Sat, May 18, 2024
Volume 9, Issue 3 (Summer 2023)
Caspian J Neurol Sci 2023, 9(3): 135-142 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bahran Ahmadi M, Jahani S, Elhaee A, Sayadi N. Validation of Healthy Aging Brain Care Monitor Selfreport Questionnaire in Patients With Post-intensive Care Syndrome. Caspian J Neurol Sci 2023; 9 (3) :135-142
URL: http://cjns.gums.ac.ir/article-1-637-en.html
URL: http://cjns.gums.ac.ir/article-1-637-en.html
1- Nursing Care Research Center in Chronic Disease, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2- Department of Medical and Surgical Nursing, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Department of Biostatics and Epidemiology, School of Health, Mazandaran University of Medical Sciences, Mazandaran, Iran.
2- Department of Medical and Surgical Nursing, Nursing Care Research Center in Chronic Disease, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
3- Department of Biostatics and Epidemiology, School of Health, Mazandaran University of Medical Sciences, Mazandaran, Iran.
Full-Text [PDF 1340 kb]
(357 Downloads)
| Abstract (HTML) (372 Views)
The Cronbach α and ICC of the p-HABC were 0.828 and 0.725, respectively.
Discussion
This research aimed to define the psychometric properties of the Persian HABC-M-SR in patients with PICS. All 27 items of the main questionnaire were found to have suitable face validity. In the content validity check, all the questions were accepted in the CVI and CVR stage. Then, exploratory factor analysis was done, assuming that three factors are constant on the questionnaire. Also, questions 7, 8, 9, and 12 were removed due to low factor loading, and confirmatory factor analysis was performed on 23 questions. The Cronbach α (0.828) and ICC (0.752) results were acceptable. Then, for the remaining 23 questions of the questionnaire, 230 samples were taken, and confirmatory factor analysis was performed, and the results were almost within the acceptable range. Principal component analysis and scree plot confirmed the single-factor structure for 23 items. CFA also confirmed the single-factor structure, and the goodness of fit indices confirmed the fitness of the model examined in this study. Consistent with our results, Monahan et al. have also reported that the HABC-M-SR has good reliability and validity and can be used to measure and monitor the cognitive, functional, and psychological health of older adults attending primary care clinics [21].
The HABC-M-SR can monitor symptoms, provide feedback, and modify care plans in older adults and ICU survivors. In addition, information from the HABC can be relied upon for patients who demonstrate impairment on cognitive tests [21]. Despite technological advances and specialized care provided in ICUs, the symptoms cannot be visible in the post-hospital setting. So, the HABC can contribute to the rapid assessment of a broad span of physical, mental, and perceptive impairments in older adults and ICU survivors. Our findings align with those of Wang et al. and confirm the effectiveness of the HABC-M-SR in measuring the severity of psychological and functional symptoms of PICS [5].
Patients admitted to ICUs experience more severe cognitive, psychological, and functional symptoms than those admitted to other hospital wards. Some studies have also shown that young ICU survivors may suffer from similar aging symptoms as older patients, regardless of age. Therefore, all ICU survivors with cognitive symptoms should undergo detailed neuropsychological examinations. Nonetheless, normal scores on the cognitive subscale should not prevent physicians from more assessment, especially if the patient’s medical history and assessment raise concerns about their cognitive status [5, 22].
Prolonged hospitalization in the ICU is not only very harmful to the health of patients but also negatively impacts society [23]. About one-third of patients who encounter PICS never return to their job, and another third never return to their previous level of work or income. At least 25% of these patients encounter a significant loss of autonomy and need support with activities of regular living one year after ICU discharge, placing a significant load on informal and formal caregivers [24]. Patients who experience PICS experience reduced exercise capacity, incapacity, and cooperated quality of life for months, even years, after intensive care. Instruments such as the HABC-M-SR can help healthcare professionals diagnose patients experiencing PICS early and refer them to relevant specialists to treat their symptoms. Healthcare professionals can easily use such an instrument with little or no expertise to screen and treat PICS symptoms [22].
Conclusion
This research showed the acceptable psychometric properties of the p-HABC questionnaire in patients with PICS. However, this study also has limitations. The HABC-M-SR is suitable for adult patients 18 years of age and older, and the results cannot be generalized to all patients admitted to all ICUs. Among the strengths of this study, the following can be mentioned. This study makes us more familiar with the factors that cause PICS. In addition, using the p-HABC may stimulate further studies on the early diagnosis and treatment of PICS in ICU survivors in Iran.
Ethical Considerations
Compliance with ethical guidelines
Permission was obtained from the developer of the HABC-M-SR. All study procedures were approved by the Ethics Committee of Ahvaz University of Medical Sciences (Code: IR.AJUMS.REC.1399.744). Informed consent was obtained from all participants included in the study.
Funding
This study was extracted from MSc thesis of the Mehdi Bahran Ahmadi at Ahvaz Jundishapur University of Medical Sciences (Code: n.n000344).
Authors contributions
Conceptualization: Mehdi Behran Ahmadi, Nada Sayadi, and Simin Jahani; Investigation, writing the original draft: Mehdi Behran Ahmadi, Nada Sayadi, Simin Jahani, and Amir Elhaee; Writing, review, and editing, methodology, and resources: All authors; Supervision, project administration, funding acquisition: Nada Sayadi; Software, validation, formal analysis, data curation: Amir Elhaee; Visualization: Mehdi Behran Ahmadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The research team would like to express their deepest gratitude to the management, personnel, and patients of ICU departments of Golestan, Imam, and Razi hospitals, and the Office of Deputy Vice-chancellor for Research at Ahvaz Jundishapur University of Medical Sciences.
References
Full-Text: (143 Views)
Introduction
Advances in intensive care medicine and nursing, standardization of medications and respiratory support equipment of intensive care units (ICUs), and focused training programs have significantly reduced mortality in these units and resulted in more patients recovering from acute and critical illnesses [1, 2]. However, many ICU survivors suffer from functional disabilities and significant physical, psychological, and cognitive impairments [3]. The society of critical care medicine has termed these disorders post-intensive care syndrome (PICS) [4]. The PICS encompasses a range of symptoms (i.e. neuromuscular weakness, impaired thinking and judgment, and mental impairment) that occur when patients are hospitalized in the ICU or after discharge from this department [3]. This syndrome occurs in 50% to 70% of ICU survivors, may persist for 5 to 15 years after hospital discharge [5], and adversely affects the mental health of the patients’ family caregivers [6].
Cognitive impairment is one of the fundamental elements of PICS. The prevalence of perceptive impairment in ICU survivors varies between 25% and 75% [7, 8]. The prevalence of PICS may be even higher because mild neurocognitive impairments are difficult to diagnose, and therefore, mild PICS often remains undiagnosed [9]. Mental disorders are another component of PICS. The threat of evolving psychological disorders, for instance, depression, anxiety, and post-traumatic stress disorder (PTSD) after discharge from the ICU, ranges from 1% to 62%. Risk factors for mental disorders are the same as those for cognitive impairment, but other risk factors comprise female gender, lower ranks of instruction, preexisting disability, and receiving sedatives and analgesics in the ICU [10, 11]. Physical impairments are the third component of PICS. Physical impairments involve pulmonary dysfunction, neuromuscular weakness, decreased activity, stiffness of major joints, foot drop, and inability to return to work, occurring in 25% to 80% of ICU survivors and may persist for more than 5 years after hospital discharge [12].
According to ICU guidelines, all ICU survivors should be screened for PICS within 1 year of discharge to facilitate recovery and early diagnosis and treatment of this syndrome [13]. Nurses play a key role in implementing PICS preventive measures. However, a primary difficulty in achieving this goal is the absence of valid instruments to easily assess the three components of PICS [5]. To address this need, Wang et al. developed the self-report form of the healthy aging brain care monitor (HABC-M-SR) questionnaire. This instrument enables healthcare professionals, including nurses, to identify patients with PICS symptoms and refer them to relevant specialists [5]. This questionnaire is widely used in the United States and has demonstrated acceptable validity and reliability. Considering the importance of early diagnosis of PICS and its role in accelerating rehabilitation, advancing quality of life, and reducing costs for patients and their families, the current study was designed to translate and examine the psychometric properties of the Persian form of the HABC-M-SR (p-HABC).
Materials and Methods
A methodological study was conducted on adult patients discharged from the ICUs of five teaching hospitals (i.e. Imam, Golestan, Razi, Sina, and Beqaei hospitals) of Ahvaz University of Medical Sciences, Ahvaz City, Iran.
The translation phase
First, written approval was taken via email from the developer of the first instrument. Then, the HABC-M-SR was translated based on the technique defined by Wild et al. [14]. In this regard, the English form of the HABC-M-SR was individually translated into Persian by two people fluent in Persian and English. One of the translators was also acquainted with medical terminology, but the other was not. The translations were then reviewed and compared by a panel of experts. They verified the translations’ spelling, grammar, and fluency, made necessary revisions, and prepared a single Persian version of the questionnaire. The Persian translation and a copy of the original English instrument were presented to two experts fluent in Persian and English, who were not involved in earlier steps, to check the correspondence between the translated draft and the original instrument. After their approval, the Persian version was passed to a Persian language expert for vocabulary and grammar checking and editing. The Persian HABC-M-SR (p-HABC) was then back-translated into English via another bilingual translator fluent in Persian and English and familiar with the relevant texts. The back-translated English form was emailed to the initial developer, who checked it for similarity to the original version and commented on bugs. Afterward, 10 people from the target groups (i.e. ICU nurses and patients discharged from the ICU) were invited to judgment on the suitability of wording, readability, ambiguity, and understandability of the items in the Persian version. Amendments were created on the comments received, and the p-HABC was finally prepared for psychometric assessments. In addition, the time required to complete the questionnaire was estimated at this stage.
Face validity
For the qualitative face validity, the researcher asked 10 patients and 10 nurses to assess the questionnaire’s clarity, simplicity, and fluency. For the quantitative face validity assessment, 10 patients were asked to rate the significance of the instrument’s items on a 5-point Likert scale from 1 (not important) to 5 (absolutely important). Accordingly, the impact score of the items was estimated by Equation 1:
1. Impact score=Importance×Frequency (%)
The impact score of an item was determined by multiplying the frequency of patients who had rated the item as 4 or 5 by the mean importance score of that item. Items with an impact score above 1.5 were kept for further analysis [14, 15].
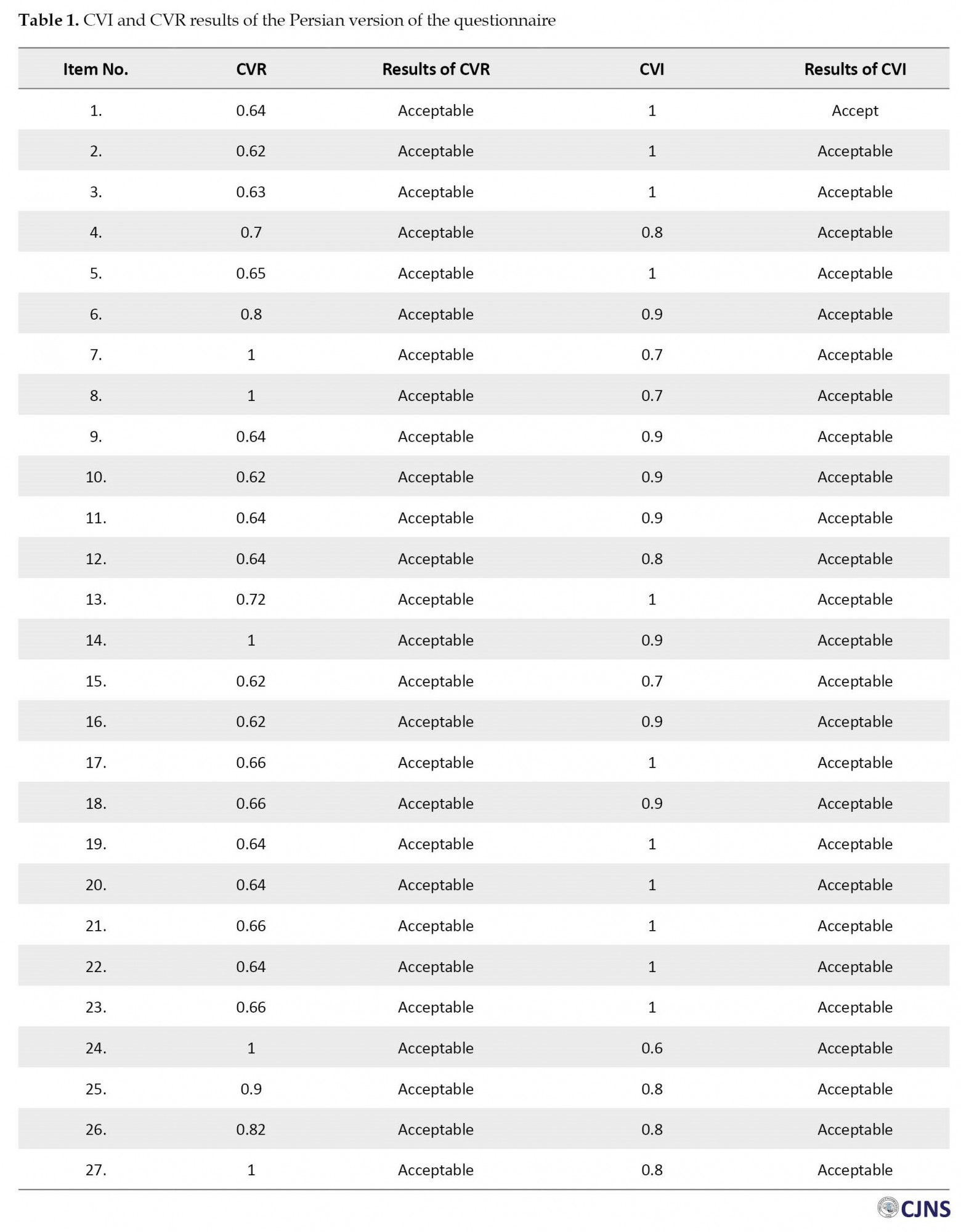
Content validity
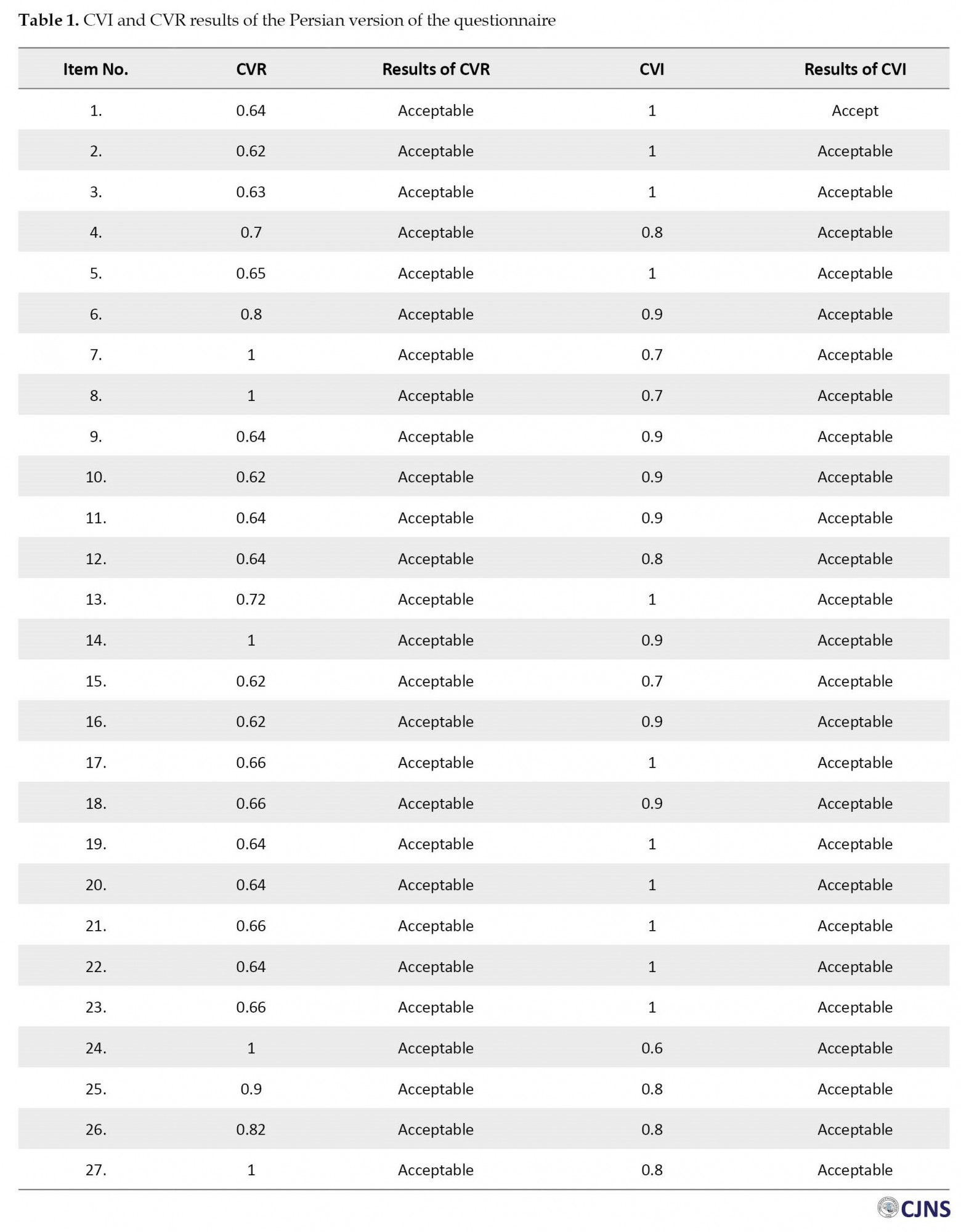
For assessing the qualitative content validity, 15 experts in nursing, critical care, and psychometric assessment (10 nurses with PhDs, 2 ICU nurses, and 3 anesthesiologists) were invited to review the instrument in detail and share their views on the wording, grammar, simplicity, and clarity of the items. They also commented on the importance and main aspects of the concept and the components and entirety of the questionnaire. Amendments were then made to the items by the research team [16]. In the quantitative content validity assessment, the content validity ratio (CVR) and content validity index (CVI) were evaluated, and the specialists shared their opinions on the essentiality and relevance of the items. The relevance of the items is usually considered more important [17].
Construct validity
The sample size was defined according to the preconditions of factor analysis. It is recommended to select 5 to 10 subjects per item [14, 18]. In this study, 10 subjects were selected for each item. Since the p-HABC includes 27 items, 270 eligible patients were recruited from the ICUs mentioned above.
The inclusion criteria included age older than 18 years, hospitalization in the ICU, receiving mechanical ventilation for more than 48 hours, and a medical recommendation for post-discharge follow-up [5]. Patients with neurologic disorders, those who received palliative care during the study, and those who withdrew from the study were excluded [5]. Data were gathered by a demographic information form and the HABC-M-SR questionnaire. After data collection, exploratory and confirmatory factor analysis was performed.
Hidden latent factors were extracted through exploratory factor analysis (EFA). Sampling sufficiency was examined by the Kaiser-Meyer-Olkin (KMO) test. Bartlett’s test of sphericity was used to verify the appropriateness of the data for EFA and the significant correlation between items. KMO values of 0.7-0.8 and 0.8-0.9 are counted as good and large, respectively [19]. Principal component analysis with varimax rotation was used to obtain the latent factors, and eigenvalues and scree plots were utilized to verify the number of factors. Statistical analyses were performed by the SPSS software, version 22.
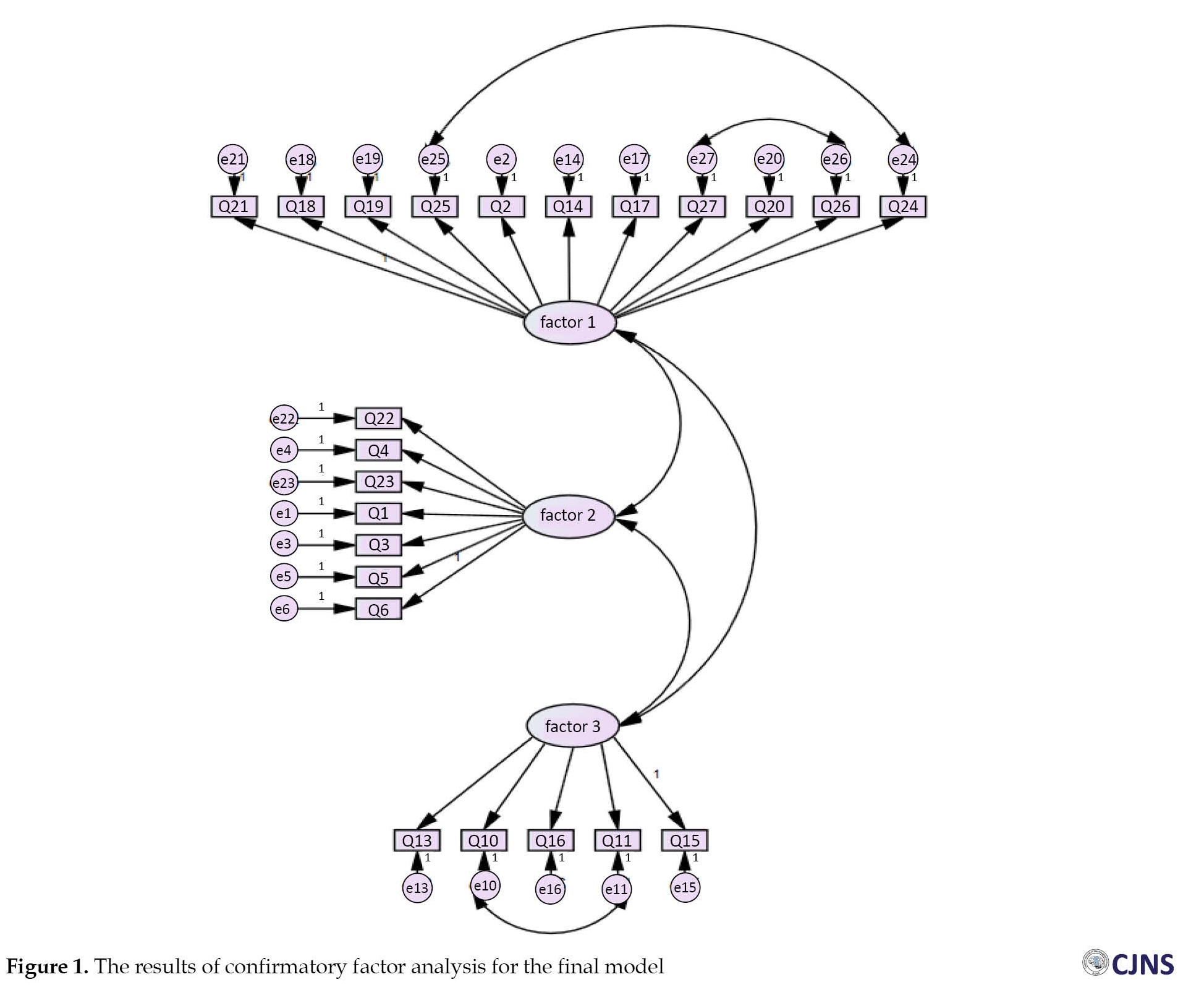
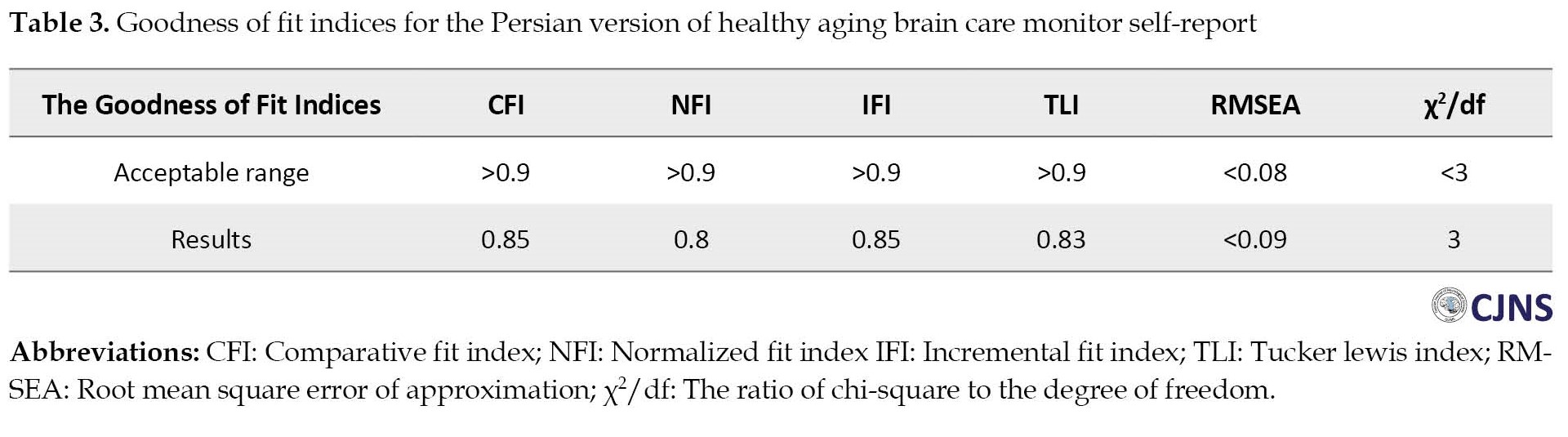
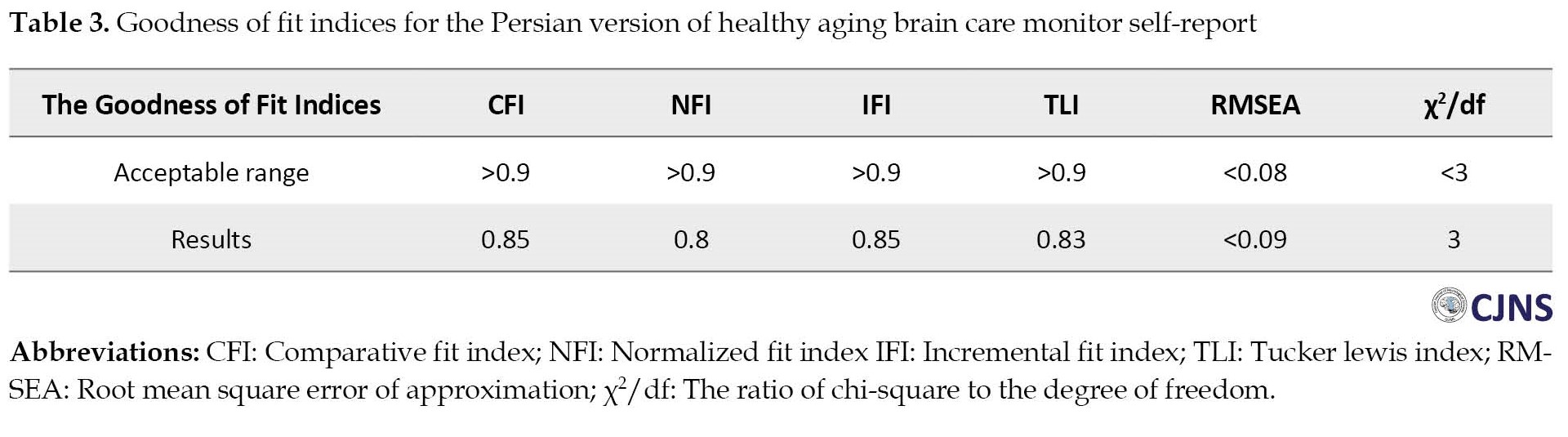
In confirmatory factor analysis (CFA), the most common goodness of fit indicators (i.e. chi-square, goodness-of-fit index, root mean square error of approximation (RMSEA), comparative fit index (CFI), normalized fit index (NFI), modified goodness-of-fit, and the ratio of chi-square to the degree of freedom (χ2/df) and maximum likelihood were used to check the model based on the accepted thresholds. CFA was performed using the AMOS software [20].
Reliability and stability
The internal consistency of the whole instrument (final version) and its subscales (factors extracted in factor analysis) was calculated using the Cronbach α coefficient. Moreover, the stability of the scale was checked by the test-retest procedure, and the interclass correlation coefficient (ICC) was calculated.
Results
Face and content validity
The Persian form of the HABC-M-SR consisted of 23 items. In the qualitative and quantitative face validity phase, the questions were found suitable for subsequent analysis, and all items had an impact score greater than 1.5. Also, the CVI value of all items was greater than 0.79 and the CVR value of all items was greater than 0.62. Therefore, no other items were excluded in the content validity evaluation, according to the Lawshe scale Table 1.
Then exploratory factor analysis was done, 4 questions were removed from the main questionnaire, confirmatory factor analysis was done for 23 questions, and all indicators of confirmatory factor analysis were within the acceptable range.
Construct validity
Patients had a mean age of 52.82±16.49 years and spent 10.87±15.13 and 16.35±16.41 days in the ICU and hospital, respectively (Table 2).

The findings of the KMO test (test value: 0.879, P<0.0001) and (Bartlett’s test=3) showed that the sample size and figures were appropriate for factor analysis. Four items (i.e. items 7, 8, 9, and 12) were removed during EFA because of low factor loading values, and a single factor was extracted that could explain 55.297% of the total variance of the total score of the Persian HABC-M-SR. Regarding CFA, all indices were within acceptable ranges, confirming an acceptable model fit (Figure 1) and Table 3.
Advances in intensive care medicine and nursing, standardization of medications and respiratory support equipment of intensive care units (ICUs), and focused training programs have significantly reduced mortality in these units and resulted in more patients recovering from acute and critical illnesses [1, 2]. However, many ICU survivors suffer from functional disabilities and significant physical, psychological, and cognitive impairments [3]. The society of critical care medicine has termed these disorders post-intensive care syndrome (PICS) [4]. The PICS encompasses a range of symptoms (i.e. neuromuscular weakness, impaired thinking and judgment, and mental impairment) that occur when patients are hospitalized in the ICU or after discharge from this department [3]. This syndrome occurs in 50% to 70% of ICU survivors, may persist for 5 to 15 years after hospital discharge [5], and adversely affects the mental health of the patients’ family caregivers [6].
Cognitive impairment is one of the fundamental elements of PICS. The prevalence of perceptive impairment in ICU survivors varies between 25% and 75% [7, 8]. The prevalence of PICS may be even higher because mild neurocognitive impairments are difficult to diagnose, and therefore, mild PICS often remains undiagnosed [9]. Mental disorders are another component of PICS. The threat of evolving psychological disorders, for instance, depression, anxiety, and post-traumatic stress disorder (PTSD) after discharge from the ICU, ranges from 1% to 62%. Risk factors for mental disorders are the same as those for cognitive impairment, but other risk factors comprise female gender, lower ranks of instruction, preexisting disability, and receiving sedatives and analgesics in the ICU [10, 11]. Physical impairments are the third component of PICS. Physical impairments involve pulmonary dysfunction, neuromuscular weakness, decreased activity, stiffness of major joints, foot drop, and inability to return to work, occurring in 25% to 80% of ICU survivors and may persist for more than 5 years after hospital discharge [12].
According to ICU guidelines, all ICU survivors should be screened for PICS within 1 year of discharge to facilitate recovery and early diagnosis and treatment of this syndrome [13]. Nurses play a key role in implementing PICS preventive measures. However, a primary difficulty in achieving this goal is the absence of valid instruments to easily assess the three components of PICS [5]. To address this need, Wang et al. developed the self-report form of the healthy aging brain care monitor (HABC-M-SR) questionnaire. This instrument enables healthcare professionals, including nurses, to identify patients with PICS symptoms and refer them to relevant specialists [5]. This questionnaire is widely used in the United States and has demonstrated acceptable validity and reliability. Considering the importance of early diagnosis of PICS and its role in accelerating rehabilitation, advancing quality of life, and reducing costs for patients and their families, the current study was designed to translate and examine the psychometric properties of the Persian form of the HABC-M-SR (p-HABC).
Materials and Methods
A methodological study was conducted on adult patients discharged from the ICUs of five teaching hospitals (i.e. Imam, Golestan, Razi, Sina, and Beqaei hospitals) of Ahvaz University of Medical Sciences, Ahvaz City, Iran.
The translation phase
First, written approval was taken via email from the developer of the first instrument. Then, the HABC-M-SR was translated based on the technique defined by Wild et al. [14]. In this regard, the English form of the HABC-M-SR was individually translated into Persian by two people fluent in Persian and English. One of the translators was also acquainted with medical terminology, but the other was not. The translations were then reviewed and compared by a panel of experts. They verified the translations’ spelling, grammar, and fluency, made necessary revisions, and prepared a single Persian version of the questionnaire. The Persian translation and a copy of the original English instrument were presented to two experts fluent in Persian and English, who were not involved in earlier steps, to check the correspondence between the translated draft and the original instrument. After their approval, the Persian version was passed to a Persian language expert for vocabulary and grammar checking and editing. The Persian HABC-M-SR (p-HABC) was then back-translated into English via another bilingual translator fluent in Persian and English and familiar with the relevant texts. The back-translated English form was emailed to the initial developer, who checked it for similarity to the original version and commented on bugs. Afterward, 10 people from the target groups (i.e. ICU nurses and patients discharged from the ICU) were invited to judgment on the suitability of wording, readability, ambiguity, and understandability of the items in the Persian version. Amendments were created on the comments received, and the p-HABC was finally prepared for psychometric assessments. In addition, the time required to complete the questionnaire was estimated at this stage.
Face validity
For the qualitative face validity, the researcher asked 10 patients and 10 nurses to assess the questionnaire’s clarity, simplicity, and fluency. For the quantitative face validity assessment, 10 patients were asked to rate the significance of the instrument’s items on a 5-point Likert scale from 1 (not important) to 5 (absolutely important). Accordingly, the impact score of the items was estimated by Equation 1:
1. Impact score=Importance×Frequency (%)
The impact score of an item was determined by multiplying the frequency of patients who had rated the item as 4 or 5 by the mean importance score of that item. Items with an impact score above 1.5 were kept for further analysis [14, 15].
Content validity
For assessing the qualitative content validity, 15 experts in nursing, critical care, and psychometric assessment (10 nurses with PhDs, 2 ICU nurses, and 3 anesthesiologists) were invited to review the instrument in detail and share their views on the wording, grammar, simplicity, and clarity of the items. They also commented on the importance and main aspects of the concept and the components and entirety of the questionnaire. Amendments were then made to the items by the research team [16]. In the quantitative content validity assessment, the content validity ratio (CVR) and content validity index (CVI) were evaluated, and the specialists shared their opinions on the essentiality and relevance of the items. The relevance of the items is usually considered more important [17].
Construct validity
The sample size was defined according to the preconditions of factor analysis. It is recommended to select 5 to 10 subjects per item [14, 18]. In this study, 10 subjects were selected for each item. Since the p-HABC includes 27 items, 270 eligible patients were recruited from the ICUs mentioned above.
The inclusion criteria included age older than 18 years, hospitalization in the ICU, receiving mechanical ventilation for more than 48 hours, and a medical recommendation for post-discharge follow-up [5]. Patients with neurologic disorders, those who received palliative care during the study, and those who withdrew from the study were excluded [5]. Data were gathered by a demographic information form and the HABC-M-SR questionnaire. After data collection, exploratory and confirmatory factor analysis was performed.
Hidden latent factors were extracted through exploratory factor analysis (EFA). Sampling sufficiency was examined by the Kaiser-Meyer-Olkin (KMO) test. Bartlett’s test of sphericity was used to verify the appropriateness of the data for EFA and the significant correlation between items. KMO values of 0.7-0.8 and 0.8-0.9 are counted as good and large, respectively [19]. Principal component analysis with varimax rotation was used to obtain the latent factors, and eigenvalues and scree plots were utilized to verify the number of factors. Statistical analyses were performed by the SPSS software, version 22.
In confirmatory factor analysis (CFA), the most common goodness of fit indicators (i.e. chi-square, goodness-of-fit index, root mean square error of approximation (RMSEA), comparative fit index (CFI), normalized fit index (NFI), modified goodness-of-fit, and the ratio of chi-square to the degree of freedom (χ2/df) and maximum likelihood were used to check the model based on the accepted thresholds. CFA was performed using the AMOS software [20].
Reliability and stability
The internal consistency of the whole instrument (final version) and its subscales (factors extracted in factor analysis) was calculated using the Cronbach α coefficient. Moreover, the stability of the scale was checked by the test-retest procedure, and the interclass correlation coefficient (ICC) was calculated.
Results
Face and content validity
The Persian form of the HABC-M-SR consisted of 23 items. In the qualitative and quantitative face validity phase, the questions were found suitable for subsequent analysis, and all items had an impact score greater than 1.5. Also, the CVI value of all items was greater than 0.79 and the CVR value of all items was greater than 0.62. Therefore, no other items were excluded in the content validity evaluation, according to the Lawshe scale Table 1.
Then exploratory factor analysis was done, 4 questions were removed from the main questionnaire, confirmatory factor analysis was done for 23 questions, and all indicators of confirmatory factor analysis were within the acceptable range.
Construct validity
Patients had a mean age of 52.82±16.49 years and spent 10.87±15.13 and 16.35±16.41 days in the ICU and hospital, respectively (Table 2).

The findings of the KMO test (test value: 0.879, P<0.0001) and (Bartlett’s test=3) showed that the sample size and figures were appropriate for factor analysis. Four items (i.e. items 7, 8, 9, and 12) were removed during EFA because of low factor loading values, and a single factor was extracted that could explain 55.297% of the total variance of the total score of the Persian HABC-M-SR. Regarding CFA, all indices were within acceptable ranges, confirming an acceptable model fit (Figure 1) and Table 3.
The Cronbach α and ICC of the p-HABC were 0.828 and 0.725, respectively.
Discussion
This research aimed to define the psychometric properties of the Persian HABC-M-SR in patients with PICS. All 27 items of the main questionnaire were found to have suitable face validity. In the content validity check, all the questions were accepted in the CVI and CVR stage. Then, exploratory factor analysis was done, assuming that three factors are constant on the questionnaire. Also, questions 7, 8, 9, and 12 were removed due to low factor loading, and confirmatory factor analysis was performed on 23 questions. The Cronbach α (0.828) and ICC (0.752) results were acceptable. Then, for the remaining 23 questions of the questionnaire, 230 samples were taken, and confirmatory factor analysis was performed, and the results were almost within the acceptable range. Principal component analysis and scree plot confirmed the single-factor structure for 23 items. CFA also confirmed the single-factor structure, and the goodness of fit indices confirmed the fitness of the model examined in this study. Consistent with our results, Monahan et al. have also reported that the HABC-M-SR has good reliability and validity and can be used to measure and monitor the cognitive, functional, and psychological health of older adults attending primary care clinics [21].
The HABC-M-SR can monitor symptoms, provide feedback, and modify care plans in older adults and ICU survivors. In addition, information from the HABC can be relied upon for patients who demonstrate impairment on cognitive tests [21]. Despite technological advances and specialized care provided in ICUs, the symptoms cannot be visible in the post-hospital setting. So, the HABC can contribute to the rapid assessment of a broad span of physical, mental, and perceptive impairments in older adults and ICU survivors. Our findings align with those of Wang et al. and confirm the effectiveness of the HABC-M-SR in measuring the severity of psychological and functional symptoms of PICS [5].
Patients admitted to ICUs experience more severe cognitive, psychological, and functional symptoms than those admitted to other hospital wards. Some studies have also shown that young ICU survivors may suffer from similar aging symptoms as older patients, regardless of age. Therefore, all ICU survivors with cognitive symptoms should undergo detailed neuropsychological examinations. Nonetheless, normal scores on the cognitive subscale should not prevent physicians from more assessment, especially if the patient’s medical history and assessment raise concerns about their cognitive status [5, 22].
Prolonged hospitalization in the ICU is not only very harmful to the health of patients but also negatively impacts society [23]. About one-third of patients who encounter PICS never return to their job, and another third never return to their previous level of work or income. At least 25% of these patients encounter a significant loss of autonomy and need support with activities of regular living one year after ICU discharge, placing a significant load on informal and formal caregivers [24]. Patients who experience PICS experience reduced exercise capacity, incapacity, and cooperated quality of life for months, even years, after intensive care. Instruments such as the HABC-M-SR can help healthcare professionals diagnose patients experiencing PICS early and refer them to relevant specialists to treat their symptoms. Healthcare professionals can easily use such an instrument with little or no expertise to screen and treat PICS symptoms [22].
Conclusion
This research showed the acceptable psychometric properties of the p-HABC questionnaire in patients with PICS. However, this study also has limitations. The HABC-M-SR is suitable for adult patients 18 years of age and older, and the results cannot be generalized to all patients admitted to all ICUs. Among the strengths of this study, the following can be mentioned. This study makes us more familiar with the factors that cause PICS. In addition, using the p-HABC may stimulate further studies on the early diagnosis and treatment of PICS in ICU survivors in Iran.
Ethical Considerations
Compliance with ethical guidelines
Permission was obtained from the developer of the HABC-M-SR. All study procedures were approved by the Ethics Committee of Ahvaz University of Medical Sciences (Code: IR.AJUMS.REC.1399.744). Informed consent was obtained from all participants included in the study.
Funding
This study was extracted from MSc thesis of the Mehdi Bahran Ahmadi at Ahvaz Jundishapur University of Medical Sciences (Code: n.n000344).
Authors contributions
Conceptualization: Mehdi Behran Ahmadi, Nada Sayadi, and Simin Jahani; Investigation, writing the original draft: Mehdi Behran Ahmadi, Nada Sayadi, Simin Jahani, and Amir Elhaee; Writing, review, and editing, methodology, and resources: All authors; Supervision, project administration, funding acquisition: Nada Sayadi; Software, validation, formal analysis, data curation: Amir Elhaee; Visualization: Mehdi Behran Ahmadi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The research team would like to express their deepest gratitude to the management, personnel, and patients of ICU departments of Golestan, Imam, and Razi hospitals, and the Office of Deputy Vice-chancellor for Research at Ahvaz Jundishapur University of Medical Sciences.
References
- Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: Its pathophysiology, prevention, and future directions. Acute Med Surg. 2019; 6(3):233-46. [DOI:10.1002/ams2.415] [PMID] [PMCID]
- Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. Depressive symptoms after critical Illness: A systematic review and meta-analysis. Crit Care Med. 2016; 44(9):1744-53. [DOI:10.1097/CCM.0000000000001811] [PMID] [PMCID]
- Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: An overview. J Transl Int Med. 2017; 5(2):90-2.[DOI:10.1515/jtim-2016-0016] [PMID] [PMCID]
- Fan E, Dowdy DW, Colantuoni E, Mendez-Tellez PA, Sevransky JE, Shanholtz C, et al. Physical complications in acute lung injury survivors: A two-year longitudinal prospective study. Crit Care Med. 2014; 42(4):849-59. [DOI:10.1097/CCM.0000000000000040] [PMID] [PMCID]
- Wang S, Allen D, Perkins A, Monahan P, Khan S, Lasiter S, et al. Validation of a New clinical tool for post-intensive care syndrome. Am J Crit Care. 2019; 28(1):10-8. [DOI:10.4037/ajcc2019639] [PMID] [PMCID]
- Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders' conference. Crit Care Med. 2012; 40(2):502-9. [DOI:10.1097/CCM.0b013e318232da75] [PMID]
- Needham DM, Dinglas VD, Morris PE, Jackson JC, Hough CL, Mendez-Tellez PA, et al. Physical and cognitive performance of patients with acute lung injury 1 year after initial trophic versus full enteral feeding. EDEN trial follow-up. Am J Respir Crit Care Med. 2013; 188(5):567-76. [DOI:10.1164/rccm.201304-0651OC] [PMID] [PMCID]
- Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013; 369(14):1306-16. [DOI:10.1056/NEJMoa1301372] [PMID] [PMCID]
- Burnham EL, Hyzy RC, Paine R, Coley C, Kelly AM, Quint LE, et al. Chest CT features are associated with poorer quality of life in acute lung injury survivors. Crit Care Med. 2013; 41(2):445-56. [DOI:10.1097/CCM.0b013e31826a5062] [PMID] [PMCID]
- Gawlytta R, Brunkhorst F, Niemeyer H, Boettche M, Knaevelsrud C, Rosendahl J. Dyadic post-traumatic stress after intensive care: Case report of a sepsis patient and his wife. Intensive Crit Care Nurs. 2020; 58:102806. [DOI:10.1016/j.iccn.2020.102806] [PMID]
- Wunsch H, Christiansen CF, Johansen MB, Olsen M, Ali N, Angus DC, et al. Psychiatric diagnoses and psychoactive medication use among nonsurgical critically ill patients receiving mechanical ventilation. JAMA. 2014; 311(11):1133-42. [DOI:10.1001/jama.2014.2137] [PMID]
- Kang J, Jeong YJ. Embracing the new vulnerable self: A grounded theory approach on critical care survivors' post-intensive care syndrome. Intensive Crit Care Nurs. 2018; 49:44-50. [DOI:10.1016/j.iccn.2018.08.004] [PMID]
- Milton A, Brück E, Schandl A, Bottai M, Sackey P. Early psychological screening of intensive care unit survivors: A prospective cohort study. Crit Care. 2017; 21(1):273.[DOI:10.1186/s13054-017-1813-z] [PMID] [PMCID]
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005; 8(2):94-104. [DOI:10.1111/j.1524-4733.2005.04054.x] [PMID]
- Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007; 16(2):234-43. [DOI:10.1111/j.1365-2702.2006.01573.x] [PMID]
- Sharif Nia H, Pahlevan Sharif S, Goudarzian AH, Haghdoost AA, Ebadi A, Soleimani MA. [An evaluation of psychometric properties of the templer’s death anxiety scale-extended among a sample of Iranian chemical warfare veterans (Persian)]. Hayat. 2016; 22(3):229-44. [Link]
- Polit DF, Beck CT. Essentials of nursing research: Appraising evidence for nursing practice. 8th ed. Philadelphia : Wolters Kluwer Health; 2014. [Link]
- Worthington RL, Whittaker TA. Scale development research: A content analysis and recommendations for best practices. Couns Psychol. 2006; 34(6):806-38. [DOI:10.1177/0011000006288127]
- Sharif Nia H, Ebadi A, Lehto RH, Mousavi B, Peyrovi H, Chan YH. Reliability and validity of the persian version of templer death anxiety scale-extended in veterans of iran-iraq warfare. Iran J Psychiatry Behav Sci. 2014; 8(4):29-37. [PMID] [PMCID]
- Jaccard J, Wan CK. LISREL approaches to interaction effects in multiple regression. California: SAGE Publications, Inc; 1996. [DOI:10.4135/9781412984782]
- Monahan PO, Alder CA, Khan BA, Stump T, Boustani MA. The healthy aging brain care (HABC) monitor: Validation of the patient self-report version of the clinical tool designed to measure and monitor cognitive, functional, and psychological health. Clin Interv Aging. 2014; 9:2123-32.[DOI:10.2147/CIA.S64140] [PMID] [PMCID]
- Wang S, Allen D, Kheir YN, Campbell N, Khan B. Aging and post-intensive care syndrome: A critical need for geriatric psychiatry. Am J Geriatr Psychiatry. 2018; 26(2):212-21. [DOI:10.1016/j.jagp.2017.05.016] [PMID] [PMCID]
- Elliott D, Davidson JE, Harvey MA, Bemis-Dougherty A, Hopkins RO, Iwashyna TJ, et al. Exploring the scope of post-intensive care syndrome therapy and care: Engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med. 2014; 42(12):2518-26. [DOI:10.1097/CCM.0000000000000525] [PMID]
- Griffiths J, Hatch RA, Bishop J, Morgan K, Jenkinson C, Cuthbertson BH, et al. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: A 12-month follow-up study. Crit Care. 2013; 17(3):R100.[DOI:10.1186/cc12745] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
Received: 2023/07/5 | Accepted: 2023/07/28 | Published: 2023/07/28
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |