Fri, Jan 30, 2026
Volume 11, Issue 3 (Summer 2025)
Caspian J Neurol Sci 2025, 11(3): 230-236 |
Back to browse issues page
Ethics code: IR.SSU.MEDICINE.REC.1400.222
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Edalatkhah R, Rasoulizadeh Z, Mohammadi M, Aflatoonian M. Sleep Disorders in Children With Celiac Disease: An Analytic Cross-sectional Study. Caspian J Neurol Sci 2025; 11 (3) :230-236
URL: http://cjns.gums.ac.ir/article-1-751-en.html
URL: http://cjns.gums.ac.ir/article-1-751-en.html
1- Hematology and Oncology Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. & Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,maryammohammadi1375@gmail.com
2- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Full-Text [PDF 1013 kb]
(380 Downloads)
| Abstract (HTML) (762 Views)
Full-Text: (180 Views)
Introduction
Celiac disease (CD) is a complex autoimmune disorder with a genetic predisposition triggered by the ingestion of gluten-containing grains such as wheat [1]. The disease presents many gastrointestinal and extra-gastrointestinal symptoms, including diarrhea, bloating, and steatorrhea [2]. While the global prevalence of CD is estimated to be between 1% and 2%, some studies suggest that the actual numbers could be higher [2, 3].
Globally, approximately 1% of the population is affected by CD, with varying prevalence rates in different countries such as New Zealand, Argentina, Hungary, Sweden, Finland, India, and Egypt [4]. Western Europe region reports the highest prevalence, and Middle Eastern countries like Iran also show comparable rates, with about 1% of the general population affected [5].
CD often manifests in early childhood, particularly when children are first introduced to gluten-containing foods [6]. The only effective treatment for managing the disease’s multifaceted clinical, histological, and serological aspects is a lifelong adherence to a gluten-free diet [7]. Although primarily affecting the intestine, CD is a systemic disease affecting multiple tissues, including the nervous system [8]. Sleep, a vital component of children’s physical and mental well-being, is often compromised in chronic medical conditions, including autoimmune and atopic diseases [9, 10]. Conditions such as asthma, cystic fibrosis, sickle cell anemia, gastroesophageal reflux disease, neuromuscular disorders, and chromosomal abnormalities are associated with poor sleep quality [11].
In light of the significance of sleep in children’s overall health and its frequent disturbance in autoimmune and gastrointestinal diseases, this study aims to investigate the association between sleep disorders and tissue transglutaminase antibody (TTG Ab) levels in pediatric patients with CD.
Materials and Methods
Study design and participants
This analytic cross-sectional study was conducted from 2016 to 2022, focusing on pediatric patients referred at Shahid Sadoughi Hospital’s Gastroenterology Clinic in Yazd, Iran. The research population consists of all children diagnosed with CD whose records were registered in the Yazd celiac system during this period. The diagnosis of CD was based on the presence of IgA/IgG antibodies (TTG-IgA/IgG) in the serum and the results of duodenal biopsies. Testing was performed on all patients with TTG-IgA deficiency to rule out the possibility of selective IgA deficiency. Using Marsh classification, biopsies from the duodenum and bulbous were analyzed, and CD diagnosis was made [12]. A total of 55 records were analyzed after data screening out of 202 individuals registered in the system, 80 of whom were under 16. The inclusion criteria were age between 1 to 16 years, diagnosis of CD, and undergoing gluten-free diet therapy. The exclusion criteria included age older than 16 or younger than 1, history of any disease such as diabetes, malignancies, metabolic disorders, psychiatric disorders, gastrointestinal disorders, and history of medication use for mental disorders or chronic disorders.
Data collection
Data were collected after obtaining ethical clearance and identifying patients who met the inclusion criteria from the Yazd celiac system records. An online questionnaire was sent to the participants, who were requested to answer carefully. Two types of questionnaires were used: 1) Demographic information questionnaire including relevant information such as age, gender, age at diagnosis, the serum level of TTG Ab, medication use, gluten-free diet duration, and parents’ education, and 2) Children’s sleep habits questionnaire (CSHQ). This study used the Persian version of parent-reported CSHQ. It consists of 45 questions, of which only 33 are considered for scoring. Eight subscales of CSHQ were measured: Bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night waking, parasomnias, daytime sleepiness, and sleep-disordered breathing. Each item is scored between 1 and 3 (“rarely” to “usually”), except for specific reverse-scored items. The score range is 33-99. Sleep disturbances are defined by a score of 41 [13]. Fallahzadeh et al. evaluated the validity and reliability of the Persian version of CSHQ using the Cronbach α coefficient. A Cronbach α coefficient of 0.80 was calculated for the entire questionnaire. There was a range of convergence validity of 0.4 to 0.86 [13].
Statistical analysis
The collected data were systematically imported into SPSS software, version 26 (SPSS Inc., Chicago, IL, USA). for analysis according to the research objectives. Descriptive statistics were employed, including mean and standard deviation for quantitative data and frequency and percentage for qualitative data. The chi-square and Fisher exact tests were used to compare frequency distributions. A t-test was employed to compare the means. The normality of the data was tested using the Kolmogorov-Smirnov test, and a P<0.05 was considered statistically significant. The sample size was calculated using the formula for comparing means, considering alpha=0.05, beta=0.2, and a TTG level difference of 0.1 between individuals with and without sleep disorder. Accordingly, the sample size was estimated at 48.
Results
Demographics and baseline characteristics
The study involved participants with a mean age of 10.70±2.6 years and a mean age at diagnosis of 6.09±2.62 years. Of 55 participants, 33(60%) were female and 22(40%) were male. The latest TTG results revealed that 20 children (36.4%) had values below 10, while 35(63.6%) had values above 10. Parental education was diverse: 30(54.5%) of fathers and 22(40%) of mothers had education below diploma level; 18(32.7%) of fathers and 24(43.6%) of mothers had a diploma; and 7(12.7%) of fathers and 8(14.5%) of mothers had university-level education (Table 1).
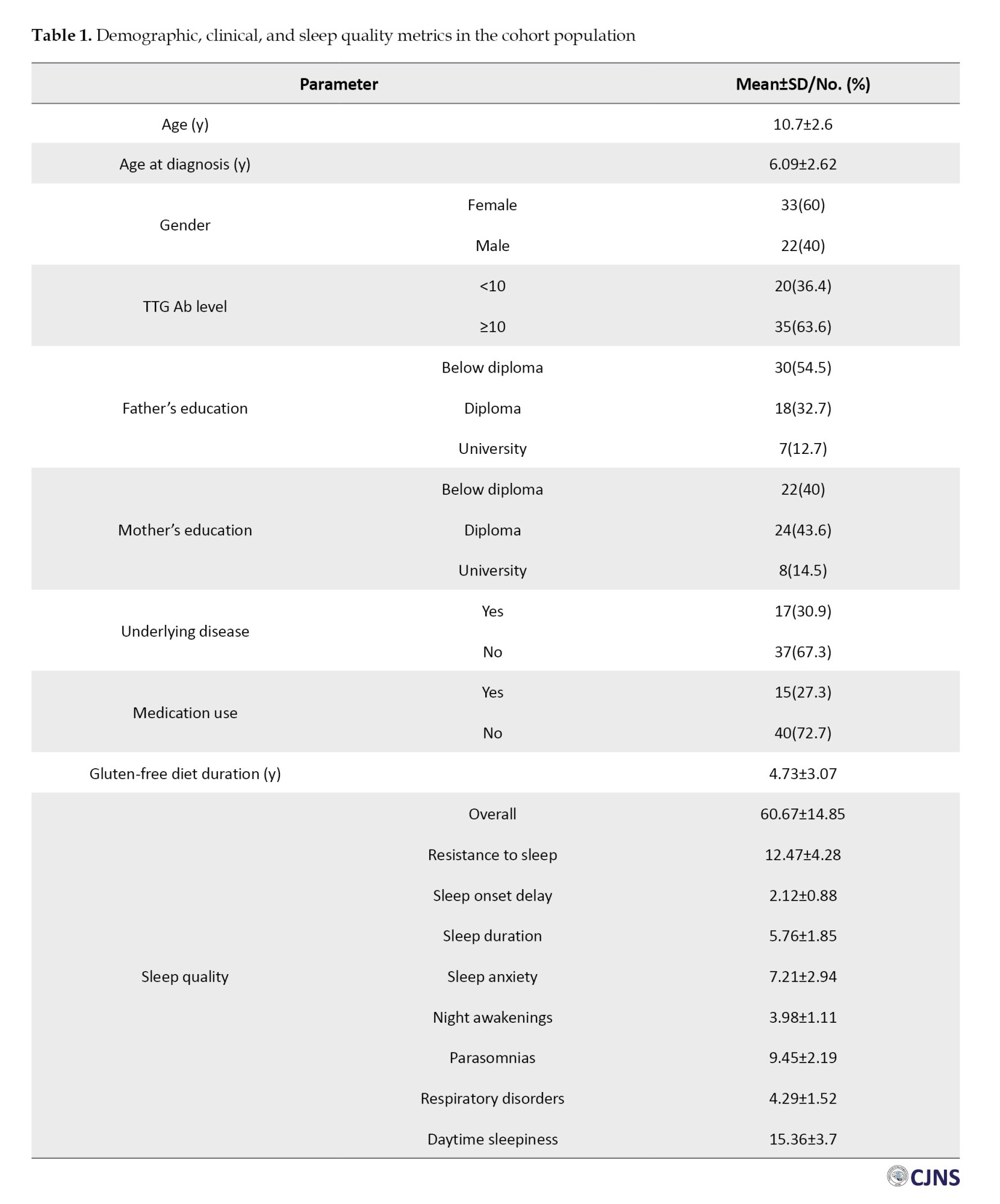
Health status and sleep quality metrics
Regarding health status, 17 children (30.9%) had concurrent diseases related to celiac, contrasting with 37(67.3%) who did not. Medication was being taken by 15 children (27.3%), while 40 (72.7%) were not on any medication. Participants had been adhering to a gluten-free diet for an average of 4.73±3.07 years (Table 1).
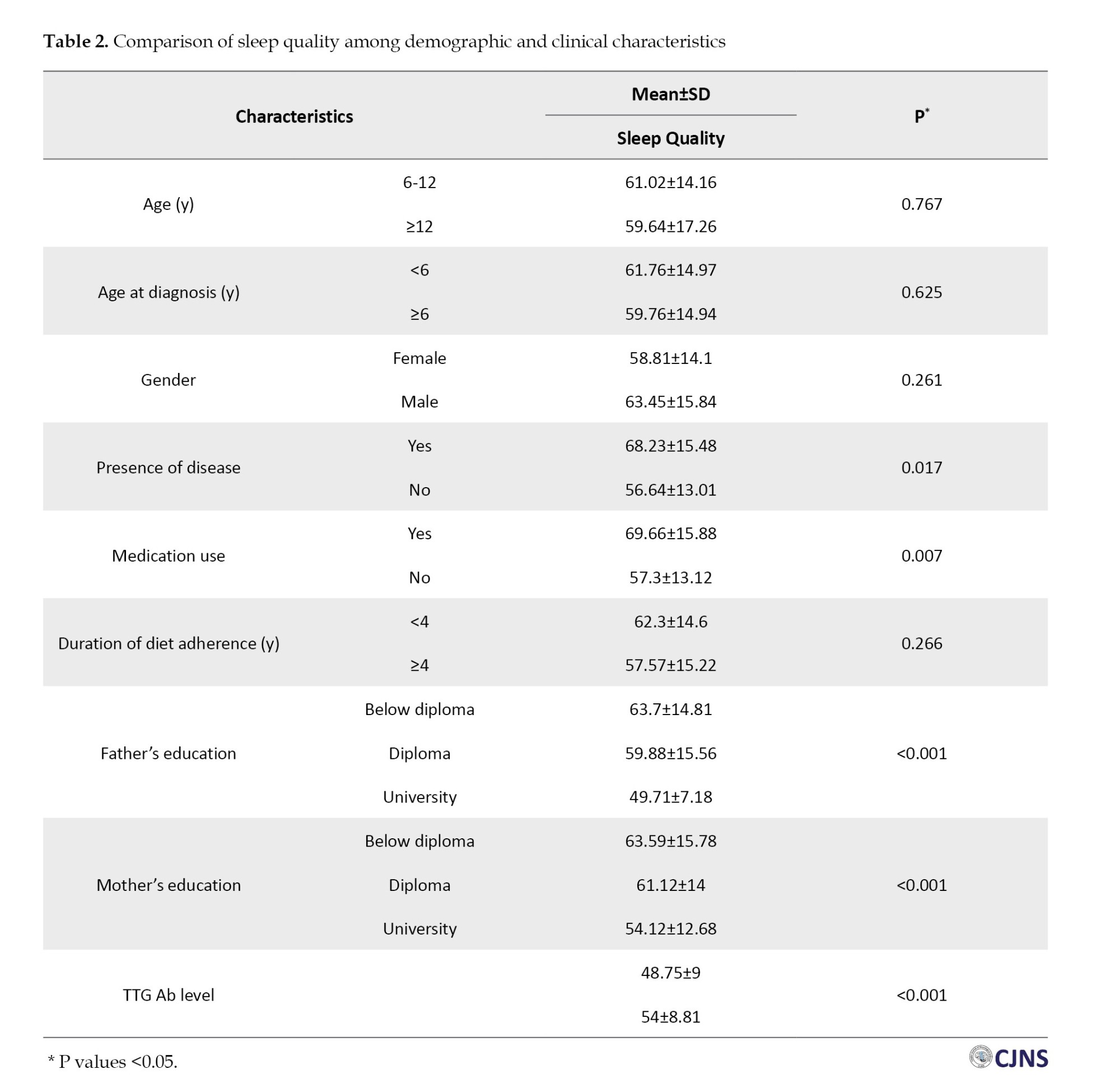
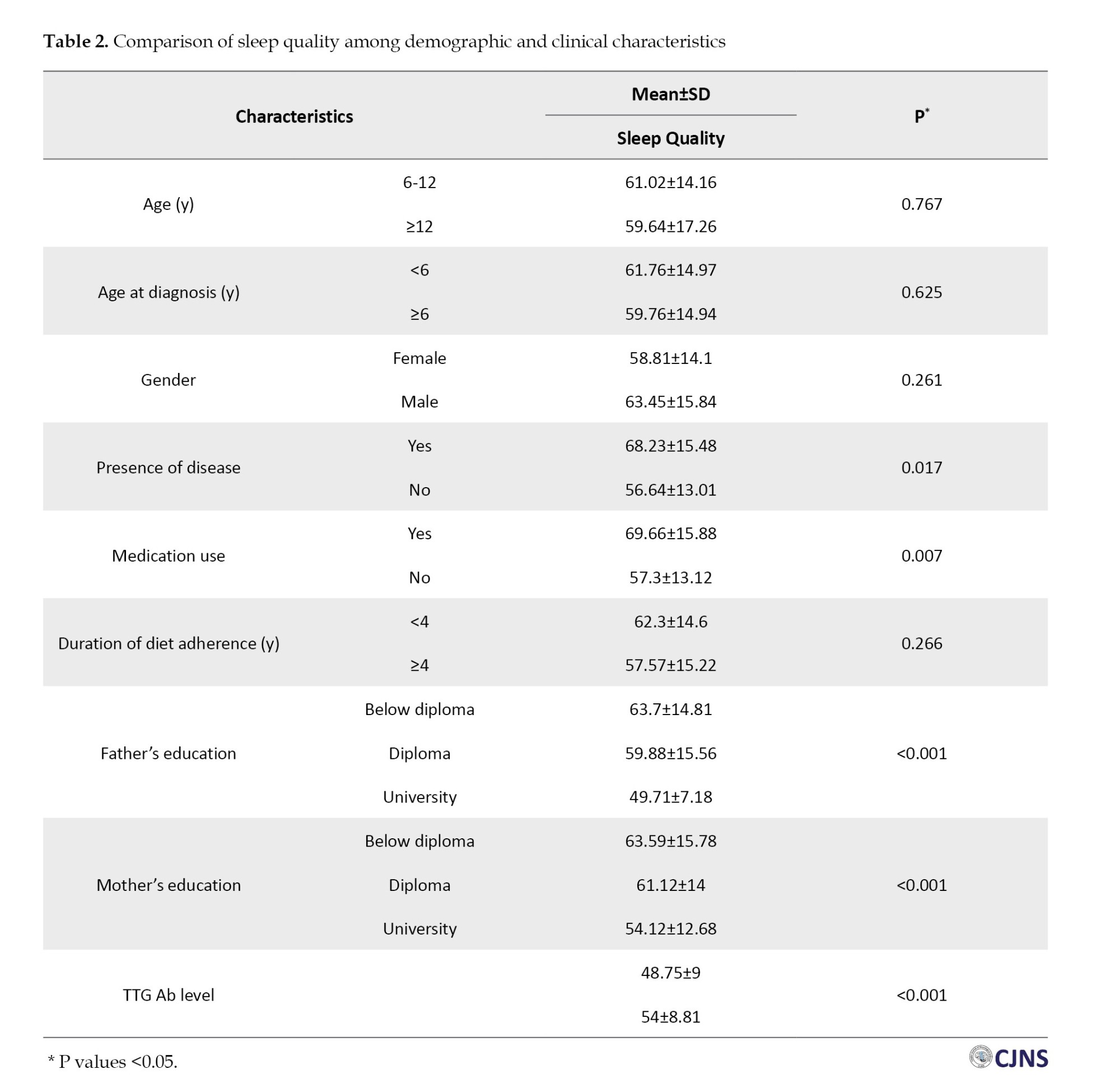
Sleep quality was assessed through various metrics: The mean overall sleep habits score was 60.67±14.85, sleep resistance was 12.47±4.28, and delay in sleep onset was 2.12±0.88. No significant differences were observed in sleep habits based on gender (P=0.261), age (P=0.767), age at diagnosis (P=0.625), or duration of diet adherence (P=0.266). However, there was a discernible association between sleep habits and the presence of disease (P=0.017), medication use (P=0.007), and the latest TTG results (P≤0.001). Moreover, sleep disorders decreased with increasing levels of parental education: Fathers with university-level education had a mean sleep score of 49.71±7.18, and mothers with university-level education had a mean sleep score of 54.12±12.68 (Table 2).
Discussion
People with chronic illnesses typically suffer from sleep problems, which may complicate treatment and worsen symptoms [14]. The rate of sleep deficiency in patients with CD is among the worst among those suffering from gastrointestinal disorders [15]. CD is a chronic medical condition associated with different psychological and behavioral symptoms, including sleep disorders [16]. The primary focus of this study was to explore the relationship between sleep disorders and TTG Ab levels in children aged 1 to 16 years with CD. Based on the findings, a significant correlation between sleep disorders and elevated TTG Ab levels was found in children with CD.
Similar to our findings, Reiter et al. reported the high rates of sleep disturbances in celiac patients compared with healthy children. A gluten-free diet did not improve sleep disturbances and may be a result of abdominal pain [17]. Yerushalmy-Feler et al. conducted a study on 34 celiac children and found that a gluten-free diet significantly improved symptoms related to obstructive sleep apnea [18]. Zingone et al. included adult celiac patients and found that sleep disorders were common both at diagnosis and during treatment with a gluten-free diet, affecting factors like depression, anxiety, and fatigue [20]. These studies support our findings and emphasize the need for more targeted research on the relationship between sleep disorders and CD.
Moreover, the chronic nature of CD has been previously reported to impact sleep quality. Mastrogiorgio et al. found a higher prevalence of sleep-disordered breathing in children with CD [20]. Alkhayyat et al. conducted a large-scale study involving 3746810 celiac patients and found a higher risk for multiple psychiatric disorders, including anxiety and depression [21]. While our study did not find a direct link between psychiatric disorders and sleep issues, it suggests that personality traits like anxiety sensitivity could be contributing factors.
Our study also revealed that sleep disorders were significantly lower in children with higher levels of parental education and higher in those with comorbidities or on medication. This finding aligns with the study by Khanijow et al., which concluded that treating sleep disorders could improve gastrointestinal symptoms and vice versa [22]. These findings suggest that a multifaceted approach, considering both medical and socio-economic factors, may be necessary for the effective management of sleep disorders in celiac patients.
Conclusion
Our study contributes to the existing literature by focusing on the significant association between sleep disorders and elevated TTG Ab levels in children with CD. It corroborates previous research on the prevalence of sleep disorders in this population while introducing the novel finding of a statistically significant correlation with TTG Ab levels. Our study lays the groundwork for more comprehensive research to delve deeper into the physiological and psychological factors affecting sleep quality in children with CD. Given the study’s limitations, future research must validate these findings and develop multifaceted treatment approaches considering medical and socio-economic factors.
Limitations and future research
While our study provides valuable insights into the relationship between sleep disorders and TTG Ab levels in children with CD, it is crucial to acknowledge its limitations. First, our study was confined to patients registered in the Celiac System of Shahid Sadoughi University of Medical Sciences in Yazd, which restricts the generalizability of our findings to the broader population of children with CD. Second, the study relied on self-reported data, which introduces the possibility of reporting bias and may affect the accuracy of our findings. Third, the study focused on a relatively short-term evaluation of sleep disorders and TTG Ab levels, necessitating longer-term studies to validate these initial observations. Additionally, the absence of specialized questionnaires for assessing sleep disorders in celiac patients presents a methodological constraint that could affect our data’s comprehensiveness.
For future research, we recommend expanding the scope of the study to include multiple healthcare settings and extending the evaluation period for sleep disorders and TTG Ab levels. Developing specialized questionnaires for celiac patients to assess sleep quality more accurately would also be beneficial. Given our findings on the impact of parental education and comorbidities, future studies should consider these variables in more depth, possibly through stratified sampling or multivariate analysis.
Ethical Considerations
Compliance with ethical guidelines
Ethical Considerations
Ethical clearance for this study was obtained from the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1400.222). All participants were fully informed about the research objectives and assured of the confidentiality of their information. It was emphasized that all personally identifiable information would be kept strictly confidential. Informed consent was obtained from the parents or legal guardians of all participating children. Acknowledgments were given to all who contributed to the research.
Funding
This article was extracted from the general medical doctorate thesis of Maryam Mohammadi, approved by Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: 11304).
Authors contributions
Conceptualization, methodology, supervision, and project administration: Roohollah Edalatkhah and Majid Aflatoonianm: Data collection: Roohollah Edalatkhah, Maryam Mohammadi, Majid Aflatoonianm, and Zahra Rasoulizadeh; Statistical analysis: Maryam Mohammadi; Writing the original draft: Roohollah Edalatkhah and Zahra Rasoulizadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all the parents and children who participated in this study.
References
Celiac disease (CD) is a complex autoimmune disorder with a genetic predisposition triggered by the ingestion of gluten-containing grains such as wheat [1]. The disease presents many gastrointestinal and extra-gastrointestinal symptoms, including diarrhea, bloating, and steatorrhea [2]. While the global prevalence of CD is estimated to be between 1% and 2%, some studies suggest that the actual numbers could be higher [2, 3].
Globally, approximately 1% of the population is affected by CD, with varying prevalence rates in different countries such as New Zealand, Argentina, Hungary, Sweden, Finland, India, and Egypt [4]. Western Europe region reports the highest prevalence, and Middle Eastern countries like Iran also show comparable rates, with about 1% of the general population affected [5].
CD often manifests in early childhood, particularly when children are first introduced to gluten-containing foods [6]. The only effective treatment for managing the disease’s multifaceted clinical, histological, and serological aspects is a lifelong adherence to a gluten-free diet [7]. Although primarily affecting the intestine, CD is a systemic disease affecting multiple tissues, including the nervous system [8]. Sleep, a vital component of children’s physical and mental well-being, is often compromised in chronic medical conditions, including autoimmune and atopic diseases [9, 10]. Conditions such as asthma, cystic fibrosis, sickle cell anemia, gastroesophageal reflux disease, neuromuscular disorders, and chromosomal abnormalities are associated with poor sleep quality [11].
In light of the significance of sleep in children’s overall health and its frequent disturbance in autoimmune and gastrointestinal diseases, this study aims to investigate the association between sleep disorders and tissue transglutaminase antibody (TTG Ab) levels in pediatric patients with CD.
Materials and Methods
Study design and participants
This analytic cross-sectional study was conducted from 2016 to 2022, focusing on pediatric patients referred at Shahid Sadoughi Hospital’s Gastroenterology Clinic in Yazd, Iran. The research population consists of all children diagnosed with CD whose records were registered in the Yazd celiac system during this period. The diagnosis of CD was based on the presence of IgA/IgG antibodies (TTG-IgA/IgG) in the serum and the results of duodenal biopsies. Testing was performed on all patients with TTG-IgA deficiency to rule out the possibility of selective IgA deficiency. Using Marsh classification, biopsies from the duodenum and bulbous were analyzed, and CD diagnosis was made [12]. A total of 55 records were analyzed after data screening out of 202 individuals registered in the system, 80 of whom were under 16. The inclusion criteria were age between 1 to 16 years, diagnosis of CD, and undergoing gluten-free diet therapy. The exclusion criteria included age older than 16 or younger than 1, history of any disease such as diabetes, malignancies, metabolic disorders, psychiatric disorders, gastrointestinal disorders, and history of medication use for mental disorders or chronic disorders.
Data collection
Data were collected after obtaining ethical clearance and identifying patients who met the inclusion criteria from the Yazd celiac system records. An online questionnaire was sent to the participants, who were requested to answer carefully. Two types of questionnaires were used: 1) Demographic information questionnaire including relevant information such as age, gender, age at diagnosis, the serum level of TTG Ab, medication use, gluten-free diet duration, and parents’ education, and 2) Children’s sleep habits questionnaire (CSHQ). This study used the Persian version of parent-reported CSHQ. It consists of 45 questions, of which only 33 are considered for scoring. Eight subscales of CSHQ were measured: Bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night waking, parasomnias, daytime sleepiness, and sleep-disordered breathing. Each item is scored between 1 and 3 (“rarely” to “usually”), except for specific reverse-scored items. The score range is 33-99. Sleep disturbances are defined by a score of 41 [13]. Fallahzadeh et al. evaluated the validity and reliability of the Persian version of CSHQ using the Cronbach α coefficient. A Cronbach α coefficient of 0.80 was calculated for the entire questionnaire. There was a range of convergence validity of 0.4 to 0.86 [13].
Statistical analysis
The collected data were systematically imported into SPSS software, version 26 (SPSS Inc., Chicago, IL, USA). for analysis according to the research objectives. Descriptive statistics were employed, including mean and standard deviation for quantitative data and frequency and percentage for qualitative data. The chi-square and Fisher exact tests were used to compare frequency distributions. A t-test was employed to compare the means. The normality of the data was tested using the Kolmogorov-Smirnov test, and a P<0.05 was considered statistically significant. The sample size was calculated using the formula for comparing means, considering alpha=0.05, beta=0.2, and a TTG level difference of 0.1 between individuals with and without sleep disorder. Accordingly, the sample size was estimated at 48.
Results
Demographics and baseline characteristics
The study involved participants with a mean age of 10.70±2.6 years and a mean age at diagnosis of 6.09±2.62 years. Of 55 participants, 33(60%) were female and 22(40%) were male. The latest TTG results revealed that 20 children (36.4%) had values below 10, while 35(63.6%) had values above 10. Parental education was diverse: 30(54.5%) of fathers and 22(40%) of mothers had education below diploma level; 18(32.7%) of fathers and 24(43.6%) of mothers had a diploma; and 7(12.7%) of fathers and 8(14.5%) of mothers had university-level education (Table 1).
Health status and sleep quality metrics
Regarding health status, 17 children (30.9%) had concurrent diseases related to celiac, contrasting with 37(67.3%) who did not. Medication was being taken by 15 children (27.3%), while 40 (72.7%) were not on any medication. Participants had been adhering to a gluten-free diet for an average of 4.73±3.07 years (Table 1).
Sleep quality was assessed through various metrics: The mean overall sleep habits score was 60.67±14.85, sleep resistance was 12.47±4.28, and delay in sleep onset was 2.12±0.88. No significant differences were observed in sleep habits based on gender (P=0.261), age (P=0.767), age at diagnosis (P=0.625), or duration of diet adherence (P=0.266). However, there was a discernible association between sleep habits and the presence of disease (P=0.017), medication use (P=0.007), and the latest TTG results (P≤0.001). Moreover, sleep disorders decreased with increasing levels of parental education: Fathers with university-level education had a mean sleep score of 49.71±7.18, and mothers with university-level education had a mean sleep score of 54.12±12.68 (Table 2).
Discussion
People with chronic illnesses typically suffer from sleep problems, which may complicate treatment and worsen symptoms [14]. The rate of sleep deficiency in patients with CD is among the worst among those suffering from gastrointestinal disorders [15]. CD is a chronic medical condition associated with different psychological and behavioral symptoms, including sleep disorders [16]. The primary focus of this study was to explore the relationship between sleep disorders and TTG Ab levels in children aged 1 to 16 years with CD. Based on the findings, a significant correlation between sleep disorders and elevated TTG Ab levels was found in children with CD.
Similar to our findings, Reiter et al. reported the high rates of sleep disturbances in celiac patients compared with healthy children. A gluten-free diet did not improve sleep disturbances and may be a result of abdominal pain [17]. Yerushalmy-Feler et al. conducted a study on 34 celiac children and found that a gluten-free diet significantly improved symptoms related to obstructive sleep apnea [18]. Zingone et al. included adult celiac patients and found that sleep disorders were common both at diagnosis and during treatment with a gluten-free diet, affecting factors like depression, anxiety, and fatigue [20]. These studies support our findings and emphasize the need for more targeted research on the relationship between sleep disorders and CD.
Moreover, the chronic nature of CD has been previously reported to impact sleep quality. Mastrogiorgio et al. found a higher prevalence of sleep-disordered breathing in children with CD [20]. Alkhayyat et al. conducted a large-scale study involving 3746810 celiac patients and found a higher risk for multiple psychiatric disorders, including anxiety and depression [21]. While our study did not find a direct link between psychiatric disorders and sleep issues, it suggests that personality traits like anxiety sensitivity could be contributing factors.
Our study also revealed that sleep disorders were significantly lower in children with higher levels of parental education and higher in those with comorbidities or on medication. This finding aligns with the study by Khanijow et al., which concluded that treating sleep disorders could improve gastrointestinal symptoms and vice versa [22]. These findings suggest that a multifaceted approach, considering both medical and socio-economic factors, may be necessary for the effective management of sleep disorders in celiac patients.
Conclusion
Our study contributes to the existing literature by focusing on the significant association between sleep disorders and elevated TTG Ab levels in children with CD. It corroborates previous research on the prevalence of sleep disorders in this population while introducing the novel finding of a statistically significant correlation with TTG Ab levels. Our study lays the groundwork for more comprehensive research to delve deeper into the physiological and psychological factors affecting sleep quality in children with CD. Given the study’s limitations, future research must validate these findings and develop multifaceted treatment approaches considering medical and socio-economic factors.
Limitations and future research
While our study provides valuable insights into the relationship between sleep disorders and TTG Ab levels in children with CD, it is crucial to acknowledge its limitations. First, our study was confined to patients registered in the Celiac System of Shahid Sadoughi University of Medical Sciences in Yazd, which restricts the generalizability of our findings to the broader population of children with CD. Second, the study relied on self-reported data, which introduces the possibility of reporting bias and may affect the accuracy of our findings. Third, the study focused on a relatively short-term evaluation of sleep disorders and TTG Ab levels, necessitating longer-term studies to validate these initial observations. Additionally, the absence of specialized questionnaires for assessing sleep disorders in celiac patients presents a methodological constraint that could affect our data’s comprehensiveness.
For future research, we recommend expanding the scope of the study to include multiple healthcare settings and extending the evaluation period for sleep disorders and TTG Ab levels. Developing specialized questionnaires for celiac patients to assess sleep quality more accurately would also be beneficial. Given our findings on the impact of parental education and comorbidities, future studies should consider these variables in more depth, possibly through stratified sampling or multivariate analysis.
Ethical Considerations
Compliance with ethical guidelines
Ethical Considerations
Ethical clearance for this study was obtained from the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1400.222). All participants were fully informed about the research objectives and assured of the confidentiality of their information. It was emphasized that all personally identifiable information would be kept strictly confidential. Informed consent was obtained from the parents or legal guardians of all participating children. Acknowledgments were given to all who contributed to the research.
Funding
This article was extracted from the general medical doctorate thesis of Maryam Mohammadi, approved by Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: 11304).
Authors contributions
Conceptualization, methodology, supervision, and project administration: Roohollah Edalatkhah and Majid Aflatoonianm: Data collection: Roohollah Edalatkhah, Maryam Mohammadi, Majid Aflatoonianm, and Zahra Rasoulizadeh; Statistical analysis: Maryam Mohammadi; Writing the original draft: Roohollah Edalatkhah and Zahra Rasoulizadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank all the parents and children who participated in this study.
References
- Pourhoseingholi MA, Rostami-Nejad M, Barzegar F, Rostami K, Volta U, Sadeghi A, et al. Economic burden made celiac disease an expensive and challenging condition for Iranian patients. Gastroenterol Hepatol Bed Bench. 2017; 10(4):258. [PMID]
- Sahin Y. Celiac disease in children: A review of the literature. World J Clin Pediatr. 2021; 10(4):53-71. [DOI:10.5409/wjcp.v10.i4.53] [PMID] [PMCID]
- Mohammadibakhsh R, Sohrabi R, Salemi M, Mirghaed MT, Behzadifar M. Celiac disease in Iran: A systematic review and meta-analysis. Electron Physician. 2017; 9(3):3883-95. [DOI:10.19082/3883] [PMID] [PMCID]
- Patel SC, Shreya D, Zamora DI, Patel GS, Grossmann I, Rodriguez K, et al. Celiac disease, beyond the bowel: A review of its neurological manifestations. Cureus. 2021; 13(12):e20112. [DOI:10.7759/cureus.20112]
- Raiteri A, Granito A, Giamperoli A, Catenaro T, Negrini G, Tovoli F. Current guidelines for the management of celiac disease: A systematic review with comparative analysis. World J Gastroenterol. 2022; 28(1):154-75. [DOI:10.3748/wjg.v28.i1.154] [PMID] [PMCID]
- Nye-Wood MG, Juhász A, Bose U, Colgrave ML. Proteome analysis and epitope mapping in a commercial reduced-gluten wheat product. Front Nutr. 2021; 8:705822. [DOI:10.3389/fnut.2021.705822] [PMID] [PMCID]
- Mostafaei FS, Hajinabi Y, Rezaei-Tavirani M, Daryani NE, Zali M. The high costs of gluten-free products for iranian patients with celiac disease. Govaresh. 2019; 24(3):156-62. [Link]
- Bushara KO. Neurologic presentation of celiac disease. Gastroenterology. 2005; 128(4 Suppl 1):S92-7. [DOI:10.1053/j.gastro.2005.02.018] [PMID]
- Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016; 12(6):785-6. [DOI:10.5664/jcsm.5866] [PMID] [PMCID]
- Koinis-Mitchell D, Craig T, Esteban CA, Klein RB. Sleep and allergic disease: A summary of the literature and future directions for research. J Allergy Clin Immunol. 2012; 130(6):1275-81. [DOI:10.1016/j.jaci.2012.06.026] [PMID] [PMCID]
- Bandla H, Splaingard M. Sleep problems in children with common medical disorders. Pediatr Clin North Am. 2004; 51(1):203-27. [DOI:10.1016/S0031-3955(03)00185-8] [PMID]
- Husby S, Koletzko S, Korponay-Szabó IR, Mearin ML, Phillips A, Shamir R, et al. European society for pediatric gastroenterology, hepatology, and nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012; 54(1):136-60. [DOI:10.1097/MPG.0b013e31821a23d0] [PMID]
- Fallahzadeh H, Etesam F, Asgarian FS. Validity and reliability related to the Persian version of the children’s sleep habits questionnaire. Sleep Biol Rhythms. 2015; 13(3):271-8. [DOI:10.1111/sbr.12114]
- Baiardini I, Braido F, Cauglia S, Canonica GW. Sleep disturbances in allergic diseases. Allergy. 2006; 61(11):1259-67. [DOI:10.1111/j.1398-9995.2006.01221.x] [PMID]
- Ballou S, Alhassan E, Hon E, Lembo C, Rangan V, Singh P, et al. Sleep disturbances are commonly reported among patients presenting to a gastroenterology clinic. Dig Dis Sci. 2018; 63(11):2983-91. [DOI:10.1007/s10620-018-5237-7] [PMID]
- Smith LB, Lynch KF, Kurppa K, Koletzko S, Krischer J, Liu E, et al. Psychological manifestations of celiac disease autoimmunity in young children. Pediatrics. 2017; 139(3):e20162848. [DOI:10.1542/peds.2016-2848] [PMID] [PMCID]
- Reiter J, Abuelhija H, Slae M, Millman P, Davidovics Z, Chaimov E, et al. Sleep disorders in children with celiac disease: A prospective study. J Clin Sleep Med. 2023; 19(3):591-4. [DOI:10.5664/jcsm.10396] [PMID] [PMCID]
- Yerushalmy-Feler A, Tauman R, Derowe A, Averbuch E, Ben-Tov A, et al. Gluten-free diet may improve obstructive sleep apnea-related symptoms in children with celiac disease. BMC Pediatr. 2018; 18(1):35. [DOI:10.1186/s12887-018-1039-5] [PMID] [PMCID]
- Zingone F, Siniscalchi M, Capone P, Tortora R, Andreozzi P, Capone E, Ciacci C. The quality of sleep in patients with coeliac disease. Aliment Pharmacol Ther. 2010; 32(8):1031-6. [DOI:10.1111/j.1365-2036.2010.04432.x] [PMID]
- Mastrogiorgio G, Ferretti A, Pietropaoli N, Rabasco J, Petrarca L, Florio M, et al. Prevalence of sleep disordered breathing in coeliac children. Eur Respir J. 2013; 42(Suppl 57):P4282. [Link]
- Alkhayyat M, Qapaja T, Aggarwal M, Almomani A, Abureesh M, Al-Otoom O, et al. Epidemiology and risk of psychiatric disorders among patients with celiac disease: A population-based national study. J Gastroenterol Hepatol. 2021; 36(8):2165-70. [DOI:10.1111/jgh.15437] [PMID]
- Khanijow V, Prakash P, Emsellem HA, Borum ML, Doman DB. Sleep Dysfunction and Gastrointestinal Diseases. Gastroenterol Hepatol. 2015; 11(12):817-25. [PMID]
Type of Study: Research |
Subject:
Special
Received: 2024/03/5 | Accepted: 2025/05/6 | Published: 2025/07/1
Received: 2024/03/5 | Accepted: 2025/05/6 | Published: 2025/07/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |