Health-related quality of life in multiple sclerosis: Links to acceptance, coping strategies and disease severity. Disabil Health J. 2019 Oct; 12(4):608-14. [DOI:10.1016/j.dhjo.2019.06.003] [PMID]
- Tomczak M, Kleka P, Wilski M. Psychometric properties of the polish version of the multiple sclerosis self-management scale - revised. Disabil Rehabil. 2022; 44(10):2113-22. [DOI:10.1080/09638288.2020.1822933] [PMID]
- Wilski M, Brola W, Łuniewska M, Tomczak M. The perceived impact of multiple sclerosis and self-management: The mediating role of coping strategies. Plos One. 2021; 16(3):e0248135. [DOI:10.1371/journal.pone.0248135] [PMID]
- Mokhberdezfuli M, Ayatollahi H, Naser Moghadasi A. A smartphone-based application for self-management in multiple sclerosis. J Healthc Eng. 2021; 2021:6749951. [DOI:10.1155/2021/6749951] [PMID]
- Plow M, Finlayson M, Liu J, Motl RW, Bethoux F, Sattar A. Randomized controlled trial of a telephone-delivered physical activity and fatigue self-management interventions in adults with multiple sclerosis. Arch Phys Med Rehabil. 2019; 100(11):2006-14. [DOI:10.1016/j.apmr.2019.04.022] [PMID]
- Bishop ML, Frain MP, Li J, Chiu CY, McDaniels B, Kim BJ. The multiple sclerosis self-management scale-2: Evaluation of an updated scale. J Appl Rehabil Couns. 2019; 50(3):210-26. [DOI:10.1891/0047-2220.50.3.210]
- Saadat S, Kajbaf MB, Kalantari M, Hosseininezhad M. The Multiple sclerosis self-management scale-revised (MSSM-R): Persian version and psychometric analysis. Int J MS Care. 2020; 22(1):37-42. [DOI:10.7224/1537-2073.2018-090] [PMID]
- Wilski M, Kocur P, Brola W, Tasiemski T. Psychological factors associated with self-management in multiple sclerosis. Acta Neurol Scand. 2020; 142(1):50-57. [DOI:10.1111/ane.13236] [PMID]
- Eghbali BB, Saadat S, Hasanzadeh K, Pourramzani A, Khatami SS, Saberi A, et al. Relationship between self-compassion and psychological well-being with the mediating role of resilience in people with multiple sclerosis. Postep Psychiatr Neurol. 2022; 31(2):43-51. [DOI:10.5114/ppn.2022.117999] [PMID]
- Sua YS, Jiang Y, Thompson DR, Wang W. Effectiveness of mobile phone-based self-management interventions for medication adherence and change in blood pressure in patients with coronary heart disease: A systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2020; 19(3):192-200. [DOI:10.1177/1474515119895678] [PMID]
- Pétrin J, Donnelly C, McColl MA, Finlayson M. Is it worth it?: The experiences of persons with multiple sclerosis as they access health care to manage their condition. Health Expect. 2020; 23(5):1269-79. [DOI:10.1111/hex.13109] [PMID]
- Motl RW, Cutter G, Bamman MM, Brown CJ, Rinker J. The importance and opportunity for healthy aging through lifestyle, behavior medicine among older adults with multiple sclerosis: The case based on physical activity. Curr Treat Options Neurol. 2021; 23(8):23. [DOI:10.1007/s11940-021-00680-6]
- Meek C, Moghaddam NG, Evangelou N, Oates LL, Topcu G, Allen C, et al. Acceptance-based telephone support around the time of transition to secondary progressive multiple sclerosis: A feasibility randomised controlled trial. J Contextual Behav Sci. 2021; 21:158-70. [DOI:10.1016/j.jcbs.2021.07.001]
- Saadat S, Kalantari M, Kajbaf MB, Hosseininezhad M. [The effect of a psychological training program on self-management in women with multiple sclerosis (Persian)]. Razi J Med Sci. 2019; 26(7):88-98. [Link]
- Ehde DM, Elzea JL, Verrall AM, Gibbons LE, Smith AE, Amtmann D. Efficacy of a telephone-delivered self-management intervention for persons with multiple sclerosis: a randomized controlled trial with a one-year follow-up. Arch Phys Med Rehabil. 2015; 96(11):1945-58.e2. [DOI:10.1016/j.apmr.2015.07.015] [PMID]
- Bishop M, Frain MP. The multiple sclerosis self-management scale: Revision and psychometric analysis. Rehabil Psychol. 2011; 56(2):150-9. [DOI:10.1037/a0023679] [PMID]
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30(6):473-83. [DOI:10.1097/00005650-199206000-00002] [PMID]
- Motamed N, Ayatollahi SA, Zare N, Sadeghi Hasanabadi A. Reliability and validity of SF-36 questionnaire in the staff of Shiraz Medical School, 2001. J Adv Med Biomed Res. 2002; 10(38):38-46. [Link]
- Bombardier CH, Cunniffe M, Wadhwani R, Gibbons LE, Blake KD, Kraft GH. The efficacy of telephone counseling for health promotion in people with multiple sclerosis: A randomized controlled trial. Arch Phys Med Rehabil. 2008; 89(10):1849-56. [DOI:10.1016/j.apmr.2008.03.021.] [PMID]
- Deibel F, Edwards M, Edwards A. Patients’, carers’ and providers’ experiences and requirements for support in self-management of multiple sclerosis: A qualitative study. Eur J Person Cent Healthc. 2013; 1(2):457-67. [DOI:10.5750/ejpch.v1i2.687]
- Graziano F, Calandri E, Borghi M, Bonino S. The effects of a group-based cognitive behavioral therapy on people with multiple sclerosis: A randomized controlled trial. Clin Rehabil. 2014; 28(3):264-74. [DOI:10.1177/0269215513501525.] [PMID]
- Baharian E, Abolhassani S, Alijani M. Association between perceived social support and self-management in people with multiple sclerosis: A cross-sectional study. Asian J So Health Behav. 2023; 6(1):1-6. [DOI:10.4103/shb.shb_188_22]
- Finlayson M, Preissner K, Cho C, Plow M. Randomized trial of a teleconference-delivered fatigue management program for people with multiple sclerosis. Mult Scler. 2011 Sep;17(9):1130-40. [DOI:10.1177/1352458511404272] [PMID]
- Proctor BJ, Moghaddam N, Vogt W, Das Nair R. Telephone psychotherapy in multiple sclerosis: A systematic review and meta-analysis. Rehab Psychol. 2018; 63(1):16. [DOI:10.1037/rep0000182] [PMID]
- Moss-Morris R, McCrone P, Yardley L, van Kessel K, Wills G, Dennison L. A pilot randomised controlled trial of an Internet-based cognitive behavioural therapy self-management programme (MS Invigor8) for multiple sclerosis fatigue. Behav Res Ther. 2012; 50(6):415-21. [DOI:10.1016/j.brat.2012.03.001] [PMID]
- Plow M, Packer T, Mathiowetz VG, Preissner K, Ghahari S, Sattar A, et al. REFRESH protocol: A non-inferiority randomised clinical trial comparing internet and teleconference to in-person 'Managing Fatigue' interventions on the impact of fatigue among persons with multiple sclerosis. BMJ Open. 2020; 10(8):e035470. [DOI:10.1136/bmjopen-2019-035470] [PMID]
- Ehde DM, Arewasikporn A, Alschuler KN, Hughes AJ, Turner AP. Moderators of treatment outcomes after telehealth self-management and education in adults with multiple sclerosis: A secondary analysis of a randomized controlled trial. Arch Phys Med Rehabil. 2018; 99(7):1265-72. [DOI:10.1016/j.apmr.2017.12.012] [PMID]
- Turner AP, Hartoonian N, Sloan AP, Benich M, Kivlahan DR, Hughes C, et al. Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol. 2016; 84(4):297-309. [DOI:10.1037/ccp0000086] [PMID]
Type of Study: Research |
Subject:
General
Received: 2024/01/21 | Accepted: 2024/03/15 | Published: 2025/01/1
Received: 2024/01/21 | Accepted: 2024/03/15 | Published: 2025/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |