Wed, May 8, 2024
Volume 10, Issue 2 (Spring 2024)
Caspian J Neurol Sci 2024, 10(2): 117-125 |
Back to browse issues page
Ethics code: I.R.GUMS.REC.1400.354
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pourramzani A, Gharaei Nejad K, Sayar S. Alexithymia and Suicidal Ideation in Iranian Patients With Psoriasis. Caspian J Neurol Sci 2024; 10 (2) :117-125
URL: http://cjns.gums.ac.ir/article-1-677-en.html
URL: http://cjns.gums.ac.ir/article-1-677-en.html
1- Kavosh Behavioral, Cognitive and Addiction Research Center, Shafa Hospital, Guilan University of Medical Science, Rasht, Iran.
2- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences (GUMS), Rasht, Iran. , kavehgharaeinejad@gmail.com
3- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences (GUMS), Rasht, Iran.
2- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences (GUMS), Rasht, Iran. , kavehgharaeinejad@gmail.com
3- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences (GUMS), Rasht, Iran.
Full-Text [PDF 1270 kb]
(93 Downloads)
| Abstract (HTML) (140 Views)
Full-Text: (60 Views)
Introduction
Psoriasis, as a chronic inflammatory skin disorder affecting millions worldwide, not only causes physical challenges but also takes a toll on mental health. Psoriasis affects approximately 2% of the world’s population and significantly influence the patients’ quality of life. Psoriasis has adverse mental health outcomes such as psychosis, suicidal thoughts, anxiety, depression, distressing emotions, and emotional dysregulation [1-3]. In addition, studies have highlighted the increased prevalence of mental health issues, such as alexithymia and suicidal thoughts, among individuals with psoriasis. Investigating the prevalence, associated factors, and implications of this disease is crucial for designing effective interventions and comprehensive care strategies [4, 5]. Patients with psoriasis often face psychosocial stressors, such as social stigma, negative body image, and reduced quality of life, which can contribute to the development of mental health problems [6, 7]. Alexithymia is a personality trait with difficulty externally oriented thinking, emotion perception and expression. Patients with alexithymia and psoriasis have lower quality of life and higher anxiety and depression and are at a higher risk of alcoholism than those with only mild alexithymia [8, 9]. Alexithymia is more common in women and young people, with a younger age of disease onset and skin lesions in sensitive areas such as hands, scalp, face, and genitalia [1].
The presence of suicidal thoughts among patients with psoriasis demands urgent attention. Studies have indicated a higher prevalence of suicidal ideation in these people compared to the general population, emphasizing the need for tailored suicide prevention strategies [10, 11]. Recognizing the factors associated with suicidal thoughts, such as disease severity, demographic characteristics, and comorbid psychiatric conditions, can aid in risk assessment, early intervention, and improved patient outcomes [12, 13]. Therefore, conducting a systematic investigation of the prevalence of alexithymia and suicidal thoughts and the related factors in patients with psoriasis is important [14, 15]. In this regard, the present study aims to investigate the prevalence and comorbidity of alexithymia and suicidal ideation in individuals with psoriasis in Iran. The findings can help develop targeted screening protocols and personalized intervention strategies, integrate mental health care into routine psoriasis management, and consequenctly improve the overall well-being and quality of life of the patients.
Materials and Methods
Study design and sample size
This cross-sectional study was conducted on 100 patients with psoriasis referred to Razi Dermatology Clinic and Beesat Clinic of hospitals affiliated to Guilan University of Medical Sciences, Rasht, Iran, in 2020. They all declared their informed consent to participate in the study. The individuals whose psoriasis was diagnosed and confirmed by a dermatologist (second author) were included in this study, and those with other skin diseases, cancer, autoimmune diseases, and psychological and psychiatric diseases, or incomplete data were excluded from the study. A correlation-based formula was used to determine the sample size. Considering the statistical power of 80%, the significance level of 0.05, and the correlation coefficient of 0.28 between total positive symptoms and alexithymia obtained from a previous study [16], the minimum sample size was determined to be 98. The demographic and clinical characteristics such as age, gender, and educational level were first recorded.
Measures
Psoriasis area and severity index
The severity of psoriasis was assessed by calculating the psoriasis area and severity index (PASI), which categorizes the severity of psoriasis as mild, moderate, and severe. The PASI measures the severity of psoriasis based on four factors: Proportion of skin affected, skin flaking, skin erythema (redness), and thickness of plaque on the skin. These factors are measured in four regions of: Head, trunk, upper extremities, and lower extremities. PASI scores range from 0 to 72, with higher scores indicating higher severity of psoriasis. A score <7 indicates a mild degree, a score of 7-12 shows a moderate degree, and a score >12 shows a severe degree [17].
Toronto alexithymia scale
The Toronto alexithymia scale-20 item (TAS-20) was employed to evaluate alexithymia [18]. This questionnaire has 20 items rated on a 5-point Likert scale from “strongly disagree” to “strongly agree”. The TAS-20 assesses alexithymia in three areas: Inability to identify emotions, inability to describe emotions, and difficulty with externally oriented thinking. A total score of 61 or higher indicates alexithymia, while a score less than 61 indicates no alexithymia. The internal consistency of the Persian version of the TAS-20 using Cronbach’s α is 0.79 for healthy adults, and its test re-test reliability is 0.77 for the patients [19]. In another study in Iran, its internal consistency was between 0.66 and 0.79, and the test re-test reliability was 0.77 [20].
Beck scale for suicidal ideation
The Beck scale for suicidal ideation (BSSI) is a 19-item tool that was used to measure the intensity of suicidal thoughts in the past week [21]. It was developed by Beck et al. in 1988 [22]. The total score of BSSI ranged from 0 to 38, and each item was scored based on an ordinal scale from 0 to 2. Each person answers the first five items. If the person’s responses are positive (score 1 or 2), s/he is asked to answer the remaining items; otherwise, the questions are ended. No cutoff point is used to categorize the outcomes [23]. According to the BSSI, a score of 0-5 indicates low risk of suicide, a score of 6-19 shows high risk of suicide, and a score of 20-38 indicates a suicide attempt (very high risk). The BSSI’s reliability and validity have been confirmed in other studies, which have reported a Cronbach’s α value greater than 0.85 [22, 24, 25]. For the Persian version, Cronbach’s α coefficient was 0.79 [26].
Statistical analysis
Statistical analysis was performed in SPSS software, version 26. Frequency and percentage were used to describe qualitative data, while Mean±SD were used for quantitative data. The Kolmogorov-Smirnov test was conducted to assess whether the data were normally distributed. Levene’s test was also used to examine the homogeneity of variances. The association of the severity of psoriasis with alexithymia and suicidal ideation was evaluated using Pearson’s correlation test and Fisher’s exact test. The differences in study variables based on the demographic and clinical characteristics were assessed using the independent t-test, ANOVA, and Kruskal Wallis test. Fisher’s exact test and Spearman’s correlation test were employed to determine the association between suicidal ideation and alexithymia. P<0.05 was considered statistically significant.
Results
The mean age of participants was 37.56±10.58 years, and 51% of the patients were female. Most of the patients had mild psoriasis (81%), and the highest frequency of lesions was observed in limbs (75%; Table 1).
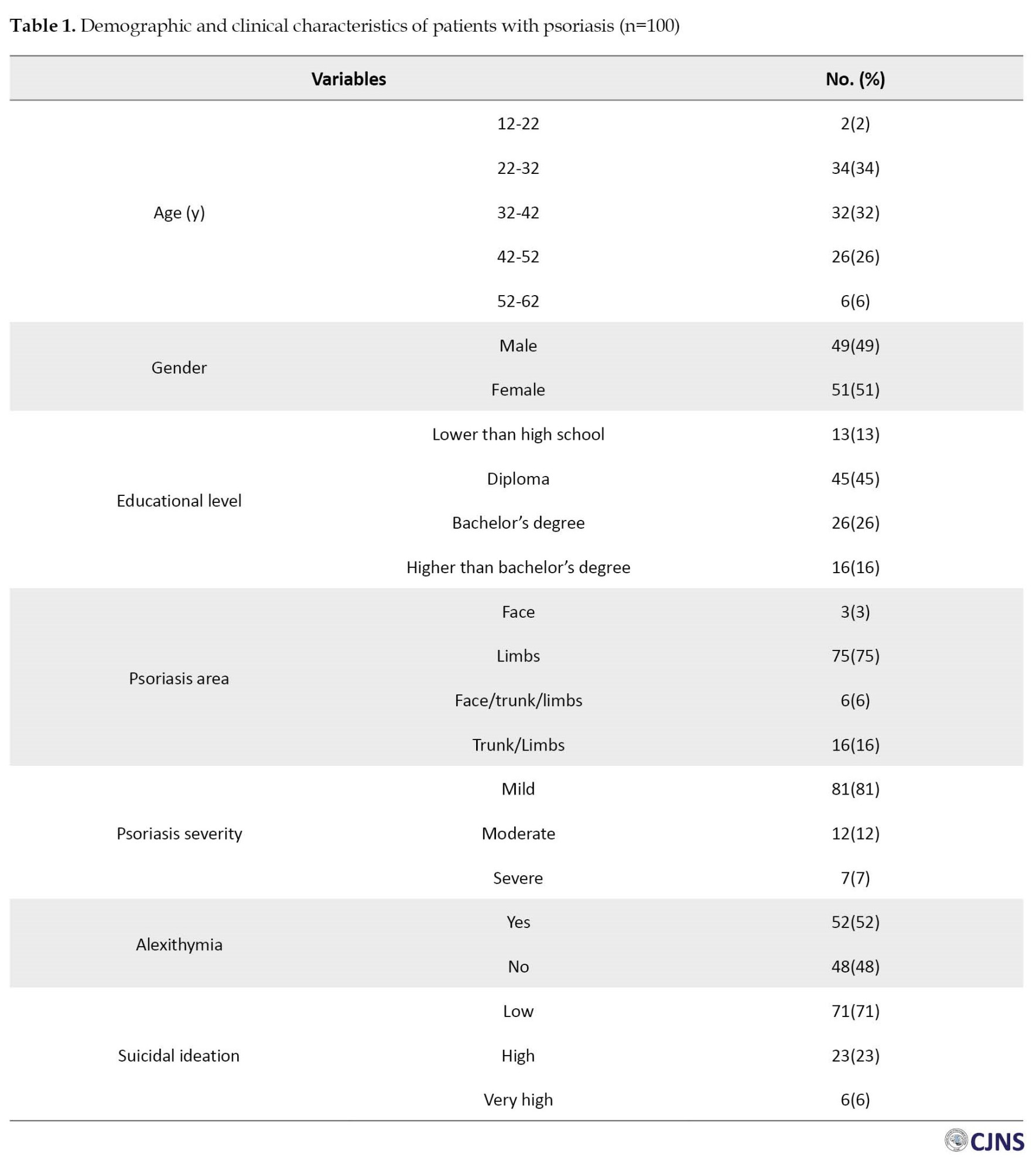
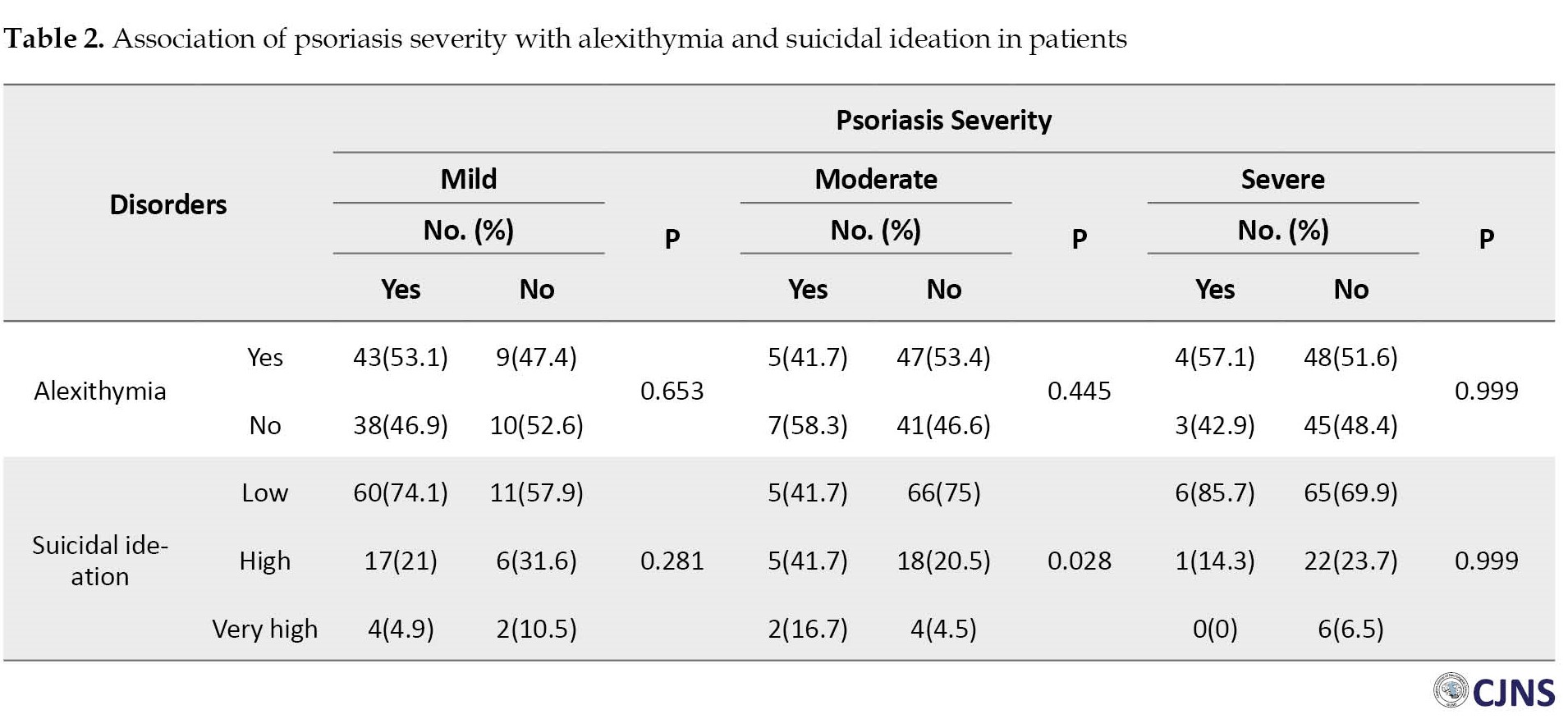
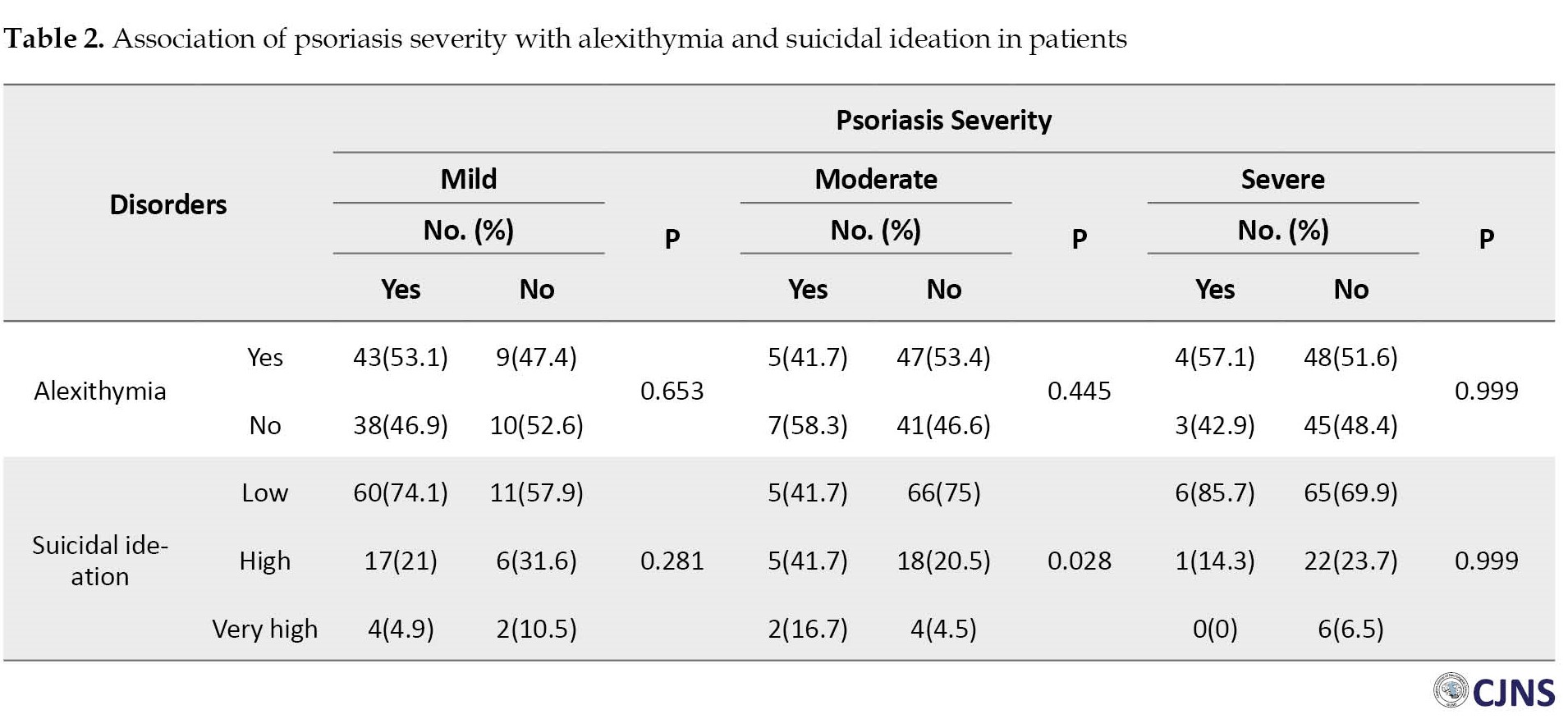
The mean TAS-20 and BSSI scores were 62.91±9.12 and 4.17±6.30, respectively. Among the patients, 52% had alexithymia. The TAS-20 score ranged from 40 to 92. In addition, 23% of the patients were at high risk, and 6% were at very high risk of suicide. The BSSI score ranged from 0 to 25. There was no significant association between mild, moderate, and severe categories of psoriasis and the prevalence of alexithymia among patients (P>0.05, Table 1). The patients with moderate severity of psoriasis were at high and very high risk of suicide more than other severity groups (P=0.028, Table 2).
Patients with alexithymia had lower mean age than those without alexithymia (35.02±9.70 vs 40.31±10.90, P=0.012). In addition, the alexithymia score had a negative association with age (P=0.042). The presence of alexithymia had no significant relationship with gender (P=0.070), while the score of alexithymia was significantly higher in males (64.96±10.07) than in females (60.94±7.72) (P=0.028, Table 3).
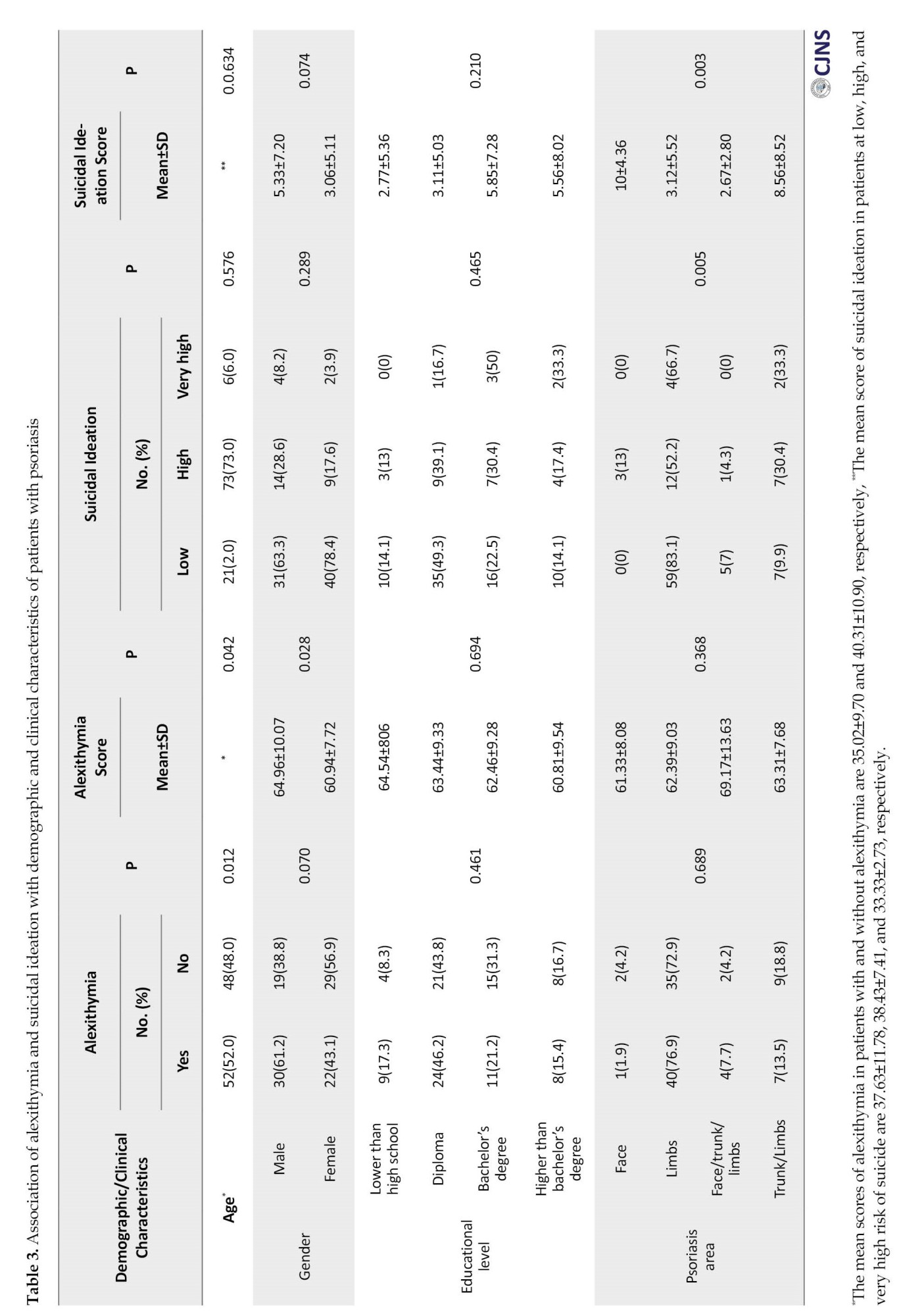
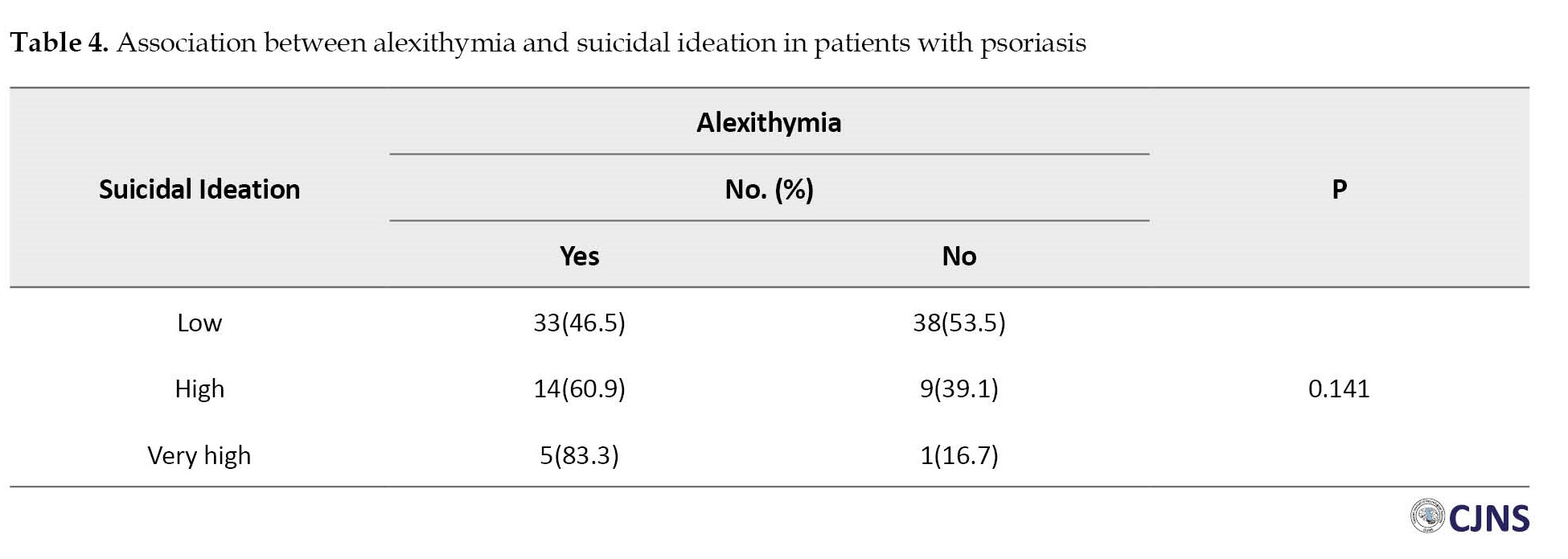
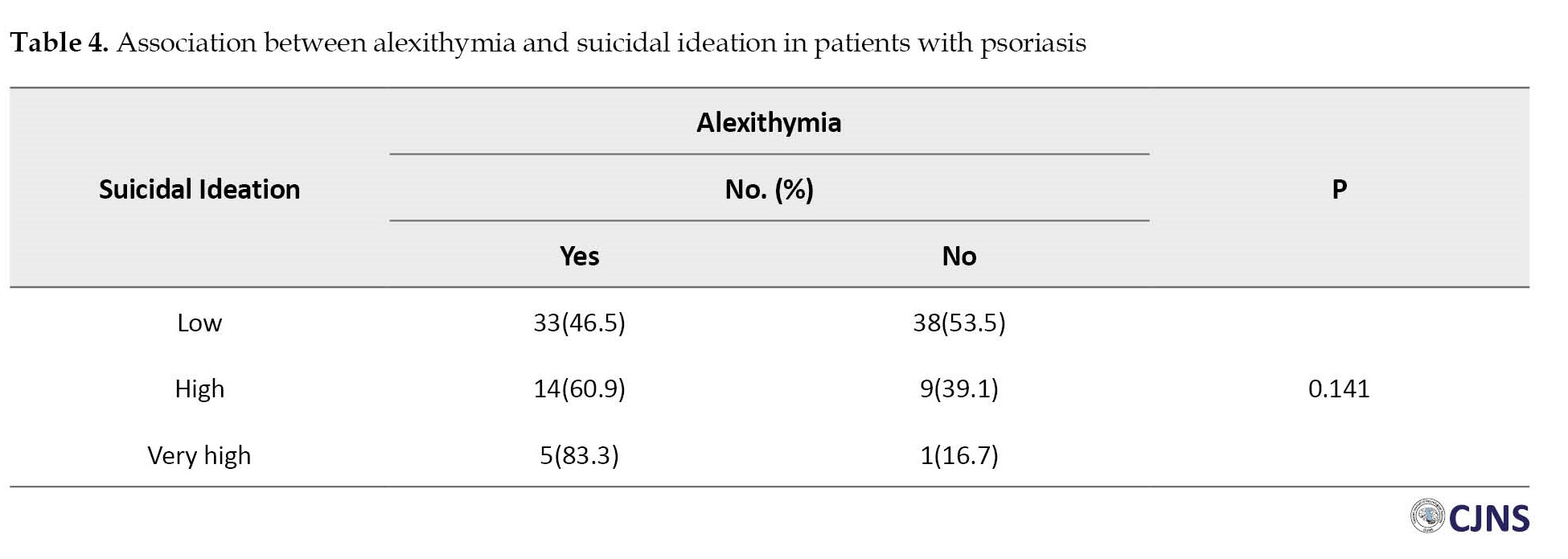
Finally, the association of age, gender, and educational level with suicidal ideation was not statistically significant (P>0.05, Table). No significant differences were found between the scores of suicidal ideation and the factors of age, gender, and educational level either (P>0.05, Table). Suicidal ideation was significantly correlated with the psoriasis area (P=0.005). Most of the patients at high and very high risk of suicide had a higher frequency of limb lesions. The highest score of BSSI was seen in those with lesions in the face and limb/trunk (10±4.36, 8.56±8.52, respectively; P=0.003). No significant difference was found in alexithymia among patients with different severity of suicidal thoughts (P=0.141, Table 4).
Based on Spearman’s correlation test, a direct and significant relationship was observed between suicidal thoughts and alexithymia; with the increase of alexithymia, suicidal thoughts also increased (r=0.28, P=0.005).
Discussion
The increasing prevalence of psychiatric disorders in patients with skin disorders brings much attention to these complications. Patients with psoriasis can be at higher risk of comorbid psychiatric conditions, including alexithymia and suicidal thoughts, compared to patients with other skin disorders [2, 5, 27]. In this regard, this study examined the prevalence and comorbidity of alexithymia and suicidal ideation in patients with psoriasis. Previous research has revealed that patients with psoriasis had higher scores of TAS-20 than healthy individuals (52.62±13.46 vs 39.63±10.21) [28]. Similarly, in our study, more than half of patients with psoriasis had alexithymia with a TAS-20 score of 62.91±9.12. Other studies reported a prevalence of 44.0% [2], 24.8% [8], 33.3% [9], and 32.4% [28] which are lower than those in our results. Furthermore, in our study, 29.0% of patients with psoriasis were at a high risk of suicide. Consistent with this result, other studies reported a higher risk of suicide in these patients compared to healthy peers [11, 29, 30].
Psoriasis severity can also be related to alexithymia and suicidal ideation, as a study showed that an increased psoriasis severity was associated with more decline in patients’ quality of life [2, 3]. Several studies have found that patients with severe psoriasis are more likely to have suicidal ideation and suicide attempts [10, 31]. In the present study, the moderate severity of psoriasis was significantly associated with suicidal thoughts. The patients with severe psoriasis had a higher alexithymia, but this association was not statistically significant. The results of studies regarding the relationship of psoriasis severity with alexithymia and suicidal ideation are conflicting; some studies found no significant association [9, 28, 32, 33]. It may indicate that alexithymia is a reasonably stable trait and not a reaction to chronic illness influenced by duration or severity [34]. Moreover, we found that the individuals with alexithymia were younger than those with no alexithymia, and the score of alexithymia decreased with the increase of age. Consistent with this finding, Lim et al. observed that younger patients and those with lower age of onset were more likely to be susceptible to alexithymia [1]. Younger patients seem more vulnerable to psoriasis and more likely to experience psychological complications. In contrast to our findings, Cherrez-Ojeda et al. found that age was not associated with alexithymia in subjects with psoriasis [9]. Based on other reports, it seems that there is an increased prevalence of alexithymia as an identity characteristic in females compared to males [4, 35, 36]. However, in our study, the alexithymia score was higher in males than in females. This may be because men have to suppress their feelings and may require more support to express their emotions compared to women, which can be related to social norms and the socialization of males [37]. In our study, most of patients with psoriasis who were at high or very high risk of suicide reported lesions in their limbs. Furthermore, the highest score of BSSI was found in those with lesions in the face and limb/trunk. Some studies showed that patients with psoriasis lesions in visible or sensitive areas are at higher risk of developing depressive disorders [1, 38-40].
Also, the mediation analysis in our study revealed that the presence of alexithymia in psoriasis patients increased suicidal ideation. Few studies have assessed the association between alexithymia and suicidal thoughts in individuals with psoriasis. Evidence suggests that psoriasis patients with alexithymia are more susceptible to negative feelings, which can negatively affect their mental health. Therefore, negative emotions due to alexithymia may be a fundamental mechanism for reducing mental health in individuals with psoriasis [2]. Our findings are also similar to the results of Tsiori et al., who showed that patients with psoriasis who were suspicious of alexithymia had higher scores in all psychopathology disorder subscales than patients with non-alexithymia [4]. Alexithymia may be associated with the expression of negative thoughts and feelings that can result in anhedonia as one of the depression symptoms [41].
The strength of this study was the examination of both the prevalence and comorbidity of alexithymia and suicidal ideation in patients with psoriasis in Iran, followed by assessing the demographic and clinical factors related to these disorders. The cross-sectional design and the small sample size were, however, the limitations of this study. Further study using a larger sample size is recommended by considering the different durations of psoriasis.
Conclusion
There is a high prevalence of alexithymia and suicidal thoughts in individuals with psoriasis in Iran, and the moderate severity of psoriasis is related to suicidal thoughts. Also, younger age and male gender were factors related to alexithymia in patients with psoriasis. Alexithymia and suicidal thoughts screening in routine clinical practice and the assessment of clinical correlates should be included in psoriasis management programs, including suicide prevention interventions.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.354). Informed consent was obtained from all participants.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, supervision, funding acquisition, review and editing: Ali Pourramzani and Kaveh Gharaei Nejad; Methodology, resources and writing the original draft: All authors; Investigation: Soheila Sayar and Kaveh Gharaei Nejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Special thanks to subjects for participating in this study and the Guilan University of Medical Science, for cooperation in data collection.
References
Psoriasis, as a chronic inflammatory skin disorder affecting millions worldwide, not only causes physical challenges but also takes a toll on mental health. Psoriasis affects approximately 2% of the world’s population and significantly influence the patients’ quality of life. Psoriasis has adverse mental health outcomes such as psychosis, suicidal thoughts, anxiety, depression, distressing emotions, and emotional dysregulation [1-3]. In addition, studies have highlighted the increased prevalence of mental health issues, such as alexithymia and suicidal thoughts, among individuals with psoriasis. Investigating the prevalence, associated factors, and implications of this disease is crucial for designing effective interventions and comprehensive care strategies [4, 5]. Patients with psoriasis often face psychosocial stressors, such as social stigma, negative body image, and reduced quality of life, which can contribute to the development of mental health problems [6, 7]. Alexithymia is a personality trait with difficulty externally oriented thinking, emotion perception and expression. Patients with alexithymia and psoriasis have lower quality of life and higher anxiety and depression and are at a higher risk of alcoholism than those with only mild alexithymia [8, 9]. Alexithymia is more common in women and young people, with a younger age of disease onset and skin lesions in sensitive areas such as hands, scalp, face, and genitalia [1].
The presence of suicidal thoughts among patients with psoriasis demands urgent attention. Studies have indicated a higher prevalence of suicidal ideation in these people compared to the general population, emphasizing the need for tailored suicide prevention strategies [10, 11]. Recognizing the factors associated with suicidal thoughts, such as disease severity, demographic characteristics, and comorbid psychiatric conditions, can aid in risk assessment, early intervention, and improved patient outcomes [12, 13]. Therefore, conducting a systematic investigation of the prevalence of alexithymia and suicidal thoughts and the related factors in patients with psoriasis is important [14, 15]. In this regard, the present study aims to investigate the prevalence and comorbidity of alexithymia and suicidal ideation in individuals with psoriasis in Iran. The findings can help develop targeted screening protocols and personalized intervention strategies, integrate mental health care into routine psoriasis management, and consequenctly improve the overall well-being and quality of life of the patients.
Materials and Methods
Study design and sample size
This cross-sectional study was conducted on 100 patients with psoriasis referred to Razi Dermatology Clinic and Beesat Clinic of hospitals affiliated to Guilan University of Medical Sciences, Rasht, Iran, in 2020. They all declared their informed consent to participate in the study. The individuals whose psoriasis was diagnosed and confirmed by a dermatologist (second author) were included in this study, and those with other skin diseases, cancer, autoimmune diseases, and psychological and psychiatric diseases, or incomplete data were excluded from the study. A correlation-based formula was used to determine the sample size. Considering the statistical power of 80%, the significance level of 0.05, and the correlation coefficient of 0.28 between total positive symptoms and alexithymia obtained from a previous study [16], the minimum sample size was determined to be 98. The demographic and clinical characteristics such as age, gender, and educational level were first recorded.
Measures
Psoriasis area and severity index
The severity of psoriasis was assessed by calculating the psoriasis area and severity index (PASI), which categorizes the severity of psoriasis as mild, moderate, and severe. The PASI measures the severity of psoriasis based on four factors: Proportion of skin affected, skin flaking, skin erythema (redness), and thickness of plaque on the skin. These factors are measured in four regions of: Head, trunk, upper extremities, and lower extremities. PASI scores range from 0 to 72, with higher scores indicating higher severity of psoriasis. A score <7 indicates a mild degree, a score of 7-12 shows a moderate degree, and a score >12 shows a severe degree [17].
Toronto alexithymia scale
The Toronto alexithymia scale-20 item (TAS-20) was employed to evaluate alexithymia [18]. This questionnaire has 20 items rated on a 5-point Likert scale from “strongly disagree” to “strongly agree”. The TAS-20 assesses alexithymia in three areas: Inability to identify emotions, inability to describe emotions, and difficulty with externally oriented thinking. A total score of 61 or higher indicates alexithymia, while a score less than 61 indicates no alexithymia. The internal consistency of the Persian version of the TAS-20 using Cronbach’s α is 0.79 for healthy adults, and its test re-test reliability is 0.77 for the patients [19]. In another study in Iran, its internal consistency was between 0.66 and 0.79, and the test re-test reliability was 0.77 [20].
Beck scale for suicidal ideation
The Beck scale for suicidal ideation (BSSI) is a 19-item tool that was used to measure the intensity of suicidal thoughts in the past week [21]. It was developed by Beck et al. in 1988 [22]. The total score of BSSI ranged from 0 to 38, and each item was scored based on an ordinal scale from 0 to 2. Each person answers the first five items. If the person’s responses are positive (score 1 or 2), s/he is asked to answer the remaining items; otherwise, the questions are ended. No cutoff point is used to categorize the outcomes [23]. According to the BSSI, a score of 0-5 indicates low risk of suicide, a score of 6-19 shows high risk of suicide, and a score of 20-38 indicates a suicide attempt (very high risk). The BSSI’s reliability and validity have been confirmed in other studies, which have reported a Cronbach’s α value greater than 0.85 [22, 24, 25]. For the Persian version, Cronbach’s α coefficient was 0.79 [26].
Statistical analysis
Statistical analysis was performed in SPSS software, version 26. Frequency and percentage were used to describe qualitative data, while Mean±SD were used for quantitative data. The Kolmogorov-Smirnov test was conducted to assess whether the data were normally distributed. Levene’s test was also used to examine the homogeneity of variances. The association of the severity of psoriasis with alexithymia and suicidal ideation was evaluated using Pearson’s correlation test and Fisher’s exact test. The differences in study variables based on the demographic and clinical characteristics were assessed using the independent t-test, ANOVA, and Kruskal Wallis test. Fisher’s exact test and Spearman’s correlation test were employed to determine the association between suicidal ideation and alexithymia. P<0.05 was considered statistically significant.
Results
The mean age of participants was 37.56±10.58 years, and 51% of the patients were female. Most of the patients had mild psoriasis (81%), and the highest frequency of lesions was observed in limbs (75%; Table 1).
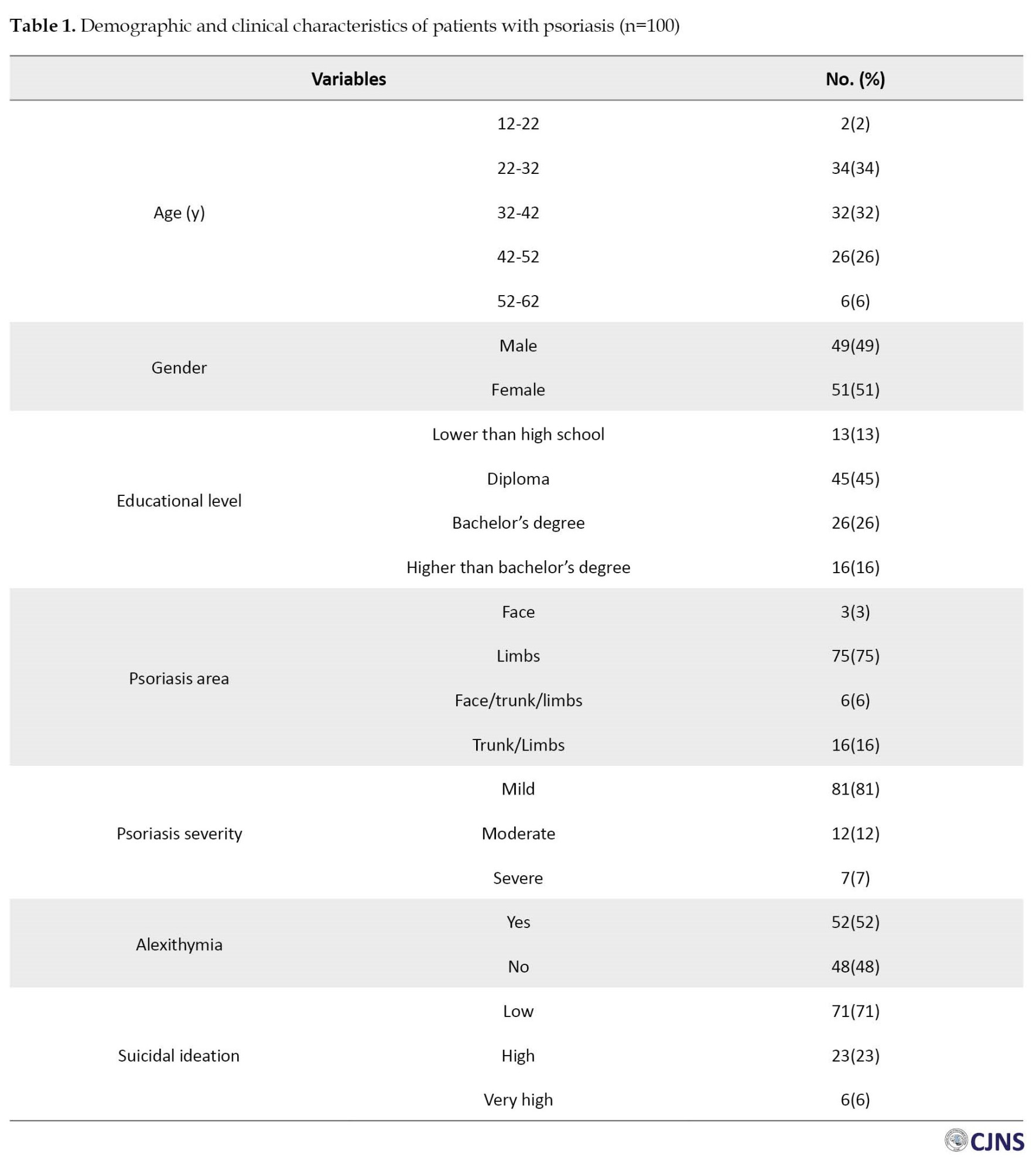
The mean TAS-20 and BSSI scores were 62.91±9.12 and 4.17±6.30, respectively. Among the patients, 52% had alexithymia. The TAS-20 score ranged from 40 to 92. In addition, 23% of the patients were at high risk, and 6% were at very high risk of suicide. The BSSI score ranged from 0 to 25. There was no significant association between mild, moderate, and severe categories of psoriasis and the prevalence of alexithymia among patients (P>0.05, Table 1). The patients with moderate severity of psoriasis were at high and very high risk of suicide more than other severity groups (P=0.028, Table 2).
Patients with alexithymia had lower mean age than those without alexithymia (35.02±9.70 vs 40.31±10.90, P=0.012). In addition, the alexithymia score had a negative association with age (P=0.042). The presence of alexithymia had no significant relationship with gender (P=0.070), while the score of alexithymia was significantly higher in males (64.96±10.07) than in females (60.94±7.72) (P=0.028, Table 3).
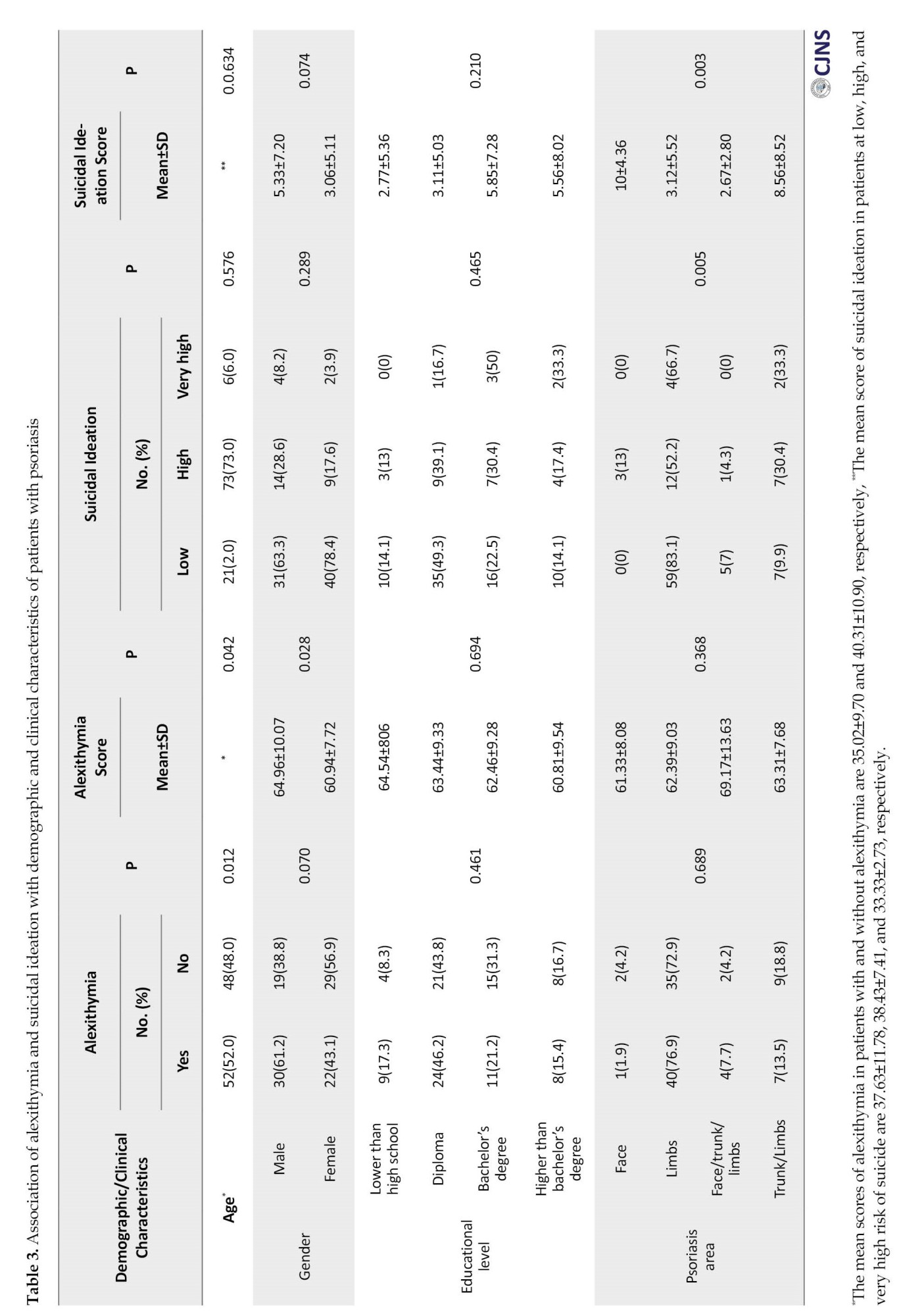
Finally, the association of age, gender, and educational level with suicidal ideation was not statistically significant (P>0.05, Table). No significant differences were found between the scores of suicidal ideation and the factors of age, gender, and educational level either (P>0.05, Table). Suicidal ideation was significantly correlated with the psoriasis area (P=0.005). Most of the patients at high and very high risk of suicide had a higher frequency of limb lesions. The highest score of BSSI was seen in those with lesions in the face and limb/trunk (10±4.36, 8.56±8.52, respectively; P=0.003). No significant difference was found in alexithymia among patients with different severity of suicidal thoughts (P=0.141, Table 4).
Based on Spearman’s correlation test, a direct and significant relationship was observed between suicidal thoughts and alexithymia; with the increase of alexithymia, suicidal thoughts also increased (r=0.28, P=0.005).
Discussion
The increasing prevalence of psychiatric disorders in patients with skin disorders brings much attention to these complications. Patients with psoriasis can be at higher risk of comorbid psychiatric conditions, including alexithymia and suicidal thoughts, compared to patients with other skin disorders [2, 5, 27]. In this regard, this study examined the prevalence and comorbidity of alexithymia and suicidal ideation in patients with psoriasis. Previous research has revealed that patients with psoriasis had higher scores of TAS-20 than healthy individuals (52.62±13.46 vs 39.63±10.21) [28]. Similarly, in our study, more than half of patients with psoriasis had alexithymia with a TAS-20 score of 62.91±9.12. Other studies reported a prevalence of 44.0% [2], 24.8% [8], 33.3% [9], and 32.4% [28] which are lower than those in our results. Furthermore, in our study, 29.0% of patients with psoriasis were at a high risk of suicide. Consistent with this result, other studies reported a higher risk of suicide in these patients compared to healthy peers [11, 29, 30].
Psoriasis severity can also be related to alexithymia and suicidal ideation, as a study showed that an increased psoriasis severity was associated with more decline in patients’ quality of life [2, 3]. Several studies have found that patients with severe psoriasis are more likely to have suicidal ideation and suicide attempts [10, 31]. In the present study, the moderate severity of psoriasis was significantly associated with suicidal thoughts. The patients with severe psoriasis had a higher alexithymia, but this association was not statistically significant. The results of studies regarding the relationship of psoriasis severity with alexithymia and suicidal ideation are conflicting; some studies found no significant association [9, 28, 32, 33]. It may indicate that alexithymia is a reasonably stable trait and not a reaction to chronic illness influenced by duration or severity [34]. Moreover, we found that the individuals with alexithymia were younger than those with no alexithymia, and the score of alexithymia decreased with the increase of age. Consistent with this finding, Lim et al. observed that younger patients and those with lower age of onset were more likely to be susceptible to alexithymia [1]. Younger patients seem more vulnerable to psoriasis and more likely to experience psychological complications. In contrast to our findings, Cherrez-Ojeda et al. found that age was not associated with alexithymia in subjects with psoriasis [9]. Based on other reports, it seems that there is an increased prevalence of alexithymia as an identity characteristic in females compared to males [4, 35, 36]. However, in our study, the alexithymia score was higher in males than in females. This may be because men have to suppress their feelings and may require more support to express their emotions compared to women, which can be related to social norms and the socialization of males [37]. In our study, most of patients with psoriasis who were at high or very high risk of suicide reported lesions in their limbs. Furthermore, the highest score of BSSI was found in those with lesions in the face and limb/trunk. Some studies showed that patients with psoriasis lesions in visible or sensitive areas are at higher risk of developing depressive disorders [1, 38-40].
Also, the mediation analysis in our study revealed that the presence of alexithymia in psoriasis patients increased suicidal ideation. Few studies have assessed the association between alexithymia and suicidal thoughts in individuals with psoriasis. Evidence suggests that psoriasis patients with alexithymia are more susceptible to negative feelings, which can negatively affect their mental health. Therefore, negative emotions due to alexithymia may be a fundamental mechanism for reducing mental health in individuals with psoriasis [2]. Our findings are also similar to the results of Tsiori et al., who showed that patients with psoriasis who were suspicious of alexithymia had higher scores in all psychopathology disorder subscales than patients with non-alexithymia [4]. Alexithymia may be associated with the expression of negative thoughts and feelings that can result in anhedonia as one of the depression symptoms [41].
The strength of this study was the examination of both the prevalence and comorbidity of alexithymia and suicidal ideation in patients with psoriasis in Iran, followed by assessing the demographic and clinical factors related to these disorders. The cross-sectional design and the small sample size were, however, the limitations of this study. Further study using a larger sample size is recommended by considering the different durations of psoriasis.
Conclusion
There is a high prevalence of alexithymia and suicidal thoughts in individuals with psoriasis in Iran, and the moderate severity of psoriasis is related to suicidal thoughts. Also, younger age and male gender were factors related to alexithymia in patients with psoriasis. Alexithymia and suicidal thoughts screening in routine clinical practice and the assessment of clinical correlates should be included in psoriasis management programs, including suicide prevention interventions.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.354). Informed consent was obtained from all participants.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, supervision, funding acquisition, review and editing: Ali Pourramzani and Kaveh Gharaei Nejad; Methodology, resources and writing the original draft: All authors; Investigation: Soheila Sayar and Kaveh Gharaei Nejad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Special thanks to subjects for participating in this study and the Guilan University of Medical Science, for cooperation in data collection.
References
- Lim DS, Bewley A, Oon HH. Psychological profile of patients with psoriasis. Ann Acad Med Singap. 2018; 47(12):516-22. [DOI:10.47102/annals-acadmedsg.V47N12p516] [PMID]
- Quinto RM, De Vincenzo F, Graceffa D, Bonifati C, Innamorati M, Iani L. The relationship between alexithymia and mental health is fully mediated by anxiety and depression in patients with psoriasis. Int J Environ Res Public Health. 2022; 19(6):3649. [DOI:10.3390%2Fijerph19063649] [PMID]
- Liang SE, Cohen JM, Ho RS. Psoriasis and suicidality: A review of the literature. Dermatol Ther. 2019; 32(1):e12771. [DOI:10.1111/dth.12771] [PMID]
- Tsiori S, Rompoti N, Kontoangelos K, Papageorgiou C, Papageorgiou C, Stratigos A, et al. Psychopathology and alexithymia in patients with moderate-to-severe psoriasis: Development of a novel index with prognostic value. Int J Environ Res Public Health. 2022; 19(7):4029. [DOI:10.3390/ijerph19074029] [PMID]
- Pompili M, Innamorati M, Forte A, Erbuto D, Lamis DA, Narcisi A, et al. Psychiatric comorbidity and suicidal ideation in psoriasis, melanoma and allergic disorders. Int J Psychiatry Clin Pract. 2017; 21(3):209-14. [DOI:10.1080/13651501.2017.1301482] [PMID]
- Carniciu S, Hafi B, Gkini MA, Tzellos T, Jafferany M, Stamu-O'Brien C. Secondary psychiatric disorders and the skin. Dermatological Reviews. 2023; 4:162-72. [DOI:10.1002/der2.211]
- Bandyopadhyay A, Hussain Kh, Bewley AP. Psychodermatology and psoriasis. Paper presented at: Proceedings of the 6th IFPA WPPA Conference. 30 June 2023; Stockholm, Sweden. [DOI:10.55788/9370f84c]
- Sampogna F, Puig L, Spuls P, Girolomoni G, Radtke MA, Kirby B, et al. Prevalence of alexithymia in patients with psoriasis and its association with disease burden: A multicentre observational study. Br J Dermatol. 2017; 176(5):1195-203. [DOI:10.1111/bjd.15243] [PMID]
- Cherrez-Ojeda I, Vanegas E, Felix M, Cherrez S, Suárez-Almendariz D, Ponton J, et al. Alexithymia in patients with psoriasis: A cross-sectional study from ecuador. Psychol Res Behav Manag. 2019; 1121-6. [DOI:10.2147/PRBM.S227021] [PMID]
- Kurd SK, Troxel AB, Crits-Christoph P, Gelfand JM. The risk of depression, anxiety, and suicidality in patients with psoriasis: A population-based cohort study. Arch Dermatol. 2010; 146(8):891-5. [DOI:10.1001/archdermatol.2010.186] [PMID]
- Singh S, Taylor C, Kornmehl H, Armstrong AW. Psoriasis and suicidality: A systematic review and meta-analysis. J Am Acad Dermatol. 2017; 77(3):425-40.e2. [DOI:10.1016/j.jaad.2017.05.019] [PMID]
- Blackstone B, Patel R, Bewley A. Assessing and improving psychological well-being in psoriasis: Considerations for the clinician. Psoriasis Targets Ther. 2022; 12:25-33. [DOI:10.2147/ptt.s328447] [PMID]
- Lada G, Chinoy H, Heal C, Warren RB, Talbot PS, Kleyn CE. Depression and suicidality in patients with psoriasis and the role of psoriatic arthritis: A cross-sectional study in a tertiary setting. J Acad Consult Psychiatry. 2022; 63(4):372-83. [DOI:10.1016/j.jaclp.2021.12.007] [PMID]
- De Berardis D, Campanella D, Serroni N, Moschetta FS, Di Emidio F, Conti C, et al. Alexithymia, suicide risk and serum lipid levels among adult outpatients with panic disorder. Compr Psychiatry. 2013; 54(5):517-22. [DOI:10.1016/j.comppsych.2012.12.013] [PMID]
- Luna PC, Chu CY, Fatani M, Borlenghi C, Adora A, Llamado LQ, et al. Psychosocial burden of psoriasis: A systematic literature review of depression among patients with psoriasis. Dermatol Ther (Heidelb). 2023; 13:3043–55. [DOI:10.1007%2Fs13555-023-01060-5]
- Hemming L, Taylor P, Haddock G, Shaw J, Pratt D. A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behaviour. J Affect Disord. 2019; 254:34-48. [DOI:10.1016/j.jad.2019.05.013] [PMID]
- Fredriksson T, Pettersson U. Severe psoriasis--oral therapy with a new retinoid. Dermatologica. 1978; 157(4):238-44. [DOI:10.1159/000250839] [PMID]
- Bressi C, Taylor G, Parker J, Bressi S, Brambilla V, Aguglia E, et al. Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: An Italian multicenter study. J Psychosom Res. 1996; 41(6):551-9. [DOI:10.1016/s0022-3999(96)00228-0] [PMID]
- Besharat MA. Psychometric characteristics of Persian version of the Toronto Alexithymia Scale-20 in clinical and non-clinical samples. Iran J Med Sci. 2008; 33(1):1-6. [Link]
- Afshari A, Afshar H, Shafiei K, Eskandari E, Adibi N. Dimentions of alexithymia, and their relationships to anxiety and depression in psychodermatologic patients. Intern Med Today. 2014; 19(5 Supplement):33-9. [Link]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psychol. 1979; 47(2):343-52. [DOI:10.1037//0022-006x.47.2.343] [PMID]
- Beck AT, Steer RA, Ranieri WF. Scale for Suicide Ideation: Psychometric properties of a self-report version. J Clin Psychol. 1988; 44(4):499-505. [DOI:10.1002/1097-4679(198807)44:4%3C499::aid-jclp2270440404%3E3.0.co;2-6] [PMID]
- Reinecke MA, Franklin-Scott RL. Assessment of suicide: Beck’s Scales for Assessing Mood and Suicidality. In: Yufit R I, Lester D, editors. Assessment, treatment, and prevention of suicidal behavior. New Jersey: John Wiley & Sons, Inc; 2005.[Link]
- Healy DJ, Barry K, Blow F, Welsh D, Milner KK. Routine use of the Beck Scale for Suicide Ideation in a psychiatric emergency department. Gen Hosp Psychiatry. 2006; 28(4):323-9. [DOI:10.1016/j.genhosppsych.2006.04.003] [PMID]
- Witte TK, Joiner Jr TE, Brown GK, Beck AT, Beckman A, Duberstein P, et al. Factors of suicide ideation and their relation to clinical and other indicators in older adults. J Affect Disord. 2006; 94(1-3):165-72. [DOI:10.1016/j.jad.2006.04.005] [PMID]
- Esfahani M, Hashemi Y, Alavi K. Psychometric assessment of beck scale for suicidal ideation (BSSI) in general population in Tehran. Med J Islam Repub Iran. 2015; 29:268. [PMID]
- De Berardis D, Fornaro M, Orsolini L, Valchera A, Carano A, Vellante F, et al. Alexithymia and suicide risk in psychiatric disorders: A mini-review. Front Psychiatry. 2017; 8:148. [DOI:10.3389%2Ffpsyt.2017.00148] [PMID]
- Korkoliakou P, Christodoulou C, Kouris A, Porichi E, Efstathiou V, Kaloudi E, et al. Alexithymia, anxiety and depression in patients with psoriasis: A case-control study. Ann Gen Psychiatry. 2014; 13(1):38. [DOI:10.1186/s12991-014-0038-7] [PMID]
- Rehman A, Gumley A, Biello S. Sleep quality and paranoia: The role of alexithymia, negative emotions and perceptual anomalies. Psychiatry Res. 2018; 259:216-22 [DOI:10.1016/j.psychres.2017.09.066] [PMID]
- Taiminen TJ, Saarijärvi S, Helenius H, Keskinen A, Korpilahti T. Alexithymia in suicide attempters. Acta Psychiatr Scand. 1996; 93(3):195-8. [DOI:10.1111/j.1600-0447.1996.tb10631.x] [PMID]
- Egeberg A, Hansen PR, Gislason GH, Skov L, Mallbris L. Risk of self-harm and nonfatal suicide attempts, and completed suicide in patients with psoriasis: A population-based cohort study. Br J Dermatol. 2016; 175(3):493-500. [DOI:10.1111/bjd.14633] [PMID]
- Chi CC, Chen TH, Wang SH, Tung TH. Risk of suicidality in people with psoriasis: A systematic review and meta-analysis of cohort studies. Am J Clin Dermatol. 2017; 18(5):621-7. [DOI:10.1007/s40257-017-0281-1] [PMID]
- Wu JJ, Penfold RB, Primatesta P, Fox TK, Stewart C, Reddy SP, et al. The risk of depression, suicidal ideation and suicide attempt in patients with psoriasis, psoriatic arthritis or ankylosing spondylitis. J Eur Acad Dermatology Venereol. 2017; 31(7):1168-75. [DOI:10.1111/jdv.14175] [PMID]
- Larsen MH, Krogstad AL, Wahl AK. Alexithymia, illness perception and self-management competency in psoriasis. Acta Derm Venereol. 2017; 97(8):934-40. [DOI:10.2340/00015555-2707] [PMID]
- Snast I, Reiter O, Atzmony L, Leshem YA, Hodak E, Mimouni D, et al. Psychological stress and psoriasis: A systematic review and meta-analysiss. Br J Dermatol. 2018; 178(5):1044-55. [DOI:10.1111/bjd.16116] [PMID]
- Korkoliakou P, Efstathiou V, Giannopoulou I, Christodoulou C, Kouris A, Rigopoulos D, et al. Psychopathology and alexithymia in patients with psoriasis. An Bras Dermatol. 2017; 92(4):510-15. [DOI:10.1590/abd1806-4841.20175660] [PMID]
- Levant RF, Wong YJ, Karakis EN, Welsh MM. Mediated moderation of the relationship between the endorsement of restrictive emotionality and alexithymia. Psychol Men Masc. 2015; 16(4):459-67. [DOI:10.1037/a0039739]
- Martínez-Ortega JM, Nogueras P, Muñoz-Negro JE, Gutiérrez-Rojas L, González-Domenech P, Gurpegui M. Quality of life, anxiety and depressive symptoms in patients with psoriasis: A case-control study. J Psychosom Res. 2019; 124:109780. [DOI:10.1016/j.jpsychores.2019.109780] [PMID]
- Sahi FM, Masood A, Danawar NA, Mekaiel A, Malik BH. Association between psoriasis and depression: A traditional review. Cureus. 2020; 12(8). [DOI:10.7759%2Fcureus.9708]
- Talamonti M, Galluzzo M, Servoli S, D'Adamio S, Bianchi L. Alexithymia and plaque psoriasis: Preliminary investigation in a clinical sample of 250 patients. Dermatology. 2017; 232(6):648-54. [DOI:10.1159/000453661] [PMID]
- Leweke F, Leichsenring F, Kruse J, Hermes S. Is alexithymia associated with specific mental disorders? Psychopathology. 2012; 45(1):22-8. [DOI:10.1159/000325170] [PMID]
Type of Study: Research |
Subject:
General
Received: 2023/05/23 | Accepted: 2023/06/27 | Published: 2024/04/1
Received: 2023/05/23 | Accepted: 2023/06/27 | Published: 2024/04/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |