Sat, Jan 3, 2026
Volume 10, Issue 3 (Summer 2024)
Caspian J Neurol Sci 2024, 10(3): 190-197 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zargar F, Kolahkaj B, Majdinasab N, Javad Tarrahi M. The Effectiveness of Mindfulness-based Stress Reduction on Sleep Quality in Patients With Multiple Sclerosis. Caspian J Neurol Sci 2024; 10 (3) :190-197
URL: http://cjns.gums.ac.ir/article-1-593-en.html
URL: http://cjns.gums.ac.ir/article-1-593-en.html
1- Behavioral Sciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Clinical Psychology, Faculty of Psychology, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran. ,hodakolahkaj@yahoo.com
3- Physiology Research Center, Ahwaz Jondishapour University of Medical Sciences, Ahwaz, Iran.
4- Department of Epidemiology and Biostatistics, School of Health, Behavioral Sciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Clinical Psychology, Faculty of Psychology, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran. ,
3- Physiology Research Center, Ahwaz Jondishapour University of Medical Sciences, Ahwaz, Iran.
4- Department of Epidemiology and Biostatistics, School of Health, Behavioral Sciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 1215 kb]
(719 Downloads)
| Abstract (HTML) (1176 Views)
Full-Text: (796 Views)
Introduction
In multiple sclerosis (MS), the myelin sheath covering the nerves is damaged [1-4]. MS is the second cause of neurological disability in the young workforce. Moreover, due to the economic burden and chronicity of the disease, MS is costly [1, 2]. The number of people living with MS in the world is estimated at 2.5 million. The prevalence of MS increased from 3.033 per 100000 in 1996 to 183.9 per 100000 in Isfahan City, Iran, in 2021 [3 ,4, 5]. The data suggest that the total prevalence and incidence of MS in Khuzestan Province, Iran, are 16.28 and 2.20, respectively [6]. Fatigue, body temperature rise, sleepiness, and loss of appetite are the most common complaints in MS patients [7].
Sleep disturbance as an illness representation [8], which is often under-recognized and is common in MS. It is argued that 60% of MS patients have sleep problems [9]. Females, compared to males, experience more sleep problems [10]. Sleep quality (SQ) hinges upon the patterns of sleep dysfunction, including delayed sleep, sleep adequacy, sleep disorder, the use of sleeping pills, and drowsiness in the daytime [11]. Poor SQ is associated with fatigue, lack of concentration, low pain threshold, anxiety, inflexible thoughts, and lack of enthusiasm [11].
SQ in MS is also impacted by side effects of medications, such as fatigue, napping, temperature dysregulation, and unpleasant emotional states [12]. Also, muscle spasticity, restless legs, and pain cause difficulties in sleeping for MS patients. Furthermore, frequent nighttime urination reduces the time spent in deep sleep [13]. Poor SQ may affect the efficiency of remyelination processes and symptoms of MS [14].
To treat MS patients’ sleeplessness, antidepressants, particularly clonazepam, are often prescribed [15]. Although sleep problems can be partially tackled with pharmacotherapy, medications have side effects. Several therapeutic techniques have been developed, such as hydrotherapy, occupational therapy, and acupuncture [16].
One psychological therapy is mindfulness-based intervention. It is a short-term group plan, including mindfulness-based stress reduction (MBSR). It involves awareness of internal experiences, attentional control, and acceptance that target sleep disturbances [17]. In MBSR, people are trained to monitor their internal events, including thoughts, emotions, memories, bodily sensations, pain and impulses, and external events (attentional control and experiential awareness). Furthermore, participants are trained to have an objective and non-judgmental approach to their internal and external events (acceptance) [18]. So, they allow their thoughts to exist freely without suppression and accept thoughts as they are and not as reality. Mindfulness training breaks up rumination and anxiety, which can reduce sleeplessness [19 ,20]. Furthermore, MBSR, through these practices and formal and informal practices such as rebreathing, body scan, mindful sitting, etc. could decrease cortisol levels and improve anxiety, muscle spasticity, sleep-related breathing disorders (SRBD), and fatigue, and subsequently, SQ.
On the other hand, sleepless patients tend to attribute every problem, such as fatigue, inaction, slow performance, and temperament disorders, to sleeplessness. Mindfulness reduces concentration on sleeplessness caused by fatigue and slow performance. MBSR is described as waking, living, and consciousness, which is opposed to drowsiness and fatigue, which may lead to better SQ at night. As a result of mindfulness-based programs, enhanced “acceptance” without “judgment” brings about “acceptance” for fatigue during the day and improves SQ [18].
Various studies have reported the efficacy of mindfulness-based intervention on SQ and sleep problems and bedtime destructive critical thoughts in different disorders such as depression, insomnia, and cancer [21-23], as well as SQ in MS [24, 25]. Although these studies reported the effectiveness of mindful practices in SQ, they did not use a specific and structured protocol such as MBSR. So, this study aimed to use a standard protocol (such as MBSR) to improve SQ in MS patients.
Materials and Methods
Statistical population, inclusion, and exclusion criteria
This study is a randomized controlled clinical trial with three phases (pre-test, post-test, and a 2-month follow-up) performed in 2019. The study population comprised all female MS patients aged 20 to 50 referred to Ahvaz City MS Society, Iran, from January to June 2019.
The sample size was calculated based on a previous study in which Pouyanfard, et al [25] investigated the effectiveness of mindfulness-integrated cognitive-behavioral therapy (MBCT) on.
SQ, anxiety, and fatigue in patients with MS. In this study, the Mean±SD values of SQ before the intervention was 19.37±2.12 and changed to 12.37±2.13 after the intervention [25]. According to a 95% confidence interval, test power of 0.90, and a minimum difference of 2.25 in the mean sleep quality scores, and using the Cohen formula [26] for calculating the sample size for comparing two means, 15 subjects were estimated to be needed in each group. However, we recruited 24 patients in each group for more reliable results.
The inclusion criteria for the participants of the study were as follows: Women aged 20 to 50 who were diagnosed with a relapsing-remitting type of MS (which is characterized by recurrent relapses followed by partial or complete recovery), having scores between 1 to 5.5 based on the expanded disability status scale (EDSS) and functional system score (FSS) by neurologists, gaining a cutoff score of more than 7 points in the Pittsburgh sleep quality index (PSQI), lacking other neurological disorders such as dementia, stroke, Parkinson disease, brain tumors, and major psychiatric disorders (according to the structural clinical interview for DSM-5-SCID, administered by a clinical psychologist), holding at least secondary school education, and lacking any other psychotherapy since three months ago. The exclusion criteria of the study were as follows: Suffering from psychiatric disorders, absence of more than three sessions from MBSR therapy, and MS relapse.
Among the patients visiting Ahwaz MS Clinic and signing the consent form, 48 available patients were selected to participate in the briefing, which provided a general explanation of the research procedure and treatment. Then, the patients were randomly allocated to two groups (intervention and control). They were assigned by permuted block random allocation, and each block included 4 participants. During the treatment period, no intervention was applied to the control group. Both groups completed the study questionnaires before, right after, and two months after the treatment period.
Research tools
Pittsburgh SQ index
PSQI is a standard self-report questionnaire developed by Buysse et al. [27] to investigate SQ in the past month. The questionnaire can differentiate favorable and poor SQ and consists of 7 subscales: Subjective SQ, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime drowsiness. The questionnaire is composed of 18 questions. The first four questions concern falling asleep, staying in bed, waking time, and sleep duration. The following 14 questions are scored from 0 to 3 (with 0 indicating no occurrence in a week and 3 suggesting three occurrences during a week). The total score ranges from 0 to 21. Each subscale is assigned a score of 0 to 3, and the total questionnaire score was obtained from the average subscale scores. A high score implies poor SQ. In other words, a score of 5 or higher signifies poor SQ of the subject and moderate problems in at least three fields. A score of 21 indicates the worst SQ, and 0 means the best SQ [28]. The reliability of the questionnaire was estimated to be 0.82 (7). The reliability coefficients of the Persian version of PSQI were 0.79 and 0.89 in two studies [29]. In the current study, the Cronbach α was employed, and the reliability coefficient was 0.89.
Developing the MBSR program
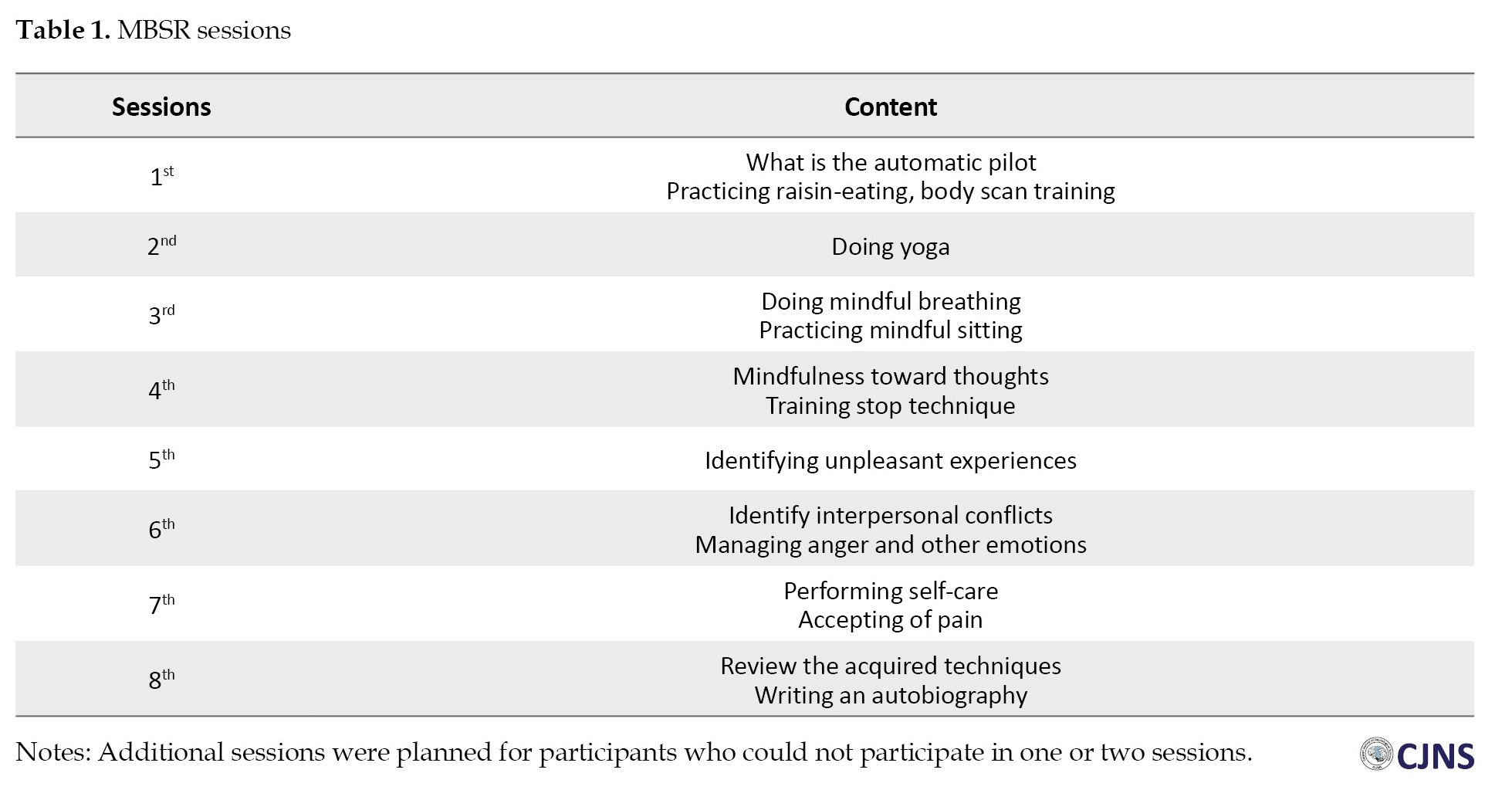
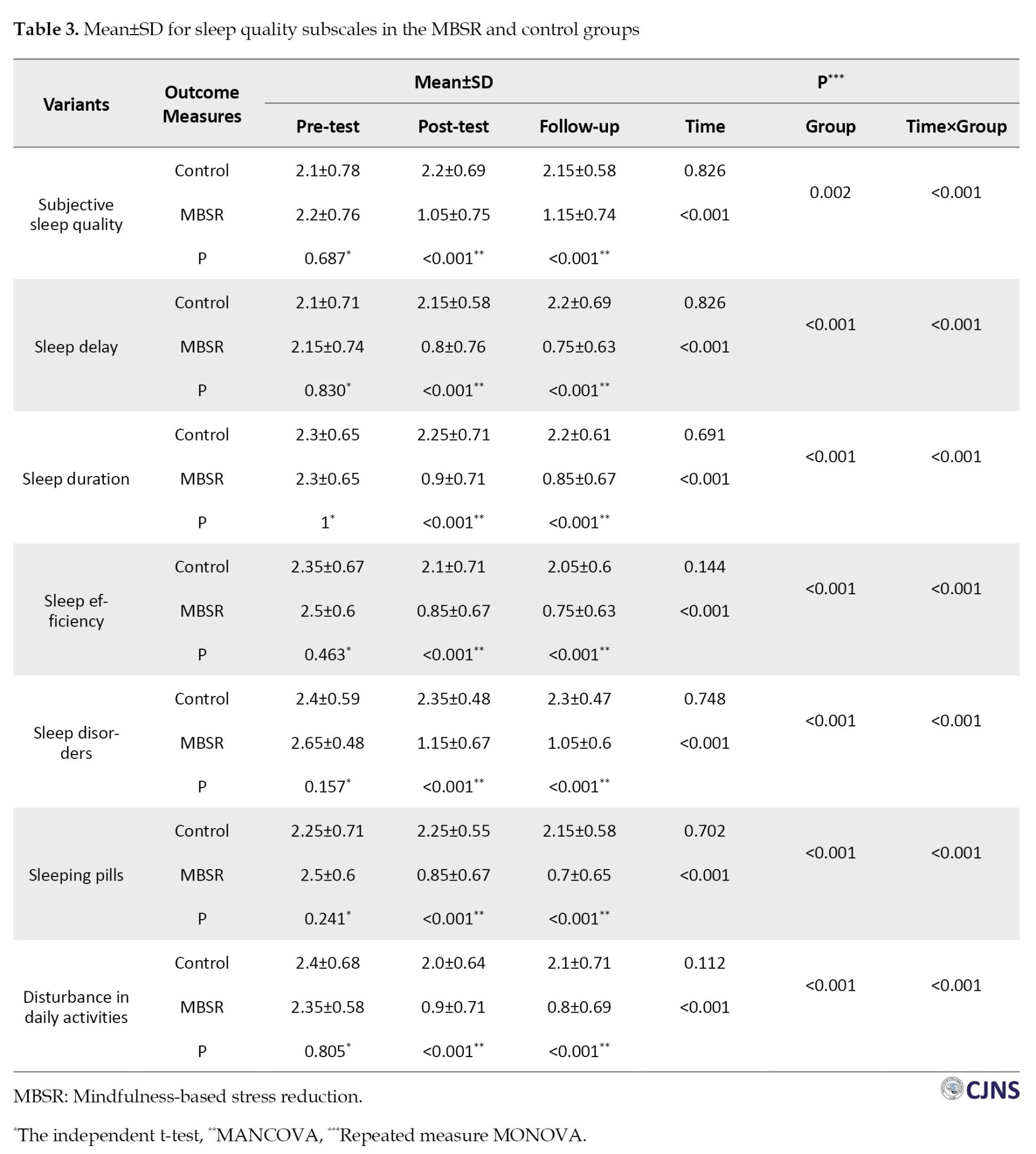
The MBSR group received 8 two-hour treatment sessions of MBSR according to the Kabat-Zinn protocol [30] that a trained clinical psychologist accomplished. The outline of the protocol is shown in Table 1.
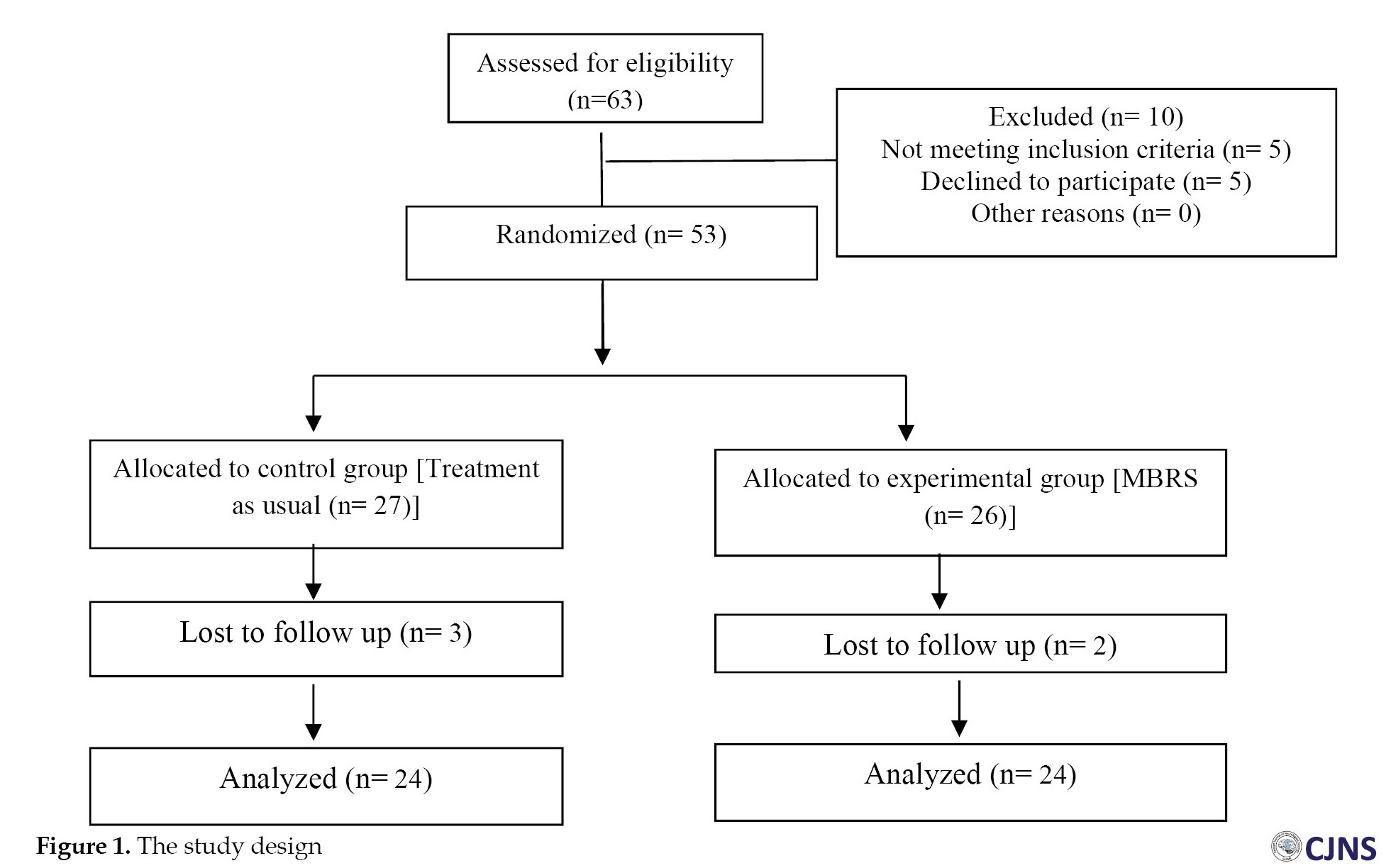
Four patients were excluded from the research due to their absences and relapse to illness (Figure 1). SPSS software, version 19, analyzed the data obtained from PSQI. As regards the descriptive statistics, Mean±SD were evaluated. Regarding inferential statistics, the independent t-test, multivariate analysis of covariance (MANCOVA), and repeated measure of analysis of covariance were utilized.
Results
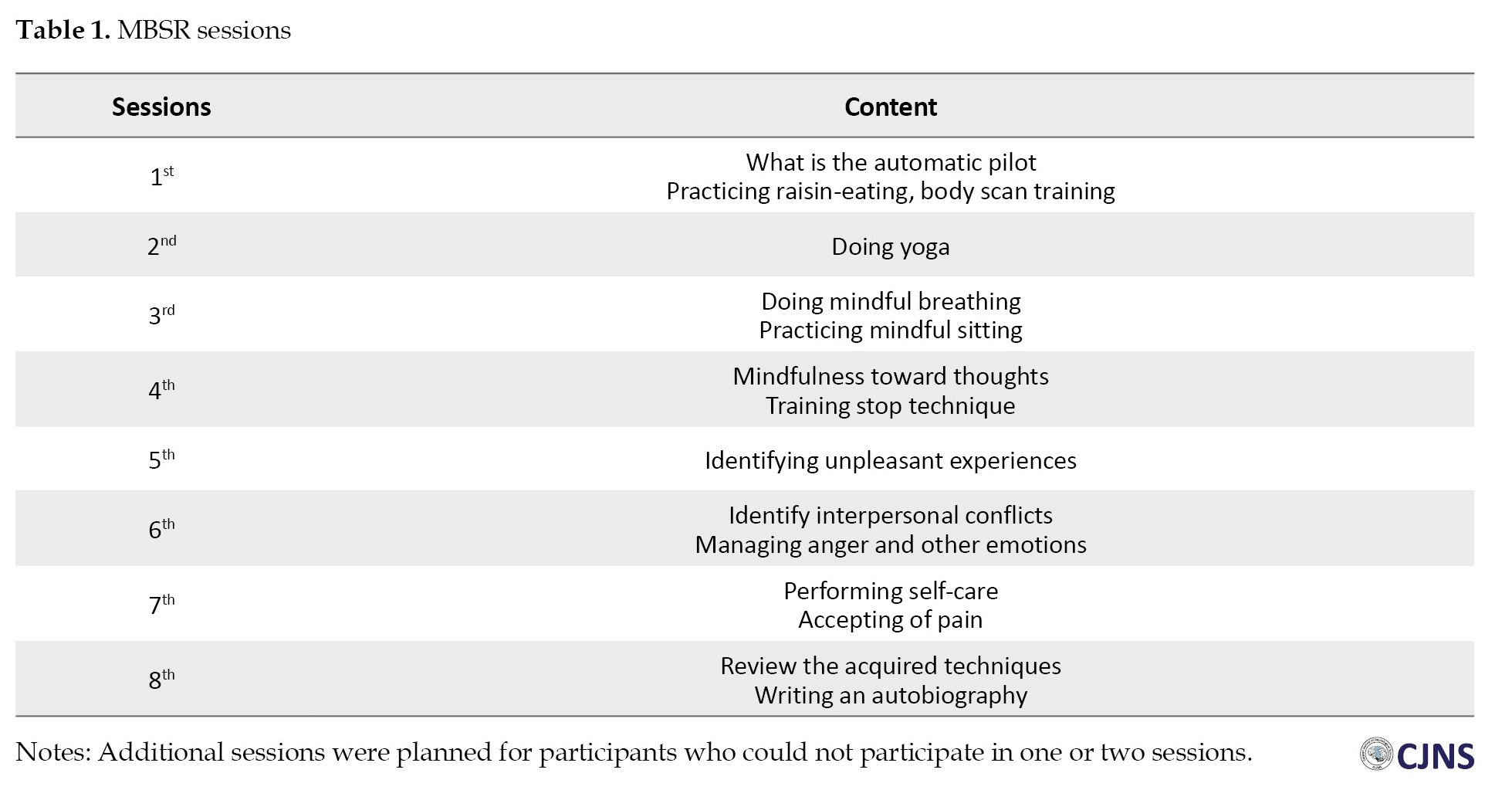
Demographic features of the research samples, including average age, marital status, and educational status, along with the student t-test and chi-squared test, are presented in Table 2.
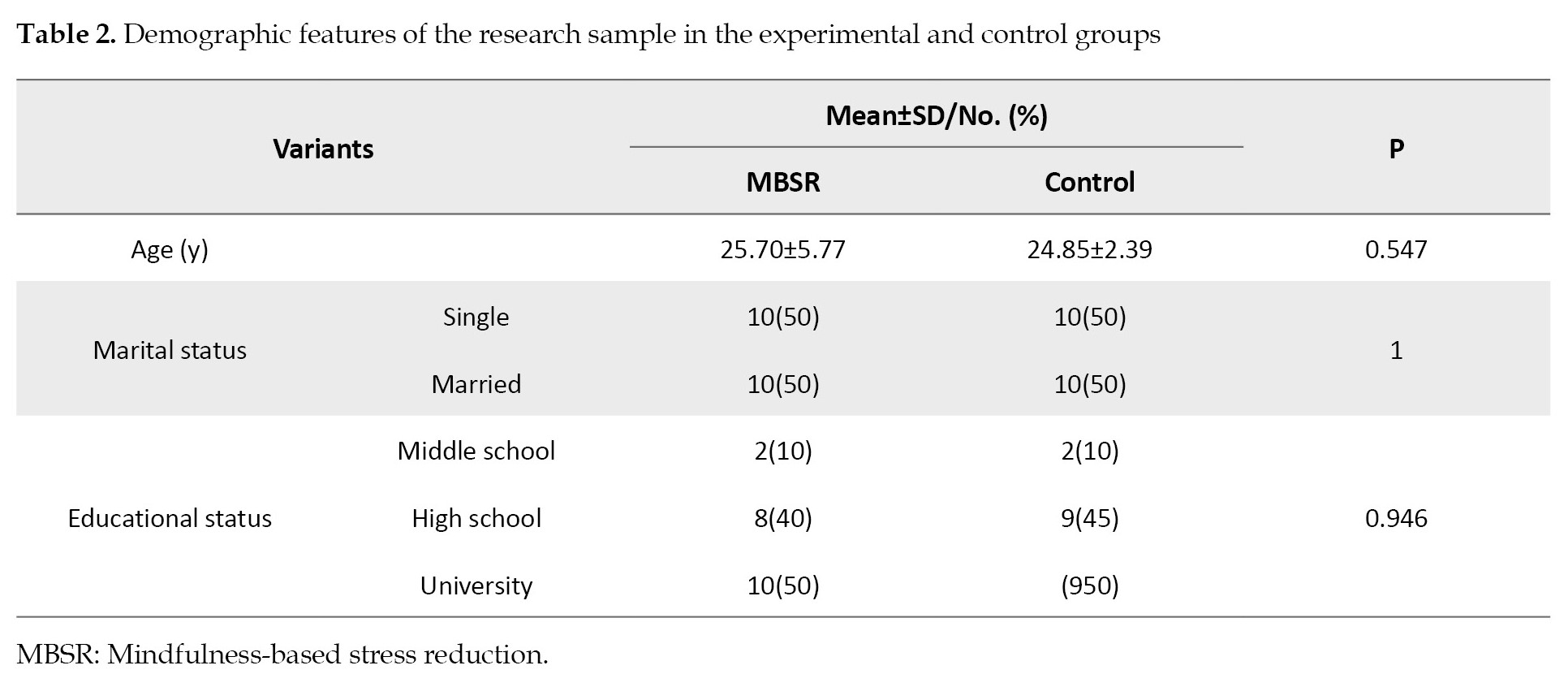
In addition, the frequencies of marital and educational status are given in parentheses.
The chi-square test results show that the two groups are homogeneous regarding marital and educational status. Also, the subjects’ Mean±SD ages are provided for MBSR (25.70±5.77 year) and control groups (24.85±2.39 year). The t-test for the independent samples showed no significant differences between 2 groups (P=0.547).
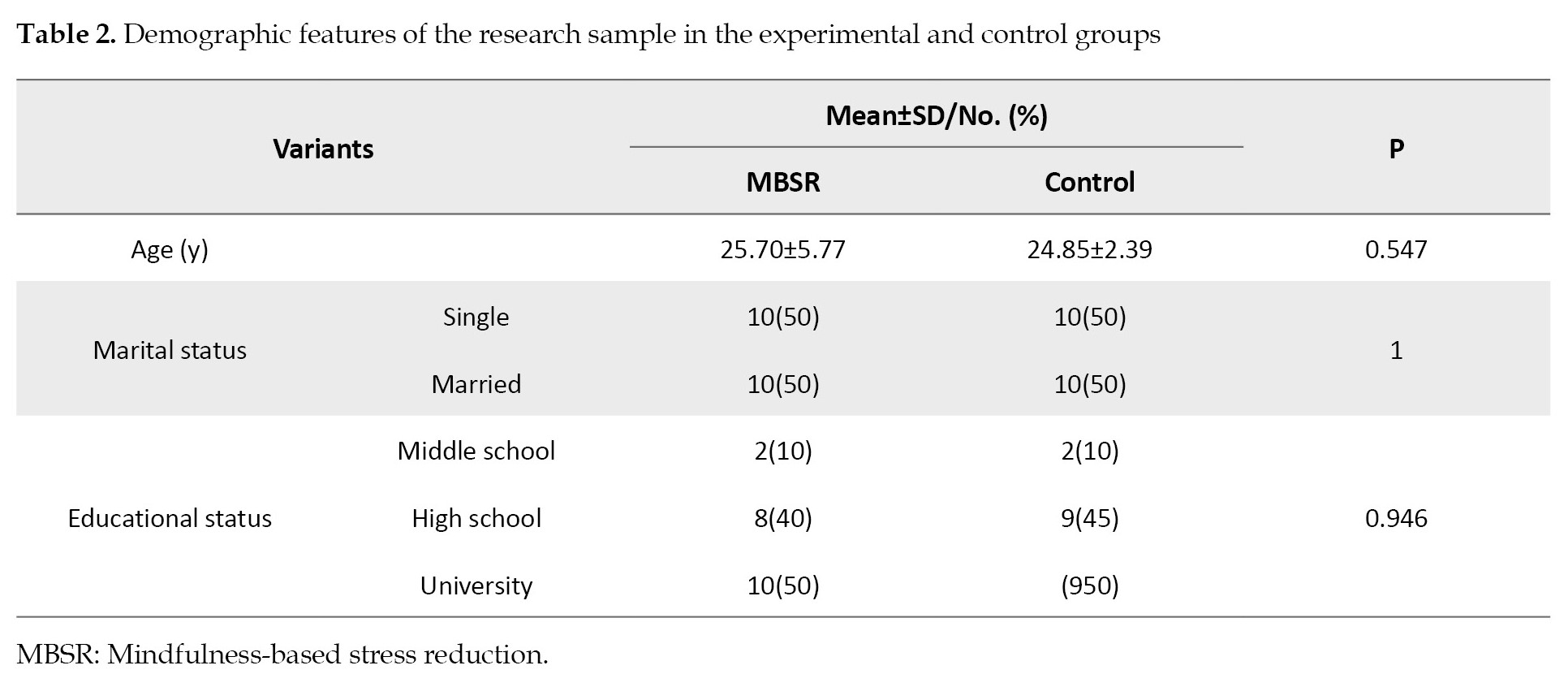
Table 3 presents the Mean±SD of the scores for SQ subscales in the pre-test, post-test, and follow-up for MBSR and control groups.
A frequency measure test was employed to check out the significance of the difference. Regarding the equality of covariance matrices, the analysis of the results obtained from the M-box test revealed satisfactory homogeneity in variance and covariance matrix. In other words, covariance matrices of the dependent variants were equal in all groups (F(28, 5031)=1.155, P=0.21). Moreover, checking the results obtained from Levene’s test for the equality of the error matrices proved that error variances of the dependent variants were identical in all groups (P>0.05). The results of the variance analysis are demonstrated in Table 3.
The results of Table 3 suggested that the two groups had significant differences in three phases. Overall, the obtained results showed the effectiveness of MBSR on SQ in females suffering from MS.
Discussion
This study showed that MBSR positively improved SQ in MS female patients in the post-test and after two months in all subscales of PSQI. Kotterba et al. showed that poor SQ was reported by 55% of MS patients [31]. Consequently, the results of this study were consistent with the other investigations that showed the effectiveness of mindful practices on SQ [17, 21-25]. Some of these studies have specifically used mindful practices for SQ in Ms. For example, Lorenz et al. (2021) studied mindfulness plus sleep education via videoconference compared to onsite education among adults with MS. They reported the effectiveness of the therapy on sleep efficiency and total sleep time [24]. Also, Pouyanfard et al. (2019) investigated the efficacy of mindfulness and cognitive and behavioral techniques on sleep quality in MS [25]. These two studies showed mindfulness’s effect on SQ, but they used a non-randomized wait-list control or did not use a standard mindful protocol such as MBSR. They added some complementary techniques, such as cognitive and behavioral techniques or psychoeducation. It seems these adjunction techniques were used to increase the effect of mindful practices, but our study showed the effect of pure MBSR on SQ. So, we can use this specific protocol that is obvious, feasible and standard.
Recognizing the mechanisms of insomnia could show why MBSR is a suitable psychological treatment. Some studies pointed to cognitive mechanisms of insomnia. For example, Ong et al. [32] showed that insomnia was caused by increased arousal, with negative thoughts causing insomnia, as well as metacognitions related to the interpretation of insomnia. Mindfulness techniques specifically target secondary arousal with an acceptance state. So, people could perceive insomnia as just an event, not a situation that can ruin their whole day [32]. Other studies show that sleepiness is related to other mental conditions such as anxiety, depression, etc. For example, Yu et al. (2022) showed that dispositional mindfulness might buffer against the negative impact of rumination (as a cognitive feature of depression) on sleep problems [33]. Other studies showed mindfulness through reducing these conditions could reduce sleep problems [34]. Mindfulness techniques are practiced all day long to allow a person to react correctly to environmental stressors. Furthermore, people learn to resist “automatic pilot,” conditioning, and harmful reactions. Mindfulness training breaks up rumination, anxiety, and oral dysfunction, which can reduce sleeplessness [34].
On the other hand, investigating the subscales of PSQI can help recognize the mechanisms of MBSR on SQ. The present study showed that MBSR improved all subscales of PSQI. Some items of the sleep disturbance subscale are as follows: Have a bad dream, feel pain, cannot breathe comfortably, cough or snore loudly, and have pauses between breaths (apnea) while asleep. Some questions are related to SRBD. Wang et al. (2023) showed that MBSR could improve apnea in patients with alcohol use disorder [35]. Through training mindful breathing, MBSR can help patients rebreathe during the day and at night. Also, MBSR techniques, through reducing stress, anxiety, and depression, could improve night sleep and SRBD. Furthermore, mindfulness practices could alleviate pain and catastrophizing (a cognitive appraisal of pain harmfulness). Several studies showed the efficacy of mindful practices on pain (i.e. Chen et al. studied MBSR vs cognitive-behavioral therapy for chronic low back pain. They reported the effectiveness of MBSR for pain [36]. Reducing pain may occur through improving the overall quality of life in MS patients. Another subscale of PSQI is daytime dysfunction and MBSR; increasing attention and awareness of daily activities could help patients improve their daily function. On the other hand, improving QOL, sleep disturbance, and daytime dysfunction leads to decreasing sleep latency subscale of PSQI. Rumination and anxiety about past and future events before sleep are the most critical factors that could lead to sleep latency. By improving attention to the present moment and the patient’s mood states, MBSR could decrease these factors and sleep latency. Some studies showed the effect of MBSR on sleep latency. For example, Rung et al. showed a mobile mindfulness meditation intervention could decrease sleep latency [37].
This study had some limitations. It was carried out only with patients with relapsing-remitting type of MS. Also, the patients were not separated regarding severity and types of sleep disorders. Furthermore, this study investigated only the females suffering from MS.
Conclusion
MBSR effectively reduces sleep problems based on PSQI among females with MS.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were conducted in compliance with the ethical guidelines of the 2013 Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences (Code: IR.ARI.MUI.REC.1402.247). This study was registered at Iranian Registry of Clinical Trials (IRCT)(Code: IRCT201507087227N5).
Funding
This study was extracted from a research project (No.: 2402219), funded by Isfahan University of Medical Sciences.
Authors contributions
Conceptualization, methodology and final approval: All authors; Data collection and resources: BentolHoda KolahKaj; Statistical analyses: Fatemeh Zargar and Mohammad Javad Tarrahi; Drafting the original paper: Fatemeh Zarga and Nastaran Majdinasab; Review and editing: Fatemeh Zargar and Nastaran Majdinasab.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are grateful to staff of Ahvaz MS Society and participants.
References
In multiple sclerosis (MS), the myelin sheath covering the nerves is damaged [1-4]. MS is the second cause of neurological disability in the young workforce. Moreover, due to the economic burden and chronicity of the disease, MS is costly [1, 2]. The number of people living with MS in the world is estimated at 2.5 million. The prevalence of MS increased from 3.033 per 100000 in 1996 to 183.9 per 100000 in Isfahan City, Iran, in 2021 [3 ,4, 5]. The data suggest that the total prevalence and incidence of MS in Khuzestan Province, Iran, are 16.28 and 2.20, respectively [6]. Fatigue, body temperature rise, sleepiness, and loss of appetite are the most common complaints in MS patients [7].
Sleep disturbance as an illness representation [8], which is often under-recognized and is common in MS. It is argued that 60% of MS patients have sleep problems [9]. Females, compared to males, experience more sleep problems [10]. Sleep quality (SQ) hinges upon the patterns of sleep dysfunction, including delayed sleep, sleep adequacy, sleep disorder, the use of sleeping pills, and drowsiness in the daytime [11]. Poor SQ is associated with fatigue, lack of concentration, low pain threshold, anxiety, inflexible thoughts, and lack of enthusiasm [11].
SQ in MS is also impacted by side effects of medications, such as fatigue, napping, temperature dysregulation, and unpleasant emotional states [12]. Also, muscle spasticity, restless legs, and pain cause difficulties in sleeping for MS patients. Furthermore, frequent nighttime urination reduces the time spent in deep sleep [13]. Poor SQ may affect the efficiency of remyelination processes and symptoms of MS [14].
To treat MS patients’ sleeplessness, antidepressants, particularly clonazepam, are often prescribed [15]. Although sleep problems can be partially tackled with pharmacotherapy, medications have side effects. Several therapeutic techniques have been developed, such as hydrotherapy, occupational therapy, and acupuncture [16].
One psychological therapy is mindfulness-based intervention. It is a short-term group plan, including mindfulness-based stress reduction (MBSR). It involves awareness of internal experiences, attentional control, and acceptance that target sleep disturbances [17]. In MBSR, people are trained to monitor their internal events, including thoughts, emotions, memories, bodily sensations, pain and impulses, and external events (attentional control and experiential awareness). Furthermore, participants are trained to have an objective and non-judgmental approach to their internal and external events (acceptance) [18]. So, they allow their thoughts to exist freely without suppression and accept thoughts as they are and not as reality. Mindfulness training breaks up rumination and anxiety, which can reduce sleeplessness [19 ,20]. Furthermore, MBSR, through these practices and formal and informal practices such as rebreathing, body scan, mindful sitting, etc. could decrease cortisol levels and improve anxiety, muscle spasticity, sleep-related breathing disorders (SRBD), and fatigue, and subsequently, SQ.
On the other hand, sleepless patients tend to attribute every problem, such as fatigue, inaction, slow performance, and temperament disorders, to sleeplessness. Mindfulness reduces concentration on sleeplessness caused by fatigue and slow performance. MBSR is described as waking, living, and consciousness, which is opposed to drowsiness and fatigue, which may lead to better SQ at night. As a result of mindfulness-based programs, enhanced “acceptance” without “judgment” brings about “acceptance” for fatigue during the day and improves SQ [18].
Various studies have reported the efficacy of mindfulness-based intervention on SQ and sleep problems and bedtime destructive critical thoughts in different disorders such as depression, insomnia, and cancer [21-23], as well as SQ in MS [24, 25]. Although these studies reported the effectiveness of mindful practices in SQ, they did not use a specific and structured protocol such as MBSR. So, this study aimed to use a standard protocol (such as MBSR) to improve SQ in MS patients.
Materials and Methods
Statistical population, inclusion, and exclusion criteria
This study is a randomized controlled clinical trial with three phases (pre-test, post-test, and a 2-month follow-up) performed in 2019. The study population comprised all female MS patients aged 20 to 50 referred to Ahvaz City MS Society, Iran, from January to June 2019.
The sample size was calculated based on a previous study in which Pouyanfard, et al [25] investigated the effectiveness of mindfulness-integrated cognitive-behavioral therapy (MBCT) on.
SQ, anxiety, and fatigue in patients with MS. In this study, the Mean±SD values of SQ before the intervention was 19.37±2.12 and changed to 12.37±2.13 after the intervention [25]. According to a 95% confidence interval, test power of 0.90, and a minimum difference of 2.25 in the mean sleep quality scores, and using the Cohen formula [26] for calculating the sample size for comparing two means, 15 subjects were estimated to be needed in each group. However, we recruited 24 patients in each group for more reliable results.
The inclusion criteria for the participants of the study were as follows: Women aged 20 to 50 who were diagnosed with a relapsing-remitting type of MS (which is characterized by recurrent relapses followed by partial or complete recovery), having scores between 1 to 5.5 based on the expanded disability status scale (EDSS) and functional system score (FSS) by neurologists, gaining a cutoff score of more than 7 points in the Pittsburgh sleep quality index (PSQI), lacking other neurological disorders such as dementia, stroke, Parkinson disease, brain tumors, and major psychiatric disorders (according to the structural clinical interview for DSM-5-SCID, administered by a clinical psychologist), holding at least secondary school education, and lacking any other psychotherapy since three months ago. The exclusion criteria of the study were as follows: Suffering from psychiatric disorders, absence of more than three sessions from MBSR therapy, and MS relapse.
Among the patients visiting Ahwaz MS Clinic and signing the consent form, 48 available patients were selected to participate in the briefing, which provided a general explanation of the research procedure and treatment. Then, the patients were randomly allocated to two groups (intervention and control). They were assigned by permuted block random allocation, and each block included 4 participants. During the treatment period, no intervention was applied to the control group. Both groups completed the study questionnaires before, right after, and two months after the treatment period.
Research tools
Pittsburgh SQ index
PSQI is a standard self-report questionnaire developed by Buysse et al. [27] to investigate SQ in the past month. The questionnaire can differentiate favorable and poor SQ and consists of 7 subscales: Subjective SQ, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime drowsiness. The questionnaire is composed of 18 questions. The first four questions concern falling asleep, staying in bed, waking time, and sleep duration. The following 14 questions are scored from 0 to 3 (with 0 indicating no occurrence in a week and 3 suggesting three occurrences during a week). The total score ranges from 0 to 21. Each subscale is assigned a score of 0 to 3, and the total questionnaire score was obtained from the average subscale scores. A high score implies poor SQ. In other words, a score of 5 or higher signifies poor SQ of the subject and moderate problems in at least three fields. A score of 21 indicates the worst SQ, and 0 means the best SQ [28]. The reliability of the questionnaire was estimated to be 0.82 (7). The reliability coefficients of the Persian version of PSQI were 0.79 and 0.89 in two studies [29]. In the current study, the Cronbach α was employed, and the reliability coefficient was 0.89.
Developing the MBSR program
The MBSR group received 8 two-hour treatment sessions of MBSR according to the Kabat-Zinn protocol [30] that a trained clinical psychologist accomplished. The outline of the protocol is shown in Table 1.
Four patients were excluded from the research due to their absences and relapse to illness (Figure 1). SPSS software, version 19, analyzed the data obtained from PSQI. As regards the descriptive statistics, Mean±SD were evaluated. Regarding inferential statistics, the independent t-test, multivariate analysis of covariance (MANCOVA), and repeated measure of analysis of covariance were utilized.
Results
Demographic features of the research samples, including average age, marital status, and educational status, along with the student t-test and chi-squared test, are presented in Table 2.
In addition, the frequencies of marital and educational status are given in parentheses.
The chi-square test results show that the two groups are homogeneous regarding marital and educational status. Also, the subjects’ Mean±SD ages are provided for MBSR (25.70±5.77 year) and control groups (24.85±2.39 year). The t-test for the independent samples showed no significant differences between 2 groups (P=0.547).
Table 3 presents the Mean±SD of the scores for SQ subscales in the pre-test, post-test, and follow-up for MBSR and control groups.
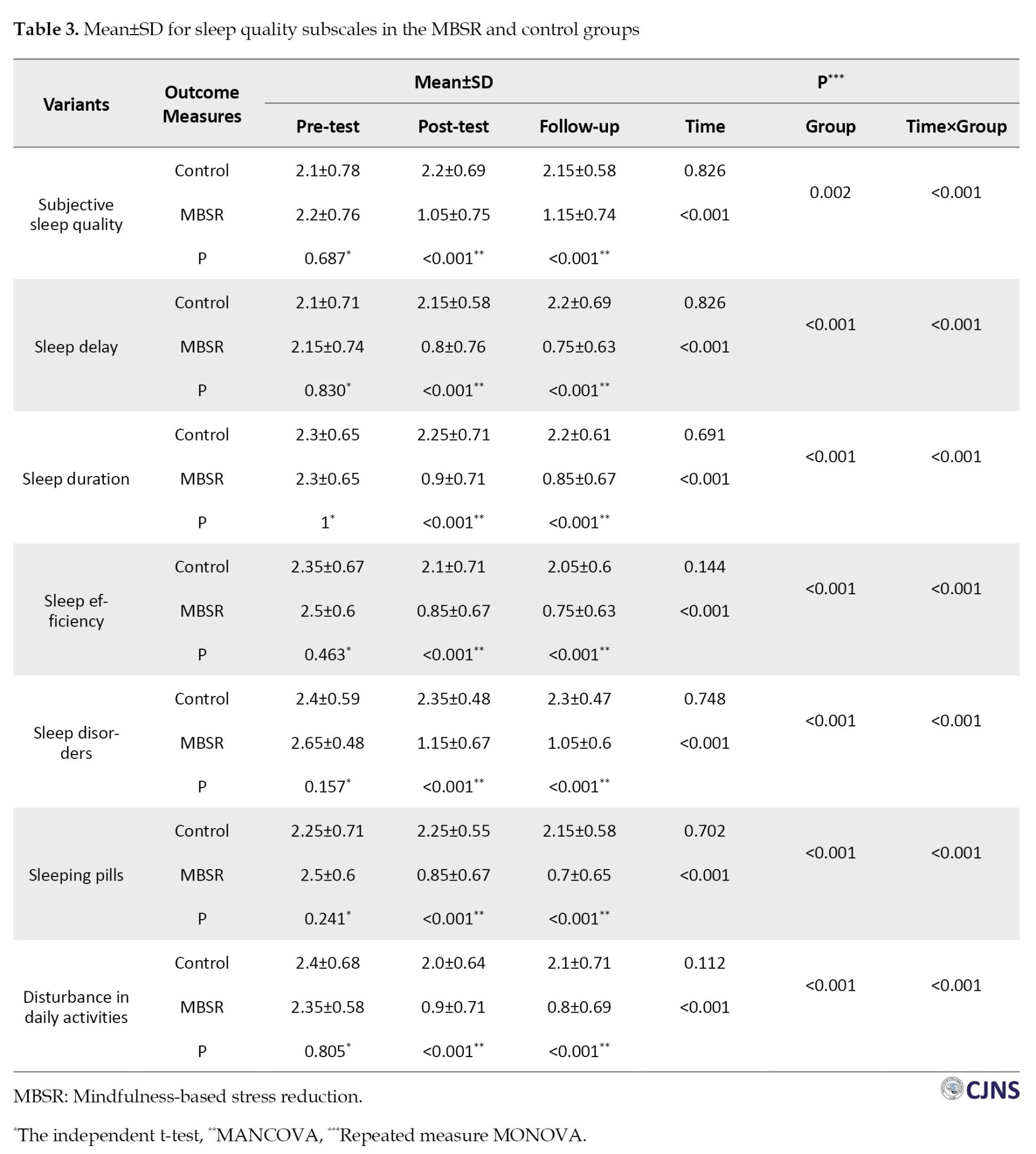
A frequency measure test was employed to check out the significance of the difference. Regarding the equality of covariance matrices, the analysis of the results obtained from the M-box test revealed satisfactory homogeneity in variance and covariance matrix. In other words, covariance matrices of the dependent variants were equal in all groups (F(28, 5031)=1.155, P=0.21). Moreover, checking the results obtained from Levene’s test for the equality of the error matrices proved that error variances of the dependent variants were identical in all groups (P>0.05). The results of the variance analysis are demonstrated in Table 3.
The results of Table 3 suggested that the two groups had significant differences in three phases. Overall, the obtained results showed the effectiveness of MBSR on SQ in females suffering from MS.
Discussion
This study showed that MBSR positively improved SQ in MS female patients in the post-test and after two months in all subscales of PSQI. Kotterba et al. showed that poor SQ was reported by 55% of MS patients [31]. Consequently, the results of this study were consistent with the other investigations that showed the effectiveness of mindful practices on SQ [17, 21-25]. Some of these studies have specifically used mindful practices for SQ in Ms. For example, Lorenz et al. (2021) studied mindfulness plus sleep education via videoconference compared to onsite education among adults with MS. They reported the effectiveness of the therapy on sleep efficiency and total sleep time [24]. Also, Pouyanfard et al. (2019) investigated the efficacy of mindfulness and cognitive and behavioral techniques on sleep quality in MS [25]. These two studies showed mindfulness’s effect on SQ, but they used a non-randomized wait-list control or did not use a standard mindful protocol such as MBSR. They added some complementary techniques, such as cognitive and behavioral techniques or psychoeducation. It seems these adjunction techniques were used to increase the effect of mindful practices, but our study showed the effect of pure MBSR on SQ. So, we can use this specific protocol that is obvious, feasible and standard.
Recognizing the mechanisms of insomnia could show why MBSR is a suitable psychological treatment. Some studies pointed to cognitive mechanisms of insomnia. For example, Ong et al. [32] showed that insomnia was caused by increased arousal, with negative thoughts causing insomnia, as well as metacognitions related to the interpretation of insomnia. Mindfulness techniques specifically target secondary arousal with an acceptance state. So, people could perceive insomnia as just an event, not a situation that can ruin their whole day [32]. Other studies show that sleepiness is related to other mental conditions such as anxiety, depression, etc. For example, Yu et al. (2022) showed that dispositional mindfulness might buffer against the negative impact of rumination (as a cognitive feature of depression) on sleep problems [33]. Other studies showed mindfulness through reducing these conditions could reduce sleep problems [34]. Mindfulness techniques are practiced all day long to allow a person to react correctly to environmental stressors. Furthermore, people learn to resist “automatic pilot,” conditioning, and harmful reactions. Mindfulness training breaks up rumination, anxiety, and oral dysfunction, which can reduce sleeplessness [34].
On the other hand, investigating the subscales of PSQI can help recognize the mechanisms of MBSR on SQ. The present study showed that MBSR improved all subscales of PSQI. Some items of the sleep disturbance subscale are as follows: Have a bad dream, feel pain, cannot breathe comfortably, cough or snore loudly, and have pauses between breaths (apnea) while asleep. Some questions are related to SRBD. Wang et al. (2023) showed that MBSR could improve apnea in patients with alcohol use disorder [35]. Through training mindful breathing, MBSR can help patients rebreathe during the day and at night. Also, MBSR techniques, through reducing stress, anxiety, and depression, could improve night sleep and SRBD. Furthermore, mindfulness practices could alleviate pain and catastrophizing (a cognitive appraisal of pain harmfulness). Several studies showed the efficacy of mindful practices on pain (i.e. Chen et al. studied MBSR vs cognitive-behavioral therapy for chronic low back pain. They reported the effectiveness of MBSR for pain [36]. Reducing pain may occur through improving the overall quality of life in MS patients. Another subscale of PSQI is daytime dysfunction and MBSR; increasing attention and awareness of daily activities could help patients improve their daily function. On the other hand, improving QOL, sleep disturbance, and daytime dysfunction leads to decreasing sleep latency subscale of PSQI. Rumination and anxiety about past and future events before sleep are the most critical factors that could lead to sleep latency. By improving attention to the present moment and the patient’s mood states, MBSR could decrease these factors and sleep latency. Some studies showed the effect of MBSR on sleep latency. For example, Rung et al. showed a mobile mindfulness meditation intervention could decrease sleep latency [37].
This study had some limitations. It was carried out only with patients with relapsing-remitting type of MS. Also, the patients were not separated regarding severity and types of sleep disorders. Furthermore, this study investigated only the females suffering from MS.
Conclusion
MBSR effectively reduces sleep problems based on PSQI among females with MS.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were conducted in compliance with the ethical guidelines of the 2013 Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Isfahan University of Medical Sciences (Code: IR.ARI.MUI.REC.1402.247). This study was registered at Iranian Registry of Clinical Trials (IRCT)(Code: IRCT201507087227N5).
Funding
This study was extracted from a research project (No.: 2402219), funded by Isfahan University of Medical Sciences.
Authors contributions
Conceptualization, methodology and final approval: All authors; Data collection and resources: BentolHoda KolahKaj; Statistical analyses: Fatemeh Zargar and Mohammad Javad Tarrahi; Drafting the original paper: Fatemeh Zarga and Nastaran Majdinasab; Review and editing: Fatemeh Zargar and Nastaran Majdinasab.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are grateful to staff of Ahvaz MS Society and participants.
References
- Gudesblatt M, Xian S, Zarif M, Bumstead B, Thotam S, Fafard L, et al. Multiple Sclerosis & Sleep Disorders: Exploration of Sleep Disordered Breathing -Apnea Hypopnea Index Non-REM versus REM in a Community Cohort of patients with Multiple Sclerosis who Report Fatigue (P1.129). Neurology. 2015; 84(14 Supplement). [Link]
- Schirda B, Nicholas JA, Prakash RS. Examining trait mindfulness, emotion dysregulation, and quality of life in multiple sclerosis. Health Psychol. 2015; 34(11):1107-15. [DOI:10.1037/hea0000215] [PMID]
- Rupprecht S, Kluckow S, Yahiaoui-Doktor M, Aktas O, Chan A, Dressel A, et al. Prevalence of sleep disturbances, fatigue, anxiety and depression in multiple sclerosis (MS) (P1.128). Neurology. 2015. 84(14 Supplement). [Link]
- Amtmann D, Askew RL, Kim J, Chung H, Ehde DM, Bombardier CH, et al. Pain affects depression through anxiety, fatigue, and sleep in multiple sclerosis. Rehabil Psychol. 2015; 60(1):81-90. [DOI:10.1037/rep0000027] [PMID] [PMCID]
- Bagherieh S, Mirmosayyeb O, Vaheb S, Afshari-Safavi A, Barzegar M, Ashtari F, et al. Prevalence and incidence of multiple sclerosis in Isfahan Province, Iran: A 25-Year Population-Based Study. Mult Scler Relat Disord. 2023; 71:104310. [DOI:10.1016/j.msard.2022.104310]
- Zabihi R, Galehdari H, Shafiee M, Kazeminejad SR, Alavi SM. Analysis of HLA-DQB1*0602 in multiple sclerosis patients in Khuzestan Province, Iran. Arch Iran Med. 2015; 18(10):698-702. [PMID]
- Braley TJ, Chervin RD. Fatigue in multiple sclerosis: Mechanisms, evaluation, and treatment. Sleep. 2010; 33(8):1061-7. [DOI:10.1093/sleep/33.8.1061] [PMID] [PMCID]
- Reichardt J, Ebrahimi A, Nasiri Dehsorkhi H, Mewes R, Weise C, Afshar H, et al. Why is this happening to me?-A comparison of illness representations between Iranian and German people with mental illness. BMC Psychol. 2018; 6(1):33. [DOI:10.1186/s40359-018-0250-3] [PMID] [PMCID]
- Sakkas GK, Giannaki CD, Karatzaferi C, Manconi M. Sleep abnormalities in multiple sclerosis. Curr Treat Options Neurol. 2019; 21(1):4. [DOI:10.1007/s11940-019-0544-7] [PMID]
- Brass SD, Duquette P, Proulx-Therrien J, Auerbach S. Sleep disorders in patients with multiple sclerosis. Sleep Med Rev. 2010; 14(2):121-9. [DOI:10.1016/j.smrv.2009.07.005] [PMID]
- Cederberg KLJ, Jeng B, Sasaki JE, Sikes EM, Cutter G, Motl RW. Physical activity and self-reported sleep quality in adults with multiple sclerosis. Disabil Health J. 2021; 14(4):101133. [DOI:10.1016/j.dhjo.2021.101133] [PMID] [PMCID]
- Tobore TO. Towards a comprehensive etiopathogenetic and pathophysiological theory of multiple sclerosis. Int J Neurosci. 2020; 130(3):279-300. [DOI:10.1080/00207454.2019.1677648] [PMID]
- Zhang Y, Ren R, Yang L, Zhang H, Shi Y, Vitiello MV, et al. Sleep in multiple sclerosis: A systematic review and meta-analysis of polysomnographic findings. J Clin Sleep Med. 2023; 19(2):253-265. [DOI:10.5664/jcsm.10304] [PMID] [PMCID]
- Buratti L, Iacobucci DE, Viticchi G, Falsetti L, Lattanzi S, Pulcini A, et al. Sleep quality can influence the outcome of patients with multiple sclerosis. Sleep Med. 2019; 58:56-60. [DOI:10.1016/j.sleep.2019.02.020] [PMID]
- Weiner HL, Stankiewicz J. Multiple sclerosis: Diagnosis and therapy. New Jersey: John Wiley & Sons; 2012. [Link]
- Peritcard S. A manual of Chinese massage therapy. Edinburgh, UK: Churchill Livingstone, 2010. [Link]
- Shallcross AJ, Visvanathan PD, Sperber SH, Duberstein ZT. Waking up to the problem of sleep: Can mindfulness help? A review of theory and evidence for the effects of mindfulness for sleep. Curr Opin Psychol. 2019; 28:37-41. [DOI:10.1016/j.copsyc.2018.10.005] [PMID] [PMCID]
- Zargar F, Rahafrouz L, Tarrahi MJ. Effect of mindfulness-based stress reduction program on psychological symptoms, quality of life, and symptom severity in patients with somatic symptom disorder. Adv Biomed Res. 2021; 10:9.[DOI:10.4103/abr.abr_111_19] [PMID] [PMCID]
- Tingaz EO, Çakmak S. Do correlations between mindfulness components and rumination in student athletes support mindfulness training to reduce rumination? Percept Mot Skills. 2021; 128(4):1409-20. [DOI:10.1177/00315125211005243] [PMID]
- Van Doren N, Roeser RW. Examining the impacts of mindfulness training and medication on reductions in depressive and anxious symptoms in public school teachers. 2021. [Link]
- Yuan X, Jia S, FU S, Guo W. Evaluation of the effects of mindfulness training on sleep, anxiety and depression in college students. Chin J School Health. 2021; 1655-9. [Link]
- Suh HW, Jeong HY, Hong S, Kim JW, Yoon SW, Lee JY, et al. The mindfulness-based stress reduction program for improving sleep quality in cancer survivors: A systematic review and meta-analysis. Complement Ther Med. 2021; 57:102667. [DOI:10.1016/j.ctim.2021.102667] [PMID]
- Perini F, Wong KF, Lin J, Hassirim Z, Ong JL, Lo J, et al. Mindfulness-based therapy for insomnia for older adults with sleep difficulties: A randomized clinical trial. Psychol Med. 2023; 53(3):1038-48. [DOI:10.1017/S0033291721002476] [PMID] [PMCID]
- Lorenz RA, Auerbach S, Nisbet P, Sessanna L, Alanazi N, Lach H, et al. Improving sleep among adults with multiple sclerosis using mindfulness plus sleep education. West J Nurs Res. 2021; 43(3):273-83. [DOI:10.1177/0193945920947409] [PMID]
- Pouyanfard S, Mohammadpour M, Parvizifard AA, Foroughi AA. The effectiveness of mindfulness-integrated cognitive-behavioral therapy on sleep quality, anxiety, and fatigue in patients with multiple sclerosis: A randomized clinical trial. J Sleep Sci. 2019. 4(1-2):1-8. [Link]
- Rosner BA. Fundamentals of biostatistics. Massachusetts: Cengage learning; 2015. [Link]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;2 8(2):193-213. [DOI:10.1016/0165-1781(89)90047-4] [PMID]
- Bagheri H, Shahabi Z, Ebrahimi H, Alaeenejad F. [The association between quality of sleep and health-related quality of life in nurses (Persian)]. J Hayat. 2007; 12(4):13-20. [Link]
- Afkham EA, Ghalehbandi M, Salehi M, Kafian TA, Vakili Y, Akhlaghi FE. [Sleep parameters and the factors affecting the quality of sleep in patients attending selected clinics of Rasoul-e-Akram Hospital (Persian)]. Razi J Med Sci. 2009; 58(17):30-22. [Link]
- Kabat-Zinn J. Bringing mindfulness to medicine: An interview with Jon Kabat-Zinn, PhD. Interview by Karolyn Gazella. Adv Mind Body Med. 2005; 21(2):22-7. [PMID]
- Kotterba S, Neusser T, Norenberg C, Bussfeld P, Glaser T, Dörner M, et al. Sleep quality, daytime sleepiness, fatigue, and quality of life in patients with multiple sclerosis treated with interferon beta-1b: Results from a prospective observational cohort study. BMC Neurol. 2018; 18(1):123. [DOI:10.1186/s12883-018-1113-5] [PMID] [PMCID]
- Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia. Behav Res Ther. 2012; 50(11):651-60.[DOI:10.1016/j.brat.2012.08.001] [PMID] [PMCID]
- Yu X, Langberg JM, Becker SP. Dispositional mindfulness moderates the relation between brooding rumination and sleep problems in adolescents.Sleep Med. 2022; 90:131-4. [DOI:10.1016/j.sleep.2022.01.017] [PMID]
- Bolderston DH, Mindfulness-Based Meditation. In: Belchamber C, editor. Payne’s handbook of relaxation techniques e-book: A practical handbook for the health care professional. Amsterdam: Elsevier Health Sciences; 2021. [Link]
- Wang Y, Chen C, Gu L, Zhai Y, Sun Y, Gao G, et al. Effect of short-term mindfulness-based stress reduction on sleep quality in male patients with alcohol use disorder. Front Psychiatry. 2023; 14:928940. [DOI:10.3389/fpsyt.2023.928940] [PMID] [PMCID]
- Chen JA, Anderson ML, Cherkin DC, Balderson BH, Cook AJ, Sherman KJ, et al. Moderators and nonspecific predictors of treatment benefits in a randomized trial of mindfulness-based stress reduction vs cognitive-behavioral therapy vs usual care for chronic low back pain. J Pain. 2023; 24(2):282-303. [DOI:10.1016/j.jpain.2022.09.014] [PMID] [PMCID]
- Rung AL, Oral E, Berghammer L, Peters ES. Feasibility and acceptability of a mobile mindfulness meditation intervention among women: Intervention study. JMIR Mhealth Uhealth. 2020; 8(6):e15943. [DOI:10.2196/15943] [PMID] [PMCID]
Type of Study: Research |
Subject:
Special
Received: 2022/12/19 | Accepted: 2024/05/13 | Published: 2024/07/7
Received: 2022/12/19 | Accepted: 2024/05/13 | Published: 2024/07/7
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |