Sat, May 18, 2024
Volume 9, Issue 3 (Summer 2023)
Caspian J Neurol Sci 2023, 9(3): 143-153 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Safarionpur K, Zebardast A, Saberi A. Effectiveness of Behavior Management Intervention in Migraine With a Focus on Comorbid Depressive Symptoms. Caspian J Neurol Sci 2023; 9 (3) :143-153
URL: http://cjns.gums.ac.ir/article-1-638-en.html
URL: http://cjns.gums.ac.ir/article-1-638-en.html
1- Department of Psychology, Faculty of Literature and Humanities, University of Guilan, Rasht, Iran.
2- Department of Neurology, Faculty of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Neurology, Faculty of Medicine, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 1495 kb]
(262 Downloads)
| Abstract (HTML) (689 Views)
Full-Text: (163 Views)
Introduction
Migraine is a headache disorder characterized by clinical symptoms such as throbbing and pulsating attacks [1]. According to the World Health Organization (WHO), migraine is the third most common disease, affecting approximately one billion people worldwide [2]. The global prevalence of migraine is 11.6%, affecting nearly 1 in 10 people worldwide [3].Migraine is associated with a high prevalence of psychological comorbidities such as depression, anxiety, personality disorders, obsessions, and sleep disorders [4].Migraine-associated comorbidities are risk factors for developing episodic to chronic migraines [5]. The most common comorbidity with migraine is depression [6].There is a bidirectional relationship between depression and migraine [7], i.e. the risk of migraine is tripled by depression, and vice versa. However, the basic mechanism of this relationship is still poorly understood [8].
Notably, migraine treatment interventions usually focus on examining migraine indicators, including the intensity, duration, and frequency of attacks. Although diagnosis and treatment of migraine-related disabilities are necessary for achieving effective clinical outcomes, these issues are not the focus of interest for researchers and healthcare specialists [9]. Migraine-related disabilities refer to patients’ inability to perform activities they would have been able to do easily without a migraine [10]. According to the global burden of disease (GBD), migraine is the second leading cause of years lost due to disability (YLD), which dramatically disrupts a person’s social, familial, and personal roles [11]. People with migraine also carry an additional psychological burden due to fear of the next attack and difficulty planning [12].
In recent years, nonpharmacological treatment approaches have been used independently or in combination with pharmacological approaches to treat various types of migraine [13]. Research suggests that a combination of pharmacological and psychological therapeutic approaches is more effective than either approach alone [14]. With a therapeutic effectiveness of 35%-55%, the American Academy of Neurology proposed the behavior management approach as the most effective psychological approach to reduce migraine-related disabilities [15]. The behavior management approach focuses on observable behaviors and replaces ineffective behaviors with effective habits and behaviors [16]. Behavior management therapies used to treat migraine patients are primarily aimed at reducing the frequency and intensity of pain, reducing migraine-related disabilities, controlling disease progression, improving patients’ quality of life, reducing dependence on medications, and increasing treatment adherence [14]. Although research has confirmed the positive impact of the behavior management approach on migraine patients, it has failed to treat 62% of migraine patients with comorbid depression or has even worsened their condition in the long term [17]. Authors of a meta-analysis argued that some psychotherapeutic approaches could help prevent and control migraine by facilitating the management and regulation of triggers such as stress, emotional experience, sleep, and some comorbid symptoms [18]. Lipton et al. have concluded that recognizing comorbid depressive symptoms influences appropriate medication selection and treatment adherence in migraine patients [19]. In addition, addressing the comorbidity of migraine and depression in the treatment process can increase the response rate and accelerate the recovery process [20]. Peck et al. report that behavior therapy and preventive pharmacotherapy can effectively treat patients with mild to moderate depression and severe migraine [21].
Few studies have examined the effectiveness of different therapeutic approaches in treating migraine patients with comorbid depression. There is a huge research gap in the literature in all countries, especially Iran. Accordingly, this study investigated the effectiveness of combined behavior management interventions and pharmacotherapy in reducing migraine-related disabilities and indicators with and without focusing on comorbid depressive symptoms.
Materials and Methods
This quasi-experimental study was conducted using a two-group pre-test & post-test design. The study population consisted of all (male and female) migraine patients with comorbid depressive symptoms referring to neurology clinics in Rasht City, Iran, in 2021. A neurologist and the researcher conducted clinical interviews with the migraine patients and completed relevant questionnaires to identify those with comorbid depressive symptoms. A total of 18 eligible female patients out of 56 were selected as the sample using purposive sampling and randomly (simple randomization) assigned to two groups (n=9) homogenized in terms of age and severity of depression of 56 people who filled out the questionnaire, 34 had at least mild depression. Of them, 22 met all the inclusion criteria and agreed to participate in the intervention. But 4 people did not continue to cooperate when signing the consent form to start the intervention. Enrolled in the study were migraine patients between the ages of 25 and 50 with comorbid depressive symptoms (with the diagnosis of a psychiatrist, based on DSM-5 criteria [22]and Beck’s depression inventory/cut of point=19 [23]). The exclusion criteria included failing to complete the questionnaires (at any stage of the study), receiving any psychological treatment to control migraine or depression during the study, and taking medications other than those prescribed by the neurologist (who collaborated in the study) to control migraine or depression.
Study procedure
In sample selection, due to the restrictions caused by COVID-19, through virtual media, all people who had symptoms of migraine headaches were invited to answer online questionnaires on the diagnostic criteria of migraine (based on ICHD-3 beta) [24] and depression (based on DSM-5 criteria and Beck’s depression inventory/cut of point=19) [22, 23]. Then, those who met the basic conditions were referred to the neurologist’s office for a definitive migraine diagnosis. According to the results of interviews and questionnaires, 22 people who met the inclusion criteria were selected. During the research process, 4 people dropped out, and finally, 18 women remained until the end of the research. In this plan, subjects were placed in two combined treatment groups (drug therapy and behavioral management) after completing the pre-test (migraine disability questionnaire, Beck depression, and one-month monitoring of migraine indicators) and matching based on age and severity of depression. The first group received a combined treatment intervention focusing on the symptoms of depression in their co-workers, and the second group received a combined treatment intervention without focusing on the symptoms of depression in their co-workers provided by the researcher under the supervision of a faculy member in the department of psychology at the University of Guilan. The post-test was taken through the questionnaires above. The intervention was carried out during eight 1-hour sessions (one session per week) and individually to comply with health protocols and social distancing (due to the spread of COVID-19) and to maintain the health of the participants online through video calls using the program WhatsApp was conducted for two months in September and November 2021.
Research tools
Beck’s depression inventory-second edition (BDI-II)
The BDI was published in 1996 by Beck et al. [23]. BDI-II is a 21-item tool that measures the somatic, affective, and cognitive symptoms of depression. Each item includes 4 to 7 statements, and the items are scored on a 4-point Likert scale ranging from no depression to mild depression (score 0) to severe depression (score 3). Respondents must answer questions about their moods and feelings over the past two weeks. The total score is the sum of the scores given to all statements (total score range: 0-63). The scores 0 to 13, 14 to 19, 20 to 28, and 29 to 63, respectively, indicate normal, mild, moderate, and severe levels of depression [23]. According to Beck et al. the internal consistency of the tool ranges between 0.73 and 0.92 (mean=0.86). In addition, the convergent validity of the tool has been obtained as 0.71 using the Hamilton depression rating scale (HDRS). Asghari et al. confirmed the reliability of BDI-II with a Cronbach α value of 0.89 in Iran [25].
Headache disability inventory (HDI)
HDI was designed by Jacobsen et al. to measure the debilitating impacts of headaches on a person’s life [26]. This 25-item tool measures emotional (unpleasant feelings caused by headaches) and functional (personal and social limitations caused by headaches) aspects of disability. The 3-choice items are scored as yes (score 4), sometimes (score 2), and no (score 0). The total score ranges from 0 to 88, with higher scores indicating more severe disabilities. In the Persian version of the scale, items 7, 15, and 22 were recognized as duplicates and removed. HDI has good validity and acceptable reliability. Jacobsen et al. (1994) confirmed the reliability of the tool with a Cronbach α value of 0.83. The concurrent validity of emotional and functional subscales of HDI with SCL-25 has been calculated as 0.79 and -0.91, respectively. The reliability of HDI was confirmed with a Cronbach α value of 0.83 in Iran. In addition, a Cronbach α value of 0.86 was obtained for the two subscales of HDI in a study in Iran [27].
Headache diary (HD)
This researcher-made self-report tool assesses migraine headache indicators, including the intensity, duration, and frequency of attacks. The participants who had already received the necessary training recorded the intensity, duration, and frequency of their migraine attacks every day during a 1-month follow-up before and after the interventions. The intensity of each attack was measured using a 10-point visual analog scale (VAS), a convenient and frequently used tool for measuring perceived pain intensity. On this scale, scores of 0 and 10 represent no pain and the most severe pain, respectively, whereas scores between 1 and 3, 4 to 7, and 8 to 10 correspond to mild, moderate, and severe pain, respectively. Participants were also asked to record the number of hours each attack lasted (duration) and the number of migraine attacks per month (frequency).
Intervention programs
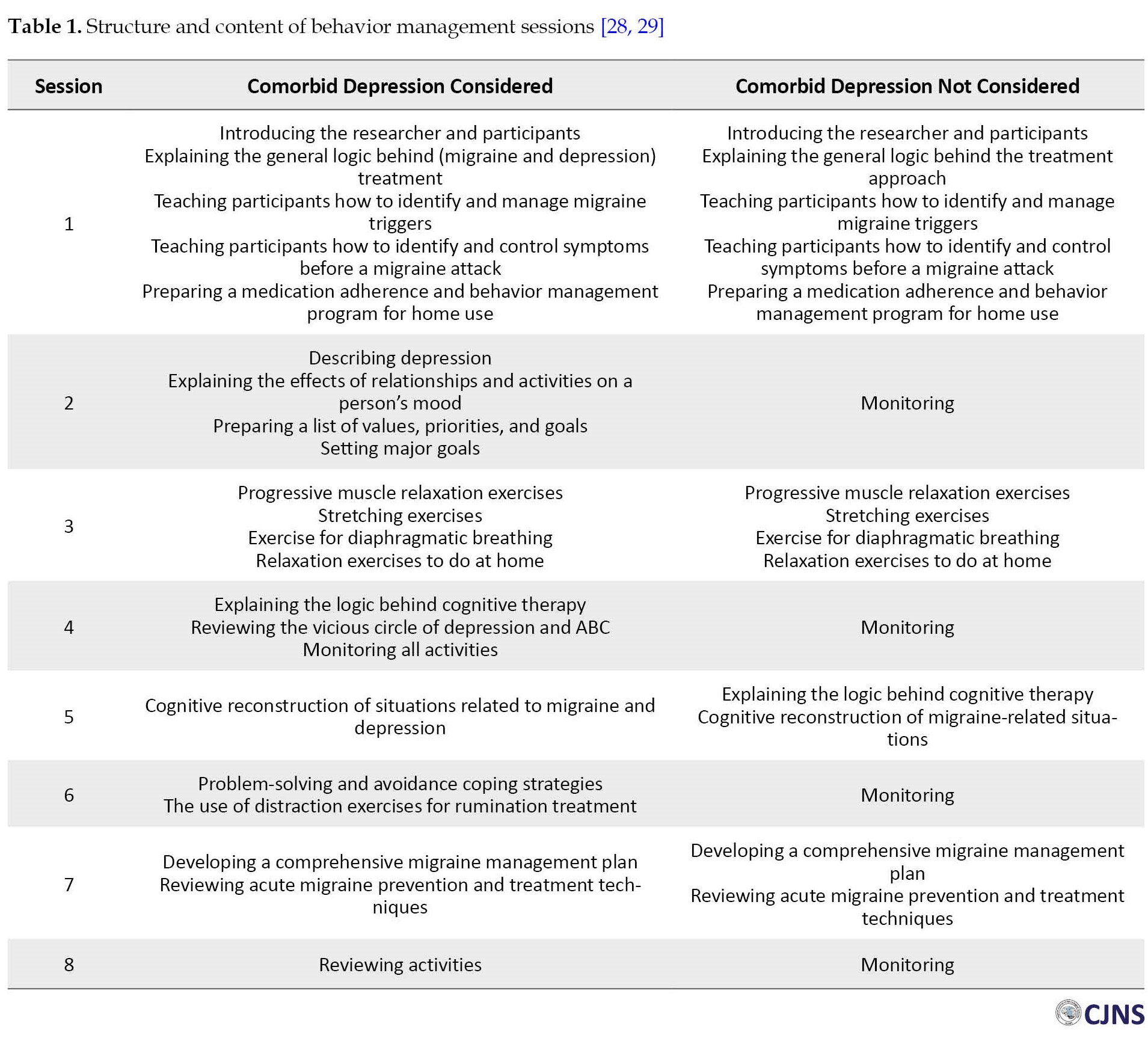
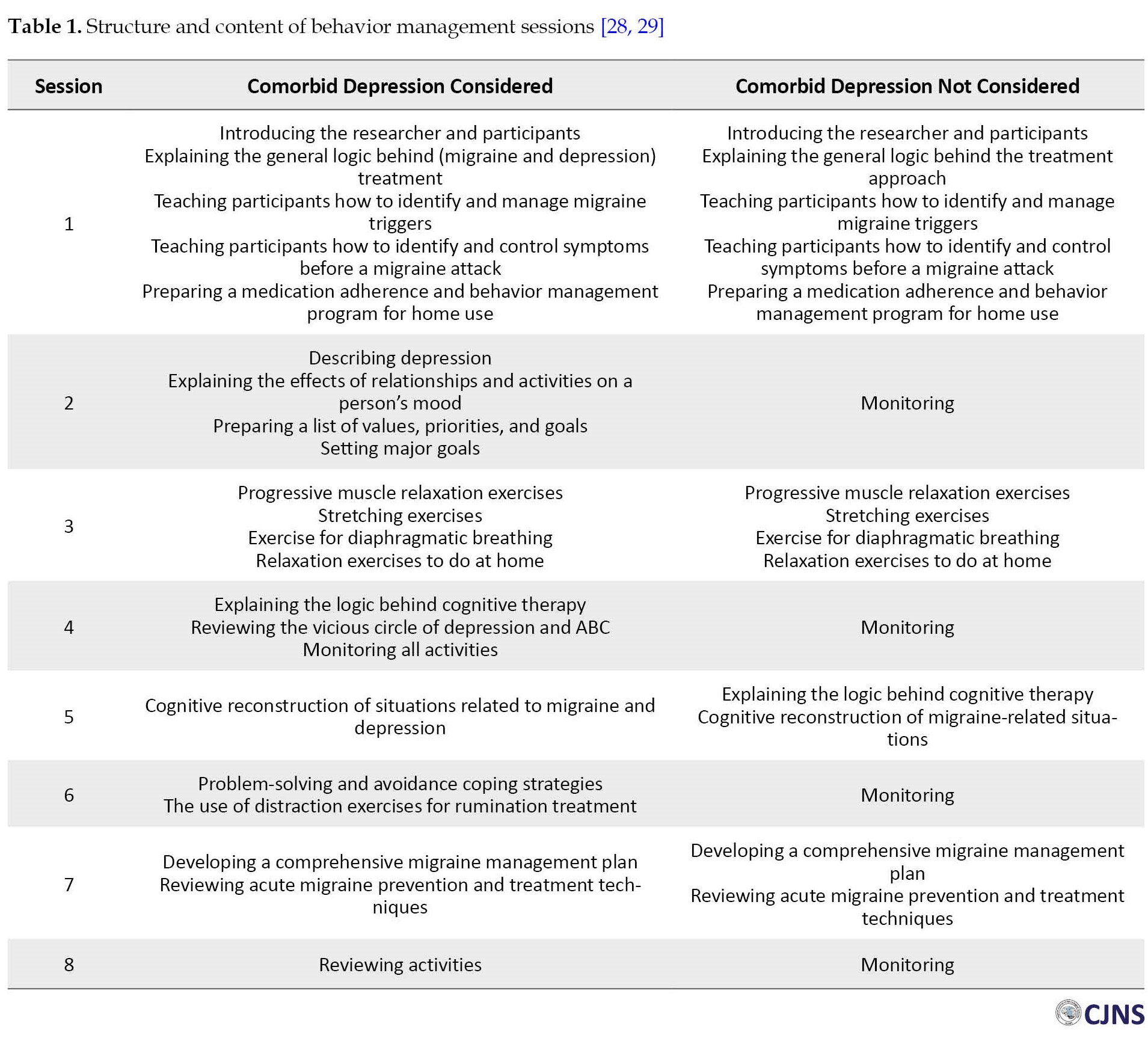
The intervention program to prevent and improve migraine was developed based on Seng’s study and according to behavioral theory [28]. The program to improve comorbid depressive symptoms was designed based on the behavioral activation for depression model developed by Martell et al. [29] (Table 1).
Before the intervention, three experts (two psychologists and one neurologist) confirmed the content validity of the therapeutic methods. The data were analyzed in SPSS software, version 24 using descriptive statistics (Mean±SD) and inferential statistics (paired-sample t-test and multivariate analysis of covariance [MANCOVA]).
Results
The Mean±SD ages of participants in the first intervention group (combined therapy with focusing on comorbid depression) and second intervention group (combined therapy without focusing on comorbid depression) were 32.56±3.67 and 33.78±6.05 years, respectively. The Mean±SD age of all participants was 33.17±4.90 years, with the youngest and oldest participants being 26 and 45 years old, respectively.
According to Table 2, the t value obtained for migraine-related disabilities was 2.96, and the respective level of significance was <0.05.

Thus, given the results of Table 2, the mean score of migraine-related disabilities significantly reduced after the interventions. This finding confirms the effectiveness of the combined therapeutic approach in reducing migraine-related disabilities. In addition, the t value obtained for the variable of migraine indicators was 5.13, and the respective significance level was <0.05. Accordingly, given the results of Table 2, the mean score of the migraine indicator has significantly decreased after the interventions. This finding confirms the effectiveness of the combined therapeutic approach in reducing migraine indicators.
In the following, MANCOVA was employed to investigate the effectiveness of combined behavior management therapy and pharmacotherapy in reducing migraine-related disabilities and indicators with and without focusing on comorbid depressive symptoms. The normality of the data distribution was tested using the Shapiro-Wilk test. P for migraine-related disabilities and migraine indicators (except frequency of attack in the pre-test and post-test stage) were greater than 0.05 before and after the interventions; thus, the data had a normal distribution. Levene’s test was used to assess the assumption of homogeneity of variances in both groups. Since P for all variables of migraine-related disabilities and migraine indicators were greater than 0.05, the assumption of homogeneity of variances was confirmed for all research variables. The results of the box test to check the equality of the covariance matrix of the dependent variables in the two experimental and control groups also showed that the covariance matrix of the dependent variables in the two groups is equal (box M= 0.864, F=0.249, P<0.862); therefore, the data were analyzed using MANCOVA. Multivariate statistical tests were utilized to evaluate the effects of group membership, which revealed a statistically significant difference between the two groups following the interventions concerning at least one dependent variable of migraine-related disabilities or migraine indicators (F(2, 13)=10.43, P<0.05, Wilks Lambda=0.384, partial Ƞ2=0.616).
After the interventions, the F value obtained for the variable of migraine-related disabilities was 8.20, and the respective level of significance was <0.05, indicating a significant difference between the two groups (Table 3).

Hence, a more decrease was observed in the mean score of migraine-related disabilities of participants in the combined therapy focusing on depressive symptoms than those in the second intervention group. About 37% of the difference between the groups regarding migraine-related disabilities was due to interventions in the post-test stage with statistical control of the pre-test scores.
In addition, after the interventions, the F value obtained for the variable of migraine indicators was 9.31, and the respective level of significance was smaller than 0.05, indicating a significant difference between the two groups; thus, a greater decrease in the mean score of migraine indicators was observed among participants in the first intervention group than among those in the second intervention group. Also, 40% of the difference between the groups in terms of migraine indicators was due to interventions in the post-test stage with statistical control of the pre-test scores.
Also, this hypothesis was investigated that combined intervention reduces migraine-related disability and migraine indicators in migraine patients with comorbid depression (in both groups). The results are reported in Tables 4 and 5.
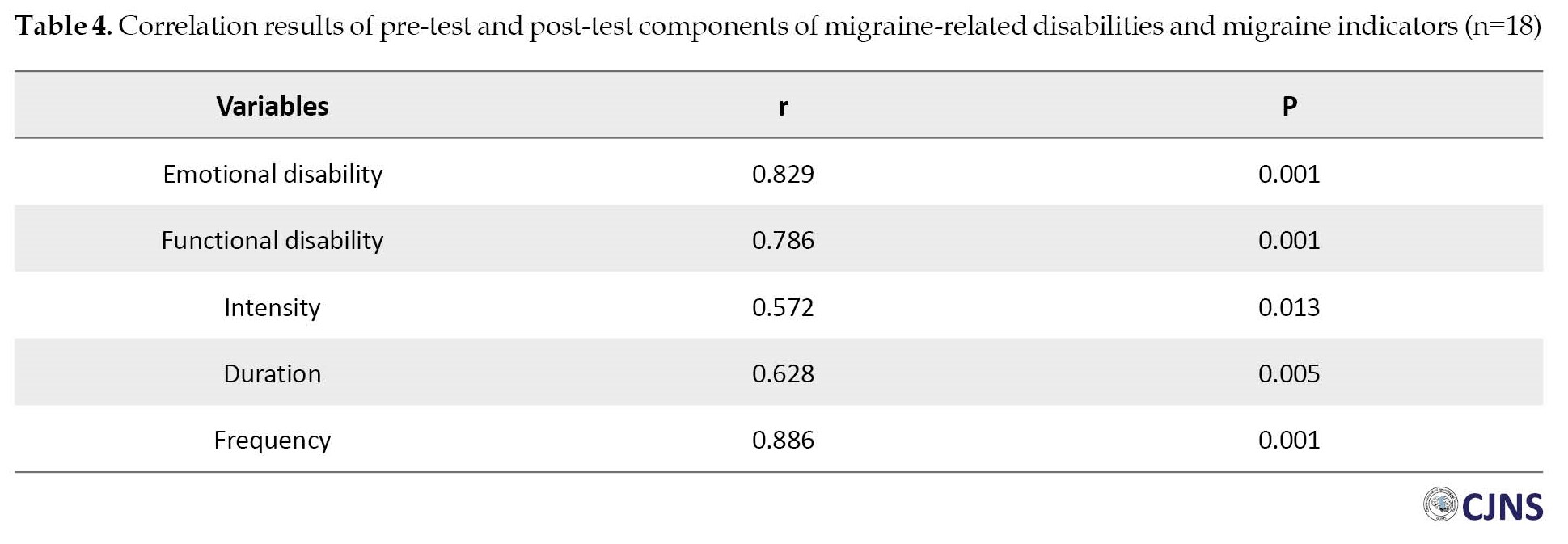

Table 5 shows a significant difference between the pre-test and post-test average duration of migraine attacks (P<0.05). Still, there is no significant difference between the average intensity of migraine attacks and the frequency of migraine attacks. And there is a significant difference between the pre-test and the post-test of emotional disability (P<0.05), but there is no significant difference for functional disability.
Discussion
The study investigated the effectiveness of combined behavior management intervention and pharmacotherapy in reducing migraine-related disabilities with and without focusing on comorbid depressive symptoms. The combination of behavior management intervention and pharmacotherapy focusing on comorbid depressive symptoms effectively reduced migraine-related disabilities in migraine patients with comorbid depressive symptoms. The treatment significantly reduced emotional disability in migraine patients with comorbid depressive symptoms but had no significant effect on functional disability in these participants. These results align with previous studies’ findings [7, 30, 31]. Considering the nature of the proposed combined therapeutic approach, various behavioral techniques are used in behavior management to increase the self-efficacy of sufferers during headache attacks. The intervention sessions provided participants with comprehensive information regarding the nature of migraine, its stages and triggers, timely recognition of attack symptoms, coping techniques, and timely use of effective sedatives. In addition, patients’ distorted cognitions, particularly about migraine attacks, were challenged.
During the interventions, patients were asked to monitor their condition by identifying and recording migraine attack indicators, frequency of sedative use, and possible migraine attack triggers in a headache diary. This self-monitoring gave the sufferers a feeling of having more command over their disease and thus facilitated the acceptance process. This acceptance and understanding reduced the burden of self-blame and the shame of migraine patients. Moreover, they were encouraged to raise awareness among their family members and friends and ask for compassion and companionship. These changes effectively reduced the participants’ emotional burden of migraine.
Behavior management therapy and pharmacotherapy effectively reduced migraine indicators in patients with comorbid depressive symptoms. The treatment significantly reduced the duration of migraine attacks in migraine sufferers with comorbid depressive symptoms but had no significant impact on the frequency and intensity of attacks in these patients. These findings are consistent with the results of previous studies [14, 32, 33]. Importantly, preventive/acute medications can, in many cases, prevent headache attacks or reduce the intensity or duration of headaches if prescribed and taken according to the patient’s needs. On the other hand, obtaining insight into migraine and learning appropriate management techniques can help patients effectively prevent or cope with their migraine attacks.
The combined therapeutic approach significantly reduced the duration of migraine attacks but had no significant impact on the frequency and intensity of attacks (Table 5). The behavior management approach consists of techniques that change a person’s lifestyle. During the intervention sessions, participants were given insights into the migraine triggers that initiate or accelerate headache attacks. They were subsequently asked to control some modifiable triggers (changes in sleep habits, including certain foods in the diet, etc.). These changes in the patient’s lifestyle take time; therefore, a long-term follow-up may reveal the effectiveness of the results. In addition, although lifestyle change requires a high level of motivation, low mood and low motivation of migraine patients with comorbid depression reduce their treatment during the intervention process. Furthermore, some behavioral techniques such as muscle relaxation, breathing exercises, and trigger point massage are only effective when performed continuously daily. Performing them during a migraine attack only worsens the patient’s condition. This finding complies with that of Meyer et al. [34].
A more decrease was observed in migraine-related disabilities of participants in the first intervention group (combined therapy with focusing on comorbid depression) than those in the second group (combined therapy without focusing on comorbid depression). This finding aligns with previous studies’ results [17, 19, 31]. Although the combined treatment approach was found to reduce migraine-related disabilities, depression reduced the effectiveness of treatment. Combined therapy with a focus on comorbid depressive symptoms targeted poor treatment adherence (passivity), which is a major barrier to treatment in patients with depression. People need intrinsic motivation to engage in various activities, yet depression often reduces this potential motivation and causes people to postpone their tasks and duties. The behavioral activation technique helped participants specify and prioritize their values and goals and gradually incorporate them into their daily and weekly schedules. It also taught them how to change their feelings by simply changing their daily activities without the need for internal motivation. The reduction in depression levels during the sessions resulted in higher cooperation and treatment adherence among the first intervention group members. The careful monitoring of daily headaches in this group proves this assertion.
On the other hand, some migraine attacks are triggered by low mood, crying, stress, and constant rumination. The intervention program provided participants in the first group with useful information about rumination and taught them how to replace avoidance with problem-solving. The program also helped these individuals have fewer headache attacks by changing their lifestyles. The results revealed a higher decrease in migraine-related disabilities of participants in the first intervention group than those of participants in the second group. There was no significant difference between the two groups in terms of functional migraine-related disabilities. This result may be because functional disabilities can only improve over time. A lower level of depression motivates individuals to change their lifestyle, and the gradual lifestyle change reduces confrontation with migraine triggers, leading to improved functional abilities.
Lastly, a more pronounced reduction was observed in the frequency of migraine attacks of participants in the first intervention group (combined therapy focused on comorbid depression) than in the second group (combined therapy without a focus on comorbid depression). However, no significant differences were found between the two groups regarding the intensity and duration of attacks. These results are consistent with previous research findings (Table 3) [19, 28].
In this regard, one should consider the nature of depression and its impact on the treatment process. As mentioned earlier, low motivation of people with high depression decreases their treatment adherence and cooperation during the therapeutic intervention. Through the therapeutic sessions, depression was gradually reduced, and the general mood of the members of the first intervention group improved, resulting in better cooperation in the treatment process. For example, these individuals attended the sessions more eagerly, followed the intervention instructions more strictly, and changed their negative biases toward pharmacotherapy. On the other hand, constant, worrisome rumination increases tension and stress levels in people with depression. In addition to relaxation techniques, participants in the first group also received useful information about rumination and problem-solving techniques that enabled them to better manage their rumination and stress. Since stress is an important trigger for migraine, managing stress appropriately can effectively reduce the frequency of attacks. Furthermore, participants in the first group reported higher lifestyle changes and behavior management techniques (e.g. taking sedatives and preventive medications promptly, improving sleep quality, eliminating triggers in their diet, and performing relaxation techniques frequently). Therefore, participants in the first group were more likely to avoid migraine triggers than those in the second group. Accordingly, a greater decrease in total migraine indicators and frequency of migraine attacks was observed in members of the first intervention group than in the second group. However, the two groups had no significant difference regarding the duration and intensity of attacks. This result may be due to the simultaneous treatment of migraine and depression in this study.
Undoubtedly, the treatment of depression influences the recovery of migraine patients. However, more time seems to be needed for the full recovery of patients with depression. In addition, the severity of depressive symptoms affects the recovery process. On the other hand, as mentioned before, patients’ lifestyle habits gradually change; therefore, a long-term follow-up may unveil effective results.
Study limitations
The use of convenience sampling (because of the difficulty in accessing the target population) and the fact that no male participants were included in the study (because of the higher prevalence of migraine among women and the poor cooperation of men with the researchers) were the main limitations of the present study. Therefore, the results must be cautiously generalized to the general population. In addition, although the type of migraine may affect the number of monthly headache days, episodic and chronic migraine were not studied separately. Also, the power of the test below 0.70 was calculated. Therefore, it is necessary to select a larger sample size to test the hypothesis in future studies.
Study suggestions
Researchers are suggested to separately examine the effects of the proposed therapeutic approach on episodic and chronic migraine patients in future studies. Researchers are also suggested to investigate the role of other comorbidities, such as anxiety and obsession, in treating migraine patients and compare their findings with the present results.
Results generally indicated associations between several psychological factors and migraine. Considering the importance of understanding psychological comorbidities of migraine, the present findings can help educational and clinical professionals assess the presence of comorbid depressive symptoms in migraine patients and thus more accurately identify the causes of migraine and more effectively treat migraine sufferers.
Conclusion
Behavior management therapy and pharmacotherapy effectively reduced migraine-related disabilities and indicators in migraine patients with comorbid depressive symptoms. In addition, combined treatment resulted in greater reductions in migraine-related disabilities and migraine indicators among participants in the first intervention group (with a focus on comorbid depression) than among those in the second group (without a focus on comorbid depression).
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of University of Guilan (Code: IR.GUILAN.REC.1400.021), and informed consent was obtained from all subjects.
Funding
This article extracted from Master’s thesis of the Kimia Safarionpur at the Department of Psychology, University of Guilan (Code: 73672).
Authors contributions
Conceptualization and methodology: Azra Zebardast, Alia Saberi and Kimia Safarionpur; Drafting the original paper, collecting resources, data collection, and statistical analyses: Kimia Safarionpur; Writing, reviewing, and editing: Azra Zebardast and Alia Saberi; Supervision: Azra Zebardast; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors of this article are grateful to all the participants in the research.
Migraine is a headache disorder characterized by clinical symptoms such as throbbing and pulsating attacks [1]. According to the World Health Organization (WHO), migraine is the third most common disease, affecting approximately one billion people worldwide [2]. The global prevalence of migraine is 11.6%, affecting nearly 1 in 10 people worldwide [3].Migraine is associated with a high prevalence of psychological comorbidities such as depression, anxiety, personality disorders, obsessions, and sleep disorders [4].Migraine-associated comorbidities are risk factors for developing episodic to chronic migraines [5]. The most common comorbidity with migraine is depression [6].There is a bidirectional relationship between depression and migraine [7], i.e. the risk of migraine is tripled by depression, and vice versa. However, the basic mechanism of this relationship is still poorly understood [8].
Notably, migraine treatment interventions usually focus on examining migraine indicators, including the intensity, duration, and frequency of attacks. Although diagnosis and treatment of migraine-related disabilities are necessary for achieving effective clinical outcomes, these issues are not the focus of interest for researchers and healthcare specialists [9]. Migraine-related disabilities refer to patients’ inability to perform activities they would have been able to do easily without a migraine [10]. According to the global burden of disease (GBD), migraine is the second leading cause of years lost due to disability (YLD), which dramatically disrupts a person’s social, familial, and personal roles [11]. People with migraine also carry an additional psychological burden due to fear of the next attack and difficulty planning [12].
In recent years, nonpharmacological treatment approaches have been used independently or in combination with pharmacological approaches to treat various types of migraine [13]. Research suggests that a combination of pharmacological and psychological therapeutic approaches is more effective than either approach alone [14]. With a therapeutic effectiveness of 35%-55%, the American Academy of Neurology proposed the behavior management approach as the most effective psychological approach to reduce migraine-related disabilities [15]. The behavior management approach focuses on observable behaviors and replaces ineffective behaviors with effective habits and behaviors [16]. Behavior management therapies used to treat migraine patients are primarily aimed at reducing the frequency and intensity of pain, reducing migraine-related disabilities, controlling disease progression, improving patients’ quality of life, reducing dependence on medications, and increasing treatment adherence [14]. Although research has confirmed the positive impact of the behavior management approach on migraine patients, it has failed to treat 62% of migraine patients with comorbid depression or has even worsened their condition in the long term [17]. Authors of a meta-analysis argued that some psychotherapeutic approaches could help prevent and control migraine by facilitating the management and regulation of triggers such as stress, emotional experience, sleep, and some comorbid symptoms [18]. Lipton et al. have concluded that recognizing comorbid depressive symptoms influences appropriate medication selection and treatment adherence in migraine patients [19]. In addition, addressing the comorbidity of migraine and depression in the treatment process can increase the response rate and accelerate the recovery process [20]. Peck et al. report that behavior therapy and preventive pharmacotherapy can effectively treat patients with mild to moderate depression and severe migraine [21].
Few studies have examined the effectiveness of different therapeutic approaches in treating migraine patients with comorbid depression. There is a huge research gap in the literature in all countries, especially Iran. Accordingly, this study investigated the effectiveness of combined behavior management interventions and pharmacotherapy in reducing migraine-related disabilities and indicators with and without focusing on comorbid depressive symptoms.
Materials and Methods
This quasi-experimental study was conducted using a two-group pre-test & post-test design. The study population consisted of all (male and female) migraine patients with comorbid depressive symptoms referring to neurology clinics in Rasht City, Iran, in 2021. A neurologist and the researcher conducted clinical interviews with the migraine patients and completed relevant questionnaires to identify those with comorbid depressive symptoms. A total of 18 eligible female patients out of 56 were selected as the sample using purposive sampling and randomly (simple randomization) assigned to two groups (n=9) homogenized in terms of age and severity of depression of 56 people who filled out the questionnaire, 34 had at least mild depression. Of them, 22 met all the inclusion criteria and agreed to participate in the intervention. But 4 people did not continue to cooperate when signing the consent form to start the intervention. Enrolled in the study were migraine patients between the ages of 25 and 50 with comorbid depressive symptoms (with the diagnosis of a psychiatrist, based on DSM-5 criteria [22]and Beck’s depression inventory/cut of point=19 [23]). The exclusion criteria included failing to complete the questionnaires (at any stage of the study), receiving any psychological treatment to control migraine or depression during the study, and taking medications other than those prescribed by the neurologist (who collaborated in the study) to control migraine or depression.
Study procedure
In sample selection, due to the restrictions caused by COVID-19, through virtual media, all people who had symptoms of migraine headaches were invited to answer online questionnaires on the diagnostic criteria of migraine (based on ICHD-3 beta) [24] and depression (based on DSM-5 criteria and Beck’s depression inventory/cut of point=19) [22, 23]. Then, those who met the basic conditions were referred to the neurologist’s office for a definitive migraine diagnosis. According to the results of interviews and questionnaires, 22 people who met the inclusion criteria were selected. During the research process, 4 people dropped out, and finally, 18 women remained until the end of the research. In this plan, subjects were placed in two combined treatment groups (drug therapy and behavioral management) after completing the pre-test (migraine disability questionnaire, Beck depression, and one-month monitoring of migraine indicators) and matching based on age and severity of depression. The first group received a combined treatment intervention focusing on the symptoms of depression in their co-workers, and the second group received a combined treatment intervention without focusing on the symptoms of depression in their co-workers provided by the researcher under the supervision of a faculy member in the department of psychology at the University of Guilan. The post-test was taken through the questionnaires above. The intervention was carried out during eight 1-hour sessions (one session per week) and individually to comply with health protocols and social distancing (due to the spread of COVID-19) and to maintain the health of the participants online through video calls using the program WhatsApp was conducted for two months in September and November 2021.
Research tools
Beck’s depression inventory-second edition (BDI-II)
The BDI was published in 1996 by Beck et al. [23]. BDI-II is a 21-item tool that measures the somatic, affective, and cognitive symptoms of depression. Each item includes 4 to 7 statements, and the items are scored on a 4-point Likert scale ranging from no depression to mild depression (score 0) to severe depression (score 3). Respondents must answer questions about their moods and feelings over the past two weeks. The total score is the sum of the scores given to all statements (total score range: 0-63). The scores 0 to 13, 14 to 19, 20 to 28, and 29 to 63, respectively, indicate normal, mild, moderate, and severe levels of depression [23]. According to Beck et al. the internal consistency of the tool ranges between 0.73 and 0.92 (mean=0.86). In addition, the convergent validity of the tool has been obtained as 0.71 using the Hamilton depression rating scale (HDRS). Asghari et al. confirmed the reliability of BDI-II with a Cronbach α value of 0.89 in Iran [25].
Headache disability inventory (HDI)
HDI was designed by Jacobsen et al. to measure the debilitating impacts of headaches on a person’s life [26]. This 25-item tool measures emotional (unpleasant feelings caused by headaches) and functional (personal and social limitations caused by headaches) aspects of disability. The 3-choice items are scored as yes (score 4), sometimes (score 2), and no (score 0). The total score ranges from 0 to 88, with higher scores indicating more severe disabilities. In the Persian version of the scale, items 7, 15, and 22 were recognized as duplicates and removed. HDI has good validity and acceptable reliability. Jacobsen et al. (1994) confirmed the reliability of the tool with a Cronbach α value of 0.83. The concurrent validity of emotional and functional subscales of HDI with SCL-25 has been calculated as 0.79 and -0.91, respectively. The reliability of HDI was confirmed with a Cronbach α value of 0.83 in Iran. In addition, a Cronbach α value of 0.86 was obtained for the two subscales of HDI in a study in Iran [27].
Headache diary (HD)
This researcher-made self-report tool assesses migraine headache indicators, including the intensity, duration, and frequency of attacks. The participants who had already received the necessary training recorded the intensity, duration, and frequency of their migraine attacks every day during a 1-month follow-up before and after the interventions. The intensity of each attack was measured using a 10-point visual analog scale (VAS), a convenient and frequently used tool for measuring perceived pain intensity. On this scale, scores of 0 and 10 represent no pain and the most severe pain, respectively, whereas scores between 1 and 3, 4 to 7, and 8 to 10 correspond to mild, moderate, and severe pain, respectively. Participants were also asked to record the number of hours each attack lasted (duration) and the number of migraine attacks per month (frequency).
Intervention programs
The intervention program to prevent and improve migraine was developed based on Seng’s study and according to behavioral theory [28]. The program to improve comorbid depressive symptoms was designed based on the behavioral activation for depression model developed by Martell et al. [29] (Table 1).
Before the intervention, three experts (two psychologists and one neurologist) confirmed the content validity of the therapeutic methods. The data were analyzed in SPSS software, version 24 using descriptive statistics (Mean±SD) and inferential statistics (paired-sample t-test and multivariate analysis of covariance [MANCOVA]).
Results
The Mean±SD ages of participants in the first intervention group (combined therapy with focusing on comorbid depression) and second intervention group (combined therapy without focusing on comorbid depression) were 32.56±3.67 and 33.78±6.05 years, respectively. The Mean±SD age of all participants was 33.17±4.90 years, with the youngest and oldest participants being 26 and 45 years old, respectively.
According to Table 2, the t value obtained for migraine-related disabilities was 2.96, and the respective level of significance was <0.05.

Thus, given the results of Table 2, the mean score of migraine-related disabilities significantly reduced after the interventions. This finding confirms the effectiveness of the combined therapeutic approach in reducing migraine-related disabilities. In addition, the t value obtained for the variable of migraine indicators was 5.13, and the respective significance level was <0.05. Accordingly, given the results of Table 2, the mean score of the migraine indicator has significantly decreased after the interventions. This finding confirms the effectiveness of the combined therapeutic approach in reducing migraine indicators.
In the following, MANCOVA was employed to investigate the effectiveness of combined behavior management therapy and pharmacotherapy in reducing migraine-related disabilities and indicators with and without focusing on comorbid depressive symptoms. The normality of the data distribution was tested using the Shapiro-Wilk test. P for migraine-related disabilities and migraine indicators (except frequency of attack in the pre-test and post-test stage) were greater than 0.05 before and after the interventions; thus, the data had a normal distribution. Levene’s test was used to assess the assumption of homogeneity of variances in both groups. Since P for all variables of migraine-related disabilities and migraine indicators were greater than 0.05, the assumption of homogeneity of variances was confirmed for all research variables. The results of the box test to check the equality of the covariance matrix of the dependent variables in the two experimental and control groups also showed that the covariance matrix of the dependent variables in the two groups is equal (box M= 0.864, F=0.249, P<0.862); therefore, the data were analyzed using MANCOVA. Multivariate statistical tests were utilized to evaluate the effects of group membership, which revealed a statistically significant difference between the two groups following the interventions concerning at least one dependent variable of migraine-related disabilities or migraine indicators (F(2, 13)=10.43, P<0.05, Wilks Lambda=0.384, partial Ƞ2=0.616).
After the interventions, the F value obtained for the variable of migraine-related disabilities was 8.20, and the respective level of significance was <0.05, indicating a significant difference between the two groups (Table 3).

Hence, a more decrease was observed in the mean score of migraine-related disabilities of participants in the combined therapy focusing on depressive symptoms than those in the second intervention group. About 37% of the difference between the groups regarding migraine-related disabilities was due to interventions in the post-test stage with statistical control of the pre-test scores.
In addition, after the interventions, the F value obtained for the variable of migraine indicators was 9.31, and the respective level of significance was smaller than 0.05, indicating a significant difference between the two groups; thus, a greater decrease in the mean score of migraine indicators was observed among participants in the first intervention group than among those in the second intervention group. Also, 40% of the difference between the groups in terms of migraine indicators was due to interventions in the post-test stage with statistical control of the pre-test scores.
Also, this hypothesis was investigated that combined intervention reduces migraine-related disability and migraine indicators in migraine patients with comorbid depression (in both groups). The results are reported in Tables 4 and 5.
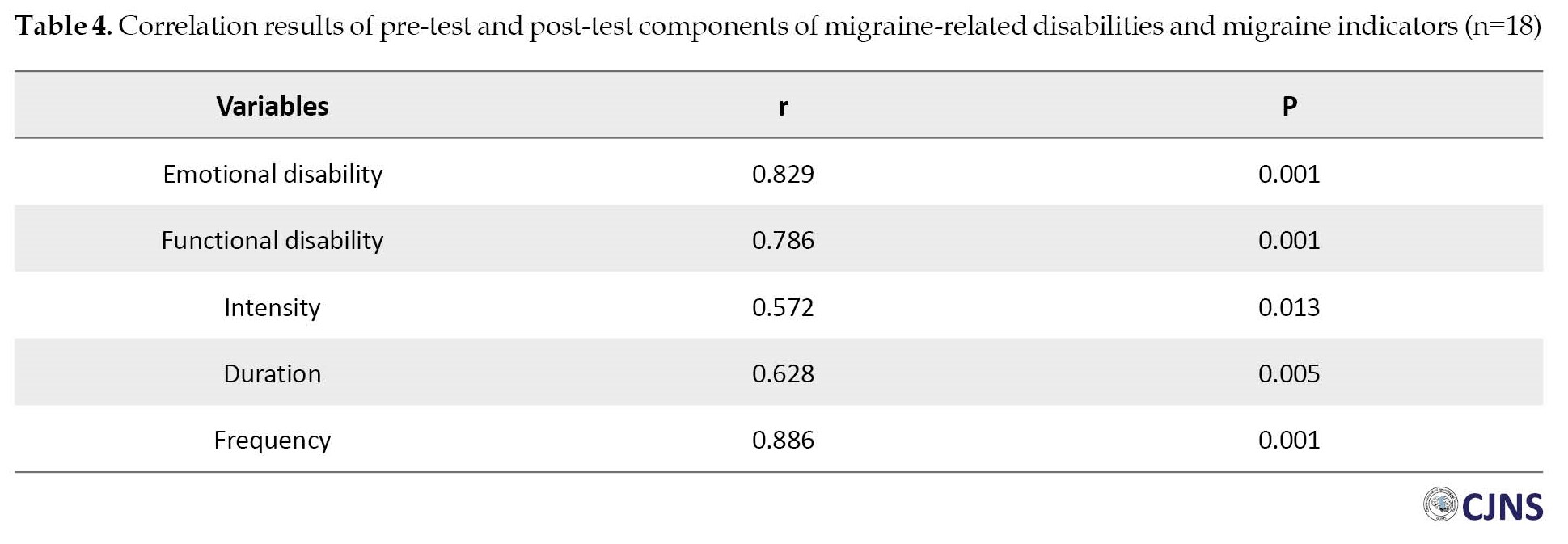

Table 5 shows a significant difference between the pre-test and post-test average duration of migraine attacks (P<0.05). Still, there is no significant difference between the average intensity of migraine attacks and the frequency of migraine attacks. And there is a significant difference between the pre-test and the post-test of emotional disability (P<0.05), but there is no significant difference for functional disability.
Discussion
The study investigated the effectiveness of combined behavior management intervention and pharmacotherapy in reducing migraine-related disabilities with and without focusing on comorbid depressive symptoms. The combination of behavior management intervention and pharmacotherapy focusing on comorbid depressive symptoms effectively reduced migraine-related disabilities in migraine patients with comorbid depressive symptoms. The treatment significantly reduced emotional disability in migraine patients with comorbid depressive symptoms but had no significant effect on functional disability in these participants. These results align with previous studies’ findings [7, 30, 31]. Considering the nature of the proposed combined therapeutic approach, various behavioral techniques are used in behavior management to increase the self-efficacy of sufferers during headache attacks. The intervention sessions provided participants with comprehensive information regarding the nature of migraine, its stages and triggers, timely recognition of attack symptoms, coping techniques, and timely use of effective sedatives. In addition, patients’ distorted cognitions, particularly about migraine attacks, were challenged.
During the interventions, patients were asked to monitor their condition by identifying and recording migraine attack indicators, frequency of sedative use, and possible migraine attack triggers in a headache diary. This self-monitoring gave the sufferers a feeling of having more command over their disease and thus facilitated the acceptance process. This acceptance and understanding reduced the burden of self-blame and the shame of migraine patients. Moreover, they were encouraged to raise awareness among their family members and friends and ask for compassion and companionship. These changes effectively reduced the participants’ emotional burden of migraine.
Behavior management therapy and pharmacotherapy effectively reduced migraine indicators in patients with comorbid depressive symptoms. The treatment significantly reduced the duration of migraine attacks in migraine sufferers with comorbid depressive symptoms but had no significant impact on the frequency and intensity of attacks in these patients. These findings are consistent with the results of previous studies [14, 32, 33]. Importantly, preventive/acute medications can, in many cases, prevent headache attacks or reduce the intensity or duration of headaches if prescribed and taken according to the patient’s needs. On the other hand, obtaining insight into migraine and learning appropriate management techniques can help patients effectively prevent or cope with their migraine attacks.
The combined therapeutic approach significantly reduced the duration of migraine attacks but had no significant impact on the frequency and intensity of attacks (Table 5). The behavior management approach consists of techniques that change a person’s lifestyle. During the intervention sessions, participants were given insights into the migraine triggers that initiate or accelerate headache attacks. They were subsequently asked to control some modifiable triggers (changes in sleep habits, including certain foods in the diet, etc.). These changes in the patient’s lifestyle take time; therefore, a long-term follow-up may reveal the effectiveness of the results. In addition, although lifestyle change requires a high level of motivation, low mood and low motivation of migraine patients with comorbid depression reduce their treatment during the intervention process. Furthermore, some behavioral techniques such as muscle relaxation, breathing exercises, and trigger point massage are only effective when performed continuously daily. Performing them during a migraine attack only worsens the patient’s condition. This finding complies with that of Meyer et al. [34].
A more decrease was observed in migraine-related disabilities of participants in the first intervention group (combined therapy with focusing on comorbid depression) than those in the second group (combined therapy without focusing on comorbid depression). This finding aligns with previous studies’ results [17, 19, 31]. Although the combined treatment approach was found to reduce migraine-related disabilities, depression reduced the effectiveness of treatment. Combined therapy with a focus on comorbid depressive symptoms targeted poor treatment adherence (passivity), which is a major barrier to treatment in patients with depression. People need intrinsic motivation to engage in various activities, yet depression often reduces this potential motivation and causes people to postpone their tasks and duties. The behavioral activation technique helped participants specify and prioritize their values and goals and gradually incorporate them into their daily and weekly schedules. It also taught them how to change their feelings by simply changing their daily activities without the need for internal motivation. The reduction in depression levels during the sessions resulted in higher cooperation and treatment adherence among the first intervention group members. The careful monitoring of daily headaches in this group proves this assertion.
On the other hand, some migraine attacks are triggered by low mood, crying, stress, and constant rumination. The intervention program provided participants in the first group with useful information about rumination and taught them how to replace avoidance with problem-solving. The program also helped these individuals have fewer headache attacks by changing their lifestyles. The results revealed a higher decrease in migraine-related disabilities of participants in the first intervention group than those of participants in the second group. There was no significant difference between the two groups in terms of functional migraine-related disabilities. This result may be because functional disabilities can only improve over time. A lower level of depression motivates individuals to change their lifestyle, and the gradual lifestyle change reduces confrontation with migraine triggers, leading to improved functional abilities.
Lastly, a more pronounced reduction was observed in the frequency of migraine attacks of participants in the first intervention group (combined therapy focused on comorbid depression) than in the second group (combined therapy without a focus on comorbid depression). However, no significant differences were found between the two groups regarding the intensity and duration of attacks. These results are consistent with previous research findings (Table 3) [19, 28].
In this regard, one should consider the nature of depression and its impact on the treatment process. As mentioned earlier, low motivation of people with high depression decreases their treatment adherence and cooperation during the therapeutic intervention. Through the therapeutic sessions, depression was gradually reduced, and the general mood of the members of the first intervention group improved, resulting in better cooperation in the treatment process. For example, these individuals attended the sessions more eagerly, followed the intervention instructions more strictly, and changed their negative biases toward pharmacotherapy. On the other hand, constant, worrisome rumination increases tension and stress levels in people with depression. In addition to relaxation techniques, participants in the first group also received useful information about rumination and problem-solving techniques that enabled them to better manage their rumination and stress. Since stress is an important trigger for migraine, managing stress appropriately can effectively reduce the frequency of attacks. Furthermore, participants in the first group reported higher lifestyle changes and behavior management techniques (e.g. taking sedatives and preventive medications promptly, improving sleep quality, eliminating triggers in their diet, and performing relaxation techniques frequently). Therefore, participants in the first group were more likely to avoid migraine triggers than those in the second group. Accordingly, a greater decrease in total migraine indicators and frequency of migraine attacks was observed in members of the first intervention group than in the second group. However, the two groups had no significant difference regarding the duration and intensity of attacks. This result may be due to the simultaneous treatment of migraine and depression in this study.
Undoubtedly, the treatment of depression influences the recovery of migraine patients. However, more time seems to be needed for the full recovery of patients with depression. In addition, the severity of depressive symptoms affects the recovery process. On the other hand, as mentioned before, patients’ lifestyle habits gradually change; therefore, a long-term follow-up may unveil effective results.
Study limitations
The use of convenience sampling (because of the difficulty in accessing the target population) and the fact that no male participants were included in the study (because of the higher prevalence of migraine among women and the poor cooperation of men with the researchers) were the main limitations of the present study. Therefore, the results must be cautiously generalized to the general population. In addition, although the type of migraine may affect the number of monthly headache days, episodic and chronic migraine were not studied separately. Also, the power of the test below 0.70 was calculated. Therefore, it is necessary to select a larger sample size to test the hypothesis in future studies.
Study suggestions
Researchers are suggested to separately examine the effects of the proposed therapeutic approach on episodic and chronic migraine patients in future studies. Researchers are also suggested to investigate the role of other comorbidities, such as anxiety and obsession, in treating migraine patients and compare their findings with the present results.
Results generally indicated associations between several psychological factors and migraine. Considering the importance of understanding psychological comorbidities of migraine, the present findings can help educational and clinical professionals assess the presence of comorbid depressive symptoms in migraine patients and thus more accurately identify the causes of migraine and more effectively treat migraine sufferers.
Conclusion
Behavior management therapy and pharmacotherapy effectively reduced migraine-related disabilities and indicators in migraine patients with comorbid depressive symptoms. In addition, combined treatment resulted in greater reductions in migraine-related disabilities and migraine indicators among participants in the first intervention group (with a focus on comorbid depression) than among those in the second group (without a focus on comorbid depression).
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Research Ethics Committee of University of Guilan (Code: IR.GUILAN.REC.1400.021), and informed consent was obtained from all subjects.
Funding
This article extracted from Master’s thesis of the Kimia Safarionpur at the Department of Psychology, University of Guilan (Code: 73672).
Authors contributions
Conceptualization and methodology: Azra Zebardast, Alia Saberi and Kimia Safarionpur; Drafting the original paper, collecting resources, data collection, and statistical analyses: Kimia Safarionpur; Writing, reviewing, and editing: Azra Zebardast and Alia Saberi; Supervision: Azra Zebardast; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors of this article are grateful to all the participants in the research.
References
- Rockett FC, de Oliveira VR, Castro K, Chaves ML, Perla Ada S, Perry ID. Dietary aspects of migraine trigger factors. Nutr Rev. 2012; 70(6):337-56. [DOI:10.1111/j.1753-4887.2012.00468.x] [PMID]
- Nowaczewska M, Wiciński M, Kaźmierczak W. The ambiguous role of caffeine in migraine headache: From trigger to treatment. Nutrients. 2020; 12(8):2259. [DOI:10.3390/nu12082259] [PMID] [PMCID]
- El-Metwally A, Toivola P, AlAhmary K, Bahkali S, AlKhathaami A, Al Ammar SA, et al. The epidemiology of migraine headache in Arab countries: A systematic review. Sci World J. 2020; 2020:4790254. [DOI:10.1155/2020/4790254] [PMID] [PMCID]
- Minen MT, Begasse De Dhaem O, Kroon Van Diest A, Powers S, Schwedt TJ, Lipton R, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. 2016; 87(7):741-9. [DOI:10.1136/jnnp-2015-3122331] [PMID]
- Peres MFP, Mercante JPP, Tobo PR, Kamei H, Bigal ME. Anxiety and depression symptoms and migraine: A symptom-based approach research. J Headache Pain. 2017; 18(1):37. [DOI:10.1186/s10194-017-0742-1] [PMID] [PMCID]
- Amoozegar F. Depression comorbidity in migraine. Int Rev Psychiatry. 2017; 29(5):504-15. [DOI:10.1080/09540261.2017.1326882] [PMID]
- Dindo LN, Recober A, Haddad R, Calarge CA. Comorbidity of migraine, major depressive disorder, and generalized anxiety disorder in adolescents and young adults. Int J Behav Med. 2017; 24(4):528-34. [DOI:10.1007/s12529-016-9620-5] [PMID] [PMCID]
- Pisanu C, Lundin E, Preisig M, Gholam-Rezaee M, Castelao E, Pistis G, et al. Major depression subtypes are differentially associated with migraine subtype, prevalence and severity. Cephalalgia. 2020; 40(4):347-56. [DOI:10.1177/0333102419884935] [PMID]
- Pérez-Muñoz A, Buse DC, Andrasik F. Behavioral interventions for migraine. Neurol Clin. 2019; 37(4):789-813. [DOI:10.1016/j.ncl.2019.07.003] [PMID]
- Atlas LY, Wager TD. How expectations shape pain. Neurosci Lett. 2012; 520(2):140-8. [DOI:10.1016/j.neulet.2012.03.039] [PMID]
- Takeshima T, Wan Q, Zhang Y, Komori M, Stretton S, Rajan N, et al. Prevalence, burden, and clinical management of migraine in China, Japan, and South Korea: a comprehensive review of the literature. J Headache Pain. 2019; 20(1):111. [DOI:10.1186/s10194-019-1062-4] [PMID] [PMCID]
- Jeyagurunathan A, Abdin E, Vaingankar JA, Chua BY, Shafie S, Chang SHS, et al. Prevalence and comorbidity of migraine headache: Results from the Singapore mental health study 2016. Soc Psychiatry Psychiatr Epidemiol. 2020; 55(1):33-43. [DOI:10.1007/s00127-019-01755-1] [PMID]
- Grazzi L, Bernstein C, Raggi A, Sansone E, Grignani E, Searl M, et al. ACT for migraine: Effect of acceptance and commitment therapy (ACT) for high-frequency episodic migraine without aura: Preliminary data of a phase-II, multicentric, randomized, open-label study. Neurol Sci. 2019; 40(Suppl 1):191-2. [DOI:10.1007/s10072-019-03802-w] [PMID]
- Faedda N, Cerutti R, Verdecchia P, Migliorini D, Arruda M, Guidetti V. Behavioral management of headache in children and adolescents. J Headache Pain. 2016; 17(1):80.[DOI:10.1186/s10194-016-0671-4] [PMID] [PMCID]
- Singer AB. Mindfulness practice and perceived stress: a secondary analysis of a randomized controlled trial of mindfulness-based cognitive therapy for migraine [PhD. Thesis]. New York: Yeshiva University; 2017. [Link]
- Corey G. Theory and practice of counseling and psychotherapy. Boston: Cengage Learning; 2012. [Link]
- Martin PR, Aiello R, Gilson K, Meadows G, Milgrom J, Reece J. Cognitive behavior therapy for comorbid migraine and/or tension-type headache and major depressive disorder: An exploratory randomized controlled trial. Behav Res Ther. 2015; 73:8-18. [DOI:10.1016/j.brat.2015.07.005] [PMID]
- Lee HJ, Lee JH, Cho EY, Kim SM, Yoon S. Efficacy of psychological treatment for headache disorder: A systematic review and meta-analysis. J Headache Pain. 2019; 20(1):17. [DOI:10.1186/s10194-019-0965-4] [PMID] [PMCID]
- Lipton RB, Seng EK, Chu MK, Reed ML, Fanning KM, Adams AM, et al. The effect of psychiatric comorbidities on headache-related disability in migraine: Results from the chronic migraine epidemiology and outcomes (CaMEO) study. Headache. 2020; 60(8):1683-96. [DOI:10.1111/head.13914] [PMID] [PMCID]
- Dresler T, Caratozzolo S, Guldolf K, Huhn JI, Loiacono C, Niiberg-Pikksööt T, et al. Understanding the nature of psychiatric comorbidity in migraine: A systematic review focused on interactions and treatment implications. J Headache Pain. 2019; 20(1):51. [DOI:10.1186/s10194-019-0988-x] [PMID] [PMCID]
- Peck KR, Smitherman TA, Baskin SM. Traditional and alternative treatments for depression: Implications for migraine management. Headache. 2015; 55(2):351-5. [DOI:10.1111/head.12521] [PMID]
- Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: Implications for clinical practice. Front Psychiatry. 2018; 9:450. [DOI:10.3389/fpsyt.2018.00450] [PMID] [PMCID]
- Beck A. T, Steer R. A, Brown G. K. Beck depression inventory (BDI-II). Washington: American Psychological Association; 1996. [DOI:10.1037/t00742-000]
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013; 33(9):629-808. [DOI:10.1177/0333102413485658] [PMID]
- Asghari soleimani M, Khanmohammadi A, Abbasi Asfajir A, Sadeghi J. [The effectiveness of flourishing training on anxiety, stress, and depression of students at babol university of medical sciences in 2019 (Persian)]. J Community Health. 2020; 14(3):65-75. [DOI:10.22123/CHJ.2020.228674.1491]
- Jacobson GP, Ramadan NM, Aggarwal SK, Newman CW. The henry ford hospital headache disability inventory (HDI). Neurology. 1994; 44(5):837-42. [DOI:10.1212/WNL.44.5.837] [PMID]
- Sajadinezhad M, Mohammadi N, Ashgahzadeh N. [The evaluation of psychometric properties of headache disability inventory in the headache patients (Persian)]. J Shahrekord Univ Med Sci. 2007; 9(1):62-55. [Link]
- Seng EK. Using cognitive behavioral therapy techniques to treat migraine. J Health Serv Psychol. 2018; 44(2):68-73. [DOI:10.1007/BF03544665] [PMID] [PMCID]
- Martell CR, Dimidjian S, Herman-Dunn R. Behavioral activation for depression: A clinician’s guide. New York: Guilford Press; 2010. [Link]
- Voerman JS, Klerk Cd, Mérelle SY, Aartsen E, Timman R, Sorbi MJ, et al. Long-term follow-up of home-based behavioral management training provided by migraine patients. Cephalalgia. 2014; 34(5):357-64.[DOI:10.1177/0333102413515337] [PMID]
- Seng EK, Holroyd KA. Behavioral migraine management modifies behavioral and cognitive coping in people with migraine. Headache. 2014; 54(9):1470-83. [DOI:10.1111/head.12426] [PMID]
- Minen MT, Friedman BW, Adhikari S, Corner S, Powers SW, Seng EK, et al. Introduction of a smartphone based behavioral intervention for migraine in the emergency department. Gen Hosp Psychiatry. 2021; 69:12-9. [DOI:10.1016/j.genhosppsych.2020.12.009] [PMID] [PMCID]
- Hosseinpour H, Akbari M, Hassani J, Zargar F. [The efficacy of pharmacotherapy combined with short-term mindfulness therapy on the reduction of migraine disability and improvement of sleep quality (Persian)]. Shefaye Khatam. 2020; 8(2):18-28. [DOI:10.29252/shefa.8.2.18]
- Meyer B, Keller A, Wöhlbier HG, Overath CH, Müller B, Kropp P. Progressive muscle relaxation reduces migraine frequency and normalizes amplitudes of contingent negative variation (CNV). J Headache Pain. 2016; 17:37. [DOI:10.1186/s10194-016-0630-0] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






