Sat, May 18, 2024
Volume 9, Issue 3 (Summer 2023)
Caspian J Neurol Sci 2023, 9(3): 175-183 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghayeghran A R, Asadi K, Yousefzadeh-Chabok S, Adineh Z, Kazemnejad-Leili E. Pattern Changes of Stroke Frequency in the COVID-19 Pandemic. Caspian J Neurol Sci 2023; 9 (3) :175-183
URL: http://cjns.gums.ac.ir/article-1-642-en.html
URL: http://cjns.gums.ac.ir/article-1-642-en.html
Amir Reza Ghayeghran * 

 1, Khatereh Asadi2
1, Khatereh Asadi2 

 , Shahrokh Yousefzadeh-Chabok3
, Shahrokh Yousefzadeh-Chabok3 

 , Zahra Adineh1
, Zahra Adineh1 

 , Ehsan Kazemnejad-Leili4
, Ehsan Kazemnejad-Leili4 




 1, Khatereh Asadi2
1, Khatereh Asadi2 

 , Shahrokh Yousefzadeh-Chabok3
, Shahrokh Yousefzadeh-Chabok3 

 , Zahra Adineh1
, Zahra Adineh1 

 , Ehsan Kazemnejad-Leili4
, Ehsan Kazemnejad-Leili4 


1- Department of Neurology, School of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Medical Nanotechnology, School of Advanced Medical Sciences and Technologies, Shiraz University of Medical Sciences, Shiraz, Iran.
3- Department of Neurosurgery, School of Medicine, Neuroscience Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Medical Nanotechnology, School of Advanced Medical Sciences and Technologies, Shiraz University of Medical Sciences, Shiraz, Iran.
3- Department of Neurosurgery, School of Medicine, Neuroscience Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
4- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 1383 kb]
(176 Downloads)
| Abstract (HTML) (349 Views)
References
Full-Text: (128 Views)
Introduction
Globally, stroke is ranked as the most common cause of death and disability. It is categorized into two major types: ischemic and hemorrhagic [1]. Ischemic stroke (IS) accounts for approximately 85% of all stroke cases. The prevalence of brain intraparenchymal hemorrhage (IPH) is 10%, leading to 40% mortality in affected middle-aged men [2]. Age, sex, race, sickle cell disease, hypertension, smoking, diabetes, and obesity are the most important risk factors for cerebral IPH [3, 4].
In early February 2020, when the coronavirus disease 2019 (COVID-19) pandemic was declared, it changed the pattern of stroke patient delivery to the healthcare system. Many previous studies reported a global decline in the stroke hospital admission rate during the initial peak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, but the admission frequency of patients with more severe stroke and higher stroke mortality risk increased in several most affected countries [5, 6, 7, 8, 9].
Recent molecular pathological evidence offers respiratory infections as a risk factor in cerebrovascular disease. S protein of SARS-CoV2 has a high affinity for broad endothelial angiotensin-converting enzyme-2 ACE2 receptors, overexpressed in the epithelial cells of the oral and nasal mucosa. Therefore, SARS-CoV-2 easily enters the brain and influences the thalamus and brain stem through the olfactory bulb nerve, eventually leading to nerve damage and affecting the nervous system [10, 11, 12, 13]. Besides, SARS-CoV-2 causes cytokine storm syndrome, which may develop into an acute cerebrovascular disease caused by vascular wall inflammation and vascular smooth muscle necrosis. Patients typically present evidence of neuropathological manifestations in the initial stages of severe infection [14]. Clinical findings have reported various neurological complications such as headache, memory loss, fatal encephalitis, meningitis, stroke, acute cerebrovascular disease, and other major pathologic conditions associated with viral invasion. Furthermore, neurological disorders have been seen in 36% of COVID-19 patients, and 5.9% of cases are associated with stroke [14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. In addition, a few studies have demonstrated that SARS-CoV-2 infections are associated with hypoxemia, changes in blood pressure, coagulation status, and C-reactive protein in aged patients, increasing cerebrovascular disease incidence [26]. Hence, we performed a study to appraise the alteration of stroke patterns during the COVID-19 pandemic. This study compared the relative frequencies of IS stroke and IPH among hospitalized patients in Poursina Hospital, Guilan Province, Iran, in two corresponding periods before and during the coronavirus pandemic.
Materials and Methods
This comparative cross-sectional study was conducted to evaluate the relative frequency of patients with acute IS stroke and IPH admitted to the Neurology ward of Poursina Hospital, Guilan, Iran, during the COVID-19 pandemic period between December 2019 and June 2020, and the similar 6-month period in the previous year. Poursina stroke center is the most important academic, public comprehensive stroke unit hospital providing early treatment and rehabilitation care for stroke patients in Guilan, northern Iran. Taking informed consent was not essential because of the retrospective nature of the survey.
Inclusion/exclusion criteria
All patients with acute IS stroke and IPH who had electronic medical records and neuroimaging data (CT scan, MRI) were included in the study. However, we excluded patients with symptoms lasting less than 24 hours, therapeutic anti-thrombolytic, bleeding disorders, head trauma, or brain tumor.
Data extraction
In this study, 1309 patients were included. Two neurologists assessed all patients according to similar stroke guidelines with regard to stroke classification, time of symptom onset, and outcomes (recovery or death).
Clinical assessment
The suspected clinical signs of stroke are hemiparesis or hemianesthesia, altered level of consciousness, speech disturbance, visual disturbances in one or both eyes, impaired standing, or maintaining balance.
Neuroimaging assessment
The brain CT scan is the gold standard for distinguishing between ischemic and hemorrhagic strokes. IPH was first detected as hyperdensity regions in CT scan images, but brain MRI (1.5 Tesla) was also performed to accurately diagnose stroke, especially ischemic stroke.
Based on previous research, patients’ demographic information (age, gender, BMI, level of education, etc.) and comorbidities (diabetes, hypertension, tuberculosis, anemia, history of transient ischemic attack, hyperlipidemia, arrhythmia, congestive heart failure, coronary heart disease, smoking history, alcohol consumption, etc.) were collected.
Statistical
Data analysis was done with the statistical package social sciences SPSS software, version 21 (IBM Corp. Armonk, NY, USA). The frequency distribution and a 95% confidence interval (CI) were used to determine the relative frequency of strokes in the two study periods. The IS to IPH stroke ratio was evaluated based on average and 95% CI. The regression logistic statistical method was used to compare the frequency distribution of IS and IPH strokes after controlling for the effects of age, sex, and other intervening variables. In this study, P<0.05 was considered the significance level of the tests.
Results
In this study, 1309 patients were included. The frequency of stroke patients admitted to Poursina Hospital during the COVID-19 pandemic (December 22, 2019, to June 20, 2020) was 467 cases (35.68%) compared to 842 cases (64.32%) during the corresponding period in the previous year. Thus, the percentage of stroke patients admitted during the COVID-19 pandemic had a 28.6% decline compared with the same time last year. This difference was statistically significant (P<0.001).
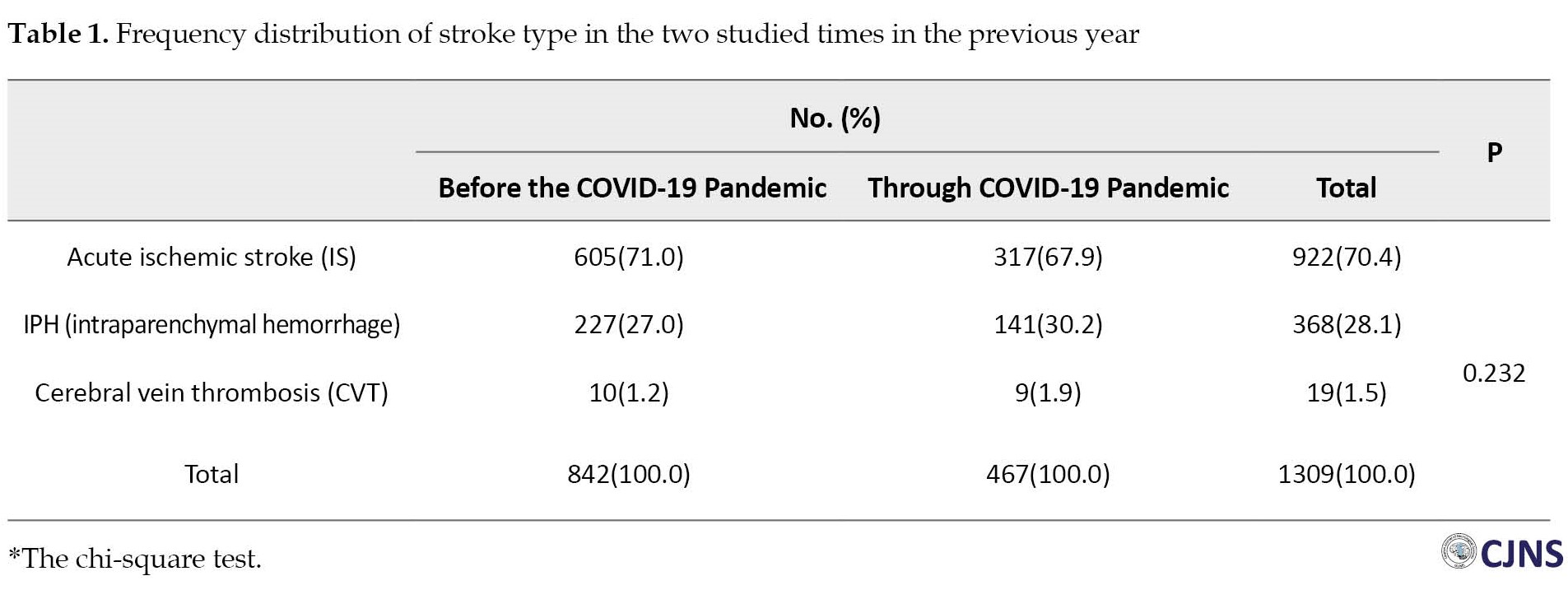
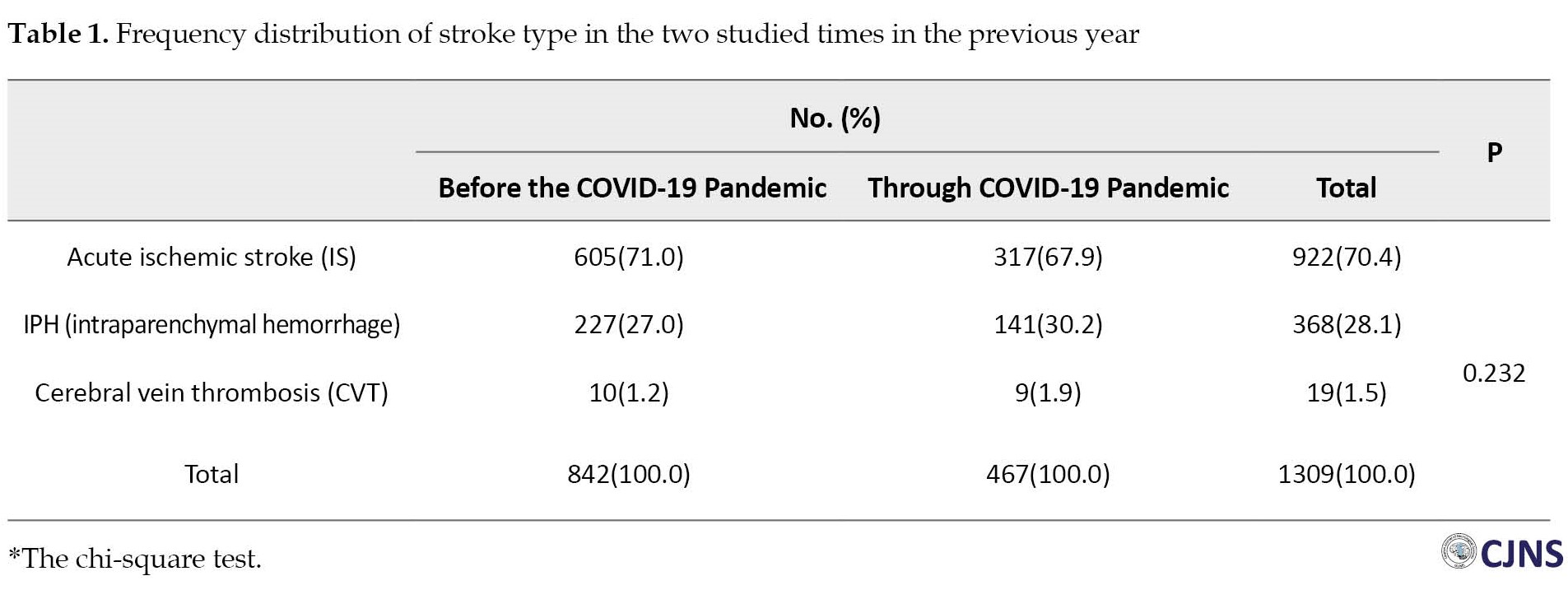
According to the results, 70.4%, 28.1%, and 1.5% of all patients were IS, IPH, and cerebral venous thrombosis (CVT), respectively. The frequency of admission of stroke patients through the SARS-CoV-2 pandemic was 67.9% for IS, 30.2% for IPH, and 1.9% for CVT, while these percentages were 71.9%, 27%, and 1.2% in a similar period in the prior year, respectively. The comparison between the percentages of IS, IPH, and CVT admission patients in two study periods based on the chi-square test was not significant (P=0.232). Furthermore, the ratio of stroke IS to stroke IPH declined from 2.6 in the corresponding period in the previous year to 2.2 during the SARS-CoV-2 pandemic period (Table 1).
There was no significant difference in smoking (P=0.808) or the number of cigarettes packs (P=0.365) between the two time periods in the referring patients, but the frequency of alcohol consumption declined (P=0.036) in the COVID-19 pandemic (11.13%) compared to the same period the previous year (15.3%) (Table 2).

The frequency of alcohol consumption during the COVID-19 pandemic (P<0.05) and the same period in the previous year (P<0.001) have significant differences (Table 3).
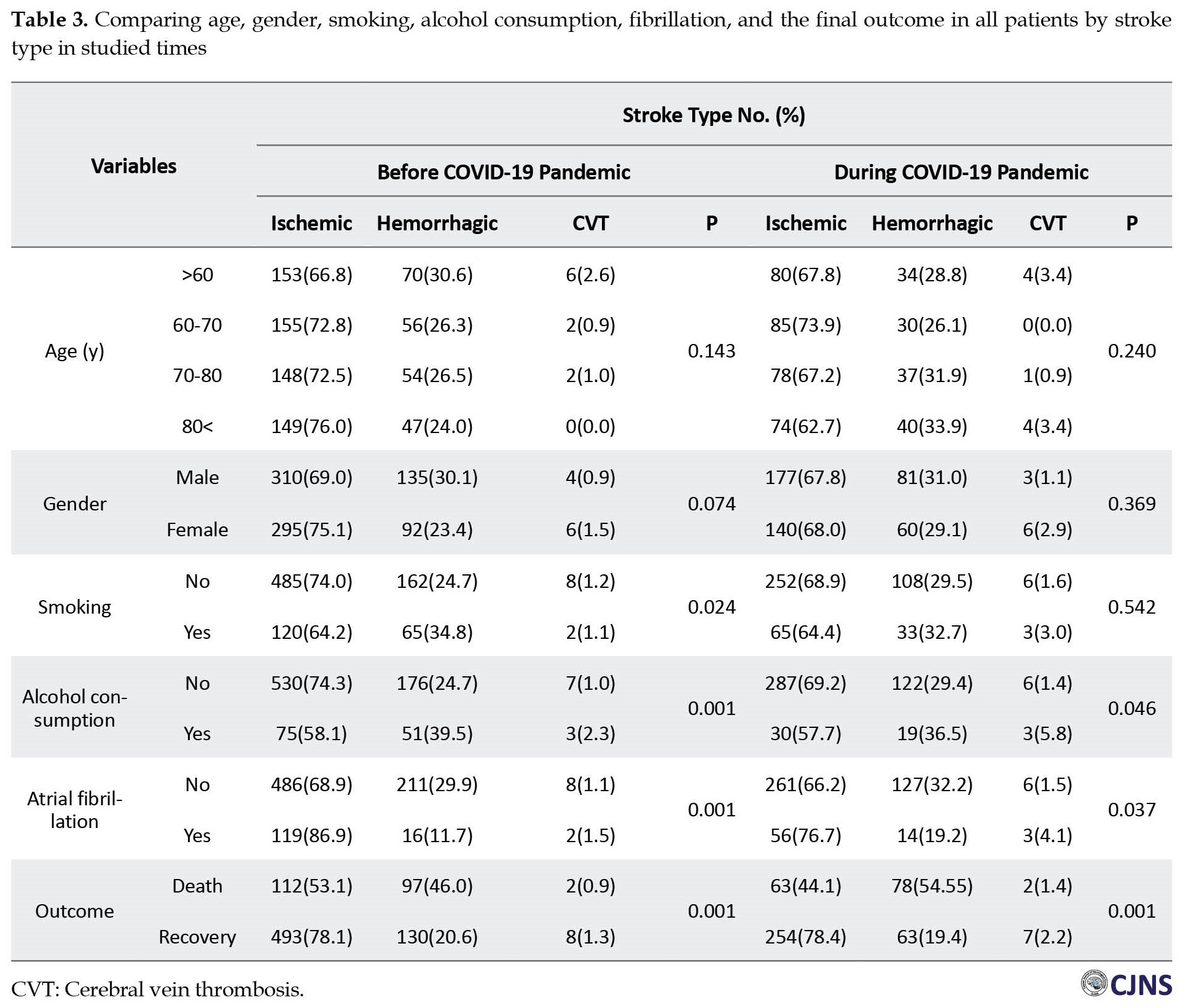
Alcohol consumption was associated with the frequency of IPH in both periods (P<0.05). The frequency of atrial fibrillation had a significant difference between IS, IPH, and CVT patients in both study times, including the COVID-19 pandemic period (P=0.037) and the similar period in the previous year (P<0.001). Furthermore, we found that CVT incidence among patients with atrial fibrillation comorbidity was 4.1% compared with patients without atrial fibrillation (1.5%) during the COVID-19 pandemic.
The frequencies of all admitted patients (IS, IPH, and CVT) according to the outcome (death or recovery) were significant (P<0.001) between both periods of the study. Also, the mortality rate of patients due to IPH stroke was higher than that of IS in both study periods.
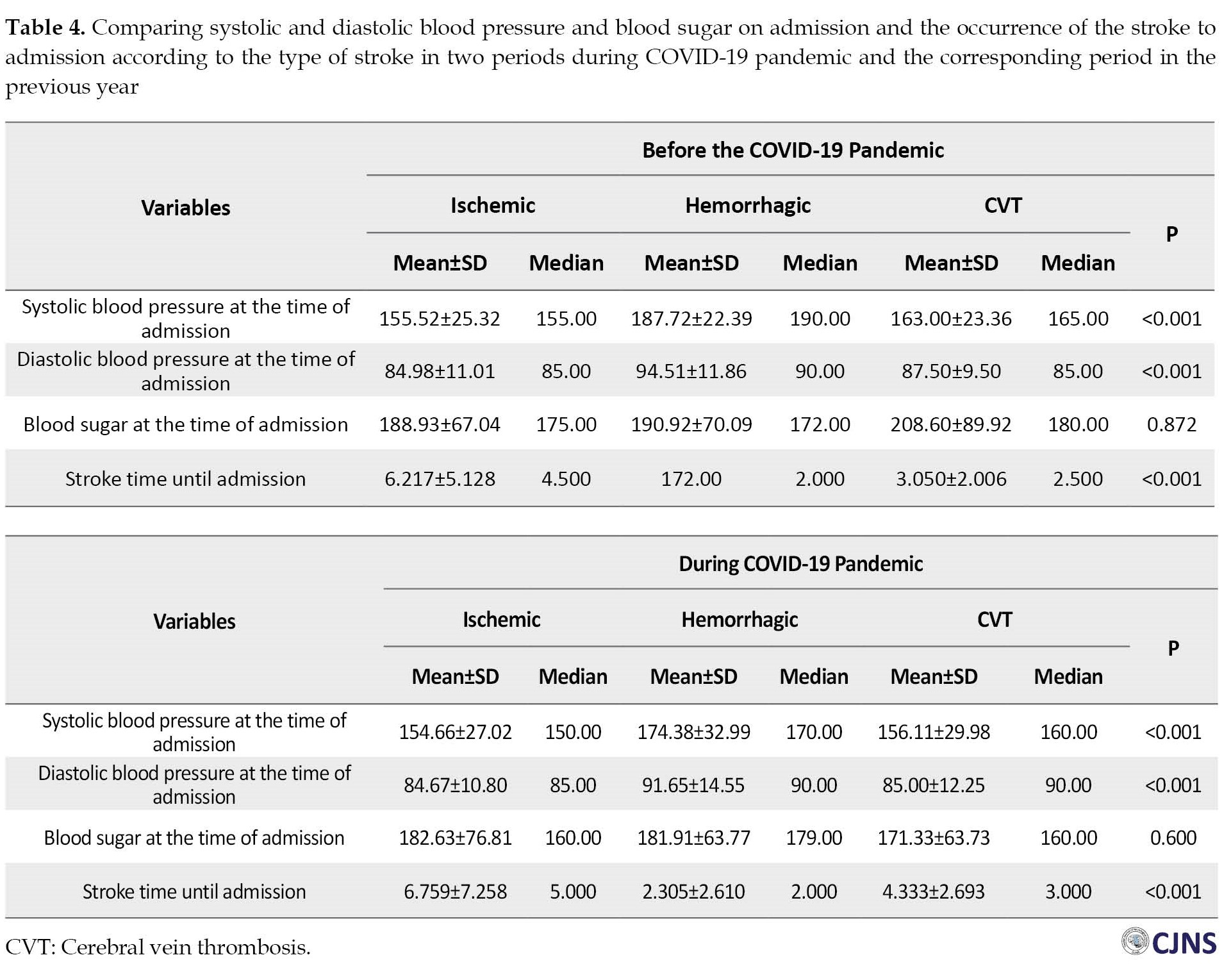
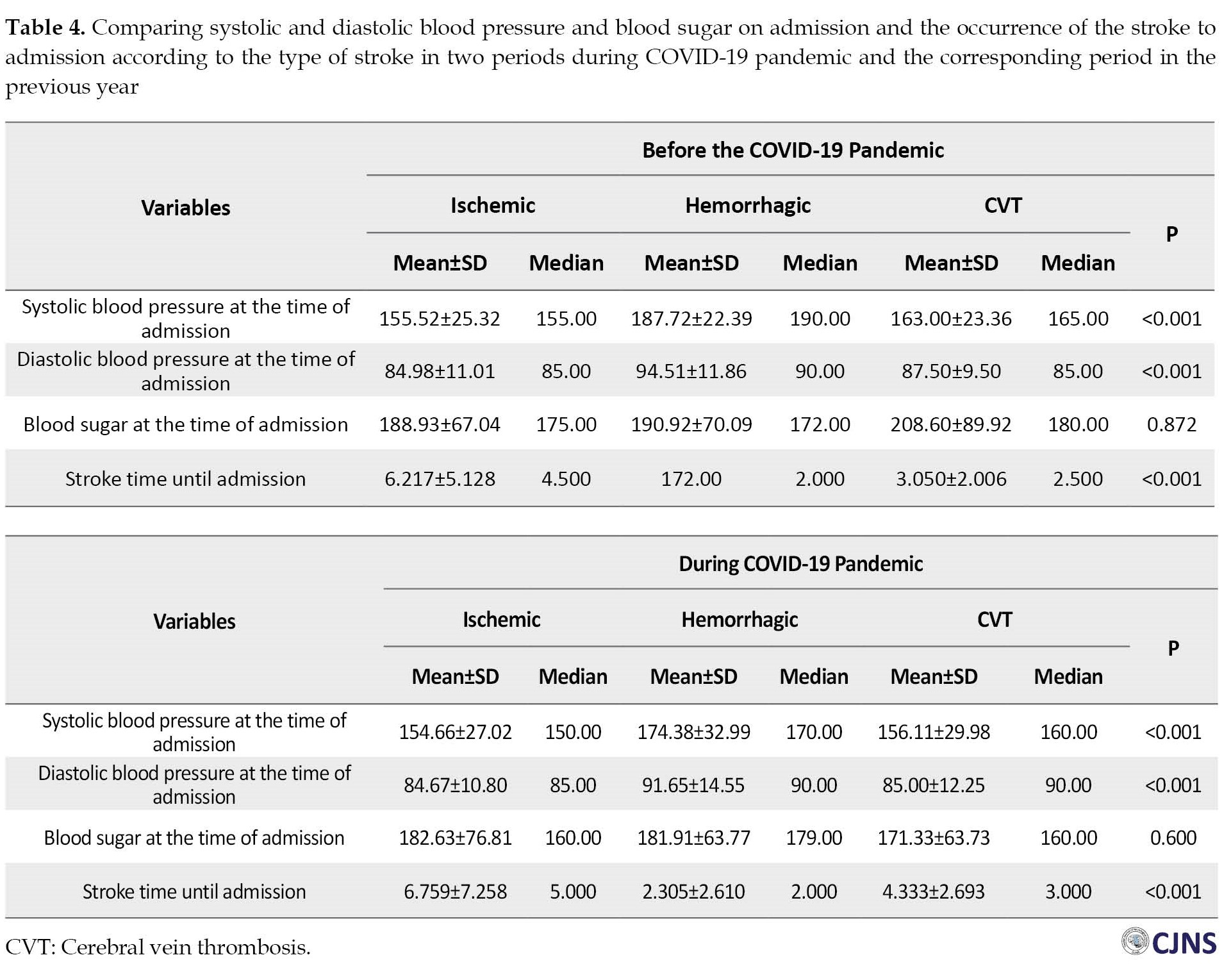
According to Table 4, the IPH patients showed higher systolic and diastolic blood pressure (at admission time) compared with patients suffering from IS stroke and CVT in both study periods (P<0.001).
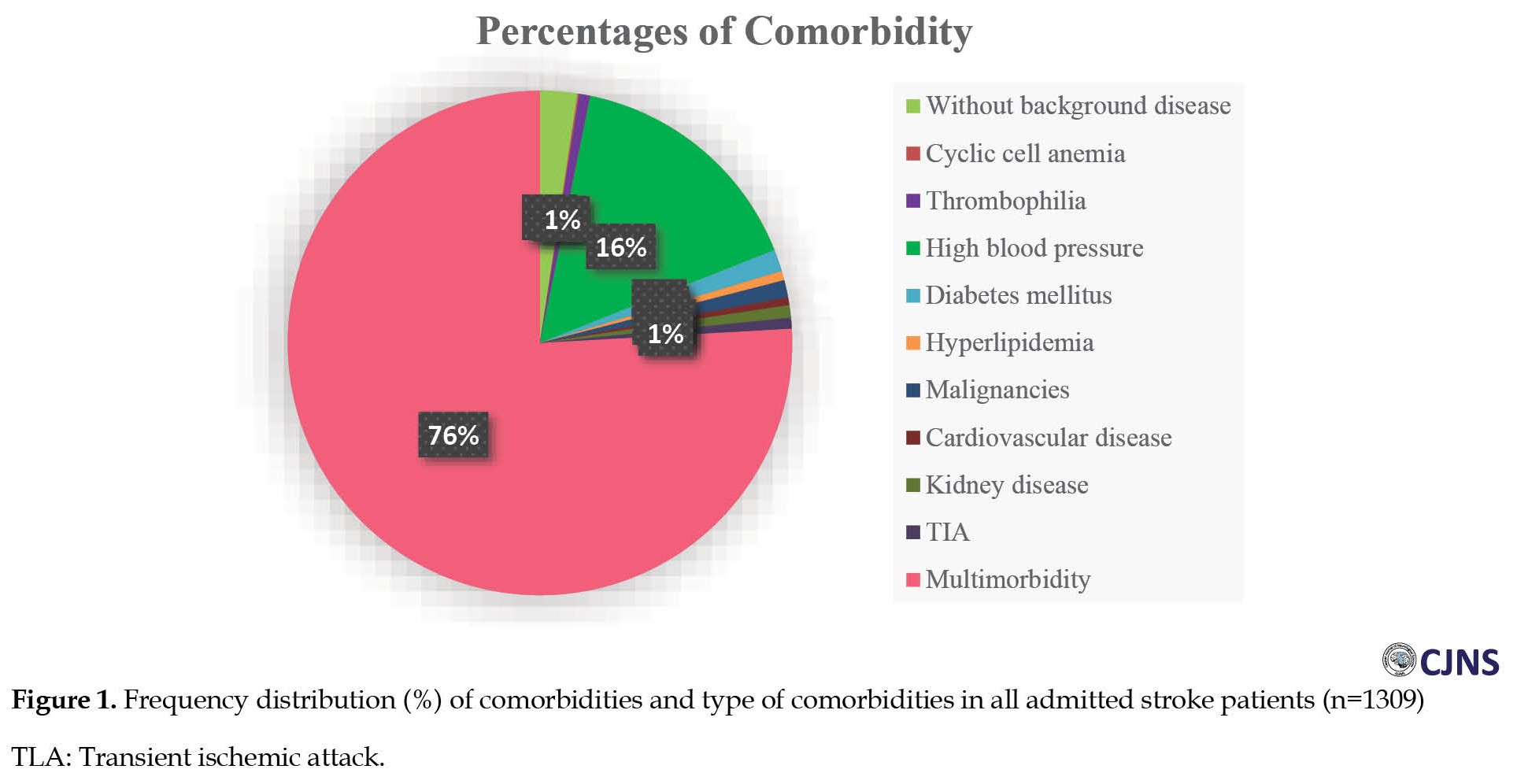
This study showed that most cases (97.6%) had comorbidity (Figure 1).
Globally, stroke is ranked as the most common cause of death and disability. It is categorized into two major types: ischemic and hemorrhagic [1]. Ischemic stroke (IS) accounts for approximately 85% of all stroke cases. The prevalence of brain intraparenchymal hemorrhage (IPH) is 10%, leading to 40% mortality in affected middle-aged men [2]. Age, sex, race, sickle cell disease, hypertension, smoking, diabetes, and obesity are the most important risk factors for cerebral IPH [3, 4].
In early February 2020, when the coronavirus disease 2019 (COVID-19) pandemic was declared, it changed the pattern of stroke patient delivery to the healthcare system. Many previous studies reported a global decline in the stroke hospital admission rate during the initial peak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, but the admission frequency of patients with more severe stroke and higher stroke mortality risk increased in several most affected countries [5, 6, 7, 8, 9].
Recent molecular pathological evidence offers respiratory infections as a risk factor in cerebrovascular disease. S protein of SARS-CoV2 has a high affinity for broad endothelial angiotensin-converting enzyme-2 ACE2 receptors, overexpressed in the epithelial cells of the oral and nasal mucosa. Therefore, SARS-CoV-2 easily enters the brain and influences the thalamus and brain stem through the olfactory bulb nerve, eventually leading to nerve damage and affecting the nervous system [10, 11, 12, 13]. Besides, SARS-CoV-2 causes cytokine storm syndrome, which may develop into an acute cerebrovascular disease caused by vascular wall inflammation and vascular smooth muscle necrosis. Patients typically present evidence of neuropathological manifestations in the initial stages of severe infection [14]. Clinical findings have reported various neurological complications such as headache, memory loss, fatal encephalitis, meningitis, stroke, acute cerebrovascular disease, and other major pathologic conditions associated with viral invasion. Furthermore, neurological disorders have been seen in 36% of COVID-19 patients, and 5.9% of cases are associated with stroke [14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25]. In addition, a few studies have demonstrated that SARS-CoV-2 infections are associated with hypoxemia, changes in blood pressure, coagulation status, and C-reactive protein in aged patients, increasing cerebrovascular disease incidence [26]. Hence, we performed a study to appraise the alteration of stroke patterns during the COVID-19 pandemic. This study compared the relative frequencies of IS stroke and IPH among hospitalized patients in Poursina Hospital, Guilan Province, Iran, in two corresponding periods before and during the coronavirus pandemic.
Materials and Methods
This comparative cross-sectional study was conducted to evaluate the relative frequency of patients with acute IS stroke and IPH admitted to the Neurology ward of Poursina Hospital, Guilan, Iran, during the COVID-19 pandemic period between December 2019 and June 2020, and the similar 6-month period in the previous year. Poursina stroke center is the most important academic, public comprehensive stroke unit hospital providing early treatment and rehabilitation care for stroke patients in Guilan, northern Iran. Taking informed consent was not essential because of the retrospective nature of the survey.
Inclusion/exclusion criteria
All patients with acute IS stroke and IPH who had electronic medical records and neuroimaging data (CT scan, MRI) were included in the study. However, we excluded patients with symptoms lasting less than 24 hours, therapeutic anti-thrombolytic, bleeding disorders, head trauma, or brain tumor.
Data extraction
In this study, 1309 patients were included. Two neurologists assessed all patients according to similar stroke guidelines with regard to stroke classification, time of symptom onset, and outcomes (recovery or death).
Clinical assessment
The suspected clinical signs of stroke are hemiparesis or hemianesthesia, altered level of consciousness, speech disturbance, visual disturbances in one or both eyes, impaired standing, or maintaining balance.
Neuroimaging assessment
The brain CT scan is the gold standard for distinguishing between ischemic and hemorrhagic strokes. IPH was first detected as hyperdensity regions in CT scan images, but brain MRI (1.5 Tesla) was also performed to accurately diagnose stroke, especially ischemic stroke.
Based on previous research, patients’ demographic information (age, gender, BMI, level of education, etc.) and comorbidities (diabetes, hypertension, tuberculosis, anemia, history of transient ischemic attack, hyperlipidemia, arrhythmia, congestive heart failure, coronary heart disease, smoking history, alcohol consumption, etc.) were collected.
Statistical
Data analysis was done with the statistical package social sciences SPSS software, version 21 (IBM Corp. Armonk, NY, USA). The frequency distribution and a 95% confidence interval (CI) were used to determine the relative frequency of strokes in the two study periods. The IS to IPH stroke ratio was evaluated based on average and 95% CI. The regression logistic statistical method was used to compare the frequency distribution of IS and IPH strokes after controlling for the effects of age, sex, and other intervening variables. In this study, P<0.05 was considered the significance level of the tests.
Results
In this study, 1309 patients were included. The frequency of stroke patients admitted to Poursina Hospital during the COVID-19 pandemic (December 22, 2019, to June 20, 2020) was 467 cases (35.68%) compared to 842 cases (64.32%) during the corresponding period in the previous year. Thus, the percentage of stroke patients admitted during the COVID-19 pandemic had a 28.6% decline compared with the same time last year. This difference was statistically significant (P<0.001).
According to the results, 70.4%, 28.1%, and 1.5% of all patients were IS, IPH, and cerebral venous thrombosis (CVT), respectively. The frequency of admission of stroke patients through the SARS-CoV-2 pandemic was 67.9% for IS, 30.2% for IPH, and 1.9% for CVT, while these percentages were 71.9%, 27%, and 1.2% in a similar period in the prior year, respectively. The comparison between the percentages of IS, IPH, and CVT admission patients in two study periods based on the chi-square test was not significant (P=0.232). Furthermore, the ratio of stroke IS to stroke IPH declined from 2.6 in the corresponding period in the previous year to 2.2 during the SARS-CoV-2 pandemic period (Table 1).
There was no significant difference in smoking (P=0.808) or the number of cigarettes packs (P=0.365) between the two time periods in the referring patients, but the frequency of alcohol consumption declined (P=0.036) in the COVID-19 pandemic (11.13%) compared to the same period the previous year (15.3%) (Table 2).

The frequency of alcohol consumption during the COVID-19 pandemic (P<0.05) and the same period in the previous year (P<0.001) have significant differences (Table 3).
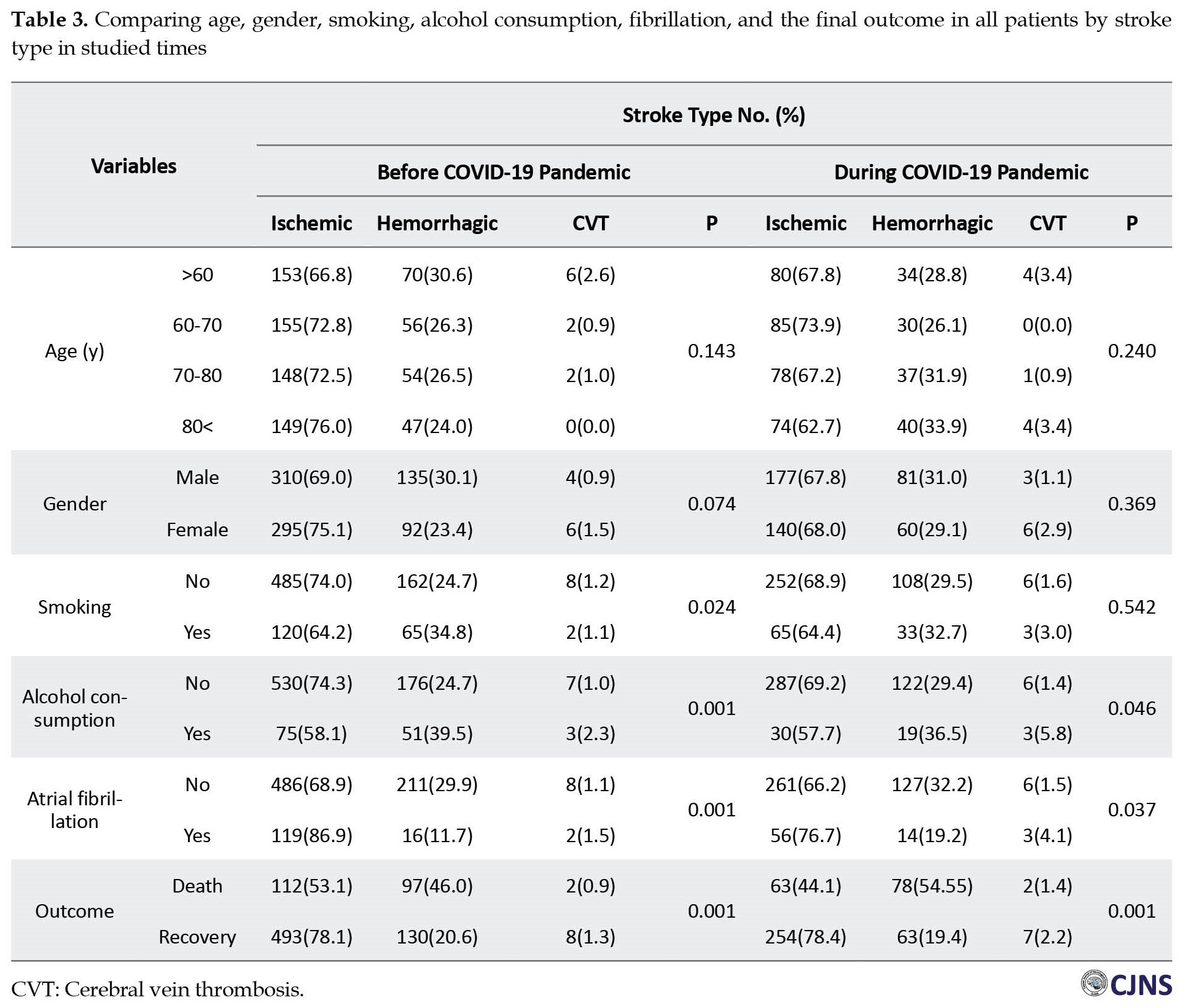
Alcohol consumption was associated with the frequency of IPH in both periods (P<0.05). The frequency of atrial fibrillation had a significant difference between IS, IPH, and CVT patients in both study times, including the COVID-19 pandemic period (P=0.037) and the similar period in the previous year (P<0.001). Furthermore, we found that CVT incidence among patients with atrial fibrillation comorbidity was 4.1% compared with patients without atrial fibrillation (1.5%) during the COVID-19 pandemic.
The frequencies of all admitted patients (IS, IPH, and CVT) according to the outcome (death or recovery) were significant (P<0.001) between both periods of the study. Also, the mortality rate of patients due to IPH stroke was higher than that of IS in both study periods.
According to Table 4, the IPH patients showed higher systolic and diastolic blood pressure (at admission time) compared with patients suffering from IS stroke and CVT in both study periods (P<0.001).
This study showed that most cases (97.6%) had comorbidity (Figure 1).
Multi-morbidity was the highest percentage (75.9%), followed by hypertension (15.8%).
According to Table 5, the percentage of comorbidities during the COVID-19 pandemic was 95.3%, while it was recorded at 98.8% in the corresponding period in the previous year.
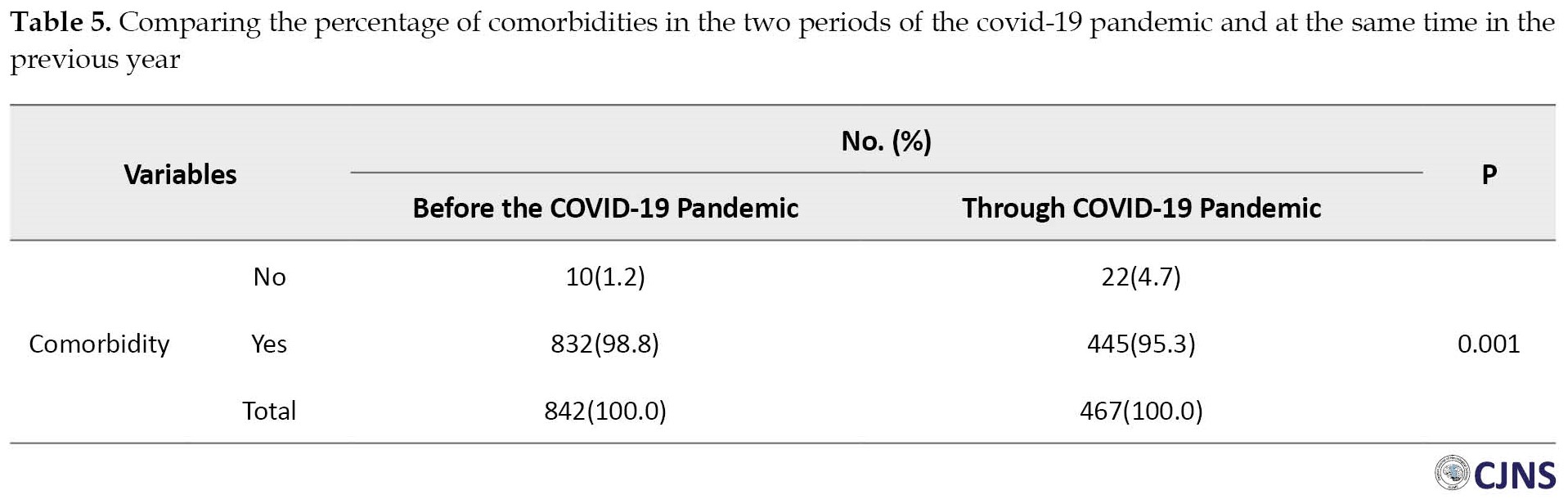
This difference between the two study periods was significant (P<0.001).
Discussion
The current study showed that the frequency of stroke patients significantly declined during the COVID-19 pandemic compared to a similar period in the previous year (before the COVID-19 pandemic) (P<0.001). In contrast, the ratio of IS and IPH stroke between the two study periods was not significantly different (P<0.232). However, it decreased from 2.6 in the corresponding period in the previous year to 2.2 during the SARS-Cov-2 pandemic period. Also, our result showed that the frequency of IPH (3%) and CVT (0.6%) was a bit more increased during the COVID-19 pandemic.
Our results support previous studies with a significant reduction (28.6%) in the relative frequency of stroke admission patients [27]. Similarly, a previous study was done on stroke admission during the COVID-19 pandemic in three European countries (Italy, France, and Germany). According to their study, a marked reduction occurred in the number of patients with stroke, and TIA referred to emergency departments in all three countries [28]. Richter et al. reported a significant reduction in stroke subtype admission during a pandemic and a higher decrease observed during the pandemic’s peak [29]. However, the principal cause of the highest frequency rate of stroke admission (during the pandemic’s first wave) is unknown.
However, the main reason behind this alteration is unclear. Nevertheless, fear of viral invasion, quarantine, and social isolation are some inevitable descriptions in this regard. Thus, COVID-19 pandemic social isolation results, such as fear of exposure to COVID-19 and the popular recommendation to “stay home, save lives,” could cause a remarkable reduction in stroke patients and an altered percentage frequency of IS and IPH strokes during the COVID-19 pandemic. Patients with less severe symptoms were less likely to seek medical attention during the COVID-19 pandemic [30, 31].
In a previous study in the United States, 814 patients with COVID-19 infection were evaluated at 3 Philadelphia hospitals, in which the frequency of patients with IS stroke and intracranial hemorrhage (ICH) was 20(2.4%) and 8(0.9%), respectively. The frequency of ICH subtypes was IPH (63%) and subarachnoid hemorrhage (SAH) (38%), but the changes relative to the non-pandemic period have not been evaluated [32].
In the current study, a significant relationship (P<0.001) was found between stroke time until admission and stroke time on admission (Table 4). Patients with IPH and CVT are referred to the emergency department quickly. However, the time until admission was far greater for patients with ischemic stroke. Probably, ischemic patients with mild to moderate signs live much longer than patients with severe symptoms. Stroke time until admission was significant in both main study periods [7].
Predominantly, the prevalence and incidence of stroke significantly correlate with some hazard factors and comorbidities (such as hypertension, diabetes mellitus, arterial fibrillation, smoking, alcohol consumption, and age). According to Table 2 we evaluated stroke risk factors in hospital-admitted stroke cases in both study periods. We found that age, gender, and smoking did not affect the percentage frequency of stroke patients in both study periods. Similar to previous studies, alcohol consumption was significant in both study periods and strongly associated with stroke incidence. Besides, we observed that alcohol consumption declined among stroke patients during the COVID-19 pandemic. This reduction was probably due to restricted social gatherings or becoming aware of ethanol’s destructive effect on the immune system. The impact of comorbidities on the frequency distributions of IS and IPH strokes and CVT was not significant (Table 5). However, a significant decline was observed in the percentage of comorbidities during the COVID-19 pandemic (95.3%) compared with the same time last year (98.8%).
Conclusion
The COVID-19 infection is spreading quickly. Unfortunately, cerebrovascular complications are common in COVID-19, so understanding the clinical and diagnostic presentations should be updated. Social isolation due to the fear of contracting COVID-19 disease in healthcare centers could be the reason for the decline in ischemic stroke patients. Our study showed the frequency of stroke patients significantly decreased during the COVID-19 pandemic, while the difference between IS stroke and IPH frequency in both study periods was not significant.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki (2013). The study protocol was approved by the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.140).
Funding
This article extracted from Zahra Adineh thesis registered at the Neurosciences Research Center, Guilan University of Medical Sciences (Code: 1166).
Authors contributions
Conceptualization, design and supervision: Shahrokh Yousefzadeh-Chabok and Amir Reza Ghayeghran; Data collection: Zahra Adineh; Data analysis and data interpretation: Ehsan Kazemnejad-Leili; Drafting and editing of the manuscript: Khatereh Asadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We acknowledge the assistance of all involved physicians, nurses, staff, and medical students of the Department of Neurology at Poursina Academic Hospital.
According to Table 5, the percentage of comorbidities during the COVID-19 pandemic was 95.3%, while it was recorded at 98.8% in the corresponding period in the previous year.
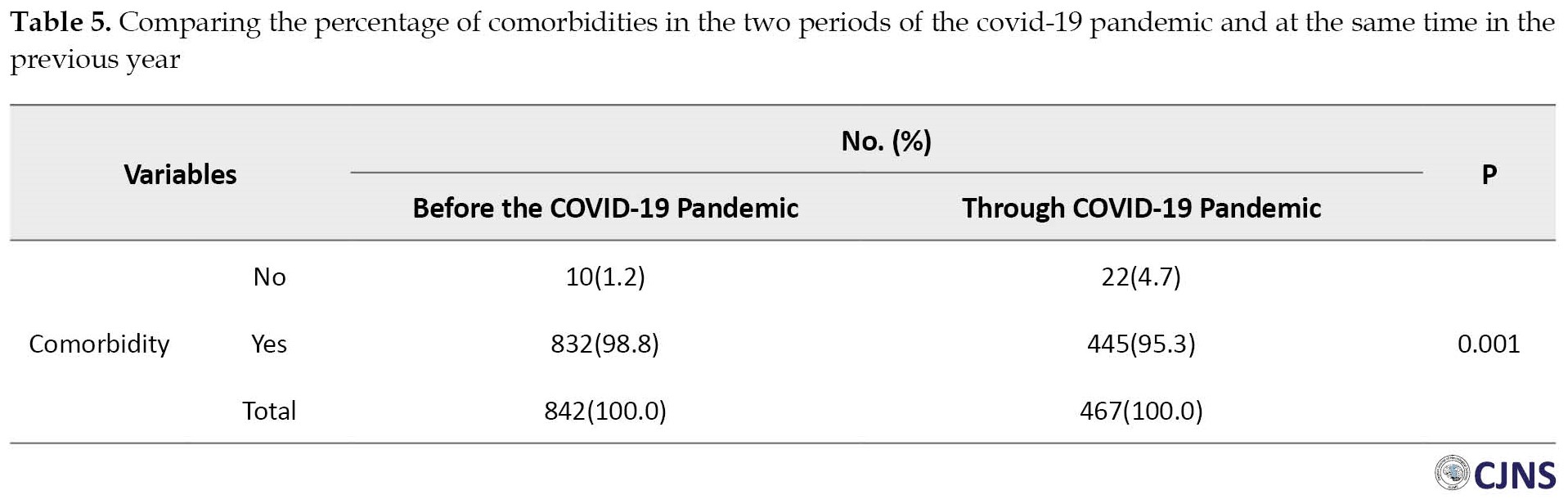
This difference between the two study periods was significant (P<0.001).
Discussion
The current study showed that the frequency of stroke patients significantly declined during the COVID-19 pandemic compared to a similar period in the previous year (before the COVID-19 pandemic) (P<0.001). In contrast, the ratio of IS and IPH stroke between the two study periods was not significantly different (P<0.232). However, it decreased from 2.6 in the corresponding period in the previous year to 2.2 during the SARS-Cov-2 pandemic period. Also, our result showed that the frequency of IPH (3%) and CVT (0.6%) was a bit more increased during the COVID-19 pandemic.
Our results support previous studies with a significant reduction (28.6%) in the relative frequency of stroke admission patients [27]. Similarly, a previous study was done on stroke admission during the COVID-19 pandemic in three European countries (Italy, France, and Germany). According to their study, a marked reduction occurred in the number of patients with stroke, and TIA referred to emergency departments in all three countries [28]. Richter et al. reported a significant reduction in stroke subtype admission during a pandemic and a higher decrease observed during the pandemic’s peak [29]. However, the principal cause of the highest frequency rate of stroke admission (during the pandemic’s first wave) is unknown.
However, the main reason behind this alteration is unclear. Nevertheless, fear of viral invasion, quarantine, and social isolation are some inevitable descriptions in this regard. Thus, COVID-19 pandemic social isolation results, such as fear of exposure to COVID-19 and the popular recommendation to “stay home, save lives,” could cause a remarkable reduction in stroke patients and an altered percentage frequency of IS and IPH strokes during the COVID-19 pandemic. Patients with less severe symptoms were less likely to seek medical attention during the COVID-19 pandemic [30, 31].
In a previous study in the United States, 814 patients with COVID-19 infection were evaluated at 3 Philadelphia hospitals, in which the frequency of patients with IS stroke and intracranial hemorrhage (ICH) was 20(2.4%) and 8(0.9%), respectively. The frequency of ICH subtypes was IPH (63%) and subarachnoid hemorrhage (SAH) (38%), but the changes relative to the non-pandemic period have not been evaluated [32].
In the current study, a significant relationship (P<0.001) was found between stroke time until admission and stroke time on admission (Table 4). Patients with IPH and CVT are referred to the emergency department quickly. However, the time until admission was far greater for patients with ischemic stroke. Probably, ischemic patients with mild to moderate signs live much longer than patients with severe symptoms. Stroke time until admission was significant in both main study periods [7].
Predominantly, the prevalence and incidence of stroke significantly correlate with some hazard factors and comorbidities (such as hypertension, diabetes mellitus, arterial fibrillation, smoking, alcohol consumption, and age). According to Table 2 we evaluated stroke risk factors in hospital-admitted stroke cases in both study periods. We found that age, gender, and smoking did not affect the percentage frequency of stroke patients in both study periods. Similar to previous studies, alcohol consumption was significant in both study periods and strongly associated with stroke incidence. Besides, we observed that alcohol consumption declined among stroke patients during the COVID-19 pandemic. This reduction was probably due to restricted social gatherings or becoming aware of ethanol’s destructive effect on the immune system. The impact of comorbidities on the frequency distributions of IS and IPH strokes and CVT was not significant (Table 5). However, a significant decline was observed in the percentage of comorbidities during the COVID-19 pandemic (95.3%) compared with the same time last year (98.8%).
Conclusion
The COVID-19 infection is spreading quickly. Unfortunately, cerebrovascular complications are common in COVID-19, so understanding the clinical and diagnostic presentations should be updated. Social isolation due to the fear of contracting COVID-19 disease in healthcare centers could be the reason for the decline in ischemic stroke patients. Our study showed the frequency of stroke patients significantly decreased during the COVID-19 pandemic, while the difference between IS stroke and IPH frequency in both study periods was not significant.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki (2013). The study protocol was approved by the Guilan University of Medical Sciences (Code: IR.GUMS.REC.1399.140).
Funding
This article extracted from Zahra Adineh thesis registered at the Neurosciences Research Center, Guilan University of Medical Sciences (Code: 1166).
Authors contributions
Conceptualization, design and supervision: Shahrokh Yousefzadeh-Chabok and Amir Reza Ghayeghran; Data collection: Zahra Adineh; Data analysis and data interpretation: Ehsan Kazemnejad-Leili; Drafting and editing of the manuscript: Khatereh Asadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We acknowledge the assistance of all involved physicians, nurses, staff, and medical students of the Department of Neurology at Poursina Academic Hospital.
References
- Neves G, Cole T, Lee J, Bueso T, Shaw C, Montalvan V. Demographic and institutional predictors of stroke hospitalization mortality among adults in the United States. eNeurologicalSci. 2022; 26:100392. [DOI:10.1016/j.ensci.2022.100392] [PMID] [PMCID]
- Rymer MM. Hemorrhagic stroke: Intracerebral hemorrhage. Mo Med. 2011; 108(1):50-4. [PMID] [PMCID]
- An SJ, Kim TJ, Yoon BW. Epidemiology, risk factors, and clinical features of intracerebral hemorrhage: An update. J Stroke. 2017; 19(1):3-10. [DOI:10.5853/jos.2016.00864] [PMID] [PMCID]
- Ascanio LC, Maragkos GA, Young BC, Boone MD, Kasper EM. Spontaneous intracranial hemorrhage in pregnancy: A systematic review of the literature. Neurocrit Care. 2019; 30(1):5-15. [DOI:10.1007/s12028-018-0501-4] [PMID]
- Sedova P, Kent JA, Bryndziar T, Jarkovsky J, Tomek A, Sramek M, et al. The decline in stroke hospitalization due to COVID-19 is unrelated to COVID-19 intensity. Eur J Neurol. 2023; 30(4):943-50. [DOI:10.1111/ene.15664] [PMID] [PMCID]
- Richter D, Eyding J, Weber R, Bartig D, Grau A, Hacke W, et al. Analysis of nationwide stroke patient care in times of COVID-19 pandemic in Germany. Stroke. 2021; 52(2):716-21. [DOI:10.1161/STROKEAHA.120.033160] [PMID] [PMCID]
- Tavanaei R, Yazdani KO, Akhlaghpasand M, Zali A, Oraee-Yazdani S. Changed pattern of hospital admission in stroke during COVID-19 pandemic period in Iran: A retrospective study. Neurol Sci. 2021; 42(2):445-53. [DOI:10.1007/s10072-020-05030-z] [PMID] [PMCID]
- White TG, Martinez G, Wang J, Gribko M, Boltyenkov A, Arora R, et al. Impact of the COVID-19 pandemic on acute ischemic stroke presentation, treatment, and outcomes. Stroke Res Treat. 2021; 2021:8653396. [DOI:10.1155/2021/8653396] [PMID] [PMCID]
- Akhtar N, Kamran S, Al-Jerdi S, Imam Y, Joseph S, Morgan D, et al. Trends in stroke admissions before, during and post-peak of the COVID-19 pandemic: A one-year experience from the Qatar stroke database. Plos One. 2022; 17(3):e0255185. [DOI:10.1371/journal.pone.0255185] [PMID] [PMCID]
- Sarubbo F, El Haji K, Vidal-Balle A, Bargay Lleonart J. Neurological consequences of COVID-19 and brain related pathogenic mechanisms: A new challenge for neuroscience. Brain Behav Immun Health. 2022; 19:100399. [DOI:10.1016/j.bbih.2021.100399] [PMID] [PMCID]
- Siegler JE, Abdalkader M, Michel P, Nguyen TN. Therapeutic trends of cerebrovascular disease during the COVID-19 pandemic and future perspectives. J Stroke. 2022; (2):179-88.[DOI:10.5853/jos.2022.00843] [PMID] [PMCID]
- Asadi K, Gholami A. Virosome-based nanovaccines; a promising bioinspiration and biomimetic approach for preventing viral diseases: A review. Int J Biol Macromol. 2021; 182:648-58. [DOI:10.1016/j.ijbiomac.2021.04.005] [PMID] [PMCID]
- Avula A, Nalleballe K, Narula N, Sapozhnikov S, Dandu V, Toom S, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020; 87:115-9. [DOI:10.1016/j.bbi.2020.04.077] [PMID] [PMCID]
- Thepmankorn P, Bach J, Lasfar A, Zhao X, Souayah S, Chong ZZ, et al. Cytokine storm induced by SARS-CoV-2 infection: The spectrum of its neurological manifestations. Cytokine. 2021; 138:155404. [DOI:10.1016/j.cyto.2020.155404][PMID] [PMCID]
- Li Y, Li M, Wang M, Zhou Y, Chang J, Xian Y, et al. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke Vasc Neurol. 2020; 5(3):279-84. [DOI:10.1136/svn-2020-000431] [PMID] [PMCID]
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020; 395(10229):1054-62. [DOI:10.1016/S0140-6736(20)30566-3] [PMID] [PMCID]
- McEntire CRS, Song KW, McInnis RP, Rhee JY, Young M, Williams E, et al. Neurologic manifestations of the world health organization's list of pandemic and epidemic diseases. Front Neurol. 2021; 12:634827. [DOI:10.3389/fneur.2021.634827] [PMID] [PMCID]
- Shahjouei S, Naderi S, Li J, Khan A, Chaudhary D, Farahmand G, et al. Risk of stroke in hospitalized SARS-CoV-2 infected patients: A multinational study. EBioMedicine. 2020; 59:102939.9 [DOI:10.1016/j.ebiom.2020.102939] [PMID] [PMCID]
- Saberi A, Ghayeghran A, Hatamian H, Hosseini-Nejad M, Bakhshayesh Eghbali B. COVID-19-associated myelitis, para/post infectious or infectious myelitis: A case report from the north of Iran. Caspian J Neurol Sci. 2020; 6(2):132-8 [DOI:10.32598/cjns.6.21.1]
- Shahjouei S, Tsivgoulis G, Farahmand G, Koza E, Mowla A, Vafaei Sadr A, et al. SARS-CoV-2 and stroke characteristics: A report from the multinational COVID-19 stroke study group. Stroke. 2021; 52(5):e117-30. [DOI:10.1161/STROKEAHA.120.032927]
- Shahjouei S, Anyaehie M, Koza E, Tsivgoulis G, Naderi S, Mowla A, et al. SARS-CoV-2 is a culprit for some, but not all acute ischemic strokes: A report from the multinational COVID-19 stroke study group. J Clin Med. 2021; 10(5):931.[DOI:10.3390/jcm10050931] [PMID] [PMCID]
- Alijani B, Saberi A, Niyasti P, Dogahe M. Transverse myelitis following covid-19 infection. What is the mechanism? A case report and literature review. Rom J Neurol. 2021; 20(2):255-63. [DOI:10.37897/RJN.2021.2.22]
- Kazemi S, Pourgholaminejad A, Saberi A. Stroke associated with SARS-CoV-2 infection and its pathogenesis: A systematic review. Basic Clin Neurosci. 202; 12(5):569-86.[DOI:10.32598/bcn.2021.3277.1] [PMID] [PMCID]
- Pourgholaminejad A, Kazemi S, Saberi A. Virology, pathophysiology and neuroinvasion mechanisms of SARS-CoV-2: A mini literature review. Rom J Neurol. 2021; 20(3):288-91. [DOI:10.37897/RJN.2021.3.3]
- Besharati A, Saberi A, Ghorbani Shirkouhi S, Ashraf A, Hatamian H, Eslami Kenarsari H, et al. Guillain-Barré syndrome during the COVID-19 pandemic and pre-pandemic periods. Caspian J Neurol Sci. 2022; 8(1):33-8. [DOI:10.32598/CJNS.8.28.213.2]
- Siepmann T, Sedghi A, Barlinn J, de With K, Mirow L, Wolz M, et al. Association of history of cerebrovascular disease with severity of COVID-19. J Neurol. 2021; 268(3):773-84. [DOI:10.1007/s00415-020-10121-0] [PMID] [PMCID]
- Van Dusen RA, Abernethy K, Chaudhary N, Paudyal V, Kurmi O. Association of the COVID-19 pandemic on stroke admissions and treatment globally: A systematic review. BMJ Open. 2023; 13(3):e062734. [DOI:10.1136/bmjopen-2022-062734] [PMID] [PMCID]
- Bersano A, Kraemer M, Touzé E, Weber R, Alamowitch S, Sibon I, et al. Stroke care during the COVID-19 pandemic: Experience from three large European countries. Eur J Neurol. 2020; 27(9):1794-800. [DOI:10.1111/ene.14375] [PMID] [PMCID]
- Richter D, Eyding J, Weber R, Bartig D, Grau A, Hacke W, et al. A full year of the COVID-19 pandemic with two infection waves and its impact on ischemic stroke patient care in Germany. Eur J Neurol. 2022; 29(1):105-13. [DOI:10.1111/ene.15057] [PMID] [PMCID]
- Libruder C, Ram A, Hershkovitz Y, Tanne D, Bornstein NM, Leker RR,et al. Reduction in acute stroke admissions during the COVID-19 pandemic: Data from a national stroke registry. Neuroepidemiology. 2021; 55(5):354-60. [DOI:10.1159/000516753] [PMID] [PMCID]
- Rothstein A, Oldridge O, Schwennesen H, Do D, Cucchiara BL. Acute cerebrovascular events in hospitalized COVID-19 patients. Stroke. 2020; 51(9):e219-22. [DOI:10.1161/STROKEAHA.120.030995] [PMID] [PMCID]
- Wang J, Chaudhry SA, Tahsili-Fahadan P, Altaweel LR, Bashir S, Bahiru Z, et al. The impact of COVID-19 on acute ischemic stroke admissions: Analysis from a community-based tertiary care center. J Stroke Cerebrovasc Dis. 2020; 29(12):105344. [DOI:10.1016/j.jstrokecerebrovasdis.2020.105344] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |