Sat, May 18, 2024
Volume 9, Issue 4 (Autumn 2023)
Caspian J Neurol Sci 2023, 9(4): 268-277 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Saraei G, Mehraeen P, Soodmand M, Khoshamuoz S, Majidi S A, Ghanbari A, et al . Relationship of Meteorological Variable and Cerebrovascular Events: An Ecological Time Series Study. Caspian J Neurol Sci 2023; 9 (4) :268-277
URL: http://cjns.gums.ac.ir/article-1-669-en.html
URL: http://cjns.gums.ac.ir/article-1-669-en.html
Ghazal Saraei * 

 1, Parisa Mehraeen2
1, Parisa Mehraeen2 

 , Mostafa Soodmand2
, Mostafa Soodmand2 

 , Sara Khoshamuoz2
, Sara Khoshamuoz2 

 , Seyed Ali Majidi3
, Seyed Ali Majidi3 

 , Ali Ghanbari4
, Ali Ghanbari4 

 , Shadi Qatran2
, Shadi Qatran2 

 , Mohammad Taghi Moghadamnia2
, Mohammad Taghi Moghadamnia2 




 1, Parisa Mehraeen2
1, Parisa Mehraeen2 

 , Mostafa Soodmand2
, Mostafa Soodmand2 

 , Sara Khoshamuoz2
, Sara Khoshamuoz2 

 , Seyed Ali Majidi3
, Seyed Ali Majidi3 

 , Ali Ghanbari4
, Ali Ghanbari4 

 , Shadi Qatran2
, Shadi Qatran2 

 , Mohammad Taghi Moghadamnia2
, Mohammad Taghi Moghadamnia2 


1- Research and Technology Deputy, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Nursing & Midwifery, Rasht Branch, Islamic Azad University, Rasht, Iran
4- Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
3- Department of Nursing & Midwifery, Rasht Branch, Islamic Azad University, Rasht, Iran
4- Department of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 1610 kb]
(187 Downloads)
| Abstract (HTML) (327 Views)
References
Full-Text: (107 Views)
Introduction
Cerebrovascular diseases are a group of blood vessel diseases that disrupt blood flow to the brain, primarily affecting the elderly population and often significantly decreasing patients’ quality of life [1]. According to the World Health Organization (WHO), stroke is the second leading cause of death and the most common cause accounting for disability in adults, significantly impacting public health [2, 3]. The quality of life of these patients is often severely affected by readmission, recurrent accidents, depression, fatigue, and other conditions. These conditions often require long-term care [2].
Stroke is a clinical syndrome characterized by an acute neurological disorder triggered by a blood clot obstruction (ischemic stroke) or a blood vessel rupture (hemorrhagic stroke). It depletes the brain’s oxygen and nutrients and consequently causes brain damage. Despite significant advances in early diagnosis and treatment of stroke, its induced deaths are among the greatest challenges in our society [3].
Climate change will be one of the most serious challenges to human health in the 21st century, as it will directly or indirectly affect the population [4, 5]. Climate change refers to the annual temperature fluctuation around the mean temperature for a particular season of the year [6]. Ischemic stroke risk factors, such as age, gender, genetic factors, and diseases, including hypertension, diabetes, and heart disease, are unlikely to change on a daily basis. Hence, climatic conditions appear to be the main responsible factors for stroke. Weather conditions may increase the risk of stroke by inducing physiological changes. For example, blood pressure, red blood cells, thrombocytes, and blood viscosity increase in cold weather, and plasma fibrinogen concentrations are higher in older patients. Increasing body temperature also increases the level of coagulation factors [7, 8].
Many epidemiological studies disclose an association between high temperature and increased mortality due to cardiovascular, cerebral, and respiratory diseases. Elderly people, children, and people with poor health or underlying conditions are subject to the negative effects of exposure to high temperatures [9, 10]. Several studies support that ambient temperature decline is associated with increased sensitivity to ischemic stroke. However, many other research cases in the United States have not reported any relationship between ambient temperature and any stroke subset of 155 hospitals in 20 countries over 5 years [11].
Although evidence supports the impact of adverse weather conditions on the increased risk of cardiovascular and respiratory diseases, previously reported studies have shown conflicting results in observational studies on the effect of ambient temperature and atmospheric pressure on stroke incidence [12]. Some studies have shown that low temperature is associated with increased ischemic stroke. In contrast, other studies have demonstrated that high temperature is related to an increase in ischemic stroke [13]. However, most studies have been conducted on the impact of climate hazards on the morbidity and mortality of patients due to cerebrovascular accidents in developed countries. Regrettably, no study has been undertaken in developing countries such as Iran. Hence, this study aimed to investigate the relationship between climate variables and the incidence of cerebrovascular events in Rasht City, the capital and the most populous city of Guilan Province in northern Iran.
Materials and Methods
This time-series study was carried out on the Rasht population during 5 years from 2014 to 2019. Independent variables of this study included exposure to cold and hot temperatures, high and low air pressure, and high and low humidity. The incidence rate of cerebrovascular diseases is considered an outcome in this study. Due to the nonlinear relationship between the independent variable (meteorological variable) and the 2 dependent variables (admission of cerebrovascular diseases), we employed a distributive lag nonlinear model (DLNM) to investigate the variables’ relationships.
The data required for this study were collected from two sources:
Meteorological data: These data consisted of daily information on the maximum, minimum, and average temperature in Celsius, daily mean air pressure in hectopascals (hPa), and relative humidity in percentage from the Meteorological Organization of Guilan for the 5-year course from March 21, 2014, to March 20, 2019. This center is located in Rasht airport and has appropriate technical equipment updates to measure and record this data.
Admission data of stroke: Due to the existence of only one specialized and sub-specialized neurology hospital in Rasht, Poursina Hospital, all patients with various cerebrovascular diseases (ischemic stroke, hemorrhagic stroke, and other cerebrovascular diseases) are referred to this center. Patients’ admissions data were obtained from 2014 to 2019 from the health information system (HIS) registered to the international classification of diseases version 9 and 10. After obtaining these data, they were entered into Excel 2019 and R software, version 3.6.3 for analysis.
To determine the effect of hot temperature and to calculate the relative risk of this temperature, the 95th percentile of temperature was compared with that of the 75th percentile. To assess the impact of cold temperature and to calculate the relative risk of this temperature, the first temperature percentile was compared with the 25th percentile. According to a 5-year study in Rasht, the average humidity was 83%, so this number was calculated as a baseline, and the relative risk of increasing and decreasing humidity was compared with this figure. Given the effect of atmospheric pressure on cerebrovascular events of patients and the average atmospheric pressure over 5 years in Rasht (1017 hPa), changes in atmospheric pressure were compared with the average, and relative risk was calculated. Since the impact of metrological variables has lag effects, this study investigated for 21 days.
Results
In this study, 7815 participants were included. Their mean age was 66.87 years, and 50.7% of the participants were male. Their minimum age was 8, and the maximum was 98 years. In this 5-year study period, the average temperature was 17.22°C, with a minimum temperature of -9.2°C and a maximum temperature of 38.7°C. The average atmospheric pressure was 1015.077 hPa, with a minimum of 997 hPa and a maximum of 1041 hPa. Also, the average humidity was 81.75%, minimum 9%, and maximum 209%. The most common reason for hospitalization was related to ICD code I64 (stroke, not specified as hemorrhage or infarction) with 4399 cases.
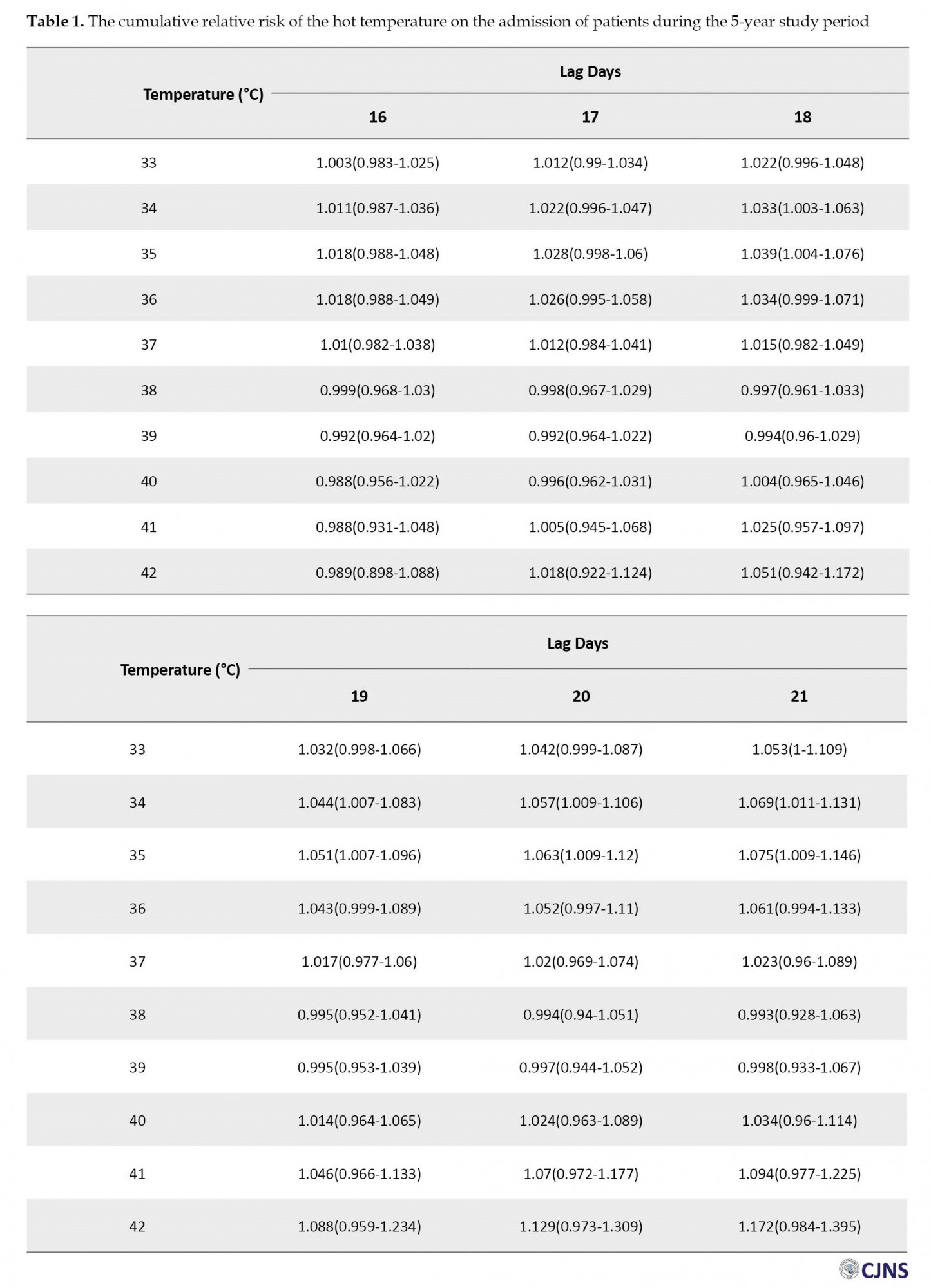
According to the findings, hot temperature (34°C) was significantly associated with an increased risk of stroke admission at lags 18 through 21 days (relative risk [RR]=1.033; 95% confidence interval [CI], 1.003%-1.063%) (RR=1.044; 95% CI, 1.007%-1.083%) (RR=1.057; 95% CI, 1.009%-1.106%) (RR=1.069; 95% CI, 1.011%-1.131%), respectively. In addition, we found positive relationship between hot temperature (35°C) and risk of stroke on 18-21 lag days (RR=1.039; 95% CI, 1.004%-1.076%) (RR=1.051; 95% CI, 1.007%-1.096%) (RR=1.063; 95% CI, 1.009%-1.12%) (RR=1.075; 95% CI, 1.009%-1.146%), as shown in Table 1 and Figure 1.
Cerebrovascular diseases are a group of blood vessel diseases that disrupt blood flow to the brain, primarily affecting the elderly population and often significantly decreasing patients’ quality of life [1]. According to the World Health Organization (WHO), stroke is the second leading cause of death and the most common cause accounting for disability in adults, significantly impacting public health [2, 3]. The quality of life of these patients is often severely affected by readmission, recurrent accidents, depression, fatigue, and other conditions. These conditions often require long-term care [2].
Stroke is a clinical syndrome characterized by an acute neurological disorder triggered by a blood clot obstruction (ischemic stroke) or a blood vessel rupture (hemorrhagic stroke). It depletes the brain’s oxygen and nutrients and consequently causes brain damage. Despite significant advances in early diagnosis and treatment of stroke, its induced deaths are among the greatest challenges in our society [3].
Climate change will be one of the most serious challenges to human health in the 21st century, as it will directly or indirectly affect the population [4, 5]. Climate change refers to the annual temperature fluctuation around the mean temperature for a particular season of the year [6]. Ischemic stroke risk factors, such as age, gender, genetic factors, and diseases, including hypertension, diabetes, and heart disease, are unlikely to change on a daily basis. Hence, climatic conditions appear to be the main responsible factors for stroke. Weather conditions may increase the risk of stroke by inducing physiological changes. For example, blood pressure, red blood cells, thrombocytes, and blood viscosity increase in cold weather, and plasma fibrinogen concentrations are higher in older patients. Increasing body temperature also increases the level of coagulation factors [7, 8].
Many epidemiological studies disclose an association between high temperature and increased mortality due to cardiovascular, cerebral, and respiratory diseases. Elderly people, children, and people with poor health or underlying conditions are subject to the negative effects of exposure to high temperatures [9, 10]. Several studies support that ambient temperature decline is associated with increased sensitivity to ischemic stroke. However, many other research cases in the United States have not reported any relationship between ambient temperature and any stroke subset of 155 hospitals in 20 countries over 5 years [11].
Although evidence supports the impact of adverse weather conditions on the increased risk of cardiovascular and respiratory diseases, previously reported studies have shown conflicting results in observational studies on the effect of ambient temperature and atmospheric pressure on stroke incidence [12]. Some studies have shown that low temperature is associated with increased ischemic stroke. In contrast, other studies have demonstrated that high temperature is related to an increase in ischemic stroke [13]. However, most studies have been conducted on the impact of climate hazards on the morbidity and mortality of patients due to cerebrovascular accidents in developed countries. Regrettably, no study has been undertaken in developing countries such as Iran. Hence, this study aimed to investigate the relationship between climate variables and the incidence of cerebrovascular events in Rasht City, the capital and the most populous city of Guilan Province in northern Iran.
Materials and Methods
This time-series study was carried out on the Rasht population during 5 years from 2014 to 2019. Independent variables of this study included exposure to cold and hot temperatures, high and low air pressure, and high and low humidity. The incidence rate of cerebrovascular diseases is considered an outcome in this study. Due to the nonlinear relationship between the independent variable (meteorological variable) and the 2 dependent variables (admission of cerebrovascular diseases), we employed a distributive lag nonlinear model (DLNM) to investigate the variables’ relationships.
The data required for this study were collected from two sources:
Meteorological data: These data consisted of daily information on the maximum, minimum, and average temperature in Celsius, daily mean air pressure in hectopascals (hPa), and relative humidity in percentage from the Meteorological Organization of Guilan for the 5-year course from March 21, 2014, to March 20, 2019. This center is located in Rasht airport and has appropriate technical equipment updates to measure and record this data.
Admission data of stroke: Due to the existence of only one specialized and sub-specialized neurology hospital in Rasht, Poursina Hospital, all patients with various cerebrovascular diseases (ischemic stroke, hemorrhagic stroke, and other cerebrovascular diseases) are referred to this center. Patients’ admissions data were obtained from 2014 to 2019 from the health information system (HIS) registered to the international classification of diseases version 9 and 10. After obtaining these data, they were entered into Excel 2019 and R software, version 3.6.3 for analysis.
To determine the effect of hot temperature and to calculate the relative risk of this temperature, the 95th percentile of temperature was compared with that of the 75th percentile. To assess the impact of cold temperature and to calculate the relative risk of this temperature, the first temperature percentile was compared with the 25th percentile. According to a 5-year study in Rasht, the average humidity was 83%, so this number was calculated as a baseline, and the relative risk of increasing and decreasing humidity was compared with this figure. Given the effect of atmospheric pressure on cerebrovascular events of patients and the average atmospheric pressure over 5 years in Rasht (1017 hPa), changes in atmospheric pressure were compared with the average, and relative risk was calculated. Since the impact of metrological variables has lag effects, this study investigated for 21 days.
Results
In this study, 7815 participants were included. Their mean age was 66.87 years, and 50.7% of the participants were male. Their minimum age was 8, and the maximum was 98 years. In this 5-year study period, the average temperature was 17.22°C, with a minimum temperature of -9.2°C and a maximum temperature of 38.7°C. The average atmospheric pressure was 1015.077 hPa, with a minimum of 997 hPa and a maximum of 1041 hPa. Also, the average humidity was 81.75%, minimum 9%, and maximum 209%. The most common reason for hospitalization was related to ICD code I64 (stroke, not specified as hemorrhage or infarction) with 4399 cases.
According to the findings, hot temperature (34°C) was significantly associated with an increased risk of stroke admission at lags 18 through 21 days (relative risk [RR]=1.033; 95% confidence interval [CI], 1.003%-1.063%) (RR=1.044; 95% CI, 1.007%-1.083%) (RR=1.057; 95% CI, 1.009%-1.106%) (RR=1.069; 95% CI, 1.011%-1.131%), respectively. In addition, we found positive relationship between hot temperature (35°C) and risk of stroke on 18-21 lag days (RR=1.039; 95% CI, 1.004%-1.076%) (RR=1.051; 95% CI, 1.007%-1.096%) (RR=1.063; 95% CI, 1.009%-1.12%) (RR=1.075; 95% CI, 1.009%-1.146%), as shown in Table 1 and Figure 1.
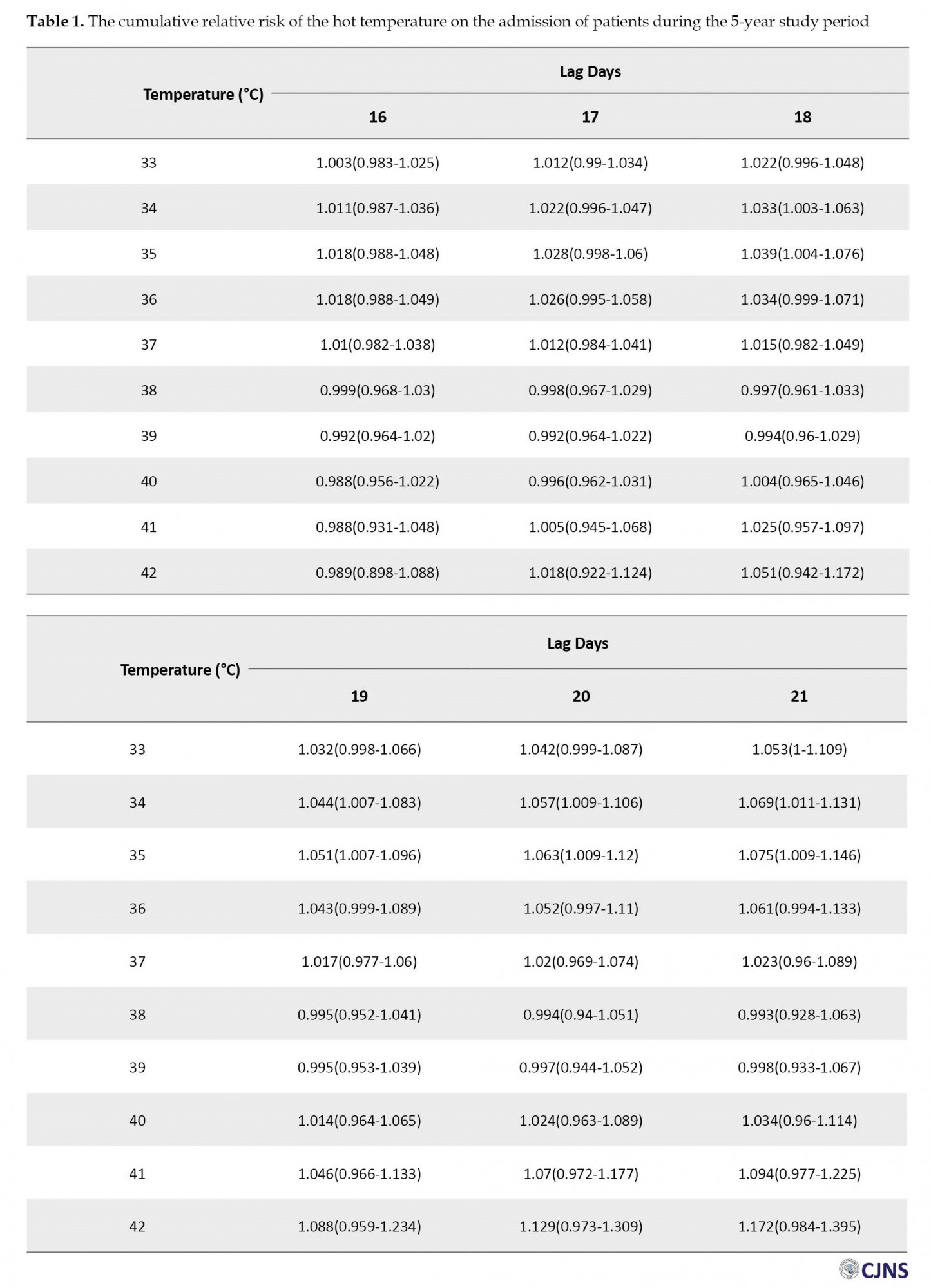
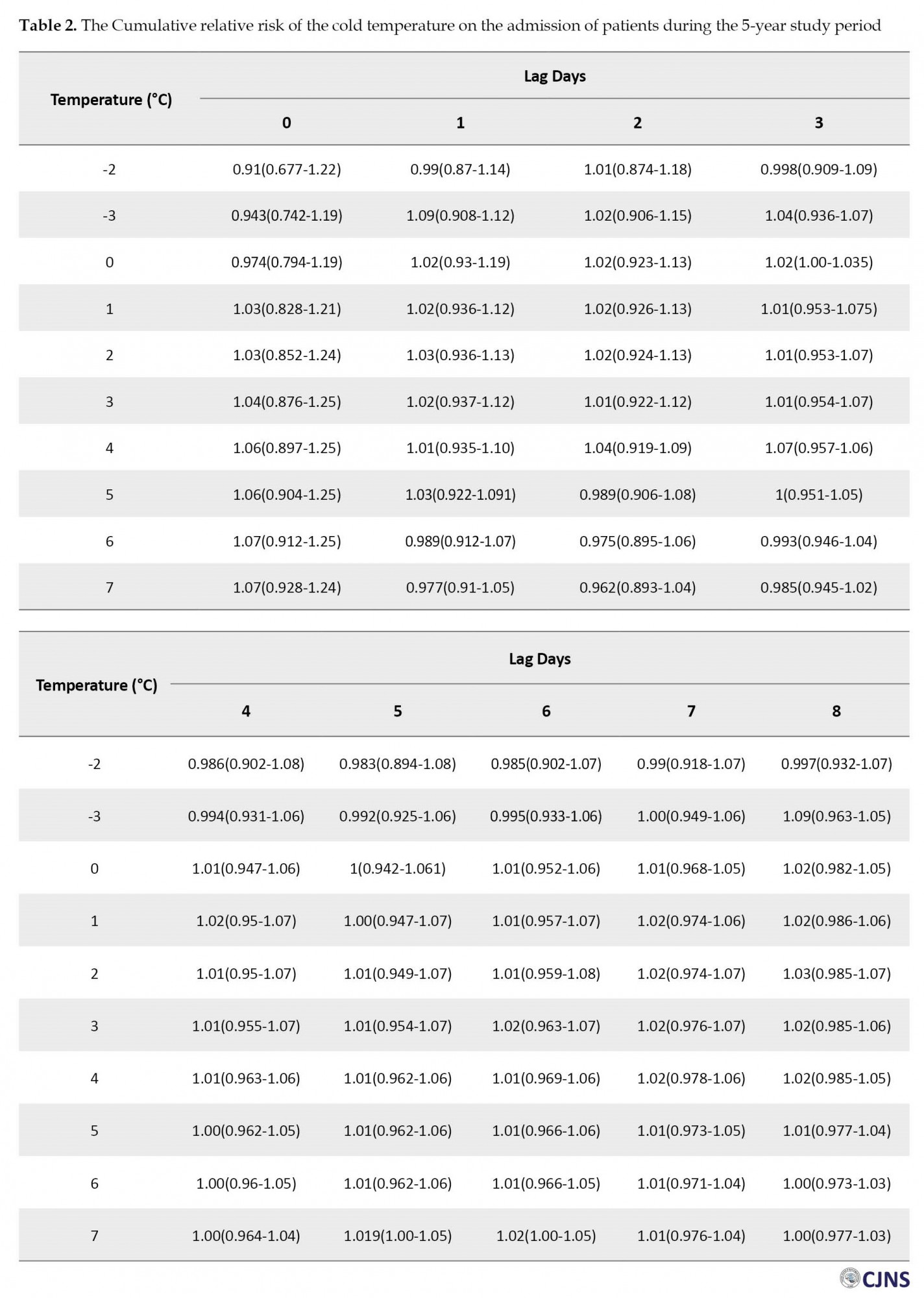
In the general population, severe cold (0°C) was significantly associated with an increased risk of stroke on the third day after exposure (RR=1.017; 95% CI, 1.00%-1.035%). Also, cold temperature (7°C) was significantly associated with the risk of stroke on lag days 5 (RR=1.019; 95% CI, 1.001%-1.051%) and 6 (RR=1.020; 95% CI, 1.002%-1.047%) as presented in Table 2.
Our findings revealed that the risk of hospital stroke admission was not significantly associated with low and high humidity (Table 3).

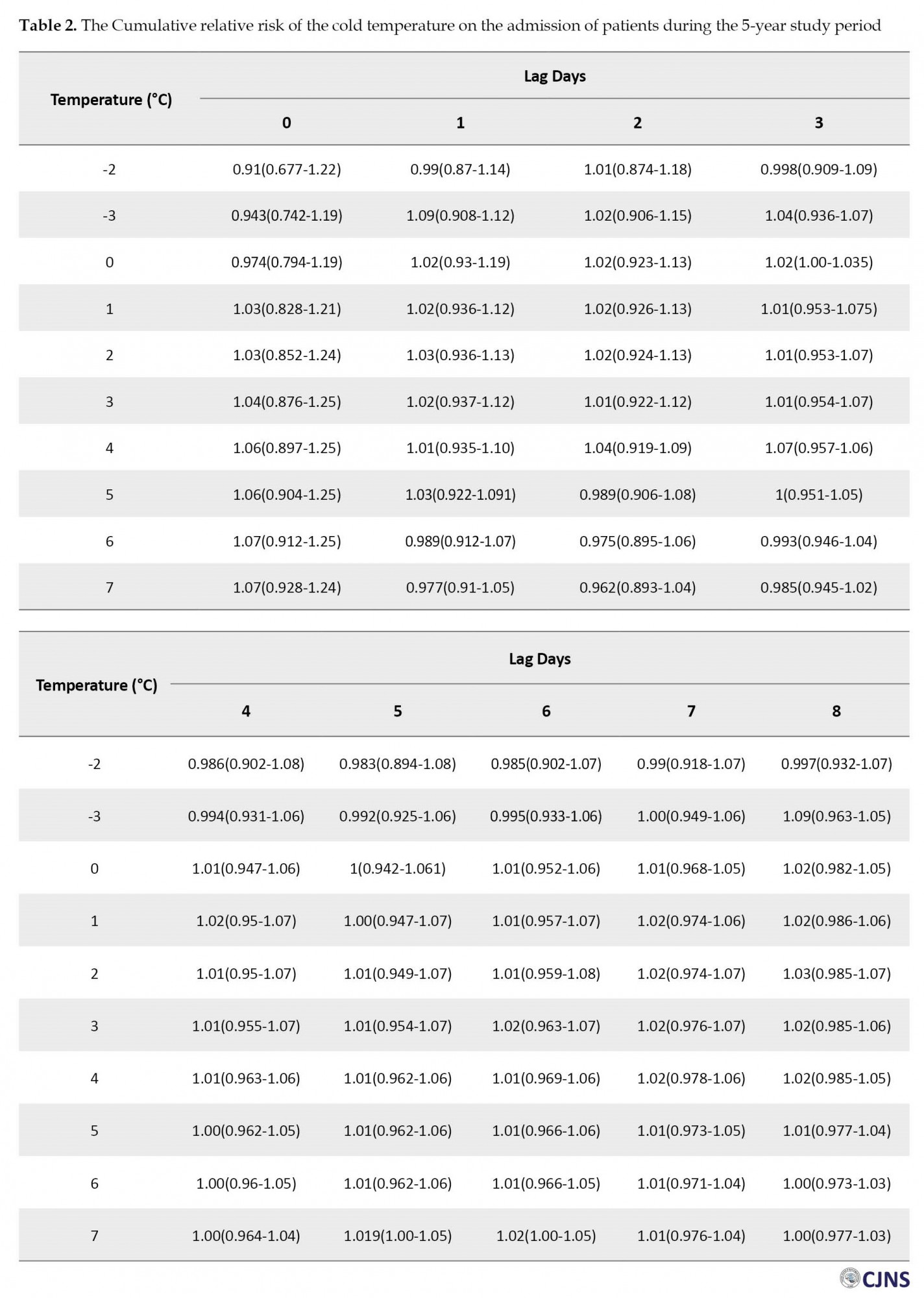
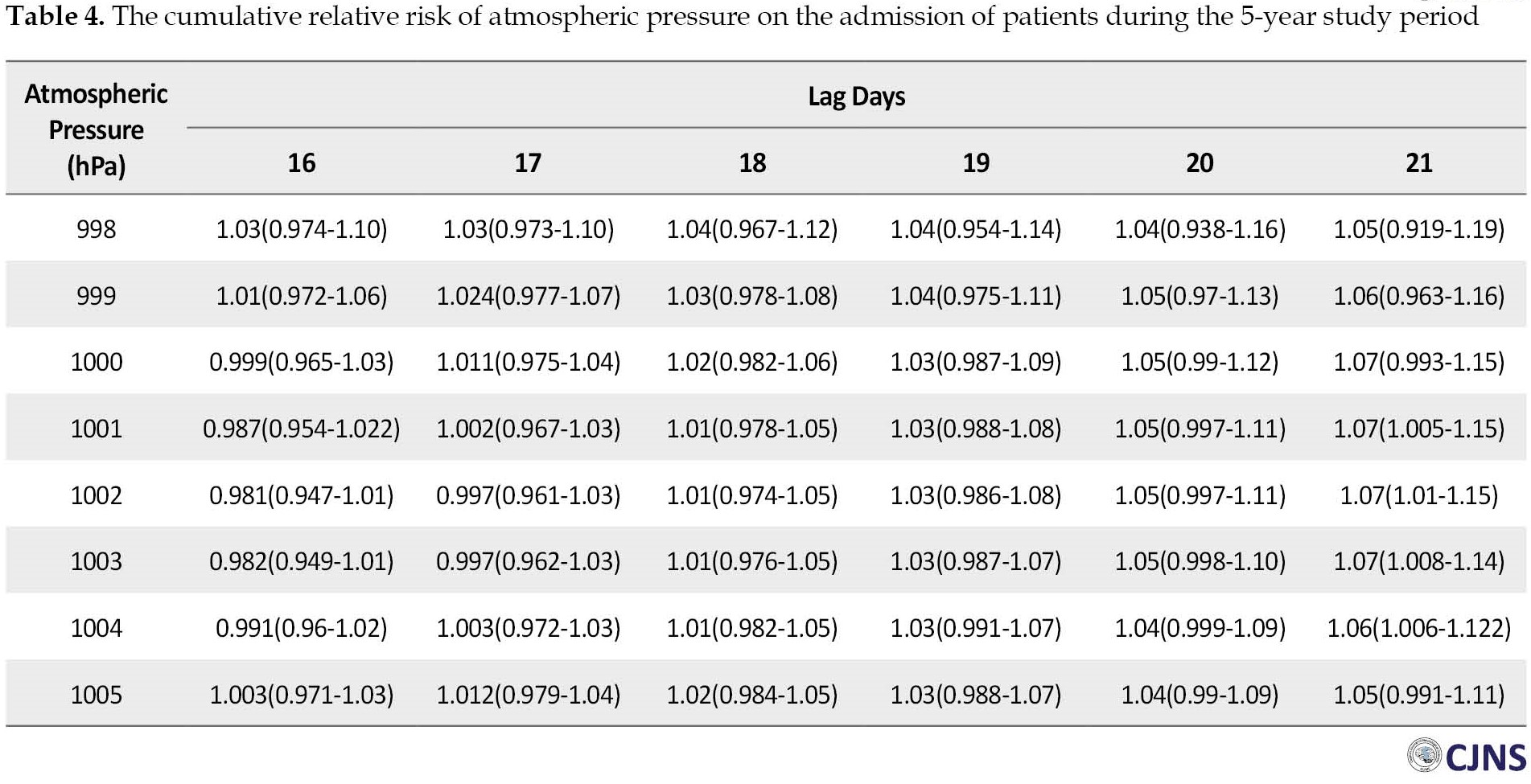
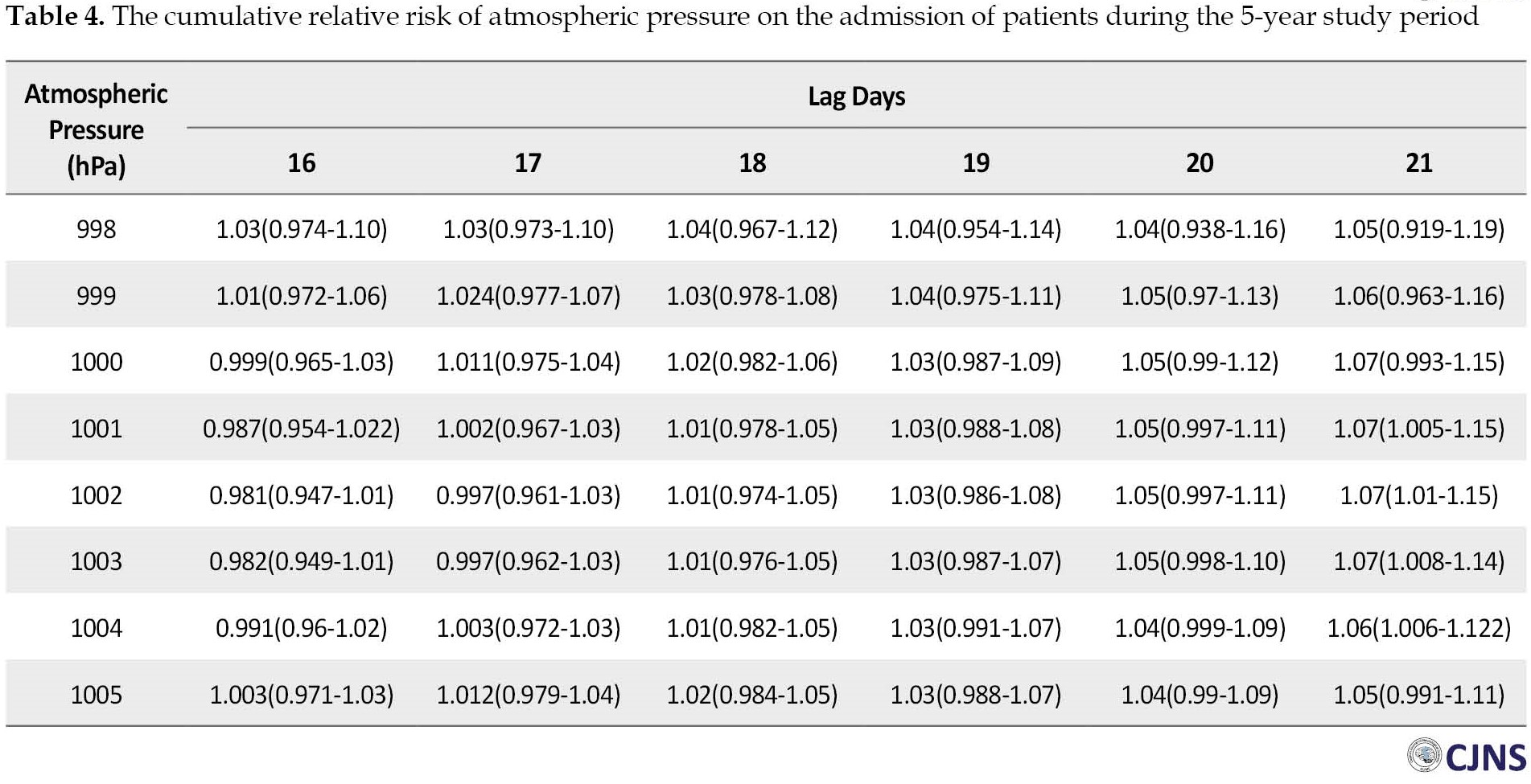
The effect of low atmospheric pressures on stroke admission in lag days 16-21 showed that pressures of 1001, 1002, 1003, and 1004 hPa, 21 days after exposure were associated with the risk of stroke (RR=1.075; 95% CI, 1.005%-1.15%) (RR=1.076; 95% CI, 1.007%-1.15%) (RR=1.072; 95% CI, 1.008%-1.14%) (RR=1.062; 95% CI, 1.006%-1.122%) respectively, as presented in detail in Table 4.
The results indicated that hot temperatures (39°C and 40°C) 16 days after exposure were significantly associated with the risk of cerebral infarction (RR=0.786; 95% CI, 0.636%-0.971%) (RR=0.79; 95% CI, 0.639%-0.976%), respectively. Low humidity (8%, 9%, and 10%) two days after exposure was significantly associated with the risk of intracerebral hemorrhage (I61.9) (RR=5.089; 95% CI, 1.002%-25.835%) (RR=4.841; 95% CI, 1.014%-23.109%) (RR=4.606; 95% CI, 1.025%-20.692%), respectively. In addition, the findings of study showed that the risk of intracranial hemorrhage (I62.9) at low humidity (7%, 8%, 9%, and 10%) one day after exposure were significant (RR=2.708; 95% CI, 1.274%-5.755%), (RR=2.59; 95% CI, 1.254%-5.348%), (RR=2.478; 95% CI, 1.234%-4.974%), (RR=2.37; 95% CI, 1.213%-4.631%), respectively. Also, exposure to humidity (7%, 8%, 9%, and 10%) was significantly associated with an increased risk of cerebral infarction on the fourth lag day (RR=29.473; 95% CI, 3.393%-255.997%) (RR=26.294; 95% CI, 3.279%-210.833%) (RR=23.46; 95% CI, 3.169%-173.696%) (RR=20.936; 95% CI, 3.061%-143.178%), and fifth lag day (RR=34.331; 95% CI, 3.95%-298.4%) (RR=30.553; 95% CI, 3.808%-245.126%) (RR=27.195; 95% CI, 3.671%-201.432%) (RR=24.21; 95% CI, 3.539%-165.616%), respectively.
This study indicated that exposure to low atmospheric pressure on 16-21 lag days was associated with the risk of Intracranial hemorrhage. Specifically, at an atmospheric pressure of 997 hPa, the relative risks of intracranial hemorrhage on 16, 17, 18, 19, 20, and 21 lag days were 1.624 (95% CI, 1.027%-2.569%), 1.72 (95% CI, 1.049%-2.821%),1.835 (95% CI, 1.053%-3.197%), 1.967 (95% CI, 1.039%-3.721%), 2.113 (95% CI, 1.012%-4.41%), respectively, which were significant in all cases. Also, 998 hPa atmospheric pressure on days 16, 17, and 18 after exposure was significantly associated with the risk of Intracranial hemorrhage (RR=1.412; %95 CI, 1.014-1.967) (RR=1.435; 95% CI, 1.021%-2.018%) (RR=1.465; 95% CI, 1.014%-2.118%). Moreover, at 999 hPa, only the 16th day after exposure was significantly associated with the risk of intracranial hemorrhage (RR=1.294; 95% CI, 1.014%-1.651%).
Discussion
This study examined the relationship between metrological variables and the incidence and outcome of cerebrovascular diseases in Rasht citizens, the capital city of Guilan Province in the northern part of Iran, for 5 years, from March 21, 2014, to March 20, 2019. This study indicates that both hot and cold temperatures are associated with an increased risk of stroke. This result is consistent with a few other studies. A study conducted in China by Chen et al. [14] reported that hot or cold weather was associated with an increased risk of stroke mortality. In the study by Guan et al. [15], hot temperature was associated with increased daily stroke hospitalization. Also, Mostofsky et al. [16], Luo et al. [17], and Guo et al. [18]reported that exposure to cold weather was associated with increasing stroke admissions.
The result of this study showed that hot temperature was associated with stroke admission rate. Also, several studies have shown that hot temperature was related to stroke admission or mortality in different countries and cities with varying climate conditions [18].
Our study in Iran found that cold temperature had a significant association with stroke admission, consistent with previous studies conducted in Korea and China [19].Several complex and potential biological mechanisms can explain these findings. For example, cold temperatures can lead to vasoconstriction to divert blood flow to vital central organs, thus increasing blood pressure [20]. High blood pressure is an important risk factor for hemorrhagic stroke. Cold weather increases the brain’s need for oxygen, which, in turn, exacerbates cerebral brain ischemia [21]. In addition, cold environments may trigger several thrombogenic factors, such as elevated blood cell counts, plasma cholesterol, C-reactive protein, fibrinogen concentration, and platelet reactivity [22].
On the other hand, exposure to a hot environment increases vasodilation, heart rate, and sweating. Dehydration on hot days may increase blood viscosity and cholesterol levels, increasing the risk of microvascular thrombosis and subsequent stroke [20]. Eventually, high temperatures cause poor endothelial function [23].
Based on our study, low humidity was not significantly associated with the admission of stroke; however, results showed that low percentage humidity (7% to 10%) was significantly associated with intracranial hemorrhage and cerebral infarction. Unlike the results of our study, some studies have shown that relative humidity can predict admission of stroke [24]. Slatilna et al. found that a rapid increase or decrease in humidity raises the incidence of stroke among Emergency Medical Care Institute patients in Sarajevo who had suffered from a cerebrovascular incident from 2004 to 2006 [25]. A study by Ohshige et al. in Japan from 1982 to 2003 showed an inverse relationship between daily high average humidity and the number of deaths from stroke [26].
In the Santurtún study, a 20% reduction in humidity significantly increased stroke hospital admissions by an average of 5.6% [3]. In contrast, in the Qi et al. study, there was no statistically significant relationship between relative humidity and stroke [27]. Different study results can be due to varying characteristics of various studies, climate and geographical area, type of study design, various statistical methods, and other confounding factors.
In the present study, atmospheric pressure positively correlates with intracerebral hemorrhage (ICH) incidence. This result is in line with a study in Korea that described a correlation between a higher incidence of ICH and higher atmospheric pressure in an older age group [28]. Also, in the Salam et al. study, the risk of ICH and ischemic stroke was at higher atmospheric pressure [29]. Tarnoki et al. found that subarachnoid hemorrhage was associated with the lowest and highest daily air pressure. Changes in air pressure can moderate the occurrence of cerebrovascular events [19].
Decreased atmospheric pressure can be associated with changes in oxygen saturation and ischemic and hemorrhagic stroke [30, 31]. Jimenez-Conde et al. pointed out that low air pressure in air travel can trigger thrombosis [32]. It can be stated that changes in air pressure may directly affect the vessel wall, causing endogenous inflammatory mechanisms and altering endothelial function.
Our study has some limitations. This study was retrospective, so there was a possibility of error in recording information. In addition, the data of this study was confined to a single hospital. The author suggests that future studies be performed with larger sample sizes from other hospitals to better explain the relationship between metrological variables and the occurrence of stroke.
Conclusion
Our study has demonstrated that metrological variables can affect cerebrovascular events. Climate change, such as cold and hot weather, humidity, and atmospheric pressure, emerge as a contributor to stroke incidence. This study concluded that global climate change may increase the incidence of such hazards by creating severe weather conditions. Healthcare providers should focus on implementing preventive measures to reduce these hazards.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. The study protocol was approved by the Ethics Committee of the Guilan University of Medical Science (Code: IR.GUMS.REC.1397.507).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors contributions
Conceptualization: Mohammad Taghi Moghadamnia, Ali Ghanbari, and Mostafa Soodmand; Methodology and data analysis: Mohammad Taghi Moghadamnia, Mostafa Soodmand, and Sara Khoshamuoz; Data collection: Ghazal Saraei, Parisa Mehraeen, and Seyed Ali Majidi; Writing the original draft, editing, and review: Mohammad Taghi Moghadamnia, Mostafa Soodmand, Ali Ghanbari, and Seyed Ali Majidi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully thank the Meteorological Organization of Guilan and Rasht Hospital (specialized and sub-specialized neurology hospital), the two sources for collecting the required data. Additionally, we acknowledge the Guilan University of Medical Sciences for the financial support.
Our findings revealed that the risk of hospital stroke admission was not significantly associated with low and high humidity (Table 3).

The effect of low atmospheric pressures on stroke admission in lag days 16-21 showed that pressures of 1001, 1002, 1003, and 1004 hPa, 21 days after exposure were associated with the risk of stroke (RR=1.075; 95% CI, 1.005%-1.15%) (RR=1.076; 95% CI, 1.007%-1.15%) (RR=1.072; 95% CI, 1.008%-1.14%) (RR=1.062; 95% CI, 1.006%-1.122%) respectively, as presented in detail in Table 4.
The results indicated that hot temperatures (39°C and 40°C) 16 days after exposure were significantly associated with the risk of cerebral infarction (RR=0.786; 95% CI, 0.636%-0.971%) (RR=0.79; 95% CI, 0.639%-0.976%), respectively. Low humidity (8%, 9%, and 10%) two days after exposure was significantly associated with the risk of intracerebral hemorrhage (I61.9) (RR=5.089; 95% CI, 1.002%-25.835%) (RR=4.841; 95% CI, 1.014%-23.109%) (RR=4.606; 95% CI, 1.025%-20.692%), respectively. In addition, the findings of study showed that the risk of intracranial hemorrhage (I62.9) at low humidity (7%, 8%, 9%, and 10%) one day after exposure were significant (RR=2.708; 95% CI, 1.274%-5.755%), (RR=2.59; 95% CI, 1.254%-5.348%), (RR=2.478; 95% CI, 1.234%-4.974%), (RR=2.37; 95% CI, 1.213%-4.631%), respectively. Also, exposure to humidity (7%, 8%, 9%, and 10%) was significantly associated with an increased risk of cerebral infarction on the fourth lag day (RR=29.473; 95% CI, 3.393%-255.997%) (RR=26.294; 95% CI, 3.279%-210.833%) (RR=23.46; 95% CI, 3.169%-173.696%) (RR=20.936; 95% CI, 3.061%-143.178%), and fifth lag day (RR=34.331; 95% CI, 3.95%-298.4%) (RR=30.553; 95% CI, 3.808%-245.126%) (RR=27.195; 95% CI, 3.671%-201.432%) (RR=24.21; 95% CI, 3.539%-165.616%), respectively.
This study indicated that exposure to low atmospheric pressure on 16-21 lag days was associated with the risk of Intracranial hemorrhage. Specifically, at an atmospheric pressure of 997 hPa, the relative risks of intracranial hemorrhage on 16, 17, 18, 19, 20, and 21 lag days were 1.624 (95% CI, 1.027%-2.569%), 1.72 (95% CI, 1.049%-2.821%),1.835 (95% CI, 1.053%-3.197%), 1.967 (95% CI, 1.039%-3.721%), 2.113 (95% CI, 1.012%-4.41%), respectively, which were significant in all cases. Also, 998 hPa atmospheric pressure on days 16, 17, and 18 after exposure was significantly associated with the risk of Intracranial hemorrhage (RR=1.412; %95 CI, 1.014-1.967) (RR=1.435; 95% CI, 1.021%-2.018%) (RR=1.465; 95% CI, 1.014%-2.118%). Moreover, at 999 hPa, only the 16th day after exposure was significantly associated with the risk of intracranial hemorrhage (RR=1.294; 95% CI, 1.014%-1.651%).
Discussion
This study examined the relationship between metrological variables and the incidence and outcome of cerebrovascular diseases in Rasht citizens, the capital city of Guilan Province in the northern part of Iran, for 5 years, from March 21, 2014, to March 20, 2019. This study indicates that both hot and cold temperatures are associated with an increased risk of stroke. This result is consistent with a few other studies. A study conducted in China by Chen et al. [14] reported that hot or cold weather was associated with an increased risk of stroke mortality. In the study by Guan et al. [15], hot temperature was associated with increased daily stroke hospitalization. Also, Mostofsky et al. [16], Luo et al. [17], and Guo et al. [18]reported that exposure to cold weather was associated with increasing stroke admissions.
The result of this study showed that hot temperature was associated with stroke admission rate. Also, several studies have shown that hot temperature was related to stroke admission or mortality in different countries and cities with varying climate conditions [18].
Our study in Iran found that cold temperature had a significant association with stroke admission, consistent with previous studies conducted in Korea and China [19].Several complex and potential biological mechanisms can explain these findings. For example, cold temperatures can lead to vasoconstriction to divert blood flow to vital central organs, thus increasing blood pressure [20]. High blood pressure is an important risk factor for hemorrhagic stroke. Cold weather increases the brain’s need for oxygen, which, in turn, exacerbates cerebral brain ischemia [21]. In addition, cold environments may trigger several thrombogenic factors, such as elevated blood cell counts, plasma cholesterol, C-reactive protein, fibrinogen concentration, and platelet reactivity [22].
On the other hand, exposure to a hot environment increases vasodilation, heart rate, and sweating. Dehydration on hot days may increase blood viscosity and cholesterol levels, increasing the risk of microvascular thrombosis and subsequent stroke [20]. Eventually, high temperatures cause poor endothelial function [23].
Based on our study, low humidity was not significantly associated with the admission of stroke; however, results showed that low percentage humidity (7% to 10%) was significantly associated with intracranial hemorrhage and cerebral infarction. Unlike the results of our study, some studies have shown that relative humidity can predict admission of stroke [24]. Slatilna et al. found that a rapid increase or decrease in humidity raises the incidence of stroke among Emergency Medical Care Institute patients in Sarajevo who had suffered from a cerebrovascular incident from 2004 to 2006 [25]. A study by Ohshige et al. in Japan from 1982 to 2003 showed an inverse relationship between daily high average humidity and the number of deaths from stroke [26].
In the Santurtún study, a 20% reduction in humidity significantly increased stroke hospital admissions by an average of 5.6% [3]. In contrast, in the Qi et al. study, there was no statistically significant relationship between relative humidity and stroke [27]. Different study results can be due to varying characteristics of various studies, climate and geographical area, type of study design, various statistical methods, and other confounding factors.
In the present study, atmospheric pressure positively correlates with intracerebral hemorrhage (ICH) incidence. This result is in line with a study in Korea that described a correlation between a higher incidence of ICH and higher atmospheric pressure in an older age group [28]. Also, in the Salam et al. study, the risk of ICH and ischemic stroke was at higher atmospheric pressure [29]. Tarnoki et al. found that subarachnoid hemorrhage was associated with the lowest and highest daily air pressure. Changes in air pressure can moderate the occurrence of cerebrovascular events [19].
Decreased atmospheric pressure can be associated with changes in oxygen saturation and ischemic and hemorrhagic stroke [30, 31]. Jimenez-Conde et al. pointed out that low air pressure in air travel can trigger thrombosis [32]. It can be stated that changes in air pressure may directly affect the vessel wall, causing endogenous inflammatory mechanisms and altering endothelial function.
Our study has some limitations. This study was retrospective, so there was a possibility of error in recording information. In addition, the data of this study was confined to a single hospital. The author suggests that future studies be performed with larger sample sizes from other hospitals to better explain the relationship between metrological variables and the occurrence of stroke.
Conclusion
Our study has demonstrated that metrological variables can affect cerebrovascular events. Climate change, such as cold and hot weather, humidity, and atmospheric pressure, emerge as a contributor to stroke incidence. This study concluded that global climate change may increase the incidence of such hazards by creating severe weather conditions. Healthcare providers should focus on implementing preventive measures to reduce these hazards.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. The study protocol was approved by the Ethics Committee of the Guilan University of Medical Science (Code: IR.GUMS.REC.1397.507).
Funding
This study was funded by Guilan University of Medical Sciences.
Authors contributions
Conceptualization: Mohammad Taghi Moghadamnia, Ali Ghanbari, and Mostafa Soodmand; Methodology and data analysis: Mohammad Taghi Moghadamnia, Mostafa Soodmand, and Sara Khoshamuoz; Data collection: Ghazal Saraei, Parisa Mehraeen, and Seyed Ali Majidi; Writing the original draft, editing, and review: Mohammad Taghi Moghadamnia, Mostafa Soodmand, Ali Ghanbari, and Seyed Ali Majidi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors gratefully thank the Meteorological Organization of Guilan and Rasht Hospital (specialized and sub-specialized neurology hospital), the two sources for collecting the required data. Additionally, we acknowledge the Guilan University of Medical Sciences for the financial support.
References
- Catalá-López F, Fernández de Larrea-Baz N, Morant-Ginestar C, Álvarez-Martín E, Díaz-Guzmán J, Gènova-Maleras R. The national burden of cerebrovascular diseases in Spain: A population-based study using disability-adjusted life years. Med Clin. 2015; 144(8):353-9. [DOI:10.1016/j.medcli.2013.11.040] [PMID]
- Beck C, Kühlbach B, Ertl M, Naumann M, Straub A, Giemsa E, et al. Stroke occurrence in the Augsburg region (Southern Germany) related to air masses and weather types. Paper presented at: 20th EGU General Assembly, EGU2018, Proceedings from the conference held. 4-13 April, 2018; Vienna, Austria. [Link]
- Santurtún A, Ruiz PB, López-Delgado L, Sanchez-Lorenzo A, Riancho J, Zarrabeitia MT. Stroke: Temporal trends and association with atmospheric variables and air pollutants in Northern Spain. Cardiovasc Toxicol. 2017; 17(3):360-7. [DOI:10.1007/s12012-016-9395-6] [PMID]
- Zhang Y, Li S, Pan X, Tong S, Jaakkola JJ, Gasparrini A, et al. The effects of ambient temperature on cerebrovascular mortality: An epidemiologic study in four climatic zones in China. Environ Health. 2014; 13(1):24.[DOI:10.1186/1476-069X-13-24] [PMID]
- Moghadamnia MT, Ardalan A, Mesdaghinia A, Naddafi K, Yekaninejad MS. The effects of apparent temperature on cardiovascular mortality using a distributed lag nonlinear model analysis: 2005 to 2014. Asia Pac J Public Health. 2018; 30(4):361-8. [PMID]
- Ebi KL, Exuzides KA, Lau E, Kelsh M, Barnston A. Weather changes associated with hospitalizations for cardiovascular diseases and stroke in California, 1983-1998. Int J Biometeorol. 2004; 49(1):48-58. [DOI:10.1007/s00484-004-0207-5]
- Gunes H, Kandis H, Saritas A, Dikici S, Buyukkaya R. The relationship between ischemic stroke and weather conditions in Duzce, Turkey. World J Emerg Med. 2015; 6(3):207-11. [DOI:10.5847/wjem.j.1920-8642.2015.03.008] [PMID]
- Moghadamnia MT, Ardalan A, Mesdaghinia A, Naddafi K, Yekaninejad MS. Association between apparent temperature and acute coronary syndrome admission in Rasht, Iran. Heart Asia. 2018; 10(2):e011068. [DOI:10.1136/heartasia-2018-011068] [PMID]
- Garland RM, Matooane M, Engelbrecht FA, Bopape MJ, Landman WA, Naidoo M, et al. Regional projections of extreme apparent temperature days in Africa and the related potential risk to human health. Int J Environ Res Public Health. 2015; 12(10):12577-604. [DOI:10.3390/ijerph121012577] [PMID]
- Borghei Y, Moghadamnia MT, Sigaroudi AE, Ghanbari A. Association between climate variables (cold and hot weathers, humidity, atmospheric pressures) with out-of-hospital cardiac arrests in Rasht, Iran. J Therm Biol. 2020; 93:102702. [DOI:10.1016/j.jtherbio.2020.102702] [PMID]
- Çevik Y, Doğan NÖ, Daş M, Ahmedali A, Kul S, Bayram H. The association between weather conditions and stroke admissions in Turkey. Int J Biometeorol. 2015; 59(7):899-905. [DOI:10.1007/s00484-014-0890-9] [PMID]
- Hong YC, Rha JH, Lee JT, Ha EH, Kwon HJ, Kim H. Ischemic stroke associated with decrease in temperature. Epidemiology. 2003; 14(4):473-8. [DOI:10.1097/01.ede.0000078420.82023.e3] [PMID]
- Sueda Y, Hosomi N, Tsunematsu M, Takamatsu K, Nomura E, Torii T, et al. Effects of meteorological conditions on the risk of ischemic stroke events in patients treated with Alteplase-HEWS-tPA. J Stroke Cerebrovasc Dis. 2015; 24(7):1500-5. [DOI:10.1016/j.jstrokecerebrovasdis.2015.03.013] [PMID]
- Chen R, Wang C, Meng X, Chen H, Thach TQ, Wong CM, et al. Both low and high temperature may increase the risk of stroke mortality. Neurology. 2013; 81(12):1064-70. [DOI:10.1212/WNL.0b013e3182a4a43c] [PMID]
- Guan W, Clay SJ, Sloan GJ, Pretlow LG. Effects of barometric pressure and temperature on acute ischemic stroke hospitalization in Augusta, GA.Transl Stroke Res. 2019; 10(3):259-64. [DOI:10.1007/s12975-018-0640-0] [PMID]
- Mostofsky E, Wilker EH, Schwartz J, Zanobetti A, Gold DR, Wellenius GA, et al. Short-term changes in ambient temperature and risk of ischemic stroke. Cerebrovasc Dis Extra. 2014; 4(1):9-18. [DOI:10.1159/000357352] [PMID]
- Luo Y, Li H, Huang F, Van Halm-Lutterodt N, Xu Q, Wang A, et al. The cold effect of ambient temperature on ischemic and hemorrhagic stroke hospital admissions: A large database study in Beijing, China between years 2013 and 2014-Utilizing a distributed lag nonlinear analysis. Environ Pollut. 2018; 232:90-6. [DOI:10.1016/j.envpol.2017.09.021] [PMID]
- Guo P, Zheng M, Wang Y, Feng W, Wu J, Deng C, et al. Effects of ambient temperature on stroke hospital admissions: Results from a time-series analysis of 104,432 strokes in Guangzhou, China. Sci Total Environ. 2017; 580:307-15. [DOI:10.1016/j.scitotenv.2016.11.093] [PMID]
- Tarnoki AD, Turker A, Tarnoki DL, Iyisoy MS, Szilagyi BK, Duong H, et al. Relationship between weather conditions and admissions for ischemic stroke and subarachnoid hemorrhage. Croat Med J. 2017; 58(1):56-62. [DOI:10.3325/cmj.2017.58.56] [PMID]
- McArthur K, Dawson J, Walters M. What is it with the weather and stroke? Expert Rev Neurother. 2010; 10(2):243-9.[DOI:10.1586/ern.09.154] [PMID]
- Croughwell N, Smith L, Quill T, Newman M, Greeley W, Kern F, et al. The effect of temperature on cerebral metabolism and blood flow in adults during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1992; 103(3):549-54. [PMID]
- Wolf K, Schneider A, Breitner S, von Klot S, Meisinger C, Cyrys J, et al. Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation. 2009; 120(9):735-42. [DOI:10.1161/CIRCULATIONAHA.108.815860] [PMID]
- Nawrot TS, Staessen JA, Fagard RH, Van Bortel LM, Struijker-Boudier HA. Endothelial function and outdoor temperature. Eur J Epidemiol. 2005; 20(5):407-10. [DOI:10.1007/s10654-005-1068-x] [PMID]
- Tian Y, Liu H, Si Y, Cao Y, Song J, Li M, et al. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: A national time-series study. PLoS Med. 2019; 16(1):e1002738. [DOI:10.1371/journal.pmed.1002738] [PMID]
- Slatina E, Music M, Babic N, Dervisevic A, Mujaric E, Salibasic M, et al. Correlation between change in air humidity and the incidence of stroke. Mater Sociomed. 2013; 25(4):242-5. [DOI:10.5455/msm.2013.25.242-245] [PMID]
- Ohshige K, Hori Y, Tochikubo O, Sugiyama M. Influence of weather on emergency transport events coded as stroke: Population-based study in Japan. Int J Biometeorol. 2006; 50(5):305-11. [DOI:10.1007/s00484-005-0018-3] [PMID]
- Qi X, Wang Z, Xia X, Xue J, Gu Y, Han S, et al. Potential impacts of meteorological variables on acute ischemic stroke onset. Risk Manag Healthc Policy. 2020; 13:615-21. [DOI:10.2147/RMHP.S253559] [PMID]
- Han MH, Yi HJ, Kim YS, Kim YS. Effect of seasonal and monthly variation in weather and air pollution factors on stroke incidence in Seoul, Korea. Stroke. 2015; 46(4):927-35. [DOI:10.1161/STROKEAHA.114.007950] [PMID]
- Salam A, Kamran S, Bibi R, Korashy HM, Parray A, Mannai AA, et al. Meteorological factors and seasonal stroke rates: A four-year comprehensive study. J Stroke Cerebrovasc Dis. 2019; 28(8):2324-31. [DOI:10.1016/j.jstrokecerebrovasdis.2019.05.032] [PMID]
- Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke. 2011; 42(3):593-600. [DOI:10.1161/STROKEAHA.110.602037] [PMID]
- Dawson J, Weir C, Wright F, Bryden C, Aslanyan S, Lees K, et al. Associations between meteorological variables and acute stroke hospital admissions in the west of Scotland. Acta Neurol Scand. 2008; 117(2):85-9. [DOI:10.1111/j.1600-0404.2007.00916.x]] [PMID
- Jimenez-Conde J, Ois A, Gomis M, Rodriguez-Campello A, Cuadrado-Godia E, Subirana I, et al. Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis. 2008; 26(4):348-54. [DOI:10.1159/000151637] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/10/11 | Accepted: 2023/10/17 | Published: 2023/10/17
Received: 2023/10/11 | Accepted: 2023/10/17 | Published: 2023/10/17
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




