Tue, May 7, 2024
Volume 8, Issue 2 (Spring 2022)
Caspian J Neurol Sci 2022, 8(2): 133-142 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bagheri-Sheykhangafshe F, Fathi-Ashtiani M, Fathi-Ashtiani A. Psychological Distress in Patients With Multiple Sclerosis and Epilepsy in the COVID-19 Pandemic: A Systematic Review. Caspian J Neurol Sci 2022; 8 (2) :133-142
URL: http://cjns.gums.ac.ir/article-1-524-en.html
URL: http://cjns.gums.ac.ir/article-1-524-en.html
1- Department of Psychology, Faculty of Humanities, Tarbiat Modares University, Tehran, Iran.
2- Department of Educational and Psychology, Shiraz University, Shiraz, Iran.
3- Behavioral Sciences Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran. , fathi@bmsu.ac.ir
2- Department of Educational and Psychology, Shiraz University, Shiraz, Iran.
3- Behavioral Sciences Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran. , fathi@bmsu.ac.ir
Full-Text [PDF 1413 kb]
(435 Downloads)
| Abstract (HTML) (1031 Views)
Full-Text: (341 Views)
Introduction
Coronavirus Disease 2019 (COVID-19) first spread in Wuhan, China, on December 17, 2019. The World Health Organization (WHO) recognized it further as a pandemic on March 11, 2020 [1]. Like a pandemic, COVID-19 can arise an array of emotions, hysterics, fear, and tension in society [2]. The adverse effects of pandemics are not restricted to physical health predicaments; they can also lead to severe consequences, such as anxiety, depression, and stress in individuals [3, 4]. Previous studies suggest that mental distress is a significant response to pandemics.
Furthermore, it is much more recognizable in the early stages of the outbreak [5, 6]. Scientists reported that 36.4% of individuals diagnosed with COVID-19 present mental symptoms in addition to systemic, respiratory symptoms, such as headache, consciousness, and paresthesia. These mental symptoms are more likely to appear in more severe COVID-19 cases than milder and moderate ones [7]. Besides, autopsy reports of deceased patients reveal minor nervous deterioration in them [8]. In addition to mentioned signs, cases of viral encephalitis caused by COVID-19 due to virus attacks on the Central Nervous System (CNS) have also been reported. Laboratory tests on cerebrospinal fluid also reveal this virus’s potential (threat) in critically damaging the nervous system [9].
In this regard, patients with epilepsy and MS whose CNS is damaged are more vulnerable to illness due to COVID-19 [10, 11]. MS is a chronic progressive disease that damages the myelin of the CNS and affects sensory and motor functions [12]. As a multidimensional and multifactorial phenomenon, stress might be a complication of MS and a factor in exacerbating or recurring the symptoms of the disease [13]. Depression and anxiety are also major mental disorders in patients with MS. The causes of depression and anxiety in these patients remain undiscovered; nonetheless, a combination of psychosocial, neurological, and disease-related factors may be involved [10-14]. Altogether, MS patients endure much higher stages of mental disorders such as depression, stress, and anxiety when compared to the healthy population. Such symptoms may root in the direct influence of inflammation and demyelination on nerves or the mental effects of MS chronic condition [15, 16].
Epilepsy also refers to recurrent seizures that occur due to sudden depletion and excessive intermittent discharges of brain neurons [17]. Anatomical disorders, such as temporal lobe tumors, cerebrovascular disorders, dead tissue in parts of the brain, including the hippocampus, trauma, fetal injuries, fever, temperature changes, and medications are some causes of epilepsy [18]. In addition to the physical problems associated with epilepsy, epilepsy patients also suffer from other psychosocial conflicts; especially during the COVID-19 pandemic, numerous patients experienced multiple seizures due to stress and anxiety [19]. Epilepsy, alongside depression, has profound effects on the patient’s life, leading to decreased daily functioning and quality of life, decreased academic achievements in children and adolescents, reduced marriage rates, increased unemployment, seizures, high mortality, and an increased requirement to medical treatments [20]. Anxiety can result from the unpredictability of seizures, decreased physical activity, self-worthlessness, or social exclusion [20, 21].
Enjoying decent mental health facilitates the process of various treatments, especially for people with MS and epilepsy [22, 23]. In addition to physical care during the COVID-19 pandemic, individuals with MS and epilepsy also appear to require psychological support. Many of these people experience extra stress as they are suggested vulnerable and need more care [24, 25]. Therefore, if they do not receive well-time interventions, they can be expected to suffer from incurable depression and anxiety [26]. In this regard, a study by Costabile examined the psychological distress of patients with MS during the COVID-19 pandemic. The results indicated that patients with MS had higher depression, anxiety, and insomnia rates than normal people. The patient’s attitude towards the current situation influenced their mental health [27]. Patients who were passive and identified themselves as being cognitively dysfunctional experienced high levels of depression. Abokalawa studied the effects of the COVID-19 pandemic on the lives of epilepsy patients. The obtained findings suggested that 55.6% of patients reported poor sleep quality. Furthermore, 66.2%, 77.2%, and 75.5% of patients developed depression, anxiety, and stress, respectively. Additionally, 23% of patients reported increased seizures during the COVID-19 pandemic [28].
Altogether, studies indicate the prevalence of psychological disorders in patients with MS and epilepsy. It is almost two years since the outbreak of the COVID-19 pandemic, and this lethal virus keeps mutating; thus, it seems necessary to pay attention to the psychological consequences of this pandemic in addition to physical examinations, especially on people with chronic neuropsychiatric disorders who are categorized in high-risk groups and whose mental health is affected by COVID-19 and its related news [29, 30]. In this regard, the present study aimed to investigate the depression, anxiety, and stress among patients with MS and epilepsy during the COVID-19 pandemic.
Materials and Methods
Search strategy
The present systematic review was performed through the PRISMA checklist examined research findings related to depression, anxiety, and stress in patients with MS and epilepsy during the prevalence of COVID-19 [31]. Articles indexed were used in scientific databases such as Google Scholar, PubMed, ISI, Scopus, EMBASE, and PsycINFO. Using the specified keywords, researchers in this study searched and extracted helpful English articles published in 2020 (May) and 2021 (July) from reliable electronic sources. By reviewing the full texts of these articles, the data were reported in a categorized manner.
Keywords
The combinations of the following keywords were used in the search strategy: (Multiple Sclerosis) OR (MS) (title/abstract) OR (Epilepsy) (title/abstract) AND (Coronavirus 2019) OR (COVID-19) (title/abstract) AND (Anxiety) OR (Distress) OR (Depression) OR (Sad) OR (Stress) OR (Tension) (title/abstract).
Exclusion and inclusion criteria
Research articles were purposefully selected based on the criteria of exclusion (the unavailability of full text of the article, letter to the editor, & no abstract) and entry into the research (relevance to the purpose of the research, having a structured research framework, & publication in a valid journal) for review.
Quality assessment
The present authors evaluated all articles after extraction from the desired databases. To further improve the quality of articles, after removing articles unrelated to the research objectives and selecting the main articles, the list of sources of selected articles was searched again to increase the assurance of identifying and reviewing existing articles. Three researchers individually analyzed the content of each of the 27 articles. Each researcher studied each article separately, then entered the data related to each article into the content analysis form. The quality of articles using the PRISMA checklist, as follows: matching the structure of the article with the type of research, research purpose, the research community, sample selection process, data collection tools, data analysis using statistical tests related to the objectives specified existence of entry and exit criteria, observance of ethics in research, the presentation of findings per the objectives of the research and discussion of the findings were evaluated based on the results of related research. The quality of the articles was evaluated using the criteria provided by Gifford et al. [32]. Based on the criteria provided for quantitative (6 criteria), qualitative (11 criteria), quasi-experimental (8 criteria), and experimental (7 criteria) studies, the articles were evaluated on a two-point scale (zero and one). The cut-off point was equal to 4 and less for quantitative articles, 6 and less for experimental and quasi-experimental studies, and 8 and less for qualitative studies.
Data extraction
Out of 394 articles related to depression, anxiety, and stress of patients with MS or epilepsy during the COVID-19 pandemic, after deleting articles that were not associated with the study’s objectives, 27 related articles were finally included in the study and examined thoroughly and accurately (Figure 1).
.jpg)
Results
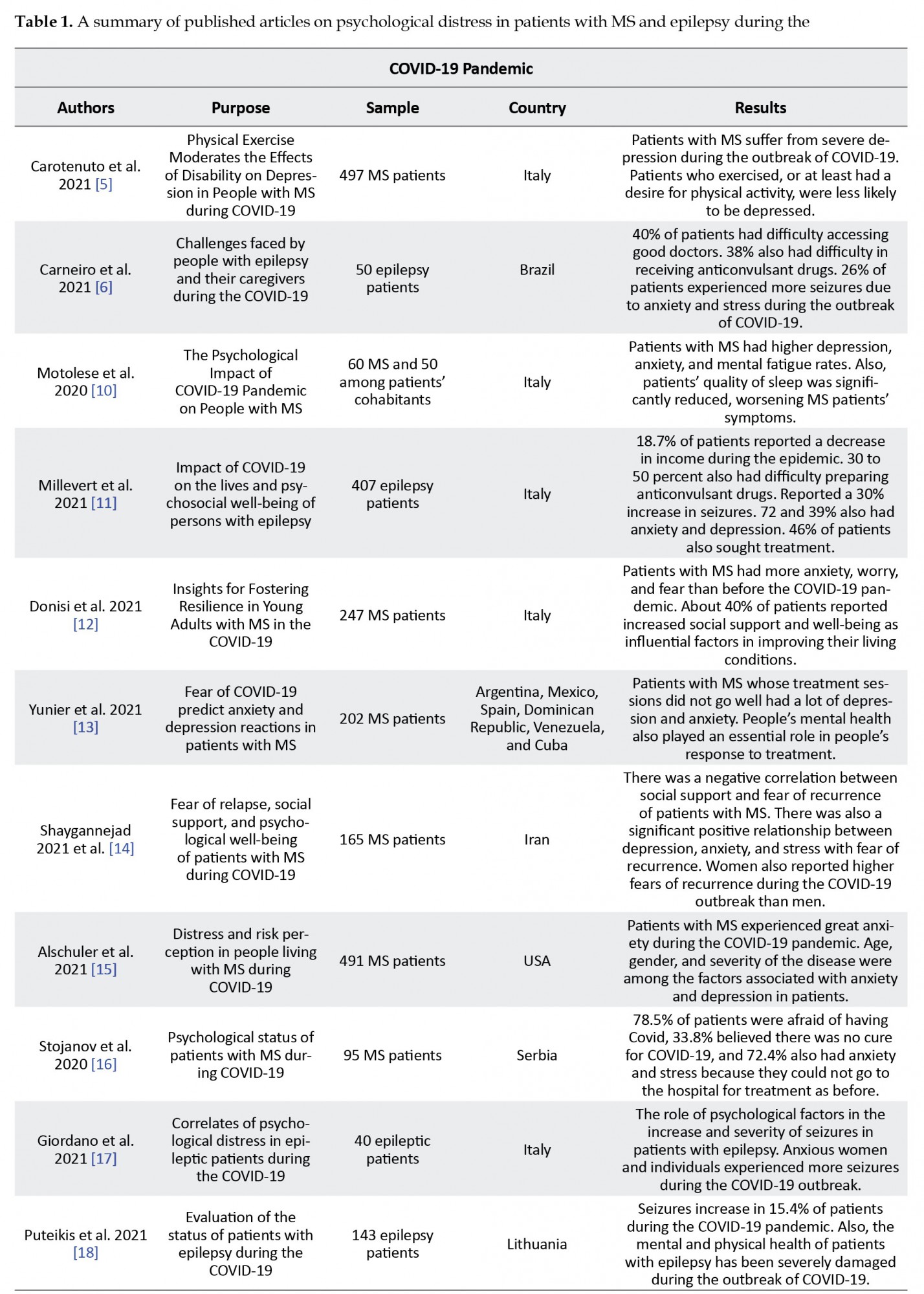
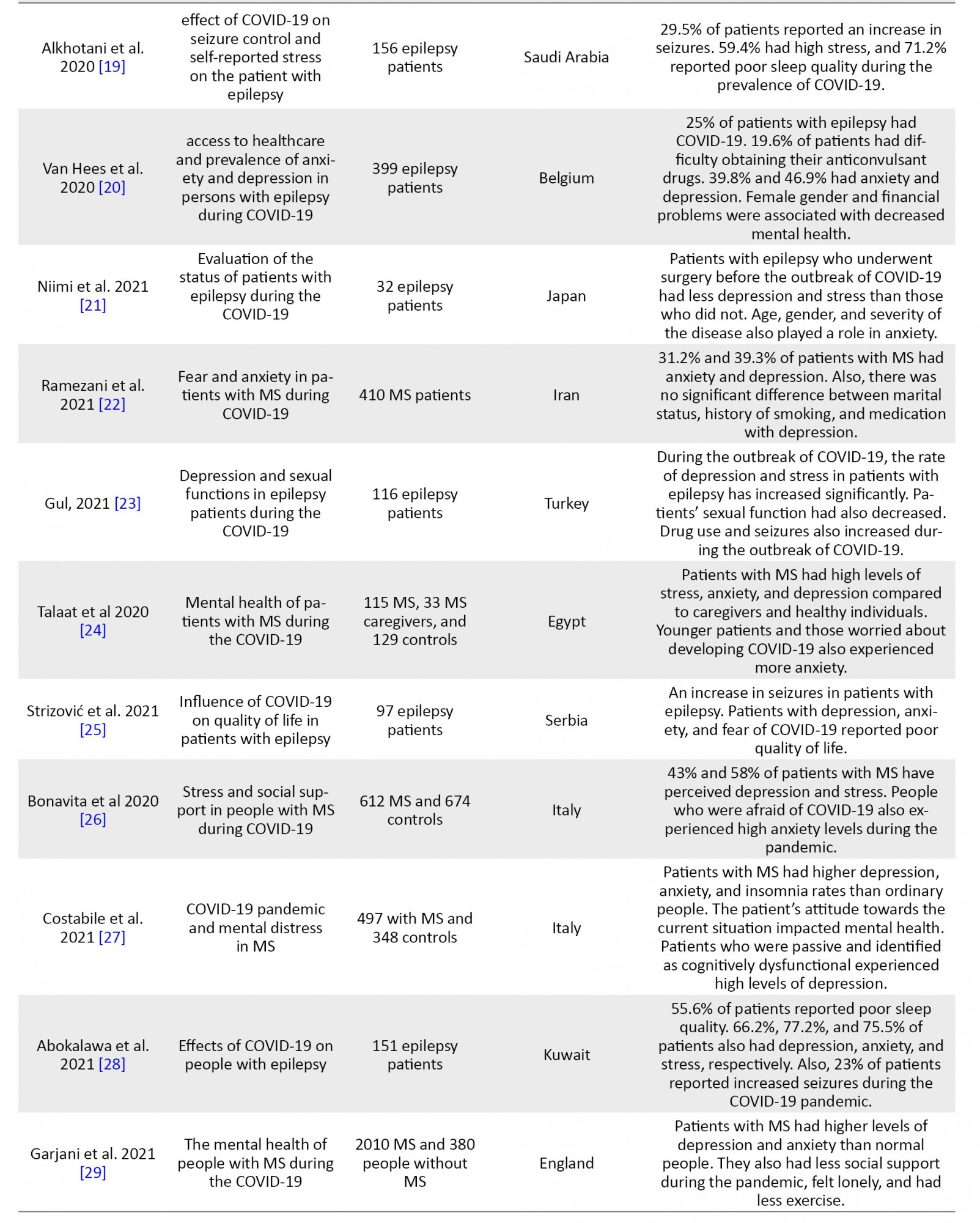
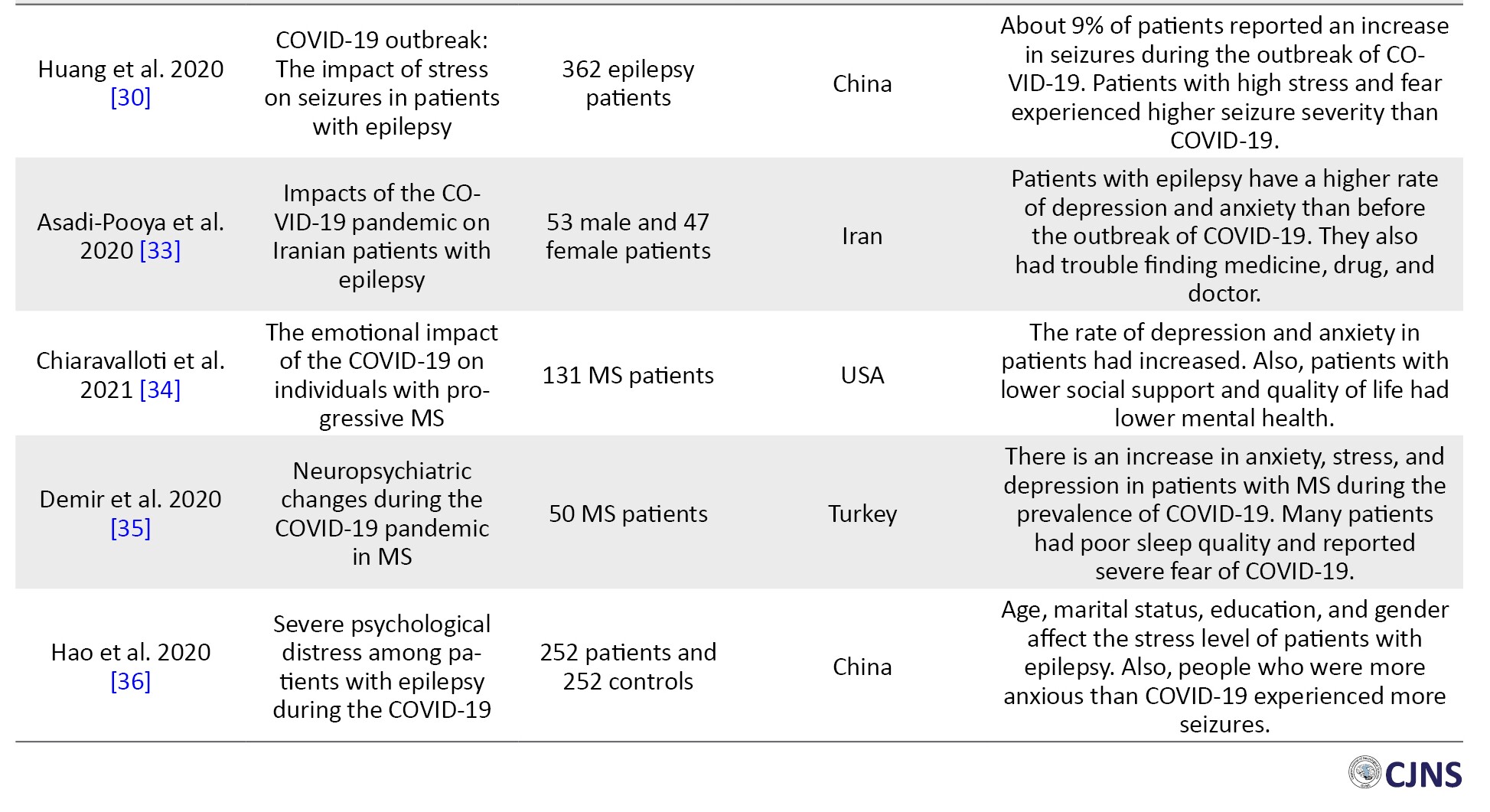
In this study, 27 eligible research articles in English were reviewed. The following are the findings of a review of articles examining depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic (Table 1).
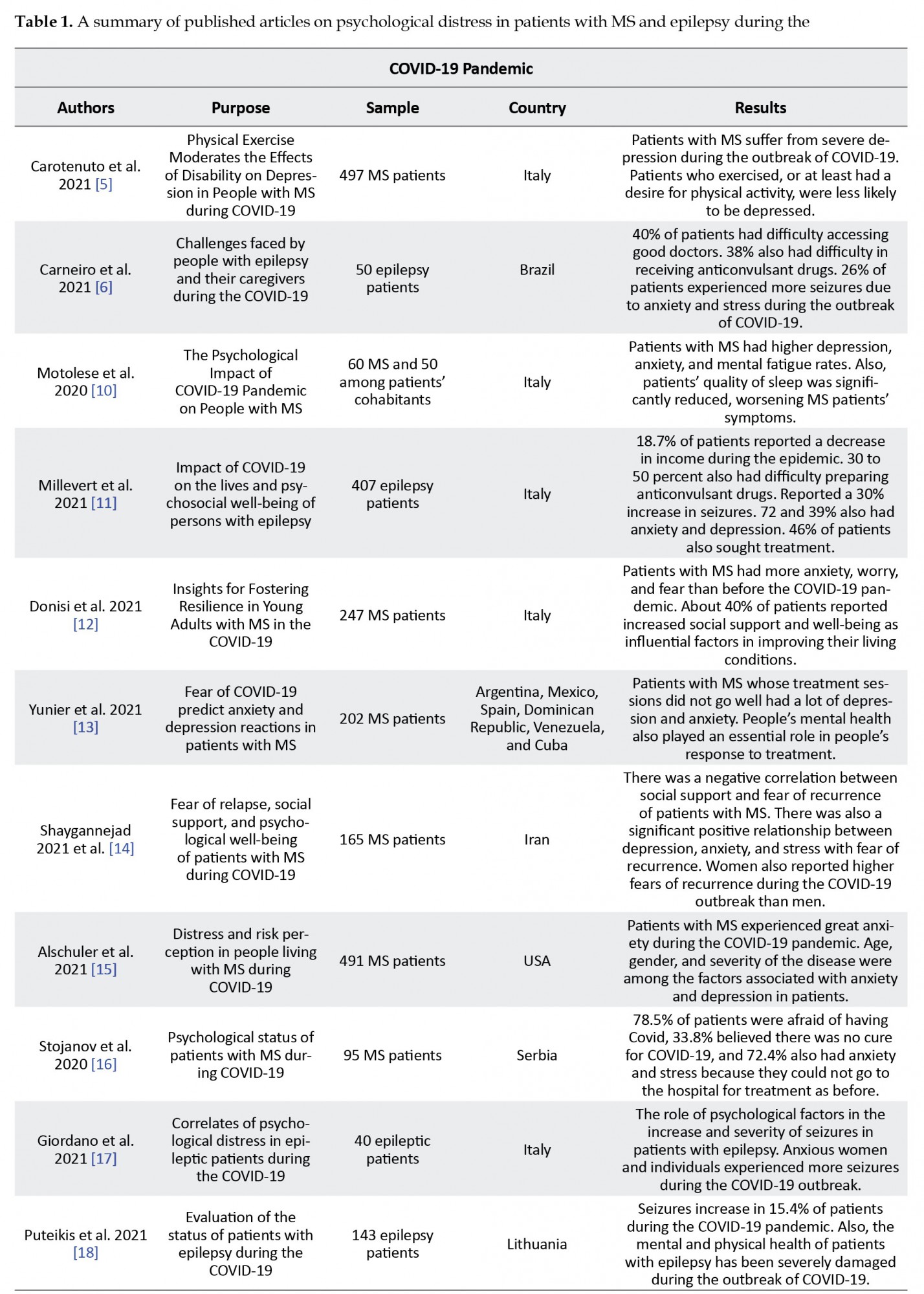
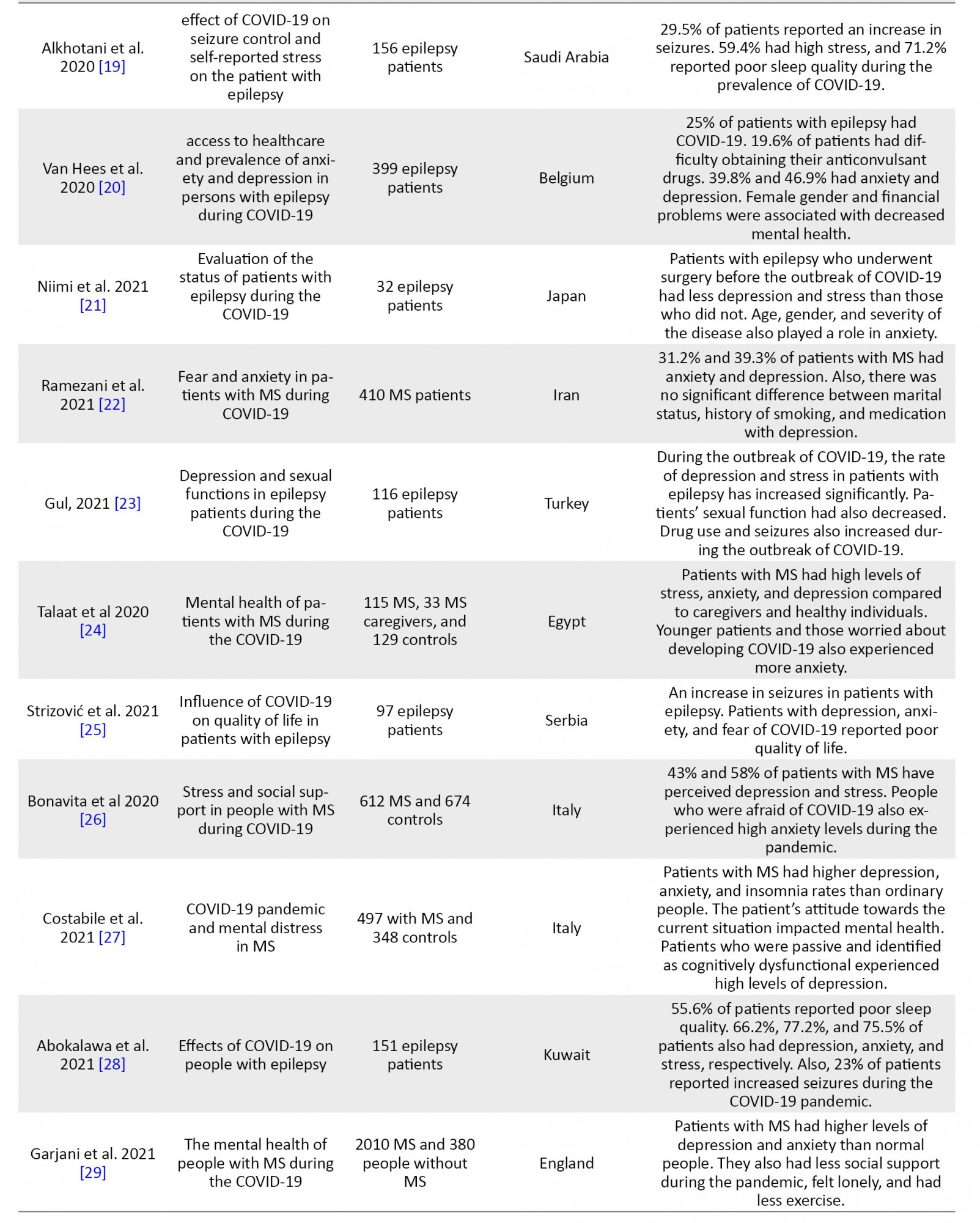
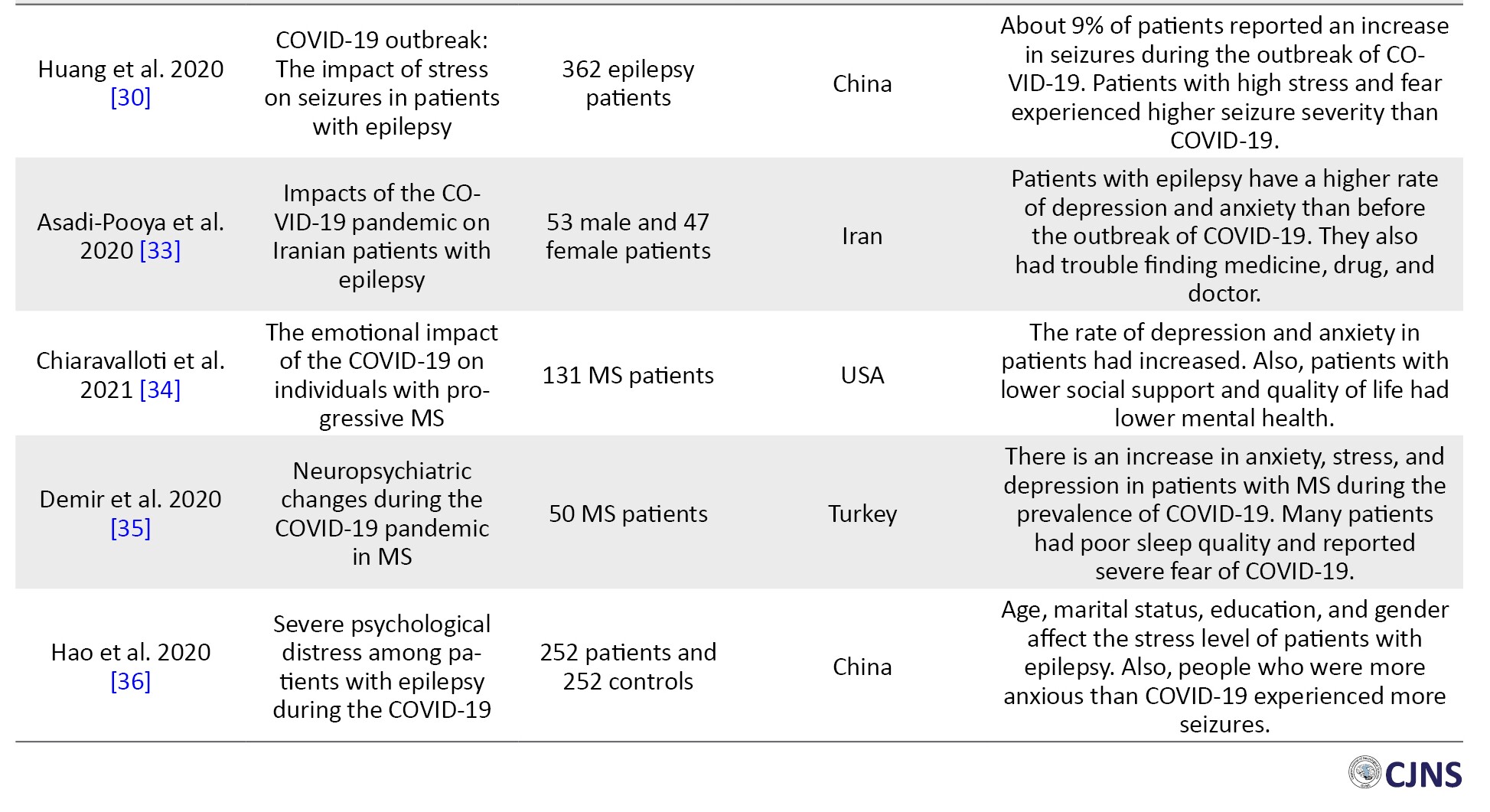
Out of 394 articles related to depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic, 27 articles were reviewed and selected with a population of 9528 based on inclusion and exclusion criteria. The systematic review also included 20 countries, as follows: Iran, China, Serbia, Turkey, Japan, Belgium, Saudi Arabia, Lithuania, Kuwait, Italy, Brazil, USA, England, Argentina, Mexico, Spain, Dominican Republic, Venezuela, Cuba, and Egypt, indicating the importance of assessing the mental health of patients with MS and epilepsy during the COVID-19 pandemic. Of the 27 articles reviewed, 40.7% and 59.3% were published in 2020 and 2021. According to the examined studies, patients with MS and epilepsy experienced depression, anxiety, stress, fear, poor sleep quality, mental fatigue, and poor quality of life during the COVID-19 pandemic. Quarantine has limited patients’ access to medication and treatment, resulting in increased seizures and disease severity. Factors such as female gender, loneliness, economic problems, lack of social support, old age, and lack of exercise also affected the severity of depressive symptoms, stress, and anxiety in patients with MS and epilepsy during the COVID-19 pandemic.
Discussion
This study investigated depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic. The obtained results indicated that patients with MS and epilepsy experienced depression, anxiety, stress, fear, and low sleep quality during the COVID-19 pandemic and home quarantine [11, 29].
At the beginning of the COVID-19 pandemic, there was news on media and social platforms that people with chronic diseases and the elderly were more vulnerable to the virus. As a result, such people had a tough year, experiencing depression, fear, and tension. This further deteriorated their immune systems. Those with chronic diseases are more likely to be infected by COVID-19 as they have weaker immune systems [17]. Excessive anxiety and stress are harmful to health, and the individual may undergo severe heart attacks. Thus, psychological distress, along with a weak immune system, has led to a rise in the death rate of individuals with chronic diseases during the COVID-19 pandemic globally [11-13]. Moreover, according to the reports on the age and background disease effects on COVID-19 severity, individuals without chronic disease or underlying medical conditions experienced lower stress and anxiety [37].
The psychological health of MS and epilepsy patients significantly declined during the COVID-19 pandemic [10, 11]. Mental health is substantially related to MS and other chronic diseases. Patients who encounter MS and epilepsy experience a mental health decline due to the repeated pain and a poor immune system, and depression, stress, and anxiety rise as the severity of the disease and pain increase. Furthermore, experiencing excessive stress may result in attacks in MS patients [5]. Psychological syndromes have complicated relationships with MS, and their spread could respond to many factors. Indeed, physical signs, e.g., fatigue, inability, significant problems in the family, work, and social life, lead to the reoccurrence of physiological syndromes and, consequently, increase disease inflammation. Also, the neurological damages imposed by MS on the CNS could be associated with psychological and cognitive syndromes [38]. MS patients also suffer from related difficulties that prevent active participation in health-based activities (i.e., active presence in society & sports activities), leading to increased consequences and limitations in life [39].
The COVID-19 pandemic decreased the interaction of MS patients with their doctors and hospitals. Therefore, they had difficulties finding their medicines and significantly relapsed [12]. Additionally, numerous MS patients had substantial stress and fear of COVID-19, which increased their anxiety [15, 16]. Home quarantine and a distance from friends and society aggravated depression in MS patients [14]. Accordingly, the results of Costabile et al. demonstrated that MS patients experienced higher depression, anxiety, and lack of sleep than normal people during the COVID-19 pandemic. The attitude of a patient toward the current situation influences their mental health. Passive patients who introduced themselves cognitively inefficient experienced high depression [27].
Epileptic patients encounter biopsychosocial conditions. Dysfunctional underlying beliefs reduce compatibility skills and the ability to deal with problems in epilepsy patients [40]. These patients were affected by COVID-19 and received lower social support. They were under home quarantine, away from their friends and society, and underwent economic losses in their incomes and jobs [18]. These mental conditions make epilepsy patients vulnerable to various psychological conditions, including stress, depression, and anxiety [21]. These psychological conditions are referred to as interictal dysphoric syndrome [11]. In the cognitive model of depression, adverse and stressful life events are the stimulators of a depressed mood. Stressful events account for most epilepsy patients’ lives [20]. Epilepsy, its treatment, and permanently dealing with a neurological disorder cause substantial stress.
In many cases, the patient can live everyday life in the interval of seizures [25]. However, the problems associated with treatment side effects and the fear of losing control and name-calling impose extensive social limitations on patients. Considering unforeseeable seizures, epilepsy patients encounter stressful and disappointing situations, such as work problems and poor social interactions [19]. Stress was recognized as a large factor that significantly predicts seizure attacks in epilepsy patients. Almost two-thirds of epilepsy patients refer to stress as the largest predictor of their seizure attacks. Seizures are twice more likely to occur in patients with a higher level of anxiety than other patients [30].
Epileptic patients experienced more frequent seizures due to stress and anxiety during the COVID-19 pandemic [28]. Patients’ limited access to medicine and physicians also exacerbated the disease in many people [33]. As a result, patients who receive inadequate social support from their families and friends undergo substantial depression and anxiety [34]. In this regard, Abokalawa et al. [28] indicated that 55.6% of epilepsy patients reported poor sleeping quality during the COVID-19 pandemic. Furthermore, 66.2%, 77.2%, and 75.5% of the patients had depression, anxiety, and stress, respectively, while 23% reported increased seizures during the pandemic. The Gul [23] study reported increased psychological distress in epilepsy patients. Furthermore, medicine consumption and seizure frequency significantly increased during the COVID-19 pandemic due to increased stress in patients.
A limitation of the present review study is the unavailability of the full text of some articles, which led to the non-inclusion of these articles in the review process. Moreover, two years have passed since the outbreak of COVID-19 in the world, and we are still witnessing the mutation of this deadly virus; therefore, it is necessary first to study the psychological consequences of the COVID-19 pandemic concerning neurological diseases. Considering the vaccination of many patients with MS and epilepsy worldwide, it was also studied on the long-term consequences of the outbreak of COVID-19, such as post-traumatic stress, post-traumatic stress disorder, and sexual and social relationships.
Coronavirus Disease 2019 (COVID-19) first spread in Wuhan, China, on December 17, 2019. The World Health Organization (WHO) recognized it further as a pandemic on March 11, 2020 [1]. Like a pandemic, COVID-19 can arise an array of emotions, hysterics, fear, and tension in society [2]. The adverse effects of pandemics are not restricted to physical health predicaments; they can also lead to severe consequences, such as anxiety, depression, and stress in individuals [3, 4]. Previous studies suggest that mental distress is a significant response to pandemics.
Furthermore, it is much more recognizable in the early stages of the outbreak [5, 6]. Scientists reported that 36.4% of individuals diagnosed with COVID-19 present mental symptoms in addition to systemic, respiratory symptoms, such as headache, consciousness, and paresthesia. These mental symptoms are more likely to appear in more severe COVID-19 cases than milder and moderate ones [7]. Besides, autopsy reports of deceased patients reveal minor nervous deterioration in them [8]. In addition to mentioned signs, cases of viral encephalitis caused by COVID-19 due to virus attacks on the Central Nervous System (CNS) have also been reported. Laboratory tests on cerebrospinal fluid also reveal this virus’s potential (threat) in critically damaging the nervous system [9].
In this regard, patients with epilepsy and MS whose CNS is damaged are more vulnerable to illness due to COVID-19 [10, 11]. MS is a chronic progressive disease that damages the myelin of the CNS and affects sensory and motor functions [12]. As a multidimensional and multifactorial phenomenon, stress might be a complication of MS and a factor in exacerbating or recurring the symptoms of the disease [13]. Depression and anxiety are also major mental disorders in patients with MS. The causes of depression and anxiety in these patients remain undiscovered; nonetheless, a combination of psychosocial, neurological, and disease-related factors may be involved [10-14]. Altogether, MS patients endure much higher stages of mental disorders such as depression, stress, and anxiety when compared to the healthy population. Such symptoms may root in the direct influence of inflammation and demyelination on nerves or the mental effects of MS chronic condition [15, 16].
Epilepsy also refers to recurrent seizures that occur due to sudden depletion and excessive intermittent discharges of brain neurons [17]. Anatomical disorders, such as temporal lobe tumors, cerebrovascular disorders, dead tissue in parts of the brain, including the hippocampus, trauma, fetal injuries, fever, temperature changes, and medications are some causes of epilepsy [18]. In addition to the physical problems associated with epilepsy, epilepsy patients also suffer from other psychosocial conflicts; especially during the COVID-19 pandemic, numerous patients experienced multiple seizures due to stress and anxiety [19]. Epilepsy, alongside depression, has profound effects on the patient’s life, leading to decreased daily functioning and quality of life, decreased academic achievements in children and adolescents, reduced marriage rates, increased unemployment, seizures, high mortality, and an increased requirement to medical treatments [20]. Anxiety can result from the unpredictability of seizures, decreased physical activity, self-worthlessness, or social exclusion [20, 21].
Enjoying decent mental health facilitates the process of various treatments, especially for people with MS and epilepsy [22, 23]. In addition to physical care during the COVID-19 pandemic, individuals with MS and epilepsy also appear to require psychological support. Many of these people experience extra stress as they are suggested vulnerable and need more care [24, 25]. Therefore, if they do not receive well-time interventions, they can be expected to suffer from incurable depression and anxiety [26]. In this regard, a study by Costabile examined the psychological distress of patients with MS during the COVID-19 pandemic. The results indicated that patients with MS had higher depression, anxiety, and insomnia rates than normal people. The patient’s attitude towards the current situation influenced their mental health [27]. Patients who were passive and identified themselves as being cognitively dysfunctional experienced high levels of depression. Abokalawa studied the effects of the COVID-19 pandemic on the lives of epilepsy patients. The obtained findings suggested that 55.6% of patients reported poor sleep quality. Furthermore, 66.2%, 77.2%, and 75.5% of patients developed depression, anxiety, and stress, respectively. Additionally, 23% of patients reported increased seizures during the COVID-19 pandemic [28].
Altogether, studies indicate the prevalence of psychological disorders in patients with MS and epilepsy. It is almost two years since the outbreak of the COVID-19 pandemic, and this lethal virus keeps mutating; thus, it seems necessary to pay attention to the psychological consequences of this pandemic in addition to physical examinations, especially on people with chronic neuropsychiatric disorders who are categorized in high-risk groups and whose mental health is affected by COVID-19 and its related news [29, 30]. In this regard, the present study aimed to investigate the depression, anxiety, and stress among patients with MS and epilepsy during the COVID-19 pandemic.
Materials and Methods
Search strategy
The present systematic review was performed through the PRISMA checklist examined research findings related to depression, anxiety, and stress in patients with MS and epilepsy during the prevalence of COVID-19 [31]. Articles indexed were used in scientific databases such as Google Scholar, PubMed, ISI, Scopus, EMBASE, and PsycINFO. Using the specified keywords, researchers in this study searched and extracted helpful English articles published in 2020 (May) and 2021 (July) from reliable electronic sources. By reviewing the full texts of these articles, the data were reported in a categorized manner.
Keywords
The combinations of the following keywords were used in the search strategy: (Multiple Sclerosis) OR (MS) (title/abstract) OR (Epilepsy) (title/abstract) AND (Coronavirus 2019) OR (COVID-19) (title/abstract) AND (Anxiety) OR (Distress) OR (Depression) OR (Sad) OR (Stress) OR (Tension) (title/abstract).
Exclusion and inclusion criteria
Research articles were purposefully selected based on the criteria of exclusion (the unavailability of full text of the article, letter to the editor, & no abstract) and entry into the research (relevance to the purpose of the research, having a structured research framework, & publication in a valid journal) for review.
Quality assessment
The present authors evaluated all articles after extraction from the desired databases. To further improve the quality of articles, after removing articles unrelated to the research objectives and selecting the main articles, the list of sources of selected articles was searched again to increase the assurance of identifying and reviewing existing articles. Three researchers individually analyzed the content of each of the 27 articles. Each researcher studied each article separately, then entered the data related to each article into the content analysis form. The quality of articles using the PRISMA checklist, as follows: matching the structure of the article with the type of research, research purpose, the research community, sample selection process, data collection tools, data analysis using statistical tests related to the objectives specified existence of entry and exit criteria, observance of ethics in research, the presentation of findings per the objectives of the research and discussion of the findings were evaluated based on the results of related research. The quality of the articles was evaluated using the criteria provided by Gifford et al. [32]. Based on the criteria provided for quantitative (6 criteria), qualitative (11 criteria), quasi-experimental (8 criteria), and experimental (7 criteria) studies, the articles were evaluated on a two-point scale (zero and one). The cut-off point was equal to 4 and less for quantitative articles, 6 and less for experimental and quasi-experimental studies, and 8 and less for qualitative studies.
Data extraction
Out of 394 articles related to depression, anxiety, and stress of patients with MS or epilepsy during the COVID-19 pandemic, after deleting articles that were not associated with the study’s objectives, 27 related articles were finally included in the study and examined thoroughly and accurately (Figure 1).
.jpg)
Results
In this study, 27 eligible research articles in English were reviewed. The following are the findings of a review of articles examining depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic (Table 1).
Out of 394 articles related to depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic, 27 articles were reviewed and selected with a population of 9528 based on inclusion and exclusion criteria. The systematic review also included 20 countries, as follows: Iran, China, Serbia, Turkey, Japan, Belgium, Saudi Arabia, Lithuania, Kuwait, Italy, Brazil, USA, England, Argentina, Mexico, Spain, Dominican Republic, Venezuela, Cuba, and Egypt, indicating the importance of assessing the mental health of patients with MS and epilepsy during the COVID-19 pandemic. Of the 27 articles reviewed, 40.7% and 59.3% were published in 2020 and 2021. According to the examined studies, patients with MS and epilepsy experienced depression, anxiety, stress, fear, poor sleep quality, mental fatigue, and poor quality of life during the COVID-19 pandemic. Quarantine has limited patients’ access to medication and treatment, resulting in increased seizures and disease severity. Factors such as female gender, loneliness, economic problems, lack of social support, old age, and lack of exercise also affected the severity of depressive symptoms, stress, and anxiety in patients with MS and epilepsy during the COVID-19 pandemic.
Discussion
This study investigated depression, anxiety, and stress in patients with MS and epilepsy during the COVID-19 pandemic. The obtained results indicated that patients with MS and epilepsy experienced depression, anxiety, stress, fear, and low sleep quality during the COVID-19 pandemic and home quarantine [11, 29].
At the beginning of the COVID-19 pandemic, there was news on media and social platforms that people with chronic diseases and the elderly were more vulnerable to the virus. As a result, such people had a tough year, experiencing depression, fear, and tension. This further deteriorated their immune systems. Those with chronic diseases are more likely to be infected by COVID-19 as they have weaker immune systems [17]. Excessive anxiety and stress are harmful to health, and the individual may undergo severe heart attacks. Thus, psychological distress, along with a weak immune system, has led to a rise in the death rate of individuals with chronic diseases during the COVID-19 pandemic globally [11-13]. Moreover, according to the reports on the age and background disease effects on COVID-19 severity, individuals without chronic disease or underlying medical conditions experienced lower stress and anxiety [37].
The psychological health of MS and epilepsy patients significantly declined during the COVID-19 pandemic [10, 11]. Mental health is substantially related to MS and other chronic diseases. Patients who encounter MS and epilepsy experience a mental health decline due to the repeated pain and a poor immune system, and depression, stress, and anxiety rise as the severity of the disease and pain increase. Furthermore, experiencing excessive stress may result in attacks in MS patients [5]. Psychological syndromes have complicated relationships with MS, and their spread could respond to many factors. Indeed, physical signs, e.g., fatigue, inability, significant problems in the family, work, and social life, lead to the reoccurrence of physiological syndromes and, consequently, increase disease inflammation. Also, the neurological damages imposed by MS on the CNS could be associated with psychological and cognitive syndromes [38]. MS patients also suffer from related difficulties that prevent active participation in health-based activities (i.e., active presence in society & sports activities), leading to increased consequences and limitations in life [39].
The COVID-19 pandemic decreased the interaction of MS patients with their doctors and hospitals. Therefore, they had difficulties finding their medicines and significantly relapsed [12]. Additionally, numerous MS patients had substantial stress and fear of COVID-19, which increased their anxiety [15, 16]. Home quarantine and a distance from friends and society aggravated depression in MS patients [14]. Accordingly, the results of Costabile et al. demonstrated that MS patients experienced higher depression, anxiety, and lack of sleep than normal people during the COVID-19 pandemic. The attitude of a patient toward the current situation influences their mental health. Passive patients who introduced themselves cognitively inefficient experienced high depression [27].
Epileptic patients encounter biopsychosocial conditions. Dysfunctional underlying beliefs reduce compatibility skills and the ability to deal with problems in epilepsy patients [40]. These patients were affected by COVID-19 and received lower social support. They were under home quarantine, away from their friends and society, and underwent economic losses in their incomes and jobs [18]. These mental conditions make epilepsy patients vulnerable to various psychological conditions, including stress, depression, and anxiety [21]. These psychological conditions are referred to as interictal dysphoric syndrome [11]. In the cognitive model of depression, adverse and stressful life events are the stimulators of a depressed mood. Stressful events account for most epilepsy patients’ lives [20]. Epilepsy, its treatment, and permanently dealing with a neurological disorder cause substantial stress.
In many cases, the patient can live everyday life in the interval of seizures [25]. However, the problems associated with treatment side effects and the fear of losing control and name-calling impose extensive social limitations on patients. Considering unforeseeable seizures, epilepsy patients encounter stressful and disappointing situations, such as work problems and poor social interactions [19]. Stress was recognized as a large factor that significantly predicts seizure attacks in epilepsy patients. Almost two-thirds of epilepsy patients refer to stress as the largest predictor of their seizure attacks. Seizures are twice more likely to occur in patients with a higher level of anxiety than other patients [30].
Epileptic patients experienced more frequent seizures due to stress and anxiety during the COVID-19 pandemic [28]. Patients’ limited access to medicine and physicians also exacerbated the disease in many people [33]. As a result, patients who receive inadequate social support from their families and friends undergo substantial depression and anxiety [34]. In this regard, Abokalawa et al. [28] indicated that 55.6% of epilepsy patients reported poor sleeping quality during the COVID-19 pandemic. Furthermore, 66.2%, 77.2%, and 75.5% of the patients had depression, anxiety, and stress, respectively, while 23% reported increased seizures during the pandemic. The Gul [23] study reported increased psychological distress in epilepsy patients. Furthermore, medicine consumption and seizure frequency significantly increased during the COVID-19 pandemic due to increased stress in patients.
A limitation of the present review study is the unavailability of the full text of some articles, which led to the non-inclusion of these articles in the review process. Moreover, two years have passed since the outbreak of COVID-19 in the world, and we are still witnessing the mutation of this deadly virus; therefore, it is necessary first to study the psychological consequences of the COVID-19 pandemic concerning neurological diseases. Considering the vaccination of many patients with MS and epilepsy worldwide, it was also studied on the long-term consequences of the outbreak of COVID-19, such as post-traumatic stress, post-traumatic stress disorder, and sexual and social relationships.
Conclusion
The obtained findings suggested a high prevalence of depression, anxiety, stress, and fear in patients with MS and epilepsy during the COVID-19 pandemic. Mental health services were mainly available online during the pandemic; thus, MS and epilepsy patients had several problems due to limited access. In addition, many patients cannot consult a physician to receive their monthly prescriptions due to social distancing and public transportation restrictions. This leads to non-treatment and exacerbated previous psychological symptoms. Besides, social exclusion’s (adverse) effects increase with hospitalization, as many hospitals located in infected areas do not allow visitors.
Moreover, depression, anxiety, stress, limited access to medication, and attending physician increased seizures in MS and epilepsy patients. Therefore, it is necessary to identify and treat psychological disorders in patients and their treatment by a psychologist. MS and epilepsy are among the most common neurological disorders; therefore, in this review study, we tried to investigate the psychological distress of these patients. The results also show an almost equal prevalence of depression, anxiety, stress, and fear of COVID-19 in patients with multiple sclerosis and epilepsy.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Moreover, depression, anxiety, stress, limited access to medication, and attending physician increased seizures in MS and epilepsy patients. Therefore, it is necessary to identify and treat psychological disorders in patients and their treatment by a psychologist. MS and epilepsy are among the most common neurological disorders; therefore, in this review study, we tried to investigate the psychological distress of these patients. The results also show an almost equal prevalence of depression, anxiety, stress, and fear of COVID-19 in patients with multiple sclerosis and epilepsy.
Ethical Considerations
Compliance with ethical guidelines
All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization and Supervision: Farzin Bagheri-Sheykhangafshe; Methodology: Mina Fathi-Ashtiani and Ali Fathi-Ashtiani; Investigation: Farzin Bagheri-Sheykhangafshe and Ali Fathi-Ashtiani; Writing the original draft, review, and editing: All authors.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors hereby consider it necessary to thank and appreciate all the researchers whose papers were examined in this study.
References
References
- Nowak-Kiczmer M, Kubicka-Bączyk K, Niedziela N, Adamczyk B, Wierzbicki K, Bartman W, et al. The course of COVID-19 infection in patients with multiple sclerosis-the experience of one center based on the population of upper silesia. Mult Scler Relat Disord 2021; 52:102984. [DOI:10.1016/j.msard.2021.102984] [PMID] [PMCID]
- Sanchez-Larsen A, Gonzalez-Villar E, Díaz-Maroto I, Layos-Romero A, Martínez-Martín Á, Alcahut-Rodriguez C, et al. Influence of the COVID-19 outbreak in people with epilepsy: Analysis of a Spanish population (EPICOVID registry). Epilepsy Behav. 2020; 112:107396. [DOI:10.1016/j.yebeh.2020.107396] [PMCID]
- Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020; 17(11):4065. [DOI:10.3390/ijerph17114065] [PMCID]
- Bagheri Sheykhangafshe F, Esmaeilinasab M. Psychological implications of coronavirus disease 2019 outbreak in patients with chronic diseases: A systematic review. Chron Dis J. 2021; 9(3):132-43. http://cdjournal.muk.ac.ir/index.php/cdj/article/view/629
- Carotenuto A, Scandurra C, Costabile T, Lavorgna L, Borriello G, Moiola L, et al. Physical exercise moderates the effects of disability on depression in people with multiple sclerosis during the COVID-19 outbreak. J Clin Med. 2021; 10(6):1234. [DOI:10.3390/jcm10061234] [PMCID]
- Carneiro RAVD, dos Santos Lunardi MS, Giacomini FMU, Rieger DK, Moreira JD, da Silva LCR, et al. Challenges faced by people with epilepsy on ketogenic diet therapy and their caregivers during the COVID-19 pandemic in Brazil. Epilepsy Behav. 2021; 122:108193. [DOI:10.1016/j.yebeh.2021.108193]
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77(6):1-9. [DOI:10.1001/jamaneurol.2020.1127] [PMCID]
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020; 8(4):420-2. [DOI:10.1016/S2213-2600(20)30076-X]
- Serrano-Castro PJ, Estivill-Torrús G, Cabezudo-García P, Reyes-Bueno JA, Petersen NC, Aguilar-Castillo MJ, et al. Impact of SARS-CoV-2 infection on neurodegenerative and neuropsychiatric diseases: A delayed pandemic?. Neurología. 2020; 35(4):245-51. [DOI:10.1016/j.nrleng.2020.04.002] [PMCID]
- Motolese F, Rossi M, Albergo G, Stelitano D, Villanova M, Di Lazzaro V, et al. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front Neurol. 2020; 11:580507. [DOI:10.3389/fneur.2020.580507] [PMID] [PMCID]
- Millevert C, Van Hees S, Siewe Fodjo JN, Wijtvliet V, Faria de Moura Villela E, Rosso B, et al. Impact of COVID-19 on the lives and psychosocial well-being of persons with epilepsy during the third trimester of the pandemic: Results from an international, online survey. Epilepsy Behav. 2021; 116:107800. [DOI:10.1016/j.yebeh.2021.107800] [PMID] [PMCID]
- Donisi V, Gajofatto A, Mazzi MA, Gobbin F, Busch IM, Ghellere A, et al. Insights for fostering resilience in young adults with multiple sclerosis in the aftermath of the COVID-19 emergency: An Italian survey. Front Psychiatry. 2021; 11:588275. [DOI:10.3389/fpsyt.2020.588275] [PMID] [PMCID]
- Broche-Pérez Y, Jiménez-Morales RM, Monasterio-Ramos LO, Vázquez-Gómez LA, Fernández-Fleites Z. Fear of COVID-19, problems accessing medical appointments, and subjective experience of disease progression, predict anxiety and depression reactions in patients with Multiple Sclerosis. Mult Scler Relat Disord. 2021; 53:103070. [DOI:10.1016/j.msard.2021.103070] [PMID] [PMCID]
- Shaygannejad V, Mirmosayyeb O, Nehzat N, Ghajarzadeh M. Fear of relapse, social support, and psychological well-being (depression, anxiety, and stress level) of patients with multiple sclerosis (MS) during the COVID-19 pandemic stage. Neurol Sci. 2021; 42(7):2615-8. [DOI:10.1007/s10072-021-05253-8] [PMID] [PMCID]
- Alschuler KN, Roberts MK, Herring TE, Ehde DM. Distress and risk perception in people living with multiple sclerosis during the early phase of the COVID-19 pandemic. Mult Scler Relat Disord. 2021; 47:102618. [DOI:10.1016/j.msard.2020.102618] [PMID] [PMCID]
- Stojanov A, Malobabic M, Milosevic V, Stojanov J, Vojinovic S, Stanojevic G, et al. Psychological status of patients with relapsing-remitting multiple sclerosis during coronavirus disease-2019 outbreak. Mult Scler Relat Disord. 2020; 45:102407. [DOI:10.1016/j.msard.2020.102407] [PMID] [PMCID]
- Giordano A, Siciliano M, De Micco R, Sant’Elia V, Russo A, Tedeschi G, et al. Correlates of psychological distress in epileptic patients during the COVID-19 outbreak. Epilepsy Behav. 2021; 115:107632. [DOI:10.1016/j.yebeh.2020.107632] [PMID] [PMCID]
- Puteikis K, Jasionis A, Mameniškienė R. Recalling the COVID-19 lockdown: Insights from patients with epilepsy. Epilepsy Behav. 2021; 115:107573. [DOI:10.1016/j.yebeh.2020.107573] [PMID] [PMCID]
- Alkhotani A, Siddiqui MI, Almuntashri F, Baothman R. The effect of COVID-19 pandemic on seizure control and self-reported stress on patient with epilepsy. Epilepsy Behav. 2020; 112:107323. [DOI:10.1016/j.yebeh.2020.107323] [PMID] [PMCID]
- Van Hees S, Siewe Fodjo JN, Wijtvliet V, Van den Bergh R, Faria de Moura Villela E, da Silva CF, et al. Access to healthcare and prevalence of anxiety and depression in persons with epilepsy during the COVID-19 pandemic: A multicountry online survey. Epilepsy Behav. 2020; 112:107350. [PMID]
- Niimi K, Fujimoto A, Sato K, Enoki H, Okanishi T. Patients with epilepsy who underwent epilepsy surgery during the COVID-19 pandemic showed less depressive tendencies. Front Neurol. 2021; 12:677828. [DOI:10.3389/fneur.2021.677828] [PMID] [PMCID]
- Ramezani N, Ashtari F, Bastami EA, Ghaderi K, Hosseini SM, Naeini MK, et al. Fear and anxiety in patients with multiple sclerosis during COVID-19 pandemic; report of an Iranian population. Mult Scler Relat Disord. 2021; 50:102798. [DOI:10.1016/j.msard.2021.102798] [PMID] [PMCID]
- Gul ZB. Depression and sexual functions in epilepsy patients: Comparison before and during the COVID-19 pandemic. Ann Med Psychol (Paris). 2022; 180(2):127-32. [DOI:10.1016/j.amp.2021.02.006] [PMID] [PMCID]
- Talaat F, Ramadan I, Aly S, Hamdy E. Are multiple sclerosis patients and their caregivers more anxious and more committed to following the basic preventive measures during the COVID-19 pandemic? Mult Scler Relat Disord. 2020; 46:102580. [DOI:10.1016/j.msard.2020.102580] [PMID] [PMCID]
- Strizović S, Vojvodić N, Kovačević M, Pejović A, Bukumirić Z, Sokić D, et al. Influence of COVID-19 pandemic on quality of life in patients with epilepsy-Follow-up study. Epilepsy Behav. 2021; 121(Pt A):108026. [DOI:10.1016/j.yebeh.2021.108026] [PMID] [PMCID]
- Bonavita S, Sparaco M, Russo A, Borriello G, Lavorgna L. Perceived stress and social support in a large population of people with multiple sclerosis recruited online through the COVID‐19 pandemic. Eur J Neurol. 2021; 28(10):3396-402. [DOI:10.1111/ene.14697] [PMID]
- Costabile T, Carotenuto A, Lavorgna L, Borriello G, Moiola L, Inglese M, et al. COVID‐19 pandemic and mental distress in multiple sclerosis: Implications for clinical management. Eur J Neurol. 2021; 28(10):3375-83. [DOI:10.1111/ene.14580] [PMID] [PMCID]
- Abokalawa F, Ahmad SF, Al-Hashel J, Hassan AM, Arabi M. The effects of coronavirus disease 2019 (COVID-19) pandemic on people with epilepsy (PwE): An online survey-based study. Acta Neurol Belg. 2021; 8:1–8. [DOI:10.1007/s13760-021-01609-1] [PMID] [PMCID]
- Garjani A, Hunter R, Law GR, Middleton RM, Tuite-Dalton KA, Dobson R, et al. Mental health of people with multiple sclerosis during the COVID-19 outbreak: A prospective cohort and cross-sectional case-control study of the UK MS Register. Mult Scler. 2021; 3:13524585211020435. [DOI:10.1177/13524585211020435] [PMID]
- Huang S, Wu C, Jia Y, Li G, Zhu Z, Lu K, et al. COVID‐19 outbreak: The impact of stress on seizures in patients with epilepsy. Epilepsia. 2020; 61(9):1884-93. [DOI:10.1111/epi.16635] [PMID] [PMCID]
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010; 8(5):336-41. [DOI:10.1016/j.ijsu.2010.02.007] [PMID]
- Gifford W, Davies B, Edwards N, Griffin P, Lybanon V. Managerial leadership for nurses’ use of research evidence: An integrative review of the literature. Worldviews Evid Based Nurs. 2007; 4(3):126-45. [DOI:10.1111/j.1741-6787.2007.00095.x] [PMID]
- Asadi-Pooya AA, Farazdaghi M, Bazrafshan M. Impacts of the COVID‐19 pandemic on Iranian patients with epilepsy. Acta Neurol Scand. 2020; 142(4):392-5. [DOI:10.1111/ane.13310] [PMID] [PMCID]
- Chiaravalloti ND, Amato MP, Brichetto G, Chataway J, Dalgas U, DeLuca J, et al. The emotional impact of the COVID-19 pandemic on individuals with progressive multiple sclerosis. J Neurol. 2021; 268(5):1598-607. [DOI:10.1007/s00415-020-10160-7] [PMID] [PMCID]
- Demir CF, Bilek F, Balgetir F. Neuropsychiatric changes during the COVID-19 pandemic in multiple sclerosis patients. Arq Neuropsiquiatr. 2020; 78(9):570-5. [PMID]
- Hao X, Zhou D, Li Z, Zeng G, Hao N, Li E, et al. Severe psychological distress among patients with epilepsy during the COVID‐19 outbreak in southwest China. Epilepsia. 2020; 61(6):1166-73. [DOI:10.1111/epi.16544] [PMID] [PMCID]
- Yan H, Valdes AM, Vijay A, Wang S, Liang L, Yang S, et al. Role of drugs used for chronic disease management on susceptibility and severity of COVID‐19: A large case‐control study. Clin Pharmacol Ther. 2020; 108(6):1185-94. [DOI:10.1002/cpt.2047] [PMID]
- Ghaffar O, Feinstein A. The neuropsychiatry of multiple sclerosis: A review of recent developments. Curr Opin Psychiatry. 2007; 20(3):278-85. [DOI:10.1097/YCO.0b013e3280eb10d7] [PMID]
- Lozano-Soto E, Cruz-López ÁJ, Gutiérrez R, González M, Sanmartino F, Rashid-Lopez R, et al. Predicting neuropsychological impairment in relapsing remitting multiple sclerosis: The role of clinical measures, treatment, and neuropsychiatry symptoms. Arch Clin Neuropsychol. 2021; 36(4):475-84. [DOI:10.1093/arclin/acaa088] [PMID]
- Myers L, Trobliger R, Bortnik K, Zeng R, Saal E, Lancman M. Psychological trauma, somatization, dissociation, and psychiatric comorbidities in patients with psychogenic nonepileptic seizures compared with those in patients with intractable partial epilepsy. Epilepsy Behav. 2019; 92:108-13. [DOI:10.1016/j.yebeh.2018.12.027] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2022/04/17 | Accepted: 2022/04/21 | Published: 2022/04/21
Received: 2022/04/17 | Accepted: 2022/04/21 | Published: 2022/04/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |