Fri, Apr 26, 2024
Volume 7, Issue 4 (Autumn 2021)
Caspian J Neurol Sci 2021, 7(4): 227-235 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sedaghati P, Hosseini A H, Zarei H. Effect of Exercise Programs on Fear of Falling in Multiple Sclerosis: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Caspian J Neurol Sci 2021; 7 (4) :227-235
URL: http://cjns.gums.ac.ir/article-1-469-en.html
URL: http://cjns.gums.ac.ir/article-1-469-en.html
1- Department of Sports Injury and Corrective Exercises, Faculty of Physical Education & Sport Sciences, University of Guilan, Rasht, Iran.
2- Department of Sports Injury and Corrective Exercises, Faculty of Physical Education & Sport Sciences, University of Guilan, Rasht, Iran. , zareei.h@yahoo.com
2- Department of Sports Injury and Corrective Exercises, Faculty of Physical Education & Sport Sciences, University of Guilan, Rasht, Iran. , zareei.h@yahoo.com
Full-Text [PDF 1359 kb]
(560 Downloads)
| Abstract (HTML) (1310 Views)
Full-Text: (583 Views)
Introduction
Multiple Sclerosis (MS) is one of the most common diseases of the Central Nervous System (CNS) [1]. MS is caused by damage to the myelin sheath [2]. The nerve damage is caused by inflammation and can occur along any area of the brain, optic nerve, and spinal cord [3]. Eventually, the disease can cause permanent damages to or deterioration of the nerves [4]. Different factors have been suggested as the underlying, causative, or accelerator factors of MS [5, 6].
The symptoms of the disease are different in people, including imbalance, lack of coordination, numbness, and limb paralysis, and fatigue [7, 8]. Decreased mobility due to imbalance, weakness, and muscle stiffness are commonly reported among MS patients [9]. Imbalance increases the risk of development of disability and the risk of falling. Falling is one of the major problems in the healthcare system. The World Health Organization (WHO) considers falling to be the third leading cause of chronic disability in the world [10]. It is a major health-related issue among MS patients. MS patients experience frequent falling [11], especially in patients who presented with balance disorders [12]. Regarding the factors affecting falling in these people, poor balance, progressive MS, and the use of assistive devices can be among the factors that increase the risk of falls [13]. In addition, Kalron et al (2013) [14] and Matsuda et al. (2011) showed that falling and Fear of falling (FOF) are the most common symptoms in MS patients and reduce their quality of life [15].
FOF is defined as a mental state limiting physical activity [16]. Tinetti and Powell (1993) described FOF as ongoing concern about falling that ultimately, limits the performance of daily activities [17]. Other authors have referred to FOF as a patient’s loss of confidence in his or her balance abilities [18, 19]. FOF can be defined as a general concept that lowers fall-related efficacy (low confidence at avoiding falls) and makes the person afraid of falling [20]. Numerous studies have reported FOF among MS patients [21, 22]. The level of FOF among MS patients can lead to excessive care, movement limitations, and lack of independence, which in turn, can lead to a decline in physical and motor function of these people [13]. Therefore, FOF and subsequent avoidance of physical activities can impair the physical and motor function of MS patients, especially their balance [23]. Finlayson et al. (2004) found that 60% of MS patients who experience falling suffer from FOF [24]. Researchers have evaluated the consequences of falling and the subsequent psychological factors. Friedman et al. (2002) investigated the relationship between falling and FOF [25].
Regular physical activity is very important for maintaining health and can increase mobility and reduce FOF among MS patients [26]. For this reason, studies have investigated the effect of participation in exercise activities as well as exercise programs on reducing falling among these people; however, it is not yet clear which exercise programs play an important role in reducing FOF among MS patients and whether exercise programs have a significant effect on FOF. Therefore, the aim of the present review and meta-analysis was to investigate the effect of exercise programs on FOF in MS patients. The present study also was done to determine which exercise program is most beneficial for reducing FOF among MS patients.
Materials and Methods
Search strategies
Articles published from inception until April 2021were found by searching 9 databases, i.e. MEDLINE/PubMed, EMBASE, SCOPUS, LILACS, CINAHL, CENTRAL (Cochrane Central Register of Controlled Trials), Web of Science, PEDro, and Google Scholar.
Keywords
The keywords were initially selected from MeSH terms and then modified to ensure that all eligible studies were found. In addition, a manual search and full review of article references was performed. The databases were searched using the following keywords:
(1) Fear of falling “OR” fall “OR” Accidental Fall; AND (2) Multiple Sclerosis “OR” MS “OR” Demyelinating Disease; AND (3) exercise training “OR”, exercise “OR”, physical exercise “OR”, exercise program “OR”, exercise therapy “OR” training “OR” exercise work-out. The “AND” operator was used between the 3 keyword groups, while the “OR” operator was used within each keyword group.
After collecting the search results, the title and then the abstract of the articles were studied. If the articles met the inclusion and exclusion criteria, their results were used in the present review, and the others were excluded. Based on the inclusion criteria and objectives of the research, nine articles were selected after the evaluation process. All full-text articles were made available.
Inclusion criteria
In the first stage, the screening of the title and abstract of descriptive studies was performed focusing on examining the effect of exercise programs on FOF in MS patients. Only randomized controlled trials (RCTs) published in peer-reviewed journals were considered. A research assistant independently reviewed abstracts of articles. In the second stage, full-text screening was performed by a researcher. A senior researcher also checked the final list of selected articles to ensure that all articles were in line with the research objective. Summary of descriptive information was collected by the research assistant and checked by the senior researcher. The typical process for selecting studies is shown in Figure 1.
.PNG)
Exclusion criteria
Articles whose study population included people other than MS patients, articles with the unspecified procedure, non-randomized clinical trials, and articles on the effect of exercise programs on factors other than the FOF factor were excluded.
Quality assessment
The PEDro scale was used to evaluate the quality of articles. This scale consists of 11 questions. One score is given for each question. Scores 7≥, 5-6, and 5≤ indicate high, moderate, and low levels of quality, respectively. High-quality articles were included in the present meta-analysis. Two independent reviewers (H.Z. and P.S.) did the search task, and independently applied further screening of title and abstract using the above criteria. Any disagreement was negotiated. The level of agreement between the reviewers was measured using Cohen’s kappa (j). A қ value of ≤0.4 indicated poor agreement, 0.41-0.6 moderate agreement, 0.61-0.8 good agreement, and 0.81-1 excellent agreement [27].
Data extraction
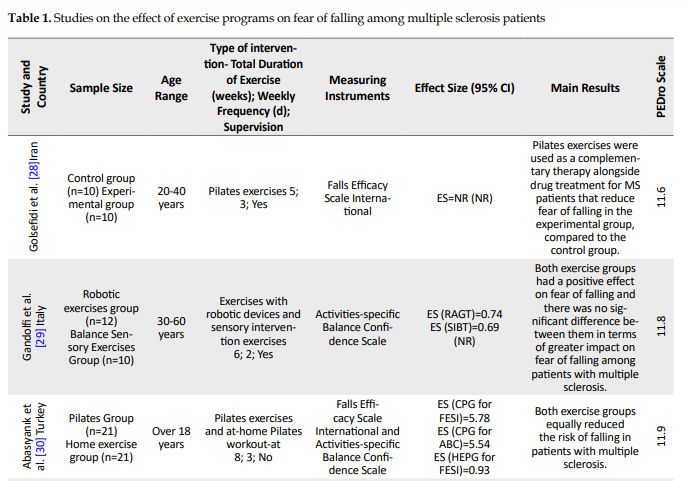
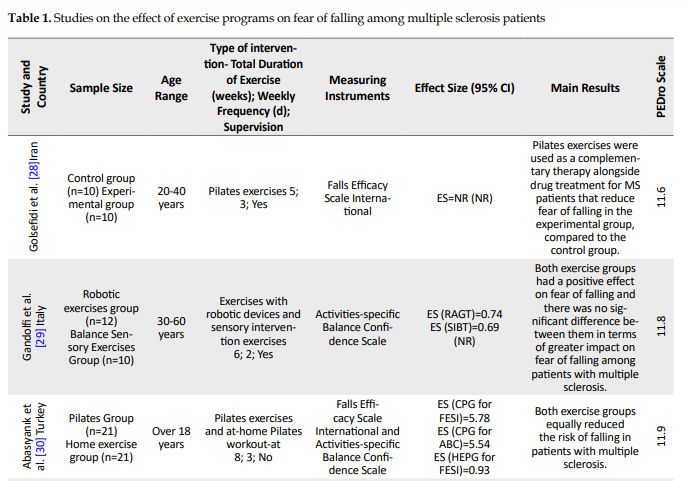
Data from studies were extracted independently by reviewers using some measures including the first author’s name, sample size, participants’ characteristics, main outcome measures, assessment instruments, intervention, main outcomes, and quality assessment of the study (Table 1).
.PNG)
.PNG)
.PNG)
Statistical Analyses
Hedges’ g (ratio of the mean difference between the two groups to the mixed weight standard deviation) was used for meta-analysis. Study heterogeneity was assessed using the I2 index. Random- and fixed-effects model methods were used respectively for heterogeneity above and below 50%. The publication bias was assessed using Egger’s test. Data analysis was carried out using Comprehensive Meta-analysis v. 2.
Results
A search of electronic references yielded 168 titles. Manual search and literature review yielded 10 more titles. After removing similar titles, 98 abstracts were identified. After reviewing the titles and abstracts of the articles, 71 articles were removed from the analysis, and 17 full-text articles were selected. After reviewing these full-text articles, 9 articles that examined the effect of exercise programs on FOF among MS patients were selected and their results were reported (Figure 1 and Table 1).
The quality level of the articles was assessed using the PEDro tool and the average score was more than seven, which indicates that the articles selected in the present meta-analysis are of high quality and the results of these studies are reliable.
CON, control group; EXP, experimental group; NR, not reported; FESI, Falls Efficacy Scale International; ABC, Activities-specific Balance Confidence Scale; CPG, Clinical Pilates Group; HEPG, Home Exercise Program Group; VR, Virtual Reality; RAGT, Robot-Assisted Gait Training; SIBT, Sensory Integration Balance Training. The I2 index showed 74% heterogeneity between studies; thus, the random effect meta-analysis model was used. The Hedges’ g value of the effect of exercise programs on FOF in MS patients was -0.15 with a 95% confidence interval (0.22 and -0.52). The results of the meta-analysis showed no significant difference between the effects of exercise programs on FOF in MS patients (P=0.44). Egger’s test value was also 0.21, which showed no publication bias between studies (Figure 2).
Discussion
The aim of the present study was to investigate the effect of exercise programs on FOF among MS patients. The literature review showed that there has been no meta-analysis on the effect of exercise programs on FOF among MS patients. The results of the present meta-analysis showed that all exercise programs have a positive effect on FOF and increase self-confidence and reduce FOF among MS patients. The results also showed no significant difference between exercise programs on the greater impact on FOF among MS patients. The results of the study showed that one exercise program cannot be considered superior to others in terms of its effect on FOF among MS patients.
The studies had used two questionnaires to assess the FOF; Falls Efficacy Scale International (FES-I) and Activities-specific Balance Confidence (ABC) Scale. The FES-I is a short, easy to administer tool that measures the level of concern about falling during social and physical activities inside and outside the home and whether or not the person does the activity. The level of concern is measured on a four-point Likert scale (1=not at all concerned to 4=very concerned). The ABC scale is a patient-reported outcome measure that asks individuals to rate how confident they are that they will not lose their balance while performing 16 different activities. The patients are asked to rate their confidence in their balance, while performing 16 activities, on a percentage scale of 0 to 100, where 0 is a certainty of falling or becoming unstable and 100 is complete confidence in the patient’s own ability to stay balanced.
Overall, nine articles had examined the effect of exercise programs on FOF among MS patients, of which the control group of only one study did not participate in exercise interventions [28]. The results of this study showed a significant reduction in FOF in the exercise group compared to the control group (impact size= 4.30). This study had used Pilates exercises for the exercise group. Pilates exercises are a good method to practice mind-body awareness and control postural movements with high neuromuscular demands [37]. This exercise method is performed in static positions (lying, sitting, and standing), and reduces the risk of joint and muscle injuries [38]. Numerous studies have also shown that Pilates exercises reduce muscle strength, balance, flexibility, and reaction time, and prevent falls [39]. In addition, Pilates exercises reduce FOF and the incidence of this accident among different populations [40, 41]. Therefore, Pilates exercises seem to be a suitable method to reduce the risk of falls and increase the self-confidence of MS patients. Although for better and more definite conclusions, it is necessary to compare these exercise programs with other exercise programs to determine which has a better and greater effect on FOF and increases the self-confidence of MS patients.
Also, in 8 out of 9 studies, the control group participated in exercise interventions. These studies had investigated the effect of two exercise programs on FOF among MS patients [29-36]. The results of these studies showed that all exercise programs had a significant effect on FOF and there was no statistically significant difference between exercise interventions. Exercise programs have almost the same level of effectiveness, and each exercise program can be used to reduce FOF and increase the self-confidence of MS patients. However, the effect size of the two exercise programs was greater than one exercise program [32]. Both studies had used virtual reality (VR) exercise programs (exergaming) [36]. Exergaming is a popular technology that allows people to use body movements to simulate physical activity on the screen [42]. The use of these exercises has received much attention in recent decades because exergaming is not only considered as an entertainment option but also as a tool to improve health status [43]. In addition, exergaming has been immediately recognized as a positive development because of its contribution as a tool against sedentary lifestyles [44]. The current generation of these exercises is also widely used for motor and rehabilitation activities [45]. Therefore, it seems that this type of exercise has a great effect on reducing FOF and increases self-confidence, leading to an increase in the desire for more mobility among MS patients. It is reported that FOF leads to inactivity and consequently, more functional dependence in these people [21, 46].
The results of the present meta-analysis showed that exercise programs have a positive effect on reducing FOF and increasing self-confidence in MS patients. In addition, Pilates and exergaming programs had a greater effect on reducing FOF than other exercise programs clinically, although statistically, the difference was not significant. It has been reported that these exercise programs have a greater effect on the mind and dual-task activities. According to Mirelman et al. study (2016), the cognitive-motor nature of VR-based exercises performing in an environment requires attention, concentration, motor planning, and problem-solving and could implicitly enhance fall-prevention strategies and improve functional performance during daily challenging and attention-demanding situations, which reduces falling in real life [47]. Besides its psychological benefits, Pilates improves personal autonomy, mobility, functional ability, and confidence in terms of movement, exercise, and other activities [41].
The Pilates practitioners are confident in their ability to perform daily activities without falling [48]. It has also been reported that FOF is a psychological variable that ultimately reduces physical activity in these individuals [21]. Therefore, it seems that exercise programs that affect both minds and physical performance of people are more effective in reducing FOF in MS patients and thus increasing the level of self-confidence in these patients during exercise. These exercises also make these patients perform their daily functional activities with fewer worries. To draw better and more definite conclusions, there is a need to further research studies as well as various other exercise programs to determine the best and most effective exercise programs in reducing FOF among MS patients. The results of all these studies encourage MS patients to increase their desire to increase physical activity, as well as to perform daily physical activity with less FOF and greater self-confidence.
The present review study had several limitations. It focused only on the FOF variable; thus, it is necessary to examine the effect of exercise programs on other functional components to determine whether exercise programs improve other functional variables in these individuals or not. This meta-analysis only examined the effect of exercise programs and did not evaluate other rehabilitation interventions; therefore, it is necessary to investigate and compare these exercise programs with other rehabilitation interventions to determine which intervention program has a better and greater effect on FOF in MS patients.
Conclusion
In the present review, it was found that all exercise programs have a significant effect on reducing FOF in MS patients and increasing their self-confidence. It was also found that there was no significant difference between exercise programs in terms of their effectiveness in reducing FOF in these patients but Pilates and exergaming were more effective than other exercise programs. However, to draw better and more definite conclusions, further studies are needed to evaluate other exercise programs.
Ethical Considerations
Compliance with ethical guidelines
All study procedures complied with the ethical guidelines of the Declaration of Helsinki, 2013.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, writing of the original draft, and writing, review, editing, and supervision: Parisa Sedaghti and Hamed Zarei; Methodology: Amir Hosseini and Hamed Zarei; Investigation, funding acquisition, resources: All author.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors want to thank the Head of the Faculty of Physical Education, University of Guilan.
Refrences:
Multiple Sclerosis (MS) is one of the most common diseases of the Central Nervous System (CNS) [1]. MS is caused by damage to the myelin sheath [2]. The nerve damage is caused by inflammation and can occur along any area of the brain, optic nerve, and spinal cord [3]. Eventually, the disease can cause permanent damages to or deterioration of the nerves [4]. Different factors have been suggested as the underlying, causative, or accelerator factors of MS [5, 6].
The symptoms of the disease are different in people, including imbalance, lack of coordination, numbness, and limb paralysis, and fatigue [7, 8]. Decreased mobility due to imbalance, weakness, and muscle stiffness are commonly reported among MS patients [9]. Imbalance increases the risk of development of disability and the risk of falling. Falling is one of the major problems in the healthcare system. The World Health Organization (WHO) considers falling to be the third leading cause of chronic disability in the world [10]. It is a major health-related issue among MS patients. MS patients experience frequent falling [11], especially in patients who presented with balance disorders [12]. Regarding the factors affecting falling in these people, poor balance, progressive MS, and the use of assistive devices can be among the factors that increase the risk of falls [13]. In addition, Kalron et al (2013) [14] and Matsuda et al. (2011) showed that falling and Fear of falling (FOF) are the most common symptoms in MS patients and reduce their quality of life [15].
FOF is defined as a mental state limiting physical activity [16]. Tinetti and Powell (1993) described FOF as ongoing concern about falling that ultimately, limits the performance of daily activities [17]. Other authors have referred to FOF as a patient’s loss of confidence in his or her balance abilities [18, 19]. FOF can be defined as a general concept that lowers fall-related efficacy (low confidence at avoiding falls) and makes the person afraid of falling [20]. Numerous studies have reported FOF among MS patients [21, 22]. The level of FOF among MS patients can lead to excessive care, movement limitations, and lack of independence, which in turn, can lead to a decline in physical and motor function of these people [13]. Therefore, FOF and subsequent avoidance of physical activities can impair the physical and motor function of MS patients, especially their balance [23]. Finlayson et al. (2004) found that 60% of MS patients who experience falling suffer from FOF [24]. Researchers have evaluated the consequences of falling and the subsequent psychological factors. Friedman et al. (2002) investigated the relationship between falling and FOF [25].
Regular physical activity is very important for maintaining health and can increase mobility and reduce FOF among MS patients [26]. For this reason, studies have investigated the effect of participation in exercise activities as well as exercise programs on reducing falling among these people; however, it is not yet clear which exercise programs play an important role in reducing FOF among MS patients and whether exercise programs have a significant effect on FOF. Therefore, the aim of the present review and meta-analysis was to investigate the effect of exercise programs on FOF in MS patients. The present study also was done to determine which exercise program is most beneficial for reducing FOF among MS patients.
Materials and Methods
Search strategies
Articles published from inception until April 2021were found by searching 9 databases, i.e. MEDLINE/PubMed, EMBASE, SCOPUS, LILACS, CINAHL, CENTRAL (Cochrane Central Register of Controlled Trials), Web of Science, PEDro, and Google Scholar.
Keywords
The keywords were initially selected from MeSH terms and then modified to ensure that all eligible studies were found. In addition, a manual search and full review of article references was performed. The databases were searched using the following keywords:
(1) Fear of falling “OR” fall “OR” Accidental Fall; AND (2) Multiple Sclerosis “OR” MS “OR” Demyelinating Disease; AND (3) exercise training “OR”, exercise “OR”, physical exercise “OR”, exercise program “OR”, exercise therapy “OR” training “OR” exercise work-out. The “AND” operator was used between the 3 keyword groups, while the “OR” operator was used within each keyword group.
After collecting the search results, the title and then the abstract of the articles were studied. If the articles met the inclusion and exclusion criteria, their results were used in the present review, and the others were excluded. Based on the inclusion criteria and objectives of the research, nine articles were selected after the evaluation process. All full-text articles were made available.
Inclusion criteria
In the first stage, the screening of the title and abstract of descriptive studies was performed focusing on examining the effect of exercise programs on FOF in MS patients. Only randomized controlled trials (RCTs) published in peer-reviewed journals were considered. A research assistant independently reviewed abstracts of articles. In the second stage, full-text screening was performed by a researcher. A senior researcher also checked the final list of selected articles to ensure that all articles were in line with the research objective. Summary of descriptive information was collected by the research assistant and checked by the senior researcher. The typical process for selecting studies is shown in Figure 1.
.PNG)
Exclusion criteria
Articles whose study population included people other than MS patients, articles with the unspecified procedure, non-randomized clinical trials, and articles on the effect of exercise programs on factors other than the FOF factor were excluded.
Quality assessment
The PEDro scale was used to evaluate the quality of articles. This scale consists of 11 questions. One score is given for each question. Scores 7≥, 5-6, and 5≤ indicate high, moderate, and low levels of quality, respectively. High-quality articles were included in the present meta-analysis. Two independent reviewers (H.Z. and P.S.) did the search task, and independently applied further screening of title and abstract using the above criteria. Any disagreement was negotiated. The level of agreement between the reviewers was measured using Cohen’s kappa (j). A қ value of ≤0.4 indicated poor agreement, 0.41-0.6 moderate agreement, 0.61-0.8 good agreement, and 0.81-1 excellent agreement [27].
Data extraction
Data from studies were extracted independently by reviewers using some measures including the first author’s name, sample size, participants’ characteristics, main outcome measures, assessment instruments, intervention, main outcomes, and quality assessment of the study (Table 1).
.PNG)
.PNG)
.PNG)
Statistical Analyses
Hedges’ g (ratio of the mean difference between the two groups to the mixed weight standard deviation) was used for meta-analysis. Study heterogeneity was assessed using the I2 index. Random- and fixed-effects model methods were used respectively for heterogeneity above and below 50%. The publication bias was assessed using Egger’s test. Data analysis was carried out using Comprehensive Meta-analysis v. 2.
Results
A search of electronic references yielded 168 titles. Manual search and literature review yielded 10 more titles. After removing similar titles, 98 abstracts were identified. After reviewing the titles and abstracts of the articles, 71 articles were removed from the analysis, and 17 full-text articles were selected. After reviewing these full-text articles, 9 articles that examined the effect of exercise programs on FOF among MS patients were selected and their results were reported (Figure 1 and Table 1).
The quality level of the articles was assessed using the PEDro tool and the average score was more than seven, which indicates that the articles selected in the present meta-analysis are of high quality and the results of these studies are reliable.
CON, control group; EXP, experimental group; NR, not reported; FESI, Falls Efficacy Scale International; ABC, Activities-specific Balance Confidence Scale; CPG, Clinical Pilates Group; HEPG, Home Exercise Program Group; VR, Virtual Reality; RAGT, Robot-Assisted Gait Training; SIBT, Sensory Integration Balance Training. The I2 index showed 74% heterogeneity between studies; thus, the random effect meta-analysis model was used. The Hedges’ g value of the effect of exercise programs on FOF in MS patients was -0.15 with a 95% confidence interval (0.22 and -0.52). The results of the meta-analysis showed no significant difference between the effects of exercise programs on FOF in MS patients (P=0.44). Egger’s test value was also 0.21, which showed no publication bias between studies (Figure 2).
Discussion
The aim of the present study was to investigate the effect of exercise programs on FOF among MS patients. The literature review showed that there has been no meta-analysis on the effect of exercise programs on FOF among MS patients. The results of the present meta-analysis showed that all exercise programs have a positive effect on FOF and increase self-confidence and reduce FOF among MS patients. The results also showed no significant difference between exercise programs on the greater impact on FOF among MS patients. The results of the study showed that one exercise program cannot be considered superior to others in terms of its effect on FOF among MS patients.
The studies had used two questionnaires to assess the FOF; Falls Efficacy Scale International (FES-I) and Activities-specific Balance Confidence (ABC) Scale. The FES-I is a short, easy to administer tool that measures the level of concern about falling during social and physical activities inside and outside the home and whether or not the person does the activity. The level of concern is measured on a four-point Likert scale (1=not at all concerned to 4=very concerned). The ABC scale is a patient-reported outcome measure that asks individuals to rate how confident they are that they will not lose their balance while performing 16 different activities. The patients are asked to rate their confidence in their balance, while performing 16 activities, on a percentage scale of 0 to 100, where 0 is a certainty of falling or becoming unstable and 100 is complete confidence in the patient’s own ability to stay balanced.
Overall, nine articles had examined the effect of exercise programs on FOF among MS patients, of which the control group of only one study did not participate in exercise interventions [28]. The results of this study showed a significant reduction in FOF in the exercise group compared to the control group (impact size= 4.30). This study had used Pilates exercises for the exercise group. Pilates exercises are a good method to practice mind-body awareness and control postural movements with high neuromuscular demands [37]. This exercise method is performed in static positions (lying, sitting, and standing), and reduces the risk of joint and muscle injuries [38]. Numerous studies have also shown that Pilates exercises reduce muscle strength, balance, flexibility, and reaction time, and prevent falls [39]. In addition, Pilates exercises reduce FOF and the incidence of this accident among different populations [40, 41]. Therefore, Pilates exercises seem to be a suitable method to reduce the risk of falls and increase the self-confidence of MS patients. Although for better and more definite conclusions, it is necessary to compare these exercise programs with other exercise programs to determine which has a better and greater effect on FOF and increases the self-confidence of MS patients.
Also, in 8 out of 9 studies, the control group participated in exercise interventions. These studies had investigated the effect of two exercise programs on FOF among MS patients [29-36]. The results of these studies showed that all exercise programs had a significant effect on FOF and there was no statistically significant difference between exercise interventions. Exercise programs have almost the same level of effectiveness, and each exercise program can be used to reduce FOF and increase the self-confidence of MS patients. However, the effect size of the two exercise programs was greater than one exercise program [32]. Both studies had used virtual reality (VR) exercise programs (exergaming) [36]. Exergaming is a popular technology that allows people to use body movements to simulate physical activity on the screen [42]. The use of these exercises has received much attention in recent decades because exergaming is not only considered as an entertainment option but also as a tool to improve health status [43]. In addition, exergaming has been immediately recognized as a positive development because of its contribution as a tool against sedentary lifestyles [44]. The current generation of these exercises is also widely used for motor and rehabilitation activities [45]. Therefore, it seems that this type of exercise has a great effect on reducing FOF and increases self-confidence, leading to an increase in the desire for more mobility among MS patients. It is reported that FOF leads to inactivity and consequently, more functional dependence in these people [21, 46].
The results of the present meta-analysis showed that exercise programs have a positive effect on reducing FOF and increasing self-confidence in MS patients. In addition, Pilates and exergaming programs had a greater effect on reducing FOF than other exercise programs clinically, although statistically, the difference was not significant. It has been reported that these exercise programs have a greater effect on the mind and dual-task activities. According to Mirelman et al. study (2016), the cognitive-motor nature of VR-based exercises performing in an environment requires attention, concentration, motor planning, and problem-solving and could implicitly enhance fall-prevention strategies and improve functional performance during daily challenging and attention-demanding situations, which reduces falling in real life [47]. Besides its psychological benefits, Pilates improves personal autonomy, mobility, functional ability, and confidence in terms of movement, exercise, and other activities [41].
The Pilates practitioners are confident in their ability to perform daily activities without falling [48]. It has also been reported that FOF is a psychological variable that ultimately reduces physical activity in these individuals [21]. Therefore, it seems that exercise programs that affect both minds and physical performance of people are more effective in reducing FOF in MS patients and thus increasing the level of self-confidence in these patients during exercise. These exercises also make these patients perform their daily functional activities with fewer worries. To draw better and more definite conclusions, there is a need to further research studies as well as various other exercise programs to determine the best and most effective exercise programs in reducing FOF among MS patients. The results of all these studies encourage MS patients to increase their desire to increase physical activity, as well as to perform daily physical activity with less FOF and greater self-confidence.
The present review study had several limitations. It focused only on the FOF variable; thus, it is necessary to examine the effect of exercise programs on other functional components to determine whether exercise programs improve other functional variables in these individuals or not. This meta-analysis only examined the effect of exercise programs and did not evaluate other rehabilitation interventions; therefore, it is necessary to investigate and compare these exercise programs with other rehabilitation interventions to determine which intervention program has a better and greater effect on FOF in MS patients.
Conclusion
In the present review, it was found that all exercise programs have a significant effect on reducing FOF in MS patients and increasing their self-confidence. It was also found that there was no significant difference between exercise programs in terms of their effectiveness in reducing FOF in these patients but Pilates and exergaming were more effective than other exercise programs. However, to draw better and more definite conclusions, further studies are needed to evaluate other exercise programs.
Ethical Considerations
Compliance with ethical guidelines
All study procedures complied with the ethical guidelines of the Declaration of Helsinki, 2013.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, writing of the original draft, and writing, review, editing, and supervision: Parisa Sedaghti and Hamed Zarei; Methodology: Amir Hosseini and Hamed Zarei; Investigation, funding acquisition, resources: All author.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors want to thank the Head of the Faculty of Physical Education, University of Guilan.
Refrences:
- Oh J, Vidal-Jordana A, Montalban X. Multiple sclerosis: Clinical aspects. Curr Opin Neurol. 2018; 31(6):752-9. [DOI:10.1097/WCO.0000000000000622] [PMID]
- Brownlee WJ, Hardy TA, Fazekas F, Miller DH. Diagnosis of multiple sclerosis: Progress and challenges. The Lancet. 2017; 389(10076):1336-46. [DOI:10.1016/S0140-6736(16)30959-X]
- Fox RJ, Coffey CS, Conwit R, Cudkowicz ME, Gleason T, Goodman A, et al. Phase 2 trial of ibudilast in progressive multiple sclerosis. N Engl J Med. 2018; 379(9):846-55. [DOI:10.1056/NEJMoa1803583] [PMID] [PMCID]
- Kamińska J, Koper OM, Piechal K, Kemona H. Multiple sclerosis-etiology and diagnostic potential. Postepy Hig Med Dosw (Online). 2017; 71:551-63. [DOI:10.5604/01.3001.0010.3836] [PMID]
- Saberi A, Akhondzadeh S, Kazemi S. Infectious agents and different course of multiple sclerosis: A systematic review. Acta Neurol Belg. 2018; 118(3):361-77. [DOI:10.1007/s13760-018-0976-y] [PMID]
- Saberi A, Kazemi S. Mitochondrial dysfunction in multiple sclerosis: A systematic review. Acta Med Iran. 2019; 57(1):5-16. [DOI:10.18502/acta.v57i1.1748]
- Dobson R, Giovannoni G. Multiple sclerosis-a review. Eur J Neurol. 2019; 26(1):27-40. [DOI:10.1111/ene.13819] [PMID]
- Saberi A, Hatamian HR, Nemati S, Banan R. Hearing statement in multiple sclerosis: A case control study using auditory brainstem responses and otoacoustic emissions. Acta Medica Iranica. 2012; 50(12):679-83. https://acta.tums.ac.ir/index.php/acta/article/view/3973
- Lassmann H. Multiple sclerosis pathology. Cold Spring Harb Perspect Med. 2018; 8(3):a028936. [DOI:10.1101/cshperspect.a028936] [PMID] [PMCID]
- O’Malley N, Clifford AM, Comber L, Coote S. Fall definitions, faller classifications and outcomes used in falls research among people with multiple sclerosis: A systematic review. Disabil Rehabil. 2020:1-8. [DOI:10.1080/09638288.2020.1786173] [PMID]
- Etemadi Y. Dual task cost of cognition is related to fall risk in patients with multiple sclerosis: A prospective study. Clin Rehabil. 2017; 31(2):278-84. [DOI:10.1177/0269215516637201] [PMID]
- Hoang PD, Baysan M, Gunn H, Cameron M, Freeman J, Nitz J, et al. Fall risk in people with MS: A Physiological Profile Assessment study. Mult Scler J Exp Transl Clin. 2016; 2:2055217316641130. [DOI:10.1177/2055217316641130] [PMID] [PMCID]
- Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: A systematic review and meta-analysis. Phys Ther. 2013; 93(4):504-13. [DOI:10.2522/ptj.20120231] [PMID]
- Kalron A, Dvir Z, Achiron A. Effect of a cognitive task on postural control in patients with a clinically isolated syndrome suggestive of multiple sclerosis. Eur J Phys Rehabil Med. 2011; 47(4):579-86. [PMID]
- Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. PM R. 2011; 3(7):624-32. [DOI:10.1016/j.pmrj.2011.04.015] [PMID]
- Uemura K, Shimada H, Makizako H, Doi T, Tsutsumimoto K, Yoshida D, et al. Effects of mild and global cognitive impairment on the prevalence of fear of falling in community-dwelling older adults. Maturitas. 2014; 78(1):62-6. [DOI:10.1016/j.maturitas.2014.02.018] [PMID]
- Tinetti ME, Powell L. Fear of falling and low self-efficacy: A cause of dependence in elderly persons. J Gerontol. 1993; 48(Special Issue):35-8. [DOI:10.1093/geronj/48.Special_Issue.35] [PMID]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988; 319(26):1701-7. [DOI:10.1056/NEJM198812293192604] [PMID]
- Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991; 46(4):M123-31. [DOI:10.1093/geronj/46.4.M123] [PMID]
- Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000; 55(5):M299-305. [DOI:10.1093/gerona/55.5.M299] [PMID]
- Khalil H, Al-Shorman A, El-Salem K, Abdo N, Alghwiri AA, Aburub A, et al. Fear of falling in people with multiple sclerosis: Which clinical characteristics are important? Phys Ther. 2017; 97(7):698-706. [DOI:10.1093/ptj/pzx044] [PMID]
- Gunn H, Markevics S, Haas B, Marsden J, Freeman J. Systematic review: The effectiveness of interventions to reduce falls and improve balance in adults with multiple sclerosis. Arch Phys Med Rehabil. 2015; 96(10):1898-912. [DOI:10.1016/j.apmr.2015.05.018] [PMID]
- Comber L, Coote S, Finlayson M, Galvin R, Quinn G, Peterson E. An exploration of fall-related, psychosocial variables in people with multiple sclerosis who have fallen. Br J Occup Ther. 2017; 80(10):587-95. [DOI:10.1177/0308022617725492]
- Finlayson M, Denend TV, Shevil E. Multiple perspectives on the health service need, use, and variability among older adults with multiple sclerosis. Occup Ther Health Care. 2004; 17(3-4):5-25. [DOI:10.1080/J003v17n03_02] [PMID]
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002; 50(8):1329-35. [DOI:10.1046/j.1532-5415.2002.50352.x] [PMID]
- Motl RW, Sandroff BM, Kwakkel G, Dalgas U, Feinstein A, Heesen C, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017; 16(10):848-56. [DOI:10.1016/S1474-4422(17)30281-8]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159-74. [DOI:10.2307/2529310] [PMID]
- Rezvankhah Golsefidi N, Emami Hashemi SA. [Effect of pilates exercise on the number of fall, fear of falling, and reaction time of women with Multiple Sclerosis (Persian)]. Sci J Rehabil Med. 2017; 6(2):150-9. [DOI:10.22037/JRM.2017.1100307]
- Gandolfi M, Geroin C, Picelli A, Munari D, Waldner A, Tamburin S, et al. Robot-assisted vs. sensory integration training in treating gait and balance dysfunctions in patients with multiple sclerosis: A randomized controlled trial. Front Hum Neurosci. 2014; 8:318. [DOI:10.3389/fnhum.2014.00318] [PMID] [PMCID]
- Abasiyanik Z, Ertekin Ö, Kahraman T, Yigit P, Özakbas S. The effects of Clinical Pilates training on walking, balance, fall risk, respiratory, and cognitive functions in persons with multiple sclerosis: A randomized controlled trial. Explore (NY). 2020; 16(1):12-20. [DOI:10.1016/j.explore.2019.07.010] [PMID]
- Seddighi-Khavidak M, Tahan N, Akbarzadeh-Baghban A. Comparing the effects of vestibular rehabilitation with and without lavender oil scents as an olfactory stimulus on balance, fear of falling down and activities of daily living of people with multiple sclerosis: A randomized clinical trial. Disabil Rehabil. 2020:1-7. [DOI:10.1080/09638288.2020.1858352] [PMID]
- Molhemi F, Monjezi S, Mehravar M, Shaterzadeh-Yazdi M-J, Salehi R, Hesam S, et al. Effects of virtual reality vs conventional balance training on balance and falls in people with multiple sclerosis: A randomized controlled trial. Arch Phys Med Rehabil. 2021; 102(2):290-9. [DOI:10.1016/j.apmr.2020.09.395] [PMID]
- Kalron A, Fonkatz I, Frid L, Baransi H, Achiron A. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: A pilot randomized controlled trial. J Neuroeng Rehabil. 2016; 13:13. [DOI:10.1186/s12984-016-0124-y] [PMID] [PMCID]
- Novotna K, Janatova M, Hana K, Svestkova O, Preiningerova Lizrova J, Kubala Havrdova E. Biofeedback based home balance training can improve balance but not gait in people with multiple sclerosis. Mult Scler Int. 2019; 2019:2854130. [DOI:10.1155/2019/2854130] [PMID] [PMCID]
- Gandolfi M, Munari D, Geroin C, Gajofatto A, Benedetti MD, Midiri A, et al. Sensory integration balance training in patients with multiple sclerosis: A randomized, controlled trial. Mult Scler. 2015; 21(11):1453-62. [DOI:10.1177/1352458514562438] [PMID]
- Badawy WM, Zakaria HM, El-Nassag BA. Influence of interactive therapy on improving balance outcomes in patients with multiple sclerosis. J Med Sci Clin Res. 2015; 03(12):8713-6. [DOI:10.18535/jmscr/v3i12.43]
- Ghorbanian B, Mahmoudpoor A. [The effect of Pilates training and massage therapy on plasma serum levels of IL-17 and IFN-β as pro-Inflammatory cytokines in patients with Multiple Sclerosis (MS) (Persian)]. J Sports Biosci. 2020; 12(1):79-92. [DOI:10.22059/JSB.2020.276588.1332]
- Hornsby E, Johnston LM. Effect of Pilates intervention on physical function of children and youth: A systematic review. Arch Phys Med Rehabil. 2020; 101(2):317-28. [DOI:10.1016/j.apmr.2019.05.023] [PMID]
- Preet, Kalra S, Yadav J, Pawaria S. Effect of pilates on lower limb strength, dynamic balance, agility and coordination skills in aspiring state level badminton players. J Clin Diagn Res. 2019; 13(7):YC01-6. [DOI:10.7860/JCDR/2019/41713.12978]
- Moreno-Segura N, Igual-Camacho C, Ballester-Gil Y, Blasco-Igual MC, Blasco JM. The effects of the pilates training method on balance and falls of older adults: A systematic review and meta-analysis of randomized controlled trials. J Aging Phys Act. 2018; 26(2):327-44. [DOI:10.1123/japa.2017-0078] [PMID]
- Hita-Contreras F, Martínez-Amat A, Cruz-Díaz D, Pérez-López F. Fall prevention in postmenopausal women: The role of Pilates exercise training. Climacteric. 2016; 19(3):229-33. [DOI:10.3109/13697137.2016.1139564] [PMID]
- Farra SL, Gneuhs M, Hodgson E, Kawosa B, Miller ET, Simon A, et al. Comparative cost of virtual reality training and live exercises for training hospital workers for evacuation. Comput Inform Nurs. 2019; 37(9):446-54. [DOI:10.1097/CIN.0000000000000540] [PMID] [PMCID]
- Mihajlovic Z, Popovic S, Brkic K, Cosic K. A system for head-neck rehabilitation exercises based on serious gaming and virtual reality. Multimed Tools Appl. 2018; 77(15):19113-37. [DOI:10.1007/s11042-017-5328-z]
- Gomez J, Hoffman HG, Bistricky SL, Gonzalez M, Rosenberg L, Sampaio M, et al. The use of virtual reality facilitates dialectical behavior therapy®”observing sounds and visuals” mindfulness skills training exercises for a Latino patient with severe burns: A case study. Front Psychol. 2017; 8:1611. [DOI:10.3389/fpsyg.2017.01611] [PMID] [PMCID]
- Costa MTS, Vieira LP, de Oliveira Barbosa E, Oliveira LM, Maillot P, Vaghetti CAO, et al. Virtual reality-based exercise with exergames as medicine in different contexts: A short review. Clin Pract Epidemiol Ment Health. 2019; 15:15-20. [DOI:10.2174/1745017901915010015]
- Perrochon A, Holtzer R, Laidet M, Armand S, Assal F, Lalive P, et al. Postural control is associated with cognition and fear of falling in patients with multiple sclerosis. J Neural Transm (Vienna). 2017; 124(4):495-500. [DOI:10.1007/s00702-016-1668-5] [PMID]
- Mirelman A, Rochester L, Maidan I, Del Din S, Alcock L, Nieuwhof F, et al. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): A randomised controlled trial. Lancet. 2016; 388(10050):1170-82. [DOI:10.1016/S0140-6736(16)31325-3]
- Cruz-Díaz D, Martínez-Amat A, Manuel J, Casuso RA, de Guevara NML, Hita-Contreras F. Effects of a six-week Pilates intervention on balance and fear of falling in women aged over 65 with chronic low-back pain: A randomized controlled trial. Maturitas. 2015; 82(4):371-6. [DOI:10.1016/j.maturitas.2015.07.022] [PMID]
Type of Study: Review |
Subject:
Special
Received: 2021/06/2 | Accepted: 2021/08/10 | Published: 2021/10/1
Received: 2021/06/2 | Accepted: 2021/08/10 | Published: 2021/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |