Tue, Feb 3, 2026
Volume 11, Issue 1 (Winter 2025)
Caspian J Neurol Sci 2025, 11(1): 28-37 |
Back to browse issues page
Ethics code: IR.GUMS.REC.1402.318
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Masihipour B, Mansour-Ghanaei F, Maroufizadeh S, Hassanipour S, Asgharnezhad M, Isanazar A, et al . The Association of Depression and Anxiety Disorders With Gastrointestinal Symptoms Among Nurses. Caspian J Neurol Sci 2025; 11 (1) :28-37
URL: http://cjns.gums.ac.ir/article-1-736-en.html
URL: http://cjns.gums.ac.ir/article-1-736-en.html
Behnam Masihipour1 

 , Fariborz Mansour-Ghanaei1
, Fariborz Mansour-Ghanaei1 

 , Saman Maroufizadeh2
, Saman Maroufizadeh2 

 , Soheil Hassanipour1
, Soheil Hassanipour1 

 , Mehrnaz Asgharnezhad1
, Mehrnaz Asgharnezhad1 

 , Adele Isanazar3
, Adele Isanazar3 

 , Kourosh Mojtahedi1
, Kourosh Mojtahedi1 

 , Farahnaz Joukar *4
, Farahnaz Joukar *4 




 , Fariborz Mansour-Ghanaei1
, Fariborz Mansour-Ghanaei1 

 , Saman Maroufizadeh2
, Saman Maroufizadeh2 

 , Soheil Hassanipour1
, Soheil Hassanipour1 

 , Mehrnaz Asgharnezhad1
, Mehrnaz Asgharnezhad1 

 , Adele Isanazar3
, Adele Isanazar3 

 , Kourosh Mojtahedi1
, Kourosh Mojtahedi1 

 , Farahnaz Joukar *4
, Farahnaz Joukar *4 


1- Gastrointestinal and Liver Diseases Research Center, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Psychiatry, School of Medicine, Shafa Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Gastrointestinal and Liver Diseases Research Center, Guilan University of Medical Sciences, Rasht, Iran. ,farajov@gmail.com
2- Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Psychiatry, School of Medicine, Shafa Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Gastrointestinal and Liver Diseases Research Center, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 1645 kb]
(629 Downloads)
| Abstract (HTML) (1099 Views)
Full-Text: (657 Views)
Introduction
The role of the gut-brain axis in maintaining a healthy status is significant [1]. The gut-brain axis is a bidirectional communication network between the gastrointestinal (GI) tract and the central nervous system, involving neural, hormonal and immune pathways [2, 3]. Dysregulation of the gut-brain axis can alter gut motility, secretion, and permeability, as well as changes in neurotransmitter signaling and immune function, all of which have been implicated in the pathophysiology of psychological and GI disorders [4, 5]. The prevalence of anxiety among individuals in different occupations can vary based on various factors, including the nature of their work, the demands of their job and the hours of working. Shift work, irregular working hours and long shifts are often associated with increased levels of anxiety due to disruptions in circadian rhythms, sleep disturbances, and challenges in achieving work-life balance [6, 7].
Healthcare workers, including nurses, physicians and other medical professionals, often work long and irregular hours, including night shifts and weekend rotations. Nurses often encounter high levels of stress during their shifts, which can lead to various complications and chronic health issues [8, 9]. The nursing profession is characterized by significant stress, demands and challenges, with job-related stress being closely associated with elevated rates of depression. Studies indicate that nurses encounter depressive symptoms at a rate double that of individuals in various other occupations [10, 11]. The demanding nature of their work, long hours, frequent exposure to emotionally challenging situations, and making critical decisions under pressure can contribute to elevated stress levels and burnout in nurses [12, 13].
Chronic stress and anxiety can manifest physically, leading to GI symptoms (with a frequency of 43%), such as abdominal discomfort, bloating, nausea, and changes in bowel habits [14]. Additionally, poor dietary habits, irregular meal times and inadequate hydration due to the fast-paced nature of nursing work can further exacerbate GI issues among nurses [15]. About 58.8% of depression and 62% of anxiety were reported among shift nurses [7]. Since it is crucial for healthcare institutions to prioritize measures to support nurses’ mental and physical well-being to mitigate the impact of stress-related complications on their health, we investigated the association between depression and anxiety with GI symptoms and the related factors among nurses in different wards of hospitals in Rasht City, Iran.
Materials and Methods
Study design
This cross-sectional study was conducted on 460 nurses working in educational and medical hospitals affiliated with the Guilan University of Medical Sciences, Rasht, Iran, in 2024. These hospitals included Heshmat Hospital (n=82 nurses), Razi Hospital (n=113 nurses), Poursina Hospital (n=116 nurses), Amir Al-Momenin Hospital (n=26 nurses), 17-Shahrivar Hospital (n=50 nurses), Velayat Hospital (n=33 nurses) and Alzahra Hospital (n=40 nurses). Participants were selected for the study using stratified and cluster random sampling methods. All individuals gave their informed consent to participate in the study. Clinical and demographical data of participants, including age, gender, marital status (single/married), educational level (bachelor/master), work experience (years), shifts (fix/rotating), professional position (nurse/head nurse), history of smoking, alcohol consumption, body mass index (BMI) (underweight <18.5 kg/m2, normal weight=18.5–24.99 kg/m2, overweight=25–29.9 kg/m2 and obese ≥30 kg/m2), underlying diseases, history of consulting a psychologist or psychiatrist, using sedatives, antianxiety, or antidepressants, GI symptoms and numbers of GI symptoms were recorded. A gastroenterologist confirmed that all GI symptoms were not structural. GI symptoms included nausea, gastroesophageal reflux, diarrhea, constipation, vomiting, flatulence, GI bleeding, abdominal pain, jaundice and weight loss. The status of anxiety and depression was assessed under the supervision of a psychiatrist. The depression, anxiety and stress scale-21 (DASS-21) was used to assess the negative emotional states of depression and anxiety in participants, which was previously confirmed for validity and reliability in several studies [16–18].
Depression anxiety and stress scale-21 item (DASS-21)
The DASS-21 is a short form of DASS, which is a self-report instrument composed of three subscales: Depression, anxiety and stress [19]. This scale consists of three 7-item subscales, each rated on a 4-point Likert scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). Because the DASS 21 is a short version of the original DASS (the long form has 42 items), the final score of each subscale must be multiplied by two. Therefore, all subscale scores can range from 0 to 42, with higher scores indicating greater levels of depression, anxiety, and stress. A total score of 10 or more indicates mild to severe depression, a score of 8 or more indicates mild to severe anxiety and a score of 15 or more indicates mild to severe stress. The Persian version of this scale is reported to have satisfactory psychometric properties among health professionals [20]. In this study, the cronbach α values for depression and anxiety subscales were 0.835 and 0.700, respectively.
Statistical analysis
Based on Haug et al.’s study [21] showing a 48% prevalence of GI issues, the sample size calculation initially yielded 383 participants. Accounting for cluster sampling, this was multiplied by a 1.2 design effect, resulting in a final sample of 460. The calculation used select-statistics software, assuming a 95% confidence level, 5% error margin and 48% prevalence.
Variables were presented as percentage, frequency, Mean±SD, median and interquartile range (IQR). The Kolmogorov-Smirnov test was employed to assess the assumption of normality for depression and anxiety. To compare the prevalence of depression and anxiety across personal and occupational characteristics of nurses, the Chi-Square test (or Fisher exact test) was utilized. Additionally, logistic regression was applied to examine the relationship between personal and occupational characteristics and depression and anxiety. Mean scores of depression and anxiety among nurses with and without GI symptoms were compared using the Mann-Whitney test. Both simple logistic regression and multiple logistic regression analyses, in both unadjusted and adjusted formats, were conducted to ascertain the relationship between depression and anxiety disorders with GI symptoms, respectively. The findings of these analyses were presented as crude odds ratios (OR) and adjusted odds ratios (aOR) alongside 95% confidence intervals (95% CI). Data analysis was conducted using SPSS software, version 16, with a significance level set at 0.05. GraphPad Prism software, version 8.0.1 was also utilized for graphing purposes.
Results
The mean age of participants was 30.08±7.43 years, of which 37.8% were ≤30 years. Most of the participants were females (95.9%). Among participants, 12.2% used sedative, antianxiety, or antidepressant drugs. Their mean work experience was 10.02±7.53 years, of which 42.8% had more than 10 years of work experience. Their mean BMI was 25.02±2.93 kg/m2, of which 49.1% had normal BMI (Table 1).
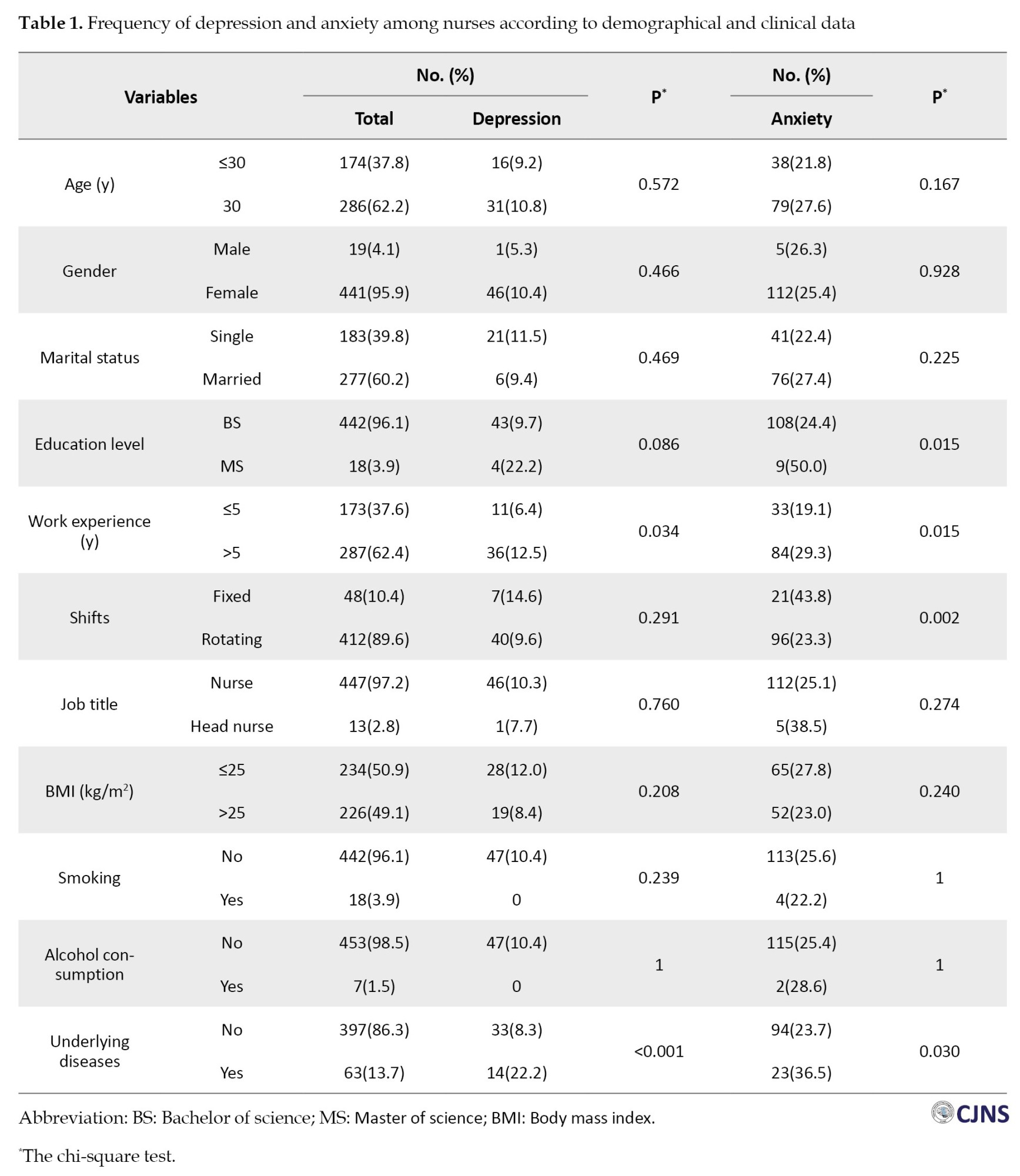
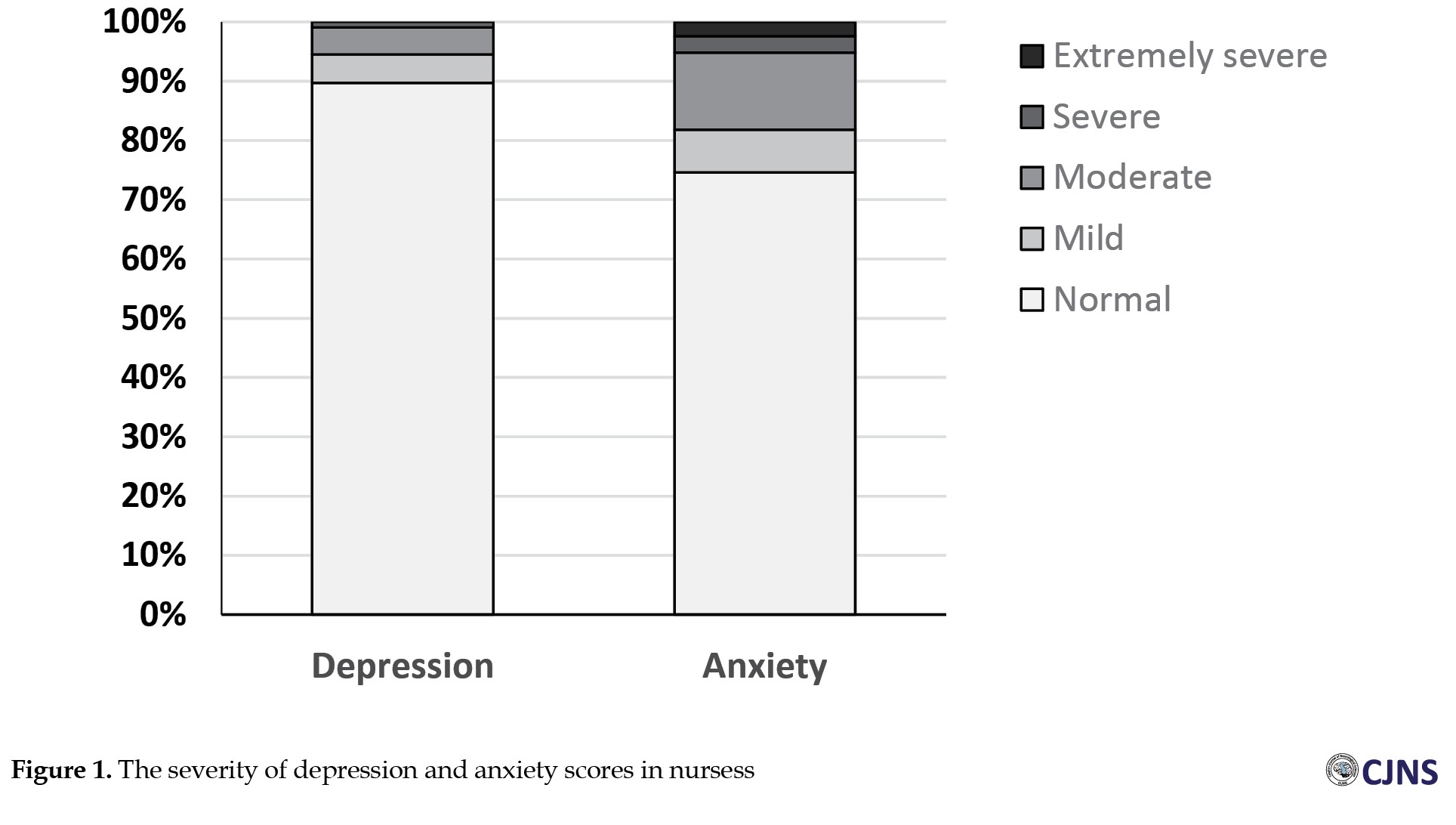
According to the DASS-21 questionnaire, the mean depression score among nurses was 2.50±4.53, with a median score of zero (IQR: 0.2-0) and a frequency of 10.2%. A total of 47(10.2%) were identified as experiencing depression, categorized as mild in 22 cases (4.8%), moderate in 21(4.6%) and severe in 4(0.9%). The average anxiety score was 4.57±5.59, with a median score of 0.4 (IQR: 0.8-0.8) and a prevalence of 25.4%. A total of 117 participants (25.4%) reported experiencing anxiety, with 33(7.2%) classified as mild, 60(13.6%) as moderate, 13(2.8%) as severe and 11(2.4%) as very severe (Figure 1). The frequency of depression and anxiety was significantly higher among nurses with more than five years of work experience and a history of underlying diseases (P<0.05). Furthermore, nurses with upper education and fixed shifts significantly reported more anxiety compared to others (P<0.05) (Table 1).
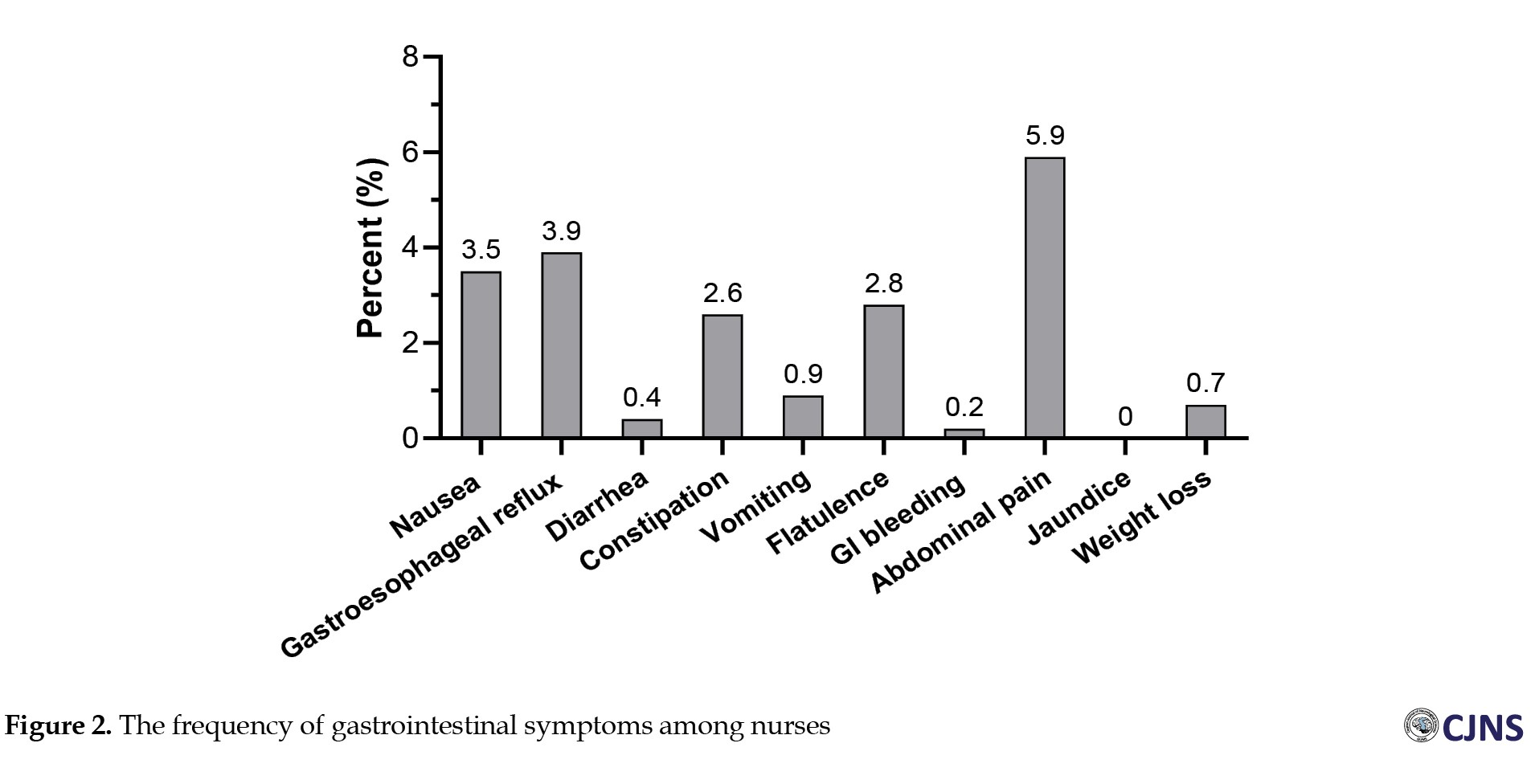
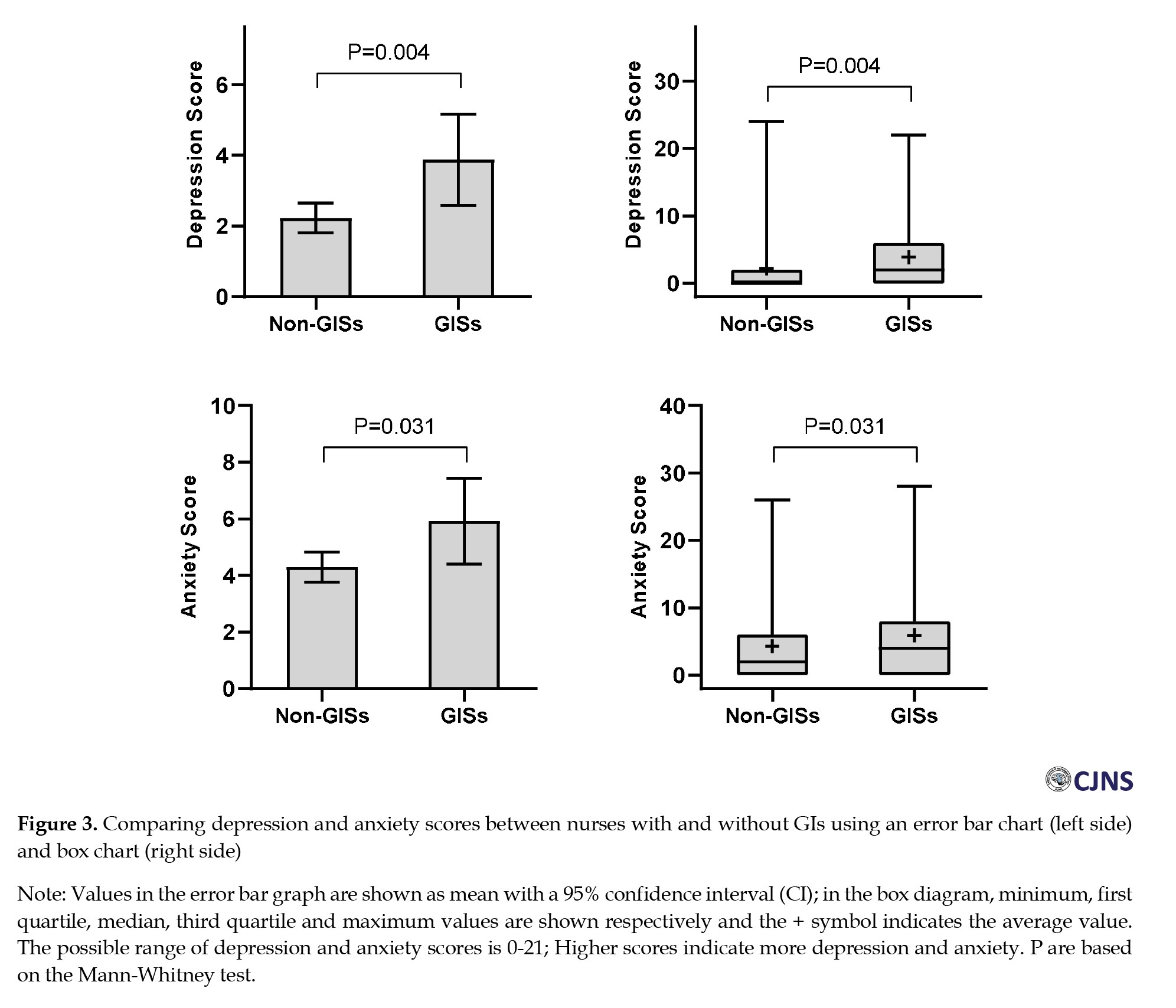
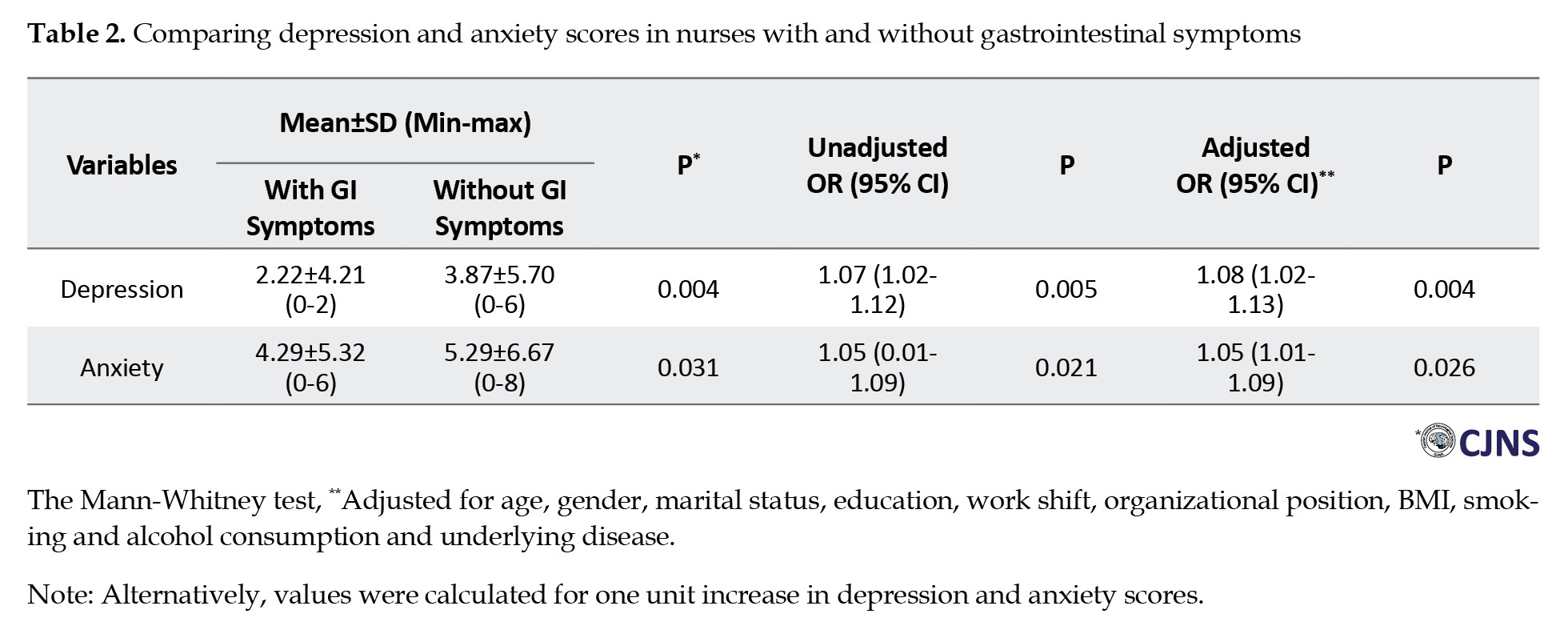
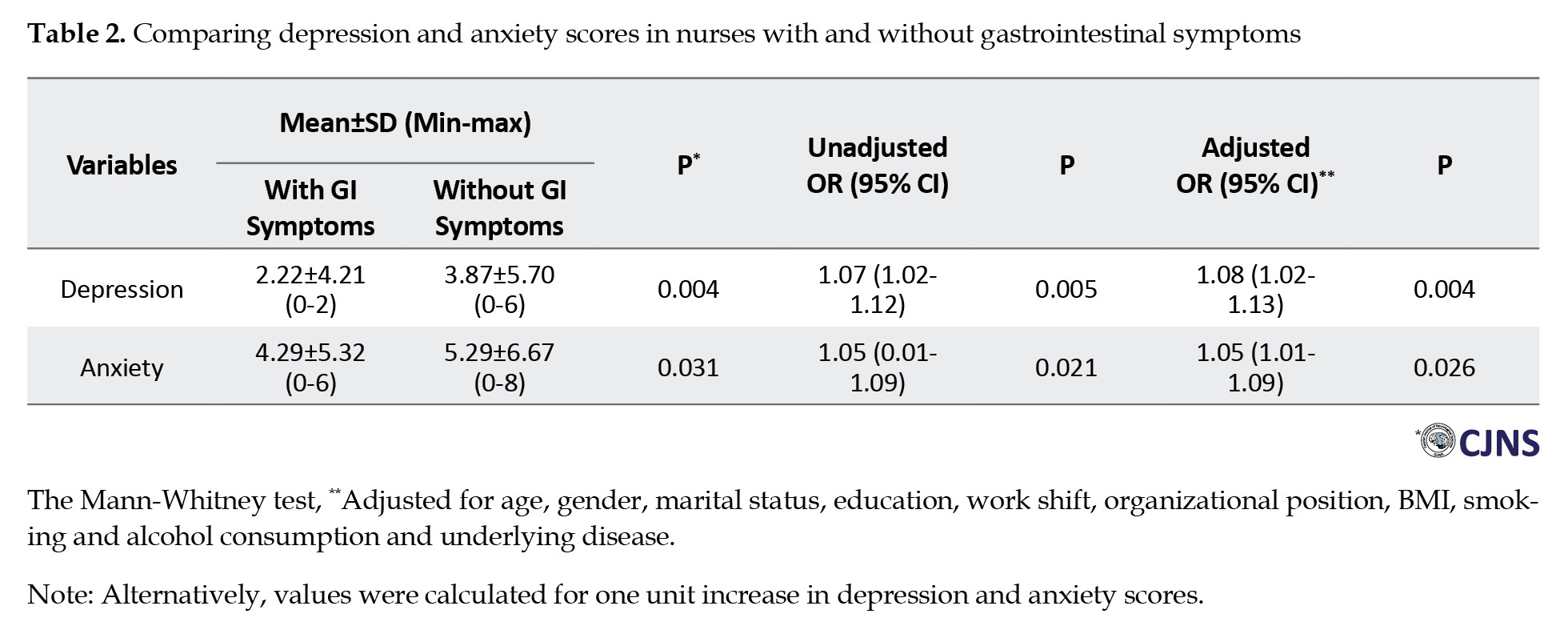
The reported prevalence of GI symptoms among all participants was 16.7%. The most frequently reported GI symptoms included abdominal pain (5.9%, n=27), gastroesophageal reflux (3.9%, n=18), nausea (3.5%, n=16), flatulence (2.8%, n=13), and constipation (2.6%, n=12). Less common symptoms were vomiting (0.9%, n=4), weight loss (0.7%, n=3), diarrhea (0.4%, n=2), and GI bleeding (0.2%, n=1). Notably, jaundice was not observed in any participant. About 14.1% (n=65) experienced one symptom, 1.5% (n=7) had two symptoms, 0.7% (n=3) had three symptoms, and 0.4% (n=2) reported four GI symptoms (Figure 2). The prevalence of depression and anxiety was significantly higher among individuals with GI symptoms (P<0.05) (Table 2 and Figure 3). For each one-unit increase in nurses’ depression and anxiety scores, there was a corresponding 7% and 5% increase in the likelihood of experiencing GI symptoms (Table 2).
The odds of experiencing depression among married nurses were found to be 70% lower compared to singles (OR=0.30, 95% CI, 0.14, 0.65, P=0.002). Similarly, nurses with work experience of more than 5 years exhibited a 3.95-fold higher likelihood of depression in comparison to those with five years or less (OR=3.95, 95% CI, 1.63, 9.57, P=0.002). Nurses with underlying diseases demonstrated a 3.04-fold increased likelihood of depression relative to those without underlying health conditions (OR=3.04, 95% CI, 1.47, 6.29, P=0.003) (Table 3).
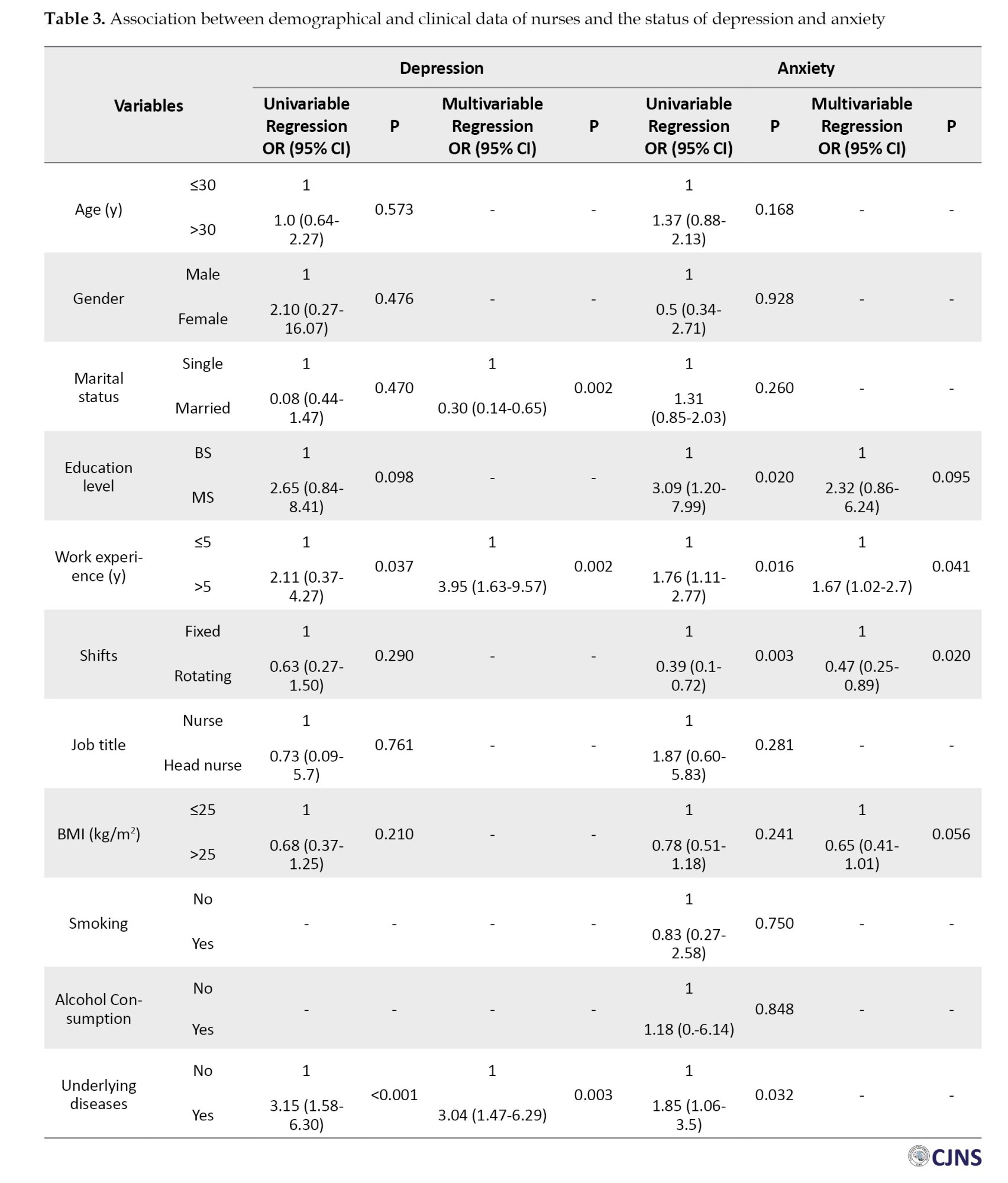
The odds of developing anxiety among nurses with a master’s degree were found to be 2.32 times higher compared to nurses with a bachelor’s degree (OR=2.32, 95% CI, 0.86, 6.24, P=0.095). Similarly, nurses with work experience of more than 5 years exhibited a 67% higher likelihood of anxiety compared to those with work experience of five years or less (OR=1.67, 95% CI, 1.02, 2.72, P=0.041). Furthermore, the likelihood of depression was significantly lower among nurses working on rotating shifts compared to those on fixed shifts (OR=0.47, 95% CI, 0.25, 0.89, P=0.020) and among nurses with a BMI>25 compared to those with a BMI<25 (OR=0.65, 95% CI, 0.41, 1.01, P=0.056) (Table 3).
Discussion
Nursing is a demanding and stressful profession that often involves long working hours, high patient loads, and emotionally challenging situations. As a result, nurses may experience various mental health issues, including depression and anxiety. Emerging research suggests that these psychological conditions may be associated with GI symptoms among nurses [22, 23]. Our findings revealed that 10.2% of nurses experienced depression, and 25.4% reported anxiety. Moreover, most of these cases fell within the mild to moderate range of severity. Depression was notably elevated among nurses who possessed over 5 years of work experience and those with underlying diseases. Similarly, anxiety levels were found to be higher among nurses with higher levels of education, more than five years of work experience, fixed shift schedules and underlying diseases.
In the study conducted by Kaushik et al. the prevalence of mental health problems among nurses was found to be significant, in which 70.8% and 74% had depression and anxiety, respectively. The factors influencing perceived job stress among nurses varied depending on their workplace settings, with notable differences observed between those employed in government and private hospitals [24]. Job satisfaction is among the most significant factors influencing anxiety and stress levels [25, 26]. Various studies reported a very high prevalence of depression and anxiety among nurses compared to our findings [27, 28]. These differences result from sample characteristics, such as geographical location and demographic composition, which can impact prevalence rates due to variations in healthcare systems and societal factors. Importantly, it should be noted that we did not categorize nurses based on their specific wards within hospitals. Various studies have shown that nurses face significant stress and anxiety due to conflicts with doctors, colleagues, patients, and supervisors. Other stressors include patient suffering, workplace conditions, fear of infectious diseases, lack of personal time, inadequate pay, and high workloads, which can affect nurses' mental health [29, 30]. We observed that anxiety was more commonly reported among nurses with longer years of work experience, higher education levels, and fixed shift schedules.
According to our findings, the prevalence of GI symptoms was 16.7%, with a notable frequency of abdominal pain, gastroesophageal reflux, and nausea reported, respectively. Approximately 14.1% of participants experienced at least one GI symptom, while around 1% of nurses reported having more than three GI symptoms. We found a significant association between depression and anxiety with GI symptoms. Hwang et al. revealed that all healthcare workers experienced varying degrees of GI symptoms, with 47% reporting at least one severe GI symptom. The study highlighted a high prevalence of GI symptoms among nurses working rotating shifts, particularly those experiencing anxiety, stress and poor sleep quality [14].
Shift workers often undergo disruptions in their meal patterns, which may involve skipping meals, eating at unconventional times, and consuming higher amounts of fatty foods and caffeine. These dietary habits can cause disturbances in GI activity and function, ultimately contributing to an increased prevalence of GI problems among shift workers [31, 32]. The differences between our findings and those previously reported in shift schedules may be attributed to the fact that we did not differentiate between different shifts, including day, evening, and night. Individuals working night shifts face an increased risk of various health issues due to disruptions in their circadian rhythm, which can affect sleep patterns, hormone regulation, and metabolism [33].
The presence of psychological distress has been found to exacerbate GI symptoms through its impact on hormone secretion, including cortisol and serotonin [34, 35]. Additionally, psychological distress can induce visceral hypersensitivity and hyperalgesia, thereby contributing to the development of GI disorders [36, 37]. Nagarethinam et al. reported that being easily stressed and female gender emerged as independent predictors of GI symptoms [38]. The current study demonstrated that the scores of depression and anxiety were significantly higher among nurses with GI symptoms by increasing the years of working in the hospital. Given the close relationship between psychological well-being and GI symptoms, it is imperative to implement comprehensive strategies that simultaneously address the detection and management of psychological distress as well as the control of GI symptoms.
The present study highlighted the significant influence of nurses’ psychological well-being on GI symptoms. In comparison to previous research, we observed a lower frequency of GI symptoms, depression and anxiety, which may be attributed to differences in sample characteristics, measurement tools, and study design. However, it is important to acknowledge limitations such as our study’s cross-sectional design, which restricts our ability to establish causal relationships between psychological status and GI symptoms. Additionally, the lack of categorization of nurses based on specific units or departments of work and different shifts (day or night shifts) limited our understanding of how different work environments may contribute to variations in GI symptoms and psychological distress.
Conclusion
The current study revealed a notable association between psychological distress and the occurrence of GI symptoms, underscoring the importance of addressing both aspects to enhance nurses’ overall health and quality of life. However, it is crucial to acknowledge that further research is necessary to investigate the causal relationships and potential contributing factors underlying these findings.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1402.318). Informed consent was obtained from participants, a parent, and or legal guardians.
Funding
This study was extracted from a sub-specialty thesis of Behnam Masihipour, approved by Guilan University of Medical Sciences, Rasht, Iran (Code: 1464) and financially supported by Research Council of Guilan University of Medical Sciences.
Authors contributions
Supervision: Farahnaz Joukar and Kourosh Mojtahedi; Methodology: Kourosh Mojtahedi, Behnam Masihipour, Fariborz Mansour-Ghanaei and Farahnaz Joukar; Investigation: Kourosh Mojtahedi, Behnam Masihipour, Fariborz Mansour-Ghanaei and Farahnaz Joukar; Writing the original draft: Behnam Masihipour, Adele Isanazar and Kourosh Mojtahedi; Data collection: Saman Maroufizadeh, Mehrnaz Asgharnezhad and Soheil Hassanipour; Data analysis: Saman Maroufizadeh, Soheil Hassanipour, Mehrnaz Asgharnezhad and Farahnaz Joukar; Review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
The role of the gut-brain axis in maintaining a healthy status is significant [1]. The gut-brain axis is a bidirectional communication network between the gastrointestinal (GI) tract and the central nervous system, involving neural, hormonal and immune pathways [2, 3]. Dysregulation of the gut-brain axis can alter gut motility, secretion, and permeability, as well as changes in neurotransmitter signaling and immune function, all of which have been implicated in the pathophysiology of psychological and GI disorders [4, 5]. The prevalence of anxiety among individuals in different occupations can vary based on various factors, including the nature of their work, the demands of their job and the hours of working. Shift work, irregular working hours and long shifts are often associated with increased levels of anxiety due to disruptions in circadian rhythms, sleep disturbances, and challenges in achieving work-life balance [6, 7].
Healthcare workers, including nurses, physicians and other medical professionals, often work long and irregular hours, including night shifts and weekend rotations. Nurses often encounter high levels of stress during their shifts, which can lead to various complications and chronic health issues [8, 9]. The nursing profession is characterized by significant stress, demands and challenges, with job-related stress being closely associated with elevated rates of depression. Studies indicate that nurses encounter depressive symptoms at a rate double that of individuals in various other occupations [10, 11]. The demanding nature of their work, long hours, frequent exposure to emotionally challenging situations, and making critical decisions under pressure can contribute to elevated stress levels and burnout in nurses [12, 13].
Chronic stress and anxiety can manifest physically, leading to GI symptoms (with a frequency of 43%), such as abdominal discomfort, bloating, nausea, and changes in bowel habits [14]. Additionally, poor dietary habits, irregular meal times and inadequate hydration due to the fast-paced nature of nursing work can further exacerbate GI issues among nurses [15]. About 58.8% of depression and 62% of anxiety were reported among shift nurses [7]. Since it is crucial for healthcare institutions to prioritize measures to support nurses’ mental and physical well-being to mitigate the impact of stress-related complications on their health, we investigated the association between depression and anxiety with GI symptoms and the related factors among nurses in different wards of hospitals in Rasht City, Iran.
Materials and Methods
Study design
This cross-sectional study was conducted on 460 nurses working in educational and medical hospitals affiliated with the Guilan University of Medical Sciences, Rasht, Iran, in 2024. These hospitals included Heshmat Hospital (n=82 nurses), Razi Hospital (n=113 nurses), Poursina Hospital (n=116 nurses), Amir Al-Momenin Hospital (n=26 nurses), 17-Shahrivar Hospital (n=50 nurses), Velayat Hospital (n=33 nurses) and Alzahra Hospital (n=40 nurses). Participants were selected for the study using stratified and cluster random sampling methods. All individuals gave their informed consent to participate in the study. Clinical and demographical data of participants, including age, gender, marital status (single/married), educational level (bachelor/master), work experience (years), shifts (fix/rotating), professional position (nurse/head nurse), history of smoking, alcohol consumption, body mass index (BMI) (underweight <18.5 kg/m2, normal weight=18.5–24.99 kg/m2, overweight=25–29.9 kg/m2 and obese ≥30 kg/m2), underlying diseases, history of consulting a psychologist or psychiatrist, using sedatives, antianxiety, or antidepressants, GI symptoms and numbers of GI symptoms were recorded. A gastroenterologist confirmed that all GI symptoms were not structural. GI symptoms included nausea, gastroesophageal reflux, diarrhea, constipation, vomiting, flatulence, GI bleeding, abdominal pain, jaundice and weight loss. The status of anxiety and depression was assessed under the supervision of a psychiatrist. The depression, anxiety and stress scale-21 (DASS-21) was used to assess the negative emotional states of depression and anxiety in participants, which was previously confirmed for validity and reliability in several studies [16–18].
Depression anxiety and stress scale-21 item (DASS-21)
The DASS-21 is a short form of DASS, which is a self-report instrument composed of three subscales: Depression, anxiety and stress [19]. This scale consists of three 7-item subscales, each rated on a 4-point Likert scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time). Because the DASS 21 is a short version of the original DASS (the long form has 42 items), the final score of each subscale must be multiplied by two. Therefore, all subscale scores can range from 0 to 42, with higher scores indicating greater levels of depression, anxiety, and stress. A total score of 10 or more indicates mild to severe depression, a score of 8 or more indicates mild to severe anxiety and a score of 15 or more indicates mild to severe stress. The Persian version of this scale is reported to have satisfactory psychometric properties among health professionals [20]. In this study, the cronbach α values for depression and anxiety subscales were 0.835 and 0.700, respectively.
Statistical analysis
Based on Haug et al.’s study [21] showing a 48% prevalence of GI issues, the sample size calculation initially yielded 383 participants. Accounting for cluster sampling, this was multiplied by a 1.2 design effect, resulting in a final sample of 460. The calculation used select-statistics software, assuming a 95% confidence level, 5% error margin and 48% prevalence.
Variables were presented as percentage, frequency, Mean±SD, median and interquartile range (IQR). The Kolmogorov-Smirnov test was employed to assess the assumption of normality for depression and anxiety. To compare the prevalence of depression and anxiety across personal and occupational characteristics of nurses, the Chi-Square test (or Fisher exact test) was utilized. Additionally, logistic regression was applied to examine the relationship between personal and occupational characteristics and depression and anxiety. Mean scores of depression and anxiety among nurses with and without GI symptoms were compared using the Mann-Whitney test. Both simple logistic regression and multiple logistic regression analyses, in both unadjusted and adjusted formats, were conducted to ascertain the relationship between depression and anxiety disorders with GI symptoms, respectively. The findings of these analyses were presented as crude odds ratios (OR) and adjusted odds ratios (aOR) alongside 95% confidence intervals (95% CI). Data analysis was conducted using SPSS software, version 16, with a significance level set at 0.05. GraphPad Prism software, version 8.0.1 was also utilized for graphing purposes.
Results
The mean age of participants was 30.08±7.43 years, of which 37.8% were ≤30 years. Most of the participants were females (95.9%). Among participants, 12.2% used sedative, antianxiety, or antidepressant drugs. Their mean work experience was 10.02±7.53 years, of which 42.8% had more than 10 years of work experience. Their mean BMI was 25.02±2.93 kg/m2, of which 49.1% had normal BMI (Table 1).
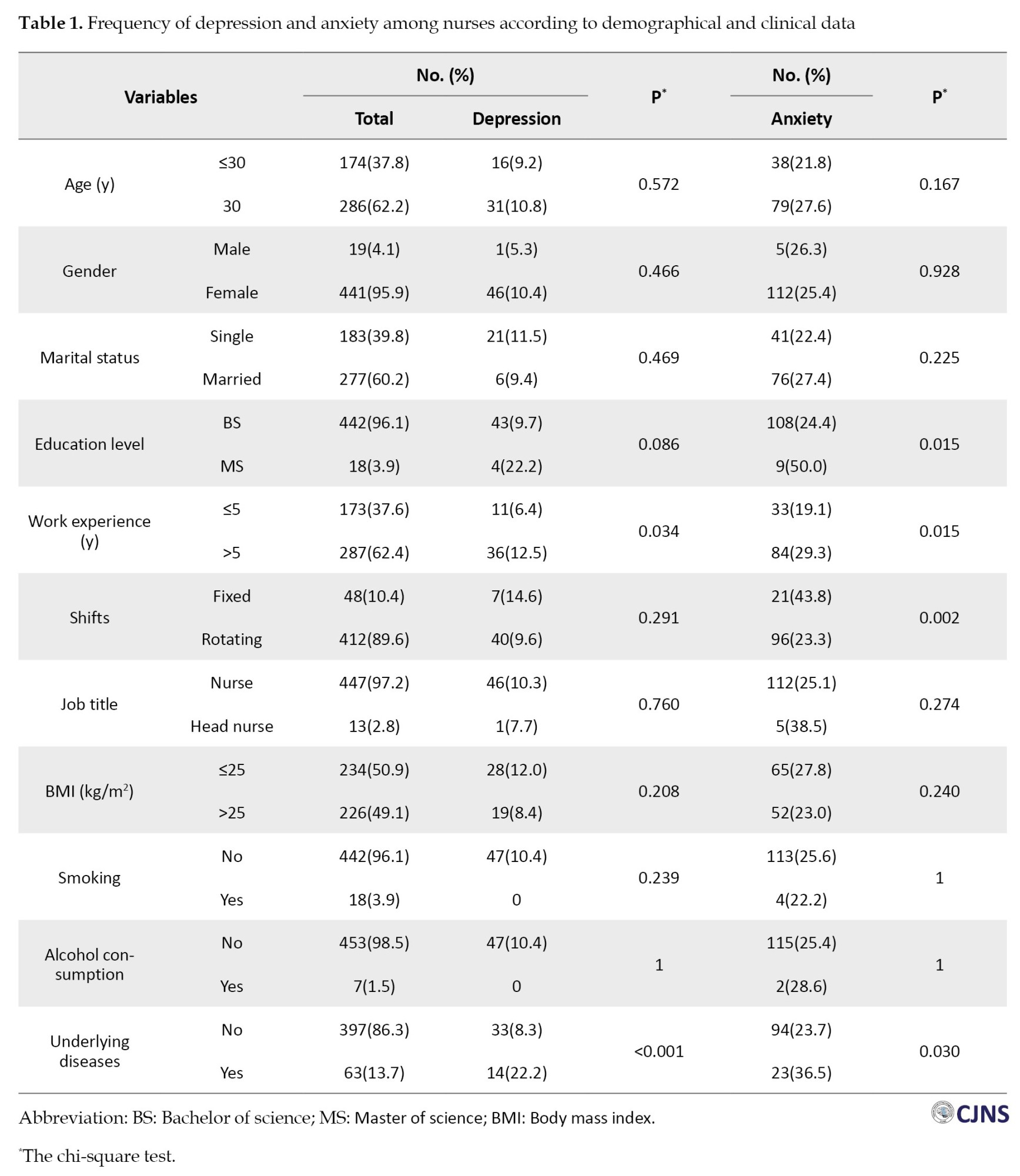
According to the DASS-21 questionnaire, the mean depression score among nurses was 2.50±4.53, with a median score of zero (IQR: 0.2-0) and a frequency of 10.2%. A total of 47(10.2%) were identified as experiencing depression, categorized as mild in 22 cases (4.8%), moderate in 21(4.6%) and severe in 4(0.9%). The average anxiety score was 4.57±5.59, with a median score of 0.4 (IQR: 0.8-0.8) and a prevalence of 25.4%. A total of 117 participants (25.4%) reported experiencing anxiety, with 33(7.2%) classified as mild, 60(13.6%) as moderate, 13(2.8%) as severe and 11(2.4%) as very severe (Figure 1). The frequency of depression and anxiety was significantly higher among nurses with more than five years of work experience and a history of underlying diseases (P<0.05). Furthermore, nurses with upper education and fixed shifts significantly reported more anxiety compared to others (P<0.05) (Table 1).
The reported prevalence of GI symptoms among all participants was 16.7%. The most frequently reported GI symptoms included abdominal pain (5.9%, n=27), gastroesophageal reflux (3.9%, n=18), nausea (3.5%, n=16), flatulence (2.8%, n=13), and constipation (2.6%, n=12). Less common symptoms were vomiting (0.9%, n=4), weight loss (0.7%, n=3), diarrhea (0.4%, n=2), and GI bleeding (0.2%, n=1). Notably, jaundice was not observed in any participant. About 14.1% (n=65) experienced one symptom, 1.5% (n=7) had two symptoms, 0.7% (n=3) had three symptoms, and 0.4% (n=2) reported four GI symptoms (Figure 2). The prevalence of depression and anxiety was significantly higher among individuals with GI symptoms (P<0.05) (Table 2 and Figure 3). For each one-unit increase in nurses’ depression and anxiety scores, there was a corresponding 7% and 5% increase in the likelihood of experiencing GI symptoms (Table 2).
The odds of experiencing depression among married nurses were found to be 70% lower compared to singles (OR=0.30, 95% CI, 0.14, 0.65, P=0.002). Similarly, nurses with work experience of more than 5 years exhibited a 3.95-fold higher likelihood of depression in comparison to those with five years or less (OR=3.95, 95% CI, 1.63, 9.57, P=0.002). Nurses with underlying diseases demonstrated a 3.04-fold increased likelihood of depression relative to those without underlying health conditions (OR=3.04, 95% CI, 1.47, 6.29, P=0.003) (Table 3).
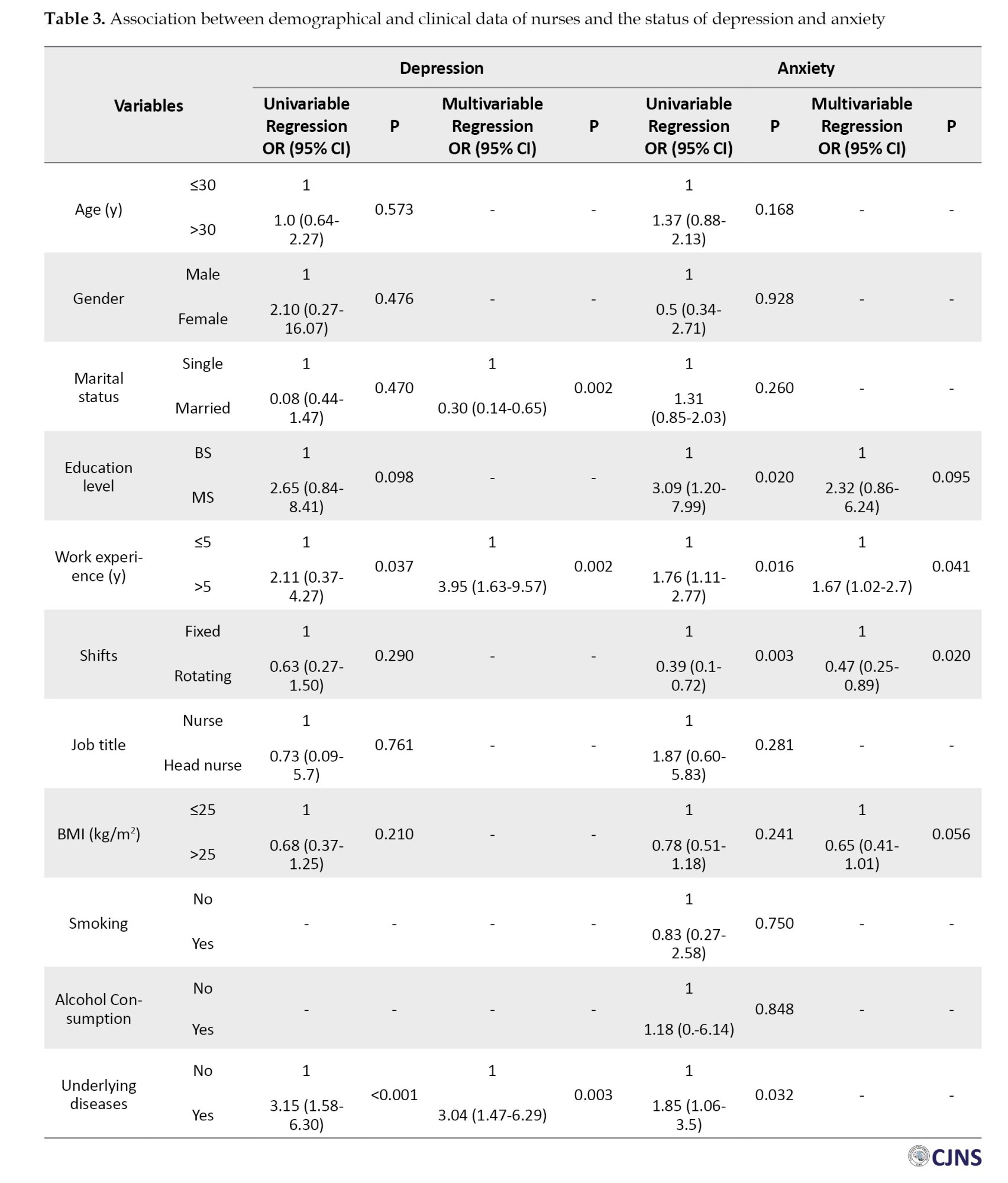
The odds of developing anxiety among nurses with a master’s degree were found to be 2.32 times higher compared to nurses with a bachelor’s degree (OR=2.32, 95% CI, 0.86, 6.24, P=0.095). Similarly, nurses with work experience of more than 5 years exhibited a 67% higher likelihood of anxiety compared to those with work experience of five years or less (OR=1.67, 95% CI, 1.02, 2.72, P=0.041). Furthermore, the likelihood of depression was significantly lower among nurses working on rotating shifts compared to those on fixed shifts (OR=0.47, 95% CI, 0.25, 0.89, P=0.020) and among nurses with a BMI>25 compared to those with a BMI<25 (OR=0.65, 95% CI, 0.41, 1.01, P=0.056) (Table 3).
Discussion
Nursing is a demanding and stressful profession that often involves long working hours, high patient loads, and emotionally challenging situations. As a result, nurses may experience various mental health issues, including depression and anxiety. Emerging research suggests that these psychological conditions may be associated with GI symptoms among nurses [22, 23]. Our findings revealed that 10.2% of nurses experienced depression, and 25.4% reported anxiety. Moreover, most of these cases fell within the mild to moderate range of severity. Depression was notably elevated among nurses who possessed over 5 years of work experience and those with underlying diseases. Similarly, anxiety levels were found to be higher among nurses with higher levels of education, more than five years of work experience, fixed shift schedules and underlying diseases.
In the study conducted by Kaushik et al. the prevalence of mental health problems among nurses was found to be significant, in which 70.8% and 74% had depression and anxiety, respectively. The factors influencing perceived job stress among nurses varied depending on their workplace settings, with notable differences observed between those employed in government and private hospitals [24]. Job satisfaction is among the most significant factors influencing anxiety and stress levels [25, 26]. Various studies reported a very high prevalence of depression and anxiety among nurses compared to our findings [27, 28]. These differences result from sample characteristics, such as geographical location and demographic composition, which can impact prevalence rates due to variations in healthcare systems and societal factors. Importantly, it should be noted that we did not categorize nurses based on their specific wards within hospitals. Various studies have shown that nurses face significant stress and anxiety due to conflicts with doctors, colleagues, patients, and supervisors. Other stressors include patient suffering, workplace conditions, fear of infectious diseases, lack of personal time, inadequate pay, and high workloads, which can affect nurses' mental health [29, 30]. We observed that anxiety was more commonly reported among nurses with longer years of work experience, higher education levels, and fixed shift schedules.
According to our findings, the prevalence of GI symptoms was 16.7%, with a notable frequency of abdominal pain, gastroesophageal reflux, and nausea reported, respectively. Approximately 14.1% of participants experienced at least one GI symptom, while around 1% of nurses reported having more than three GI symptoms. We found a significant association between depression and anxiety with GI symptoms. Hwang et al. revealed that all healthcare workers experienced varying degrees of GI symptoms, with 47% reporting at least one severe GI symptom. The study highlighted a high prevalence of GI symptoms among nurses working rotating shifts, particularly those experiencing anxiety, stress and poor sleep quality [14].
Shift workers often undergo disruptions in their meal patterns, which may involve skipping meals, eating at unconventional times, and consuming higher amounts of fatty foods and caffeine. These dietary habits can cause disturbances in GI activity and function, ultimately contributing to an increased prevalence of GI problems among shift workers [31, 32]. The differences between our findings and those previously reported in shift schedules may be attributed to the fact that we did not differentiate between different shifts, including day, evening, and night. Individuals working night shifts face an increased risk of various health issues due to disruptions in their circadian rhythm, which can affect sleep patterns, hormone regulation, and metabolism [33].
The presence of psychological distress has been found to exacerbate GI symptoms through its impact on hormone secretion, including cortisol and serotonin [34, 35]. Additionally, psychological distress can induce visceral hypersensitivity and hyperalgesia, thereby contributing to the development of GI disorders [36, 37]. Nagarethinam et al. reported that being easily stressed and female gender emerged as independent predictors of GI symptoms [38]. The current study demonstrated that the scores of depression and anxiety were significantly higher among nurses with GI symptoms by increasing the years of working in the hospital. Given the close relationship between psychological well-being and GI symptoms, it is imperative to implement comprehensive strategies that simultaneously address the detection and management of psychological distress as well as the control of GI symptoms.
The present study highlighted the significant influence of nurses’ psychological well-being on GI symptoms. In comparison to previous research, we observed a lower frequency of GI symptoms, depression and anxiety, which may be attributed to differences in sample characteristics, measurement tools, and study design. However, it is important to acknowledge limitations such as our study’s cross-sectional design, which restricts our ability to establish causal relationships between psychological status and GI symptoms. Additionally, the lack of categorization of nurses based on specific units or departments of work and different shifts (day or night shifts) limited our understanding of how different work environments may contribute to variations in GI symptoms and psychological distress.
Conclusion
The current study revealed a notable association between psychological distress and the occurrence of GI symptoms, underscoring the importance of addressing both aspects to enhance nurses’ overall health and quality of life. However, it is crucial to acknowledge that further research is necessary to investigate the causal relationships and potential contributing factors underlying these findings.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1402.318). Informed consent was obtained from participants, a parent, and or legal guardians.
Funding
This study was extracted from a sub-specialty thesis of Behnam Masihipour, approved by Guilan University of Medical Sciences, Rasht, Iran (Code: 1464) and financially supported by Research Council of Guilan University of Medical Sciences.
Authors contributions
Supervision: Farahnaz Joukar and Kourosh Mojtahedi; Methodology: Kourosh Mojtahedi, Behnam Masihipour, Fariborz Mansour-Ghanaei and Farahnaz Joukar; Investigation: Kourosh Mojtahedi, Behnam Masihipour, Fariborz Mansour-Ghanaei and Farahnaz Joukar; Writing the original draft: Behnam Masihipour, Adele Isanazar and Kourosh Mojtahedi; Data collection: Saman Maroufizadeh, Mehrnaz Asgharnezhad and Soheil Hassanipour; Data analysis: Saman Maroufizadeh, Soheil Hassanipour, Mehrnaz Asgharnezhad and Farahnaz Joukar; Review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, et al. The microbiota-gut-brain axis. Physiol Rev. 2019; 99(4):1877-2013. [DOI:10.1152/physrev.00018.2018] [PMID]
- Appleton J. The gut-brain axis: Influence of microbiota on mood and mental health. Integr Med. 2018; 17(4):28-32. [PMID]
- Person H, Keefer L. Psychological comorbidity in gastrointestinal diseases: Update on the brain-gut-microbiome axis. Prog Neuropsychopharmacol Biol Psychiatry. 2021; 107:110209. [DOI:10.1016/j.pnpbp.2020.110209] [PMID] [PMCID]
- Martin CR, Osadchiy V, Kalani A, Mayer EA. The brain-gut-microbiome axis. Cell Mol Gastroenterol Hepatol. 2018; 6(2):133-48. [DOI:10.1016/j.jcmgh.2018.04.003] [PMID] [PMCID]
- Suganya K, Koo BS. Gut-brain axis: Role of gut microbiota on neurological disorders and how probiotics/prebiotics beneficially modulate microbial and immune pathways to improve brain functions. Int J Mol Sci. 2020; 21(20):7551. [DOI:10.3390/ijms21207551] [PMID] [PMCID]
- Ferri P, Guadi M, Marcheselli L, Balduzzi S, Magnani D, Di Lorenzo R. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Manag Healthc Policy. 2016; 9:203-11. [DOI:10.2147/RMHP.S115326] [PMID] [PMCID]
- Li Y, Wang Y, Lv X, Li R, Guan X, Li L, et al. Effects of factors related to shift work on depression and anxiety in nurses. Front Public Health. 2022; 10:926988. [DOI:10.3389/fpubh.2022.926988] [PMID] [PMCID]
- Roman P, Perez-Cayuela I, Gil-Hernández E, Rodriguez-Arrastia M, Aparicio-Mota A, Ropero-Padilla C, et al. Influence of shift work on the health of nursing professionals. J Pers Med. 2023; 13(4):627. [DOI:10.3390/jpm13040627] [PMID] [PMCID]
- Al-Hrinat J, Al-Ansi AM, Hendi A, Adwan G, Hazaimeh M. The impact of night shift stress and sleep disturbance on nurses quality of life: Case in Palestine red crescent and Al-Ahli Hospital. BMC Nurs. 2024; 23(1):24. [DOI:10.1186/s12912-023-01673-3] [PMID] [PMCID]
- Letvak S, Ruhm CJ, McCoy T. Depression in hospital-employed nurses. Clin Nurse Spec. 2012; 26(3):177-82. [DOI:10.1097/NUR.0b013e3182503ef0] [PMID]
- Ganu P. Women’s safety and health issues at work. J Health Manag. 2004; 6(2):220-1. [DOI:10.1177/097206340400600214]
- Dall'Ora C, Ball J, Reinius M, Griffiths P. Burnout in nursing: A theoretical review. Hum Resour Health. 2020; 18(1):41. [DOI:10.1186/s12960-020-00469-9] [PMID] [PMCID]
- Ashipala DO, Nghole TM. Factors contributing to burnout among nurses at a district hospital in Namibia: A qualitative perspective of nurses. J Nurs Manag. 2022; 30(7):2982-91. [DOI:10.1111/jonm.13693] [PMID] [PMCID]
- Hwang SK, Lee YJ, Cho ME, Kim BK, Yoon YI. Factors associated with gastrointestinal symptoms among rotating shift nurses in South Korea: A cross-sectional study. Int J Environ Res Public Health. 2022; 19(16):9795. [DOI:10.3390/ijerph19169795] [PMID] [PMCID]
- Gifkins J, Johnston A, Loudoun R. The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiol Int. 2018; 35(6):811-820. [DOI:10.1080/07420528.2018.1466790] [PMID]
- Ali AM, Alkhamees AA, Hori H, Kim Y, Kunugi H. The depression anxiety stress scale 21: Development and validation of the depression anxiety stress scale 8-item in psychiatric patients and the general public for easier mental health measurement in a post COVID-19 world. Int J Environ Res Public Health. 2021; 18(19):10142. [DOI:10.3390/ijerph181910142] [PMID] [PMCID]
- Zanon C, Brenner RE, Baptista MN, Vogel DL, Rubin M, Al-Darmaki FR, et al. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress scale-21 (DASS-21) across eight countries. Assessment. 2021; 28(6):1531-44. [DOI:10.1177/1073191119887449] [PMID]
- Asghari A, Saed F, Dibajnia P. Psychometric properties of the depression anxiety stress scales-21 (DASS-21) in a non-clinical Iranian sample. Int J psychol. 2008; 2(2):82-102. [Link]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995; 33(3):335-43. [DOI:10.1016/0005-7967(94)00075-U] [PMID]
- Kakemam E, Navvabi E, Albelbeisi AH, Saeedikia F, Rouhi A, Majidi S. Psychometric properties of the Persian version of depression anxiety stress scale-21 items (DASS-21) in a sample of health professionals: A cross-sectional study. BMC Health Serv Res. 2022; 22(1):111. [DOI:10.1186/s12913-022-07514-4] [PMID] [PMCID]
- Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol. 2002; 37(3):294-8. [DOI:10.1080/003655202317284192] [PMID]
- Nagel C, Nilsson K. Nurses' work-related mental health in 2017 and 2020-A comparative follow-up study before and during the COVID-19 pandemic. Int J Environ Res Public Health. 2022; 19(23):15569. [DOI:10.3390/ijerph192315569] [PMID] [PMCID]
- Liu T, Liu J, Wang C, Zou D, Wang C, Xu T, et al. Prevalence of gastrointestinal symptoms and their association with psychological problems in youths. Ann Palliat Med. 2023; 12(2):311-23. [DOI:10.21037/apm-22-1316] [PMID]
- Kaushik A, Ravikiran SR, Suprasanna K, Nayak MG, Baliga K, Acharya SD. Depression, anxiety, stress and workplace stressors among nurses in tertiary health care settings. Indian J Occup Environ Med. 2021; 25(1):27-32. [DOI:10.4103/ijoem.IJOEM_123_20] [PMID] [PMCID]
- Davey A, Sharma P, Davey S, Shukla A. Is work-associated stress converted into psychological distress among the staff nurses: A hospital-based study. J Family Med Prim Care. 2019; 8(2):511-6. [DOI:10.4103/jfmpc.jfmpc_419_16] [PMID] [PMCID]
- Saquib N, Zaghloul MS, Saquib J, Alhomaidan HT, Al-Mohaimeed A, Al-Mazrou A. Association of cumulative job dissatisfaction with depression, anxiety and stress among expatriate nurses in Saudi Arabia. J Nurs Manag. 2019; 27(4):740-8. [DOI:10.1111/jonm.12762] [PMID]
- Cheung T, Yip PS. Depression, anxiety and symptoms of stress among Hong Kong nurses: A cross-sectional study. Int J Environ Res Public Health. 2015; 12(9):11072-100. [DOI:10.3390/ijerph120911072] [PMID] [PMCID]
- Tran TTT, Nguyen NB, Luong MA, Bui THA, Phan TD, Tran VO, et al. Stress, anxiety and depression in clinical nurses in Vietnam: A cross-sectional survey and cluster analysis. Int J Ment Health Syst. 2019; 13:3. [DOI:10.1186/s13033-018-0257-4] [PMID] [PMCID]
- Starc J. Stress factors among nurses at the primary and secondary level of public sector health care: The case of slovenia. Open Access Maced J Med Sci. 2018; 6(2):416-22. [DOI:10.3889/oamjms.2018.100] [PMID] [PMCID]
- Semachew A, Belachew T, Tesfaye T, Adinew YM. Predictors of job satisfaction among nurses working in Ethiopian public hospitals, 2014: Institution-based cross-sectional study. Hum Resour Health. 2017; 15(1):31. [DOI:10.1186/s12960-017-0204-5] [PMID] [PMCID]
- Khan S, Duan P, Yao L, Hou H. Shiftwork-mediated disruptions of circadian rhythms and sleep homeostasis cause serious health problems. Int J Genomics. 2018; 2018:8576890. [DOI:10.1155/2018/8576890] [PMID] [PMCID]
- Gupta CC, Centofanti S, Dorrian J, Coates AM, Stepien JM, Kennaway D, et al. Subjective hunger, gastric upset, and sleepiness in response to altered meal timing during simulated shiftwork. Nutrients. 2019 11(6):1352. [DOI:10.3390/nu11061352] [PMID] [PMCID]
- Streng AA, Loef B, Dollé MET, van der Horst GTJ, Chaves I, Proper KI, et al. Night shift work characteristics are associated with several elevated metabolic risk factors and immune cell counts in a cross-sectional study. Sci Rep. 2022; 12(1):2022. [DOI:10.1038/s41598-022-06122-w] [PMID] [PMCID]
- Leigh SJ, Uhlig F, Wilmes L, Sanchez-Diaz P, Gheorghe CE, Goodson MS, et al. The impact of acute and chronic stress on gastrointestinal physiology and function: A microbiota-gut-brain axis perspective. J Physiol. 2023; 601(20):4491-538. [DOI:10.1113/JP281951] [PMID]
- Foster JA, Rinaman L, Cryan JF. Stress & the gut-brain axis: Regulation by the microbiome. Neurobiol Stress. 2017; 7:124-36. [DOI:10.1016/j.ynstr.2017.03.001] [PMID] [PMCID]
- Tseng P, Wu M. Altered circadian rhythm, sleep disturbance, and gastrointestinal dysfunction: New evidence from rotating shift workers. Adv Dig Med. 2016; 3(3):77-9. [DOI:10.1016/j.aidm.2016.05.001]
- Greenwood-Van Meerveld B, Johnson AC. Stress-induced chronic visceral pain of gastrointestinal origin. Front Syst Neurosci. 2017; 11:86. [DOI:10.3389/fnsys.2017.00086] [PMID] [PMCID]
- Nagarethinam M, Webster H, Lee SY, Con D, Shen E. Functional gastrointestinal disorders among healthcare professionals at a tertiary Australian hospital. JGH Open. 2023; 7(4):242-8. [DOI:10.1002/jgh3.12894] [PMID] [PMCID]
Type of Study: Research |
Subject:
General
Received: 2024/03/2 | Accepted: 2024/05/25 | Published: 2025/01/1
Received: 2024/03/2 | Accepted: 2024/05/25 | Published: 2025/01/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |