Thu, May 9, 2024
Volume 10, Issue 2 (Spring 2024)
Caspian J Neurol Sci 2024, 10(2): 126-131 |
Back to browse issues page
Ethics code: IR.GUMS.REC.1400.506
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alizadeh Y, Mohammadi-Manesh G, Medghalchi A, Behboudi H, Soltani-Moghadam R, Akbari M, et al . Epidemiology of Ocular Trauma in Patients Referred to a Tertiary Center in Northern Iran. Caspian J Neurol Sci 2024; 10 (2) :126-131
URL: http://cjns.gums.ac.ir/article-1-679-en.html
URL: http://cjns.gums.ac.ir/article-1-679-en.html
Yousef Alizadeh1 

 , Ghazaleh Mohammadi-Manesh1
, Ghazaleh Mohammadi-Manesh1 

 , Abdolreza Medghalchi1
, Abdolreza Medghalchi1 

 , Hasan Behboudi1
, Hasan Behboudi1 

 , Reza Soltani-Moghadam1
, Reza Soltani-Moghadam1 

 , Mitra Akbari1
, Mitra Akbari1 

 , Ebrahim Azaripour1
, Ebrahim Azaripour1 

 , Shila Kianmehr1
, Shila Kianmehr1 

 , Narges Pour Deylami1
, Narges Pour Deylami1 

 , Haleh Alizadeh2
, Haleh Alizadeh2 

 , Ehsan Kazemnezhad Leyli3
, Ehsan Kazemnezhad Leyli3 

 , Maryam Dourandeesh *
, Maryam Dourandeesh * 

 4
4


 , Ghazaleh Mohammadi-Manesh1
, Ghazaleh Mohammadi-Manesh1 

 , Abdolreza Medghalchi1
, Abdolreza Medghalchi1 

 , Hasan Behboudi1
, Hasan Behboudi1 

 , Reza Soltani-Moghadam1
, Reza Soltani-Moghadam1 

 , Mitra Akbari1
, Mitra Akbari1 

 , Ebrahim Azaripour1
, Ebrahim Azaripour1 

 , Shila Kianmehr1
, Shila Kianmehr1 

 , Narges Pour Deylami1
, Narges Pour Deylami1 

 , Haleh Alizadeh2
, Haleh Alizadeh2 

 , Ehsan Kazemnezhad Leyli3
, Ehsan Kazemnezhad Leyli3 

 , Maryam Dourandeesh *
, Maryam Dourandeesh * 

 4
4
1- Department of Eye, Eye Research Center, School of Medicine, Amir-Almomenin Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Clinical Pharmacy, School of Pharmacy, Guilan University of Medical Science, Rasht, Iran.
3- Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Eye, Eye Research Center, School of Medicine, Amir-Almomenin Hospital, Guilan University of Medical Sciences, Rasht, Iran. , maryam.dourandeesh.dl@gmail.com
2- Department of Clinical Pharmacy, School of Pharmacy, Guilan University of Medical Science, Rasht, Iran.
3- Department of Biostatistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Eye, Eye Research Center, School of Medicine, Amir-Almomenin Hospital, Guilan University of Medical Sciences, Rasht, Iran. , maryam.dourandeesh.dl@gmail.com
Full-Text [PDF 1073 kb]
(68 Downloads)
| Abstract (HTML) (128 Views)
Full-Text: (36 Views)
Introduction
Ocular trauma is a debilitating condition and one of the most important and leading causes of visual impairments that can impose a high socioeconomic cost burden on the community [1]. According to the World Health Organization (WHO), there are 55 million annual cases of ocular trauma, which can affect daily activities [2]. Ocular trauma accounts for blindness in 75,100,000 people in developing countries and 9,100,000 people in developed countries [3]. It has been estimated that the annual incidence of hospitalized eye injuries is 6.5-27.7 per 100000 people [4].
According to studies, most of the ocular trauma cases in the U.S. are caused by unintentional injuries (77%) and assaults (22%). In European countries, as developed countries, the incidence of work-related ocular traumas is low, and most of them are caused by accident. In Asia, with developing countries having poor access to medical services, there are more cases [3]. Based on the studies, work-related and unexpected events are the most common causes of ocular trauma. Moreover, globe injuries are more common than non-globe injuries. The common globe injuries include mechanical, chemical, photic, and thermal injuries [5].
While 90% of ocular traumas are preventable, especially in childhood, there is a need to manage preventive measures and extensive epidemiological data [6]. North of Iran is one of the most common places for traumas, especially ocular traumas, due to the greater amount of physical and outdoor activities. Despite the prevalence of traumas in the north of Iran; there is limited information. Therefore, this study aims to investigate the epidemiology of ocular trauma cases in patients referred to a tertiary center in northern Iran.
Materials and Methods
This cross-sectional study was conducted in Amir-Almomenin Hospital affiliated to Guilan University of Medical Sciences in Rasht, northern Iran in 2021-22. Among 956 cases referred to the eye emergency department of Amir-Almomenin Hospital, 462 cases with ocular trauma were included in the study. Personal information (including age, sex, occupation, place of residence), location of the accident, the use of eye protection equipment, time (season/month) of the accident, and type of injury were collected using a checklist. The collected data were analyzed in SPSS software, version 26. Mean±SD and number (percentage) were used for describing quantitative and qualitative variables, respectively.
Results
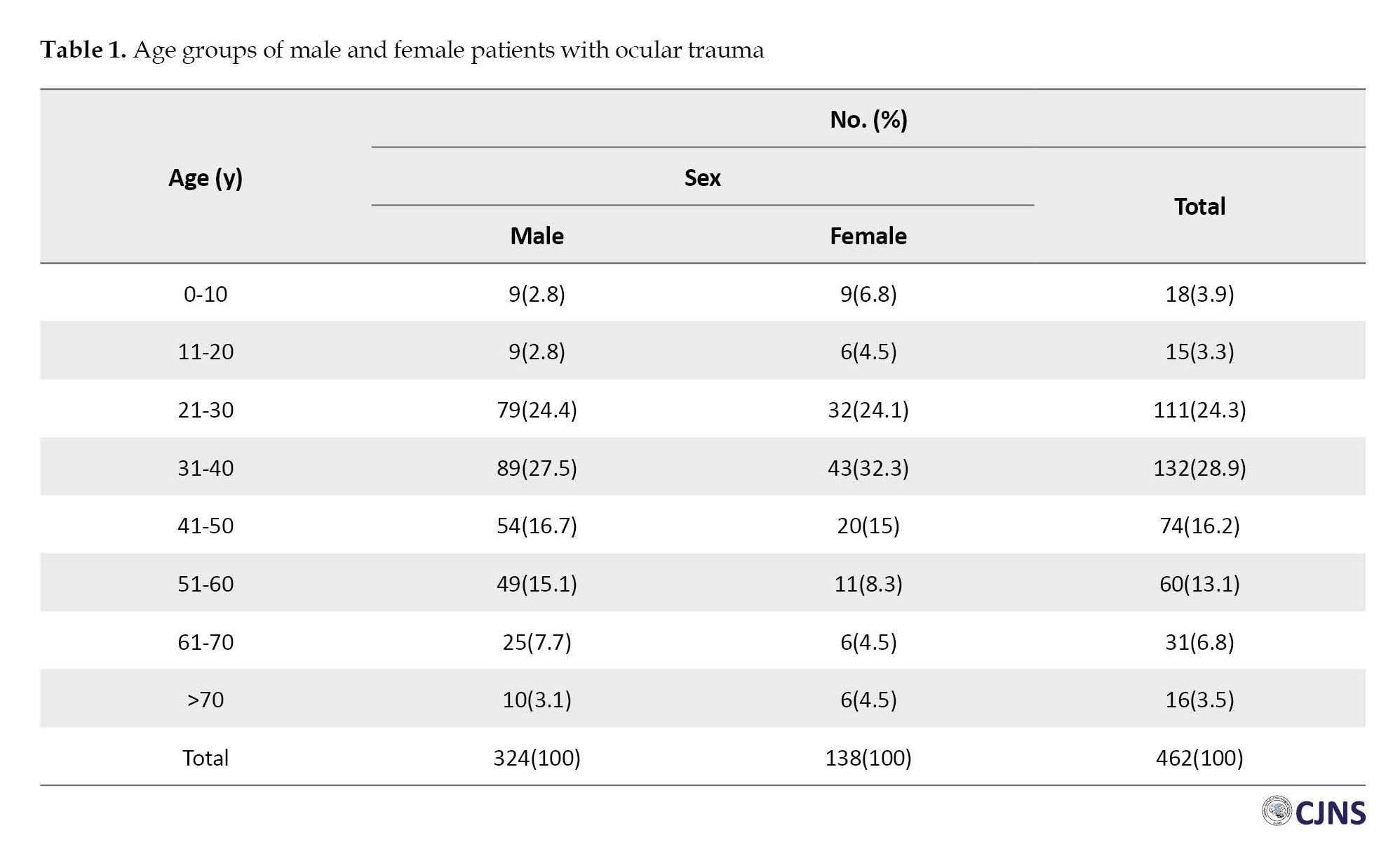
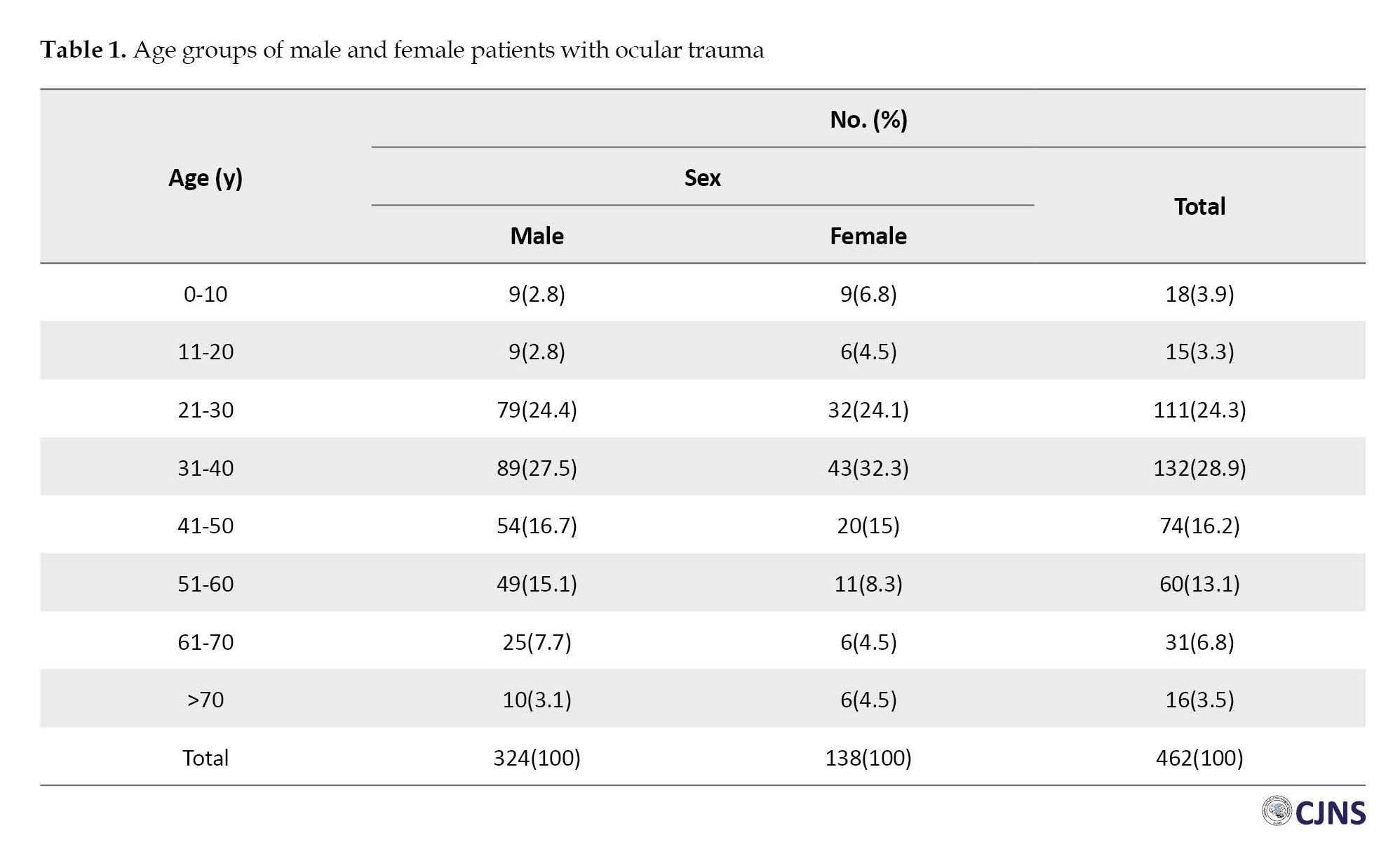
Among 462 cases with ocular trauma, 71.0% were male, and their mean age was 41.5±17.4 years, ranging from 1 to 91 years. Most of them were in the 31-40 years group (28.8%) followed by the 21-30 years group (23.3%) (Table 1).
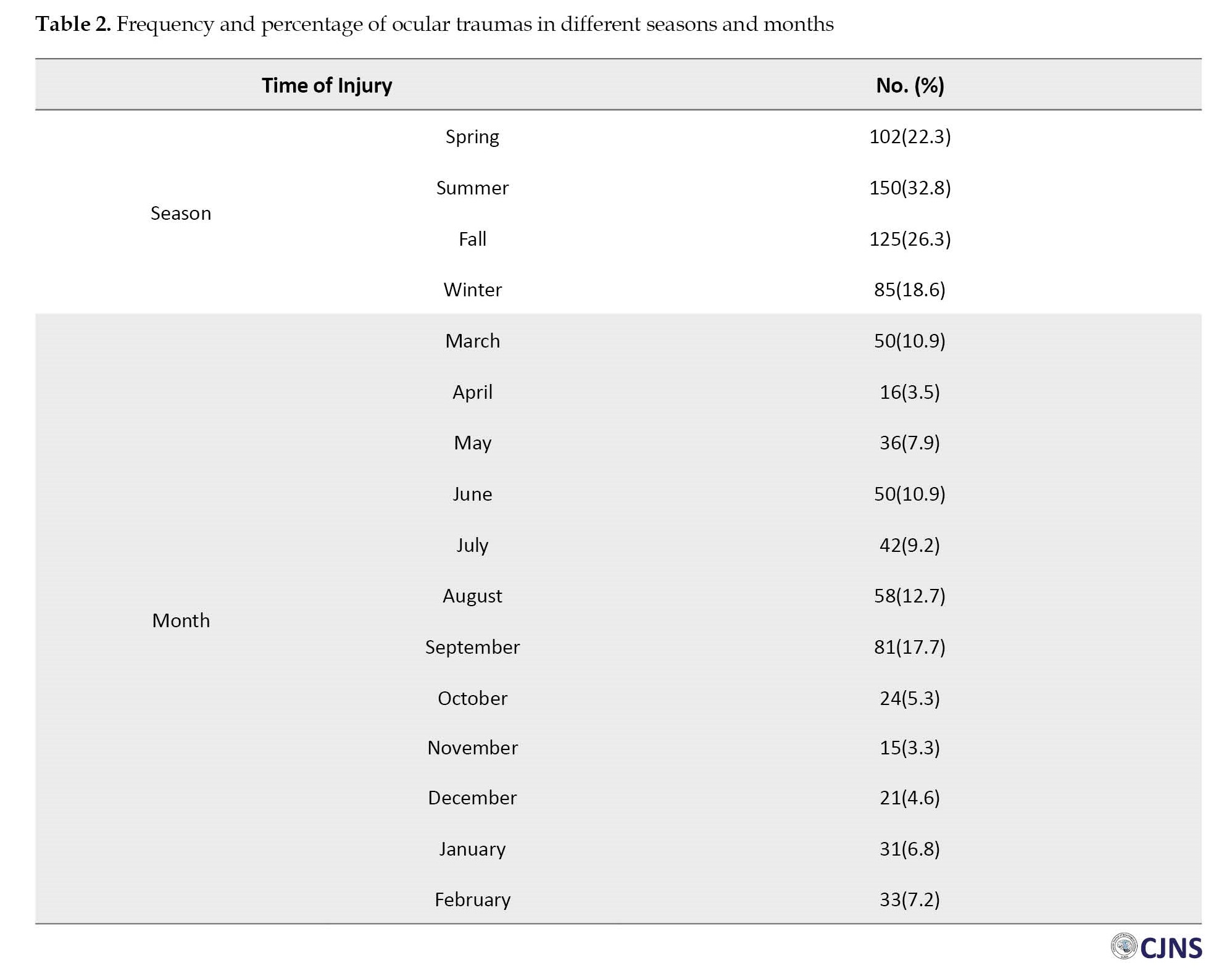
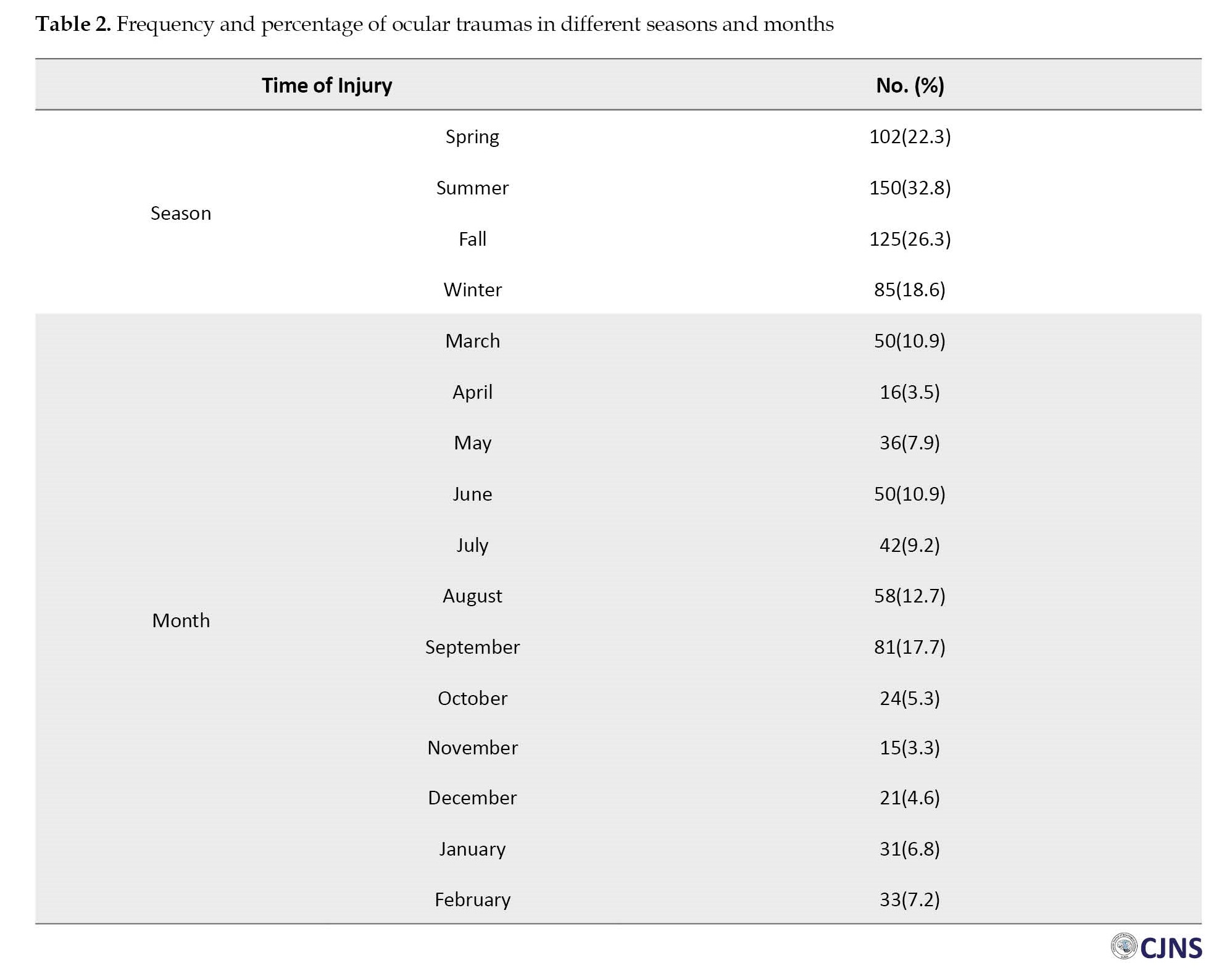
The majority of patients were living in Rasht City (81.9%), and few of them were living on the outskirts (18.1%). The majority of patients were self-employed (53.6%), while 15.5%, 12.2%, 11.8%, 5%, and 1.9% were workers, housekeepers, unemployed, retired, and farmers, respectively. The most common location of the accident was home (57.1%), followed by the workplace (42.9%). Regarding the workplace, the majority of patients were working in the private sector (30.7%). The ocular traumas occurred mostly in summer (32.8%), while 26.3% occurred in fall and 22.3% in spring. Regarding the month of injury, most of the ocular traumas occurred in September (17.7%) and August (12.7%) (Table 2).
Of 462 cases, 47.6% (n=220) had an injury in the left eye and 44.4% (n=205) in the right eye. Only 8% (n=37) had injuries in both eyes. Most of the patients (84.0%) were referred to the hospital within 12 hours after trauma, and few of them needed hospitalization (5.5%). Moreover, 13.6% were referred to the hospital within three days. Most cases (94.7%, n=437) did not use eye safety glasses. Only 4.8% (n=23) of males and 0.4% (n=2) of females had protective eyewear.
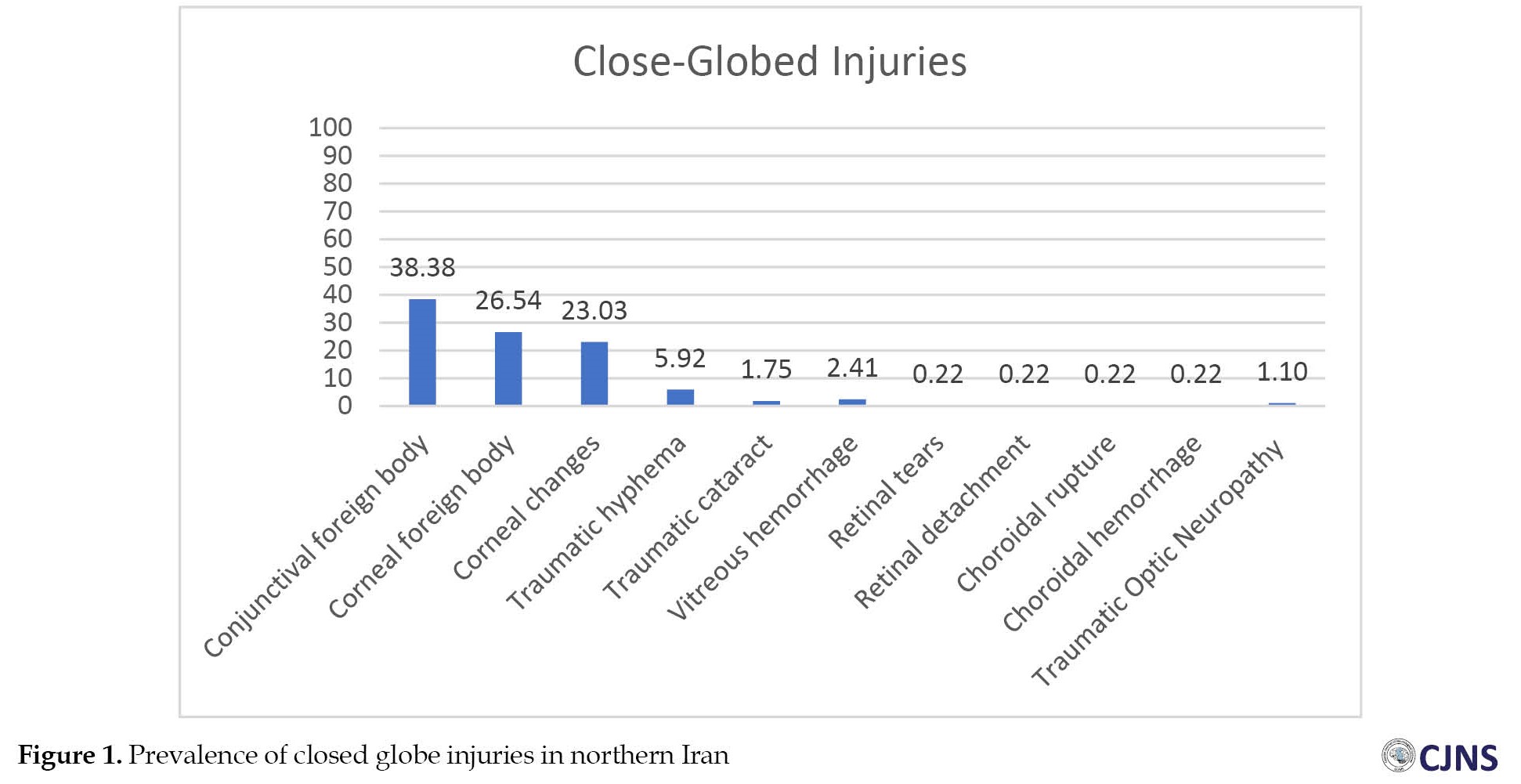
The majority of traumas were closed glob injuries (96%, n=443) in which conjunctival foreign body (38.37%, n=171), corneal foreign body (n=121, 26.23%), corneal changes (23.02%, n=105) were the most common types. Open globe injuries were seen in 4% (n=9) (Table 3).
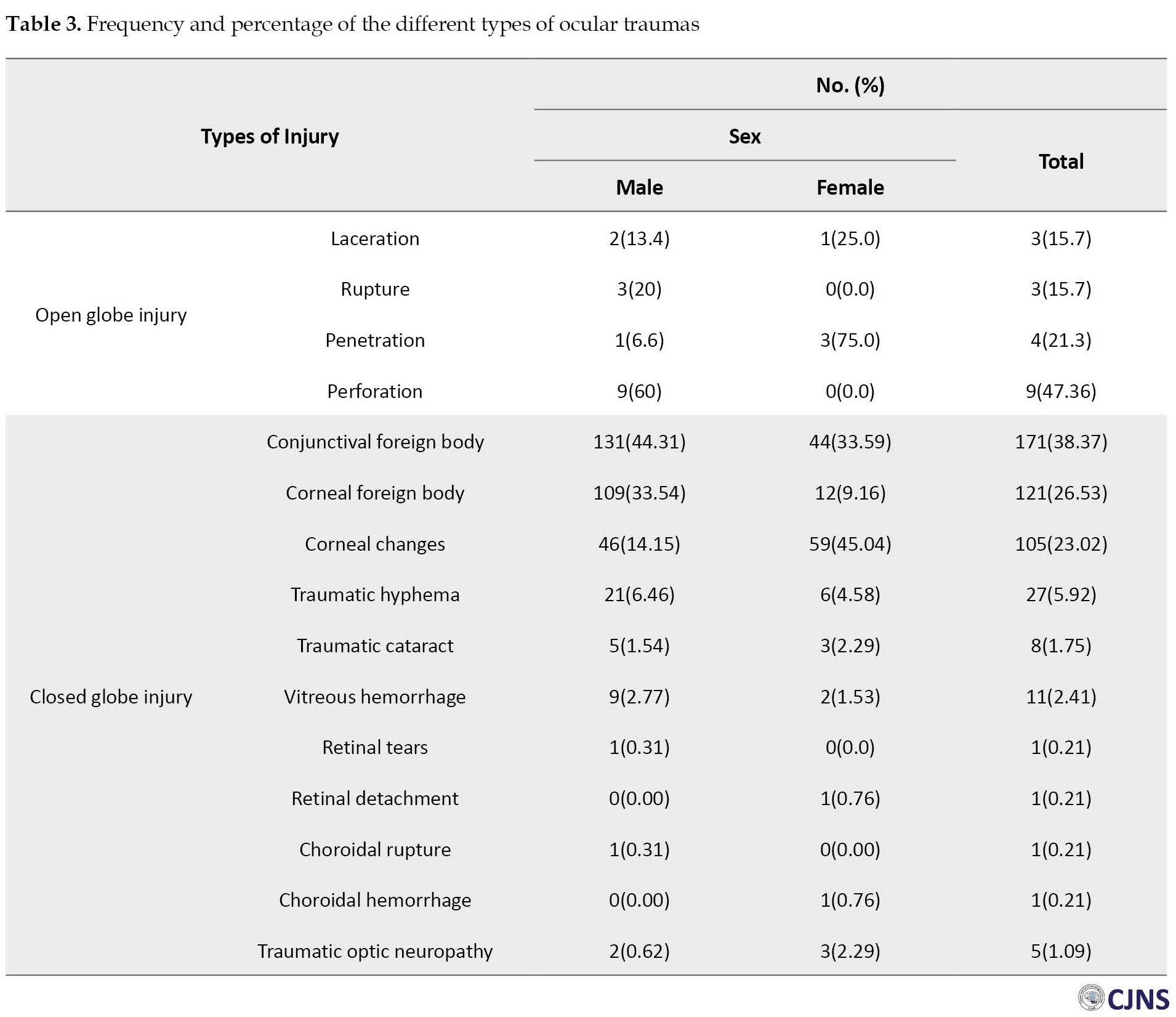
Corneal epithelial defect was the most common type of corneal changes, which was higher in females (36.1%, n=48) than in males (13.1%, n=43), while conjunctival foreign body and corneal foreign body were higher in males than in females (Table 3, Figure 1).
Discussion
Eye trauma is one of the serious public health problems worldwide and can cause blindness and visual impairments. Informing people about the risk factors and severity of eye traumas and increasing their knowledge in case of exposure to such traumas can prevent possible visual impairments. This is a large-scale epidemiological study conducted in northern Iran to investigate the epidemiology of ocular trauma cases.
The results of our study reported that most of the ocular trauma (28.8%) occurred in young and middle-aged people (31-40 years age group). In the studies conducted by Bazzazi et al., Al-Mahrouqi et al., and Taghavi et al. [7, 8, 9], the mean age of patients was 24.01, 35.49, and 23 years, respectively, while in our study the mean age of patients was 41.5±17.4 years, indicating that Guilan Province has older patients with ocular trauma. Although in most studies [7, 10-12], males had the highest rate of ocular trauma (in line with our study), females with ocular trauma in our study had a relatively higher injury rate compared to other studies in Iran. This can be one of the important points of our study because females play an important role in the family economy, and since most of the women in northern Iran work at home or in the handicraft industry, it may lead to increased ocular traumas.
Eighty percent of patients in our study visited the hospital within first 12 hours after injury while in some studies it even took 24 h [13-15]. This is because Guilan is small province with high population density and the eye emergency department was the only eye care center with appropriate accessibility. Furthermore, the literacy level of people was high which led to their quick referral. In this study, summer (31.9%) was the most common season for ocular trauma followed by fall (28.6%) and spring (22.3%), which is consistent with the results of Maurya et al. [6]. Shaeri et al. reported that the majority of traumas occurred at home (57.1%) [1] similar to our findings, while Wang et al. and other study indicated that workplace was the most common location of eye injuries [6, 16]. This discrepancy may be due to socioeconomic and geographical differences. In our study, 47.3% of patients had injury in the left eye, 44.1% in the right eye, and 8.6% in both eyes. Pawaiya et al. reported that 43.6% of patients were affected in the right eye, 50.9% in the left eye, and only nine patients had bilateral eye trauma [17]. Wang et al. also showed that 48.5% of patients had trauma in their right eye and 49.4% in their left eye, and 2.1% had bilateral trauma [16].
Our study showed that closed globe injuries were the most common types of eye traumas (96.0%) and the prevalence of open globe injuries was at a very low level (4.0%), similar to Syal et al.’s [14] study, who reported that 60.5% of traumas were closed globe injuries. Singh et al [15], found that open and closed globe injuries were the most prevalent types of traumas at 48% and 49% respectively. Pawaiya et al. also reported that closed globe injury was the most common type of eye trauma [17]. According to them, this was because the use of protective eyewear is less common among people especially those working at home. Using eye safety glasses can reduce the chance of trauma by 90% [18]. It may be true about our patients. Therefore, adopting strategies to persuade people to wear safety glasses can be helpful in reducing the prevalence of closed globe injuries. One of the limitations of this study was the incomplete records of patients and lack of documentation of some patients. This issue can affect the reported statistics, but is negligible due to the digital from of the records.
Conclusion
Most of eye trauma in northern Iran occur in young and middle-aged people and the majority of cases visit the hospital within the first 12 hours after trauma. The prevalence of eye trauma is higher in males. In addition, closed globe injuries are the most common types of ocular trauma in this region. Most of the eye traumas are preventable using protective equipment and better awareness of its risk factors. It is recommended to conducted further studies periodically.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. This study was approved by the Ethical Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.506).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization and study design: Yousef Alizadeh and Maryam Dourandeesh; Data acquisition: Narges Pourdeilami, Abdolreza Medghalchi, Hassan Behboudi, Ebrahim Azaripour, Mitra Akbari, Reza Soltani-Moghadam; Statistical analysis: Ehsan Kazemnezhad Leyli and Ghazaleh Mohammadi-Manesh; Writing: Ghazaleh Mohammadi-Manesh, Shila Kianmehr and Halleh Alizadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the patients at Amir-Almomenin Hospital who participated in this study for their cooperation.
References
Ocular trauma is a debilitating condition and one of the most important and leading causes of visual impairments that can impose a high socioeconomic cost burden on the community [1]. According to the World Health Organization (WHO), there are 55 million annual cases of ocular trauma, which can affect daily activities [2]. Ocular trauma accounts for blindness in 75,100,000 people in developing countries and 9,100,000 people in developed countries [3]. It has been estimated that the annual incidence of hospitalized eye injuries is 6.5-27.7 per 100000 people [4].
According to studies, most of the ocular trauma cases in the U.S. are caused by unintentional injuries (77%) and assaults (22%). In European countries, as developed countries, the incidence of work-related ocular traumas is low, and most of them are caused by accident. In Asia, with developing countries having poor access to medical services, there are more cases [3]. Based on the studies, work-related and unexpected events are the most common causes of ocular trauma. Moreover, globe injuries are more common than non-globe injuries. The common globe injuries include mechanical, chemical, photic, and thermal injuries [5].
While 90% of ocular traumas are preventable, especially in childhood, there is a need to manage preventive measures and extensive epidemiological data [6]. North of Iran is one of the most common places for traumas, especially ocular traumas, due to the greater amount of physical and outdoor activities. Despite the prevalence of traumas in the north of Iran; there is limited information. Therefore, this study aims to investigate the epidemiology of ocular trauma cases in patients referred to a tertiary center in northern Iran.
Materials and Methods
This cross-sectional study was conducted in Amir-Almomenin Hospital affiliated to Guilan University of Medical Sciences in Rasht, northern Iran in 2021-22. Among 956 cases referred to the eye emergency department of Amir-Almomenin Hospital, 462 cases with ocular trauma were included in the study. Personal information (including age, sex, occupation, place of residence), location of the accident, the use of eye protection equipment, time (season/month) of the accident, and type of injury were collected using a checklist. The collected data were analyzed in SPSS software, version 26. Mean±SD and number (percentage) were used for describing quantitative and qualitative variables, respectively.
Results
Among 462 cases with ocular trauma, 71.0% were male, and their mean age was 41.5±17.4 years, ranging from 1 to 91 years. Most of them were in the 31-40 years group (28.8%) followed by the 21-30 years group (23.3%) (Table 1).
The majority of patients were living in Rasht City (81.9%), and few of them were living on the outskirts (18.1%). The majority of patients were self-employed (53.6%), while 15.5%, 12.2%, 11.8%, 5%, and 1.9% were workers, housekeepers, unemployed, retired, and farmers, respectively. The most common location of the accident was home (57.1%), followed by the workplace (42.9%). Regarding the workplace, the majority of patients were working in the private sector (30.7%). The ocular traumas occurred mostly in summer (32.8%), while 26.3% occurred in fall and 22.3% in spring. Regarding the month of injury, most of the ocular traumas occurred in September (17.7%) and August (12.7%) (Table 2).
Of 462 cases, 47.6% (n=220) had an injury in the left eye and 44.4% (n=205) in the right eye. Only 8% (n=37) had injuries in both eyes. Most of the patients (84.0%) were referred to the hospital within 12 hours after trauma, and few of them needed hospitalization (5.5%). Moreover, 13.6% were referred to the hospital within three days. Most cases (94.7%, n=437) did not use eye safety glasses. Only 4.8% (n=23) of males and 0.4% (n=2) of females had protective eyewear.
The majority of traumas were closed glob injuries (96%, n=443) in which conjunctival foreign body (38.37%, n=171), corneal foreign body (n=121, 26.23%), corneal changes (23.02%, n=105) were the most common types. Open globe injuries were seen in 4% (n=9) (Table 3).
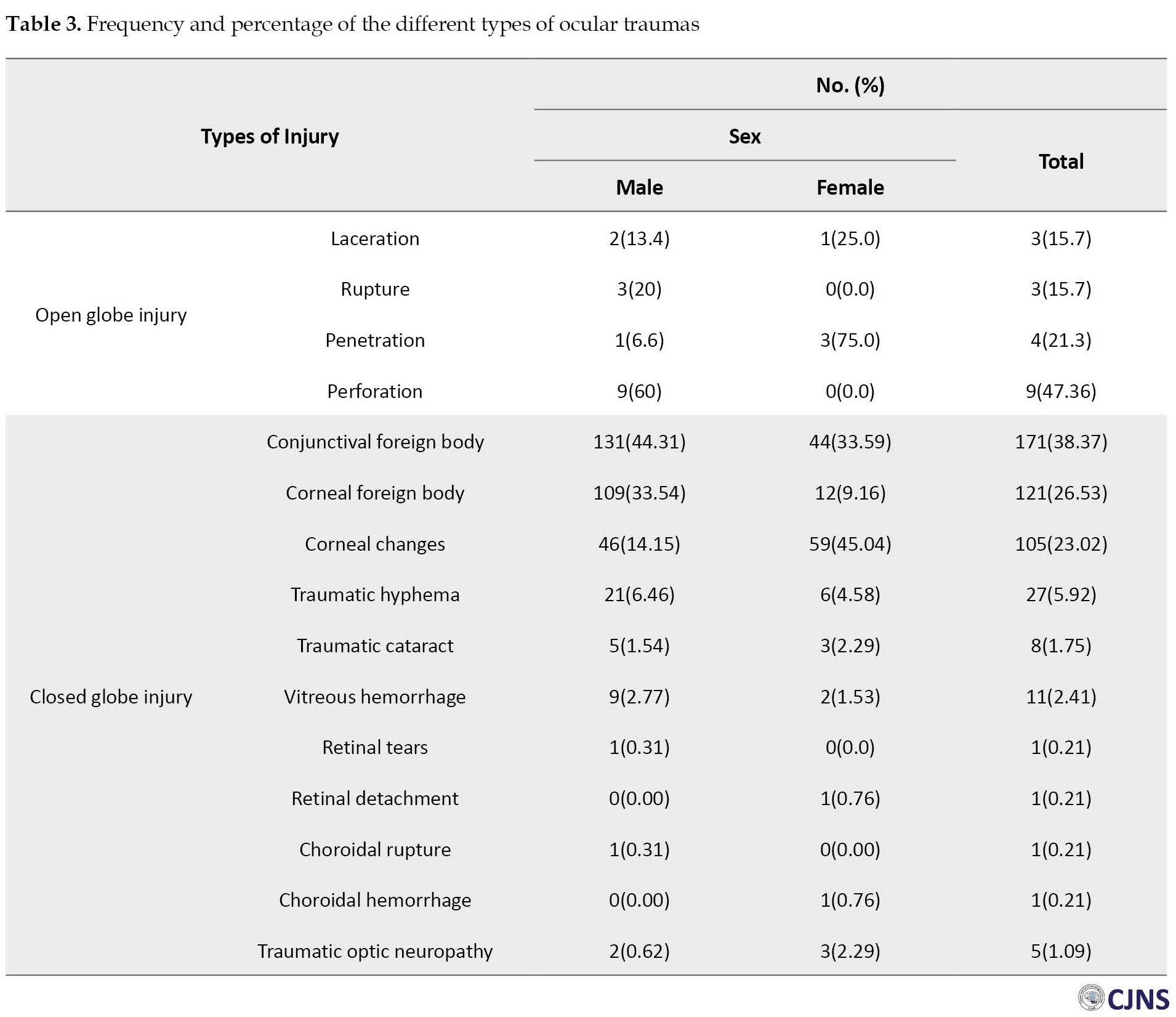
Corneal epithelial defect was the most common type of corneal changes, which was higher in females (36.1%, n=48) than in males (13.1%, n=43), while conjunctival foreign body and corneal foreign body were higher in males than in females (Table 3, Figure 1).
Discussion
Eye trauma is one of the serious public health problems worldwide and can cause blindness and visual impairments. Informing people about the risk factors and severity of eye traumas and increasing their knowledge in case of exposure to such traumas can prevent possible visual impairments. This is a large-scale epidemiological study conducted in northern Iran to investigate the epidemiology of ocular trauma cases.
The results of our study reported that most of the ocular trauma (28.8%) occurred in young and middle-aged people (31-40 years age group). In the studies conducted by Bazzazi et al., Al-Mahrouqi et al., and Taghavi et al. [7, 8, 9], the mean age of patients was 24.01, 35.49, and 23 years, respectively, while in our study the mean age of patients was 41.5±17.4 years, indicating that Guilan Province has older patients with ocular trauma. Although in most studies [7, 10-12], males had the highest rate of ocular trauma (in line with our study), females with ocular trauma in our study had a relatively higher injury rate compared to other studies in Iran. This can be one of the important points of our study because females play an important role in the family economy, and since most of the women in northern Iran work at home or in the handicraft industry, it may lead to increased ocular traumas.
Eighty percent of patients in our study visited the hospital within first 12 hours after injury while in some studies it even took 24 h [13-15]. This is because Guilan is small province with high population density and the eye emergency department was the only eye care center with appropriate accessibility. Furthermore, the literacy level of people was high which led to their quick referral. In this study, summer (31.9%) was the most common season for ocular trauma followed by fall (28.6%) and spring (22.3%), which is consistent with the results of Maurya et al. [6]. Shaeri et al. reported that the majority of traumas occurred at home (57.1%) [1] similar to our findings, while Wang et al. and other study indicated that workplace was the most common location of eye injuries [6, 16]. This discrepancy may be due to socioeconomic and geographical differences. In our study, 47.3% of patients had injury in the left eye, 44.1% in the right eye, and 8.6% in both eyes. Pawaiya et al. reported that 43.6% of patients were affected in the right eye, 50.9% in the left eye, and only nine patients had bilateral eye trauma [17]. Wang et al. also showed that 48.5% of patients had trauma in their right eye and 49.4% in their left eye, and 2.1% had bilateral trauma [16].
Our study showed that closed globe injuries were the most common types of eye traumas (96.0%) and the prevalence of open globe injuries was at a very low level (4.0%), similar to Syal et al.’s [14] study, who reported that 60.5% of traumas were closed globe injuries. Singh et al [15], found that open and closed globe injuries were the most prevalent types of traumas at 48% and 49% respectively. Pawaiya et al. also reported that closed globe injury was the most common type of eye trauma [17]. According to them, this was because the use of protective eyewear is less common among people especially those working at home. Using eye safety glasses can reduce the chance of trauma by 90% [18]. It may be true about our patients. Therefore, adopting strategies to persuade people to wear safety glasses can be helpful in reducing the prevalence of closed globe injuries. One of the limitations of this study was the incomplete records of patients and lack of documentation of some patients. This issue can affect the reported statistics, but is negligible due to the digital from of the records.
Conclusion
Most of eye trauma in northern Iran occur in young and middle-aged people and the majority of cases visit the hospital within the first 12 hours after trauma. The prevalence of eye trauma is higher in males. In addition, closed globe injuries are the most common types of ocular trauma in this region. Most of the eye traumas are preventable using protective equipment and better awareness of its risk factors. It is recommended to conducted further studies periodically.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. This study was approved by the Ethical Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.506).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization and study design: Yousef Alizadeh and Maryam Dourandeesh; Data acquisition: Narges Pourdeilami, Abdolreza Medghalchi, Hassan Behboudi, Ebrahim Azaripour, Mitra Akbari, Reza Soltani-Moghadam; Statistical analysis: Ehsan Kazemnezhad Leyli and Ghazaleh Mohammadi-Manesh; Writing: Ghazaleh Mohammadi-Manesh, Shila Kianmehr and Halleh Alizadeh.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the patients at Amir-Almomenin Hospital who participated in this study for their cooperation.
References
- Shaeri M, Mahdian M, Akbari H, Azizzadeh Asl S. Incidence and related factors of surface eye disorders in traumatic intensive care unit patients in Iran. Int J Burns Trauma. 2021; 11(4):344-9. [PMID]
- Chua D, Wong W, Lamoureux EL, Aung T, Saw SM, Wong TY. The prevalence and risk factors of ocular trauma: The Singapore Indian eye study. Ophthalmic Epidemiol. 2011; 18(6):281-7. [DOI:10.3109/09286586.2011.628775] [PMID]
- Feng K. Epidemiology of ocular trauma. In: Yan H, editor. Anatomy and examination in ocular trauma. Singapore: Springer Singapore; 2019. [DOI:10.1007/978-981-13-0068-4_6]
- Asadi F, Ramezanghorbani N, Almasi S, Rangraz MH. Eye injury registries: A review on key registry processes. Iran J Public Health. 2021; 50(12):2495-508. [PMID]
- Jafari AK, Anvari F, Ameri A, Bozorgui S, Shahverdi N. Epidemiology and sociodemographic aspects of ocular traumatic injuries in Iran. Int Ophthalmol. 2010; 30(6):691-6.[DOI:10.1007/s10792-010-9401-0] [PMID]
- Maurya RP, Srivastav T, Singh VP, Mishra CP, Al-Mujaini A. The epidemiology of ocular trauma in Northern India: A teaching hospital study. Oman J Ophthalmol. 2019; 12(2):78-83. [DOI:10.4103/ojo.OJO_149_2018] [PMID]
- Bazzazi N, Akbarzadeh S, Yavarikia M, Hosseinpour Z. [Epidemiologic evaluation of ocular trauma in patients admitted to ophthalmology ward of Farshchian Hospital in Hamadan in 2012 (Persian)]. Avicenna J Clin Med. 2014; 21(1):25-31. [Link]
- Al-Mahrouqi HH, Al-Harthi N, Al-Wahaibi M, Hanumantharayappa K. Ocular trauma: A tertiary hospital experience from Oman. Oman J Ophthalmol. 2017; 10(2):63-9. [PMID]
- Taghavi Y, Soleimani M, Mokhtaree M, Taheri A. The prevalence of ocular diseases among individuals referring to the ocular emergency unit of Moradi Hospital of Rafsanjan, Iran: 2015. J Occup Health Epidemiol. 2017; 6(2):77-83 [DOI:10.29252/johe.6.2.77]
- Ababneh LT, Mohidat H, Abdelnabi H, Kana'an MF, Tashtush NA, El-Mulki OS, et al. Hospital-based ocular trauma: Factors, treatment, and impact outcome. Clin Ophthalmol. 2019; 13:2119-26. [DOI:10.2147/OPTH.S223379] [PMID]
- Alem KD, Arega DD, Weldegiorgis ST, Agaje BG, Tigneh EG. Profile of ocular trauma in patients presenting to the department of ophthalmology at Hawassa University: Retrospective study. Plos One. 2019; 14(3):e0213893. [DOI:10.1371/journal.pone.0213893] [PMID]
- Balaghafari A, Siamian H, Aligolbandi K. Ocular trauma: 2 years retrospective study in Sari, Iran. Mater Sociomed. 2013; 25(4):230-2. [DOI:10.5455/msm.2013.25.230-232] [PMID]
- Abbasi M, Nezamzadeh M, Farsi Z, Khodamoradi B. [The frequency of ocular trauma in military victims referred to the military specialist hospitals (Persian)]. Mil Caring Sci. 2017; 4(4):266-71. [DOI:10.29252/mcs.4.4.266]
- Syal E, Dhawan M, Singh S. To study the epidemiological and clinical profile of ocular trauma at a tertiary health-care facility. Delta Journal of Ophthalmology. 2018; 19(4):259-67.[DOI:10.4103/DJO.DJO_14_18]
- Singh K, Singh J. Profile of ocular trauma patients in a tertiary care hospital in India: A prospective study. Int J Med Biomed Stud. 2020; 4(12). [DOI:10.32553/ijmbs.v4i12.1603]
- Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South-Central China. Acta Ophthalmol. 2017; 95(6):e503-10. [DOI:10.1111/aos.13438]
- Pawaiya S, Aggarwal S, Arora R, Sharma V, Kumar A, Rao S, et al. Ocular trauma: An epidemiological study in a tertiary center. Santosh Univ J Health Sci. 2022; 8(1):43-7. [Link]
- Comez AT, Ozbas M. Evaluation and management of ocular traumas. In: Lo Giudice G, editor.Vision Correction and Eye Surgery. London: IntechOpen; 2022. [Link]
Type of Study: Research |
Subject:
Special
Received: 2023/07/17 | Accepted: 2023/12/4 | Published: 2024/04/1
Received: 2023/07/17 | Accepted: 2023/12/4 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |