Mon, Dec 29, 2025
Volume 10, Issue 3 (Summer 2024)
Caspian J Neurol Sci 2024, 10(3): 210-217 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Edalatkhah R, Sazegari S, Rasoulizadeh Z. Parental Obsessive-compulsive Disorder as a Risk Factor for Pediatric Functional Abdominal Pain. Caspian J Neurol Sci 2024; 10 (3) :210-217
URL: http://cjns.gums.ac.ir/article-1-702-en.html
URL: http://cjns.gums.ac.ir/article-1-702-en.html
1- Hematology and Oncology Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Department of Pediatrics, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,rasoulizadehzahra@gmail.com
2- Department of Pediatrics, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Children Growth Disorder Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Keywords: Functional gastrointestinal disorder, Abdominal pain, Children, Obsessive-compulsive disorder
Full-Text [PDF 1134 kb]
(531 Downloads)
| Abstract (HTML) (1144 Views)
Full-Text: (380 Views)
Introduction
Functional abdominal pain (FAP) is one of the most common complaints among children. It affects approximately 25% of children and infants worldwide [1], with the highest prevalence observed in South America and Asia (16.8% and 16.5%, respectively) [2]. A child suffering from this condition may miss extended periods of school and kindergarten, experience parental anxiety, undergo many medical referrals, or undergo many diagnostic procedures as a result of significant financial burdens on the family. As no serological, mucosal, radiographic, or structural disease is evident in children with FAP, it is a diagnosis of symptoms rather than a specific cause [3]. Several factors may contribute to the development of FAP, such as interactions between the brain and gut, activation of the immune system, visceral hypersensitivity, and psychological factors.
Obsessive-compulsive disorder (OCD) is associated with excessive worrying, distress, mental preoccupation, and low self-esteem. OCD is characterized by uncontrollable repetitive thoughts (obsessions) and behaviors (compulsions), with a lifetime prevalence estimated to be between 2.3% and 3% [4]. In addition to causing significant distress and anxiety, obsessive thoughts increase the feeling of needing to engage in compulsive behaviors [5]. OCD parents tend to hide and deny their physiological disorders, which places tremendous stress on their children to conform and be loyal [6].
The cause of FAP has not been elucidated yet. Still, it is believed to be multifactorial and involves brain and gut interactions, visceral hypersensitivity, immune activation, psychological factors, and abnormal physiological responses. [7, 8]. Children with FAP suffer poorer mental status, lower SES, emotional disorders, anxiety, depression and other stressful experiences than healthy children [9]. A higher rate of anxiety, depression, and somatization is reported by the parents of children with FAP than by the parents of healthy children [10-12]. Some evidence suggests that parental anxiety may be a precursor to the development of FAP in children. During the first year of life, maternal and paternal anxiety are predicted to be associated with FAP [9, 11]. Notably, anxiety is strongly linked to the development of OCD [13]. Parental behavior is one of the most important predictors of pain-related disability in children with FAP [9].
Due to the high prevalence of FAP, it seems that parental OCD may play a significant role in pediatric FAP occurrence. However, studies on the correlation between parental mental disorders and children with FAP are limited. To the best of our knowledge, no studies have been conducted to evaluate the relationship between parental OCD and pediatric FAP. Therefore, investigating the association between parental OCD and the FAP in their siblings might provide novel insights into the concept of the FAP. Accordingly, to determine whether parental OCD and the FAP among children are related, the present case-control study was designed.
Materials and Methods
Study design and population
This gender-matched case-control study was conducted to compare the prevalence of OCD in parents of children diagnosed with or without FAP. Participants in this study were 200 parents of children (4-16 years) diagnosed with FAP (as the case group) and without FAP (as the control group) between September 2021 and September 2022. The case group included 100 parents of FAP patients referred to the Pediatric Gastroenterology Clinic of Shahid Sadougi University of Medical Sciences, Yazd City, Iran. This group was evaluated and diagnosed based on the New Rome criteria (Rome IV) [1]. All patients with FAP were diagnosed by pediatric gastroenterologists. In addition, a control group of 100 parents without FAP children was also included in the study. The children in this group were all classmates recruited from the same school as the case group. The following conditions were used as the exclusion criteria for controls: The presence of life-threatening medical disorders (e.g. diabetes, malignancies, cardiac, gastrointestinal, pulmonary, or renal disorders); other psychological disorders; history of medication use (such as chronic illness and mental disorders), treatments, pregnancy and their children had a chronic or psychological illness. Ultimately, this study recruited 188 parents (88 in the case group and 100 in the control groups) of children.
FAP detection
A pediatric gastroenterologist assessed FAP using the Rome IV criteria [14]. According to the Rome IV criteria, symptoms of FAP must occur at least four times per month for two months before a child is diagnosed:
1) Abdominal pain that is episodic or continuous and does not occur only during physiological events; 2) Do not meet the criteria for irritable bowel syndrome, functional dyspepsia, or abdominal migraines and 3) No other medical condition can fully explain symptoms after proper evaluation.
Psychological health assessment
The obsessive-compulsive inventory-revised (OCI-R), a self-report questionnaire developed by Foa et al. in 2002, consists of 18 items for diagnosing OCD [15]. The Persian version of the OCI-R was used in this study to assess various domains of OCD symptoms. This instrument consisted of six components: “Washing,” “obsessing,” “neutralizing,” “ordering,” “hoarding” and finally “checking,” each of which consisted of three items. Using a 5-point Likert scale, 18 items were rated from 0 (no distress) to 4 (extreme distress). A score of 21 or more points to the presence of OCD. There was a range of 0 to 72 in the total score. The validity of this questionnaire was determined by comparison with the Maudsley obsessive-compulsive inventory (MOCI), whose Pearson correlation coefficient was 0.61 to 0.75 for all the scales and subscales. A test re-test method was used to evaluate the reliability of the questionnaire, and the results ranged from 0.77 to 0.97 [15]. All the scales examined in the present study had reliability values ranging from 0.50 to 0.85 (according to the Cronbach α). As well as being able to distinguish OCD patients from those with other anxiety disorders (area under the curve [AUC]=0.81), it could also discriminate between those with OCD and healthy controls (AUC=0.70) [16].
Assessment of other variables
Self-administered questionnaires were used to collect other relevant information, such as age, demographic information and socioeconomic status (SES). Education level, employment status, and number of offspring were considered to assess the SES. The following information was obtained: Age, gender, health status, previous illnesses, medication history, hospitalization history for both parents and children and duration of children’s abdominal pain.
Statistical analysis
The data analysis was conducted using SPSS software, version 25 for participants who met the study inclusion criteria. Continuous variables are presented as the Mean±SD, while categorical variables are presented as frequencies and numbers. The Mann-Whitney U test was used to compare continuous variables and a chi-square test was used to compare categorical variables. The results are presented as the Mean±SD. Finally, the level of significance was set at P<0.05.
Results
Characteristics of the study population
We compared the data obtained from 88 parents of children with FAP as a case group with those of 100 parents without children diagnosed with FAP as a control group. The characteristics of the participants are illustrated in Table 1.
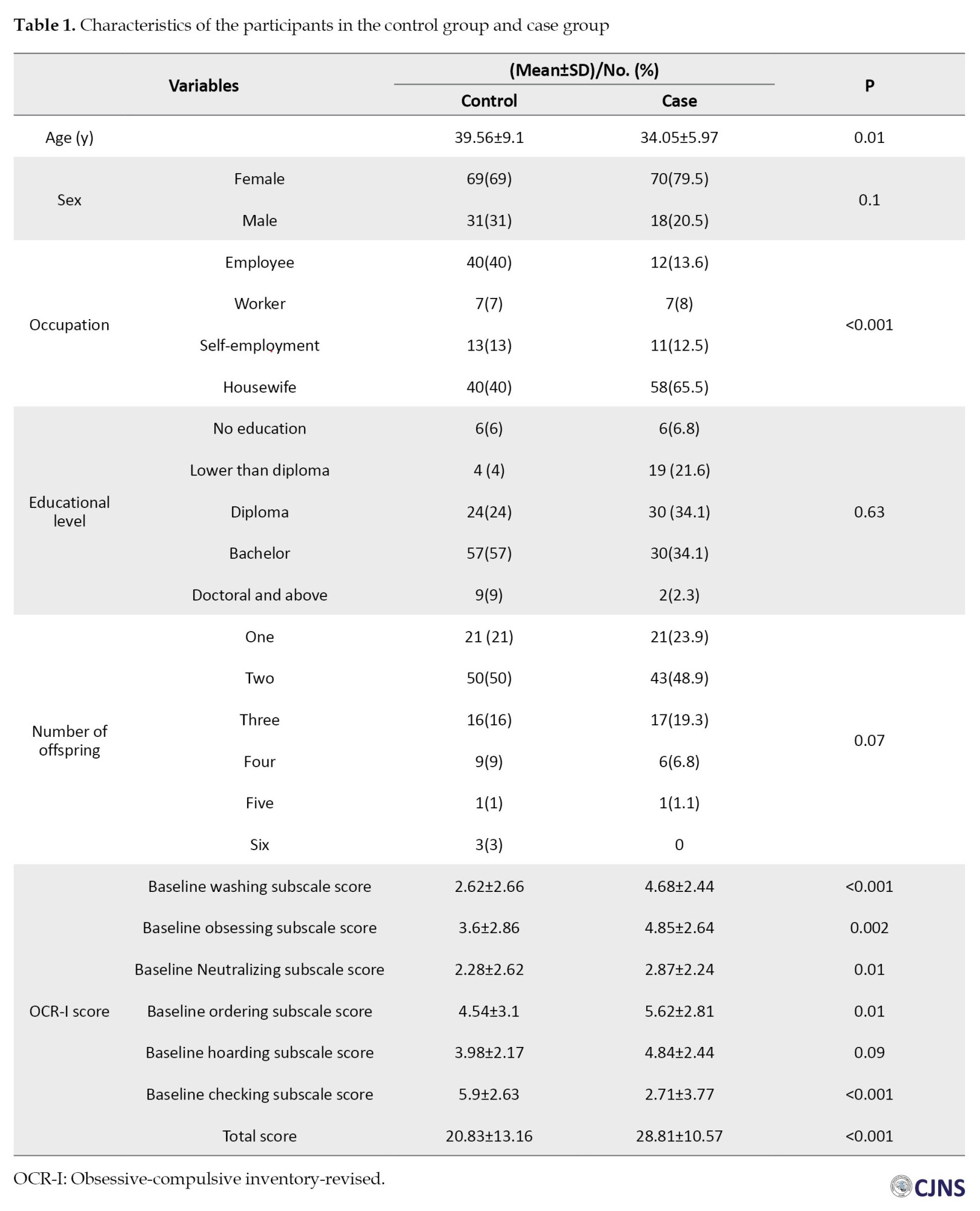
There was a significant age difference (P=0.01; the mean age of cases was 34.05±5.97 years and the mean age of the controls was 39.56±9.1 years). No significant differences were observed in gender composition between the case and control groups (cases: 79.5% female; controls: 69% female, P=0.1). The occupation and number of offspring of parents of children with FAP were significantly different from those of controls. The number of homemakers was more significant in the case group than in the control group (P<0.001). There were no significant differences in education level between the cases and controls.
The characteristics of the children in the case group and the control group are presented in Table 2.
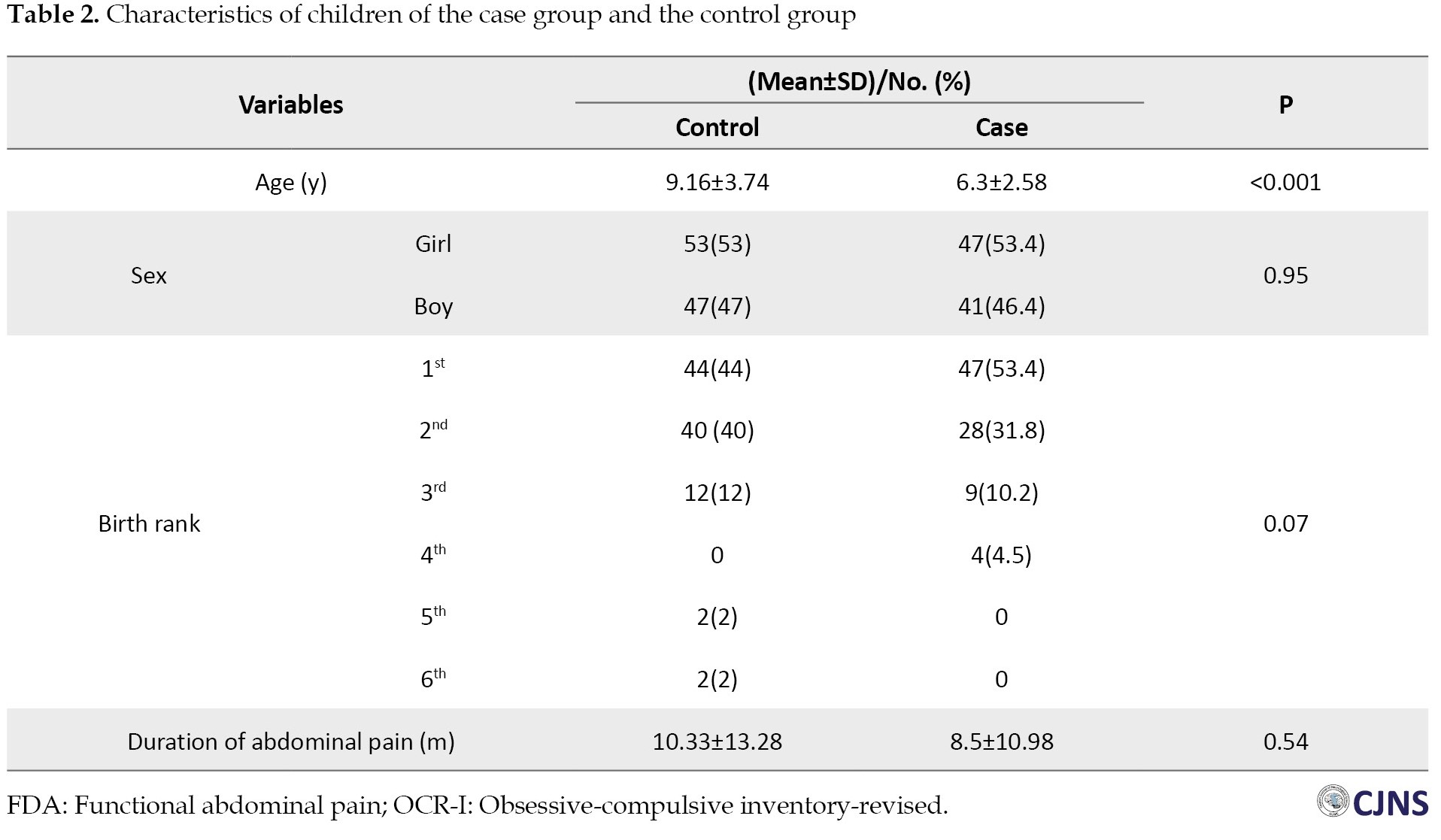
There was a significant difference in age between the case and control children (P<0.001); the mean age of the FAP children was 6.3±2.58 years, and the mean age of the controls was 9.16±3.74 years. Moreover, there were no significant differences in birth rank, gender composition, and also duration of abdominal pain between the children of the cases and controls.
OCR-I score of the participants
The baseline total OCR-I score was significantly greater in the case group than in the control group (28.81±10.57 vs 20.83±13.16; P<0.001). The baseline scores for washing, obsessing, neutralizing, ordering, and checking subscale scores were substantially higher in the cases than in the controls. The baseline hoarding subscale score did not significantly differ across cases and controls (P=0.09). A comparison of patient characteristics and OCR-I scores after controlling for gender is also presented in Table 3.

Discussion
The present study scrutinized the association between OCD in parents and the development of FAP children. Higher OCR-I total scores were observed in the parents of FAP children than in the controls. Furthermore, the study demonstrated that the scores of most components of the OCR-I were remarkably higher in the parents of children with FAP. To the best of the author’s knowledge, the present study was the first case-control study to securitize the association between parental OCD and having FAP in their children. The number of studies evaluating which psychological factors are involved in childhood FAP causation and exacerbation is so limited. Our findings showed a higher prevalence of OCD in parents of children with FAD than in parents of children without FAD.
The results of a case-control study [12] revealed that 59 mothers of children and adolescents with FAP experienced more anxiety, depression, and somatoform disorders than mothers of children without FAP. Rather than a disorder narrowly defined in terms of gastrointestinal function, FAP development in children may be better conceptualized as an emotional disorder. Mental health services are rarely utilized by mothers of children with FAP, suggesting that family attitudes toward illness and health merit investigation. A further finding of our study was that parents of children with FAP had a higher prevalence of suffering from OCD than those of control children.
Children and adults with functional GI disorders suffer from a higher level of psychological distress [10]. Stress can increase and decrease gut motility (resulting in symptoms such as fullness in the stomach and diarrhea), increase gut nerve sensitivity (inducing pain sensitivity), activate mast cells and cytokines, as well as improve gut permeability [17].
The onset of OCD symptoms is often linked to periods of stress during life or a single traumatic incident, and people with OCD frequently attribute their symptoms to psychosocial stress. OCD symptoms are exacerbated or triggered by stress and the resulting imbalance of habits and behavior [18]. Furthermore, children and adolescents with FAP experience stressful events and exhibit higher levels of stress [19, 20]. Certainly, stress can be a factor in OCD, and it can explain how parents can transmit stress to their offspring and how they can influence their perception of pain.
There was a significant association between the FAP and parental employment. The majority of parents of children with FAP are homemakers or workers rather than employees or self-employed. It has been proven that a child’s family and the health care system are both financially burdened by FAP [21, 22]. Increasingly, more children with FAP were reported to have family-related stressors than children without FAP, such as losing their parents’ jobs [19]. As a result, parents may experience worsening symptoms of OCD which can impact the progression and duration of FAP in their children. Furthermore, the SES of children is generally influenced by the family’s income, education, and occupational background. The findings showed that parental education level did not significantly correlate with the FAP in children. Nevertheless, Karunanayake et al. reported associations between FAP diseases and parental education and social status according to the parents’ profession [23]. However, Devanarayana et al. suggested a lower SES is associated with higher FAP disease prevalence [19].
The present study has several strengths. Parents of children with FAP, considered the case group, were selected from the same environment (same school) as the control group, perhaps reducing risk factors that affect the health of their children. Gender matching was also considered. We used the Rome criteria for diagnosis of the FAP, and a pediatric gastroenterologist evaluated all FAP cases. However, this study has several limitations. First, the case-control design could not explore the causal relationship between parental OCD and the development of FAP among their children. Second, given the case-control design, we could not clarify whether FAP in siblings of parents modify the risk of parental OCD or whether parental OCD influences the experiences of FAP in their children.
Conclusion
Consequently, there was a significant association between parental OCD and the FAP in their children. This study indicated that parental OCD is positively associated with the FAP in children. Hence, clinical screenings are recommended to be conducted for parental psychosocial factors such as OCD when children are diagnosed with FAP. In addition, parents should receive appropriate mental health screening and treatment. These treatments may reduce pain and disability among children with FAP and improve their health outcomes. Further longitudinal studies in different populations are needed to confirm our results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences (Code: IR.SSU.MEDICINE.REC.1400.251). The parents of the children provided their signed written informed consent.
Funding
This article was extracted from the Medical Doctor’s thesis of Sajjad Sazegari, approved by Shahid Sadoughi University of Medical Sciences (Code: 11636).
Authors contributions
Data collection: Roohollah Edalatkhah and Sajjad Sazegari; Statistical analysis: Sajjad Sazegari; Writing: Roohollah Edalatkhah and Zahra Rasoulizadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank the authorities of Shahid Sadoughi University of Medical Sciences for their support.
References
Functional abdominal pain (FAP) is one of the most common complaints among children. It affects approximately 25% of children and infants worldwide [1], with the highest prevalence observed in South America and Asia (16.8% and 16.5%, respectively) [2]. A child suffering from this condition may miss extended periods of school and kindergarten, experience parental anxiety, undergo many medical referrals, or undergo many diagnostic procedures as a result of significant financial burdens on the family. As no serological, mucosal, radiographic, or structural disease is evident in children with FAP, it is a diagnosis of symptoms rather than a specific cause [3]. Several factors may contribute to the development of FAP, such as interactions between the brain and gut, activation of the immune system, visceral hypersensitivity, and psychological factors.
Obsessive-compulsive disorder (OCD) is associated with excessive worrying, distress, mental preoccupation, and low self-esteem. OCD is characterized by uncontrollable repetitive thoughts (obsessions) and behaviors (compulsions), with a lifetime prevalence estimated to be between 2.3% and 3% [4]. In addition to causing significant distress and anxiety, obsessive thoughts increase the feeling of needing to engage in compulsive behaviors [5]. OCD parents tend to hide and deny their physiological disorders, which places tremendous stress on their children to conform and be loyal [6].
The cause of FAP has not been elucidated yet. Still, it is believed to be multifactorial and involves brain and gut interactions, visceral hypersensitivity, immune activation, psychological factors, and abnormal physiological responses. [7, 8]. Children with FAP suffer poorer mental status, lower SES, emotional disorders, anxiety, depression and other stressful experiences than healthy children [9]. A higher rate of anxiety, depression, and somatization is reported by the parents of children with FAP than by the parents of healthy children [10-12]. Some evidence suggests that parental anxiety may be a precursor to the development of FAP in children. During the first year of life, maternal and paternal anxiety are predicted to be associated with FAP [9, 11]. Notably, anxiety is strongly linked to the development of OCD [13]. Parental behavior is one of the most important predictors of pain-related disability in children with FAP [9].
Due to the high prevalence of FAP, it seems that parental OCD may play a significant role in pediatric FAP occurrence. However, studies on the correlation between parental mental disorders and children with FAP are limited. To the best of our knowledge, no studies have been conducted to evaluate the relationship between parental OCD and pediatric FAP. Therefore, investigating the association between parental OCD and the FAP in their siblings might provide novel insights into the concept of the FAP. Accordingly, to determine whether parental OCD and the FAP among children are related, the present case-control study was designed.
Materials and Methods
Study design and population
This gender-matched case-control study was conducted to compare the prevalence of OCD in parents of children diagnosed with or without FAP. Participants in this study were 200 parents of children (4-16 years) diagnosed with FAP (as the case group) and without FAP (as the control group) between September 2021 and September 2022. The case group included 100 parents of FAP patients referred to the Pediatric Gastroenterology Clinic of Shahid Sadougi University of Medical Sciences, Yazd City, Iran. This group was evaluated and diagnosed based on the New Rome criteria (Rome IV) [1]. All patients with FAP were diagnosed by pediatric gastroenterologists. In addition, a control group of 100 parents without FAP children was also included in the study. The children in this group were all classmates recruited from the same school as the case group. The following conditions were used as the exclusion criteria for controls: The presence of life-threatening medical disorders (e.g. diabetes, malignancies, cardiac, gastrointestinal, pulmonary, or renal disorders); other psychological disorders; history of medication use (such as chronic illness and mental disorders), treatments, pregnancy and their children had a chronic or psychological illness. Ultimately, this study recruited 188 parents (88 in the case group and 100 in the control groups) of children.
FAP detection
A pediatric gastroenterologist assessed FAP using the Rome IV criteria [14]. According to the Rome IV criteria, symptoms of FAP must occur at least four times per month for two months before a child is diagnosed:
1) Abdominal pain that is episodic or continuous and does not occur only during physiological events; 2) Do not meet the criteria for irritable bowel syndrome, functional dyspepsia, or abdominal migraines and 3) No other medical condition can fully explain symptoms after proper evaluation.
Psychological health assessment
The obsessive-compulsive inventory-revised (OCI-R), a self-report questionnaire developed by Foa et al. in 2002, consists of 18 items for diagnosing OCD [15]. The Persian version of the OCI-R was used in this study to assess various domains of OCD symptoms. This instrument consisted of six components: “Washing,” “obsessing,” “neutralizing,” “ordering,” “hoarding” and finally “checking,” each of which consisted of three items. Using a 5-point Likert scale, 18 items were rated from 0 (no distress) to 4 (extreme distress). A score of 21 or more points to the presence of OCD. There was a range of 0 to 72 in the total score. The validity of this questionnaire was determined by comparison with the Maudsley obsessive-compulsive inventory (MOCI), whose Pearson correlation coefficient was 0.61 to 0.75 for all the scales and subscales. A test re-test method was used to evaluate the reliability of the questionnaire, and the results ranged from 0.77 to 0.97 [15]. All the scales examined in the present study had reliability values ranging from 0.50 to 0.85 (according to the Cronbach α). As well as being able to distinguish OCD patients from those with other anxiety disorders (area under the curve [AUC]=0.81), it could also discriminate between those with OCD and healthy controls (AUC=0.70) [16].
Assessment of other variables
Self-administered questionnaires were used to collect other relevant information, such as age, demographic information and socioeconomic status (SES). Education level, employment status, and number of offspring were considered to assess the SES. The following information was obtained: Age, gender, health status, previous illnesses, medication history, hospitalization history for both parents and children and duration of children’s abdominal pain.
Statistical analysis
The data analysis was conducted using SPSS software, version 25 for participants who met the study inclusion criteria. Continuous variables are presented as the Mean±SD, while categorical variables are presented as frequencies and numbers. The Mann-Whitney U test was used to compare continuous variables and a chi-square test was used to compare categorical variables. The results are presented as the Mean±SD. Finally, the level of significance was set at P<0.05.
Results
Characteristics of the study population
We compared the data obtained from 88 parents of children with FAP as a case group with those of 100 parents without children diagnosed with FAP as a control group. The characteristics of the participants are illustrated in Table 1.
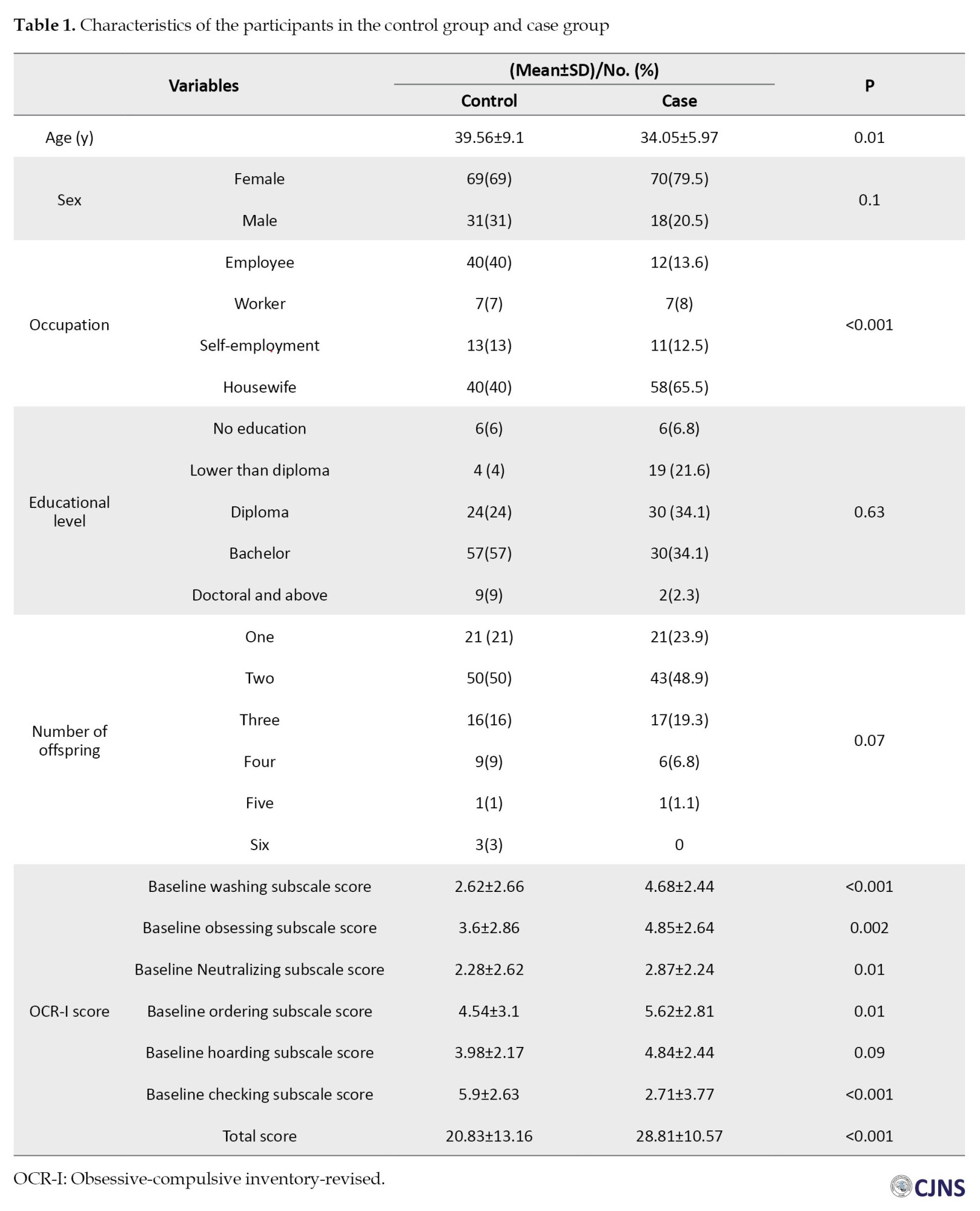
There was a significant age difference (P=0.01; the mean age of cases was 34.05±5.97 years and the mean age of the controls was 39.56±9.1 years). No significant differences were observed in gender composition between the case and control groups (cases: 79.5% female; controls: 69% female, P=0.1). The occupation and number of offspring of parents of children with FAP were significantly different from those of controls. The number of homemakers was more significant in the case group than in the control group (P<0.001). There were no significant differences in education level between the cases and controls.
The characteristics of the children in the case group and the control group are presented in Table 2.
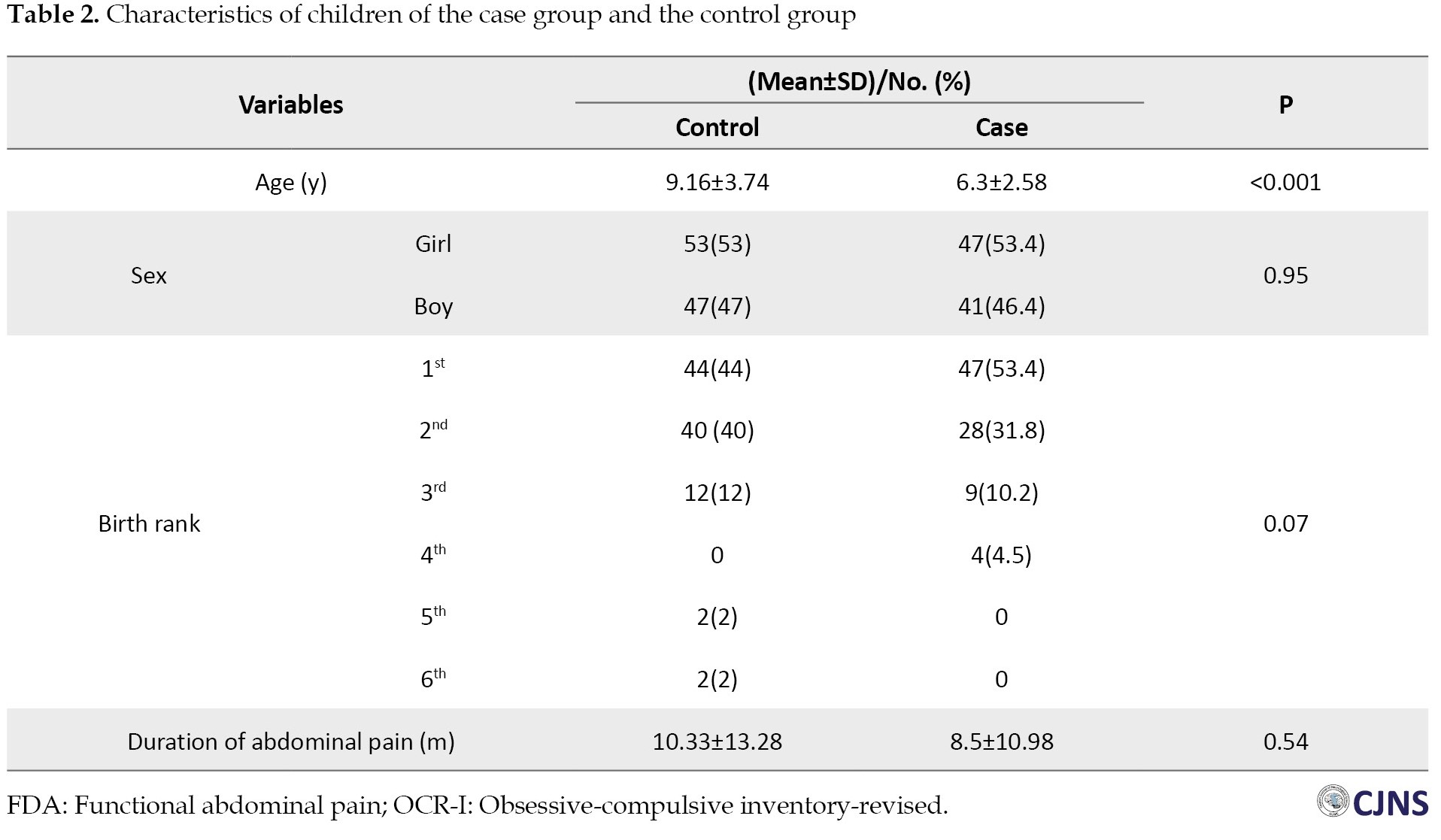
There was a significant difference in age between the case and control children (P<0.001); the mean age of the FAP children was 6.3±2.58 years, and the mean age of the controls was 9.16±3.74 years. Moreover, there were no significant differences in birth rank, gender composition, and also duration of abdominal pain between the children of the cases and controls.
OCR-I score of the participants
The baseline total OCR-I score was significantly greater in the case group than in the control group (28.81±10.57 vs 20.83±13.16; P<0.001). The baseline scores for washing, obsessing, neutralizing, ordering, and checking subscale scores were substantially higher in the cases than in the controls. The baseline hoarding subscale score did not significantly differ across cases and controls (P=0.09). A comparison of patient characteristics and OCR-I scores after controlling for gender is also presented in Table 3.

Discussion
The present study scrutinized the association between OCD in parents and the development of FAP children. Higher OCR-I total scores were observed in the parents of FAP children than in the controls. Furthermore, the study demonstrated that the scores of most components of the OCR-I were remarkably higher in the parents of children with FAP. To the best of the author’s knowledge, the present study was the first case-control study to securitize the association between parental OCD and having FAP in their children. The number of studies evaluating which psychological factors are involved in childhood FAP causation and exacerbation is so limited. Our findings showed a higher prevalence of OCD in parents of children with FAD than in parents of children without FAD.
The results of a case-control study [12] revealed that 59 mothers of children and adolescents with FAP experienced more anxiety, depression, and somatoform disorders than mothers of children without FAP. Rather than a disorder narrowly defined in terms of gastrointestinal function, FAP development in children may be better conceptualized as an emotional disorder. Mental health services are rarely utilized by mothers of children with FAP, suggesting that family attitudes toward illness and health merit investigation. A further finding of our study was that parents of children with FAP had a higher prevalence of suffering from OCD than those of control children.
Children and adults with functional GI disorders suffer from a higher level of psychological distress [10]. Stress can increase and decrease gut motility (resulting in symptoms such as fullness in the stomach and diarrhea), increase gut nerve sensitivity (inducing pain sensitivity), activate mast cells and cytokines, as well as improve gut permeability [17].
The onset of OCD symptoms is often linked to periods of stress during life or a single traumatic incident, and people with OCD frequently attribute their symptoms to psychosocial stress. OCD symptoms are exacerbated or triggered by stress and the resulting imbalance of habits and behavior [18]. Furthermore, children and adolescents with FAP experience stressful events and exhibit higher levels of stress [19, 20]. Certainly, stress can be a factor in OCD, and it can explain how parents can transmit stress to their offspring and how they can influence their perception of pain.
There was a significant association between the FAP and parental employment. The majority of parents of children with FAP are homemakers or workers rather than employees or self-employed. It has been proven that a child’s family and the health care system are both financially burdened by FAP [21, 22]. Increasingly, more children with FAP were reported to have family-related stressors than children without FAP, such as losing their parents’ jobs [19]. As a result, parents may experience worsening symptoms of OCD which can impact the progression and duration of FAP in their children. Furthermore, the SES of children is generally influenced by the family’s income, education, and occupational background. The findings showed that parental education level did not significantly correlate with the FAP in children. Nevertheless, Karunanayake et al. reported associations between FAP diseases and parental education and social status according to the parents’ profession [23]. However, Devanarayana et al. suggested a lower SES is associated with higher FAP disease prevalence [19].
The present study has several strengths. Parents of children with FAP, considered the case group, were selected from the same environment (same school) as the control group, perhaps reducing risk factors that affect the health of their children. Gender matching was also considered. We used the Rome criteria for diagnosis of the FAP, and a pediatric gastroenterologist evaluated all FAP cases. However, this study has several limitations. First, the case-control design could not explore the causal relationship between parental OCD and the development of FAP among their children. Second, given the case-control design, we could not clarify whether FAP in siblings of parents modify the risk of parental OCD or whether parental OCD influences the experiences of FAP in their children.
Conclusion
Consequently, there was a significant association between parental OCD and the FAP in their children. This study indicated that parental OCD is positively associated with the FAP in children. Hence, clinical screenings are recommended to be conducted for parental psychosocial factors such as OCD when children are diagnosed with FAP. In addition, parents should receive appropriate mental health screening and treatment. These treatments may reduce pain and disability among children with FAP and improve their health outcomes. Further longitudinal studies in different populations are needed to confirm our results.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences (Code: IR.SSU.MEDICINE.REC.1400.251). The parents of the children provided their signed written informed consent.
Funding
This article was extracted from the Medical Doctor’s thesis of Sajjad Sazegari, approved by Shahid Sadoughi University of Medical Sciences (Code: 11636).
Authors contributions
Data collection: Roohollah Edalatkhah and Sajjad Sazegari; Statistical analysis: Sajjad Sazegari; Writing: Roohollah Edalatkhah and Zahra Rasoulizadeh; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors thank the authorities of Shahid Sadoughi University of Medical Sciences for their support.
References
- Robin SG, Keller C, Zwiener R, Hyman PE, Nurko S, Saps M, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the rome IV criteria. J Pediatr. 2018; 195:134-9. [DOI:10.1016/j.jpeds.2017.12.012] [PMID]
- Korterink JJ, Diederen K, Benninga MA, Tabbers MM. Epidemiology of pediatric functional abdominal pain disorders: A meta-analysis. Plos One. 2015; 10(5):e0126982. [DOI:10.1371/journal.pone.0126982] [PMID] [PMCID]
- Quek SH. Recurrent abdominal pain in children: A clinical approach. Singapore Med J. 2015; 56(3):125-8; quiz 132. [DOI:10.11622/smedj.2015038] [PMID] [PMCID]
- Dehghan B, Saeidimehr S, Sayyah M, Rahim F. The effect of virtual reality on emotional response and symptoms provocation in patients with OCD: A systematic review and meta-analysis. Front Psychiatry. 2022; 12:733584. [DOI:10.3389/fpsyt.2021.733584] [PMID] [PMCID]
- Hirschtritt ME, Bloch MH, Mathews CA. Obsessive-compulsive disorder: Advances in diagnosis and treatment. JAMA. 2017; 317(13):1358-67. [DOI:10.1001/jama.2017.2200] [PMID]
- Belthle A, Rath L, Jungbauer J. [Impact of parental obsessive-compulsive disorder on child development - results from an in-depth interview study (German)]. Psychiatr Prax. 2022; 49(5):248-54. [DOI:10.1055/a-1577-2846] [PMID]
- Farmer AD, Aziz Q. Mechanisms and management of functional abdominal pain. J R Soc Med. 2014; 107(9):347-54. [DOI:10.1177/0141076814540880] [PMID] [PMCID]
- Bao X, Yu W, Chu Z, Gao J, Zhou M, Gu Y. Functional abdominal pain disorders in children in southern Anhui Province, China are related to academic stress rather than academic performance. BMC Pediatr. 2023; 23(1):333. [DOI:10.1186/s12887-023-04154-3] [PMID] [PMCID]
- Newton E, Schosheim A, Patel S, Chitkara DK, van Tilburg MAL. The role of psychological factors in pediatric functional abdominal pain disorders. Neurogastroenterol Motil. 2019; 31(6):e13538. [DOI:10.1111/nmo.13538] [PMID]
- van Tilburg MA, Levy RL, Walker LS, Von Korff M, Feld LD, Garner M, et al. Psychosocial mechanisms for the transmission of somatic symptoms from parents to children. World J Gastroenterol. 2015; 21(18):5532-41. [DOI:10.3748/wjg.v21.i18.5532] [PMID] [PMCID]
- Ramchandani PG, Stein A, Hotopf M, Wiles NJ; ALSPAC STUDY TEAM. Early parental and child predictors of recurrent abdominal pain at school age: Results of a large population-based study. J Am Acad Child Adolesc Psychiatry. 2006; 45(6):729-36. [DOI:10.1097/01.chi.0000215329.35928.e0] [PMID]
- Campo JV, Bridge J, Lucas A, Savorelli S, Walker L, Di Lorenzo C, et al. Physical and emotional health of mothers of youth with functional abdominal pain. Arch Pediatr Adolesc Med. 2007; 161(2):131-7. [DOI:10.1001/archpedi.161.2.131] [PMID]
- Citkowska-Kisielewska A, Rutkowski K, Sobański JA, Dembińska E, Mielimąka M. Anxiety symptoms in obsessive-compulsive disorder and generalized anxiety disorder. Psychiatr Pol. 2019; 53(4):845-64. [DOI:10.12740/PP/105378] [PMID]
- Rajindrajith S, Zeevenhooven J, Devanarayana NM, Perera BJC, Benninga MA. Functional abdominal pain disorders in children. Expert Rev Gastroenterol Hepatol. 2018; 12(4):369-90. [DOI:10.1080/17474124.2018.1438188] [PMID]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The obsessive-compulsive inventory: Development and validation of a short version. Psychol Assess. 2002; 14(4):485-96. [DOI:10.1037/1040-3590.14.4.485] [PMID]
- Flygare O, Wallert J, Chen LL, Fernández de la Cruz L, Lundström L, Mataix-Cols D, et al. Empirically defining treatment response and remission in obsessive-compulsive disorder using the obsessive-compulsive inventory-revised. Behav Ther. 2023; 54(1):43-50. [DOI:10.1016/j.beth.2022.06.009] [PMID]
- van Tilburg MAL, Carter CA. Integration of biomedical and psychosocial treatments in pediatrics functional gastrointestinal disorders. Gastroenterol Clin North Am. 2018; 47(4):863-75. [DOI:10.1016/j.gtc.2018.07.010] [PMID]
- Adams TG, Kelmendi B, Brake CA, Gruner P, Badour CL, Pittenger C. The role of stress in the pathogenesis and maintenance of obsessive-compulsive disorder. Chronic Stress (Thousand Oaks). 2018; 2:2470547018758043. [DOI:10.1177/2470547018758043] [PMID] [PMCID]
- Devanarayana NM, Mettananda S, Liyanarachchi C, Nanayakkara N, Mendis N, Perera N, et al. Abdominal pain-predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J Pediatr Gastroenterol Nutr. 2011; 53(6):659-65. [DOI:10.1097/MPG.0b013e3182296033] [PMID]
- Thapar N, Benninga MA, Crowell MD, Di Lorenzo C, Mack I, Nurko S, et al. Paediatric functional abdominal pain disorders. Nat Rev Dis Primers. 2020; 6(1):89. [DOI:10.1038/s41572-020-00222-5] [PMID]
- Dhroove G, Chogle A, Saps M. A million-dollar work-up for abdominal pain: is it worth it? J Pediatr Gastroenterol Nutr. 2010; 51(5):579-83. [DOI:10.1097/MPG.0b013e3181de0639] [PMID]
- Hoekman DR, Rutten JM, Vlieger AM, Benninga MA, Dijkgraaf MG. Annual costs of care for pediatric irritable bowel syndrome, functional abdominal pain, and functional abdominal pain syndrome. J Pediatr. 2015; 167(5):1103-8.e2. [DOI:10.1016/j.jpeds.2015.07.058] [PMID]
- Karunanayake A, Devanarayana NM, Rajindrajith S. Early life events in functional abdominal pain disorders in children. PLoS One. 2022; 17(11):e0275419. [DOI:10.1371/journal.pone.0275419] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2024/03/5 | Accepted: 2024/05/6 | Published: 2024/07/7
Received: 2024/03/5 | Accepted: 2024/05/6 | Published: 2024/07/7
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |