Sat, May 18, 2024
Volume 10, Issue 1 (Winter 2024)
Caspian J Neurol Sci 2024, 10(1): 31-37 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pourramzani A, Gharaei Nejad K, Fakhraei S, Gholipour A. Comorbidity of Adult Attention Deficit Hyperactivity Disorder With Acne Vulgaris. Caspian J Neurol Sci 2024; 10 (1) :31-37
URL: http://cjns.gums.ac.ir/article-1-646-en.html
URL: http://cjns.gums.ac.ir/article-1-646-en.html
1- Kavosh Behavioral, Cognitive and Addiction Research Center, Shafa Hospital, Guilan University of Medical Science, Rasht, Guilan, Iran
2- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Skin Research Center, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 1088 kb]
(136 Downloads)
| Abstract (HTML) (234 Views)
Full-Text: (75 Views)
Introduction
Acne vulgaris, or pimple, is the eighth most common skin disease worldwide, with an estimated prevalence of 9.38% across all age groups, according to the 2010 global burden of disease study [1]. The occurrence of acne vulgaris in adolescents and adults varies by country and ethnicity [2]. Acne can sometimes exhibit complex social and psychological effects, and patients experience severe issues with their body image, self-esteem, sociability, and even feelings, particularly anger [3]. Studies have indicated that while acne vulgaris is not life-threatening, it does have detrimental effects on individuals' body image perception. As a result, it can lead to feelings of anxiety, sadness, and difficulties in social interactions. Acne is commonly associated with psychological disorders such as anxiety and depression [4, 5, 6]. Some epidemiological studies reported that the prevalence of acne vulgaris is higher in individuals with attention deficit hyperactivity disorder (ADHD) [7, 8]. This disorder is a prevalent mental illness that typically manifests in childhood, but it can persist into adolescence and possibly adulthood, often coexisting with other psychiatric comorbidities [9]. The enhanced challenge in managing emotions experienced by young individuals with ADHD is believed to be a factor that connects ADHD and mental health disorders [10, 11, 12]. Furthermore, the attendance of ADHD is thought to be related to severe psychiatric problems in patients with acne vulgaris. Alternatively, the putative association between acne vulgaris and ADHD could be an indication of a common etiological risk factor for these disorders, like early-life exposure to higher androgen levels [9, 13]. There are few studies investigating the link between acne and ADHD with conflicting results [7, 14, 15]. These studies have used various diagnostic techniques and standards for ADHD, ranging from formal categorical approaches to multidimensional symptom checklists, which significantly differ in their design and sample characteristics. Moreover, only a few studies have detailed variations in diagnostic propensity seen among different racial/ethnic groups. Psychiatric comorbidities with acne vulgaris are important because they can significantly impact the recommended treatments for patients with acne vulgaris, in addition to increasing the likelihood of negative effects on the patient’s quality of life. To our knowledge, no research has been published in this part of Iran that looks into the connection between ADHD and acne vulgaris. In the present study, we aim to examine the comorbidity and prevalence of ADHD among individuals with acne vulgaris based on age, gender, and severity of acne vulgaris in the population of this region.
Materials and Methods
Study design and sample size
This case-control study was conducted on 85 individuals with acne vulgaris and 85 without it. According to the findings of the Davari-Ashtiani et al. study, the sample size was estimated with a 95% confidence level and 80% test power [16]. Based on the Conners’ adult ADHD rating scales (CAARS) (hyperactivity: 14±55), about 10% (6 scores) were determined for 85 individuals in each group. Initially, the participants were briefed on the study procedure, objectives, and outcomes. It was also clarified that the study process does not alter the course of treatment for the patients. The control group was selected from the patients’ companions with the same age range as the case group. Participants will be placed in the control group if their medical history indicates that they have never had body or facial pimples or acne treatment. The case group was selected from individuals suffering from acne vulgaris who were referred to the Razi Dermatology Specialist Clinic and Beesat Clinic of Guilan University of Medical Sciences, Rasht City, Iran, in 2021. These individuals must have a history of acne vulgaris or a diagnosis of acne vulgaris by a dermatologist. After obtaining informed consent in person, an online questionnaire containing demographic information (age, gender) and the CAARS scale for the examination of ADHD symptoms were provided to the individuals. For this scale, a cut-off point of 55 was used, which, according to Davari-Ashtiani et al. research, has good validity and reliability in Iranian society [16]. Also, in the prepared questionnaire, the history of childhood ADHD and its treatment approved by a physician is asked. ADHD was confirmed based on a questionnaire with the final approval of a psychiatrist.
A dermatologist diagnosed the severity of acne vulgaris in individuals. Based on the dermatologist’s diagnosis, the severity of acne vulgaris in these patients was classified into three categories: Mild, moderate, and severe. The inclusion criteria included a diagnosis of acne vulgaris by a dermatologist, and the patients with underlying diseases and incomplete data or poor participation were excluded from the study.
Conners’ adult ADHD rating scales (CAARS)
All kinds of CAARS grading are widely used worldwide. This study used the self-reporting version of CAARS to examine ADHD symptoms. This scale is available in a long-form containing 66 questions and a short form of 30 questions and is scored based on a Likert scale from 0 (not at all) to 3 (always). Both scales have good psychometric properties [17, 18]. CAARS short-form includes several scales to examine these factors (attention/memory problems and hyperactivity/restlessness, impulsivity/emotional disability, and self-concept problems) and two other scales (ADHD index and ADHD inconsistency index) [19].
This instrument used the fourth edition of the diagnostic and statistical manual of mental disorders to measure symptoms of ADHD. It uniquely integrates knowledge, clinical skills, and psychometric techniques. One of the strengths of this tool is that it is designed based on a significant statistical population. This questionnaire has 30 items and measures three groups of symptoms included in the DSM-IV: 9 items are designed for attention deficit, 9 items for hyperactivity/impulsivity, and 12 items are a set of ADHD symptoms as a separate subscale that is introduced as the ADHD index. According to the conducted studies, the questionnaire’s test re-test reliability and internal consistency are adequate, and the correlation between the items has been satisfactory. With this questionnaire, the course of recovery can be measured, and it is used in medical centers due to its validity and reliability. The CAARS-S mean reliability was 0.75, and the test re-test correlation was 0.80 [19]. Also, each of the three factors had a Cronbach α coefficient of 0.802, 0.758, and 0. 869, respectively. To distinguish between adults with ADHD and controls, the Persian version of the CAARS-S was used, which is a valid and reliable measure [20].
Statistical analysis
SPSS software, version 24 was used for all statistical analyses. The prevalence of ADHD and acne vulgaris were assessed using frequency and percentage, with a 95% confidence interval. The Fisher exact test and chi-squared test are used to compare the frequency of ADHD in two groups. Using the Mean±SD, the score of the ADHD evaluation scale was calculated. The ADHD scores of the two groups were compared using the independent t-test. The significance level of all tests was determined to be P<0.05.
Results
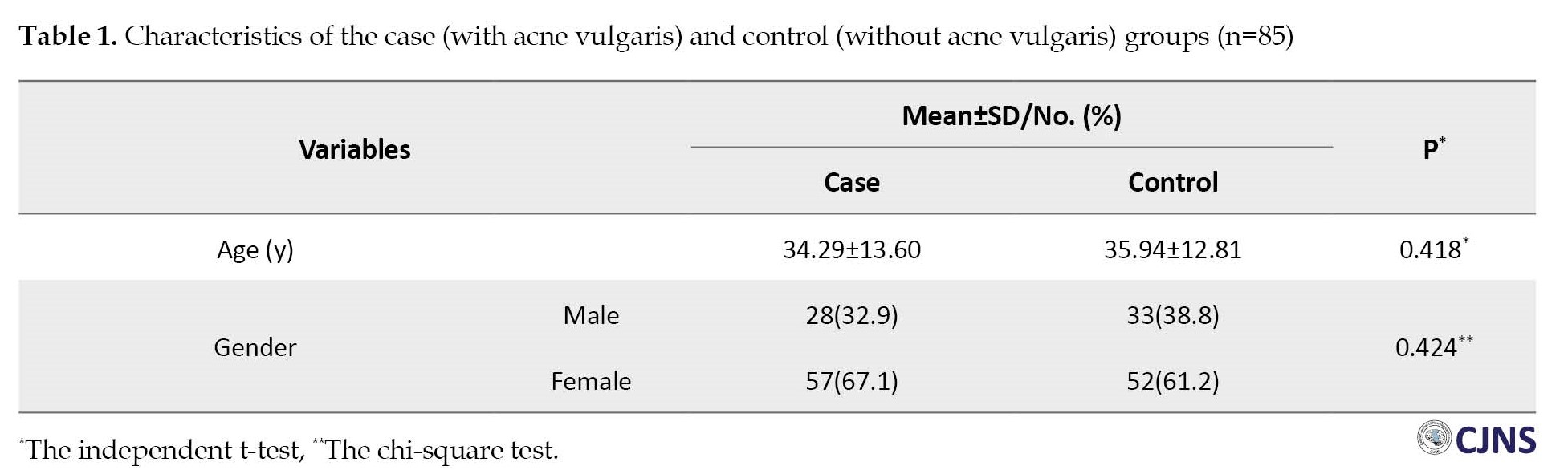
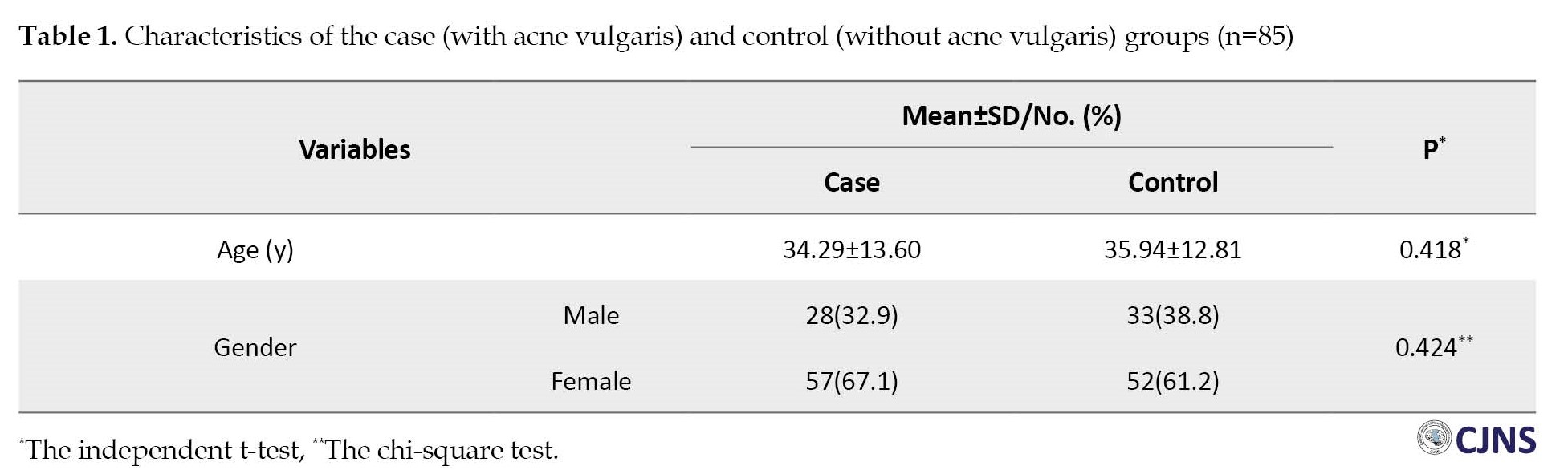
The mean age of the participants was 35.12±13.19 years, and there was no significant difference in the mean age between the case (34.29±13.60 years) and control (35.94±12.81years) groups (P=0.418). Of the participants, 35.9% (n=61) were men, and 64.1% (n=109) were women. The gender difference between the studied groups was not significant (P=0.424) (Table 1).
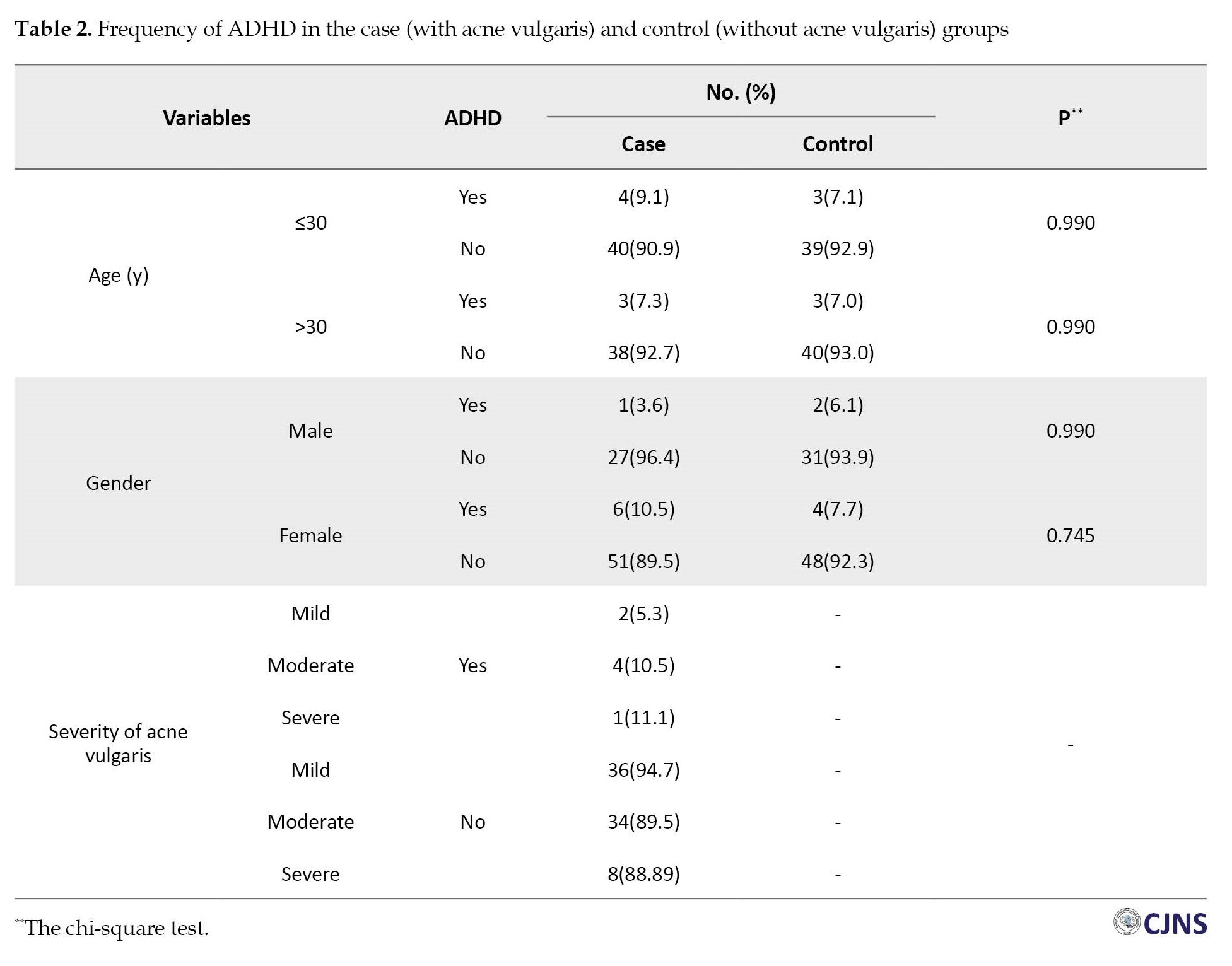
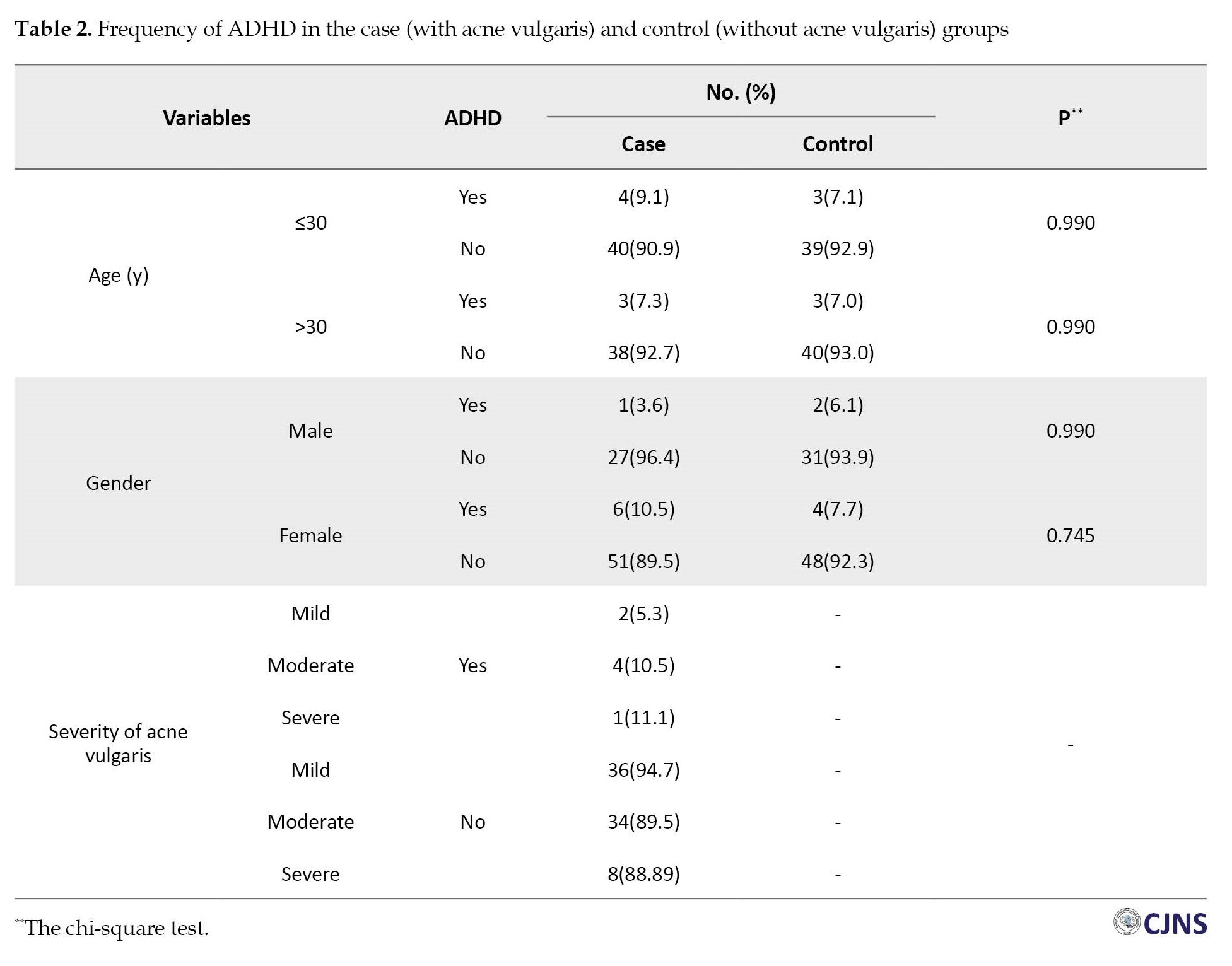
Of the total population, 7.6% (n=13) had ADHD, and the frequency of ADHD in individuals with acne vulgaris compared to control was 8.2% vs 7.1%, respectively, and this difference was not significant (P=0.773). The frequency of ADHD in individuals with acne vulgaris compared with controls was higher in those aged ≤30 years and in women. In addition, it was observed that the frequency of ADHD increases with the increase in the severity of acne vulgaris in mild, moderate, and severe forms, which are 5.3%, 10.5%, and 11.1% respectively, although not significant (P>0.05) (Table 2).
The mean score of the ADHD questionnaire was 30.21±17.18 (0 to 78), and no significant differences were found between the case (30.84±16.99) and control (29.60±17.45) groups for CAARS scores (P=0.641). The ADHD scales were higher in individuals with acne vulgaris aged ≤30 years and in women than in controls. Also, the CAARS score showed an upward trend with increasing severity of acne vulgaris. However, there was no statistically significant difference (P>0.05) between the two groups (Table 3).

Discussion
The growing list of negative consequences linked to adult ADHD emphasizes how critical it is to identify and manage the condition. Still, there are unanswered questions regarding the diagnostic procedure, the true incidence of ADHD in adults, and potential barriers to its identification. The association between ADHD and skin disorders has been a source of public and clinical concern. This condition also applies to acne, which lowers the quality of life for those with it. ADHD detrimentally affects feelings, relationships with others, physical activity, social life, and career standing [21]. Therefore, the prevalence of ADHD in people with acne vulgaris was examined in this study, along with the impact of gender and age.
In this study, the prevalence of ADHD in all participants was 7.6%, and the prevalence of ADHD in those with and without acne was 8.2% and 7.1%, respectively. A retrospective study of epidemiologically representative samples found that acne vulgaris had a greater than twofold higher likelihood of being linked to ADHD than other skin disorders [7]. Comparing the frequency of ADHD in acne vulgaris and atopic eczema, the odds ratio was 5.606, suggesting a higher prevalence of ADHD in patients with acne vulgaris than in those with other skin diseases [22]. Also, in our study, the mean score of CARRS was higher in individuals with acne vulgaris than in control. However, in general, the frequency of ADHD and the ADHD scales did not differ significantly between the two groups, possibly due to the small sample size in the present study. Likewise, Bilgic et al. indicated no statistically significant differences between patients with acne vulgaris and controls regarding ADHD scales [14]. Some studies reported that the increased rate of mental morbidity and suicidal thoughts and actions in acne vulgaris patients may be partially attributed to ADHD [23-25].
Similarly, a study revealed a link between adolescent ADHD and severe acne vulgaris [8]. Nevertheless, in clinical samples, our results did not verify a link between acne vulgaris and ADHD. In addition, it was observed that the prevalence of ADHD and its scores were higher in individuals with severe and mild acne vulgaris, respectively. However, this difference was not statistically significant between individuals with acne vulgaris and control. Similarly, Deveci et al. found no differences between groups in cognitive tests assessing attention or executive function [15]. Gupta et al. demonstrated that patients with acne vulgaris younger than 40 and females have a higher chance of ADHD [7]. Studies suggest that the association with ADHD is unlikely specific to acne vulgaris, as such psychiatric disorders have also been observed in childhood eczema and can occur in any chronic disease [26, 27]. The level of parental androgen is related to autism traits, and multiple genes involved in steroidogenesis are thought to be associated with autism, Asperger’s syndrome, and or autistic traits. Higher frequency of androgen-associated disorders, such as acne vulgaris, have been stated in females with autism spectrum disorders [28]. In our study, the frequency of ADHD and the ADHD scales were higher in individuals with acne vulgaris less than 30 years and women. However, no statistically significant differences have been observed between individuals with and without acne vulgaris. Similar findings have been indicated in the Deveci et al. study [14].
The difference observed in our results compared to other studies may be due to the type of method and validated questionnaire, sampling, ethnicity, and genetic differences in patients with acne vulgaris. The lack of a large sample size is one of our study limitations. Moreover, the information about acne vulgaris duration was unclear among participants. Therefore, it is suggested that research with a broader sample size investigate the comorbidity between acne and ADHD by considering related factors.
Conclusion
In conclusion, the results of the present study did not confirm the association between ADHD and acne vulgaris. Further investigations are necessary to clarify better the links between ADHD and risk factors in individuals with acne vulgaris.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.165). All study procedures complied with the ethical guidelines of the Declaration of Helsinki 2013.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, methodology, resources, and supervision: Ali Pourramzani and Kaveh Gharaei Nejad; Investigation, writing the original draft: Sara Fakhraei and Atena Gholipour; Review, and editing: Ali Pourramzani, Kaveh Gharaei Nejad, Sara Fakhraei, and Atena Gholipour; Funding acquisition: Kaveh Gharaei Nejad.
Conflict of interest
The authors declared no competing interests.
Acknowledgements
The authors thank all subjects for participating in this study and the Guilan University of Medical Sciences, for cooperation in data collection.
References
Acne vulgaris, or pimple, is the eighth most common skin disease worldwide, with an estimated prevalence of 9.38% across all age groups, according to the 2010 global burden of disease study [1]. The occurrence of acne vulgaris in adolescents and adults varies by country and ethnicity [2]. Acne can sometimes exhibit complex social and psychological effects, and patients experience severe issues with their body image, self-esteem, sociability, and even feelings, particularly anger [3]. Studies have indicated that while acne vulgaris is not life-threatening, it does have detrimental effects on individuals' body image perception. As a result, it can lead to feelings of anxiety, sadness, and difficulties in social interactions. Acne is commonly associated with psychological disorders such as anxiety and depression [4, 5, 6]. Some epidemiological studies reported that the prevalence of acne vulgaris is higher in individuals with attention deficit hyperactivity disorder (ADHD) [7, 8]. This disorder is a prevalent mental illness that typically manifests in childhood, but it can persist into adolescence and possibly adulthood, often coexisting with other psychiatric comorbidities [9]. The enhanced challenge in managing emotions experienced by young individuals with ADHD is believed to be a factor that connects ADHD and mental health disorders [10, 11, 12]. Furthermore, the attendance of ADHD is thought to be related to severe psychiatric problems in patients with acne vulgaris. Alternatively, the putative association between acne vulgaris and ADHD could be an indication of a common etiological risk factor for these disorders, like early-life exposure to higher androgen levels [9, 13]. There are few studies investigating the link between acne and ADHD with conflicting results [7, 14, 15]. These studies have used various diagnostic techniques and standards for ADHD, ranging from formal categorical approaches to multidimensional symptom checklists, which significantly differ in their design and sample characteristics. Moreover, only a few studies have detailed variations in diagnostic propensity seen among different racial/ethnic groups. Psychiatric comorbidities with acne vulgaris are important because they can significantly impact the recommended treatments for patients with acne vulgaris, in addition to increasing the likelihood of negative effects on the patient’s quality of life. To our knowledge, no research has been published in this part of Iran that looks into the connection between ADHD and acne vulgaris. In the present study, we aim to examine the comorbidity and prevalence of ADHD among individuals with acne vulgaris based on age, gender, and severity of acne vulgaris in the population of this region.
Materials and Methods
Study design and sample size
This case-control study was conducted on 85 individuals with acne vulgaris and 85 without it. According to the findings of the Davari-Ashtiani et al. study, the sample size was estimated with a 95% confidence level and 80% test power [16]. Based on the Conners’ adult ADHD rating scales (CAARS) (hyperactivity: 14±55), about 10% (6 scores) were determined for 85 individuals in each group. Initially, the participants were briefed on the study procedure, objectives, and outcomes. It was also clarified that the study process does not alter the course of treatment for the patients. The control group was selected from the patients’ companions with the same age range as the case group. Participants will be placed in the control group if their medical history indicates that they have never had body or facial pimples or acne treatment. The case group was selected from individuals suffering from acne vulgaris who were referred to the Razi Dermatology Specialist Clinic and Beesat Clinic of Guilan University of Medical Sciences, Rasht City, Iran, in 2021. These individuals must have a history of acne vulgaris or a diagnosis of acne vulgaris by a dermatologist. After obtaining informed consent in person, an online questionnaire containing demographic information (age, gender) and the CAARS scale for the examination of ADHD symptoms were provided to the individuals. For this scale, a cut-off point of 55 was used, which, according to Davari-Ashtiani et al. research, has good validity and reliability in Iranian society [16]. Also, in the prepared questionnaire, the history of childhood ADHD and its treatment approved by a physician is asked. ADHD was confirmed based on a questionnaire with the final approval of a psychiatrist.
A dermatologist diagnosed the severity of acne vulgaris in individuals. Based on the dermatologist’s diagnosis, the severity of acne vulgaris in these patients was classified into three categories: Mild, moderate, and severe. The inclusion criteria included a diagnosis of acne vulgaris by a dermatologist, and the patients with underlying diseases and incomplete data or poor participation were excluded from the study.
Conners’ adult ADHD rating scales (CAARS)
All kinds of CAARS grading are widely used worldwide. This study used the self-reporting version of CAARS to examine ADHD symptoms. This scale is available in a long-form containing 66 questions and a short form of 30 questions and is scored based on a Likert scale from 0 (not at all) to 3 (always). Both scales have good psychometric properties [17, 18]. CAARS short-form includes several scales to examine these factors (attention/memory problems and hyperactivity/restlessness, impulsivity/emotional disability, and self-concept problems) and two other scales (ADHD index and ADHD inconsistency index) [19].
This instrument used the fourth edition of the diagnostic and statistical manual of mental disorders to measure symptoms of ADHD. It uniquely integrates knowledge, clinical skills, and psychometric techniques. One of the strengths of this tool is that it is designed based on a significant statistical population. This questionnaire has 30 items and measures three groups of symptoms included in the DSM-IV: 9 items are designed for attention deficit, 9 items for hyperactivity/impulsivity, and 12 items are a set of ADHD symptoms as a separate subscale that is introduced as the ADHD index. According to the conducted studies, the questionnaire’s test re-test reliability and internal consistency are adequate, and the correlation between the items has been satisfactory. With this questionnaire, the course of recovery can be measured, and it is used in medical centers due to its validity and reliability. The CAARS-S mean reliability was 0.75, and the test re-test correlation was 0.80 [19]. Also, each of the three factors had a Cronbach α coefficient of 0.802, 0.758, and 0. 869, respectively. To distinguish between adults with ADHD and controls, the Persian version of the CAARS-S was used, which is a valid and reliable measure [20].
Statistical analysis
SPSS software, version 24 was used for all statistical analyses. The prevalence of ADHD and acne vulgaris were assessed using frequency and percentage, with a 95% confidence interval. The Fisher exact test and chi-squared test are used to compare the frequency of ADHD in two groups. Using the Mean±SD, the score of the ADHD evaluation scale was calculated. The ADHD scores of the two groups were compared using the independent t-test. The significance level of all tests was determined to be P<0.05.
Results
The mean age of the participants was 35.12±13.19 years, and there was no significant difference in the mean age between the case (34.29±13.60 years) and control (35.94±12.81years) groups (P=0.418). Of the participants, 35.9% (n=61) were men, and 64.1% (n=109) were women. The gender difference between the studied groups was not significant (P=0.424) (Table 1).
Of the total population, 7.6% (n=13) had ADHD, and the frequency of ADHD in individuals with acne vulgaris compared to control was 8.2% vs 7.1%, respectively, and this difference was not significant (P=0.773). The frequency of ADHD in individuals with acne vulgaris compared with controls was higher in those aged ≤30 years and in women. In addition, it was observed that the frequency of ADHD increases with the increase in the severity of acne vulgaris in mild, moderate, and severe forms, which are 5.3%, 10.5%, and 11.1% respectively, although not significant (P>0.05) (Table 2).
The mean score of the ADHD questionnaire was 30.21±17.18 (0 to 78), and no significant differences were found between the case (30.84±16.99) and control (29.60±17.45) groups for CAARS scores (P=0.641). The ADHD scales were higher in individuals with acne vulgaris aged ≤30 years and in women than in controls. Also, the CAARS score showed an upward trend with increasing severity of acne vulgaris. However, there was no statistically significant difference (P>0.05) between the two groups (Table 3).

Discussion
The growing list of negative consequences linked to adult ADHD emphasizes how critical it is to identify and manage the condition. Still, there are unanswered questions regarding the diagnostic procedure, the true incidence of ADHD in adults, and potential barriers to its identification. The association between ADHD and skin disorders has been a source of public and clinical concern. This condition also applies to acne, which lowers the quality of life for those with it. ADHD detrimentally affects feelings, relationships with others, physical activity, social life, and career standing [21]. Therefore, the prevalence of ADHD in people with acne vulgaris was examined in this study, along with the impact of gender and age.
In this study, the prevalence of ADHD in all participants was 7.6%, and the prevalence of ADHD in those with and without acne was 8.2% and 7.1%, respectively. A retrospective study of epidemiologically representative samples found that acne vulgaris had a greater than twofold higher likelihood of being linked to ADHD than other skin disorders [7]. Comparing the frequency of ADHD in acne vulgaris and atopic eczema, the odds ratio was 5.606, suggesting a higher prevalence of ADHD in patients with acne vulgaris than in those with other skin diseases [22]. Also, in our study, the mean score of CARRS was higher in individuals with acne vulgaris than in control. However, in general, the frequency of ADHD and the ADHD scales did not differ significantly between the two groups, possibly due to the small sample size in the present study. Likewise, Bilgic et al. indicated no statistically significant differences between patients with acne vulgaris and controls regarding ADHD scales [14]. Some studies reported that the increased rate of mental morbidity and suicidal thoughts and actions in acne vulgaris patients may be partially attributed to ADHD [23-25].
Similarly, a study revealed a link between adolescent ADHD and severe acne vulgaris [8]. Nevertheless, in clinical samples, our results did not verify a link between acne vulgaris and ADHD. In addition, it was observed that the prevalence of ADHD and its scores were higher in individuals with severe and mild acne vulgaris, respectively. However, this difference was not statistically significant between individuals with acne vulgaris and control. Similarly, Deveci et al. found no differences between groups in cognitive tests assessing attention or executive function [15]. Gupta et al. demonstrated that patients with acne vulgaris younger than 40 and females have a higher chance of ADHD [7]. Studies suggest that the association with ADHD is unlikely specific to acne vulgaris, as such psychiatric disorders have also been observed in childhood eczema and can occur in any chronic disease [26, 27]. The level of parental androgen is related to autism traits, and multiple genes involved in steroidogenesis are thought to be associated with autism, Asperger’s syndrome, and or autistic traits. Higher frequency of androgen-associated disorders, such as acne vulgaris, have been stated in females with autism spectrum disorders [28]. In our study, the frequency of ADHD and the ADHD scales were higher in individuals with acne vulgaris less than 30 years and women. However, no statistically significant differences have been observed between individuals with and without acne vulgaris. Similar findings have been indicated in the Deveci et al. study [14].
The difference observed in our results compared to other studies may be due to the type of method and validated questionnaire, sampling, ethnicity, and genetic differences in patients with acne vulgaris. The lack of a large sample size is one of our study limitations. Moreover, the information about acne vulgaris duration was unclear among participants. Therefore, it is suggested that research with a broader sample size investigate the comorbidity between acne and ADHD by considering related factors.
Conclusion
In conclusion, the results of the present study did not confirm the association between ADHD and acne vulgaris. Further investigations are necessary to clarify better the links between ADHD and risk factors in individuals with acne vulgaris.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1400.165). All study procedures complied with the ethical guidelines of the Declaration of Helsinki 2013.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors contributions
Conceptualization, methodology, resources, and supervision: Ali Pourramzani and Kaveh Gharaei Nejad; Investigation, writing the original draft: Sara Fakhraei and Atena Gholipour; Review, and editing: Ali Pourramzani, Kaveh Gharaei Nejad, Sara Fakhraei, and Atena Gholipour; Funding acquisition: Kaveh Gharaei Nejad.
Conflict of interest
The authors declared no competing interests.
Acknowledgements
The authors thank all subjects for participating in this study and the Guilan University of Medical Sciences, for cooperation in data collection.
References
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380(9859):2163-96. [PMID]
- Bagatin E, Timpano DL, Guadanhim LR, Nogueira VM, Terzian LR, Steiner D, et al. Acne vulgaris: Prevalence and clinical forms in adolescents from São Paulo, Brazil. An Bras Dermatol. 2014; 89(3):428-35. [DOI:10.1590/abd1806-4841.20142100] [PMID]
- Kokandi A. Evaluation of acne quality of life and clinical severity in acne female adults. Dermatol Res Pract. 2010; 2010:410809. [DOI:10.1155/2010/410809] [PMID]
- Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012; 379(9813):361-72. [DOI:10.1016/S0140-6736(11)60321-8] [PMID]
- Bowe WP, Doyle AK, Crerand CE, Margolis DJ, Shalita AR. Body image disturbance in patients with acne vulgaris. J Clin Aesthet Dermatol. 2011; 4(7):35-41. [PMID]
- Hazarika N, Archana M. The psychosocial impact of acne vulgaris. Indian J Dermatol. 2016; 61(5):515-20. [PMID]
- Gupta MA, Gupta AK, Vujcic B. Increased frequency of Attention Deficit Hyperactivity Disorder (ADHD) in acne versus dermatologic controls: analysis of an epidemiologic database from the US. J Dermatolog Treat. 2014; 25(2):115-8.[PMID]
- Silverberg JI, Silverberg NB. Epidemiology and extracutaneous comorbidities of severe acne in adolescence: A US population‐based study. Br J Dermatol. 2014; 170(5):1136-42. [DOI:10.1111/bjd.12912] [PMID]
- Becker SP, Luebbe AM, Langberg JM. Co-occurring mental health problems and peer functioning among youth with attention-deficit/hyperactivity disorder: A review and recommendations for future research. Clin Child Fam Psychol Rev. 2012; 15(4):279-302. [DOI:10.1007/s10567-012-0122-y] [PMID]
- Impey M, Heun R. Completed suicide, ideation and attempt in attention deficit hyperactivity disorder. Acta Psychiatr Scand. 2012; 125(2):93-102. [PMID]
- James A. Completed suicide, ideation and attempts in attention deficit hyperactivity disorder. Acta Psychiatr Scand. 2012; 125(2):91-2. [DOI:10.1111/j.1600-0447.2011.01775.x] [PMID]
- Seymour KE, Chronis-Tuscano A, Halldorsdottir T, Stupica B, Owens K, Sacks T. Emotion regulation mediates the relationship between ADHD and depressive symptoms in youth. J Abnorm Child Psychol. 2012; 40(4):595-606. [DOI:10.1007/s10802-011-9593-4] [PMID]
- Halvorsen JA, Stern RS, Dalgard F, Thoresen M, Bjertness E, Lien L. Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: A population-based study. J Invest Dermatol. 2011; 131(2):363-70. [DOI:10.1038/jid.2010.264] [PMID]
- Bilgic A, Bilgic Ö, Çolak RS, Altınyazar HC. Relationship between acne vulgaris and attention-deficit/hyperactivity disorder symptoms in a clinical sample of women. An Bras Dermatol. 2016; 91(2):250-2. [DOI:10.1590/abd1806-4841.20164613] [PMID]
- Deveci E, Ozturk A, Kirpinar I, Koyuncu A, Engin I, Melikoğlu M. Neurocognition in patients with acne vulgaris. J Psychiatry. 2014; 17(121):2. [Link]
- Davari-Ashtiani R, Jazayeri F, Arabgol F, Razjouyan K, Khademi M. [Psychometric properties of Persian Version of Conners’ Adult Attention Deficit/Hyperactivity Disorder Rating Scale (Screening Form-Self Reporting) (Persian)]. Iran J Psychiatry Clin Psychol. 2014; 20(3):243-51. [Link]
- Sandra Kooij JJ, Keith Conners C, Goto T, Tanaka Y, Williams D, Allen AJ, et al. Validity of Conners’ adult attention-deficit/hyperactivity disorder rating scale-investigator rated: Screening version in patients from within and outside of Europe. Psychiatry Res. 2013; 208(1):94-6. [DOI:10.1016/j.psychres.2012.12.003] [PMID]
- La Malfa G, Lassi S, Bertelli M, Pallanti S, Albertini G. Detecting attention-deficit/hyperactivity disorder (ADHD) in adults with intellectual disability: The use of Conners’ Adult ADHD Rating Scales (CAARS). Res Dev Disabil. 2008; 29(2):158-64. [DOI:10.1016/j.ridd.2007.02.002] [PMID]
- Amador-Campos JA, Gómez-Benito J, Ramos-Quiroga JA. The conners’ adult ADHD rating scales-short self-report and observer forms: Psychometric properties of the Catalan version. J Atten Disord. 2014; 18(8):671-9. [DOI:10.1177/1087054712446831] [PMID]
- Moghadasin M, Dibajnia P. [Validation of the Persian version of the Connerâ s Adult ADHD Rating Scalesâ self-report (CAARS-S-SV) (Persian)]. Clin Psychol Personal. 2020; 18(1):177-99. [DOI:10.22070/CPAP.2020.2931]
- Walker N, Lewis‐Jones M. Quality of life and acne in Scottish adolescent schoolchildren: Use of the Children’s Dermatology Life Quality Index©(CDLQI) and the Cardiff Acne Disability Index©(CADI). J Eur Acad Dermatol Venereol. 2006; 20(1):45-50. [DOI:10.1111/j.1468-3083.2005.01344.x] [PMID]
- Mishra N, kant Rastogi M, Gahalaut P, Srivastava N, Aggarwal A. Assessment of depression in patients of acne vulgaris and its correlation with severity of acne, post acne scarring and gender. J Pak Assoc Dermatol. 2017; 27(4):313-9. [Link]
- Malik F, Mari PC, Augusto Jr SN, Needlman R. Missed opportunities for suicide prevention in teens with ADHD. Journal of Affective Disorders Reports. 2023; 12:100482. [DOI:10.1016/j.jadr.2023.100482]
- Aslan Kayiran M, Karadag AS, Jafferany M. Psychodermatology of acne: Dermatologist’s guide to inner side of acne and management approach. Dermatol Ther. 2020; 33(6):e14150. [DOI:10.1111/dth.14150]
- Singam V, Rastogi S, Patel KR, Lee HH, Silverberg JI. The mental health burden in acne vulgaris and rosacea: an analysis of the US National Inpatient Sample. Clin Exp Dermatol. 2019; 44(7):766-72. [PMID]
- Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity in patients with atopic dermatitis. J Allergy Clin Immunol. 2013; 131(2):428-33. [DOI:10.1016/j.jaci.2012.10.041] [PMID]
- Blackman JA, Gurka MJ, Gurka KK, Oliver MN. Emotional, developmental and behavioural comorbidities of children with chronic health conditions. J Paediatr Child Health. 2011; 47(10):742-7. [DOI:10.1111/j.1440-1754.2011.02044.x] [PMID]
- Mascarenhas JJ, Krishna A. Blemish on the Body, Scar on the Mind-Psychiatric Aspects of Acne Vulgaris: An update. Int J Contemp Med Res. 2019; 6(10):1-7. [Link]
Type of Study: Research |
Subject:
Special
Received: 2023/07/19 | Accepted: 2023/10/25 | Published: 2024/01/10
Received: 2023/07/19 | Accepted: 2023/10/25 | Published: 2024/01/10
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |