Sat, May 18, 2024
Volume 9, Issue 4 (Autumn 2023)
Caspian J Neurol Sci 2023, 9(4): 252-258 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hashemi A, Saeedi N, Seyedhosseinzade N, Bayat S, Homam S M. Psychological Distress Among Iranian Patients With Epilepsy During COVID-19 Pandemic. Caspian J Neurol Sci 2023; 9 (4) :252-258
URL: http://cjns.gums.ac.ir/article-1-667-en.html
URL: http://cjns.gums.ac.ir/article-1-667-en.html
1- Student Research Committee, Islamic Azad University of Mashhad, Mashhad, Iran
2- Department of Neurology, School Medicine, Tehran University of Medical Sciences, Tehran, Iran
3- Department of Neurology, Faculty of Medicine, Islamic Azad University of Mashhad, Mashhad, Iran
2- Department of Neurology, School Medicine, Tehran University of Medical Sciences, Tehran, Iran
3- Department of Neurology, Faculty of Medicine, Islamic Azad University of Mashhad, Mashhad, Iran
Full-Text [PDF 1140 kb]
(96 Downloads)
| Abstract (HTML) (503 Views)
Full-Text: (65 Views)
Introduction
Epilepsy is a frequent neurologic disorder and it has been estimated that approximately 50 millions of people suffer from its worldwide [1]. More than one quarter of the patients with epilepsy (PWE) have a concurrent mental disorder [2]. It is shown that mental comorbidities are associated with decreased quality of life, increased health care services costs, reduced medication compliance, and worsened side effects of antiepileptic drugs (AEDs) [3, 4, 5]. Early detection of mental illness in PWE, improves disease management and prognosis [6]. The most frequent psychiatric diagnoses in PWE include mood, anxiety, and psychotic disorders. Depression is the top psychological illness among epilepsy patients with lifespan prevalence of 20 to 60%, which is evidently higher than the general population with the lifetime prevalence of 16%–20%. Anxiety disorders are the second most common psychiatric disorder among PWE population with prevalence rates range from 11 to 40% [7, 8].
Coronavirus disease 2019 (COVID-19) originated from the Wuhan City, China. However, its rapid spread to several countries received the world-wide attention [9]. On 30th January 2020, the World Health Organization (WHO) declared that COVID-19 outbreak is a public health emergency of international concern [10]. The absence of an effective treatment and the high contagious potency of the virus have caused significant anxiety. The current situation is similar to the previous health problem emergencies, including global severe acute respiratory syndrome (SARS) outbreak in 2013 and the Fukushima Daiichi nuclear power plant disaster in 2011. Based on an assessment performed by the WHO, these events threaten the mental health [11]. This crisis forced the governments to initiate their extremely strict preventive strategies such as quarantine, mandatory school closure, and suspension of non-essential industries and commercial activities. These restrictions have interrupted the daily life and is associated with feelings such as loneliness, anxiety, and boredom. Another problem is the flood of disaster-related news that usually create panic and anxiety in public but scientifically framed information can help people to have a better insight [12]. On the other hand, during the COVID-19 pandemic, PWE have faced with delayed outpatient visits, cancellation of their para-clinic tests, and problems in accessing to emergencies. Overall, the contribution of these factors may result in the development of a psychological distress in a vulnerable population like PWE. COVID-19 outbreak has been reported as a psychological distressing event causing negative side effects on general population as well as patients with neurological disease such as epilepsy. To our knowledge, there are a few numbers of studies which have recently explored the development of outbreak-related distress. These studies have been performed among East Asian population [13, 14, 15]. Therefore, the present study was aimed to compare the psychological distress between the PWE and the healthy control group during the COVID-19 outbreak in Mashhad, Iran to find patients who are at greater risk of developing psychiatric diseases and to provide adequate care and support for them. We also explored the risk factors for severe psychological distress among PWE. Therefore, it was hypothesized might be demographic characteristics, epilepsy related-information and the amount of attention paid to the media coverage of COVID-19 pandemic.
Materials and Methods
This is a case-control study and was performed from January 15 to March 15, 2022. We included the patients who consecutively referred to the Neurology Clinic of 22 Bahman Hospital of Mashhad, Iran and asked them about their psychological distress while they were affected by COVID-19. Accidental method was used for sampling.
Participants
To be eligible to enter to our study, patients had to: a) Be 15 years or older by March 15, and b) Have a definite diagnosis of epilepsy for at least one year before. The exclusion criteria also included: 1) Having psychogenic nonepileptic seizures, 2) Having a seizure within 48 hours before filling the questionnaire, 3) Having a history of mental retardation, alcohol or substance abuse, any history of psychosis, mania, severe depression and any history psychiatric disease, 4) Changing the dosage or type of their AEDs during 1 month prior to completing the questionnaire. This case-control study was a pilot study aimed to screen anxiety disorders in PWE. The sample size was calculated according to the number of PWE referring to 22 Bahman Outpatient Clinics. Also, we invited a number of patients companion with no remarkable past medical history, who referred to the 22 Bahman Hospital, as the control group. Noteworthy, those persons who had a psychological trauma, history of any psychiatric disease, neurologic disorder, and seizure were excluded. The control group were completely matched to case group regarding to their age and gender.
Before enrolling the patients, their electronic health records were examined carefully. Then the inclusion and exclusion criteria were checked according to the patient’s history and their recorded information. After the examination of the health records, an interview by a physician was performed with the patients whose condition was compatible with our criteria. We examined their psychiatric and mental status and also checked the epilepsy-related information. The aim and the process of the study were clearly explained to the patients. The patients who were willing to participate in the study, signed the informed consent.
Survey instruments
After the aim and method of the study was explained to participants, they were asked to sign the informed consent form. In order to send the online questionnaires of the study, the patients who signed the informed consent were asked to write down their phone numbers on the form. Online questionnaires were sent to the included patients and healthy persons through WhatsApp and they were asked to fulfill them.
Questionnaire on demographic and clinical data
This questionnaire was designed and customized for this study in order to collect demographic information such as age, gender, economic level, and marital status. Epilepsy related-information were also asked from the PWE that were as follow: Type of epilepsy, disease duration, the number of AED types, having drug resistance, and the number of seizures before and after COVID-19 infection.
The 6-item Kessler psychological distress scale
The 6-item Kessler psychological distress scale (K-6) was firstly developed by professors Ron Kessler and Dan Mroczek, as a brief dimensional measurement of non-specific psychological distress in the anxiety and depressive disorders [16, 17]. This questionnaire is the short form of K-10 questionnaire and is consisted of 6 questions scoring from 1 (none of the time) to 5 (all of the time). Finally, the scores of the 6 questions are summed and yield a minimum score 6 and maximum score of 30. Lower scores show lower levels of psychological distress and higher scores indicate higher levels psychological distress. The Persian version of Kessler questionnaire was used in this study. The Cronbach’s α reliability coefficient was reported as 0.885 by Dadfar et al. They also assessed construct validity through exploratory factor analysis. Accordingly, principal component analysis as well as a varimax rotation and kaiser normalization were used. They found one factor with eigen values 3.875 and percent of variance 64.577 were labeled as psychological distress [18]. The current study was aimed to screen psychological distress, as a predictor of anxiety and mood disorders. Beside this, regarding time shortage and high number of participants, the short form of the Kessler questionnaire was utilized.
Statistical analysis
Statistical analysis was performed by using SPSS software, version 26. We reported categorical variables as numbers and percentages; and continuous variables as Means±SD. Intergroup differences were compromised through using Pearson correlation and chi-squared tests. Multivariate logistic regression was utilized to explore factors that were independently associated with severe psychological distress in PWE. The multivariate model contained variables that were associated with P<0.05 in univariate analysis.
Results
Of the 159 PWE that were invited to participate in our study, 13(8%) were excluded because of their age (<15 years), 8(5%) because they refused to participate, and 6(3%) because of changes in their AEDs or its dosage within the previous month. Finally, a total of 132 PWE were enrolled and together with the same number of healthy individuals as the control group. More than half of the patients (56%) had generalized epilepsy, whereas 43% had focal epilepsy. Epilepsy was drug-resistant in 85(65%) patients. No significant difference was found in in marriage status and education level. However, patients reported significantly lower monthly income than controls. PWE reported significantly greater concern about the pandemic than the control group, and they spent significantly more hours per day following media reports of the COVID-19 outbreak (Table 1).

We found PWE had significantly higher K-6 scores than the controls. K-6 score higher than 12 was defined as severe psychological distress and we observed a that the proportion of persons who had K-6 score >12 was significantly higher in PWE (Table 2).

By using ANCOVA test, we found that level of concern about COVID-19 outbreak and time spent following media reports of the COVID-19 outbreak showed significant association with severe psychological distress (Table 3).

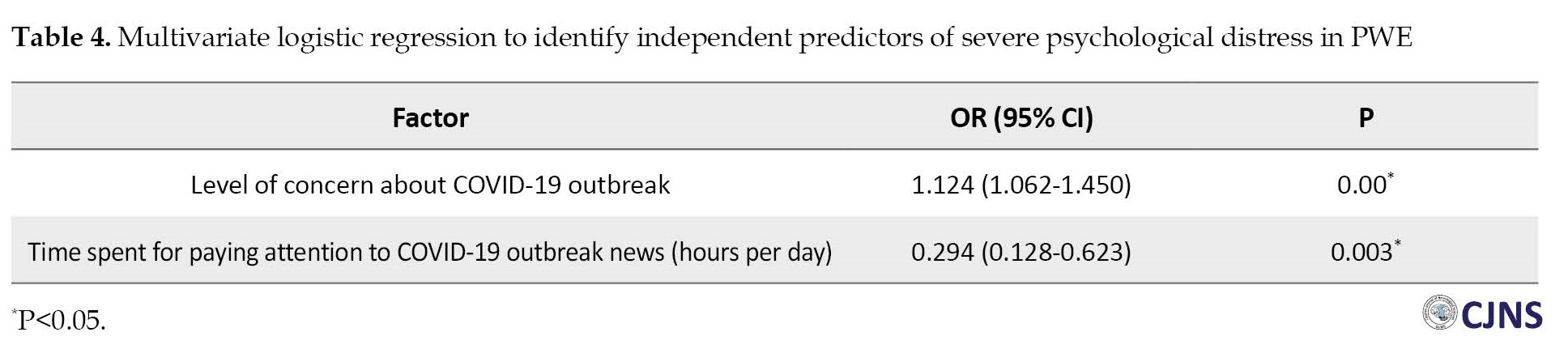
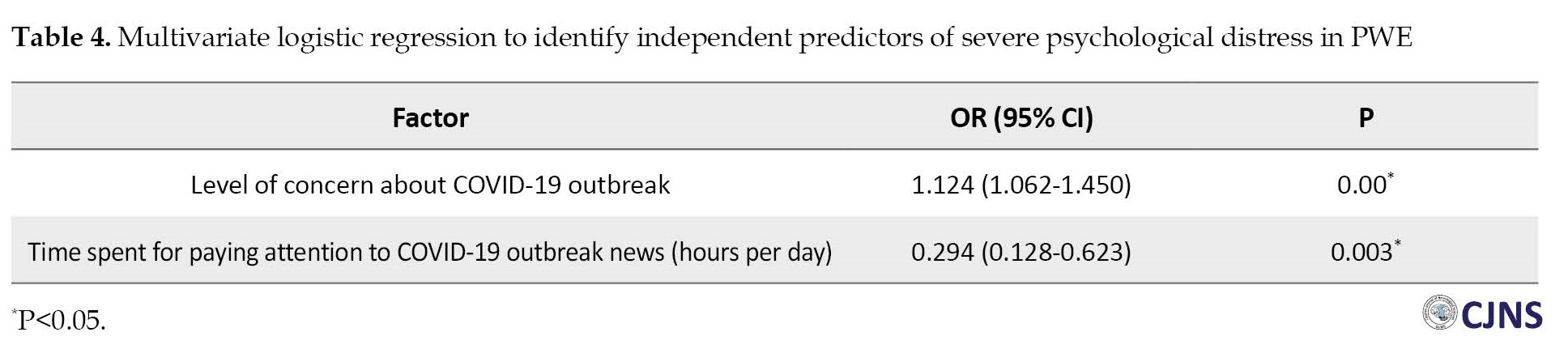
Because the level of concern about COVID-19 outbreak and the time spent for paying attention to COVID-19 outbreak news showed significant association with psychologic distress in univariate analysis, we performed logistic regression to explore whether they are independent predictors of psychologic distress. Results of logistic regression revealed that psychological distress was significantly associated with the amount of concern about COVID-19 outbreak (OR 1.124, 95% CI, 1.062%-1.450%) and the time spent for paying attention to COVID-19 outbreak news (OR 0.294, 95% CI, 0.128%-0.623%) adjusted for age, gender, and marital status (Table 4).
Discussion
Th present study describes the mental health status of PWE in northeast of Iran during the COVID-19 outbreak, and compares it with the mental health status of healthy controls from the same region, as well as exploring risk factors for severe psychological distress. Our survey was performed during the 6th major wave of COVID-19 pandemic which was associated the most severe phase of governmental restrictions on mobility, work, and public services. Following excluding psychotic PWE, we found that psychological distress had significantly higher levels among PWE than controls. Our findings showed that the proportion of patients with severe psychological distress (K-6 score >12) was significantly higher among PWE. More than 9% of our control group reported severe psychological distress which may be in consistent with the 9% prevalence of mental health problems reported for healthy individuals in Iran in the absence of an international pandemic [19].
Our results demonstrated that the amount of time on the COVID-19-related spent daily news and level of concern about COVID-19 outbreak are associated with severe psychological distress among PWE. A systematic review on 16 studies, revealed consistent results with our study. They reported that although PWE and the normal people both experienced psychological distress during COVID-19 pandemic, the degree of depression, anxiety and sleep disorders was significantly more severe in PWE [20]. In another similar study, Giordano et al. evaluated psychological distress among PWE during COVID-19 pandemic. They evaluated the patients during the pre- and post-lockdown period and compared the results. Based on their results, anxiety symptoms were significantly increased following the lockdown period [21]. Sanchez-Larsen and colleagues examined the effect of COVID-19 pandemic on PWE referred to the Outpatient Clinics. They found a significant increase in depression and anxiety level [22]. In line with this, Assenza and colleagues assessed psychological distress in PWE through measuring depression and anxiety levels and sleep quality. They claimed that PWE suffered from worsened depressive and anxiety symptoms and lowered sleep quality during COVID-19 pandemic [23]. In the present study, the number of participants who had K-6 score higher than 12 was significantly higher among PWE, comparing to control group, supporting pervious findings suggesting that PWE are more prone for psychologic diseases [3, 24, 25]. Beside this, the psychological distress level of our patients was similar with the study performed in Japan during Fukushima Daiichi nuclear power plant accident [26]. Comparing psychological distress of PWE during COVID-19 pandemic and Fukushima Daiichi nuclear accident, suggest that PWE are more prone to experience high amounts of stress and they need special care which should be provided by health care professionals including neurologists and psychiatrists.
Conclusion
During public health emergencies, health care professionals should focus not only on seizure control but also on the mental health status of PWE, particularly those with higher number of seizures. They should advise PWE not to pay too much time on the media coverage of the COVID-19 outbreak, and distract themselves with other activities like their hobbies. Patients with K-6 scores >12 should be regarded as experiencing severe psychological distress and a psychiatrist consultation is highly recommended.
Limitations
Our study has several limitations: First, we limited our study sample to the patients who had certain conditions such as having registered information at the Neurology Clinic of 22 Bahman Hospital or being able to use electronic devices. These patients do not represent the general population. Second, another bias is the information bias which is because of the nature of self-reporting. Third, the diagnosis of psychologic distress was only based on a questionnaire in the absence of a structured interview. Fourth, we assessed psychologic distress in PWE during COVID-19 pandemic but we did not evaluate the level of anxiety or depression in these patients.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. The study protocol was approved by the Ethics Committee of Mashhad Medical Science Branch of Islamic Azad University (IR.IAU.MSHD.REC.1400.104).
Funding
This article extracted from MD thesis of Anahita Hashemi, approved by Department of Medicine, Mashhad Branch, Islamic Azad University.
Authors contributions
Conceptualization, methodology, supervision, and funding acquisition: Seyed Mehran Homam; Investigation and analysis: Anahita Hashemi and Negin Seyedhosseinzade; Writing original draft, review & editing: Nikoo Saeedi and Saeid Bayat.
Conflict of interest
The authors declared no conflict of interest.
References
Epilepsy is a frequent neurologic disorder and it has been estimated that approximately 50 millions of people suffer from its worldwide [1]. More than one quarter of the patients with epilepsy (PWE) have a concurrent mental disorder [2]. It is shown that mental comorbidities are associated with decreased quality of life, increased health care services costs, reduced medication compliance, and worsened side effects of antiepileptic drugs (AEDs) [3, 4, 5]. Early detection of mental illness in PWE, improves disease management and prognosis [6]. The most frequent psychiatric diagnoses in PWE include mood, anxiety, and psychotic disorders. Depression is the top psychological illness among epilepsy patients with lifespan prevalence of 20 to 60%, which is evidently higher than the general population with the lifetime prevalence of 16%–20%. Anxiety disorders are the second most common psychiatric disorder among PWE population with prevalence rates range from 11 to 40% [7, 8].
Coronavirus disease 2019 (COVID-19) originated from the Wuhan City, China. However, its rapid spread to several countries received the world-wide attention [9]. On 30th January 2020, the World Health Organization (WHO) declared that COVID-19 outbreak is a public health emergency of international concern [10]. The absence of an effective treatment and the high contagious potency of the virus have caused significant anxiety. The current situation is similar to the previous health problem emergencies, including global severe acute respiratory syndrome (SARS) outbreak in 2013 and the Fukushima Daiichi nuclear power plant disaster in 2011. Based on an assessment performed by the WHO, these events threaten the mental health [11]. This crisis forced the governments to initiate their extremely strict preventive strategies such as quarantine, mandatory school closure, and suspension of non-essential industries and commercial activities. These restrictions have interrupted the daily life and is associated with feelings such as loneliness, anxiety, and boredom. Another problem is the flood of disaster-related news that usually create panic and anxiety in public but scientifically framed information can help people to have a better insight [12]. On the other hand, during the COVID-19 pandemic, PWE have faced with delayed outpatient visits, cancellation of their para-clinic tests, and problems in accessing to emergencies. Overall, the contribution of these factors may result in the development of a psychological distress in a vulnerable population like PWE. COVID-19 outbreak has been reported as a psychological distressing event causing negative side effects on general population as well as patients with neurological disease such as epilepsy. To our knowledge, there are a few numbers of studies which have recently explored the development of outbreak-related distress. These studies have been performed among East Asian population [13, 14, 15]. Therefore, the present study was aimed to compare the psychological distress between the PWE and the healthy control group during the COVID-19 outbreak in Mashhad, Iran to find patients who are at greater risk of developing psychiatric diseases and to provide adequate care and support for them. We also explored the risk factors for severe psychological distress among PWE. Therefore, it was hypothesized might be demographic characteristics, epilepsy related-information and the amount of attention paid to the media coverage of COVID-19 pandemic.
Materials and Methods
This is a case-control study and was performed from January 15 to March 15, 2022. We included the patients who consecutively referred to the Neurology Clinic of 22 Bahman Hospital of Mashhad, Iran and asked them about their psychological distress while they were affected by COVID-19. Accidental method was used for sampling.
Participants
To be eligible to enter to our study, patients had to: a) Be 15 years or older by March 15, and b) Have a definite diagnosis of epilepsy for at least one year before. The exclusion criteria also included: 1) Having psychogenic nonepileptic seizures, 2) Having a seizure within 48 hours before filling the questionnaire, 3) Having a history of mental retardation, alcohol or substance abuse, any history of psychosis, mania, severe depression and any history psychiatric disease, 4) Changing the dosage or type of their AEDs during 1 month prior to completing the questionnaire. This case-control study was a pilot study aimed to screen anxiety disorders in PWE. The sample size was calculated according to the number of PWE referring to 22 Bahman Outpatient Clinics. Also, we invited a number of patients companion with no remarkable past medical history, who referred to the 22 Bahman Hospital, as the control group. Noteworthy, those persons who had a psychological trauma, history of any psychiatric disease, neurologic disorder, and seizure were excluded. The control group were completely matched to case group regarding to their age and gender.
Before enrolling the patients, their electronic health records were examined carefully. Then the inclusion and exclusion criteria were checked according to the patient’s history and their recorded information. After the examination of the health records, an interview by a physician was performed with the patients whose condition was compatible with our criteria. We examined their psychiatric and mental status and also checked the epilepsy-related information. The aim and the process of the study were clearly explained to the patients. The patients who were willing to participate in the study, signed the informed consent.
Survey instruments
After the aim and method of the study was explained to participants, they were asked to sign the informed consent form. In order to send the online questionnaires of the study, the patients who signed the informed consent were asked to write down their phone numbers on the form. Online questionnaires were sent to the included patients and healthy persons through WhatsApp and they were asked to fulfill them.
Questionnaire on demographic and clinical data
This questionnaire was designed and customized for this study in order to collect demographic information such as age, gender, economic level, and marital status. Epilepsy related-information were also asked from the PWE that were as follow: Type of epilepsy, disease duration, the number of AED types, having drug resistance, and the number of seizures before and after COVID-19 infection.
The 6-item Kessler psychological distress scale
The 6-item Kessler psychological distress scale (K-6) was firstly developed by professors Ron Kessler and Dan Mroczek, as a brief dimensional measurement of non-specific psychological distress in the anxiety and depressive disorders [16, 17]. This questionnaire is the short form of K-10 questionnaire and is consisted of 6 questions scoring from 1 (none of the time) to 5 (all of the time). Finally, the scores of the 6 questions are summed and yield a minimum score 6 and maximum score of 30. Lower scores show lower levels of psychological distress and higher scores indicate higher levels psychological distress. The Persian version of Kessler questionnaire was used in this study. The Cronbach’s α reliability coefficient was reported as 0.885 by Dadfar et al. They also assessed construct validity through exploratory factor analysis. Accordingly, principal component analysis as well as a varimax rotation and kaiser normalization were used. They found one factor with eigen values 3.875 and percent of variance 64.577 were labeled as psychological distress [18]. The current study was aimed to screen psychological distress, as a predictor of anxiety and mood disorders. Beside this, regarding time shortage and high number of participants, the short form of the Kessler questionnaire was utilized.
Statistical analysis
Statistical analysis was performed by using SPSS software, version 26. We reported categorical variables as numbers and percentages; and continuous variables as Means±SD. Intergroup differences were compromised through using Pearson correlation and chi-squared tests. Multivariate logistic regression was utilized to explore factors that were independently associated with severe psychological distress in PWE. The multivariate model contained variables that were associated with P<0.05 in univariate analysis.
Results
Of the 159 PWE that were invited to participate in our study, 13(8%) were excluded because of their age (<15 years), 8(5%) because they refused to participate, and 6(3%) because of changes in their AEDs or its dosage within the previous month. Finally, a total of 132 PWE were enrolled and together with the same number of healthy individuals as the control group. More than half of the patients (56%) had generalized epilepsy, whereas 43% had focal epilepsy. Epilepsy was drug-resistant in 85(65%) patients. No significant difference was found in in marriage status and education level. However, patients reported significantly lower monthly income than controls. PWE reported significantly greater concern about the pandemic than the control group, and they spent significantly more hours per day following media reports of the COVID-19 outbreak (Table 1).

We found PWE had significantly higher K-6 scores than the controls. K-6 score higher than 12 was defined as severe psychological distress and we observed a that the proportion of persons who had K-6 score >12 was significantly higher in PWE (Table 2).

By using ANCOVA test, we found that level of concern about COVID-19 outbreak and time spent following media reports of the COVID-19 outbreak showed significant association with severe psychological distress (Table 3).

Because the level of concern about COVID-19 outbreak and the time spent for paying attention to COVID-19 outbreak news showed significant association with psychologic distress in univariate analysis, we performed logistic regression to explore whether they are independent predictors of psychologic distress. Results of logistic regression revealed that psychological distress was significantly associated with the amount of concern about COVID-19 outbreak (OR 1.124, 95% CI, 1.062%-1.450%) and the time spent for paying attention to COVID-19 outbreak news (OR 0.294, 95% CI, 0.128%-0.623%) adjusted for age, gender, and marital status (Table 4).
Discussion
Th present study describes the mental health status of PWE in northeast of Iran during the COVID-19 outbreak, and compares it with the mental health status of healthy controls from the same region, as well as exploring risk factors for severe psychological distress. Our survey was performed during the 6th major wave of COVID-19 pandemic which was associated the most severe phase of governmental restrictions on mobility, work, and public services. Following excluding psychotic PWE, we found that psychological distress had significantly higher levels among PWE than controls. Our findings showed that the proportion of patients with severe psychological distress (K-6 score >12) was significantly higher among PWE. More than 9% of our control group reported severe psychological distress which may be in consistent with the 9% prevalence of mental health problems reported for healthy individuals in Iran in the absence of an international pandemic [19].
Our results demonstrated that the amount of time on the COVID-19-related spent daily news and level of concern about COVID-19 outbreak are associated with severe psychological distress among PWE. A systematic review on 16 studies, revealed consistent results with our study. They reported that although PWE and the normal people both experienced psychological distress during COVID-19 pandemic, the degree of depression, anxiety and sleep disorders was significantly more severe in PWE [20]. In another similar study, Giordano et al. evaluated psychological distress among PWE during COVID-19 pandemic. They evaluated the patients during the pre- and post-lockdown period and compared the results. Based on their results, anxiety symptoms were significantly increased following the lockdown period [21]. Sanchez-Larsen and colleagues examined the effect of COVID-19 pandemic on PWE referred to the Outpatient Clinics. They found a significant increase in depression and anxiety level [22]. In line with this, Assenza and colleagues assessed psychological distress in PWE through measuring depression and anxiety levels and sleep quality. They claimed that PWE suffered from worsened depressive and anxiety symptoms and lowered sleep quality during COVID-19 pandemic [23]. In the present study, the number of participants who had K-6 score higher than 12 was significantly higher among PWE, comparing to control group, supporting pervious findings suggesting that PWE are more prone for psychologic diseases [3, 24, 25]. Beside this, the psychological distress level of our patients was similar with the study performed in Japan during Fukushima Daiichi nuclear power plant accident [26]. Comparing psychological distress of PWE during COVID-19 pandemic and Fukushima Daiichi nuclear accident, suggest that PWE are more prone to experience high amounts of stress and they need special care which should be provided by health care professionals including neurologists and psychiatrists.
Conclusion
During public health emergencies, health care professionals should focus not only on seizure control but also on the mental health status of PWE, particularly those with higher number of seizures. They should advise PWE not to pay too much time on the media coverage of the COVID-19 outbreak, and distract themselves with other activities like their hobbies. Patients with K-6 scores >12 should be regarded as experiencing severe psychological distress and a psychiatrist consultation is highly recommended.
Limitations
Our study has several limitations: First, we limited our study sample to the patients who had certain conditions such as having registered information at the Neurology Clinic of 22 Bahman Hospital or being able to use electronic devices. These patients do not represent the general population. Second, another bias is the information bias which is because of the nature of self-reporting. Third, the diagnosis of psychologic distress was only based on a questionnaire in the absence of a structured interview. Fourth, we assessed psychologic distress in PWE during COVID-19 pandemic but we did not evaluate the level of anxiety or depression in these patients.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013. The study protocol was approved by the Ethics Committee of Mashhad Medical Science Branch of Islamic Azad University (IR.IAU.MSHD.REC.1400.104).
Funding
This article extracted from MD thesis of Anahita Hashemi, approved by Department of Medicine, Mashhad Branch, Islamic Azad University.
Authors contributions
Conceptualization, methodology, supervision, and funding acquisition: Seyed Mehran Homam; Investigation and analysis: Anahita Hashemi and Negin Seyedhosseinzade; Writing original draft, review & editing: Nikoo Saeedi and Saeid Bayat.
Conflict of interest
The authors declared no conflict of interest.
References
- Bell GS, Sander JW. The epidemiology of epilepsy: The size of the problem. Seizure. 2002; 11(Suppl A):306-14; quiz 315-6. [PMID]
- Fiest KM, Dykeman J, Patten SB, Wiebe S, Kaplan GG, Maxwell CJ, et al. Depression in epilepsy: A systematic review and meta-analysis. Neurology. 2013; 80(6):590-9. [DOI:10.1212/WNL.0b013e31827b1ae0] [PMID]
- Lacey CJ, Salzberg MR, D’Souza WJ. Risk factors for psychological distress in community-treated epilepsy. Epilepsy Behav. 2014; 35:1-5. [DOI:10.1016/j.yebeh.2014.03.025] [PMID]
- Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003; 4 (Suppl 3):S31-8. [DOI:10.1016/j.yebeh.2003.08.019] [PMID]
- Petrovski S, Szoeke CE, Jones NC, Salzberg MR, Sheffield LJ, Huggins RM, et al. Neuropsychiatric symptomatology predicts seizure recurrence in newly treated patients. Neurology. 2010; 75(11):1015-21. [DOI:10.1212/WNL.0b013e3181f25b16] [PMID]
- Scott AJ, Sharpe L, Hunt C, Gandy M. Anxiety and depressive disorders in people with epilepsy: A meta-analysis. Epilepsia. 2017; 58(6):973-82. [DOI:10.1111/epi.13769] [PMID]
- Sezibera V, Nyirasafari D. Incidence of depression in Epilepsy patients. Rwanda J. 2013; 1(1):67-77. [DOI:10.4314/rj.v1i1.5F]
- Barr WB, Morrison C. Handbook on the neuropsychology of epilepsy. Berlin: Springer; 2014. [DOI:10.1007/978-0-387-92826-5]
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020; 395(10223):470-3. [DOI:10.1016/S0140-6736(20)30185-9] [PMID]
- Eurosurveillance editorial team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020; 25(5):200131e. [DOI:10.2807/1560-7917.ES.2020.25.5.200131e] [PMID]
- Bromet EJ. Mental health consequences of the Chernobyl disaster. J Radiol Prot. 2012; 32(1):N71-5. [DOI:10.1088/0952-4746/32/1/N71] [PMID]
- Li H, Chen X, Huang H. The novel coronavirus outbreak: What can be learned from China in public reporting? Glob Health Res Policy. 2020; 5:9. [DOI:10.1186/s41256-020-00140-9] [PMID]
- Huang S, Wu C, Jia Y, Li G, Zhu Z, Lu K, et al. COVID-19 outbreak: The impact of stress on seizures in patients with epilepsy. Epilepsia. 2020; 61(9):1884-93. [DOI:10.1111/epi.16635] [PMID]
- Hao X, Zhou D, Li Z, Zeng G, Hao N, Li E, et al. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020; 61(6):1166-73. [DOI:10.1111/epi.16544] [PMID]
- Alkhotani A, Siddiqui MI, Almuntashri F, Baothman R. The effect of COVID-19 pandemic on seizure control and self-reported stress on patient with epilepsy. Epilepsy Behav. 2020; 112:107323. [DOI:10.1016/j.yebeh.2020.107323] [PMID]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003; 60(2):184-9. [DOI:10.1001/archpsyc.60.2.184] [PMID]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002; 32(6):959-76. [DOI:10.1017/S0033291702006074] [PMID]
- Dadfar M, Atef Vahid MK, Lester D, Bahrami F. Kessler psychological distress scale (K6): Psychometric testing of the Farsi form in psychiatric outpatients. Adv Biores. 2016; 7(2):105-8. [Link]
- Hajebi A, Motevalian SA, Rahimi-Movaghar A, Sharifi V, Amin-Esmaeili M, Radgoodarzi R, et al. Major anxiety disorders in Iran: Prevalence, sociodemographic correlates and service utilization. BMC Psychiatry. 2018; 18(1):261. [DOI:10.1186/s12888-018-1828-2] [PMID]
- Tashakori-Miyanroudi M, Souresrafil A, Hashemi P, Jafar Ehsanzadeh S, Farrahizadeh M, Behroozi Z. Prevalence of depression, anxiety, and psychological distress in patients with epilepsy during COVID-19: A systematic review. Epilepsy Behav. 2021; 125:108410. [DOI:10.1016/j.yebeh.2021.108410] [PMID]
- Giordano A, Siciliano M, De Micco R, Sant’Elia V, Russo A, Tedeschi G, et al. Correlates of psychological distress in epileptic patients during the COVID-19 outbreak. Epilesy Behav. 2021; 115:107632. [DOI:10.1016/j.yebeh.2020.107632] [PMID]
- Sanchez-Larsen A, Gonzalez-Villar E, Díaz-Maroto I, Layos-Romero A, Martínez-Martín Á, Alcahut-Rodriguez C, et al. Influence of the COVID-19 outbreak in people with epilepsy: Analysis of a Spanish population (EPICOVID registry). Epilepsy Behav. 2020; 112:107396. [DOI:10.1016/j.yebeh.2020.107396] [PMID]
- Assenza G, Lanzone J, Brigo F, Coppola A, Di Gennaro G, Di Lazzaro V, et al. Epilepsy care in the time of COVID-19 pandemic in Italy: Risk factors for seizure worsening. Front Neurol. 2020; 11:737. [DOI:10.3389/fneur.2020.00737] [PMID]
- Gaitatzis A, Trimble MR, Sander JW. The psychiatric comorbidity of epilepsy. Acta Neurol Scand. 2004; 110(4):207-20. [DOI:10.1111/j.1600-0404.2004.00324.x] [PMID]
- Han SH, Kim KT, Ryu HU, Lee SA, Cho YJ, Kim JH, et al. Factors associated with social anxiety in South Korean adults with epilepsy. Epilepsy Behav. 2019; 101(Pt A):106569. [DOI:10.1016/j.yebeh.2019.106569] [PMID]
- Kunii Y, Suzuki Y, Shiga T, Yabe H, Yasumura S, Maeda M, et al. Severe psychological distress of evacuees in evacuation zone caused by the Fukushima Daiichi Nuclear Power Plant Accident: The Fukushima health management survey. PLoS One. 2016; 11(7):e0158821. [DOI:10.1371/journal.pone.0158821] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2023/10/11 | Accepted: 2023/10/17 | Published: 2023/10/17
Received: 2023/10/11 | Accepted: 2023/10/17 | Published: 2023/10/17
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






