Wed, May 8, 2024
Volume 10, Issue 2 (Spring 2024)
Caspian J Neurol Sci 2024, 10(2): 132-138 |
Back to browse issues page
Ethics code: IR.SBMU.RETECH.REC.1400.611
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghadiri Harati P, Hosseini S M, Javaheri A, Dehghan Manshadi F, Akbarzadeh Baghban A. The Reliability of the Rehabilitative Ultrasound Imaging Method for Assessing Pelvic Floor Muscles Function in Pregnant Women. Caspian J Neurol Sci 2024; 10 (2) :132-138
URL: http://cjns.gums.ac.ir/article-1-680-en.html
URL: http://cjns.gums.ac.ir/article-1-680-en.html
Parisa Ghadiri Harati1 

 , Seyed Majid Hosseini *
, Seyed Majid Hosseini * 

 2, Atiyeh Javaheri3
2, Atiyeh Javaheri3 

 , Farideh Dehghan Manshadi1
, Farideh Dehghan Manshadi1 

 , Alireza Akbarzadeh Baghban4
, Alireza Akbarzadeh Baghban4 




 , Seyed Majid Hosseini *
, Seyed Majid Hosseini * 

 2, Atiyeh Javaheri3
2, Atiyeh Javaheri3 

 , Farideh Dehghan Manshadi1
, Farideh Dehghan Manshadi1 

 , Alireza Akbarzadeh Baghban4
, Alireza Akbarzadeh Baghban4 


1- Department of Physiotherapy, Faculty of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Faculty of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , majid_hoseini@sbmu.ac.ir
3- Department of Gynecology, Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Department of Biostatistics, Proteomics Research Center, School of Allied Medical Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Physiotherapy, Faculty of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran. , majid_hoseini@sbmu.ac.ir
3- Department of Gynecology, Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Department of Biostatistics, Proteomics Research Center, School of Allied Medical Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Pelvic floor muscle, Muscle function, Ultrasound imaging, Pregnant women, Reliability, Physiotherapy
Full-Text [PDF 1473 kb]
(145 Downloads)
| Abstract (HTML) (135 Views)
Full-Text: (40 Views)
Introduction
The pelvic floor muscles (PFMs) build the pelvic diaphragm, urogenital diaphragm, and urethral and anal sphincters [1, 2, 3]. The role of PFMs is to support abdominopelvic organs, bladder continence, respiration, and trunk stabilization [4, 5, 6]. Contraction of the PFMs and their associated fascia supports the bladder, leading to displacement of the bladder base [7]. Poor contraction of these muscles can result in urinary and/or fecal incontinence. Conversely, hyperactivity may lead to issues such as urinary retention, constipation, and painful bladder syndrome [8, 9]. Furthermore, the dysfunction of PFMs is associated with low back pain [10, 11]. Women may experience urinary incontinence for the first time during and after pregnancy [12]. Research indicates a notable decline in PFM strength among pregnant women with urinary incontinence compared to healthy peers [13].
The common techniques to evaluate PFM function include pelvic floor manometry, digital examination, and electromyography [14-18]. PFM function can also be determined by measuring bladder base displacement using the rehabilitative ultrasound imaging (RUSI) method. It is a widely used technique that is simple and safe to employ in a therapeutic setting. This method does not necessitate revealing intimate body parts and is applicable to individuals at any age and with any gender. Recent studies have demonstrated the validity of this method in determining bladder base displacement [15, 19-22]. However, there is scant research on the reliability of RUSI for assessing bladder base displacement in pregnant women.
Due to the prominent role of PFMs in urinary function and their possible dysfunction and weakness in pregnant women suffering from urinary incontinence, RUSI may be crucial for the assessment. In this study, we evaluate the reliability of the RUSI of PFM contraction in pregnant women for the first time. Thus, this study aims to evaluate the reliability of the RUSI for measuring bladder base displacement in pregnant women during voluntary PFM contractions.
Materials and Methods
Participants and sample size
This cross-sectional study was conducted on Iranian pregnant women aged 18-42 years and different gestational ages determined by a gynecologist. Inclusion criteria were pregnancy, the ability to correctly contract the PFMs, and willingness to participate in the research. Exclusion criteria were a diagnosed neurological disease, and inability to understand the instructions in Persian language. Prior to the study, all participants declared their consent by signing an informed consent form. The sample size was determined utilizing the equation proposed by Bonnet [23]. Using this equation and by considering an intraclass correlation coefficient (ICC) of 0.90, 95% confidence interval (CI), and width of 0.20, the minimum sample size was obtained at 15. Given a 15% sample dropout, the sample size increased to 18.
Procedure
For the RUSI, a diagnostic ultrasound imaging device with B-mode technology and a 3.5-5 MHz convex array transducer (Resona 6, Mindray Co., China) was employed. Recent studies have described the detailed procedure to measure bladder base displacement [24-26]. To ensure optimal imaging conditions, a consistent protocol for filling the bladder was implemented prior to imaging, confirming that women had an adequate amount of fluid in their bladders. Participants were instructed to drink 600-750 mL of water for 30 minutes, about one hour before to the measurement. They were then asked to abstain from urination until after the ultrasound imaging [15, 27, 28].
Before conducting the test, a trained pelvic health physiotherapist taught the participants how to activate PFMs correctly by digital examination. During testing, participants were at a supine position with a slight bend in the knees and hips, using one pillow beneath the head. The lumbar spine was maintained in a neutral position. The ultrasound transducer was positioned in the suprapubic area on the transverse plane tilted posterior caudally to get a clear view of the lower posterior section of the bladder in the ultrasound image (Figure 1). The angle of the ultrasound transducer varied, ranging from 15 to 30 degrees, depending on factors such as bladder fullness and abdominal size. Initially, a marker was positioned on the bladder base while the participant was at a resting position. Subsequently, participants were asked to execute a voluntary contraction of the PFMs by “squeezing and lifting the muscles upon the request”. Once the contraction became visible on the ultrasound device screen, a snapshot of the image was taken, and then the participants were asked to release their PFMs [7, 29].
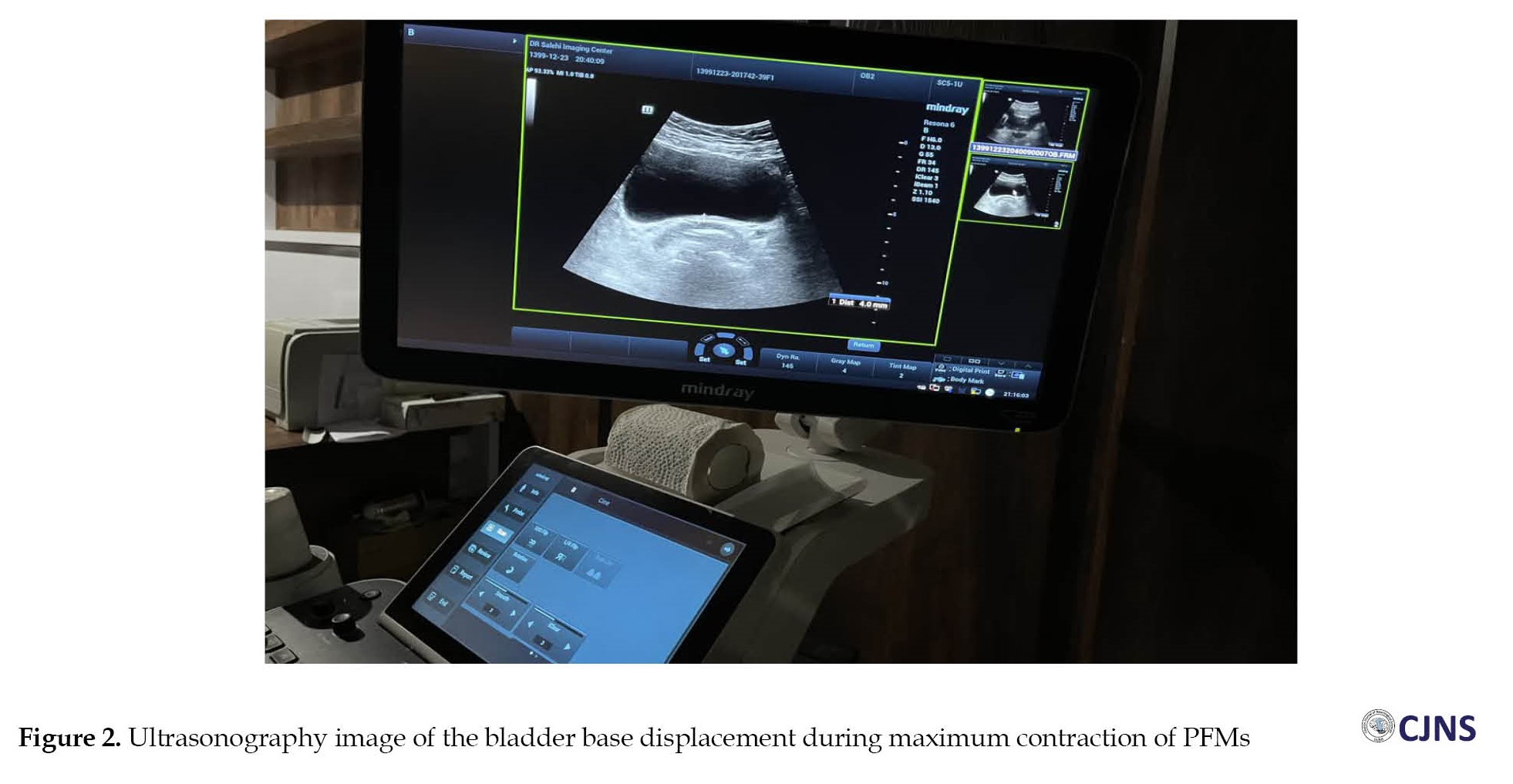
The indicator was placed on the bladder base at the location where the maximum displacement occurred while the muscles were contracting. The displacement of the bladder base from its initial resting position to the end of each contraction was measured and recorded in millimeters (Figure 2). Participants maintained the contraction for up to 3 seconds. The ultrasound transducer remained fixed throughout the testing process at a consistent position from the resting phase to the maximal contraction. Three PFM contractions were performed with a rest interval of 10 seconds, and the average of three measurements were used as a final outcome in the statistical analysis [15, 24].
Statistical analysis
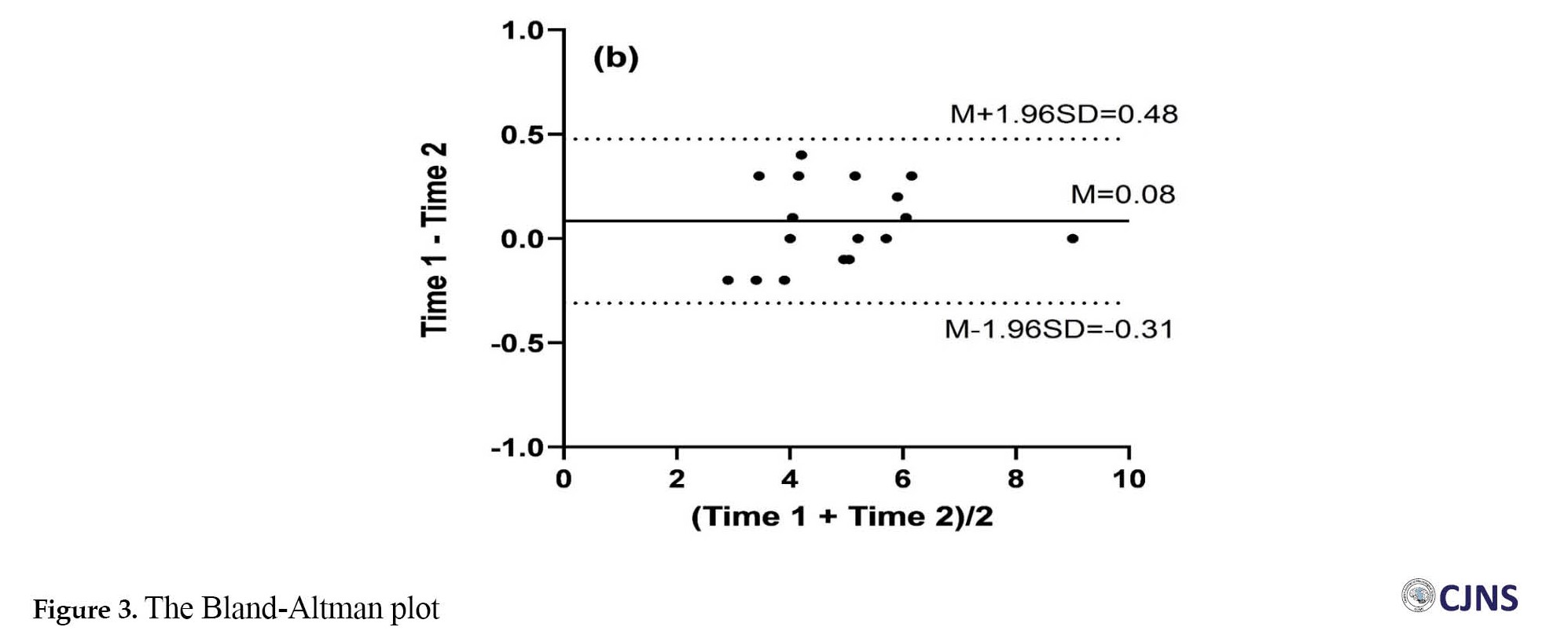
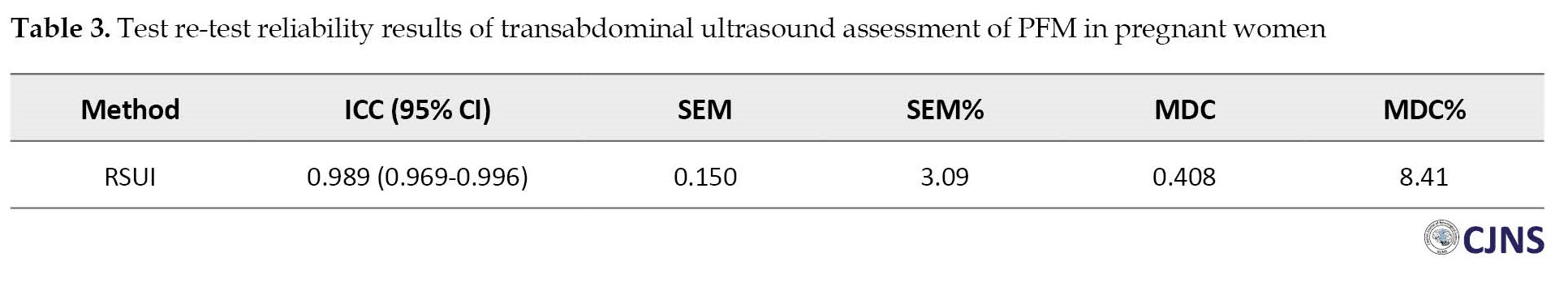
In this study, continuous variables were presented as Mean±SD, median, and inter quartile range (IQR). Test re-test reliability of the RUSI was assessed using the ICC and Bland-Altman plots with lines of equality. The ICC was computed using a two-way mixed-effects model and single measurement (ICC3, 1). Regarding the line of equality, close agreement between measurements was obtained when scatter plots fall on the 45-degree line that passes through the origin. Regarding the interpretation of ICC values, a values <0.5 indicates poor reliability, a value of 0.5-0.75 indicate moderate reliability, a value of 0.75-0.9 shows good reliability, and a value >0.9 represent excellent reliability [30]. Additionally, the standard error of measurement (SEM) and minimal detectable change (MDC) were determined using the Equations 1 and 2:
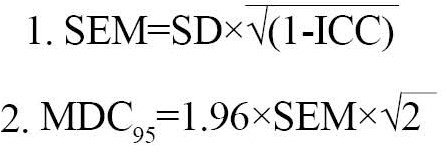
The SEM and MDC percentages were obtained as Equations 3 and 4:
3. SEM%=(SEM/M)×100
4. MDC%=(MDC⁄M)×100,
where M represents the mean of both observations from the two assessments conducted during the study. An SEM% <10% represents acceptable reliability, and an MDC% <30% was considered as acceptable and <10% as excellent. The statistical analysis was performed in SPSS software, version 26 (IBM Corp., Armonk, NY, USA) and plots were represented by GraphPad Prism software, version 8.0.1 (GraphPad Prism Software Inc., San Diego, CA, USA).
The intra-rater reliability of the RUSI was
evaluated with the participation of 18 subjects. The rater conducted measurements first. After a 30-minute interval, the measurements were repeated in a blinded and randomized manner using the same procedure. The subjects and the sequence of measurements were randomly selected, different from the initial examination sequence, aiming to minimize the impact of memory effects. All test trials were carried out in a hospital affiliated to Shahid Sadoughi University in Yazd, Iran.
Results
Characteristics of participants
The demographic characteristics of participants are presented in Table 1.
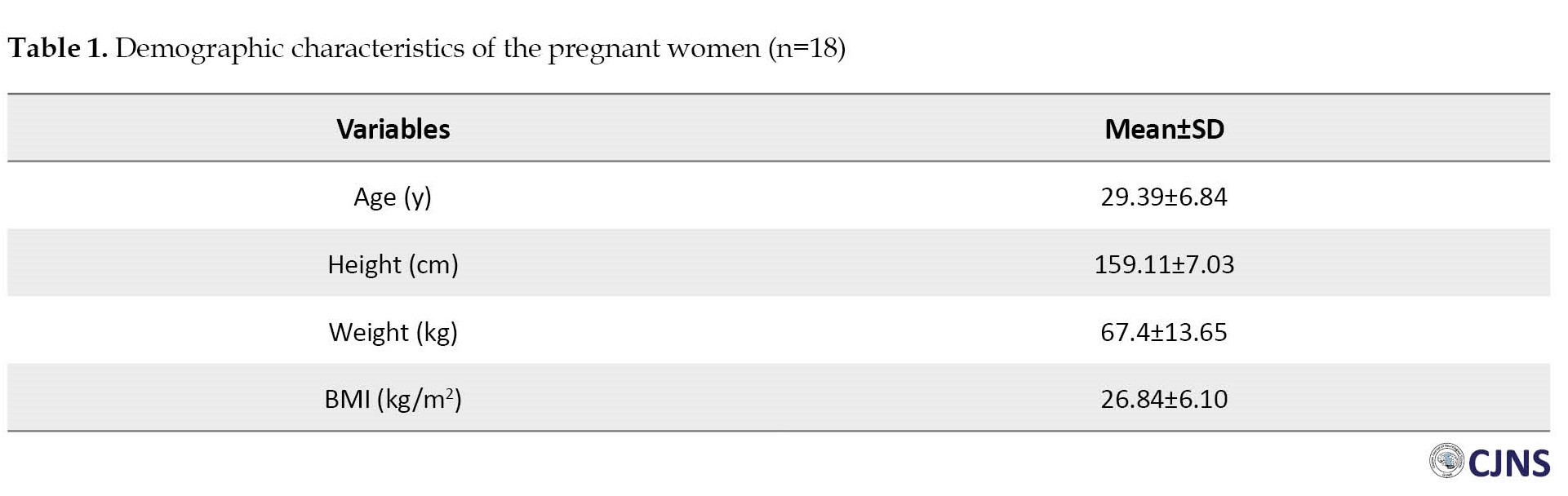
There were no statistically significant differences among subjects in terms of height, age, and weight. Their mean age was 29.39±6.84 years, ranging from 18 to 42 years and their mean body mass index (BMI) was 26.84±6.10 kg/m2, ranging from 16.96 to 36.59 kg/m2.
Table 2 presents the descriptive statistics of the transabdominal ultrasound measurement of the PFMs in the first and second measurements.
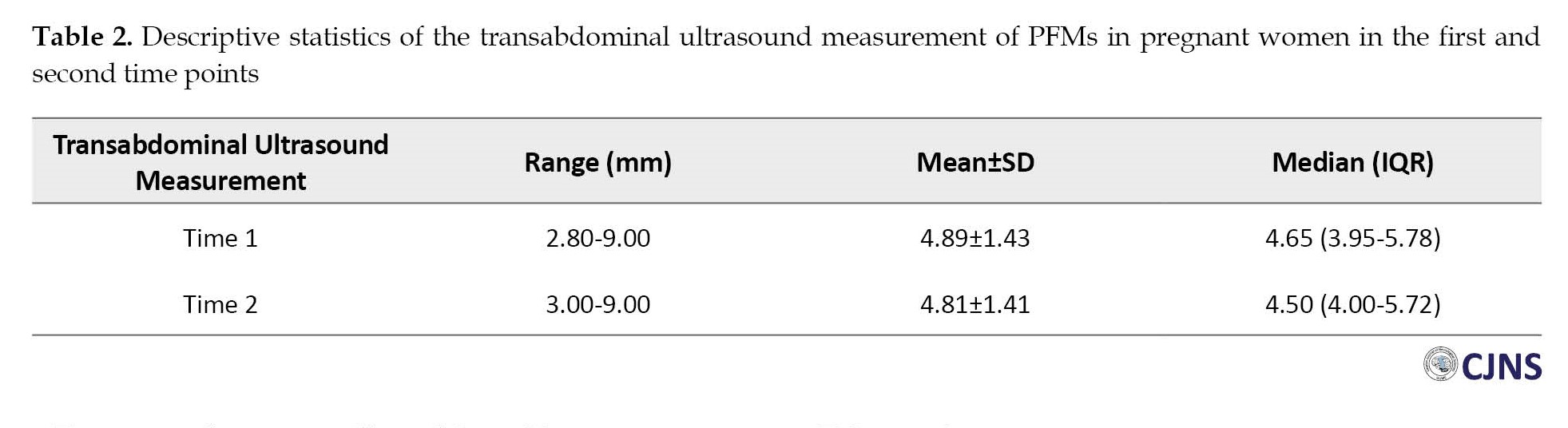
The mean value in the first time point was 4.89±1.43, ranging from 2.8 to 9.0. The ICC (1.1) value for the reliability of RUSI were 0.99. This suggests a high level of intra-rater reliability for the RUSI.
Test re-test data were collected from 18 pregnant women at a 30-min interval. The ICC was 0.989 (95% CI, 0.969%, 0.996%). The visual examination of the consistency between test and re-test results of ultrasound measurement of PFMs using the Bland-Altman plot with lines of equality was also conducted. As can be seen in Figure 3, the scatter plots indicate that the data points fell on or were close to the line of equality. The Bland-Altman plot (Figure 3) also revealed that all points fall on the lower and upper limits of agreement. Furthermore, no significant trend or bias was evident in the scattering of points. Both plots demonstrated high agreement between the test and re-test data.
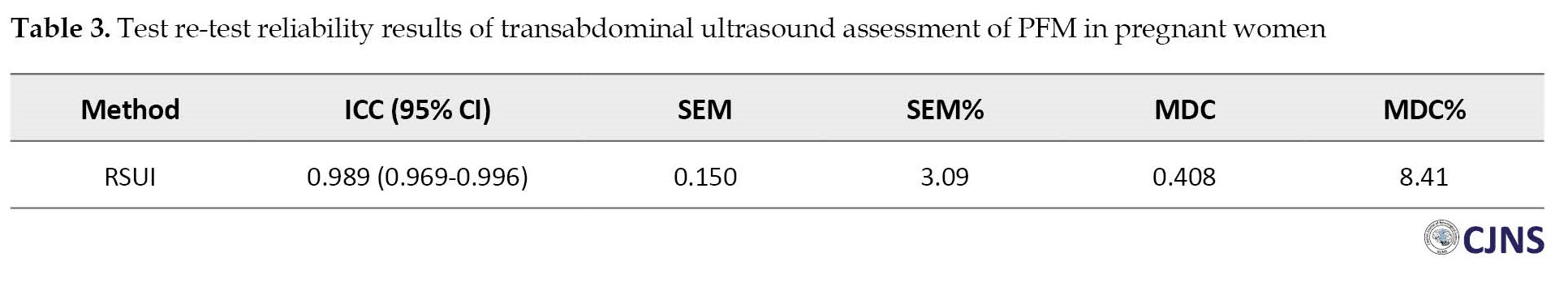
As presented in Table 3, the SEM% was 3.09% which is considered acceptable, and MDC% was 8.41% which is considered excellent.
Discussion
The RSUI method is novel and valid approach for evaluating the patterns of muscle activation during contraction. Ultrasound imaging method is commonly used to assess both voluntary and involuntary muscle activity at the subconscious level. In this study, we focused on measuring voluntary contractions. This is the first study that evaluates the reliability of RSUI in pregnant women. The findings of our study indicated that the RSUI was a reliable method for evaluating PFM contractions in pregnant women (ICC=0.99). Similar findings have been reported in recent studies [15, 24, 31], although these studies examined reliability in healthy women or women with urinary disorders. According to Landis et al. [32], the ICC of 0.81-1.00 is considered “almost perfect” agreement, 0.61–0.80 as “substantial,” 0.41–0.60 as “moderate,” 0.21–0.40 as “fair,” and 0–0.20 as “slight”. Therefore, in our study, the reliability of the RSUI was excellent.
By the use of RSUI in this study, we were able to observe the extent to which the PFMs had activation to prevent urinary incontinence. This highlighted the simplicity and effectiveness of studying PFM activities. In summary, the application of a diagnostic ultrasonic imaging device enabled the reliable measurement of bladder base displacement in pregnant women.
Conclusion
The RSUI has high reliability for evaluating PFM contractions in pregnant women. It can be used in future studies on pregnant women. Further studies are recommended to assess the effectiveness of bladder base displacement in the management and prevention of urogynecological disorders during pregnancy.
Limitations
One limitation of this study was that the RSUI for assessing the bladder base displacement lacks a fixed reference point, unlike transperineal ultrasound imaging, which is considered the gold standard for evaluating bladder neck displacement. Due to the nature of bladder base displacement that is related to a potentially movable starting point, the maintenance of the fixed position of transducer is crucial for achieving accurate and repeatable measurements. Another limitation of this study was the inability to assess inter-rater reliability, as only one rater was involved. Hence, future studies should involve multiple raters to explore inter-rater reliability of the RSUI.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (Code: IR.SBMU.RETECH.REC.1400.611). All participants were informed about the study objectives and the voluntary nature of participation.
Funding
This study did not receive any dedicated funding from governmental, commercial, or non-profit organizations.
Authors contributions
Conceptualization: Seyed Majid Hosseini, Farideh Dehghan Manshadi and Parisa Ghadiri Harati; Methodology: Farideh Dehghan Manshadi; Investigation: Atiyeh Javaheri and Parisa Ghadiri Harati; Formal analysis: Alireza Akbarzadeh Baghban; Resources: Seyed Majid Hosseini and Parisa Ghadiri Harati; Writing the original draft: Parisa Ghadiri Harati; Review & editing: Farideh Dehghan Manshadi and Seyed Majid Hosseini; Supervision: Farifdeh Dehghan Manshadi and Atiyeh Javaheri.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors acknowledge the support of the Deputy for Research and Technology of Shahid Beheshti University of Medical Sciences and the Clinical Research Development Unit of Shahid Sadoughi Hospital, and all women participated in this study for their cooperation.
References
The pelvic floor muscles (PFMs) build the pelvic diaphragm, urogenital diaphragm, and urethral and anal sphincters [1, 2, 3]. The role of PFMs is to support abdominopelvic organs, bladder continence, respiration, and trunk stabilization [4, 5, 6]. Contraction of the PFMs and their associated fascia supports the bladder, leading to displacement of the bladder base [7]. Poor contraction of these muscles can result in urinary and/or fecal incontinence. Conversely, hyperactivity may lead to issues such as urinary retention, constipation, and painful bladder syndrome [8, 9]. Furthermore, the dysfunction of PFMs is associated with low back pain [10, 11]. Women may experience urinary incontinence for the first time during and after pregnancy [12]. Research indicates a notable decline in PFM strength among pregnant women with urinary incontinence compared to healthy peers [13].
The common techniques to evaluate PFM function include pelvic floor manometry, digital examination, and electromyography [14-18]. PFM function can also be determined by measuring bladder base displacement using the rehabilitative ultrasound imaging (RUSI) method. It is a widely used technique that is simple and safe to employ in a therapeutic setting. This method does not necessitate revealing intimate body parts and is applicable to individuals at any age and with any gender. Recent studies have demonstrated the validity of this method in determining bladder base displacement [15, 19-22]. However, there is scant research on the reliability of RUSI for assessing bladder base displacement in pregnant women.
Due to the prominent role of PFMs in urinary function and their possible dysfunction and weakness in pregnant women suffering from urinary incontinence, RUSI may be crucial for the assessment. In this study, we evaluate the reliability of the RUSI of PFM contraction in pregnant women for the first time. Thus, this study aims to evaluate the reliability of the RUSI for measuring bladder base displacement in pregnant women during voluntary PFM contractions.
Materials and Methods
Participants and sample size
This cross-sectional study was conducted on Iranian pregnant women aged 18-42 years and different gestational ages determined by a gynecologist. Inclusion criteria were pregnancy, the ability to correctly contract the PFMs, and willingness to participate in the research. Exclusion criteria were a diagnosed neurological disease, and inability to understand the instructions in Persian language. Prior to the study, all participants declared their consent by signing an informed consent form. The sample size was determined utilizing the equation proposed by Bonnet [23]. Using this equation and by considering an intraclass correlation coefficient (ICC) of 0.90, 95% confidence interval (CI), and width of 0.20, the minimum sample size was obtained at 15. Given a 15% sample dropout, the sample size increased to 18.
Procedure
For the RUSI, a diagnostic ultrasound imaging device with B-mode technology and a 3.5-5 MHz convex array transducer (Resona 6, Mindray Co., China) was employed. Recent studies have described the detailed procedure to measure bladder base displacement [24-26]. To ensure optimal imaging conditions, a consistent protocol for filling the bladder was implemented prior to imaging, confirming that women had an adequate amount of fluid in their bladders. Participants were instructed to drink 600-750 mL of water for 30 minutes, about one hour before to the measurement. They were then asked to abstain from urination until after the ultrasound imaging [15, 27, 28].
Before conducting the test, a trained pelvic health physiotherapist taught the participants how to activate PFMs correctly by digital examination. During testing, participants were at a supine position with a slight bend in the knees and hips, using one pillow beneath the head. The lumbar spine was maintained in a neutral position. The ultrasound transducer was positioned in the suprapubic area on the transverse plane tilted posterior caudally to get a clear view of the lower posterior section of the bladder in the ultrasound image (Figure 1). The angle of the ultrasound transducer varied, ranging from 15 to 30 degrees, depending on factors such as bladder fullness and abdominal size. Initially, a marker was positioned on the bladder base while the participant was at a resting position. Subsequently, participants were asked to execute a voluntary contraction of the PFMs by “squeezing and lifting the muscles upon the request”. Once the contraction became visible on the ultrasound device screen, a snapshot of the image was taken, and then the participants were asked to release their PFMs [7, 29].
The indicator was placed on the bladder base at the location where the maximum displacement occurred while the muscles were contracting. The displacement of the bladder base from its initial resting position to the end of each contraction was measured and recorded in millimeters (Figure 2). Participants maintained the contraction for up to 3 seconds. The ultrasound transducer remained fixed throughout the testing process at a consistent position from the resting phase to the maximal contraction. Three PFM contractions were performed with a rest interval of 10 seconds, and the average of three measurements were used as a final outcome in the statistical analysis [15, 24].
Statistical analysis
In this study, continuous variables were presented as Mean±SD, median, and inter quartile range (IQR). Test re-test reliability of the RUSI was assessed using the ICC and Bland-Altman plots with lines of equality. The ICC was computed using a two-way mixed-effects model and single measurement (ICC3, 1). Regarding the line of equality, close agreement between measurements was obtained when scatter plots fall on the 45-degree line that passes through the origin. Regarding the interpretation of ICC values, a values <0.5 indicates poor reliability, a value of 0.5-0.75 indicate moderate reliability, a value of 0.75-0.9 shows good reliability, and a value >0.9 represent excellent reliability [30]. Additionally, the standard error of measurement (SEM) and minimal detectable change (MDC) were determined using the Equations 1 and 2:
The SEM and MDC percentages were obtained as Equations 3 and 4:
3. SEM%=(SEM/M)×100
4. MDC%=(MDC⁄M)×100,
where M represents the mean of both observations from the two assessments conducted during the study. An SEM% <10% represents acceptable reliability, and an MDC% <30% was considered as acceptable and <10% as excellent. The statistical analysis was performed in SPSS software, version 26 (IBM Corp., Armonk, NY, USA) and plots were represented by GraphPad Prism software, version 8.0.1 (GraphPad Prism Software Inc., San Diego, CA, USA).
The intra-rater reliability of the RUSI was
evaluated with the participation of 18 subjects. The rater conducted measurements first. After a 30-minute interval, the measurements were repeated in a blinded and randomized manner using the same procedure. The subjects and the sequence of measurements were randomly selected, different from the initial examination sequence, aiming to minimize the impact of memory effects. All test trials were carried out in a hospital affiliated to Shahid Sadoughi University in Yazd, Iran.
Results
Characteristics of participants
The demographic characteristics of participants are presented in Table 1.
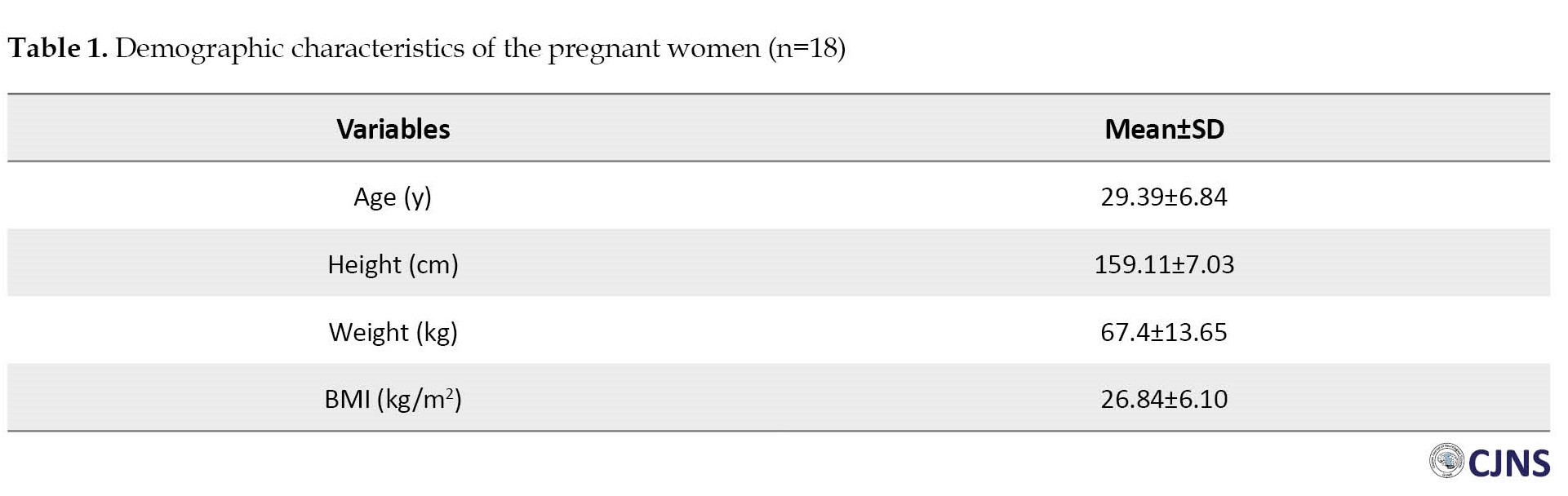
There were no statistically significant differences among subjects in terms of height, age, and weight. Their mean age was 29.39±6.84 years, ranging from 18 to 42 years and their mean body mass index (BMI) was 26.84±6.10 kg/m2, ranging from 16.96 to 36.59 kg/m2.
Table 2 presents the descriptive statistics of the transabdominal ultrasound measurement of the PFMs in the first and second measurements.
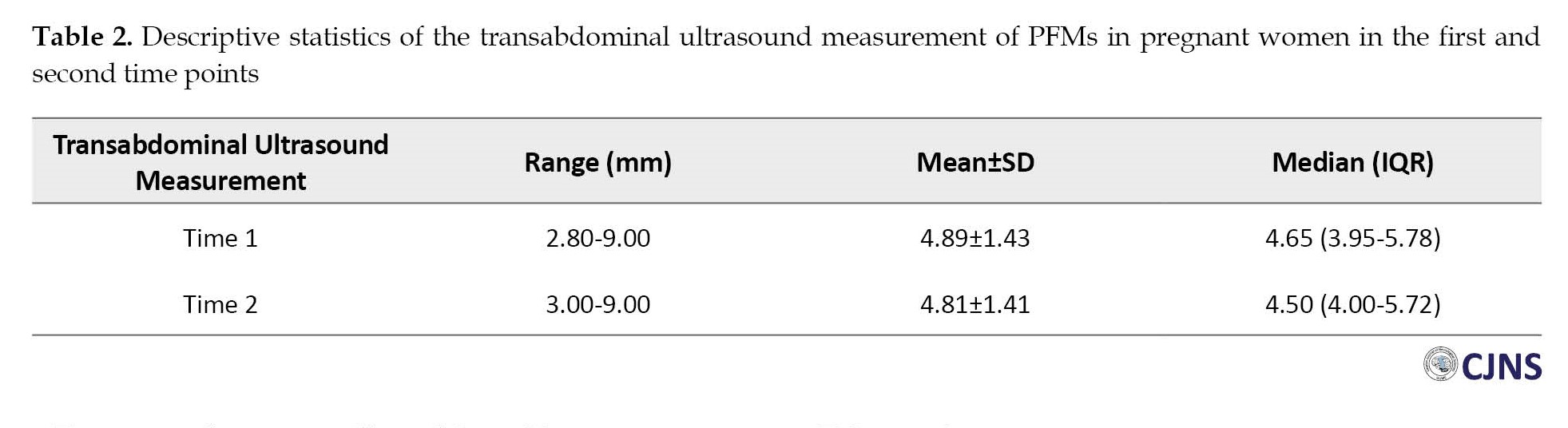
The mean value in the first time point was 4.89±1.43, ranging from 2.8 to 9.0. The ICC (1.1) value for the reliability of RUSI were 0.99. This suggests a high level of intra-rater reliability for the RUSI.
Test re-test data were collected from 18 pregnant women at a 30-min interval. The ICC was 0.989 (95% CI, 0.969%, 0.996%). The visual examination of the consistency between test and re-test results of ultrasound measurement of PFMs using the Bland-Altman plot with lines of equality was also conducted. As can be seen in Figure 3, the scatter plots indicate that the data points fell on or were close to the line of equality. The Bland-Altman plot (Figure 3) also revealed that all points fall on the lower and upper limits of agreement. Furthermore, no significant trend or bias was evident in the scattering of points. Both plots demonstrated high agreement between the test and re-test data.
As presented in Table 3, the SEM% was 3.09% which is considered acceptable, and MDC% was 8.41% which is considered excellent.
Discussion
The RSUI method is novel and valid approach for evaluating the patterns of muscle activation during contraction. Ultrasound imaging method is commonly used to assess both voluntary and involuntary muscle activity at the subconscious level. In this study, we focused on measuring voluntary contractions. This is the first study that evaluates the reliability of RSUI in pregnant women. The findings of our study indicated that the RSUI was a reliable method for evaluating PFM contractions in pregnant women (ICC=0.99). Similar findings have been reported in recent studies [15, 24, 31], although these studies examined reliability in healthy women or women with urinary disorders. According to Landis et al. [32], the ICC of 0.81-1.00 is considered “almost perfect” agreement, 0.61–0.80 as “substantial,” 0.41–0.60 as “moderate,” 0.21–0.40 as “fair,” and 0–0.20 as “slight”. Therefore, in our study, the reliability of the RSUI was excellent.
By the use of RSUI in this study, we were able to observe the extent to which the PFMs had activation to prevent urinary incontinence. This highlighted the simplicity and effectiveness of studying PFM activities. In summary, the application of a diagnostic ultrasonic imaging device enabled the reliable measurement of bladder base displacement in pregnant women.
Conclusion
The RSUI has high reliability for evaluating PFM contractions in pregnant women. It can be used in future studies on pregnant women. Further studies are recommended to assess the effectiveness of bladder base displacement in the management and prevention of urogynecological disorders during pregnancy.
Limitations
One limitation of this study was that the RSUI for assessing the bladder base displacement lacks a fixed reference point, unlike transperineal ultrasound imaging, which is considered the gold standard for evaluating bladder neck displacement. Due to the nature of bladder base displacement that is related to a potentially movable starting point, the maintenance of the fixed position of transducer is crucial for achieving accurate and repeatable measurements. Another limitation of this study was the inability to assess inter-rater reliability, as only one rater was involved. Hence, future studies should involve multiple raters to explore inter-rater reliability of the RSUI.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (Code: IR.SBMU.RETECH.REC.1400.611). All participants were informed about the study objectives and the voluntary nature of participation.
Funding
This study did not receive any dedicated funding from governmental, commercial, or non-profit organizations.
Authors contributions
Conceptualization: Seyed Majid Hosseini, Farideh Dehghan Manshadi and Parisa Ghadiri Harati; Methodology: Farideh Dehghan Manshadi; Investigation: Atiyeh Javaheri and Parisa Ghadiri Harati; Formal analysis: Alireza Akbarzadeh Baghban; Resources: Seyed Majid Hosseini and Parisa Ghadiri Harati; Writing the original draft: Parisa Ghadiri Harati; Review & editing: Farideh Dehghan Manshadi and Seyed Majid Hosseini; Supervision: Farifdeh Dehghan Manshadi and Atiyeh Javaheri.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors acknowledge the support of the Deputy for Research and Technology of Shahid Beheshti University of Medical Sciences and the Clinical Research Development Unit of Shahid Sadoughi Hospital, and all women participated in this study for their cooperation.
References
- Norton P, Brubaker L. Urinary incontinence in women. Lancet. 2006; 367(9504):57-67. [PMID]
- Bø K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther. 2005; 85(3):269-82. [DOI:10.1093/ptj/85.3.269] [PMID]
- Dietz HP, Franco AV, Shek KL, Kirby A. Avulsion injury and levator hiatal ballooning: Two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand. 2012; 91(2):211-4. [DOI:10.1111/j.1600-0412.2011.01315.x] [PMID]
- Pool-Goudzwaard AL, Slieker ten Hove MC, Vierhout ME, Mulder PH, Pool JJ, Snijders CJ, et al. Relations between pregnancy-related low back pain, pelvic floor activity and pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16(6):468-74. [DOI:10.1007/s00192-005-1292-7] [PMID]
- Smith MD, Russell A, Hodges PW. Is there a relationship between parity, pregnancy, back pain and incontinence? Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19(2):205-11. [DOI:10.1007/s00192-007-0421-x] [PMID]
- Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing: The role of fascia following pregnancy and delivery. J Bodyw Mov Ther. 2008; 12(4):333-48. [DOI:10.1016/j.jbmt.2008.05.003] [PMID]
- Whittaker JL, Thompson JA, Teyhen DS, Hodges P. Rehabilitative ultrasound imaging of pelvic floor muscle function. J Orthop Sports Phys Ther. 2007; 37(8):487-98. [DOI:10.2519/jospt.2007.2548] [PMID]
- Finamore PS, Goldstein HB, Whitmore KE. Pelvic floor muscle dysfunction: A review. Urogynecology. 2008; 14(6):417-22. [DOI:10.1097/SPV.0b013e3181907870]
- Messelink B, Benson T, Berghmans B, Bø K, Corcos J, Fowler C, et al. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the international continence society. Neurourol Urodyn. 2005; 24(4):374-80. [DOI:10.1002/nau.20144] [PMID]
- Whittaker J. Abdominal ultrasound imaging of pelvic floor muscle function in individuals with low back pain. J ManManipulative Therapy. 2004; 12(1):44-9. [DOI:10.1179/106698104790825491]
- Sapsford R. The pelvic floor: A clinical model for function and rehabilitation. Physiotherapy. 2001; 87(12):620-30. [DOI:10.1016/S0031-9406(05)61107-8]
- Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019; 22(3):217-22. [DOI:10.1080/13697137.2018.1543263] [PMID]
- Mørkved S, Salvesen KA, Bø K, Eik-Nes S. Pelvic floor muscle strength and thickness in continent and incontinent nulliparous pregnant women. Int Urogynecol J Pelvic Floor Dysfunct. 2004; 15(6):384-9; discussion 390. [DOI:10.1007/s00192-004-1194-0] [PMID]
- Auchincloss CC, McLean L. The reliability of surface EMG recorded from the pelvic floor muscles. J Neurosci Methods. 2009; 182(1):85-96. [DOI:10.1016/j.jneumeth.2009.05.027] [PMID]
- Thompson JA, O’Sullivan PB, Briffa K, Neumann P, Court S. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. Int Urogynecol J Pelvic Floor Dysfunct. 2005; 16(4):285-92. [DOI:10.1007/s00192-005-1308-3] [PMID]
- Escalona-Vargas D, Siegel ER, Oliphant S, Eswaran H. Evaluation of pelvic floor muscles in pregnancy and postpartum with non-invasive magnetomyography. IEEE J Transl Eng Health Med. 2021; 10:1800106. [DOI:10.1109/jtehm.2021.3130785] [PMID]
- Zając B, Sulowska-Daszyk I, Mika A, Stolarczyk A, Rosłoniec E, Królikowska A, et al. Reliability of pelvic floor muscle assessment with transabdominal ultrasound in young nulliparous women. J Clin Med. 2021; 10(15):3449. [DOI:10.3390/jcm10153449] [PMID]
- Aukee P, Usenius JP, Kirkinen P. An evaluation of pelvic floor anatomy and function by MRI. Eur J Obstet Gynecol Reprod Biol. 2004; 112(1):84-8. [DOI:10.1016/s0301-2115(03)00327-0] [PMID]
- Dehghan Manshadi F, Ghanbari Z, Giti M. [Application of ultrasonic imaging for assessment of pelvic floor muscle function (Persian)]. Sci J Rehabil Med. 2013; 2(1):58-66. [Link]
- Nyhus MØ, Oversand SH, Salvesen Ø, Salvesen KÅ, Mathew S, Volløyhaug I. Ultrasound assessment of pelvic floor muscle contraction: reliability and development of an ultrasound-based contraction scale. Ultrasound Obstet Gynecol. 2020; 55(1):125-31. [DOI:10.1002/uog.20382] [PMID]
- Harm-Ernandes I, Boyle V, Hartmann D, Fitzgerald CM, Lowder JL, Kotarinos R, et al. Assessment of the pelvic floor and associated musculoskeletal system: Guide for medical practitioners. Female Pelvic Med Reconstr Surg. 2021; 27(12):711-8. [DOI:10.1097/spv.0000000000001121] [PMID]
- Moser H, Luginbuehl H, Baeyens JP, Radlinger L. Reliability and validity of pelvic floor muscle displacement measurements during voluntary contractions. Int Urogynecol J. 2019; 30(12):2093-100. [DOI:10.1007/s00192-019-03932-x] [PMID]
- Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002; 21(9):1331-5. [DOI:10.1002/sim.1108] [PMID]
- Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP. Investigation of transabdominal real-time ultrasound to visualise the muscles of the pelvic floor. Aust J Physiother. 2005; 51(3):167-70. [DOI:10.1016/s0004-9514(05)70023-4] [PMID]
- Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional manoeuvres in continent and incontinent women. Int Urogynecol J Pelvic Floor Dysfunct. 2007; 18(7):779-86. [DOI:10.1007/s00192-006-0225-4] [PMID]
- Thompson JA, O’Sullivan PB, Briffa NK, Neumann P. Assessment of voluntary pelvic floor muscle contraction in continent and incontinent women using transperineal ultrasound, manual muscle testing and vaginal squeeze pressure measurements. Int Urogynecol J Pelvic Floor Dysfunct. 2006; 17(6):624-30. [DOI:10.1007/s00192-006-0081-2] [PMID]
- Barton A, Serrao C, Thompson J, Briffa K. Transabdominal ultrasound to assess pelvic floor muscle performance during abdominal curl in exercising women. Int Urogynecol J. 2015; 26(12):1789-95. [DOI:10.1007/s00192-015-2791-9] [PMID]
- Baeßler K, Junginger B. Traditional gymnastic exercises for the pelvic floor often lead to bladder neck descent - a study using perineal ultrasound. Geburtshilfe Frauenheilkd. 2017; 77(7):765-70. [DOI:10.1055/s-0043-103460] [PMID]
- Dehghan Manshadi F, Parnianpour M, Ghanbari Z, Sarrafzadeh J, Kazemnejad A. [An ultrasonic investigation of stability of pelvic floor in women with and without urinary stress incontinence (Persian)]. Iran J Obstet Gynecol Infertil. 2012; 15(13):16-25. [DOI:10.22038/ijogi.2012.5692]
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2):155-63. [DOI:10.1016/j.jcm.2016.02.012] [PMID]
- Chehrehrazi M, Arab AM, Karimi N, Zargham M. Assessment of pelvic floor muscle contraction in stress urinary incontinent women: Comparison between transabdominal ultrasound and perineometry. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20(12):1491-6. [DOI:10.1007/s00192-009-0977-8] [PMID]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159-74. [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/02/23 | Accepted: 2023/05/25 | Published: 2024/04/1
Received: 2023/02/23 | Accepted: 2023/05/25 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |