Fri, Apr 26, 2024
Volume 7, Issue 4 (Autumn 2021)
Caspian J Neurol Sci 2021, 7(4): 216-226 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Razzaghi S, Moghtader L. Effect of Mindfulness Training on Distress Tolerance and Alexithymia in Mothers With Autistic Children. Caspian J Neurol Sci 2021; 7 (4) :216-226
URL: http://cjns.gums.ac.ir/article-1-468-en.html
URL: http://cjns.gums.ac.ir/article-1-468-en.html
1- Department of Psychology, Faculty of Humanities, Islamic Azad University, Rasht Branch, Rasht, Iran.
2- Department of Psychology, Faculty of Humanities, Islamic Azad University, Rasht Branch, Rasht, Iran. , moghtaderleila@yahoo.com
2- Department of Psychology, Faculty of Humanities, Islamic Azad University, Rasht Branch, Rasht, Iran. , moghtaderleila@yahoo.com
Full-Text [PDF 1513 kb]
(733 Downloads)
| Abstract (HTML) (1393 Views)
Full-Text: (833 Views)
Introduction
Autism is a developmental disorder that occurs in the first three years of a child’s life and affects normal brain development and social interactions, as well as speech and communication skills. This disease, which is accompanied by some special behaviors, can be considered as a disorder with a spectrum that manifests itself in different forms and different intensities in affected children [1]. Autism is the most famous type of disorder that affects all four areas of development, including sensory, social, language, and cognitive areas [2]. In a study conducted on 8-year-old children, it was reported that, in general, one in every 150 children had some forms of the disorder [3].
It has been found that parents of children with developmental and psychiatric problems compared with parents of normal children experience more distress [4]. A lower level of psychological distress tolerance is one of the important psychological signs in families with autistic children, which are manifested in relation to the ability to analyze psychological situations. Distress may be the result of physical and cognitive processes, but its representation is in the form of a negative emotional state that is often manifested by a tendency to react to get rid of negative emotional experiences [5]. Mothers with low levels of distress tolerance evaluate emotional distress experienced as exhausting and unacceptable. As a result, they try to alleviate this negative emotional state but are often unable to focus their attention on something other than their distress [6].
On the other hand, alexithymia is one of the problems that mothers with autistic children always suffer from. The presence of a difficult child in the family affects the whole family system and the parents of these children feel themselves immersed in their child’s problems [7]. Research has shown that family relationships affect the other aspects of a teenager’s life, like emotional features. People with alexithymia magnify normal physical arousals and seek treatment for physical symptoms in therapeutic measures [8]. Alexithymia is a type of defect and failure that causes an inability in cognitive processing of emotional information and emotion regulation [9]. Alexithymia causes disability in the use of emotions as a sign of emotional problems, hinders abstract thinking and reduces dream recall, causes difficulty in distinguishing between emotional states and body feelings, creates poker face, lack of emotional effects on the face, and limited capacity for empathy and self-awareness [10]
The treatment widely used today for alexithymia, distress tolerance, and problems arising from them is mindfulness therapy [11, 12]. Mindfulness is unbiased, indescribable, and present-based awareness about an experience that a person at a certain moment concentrates on it. In addition, this concept includes acknowledging and accepting the mentioned experience [13]. Mindfulness techniques are effective in increasing muscle relaxation and reducing worry, stress, and anxiety. It seems that the main mechanism of self-controlled mindfulness is attention because repetitive concentration on a neutral stimulus, such as breathing creates a proper environment for attention [14]. Thao (2014) considered mindfulness-based training to be effective in improving and regulating emotion and increasing the quality of life [15-18]. Bergsma et al. (2012) in a study on the effectiveness of mindfulness exercises on children with Attention Deficit Hyperactivity Disorder (ADHD) and mindful parenting for their parents in 24 participating families, found that an 8-week mindfulness training had a significant effect on distress tolerance of mothers of children with autism [19].
Statistics show an increase in the prevalence of autism in Iran and it is estimated that one in every 158 people has this disorder and on the other hand, the birth of a child with autism is difficult for families (especially for mothers) [20]. In addition, a few studies have been done on the effect of mindfulness training on the characteristics of mothers with autistic children, and no research has examined the effect of mindfulness training on their distress tolerance and alexithymia, which is a research gap in this area.
The results of this research can be helpful in prevention and helping these mothers to reduce alexithymia in the face of difficulties ahead and increase distress tolerance. Moreover, the results of this study can be applied in family counseling centers and couple therapy. Therefore, it is necessary to consider this issue. The aim of this study was to evaluate the effect of mindfulness training on distress tolerance and alexithymia of mothers with autistic children. Accordingly, in this study, we intend to address this question: Does mindfulness training affect distress tolerance and alexithymia of mothers with autistic children?
Materials and Methods
This quasi-experimental research with the pretest-posttest design was performed with a control group. The research population consisted of all mothers of children with autism spectrum in Rasht City, Guilan, Iran, in 2019, who referred to the “Negah-e No” Counseling Center. In this study, 30 people were selected by convenience sampling method and were randomly assigned to the experimental and control groups (15 cases in each group).
For behavioral sciences studies, about 15 subjects for each variable are required. In experimental research, the Cohen method has recently been used to determine the adequacy of sample size in statistical analysis. In this study, considering the alpha level of 0.05 and the effect size equal to 0.50 with a test power of 0.76, 15 people were selected for each group.
The experimental group received eight 90-minute sessions of Mindfulness-Based Cognitive Therapy (MBCT). Inclusion and exclusion criteria were used to select the subjects. Inclusion criteria were mothers with autistic children, lack of history of receiving the medical intervention, and willingness to participate in this educational program. Exclusion criteria were the absence of more than two training sessions, the use of other training methods to treat autism, and the emergence of unpredictable problems for mothers leading to interruption or disruption of treatment sessions.
Study instruments
Distress Tolerance Scale (DTS)
This scale is a self-report index to assess distress tolerance developed by Simmons and Gauher (2005) [21]. Items of this scale evaluate distress tolerance based on individual abilities for tolerating emotional distress, mental evaluation of distress, the degree of attention to negative emotions in the case of occurrence, and regulating actions for distress relief. The scale has 15 items and four subscales, namely the emotional distress tolerance (questions 1, 3, 5), attraction by negative emotions (questions 2, 4, 14), the mental evaluation of distress (questions 6, 7, 9-12), and regulating the efforts to relieve distress (questions 8, 13, 15). Items of the scale were scored based on a five-point Likert scale, ranging from strongly disagree (score: 1) to strongly agree (score: 5). High scores on this scale indicated high distress tolerance. The content validity of the tool was confirmed by the experts and regarding the reliability of the questionnaire, Cronbach’s alpha of subscales of the questionnaire was calculated as 0.72, 0.82, 0.78, and 0.70, respectively, and for the entire scale, it was equal to 0.82. In Iran, Azizi et al. (2010) stated that the Cronbach’s alpha value of this questionnaire was equal to 0.67 and the retest validity of this questionnaire was 0.79 [22].
Persian version of Toronto Alexithymia Scale (FTAS-20)
This scale was designed by Bagby, Parker, and Taylor in 1994 and consists of three subscales of difficulty in identifying emotions, difficulty in describing emotions, and externally-oriented thinking [23]. These researchers calculated the reliability of the scale using Cronbach’s alpha coefficient (0.81) and test-retest reliability (0.77) as optimum [24]. In Iran, the 20-item alexithymia scale, in two separate studies, was translated and validated to be used on a group of drug abusers, as well as clinical and non-clinical groups [25]. The first subscale consists of 7 items (1, 3, 6, 7, 9, 13, and 14), which evaluates the subject’s ability in identifying his/her emotions and distinguishing between emotions and physical sensations. The second subscale has 5 items (2, 4, 11, 12, and 17), which assesses the subject’s ability in expressing emotions and whether he or she is able to express his/her feelings in words. The third subscale has 8 items (5, 8, 10, 15, 16, 18, 19, and 20) and examines the extent to which a person is introverted and deepened in his/her and others’ inner feelings.
The range of responses to each item varies from strongly disagree (score: 1) to strongly agree (score 5) based on a 5-point Likert scale. Items 4, 5, 10, 18, and 19 are scored in the reverse method, i.e., “strongly disagree” gets a score of 5, and “strongly agree” gets a score of 1. On this scale, higher scores indicate higher alexithymia. The content validity of the questionnaire was accepted by the experts. The concurrent validity of FTAS-20 was evaluated and confirmed in terms of the correlation between the subscales of this test and the emotional intelligence, psychological well-being, and psychological helplessness scales. Moreover, the Cronbach’s alpha coefficients of FATS-20 and its three subscales of difficulty in recognizing emotions, difficulty in describing emotions, and externally-oriented thinking were calculated at 0.85, 0.82, 0.75, and 0.72, respectively, indicating good internal consistency of the scale [25].
Subjects were first evaluated for diagnosis of the disorder. Then, detailed studies were performed and after an exclusive interview with the mothers and identifying the study subjects, the baseline of each subject was determined through clinical observations during three sessions. Training sessions were regulated according to a pre-determined schedule (a plan that was prepared before the start of training sessions) and using the theoretical foundations and training prepared with the help of experts and professors in the field of autism treatment. Training sessions were performed by the researcher as follows:
Mindfulness treatment plan
The treatment plan for subjects exposed to group mindfulness training was presented in eight sessions in group form. Each session consisted of 90 minutes and included doing the exercises, talking about the exercises, and assessing the assignments of each session. For headlines, topics, exercises, and assignments of each session, the Practical Guide to Mindfulness-Based Cognitive Therapy [26] was used.
Summary of mindfulness-based training sessions:
Session 1: Communicating, defining and conceptualizing, and the necessity of using mindfulness training;
Session 2: Introduction to relaxation, relaxation training for 12 muscle groups, including the forearm, arm, back leg muscles, thighs, abdomen, chest, shoulders, neck, lips, eyes, jaws, and forehead;
Session 3: Relaxation training for 7 muscle groups, including arms and legs, legs and thighs, abdomen and chest, neck and shoulders, jaws, forehead, and lips, and relaxation homework;
Session 4: Breathing mindfulness training: A brief overview of the previous session, familiarity with how to breathe mindfully, teaching the technique of relaxed inhaling and exhaling without thinking about anything else, as well as teaching the technique of watching breathing and homework of mindful breathing before going to bed for 20 minutes;
Session 5: Teaching body scanning technique: Teaching the technique of paying attention to body movement when breathing, focusing on body parts and their movement and searching for physical senses (hearing, taste, etc.), homework of mindful eating (eating calmly and paying attention to the taste and appearance of food);
Session 6: Teaching mindfulness: teaching paying attention to mind, negative and positive thoughts, pleasant and unpleasant thoughts, allowing negative and positive thoughts to enter the mind and easily take them out of the mind without judgment and deep attention to them, and homework of writing negative and positive daily experiences without judging them;
Session 7: Full mindfulness: Repeating the training sessions 4, 5, and 6 each for 20 to 30 minutes;
Session 8: Reviewing and summarizing the previous sessions and performing the post-test.
In order to test the research hypotheses and analyze the data, descriptive statistics [chart, Mean±SD] and inferential statistics [multivariate analysis of covariance (MANCOVA)] were used by IBM SPSS Statistics for Windows, v. 24.0 (IBM Corp., Armonk, NY, USA).
Results
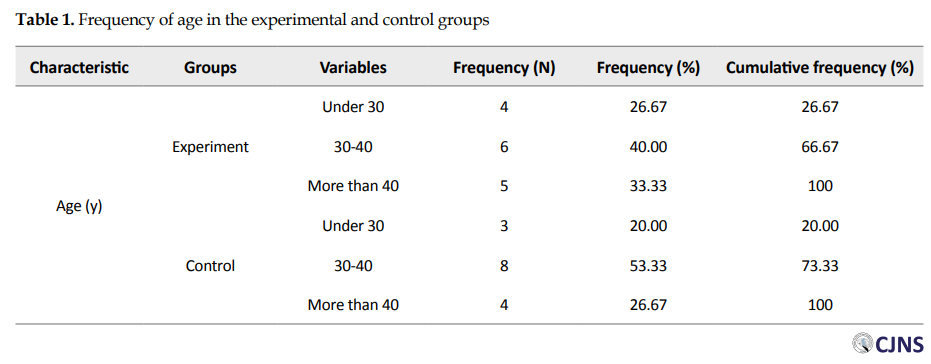
The Mean±SD age of mothers with autistic and healthy children was 38.25±2.21 and 40.32±2.01, respectively. The frequency of age in the two study groups can be seen in Table 1.
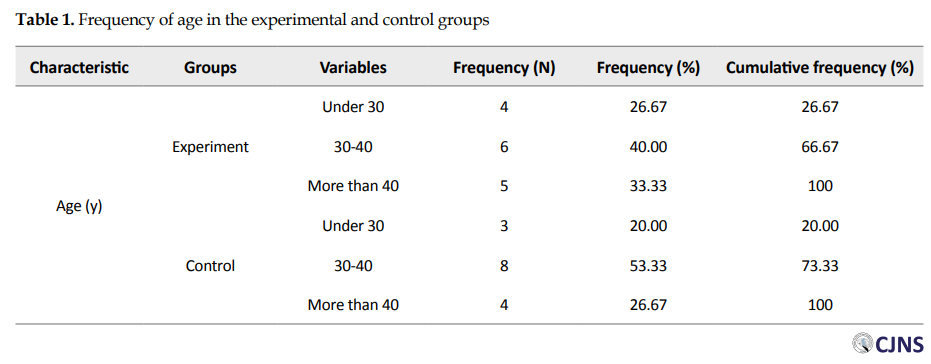
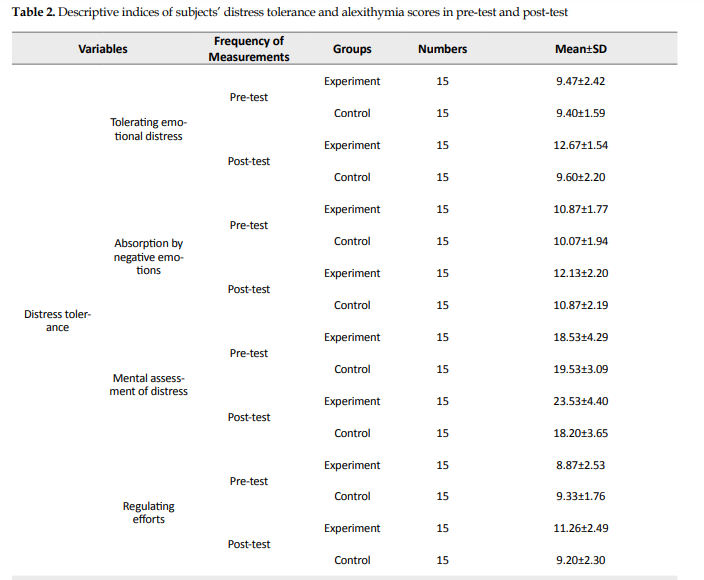
The mean scores of distress tolerance and alexithymia in pre-test and post-test in both experimental and control groups are shown in Table 2. MANCOVA was used to evaluate the effectiveness of mindfulness training on research variables.
_autism.PNG)
Given that the implementation of this analysis requires the existence of conditions or assumptions, at first, to check the normality of the data, the Kolmogorov-Smirnov test was used and due to the lack of significance of the variables, the normality of the data was confirmed. Also, the Box’s M test was used to examine the default homogeneity of the variance matrix, and the results of this test showed that the relevant condition was well observed. Therefore, in Table 2, the results of MANCOVA are presented to investigate the effect of independent variables on research variables.
Examination of outliers is also a critical part of the parametric analysis. Mahalanobis distance is one of the methods for examining outlier data. In determining the value of the critical Chi-square using the number of dependent variables as degrees of freedom (df) for identifying the outlier data, the results showed that the maximum value in the data file was 12.38, which was not outside the critical value range (20.52).
Checking the assumption of homogeneity of covariance matrix
In examining the assumption of homogeneity of the covariance matrix using the Box’s M test, the test results in the Table 1 showed that the significance level of the Box’s M test was greater than the alpha level of 0.05. Therefore, it can be said that this assumption was valid and was not violated (F(3, 141120)= 0.83, Box’s M=0.64, P>0.05).
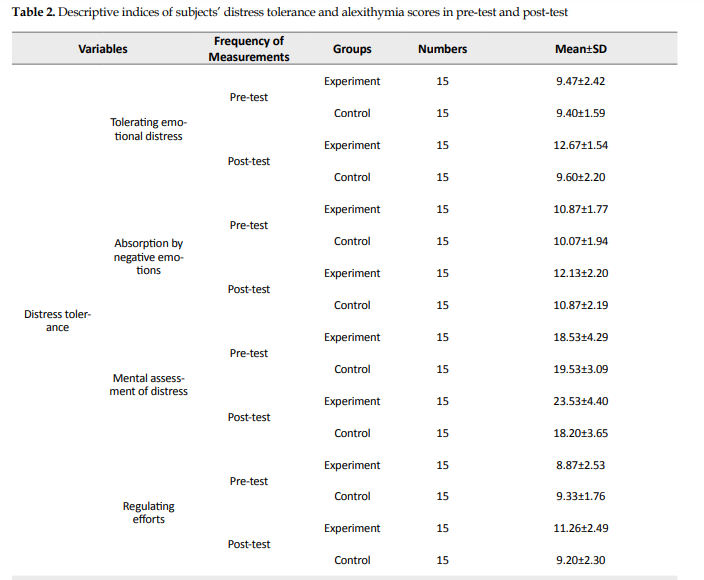
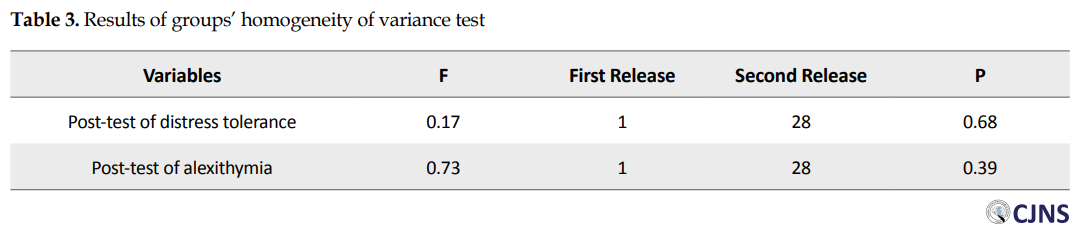
Investigation of the assumption of homogeneity of variance of groups
Findings from Levene’s test with degrees of freedom (df) of 1 and 38 in Table 3 showed that Levene’s test calculated for the post-test of distress tolerance was not statistically significant. Therefore, the assumption of homogeneity of variances was confirmed (P<0.05). Regarding the establishment of the underlying assumptions of the MANCOVA, the findings from the main purpose of the research are reported below.
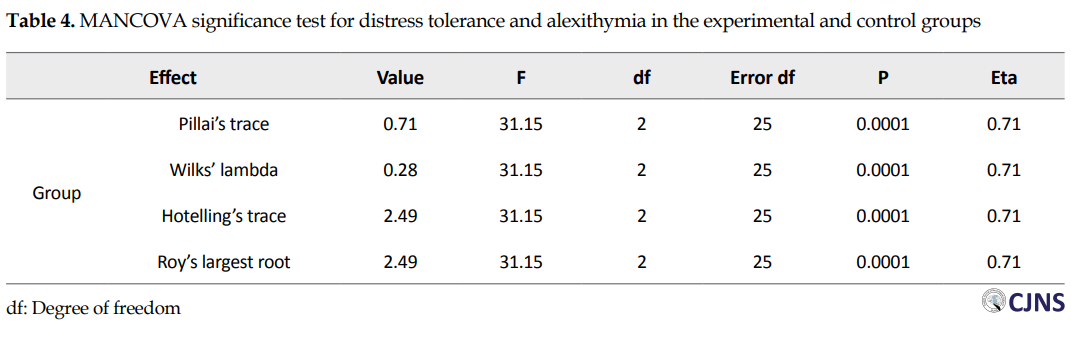
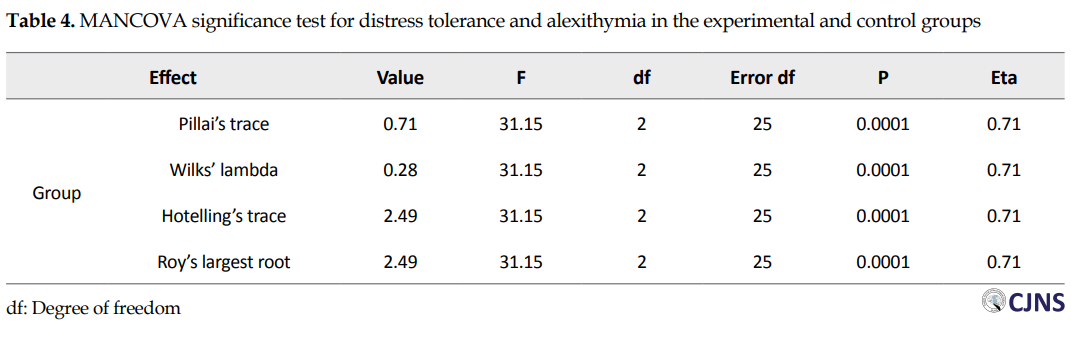
As can be seen in Table 4, the findings of the MANCOVA showed that there was a significant difference between the subjects in the experimental and control groups in the new combined variable resulting from distress tolerance and alexithymia (F(2,25)=31.15, P<0.001, Pillai’s trace= 0.71). In other words, according to this finding, it can be said that there was a significant difference between the subjects of the experimental and control groups in at least one of the variables in the post-test.
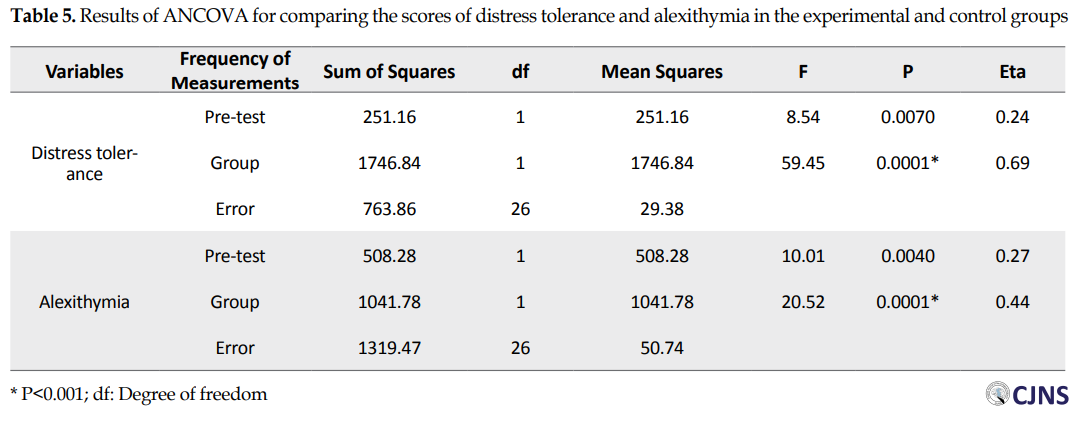
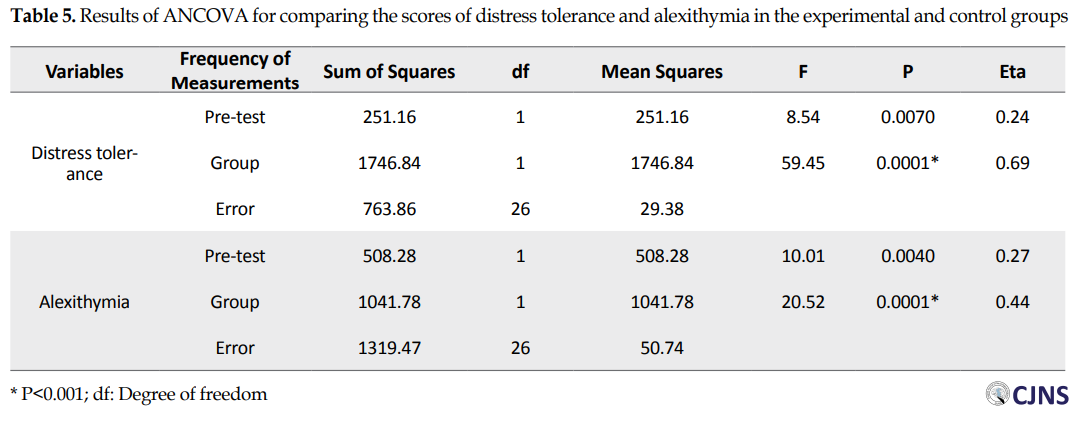
In order to investigate that the difference between the two groups in distress tolerance or alexithymia, the findings of One-way Analysis of Covariance (ANCOVA) are reported in Table 5. According to the findings of the ANCOVA in Table 5, a significant difference was observed between the post-test scores of distress tolerance (F(1,26)= 59.45, P<0.001, η2= 0.69) and alexithymia (F(1,26)= 20.52, P<0.001, η2= 0.44) of the subjects in the experimental and control groups. As can be seen in Table 2, the mean score of distress tolerance of the subjects in the experimental group in the post-test was higher than the mean scores of the subjects in the control group. Also, the mean score of alexithymia of the subjects in the experimental group in the post-test was lower than the mean scores of the subjects in the control group. Therefore, according to this finding, mindfulness training was effective on distress tolerance and alexithymia of mothers with autistic children.
Discussion
According to the results of the present study, mindfulness training was effective in increasing distress tolerance and reducing alexithymia. The findings of the present study are consistent with some studies [2, 3, 27-30] that have shown the effectiveness of mindfulness training on distress tolerance and alexithymia in relatives, including mothers of patients and children with different chronic diseases. Using mindfulness techniques and proverbs and metaphors helps mothers try to improve their lives in different ways instead of arguing without avoiding the upsetting feelings and without previous controls by acceptance and practice of being in the present time. Moreover, mindfulness can help mothers of autistic children who have a low level of distress tolerance recognize improper thoughts and evaluations and be aware of the present time without judgment [28]. In addition, mindfulness also helped them reinforce attitudes accompanying the presence of their mind, such as reassurance, patience, and acceptance, and change their relationship with the problem they are dealing with, because mindfulness involves a receptive awareness, without judgment of what is happening now. Mindful people perceive internal and external realities freely and without distortion and have a great ability to face a wide range of thoughts, emotions, and experiences (both pleasant and unpleasant) [29]. Therefore, mindfulness can cause women to accept the experience of the negative emotion without perception and judgment, take steps to absorb emotions with the acceptance they have acquired, and by avoiding or undermining the immediate experiences of their life, pay more attention to the present time. It leads to distress tolerance and improves emotional evaluation and regulation according to Simmons and Gauher (2005) [21]. According to Williams and Penman (2011) [31], when the mind is observed in practice, thoughts and emotions spontaneously disappear. Therefore, the mothers of children with autism who have low distress tolerance realize their personal values and abilities and improve their distress tolerance.
Mothers of children with autism find out that other mothers have similar problems during meetings and in interaction with the group, and in this regard, the relationship between members becomes wider. This causes emotional externalization and the exchange of emotions between group members leads to the discharge of negative emotions. Because distress tolerance depends on how you respond to negative emotions, mothers by doing homework in the next sessions, learn the strategies of increasing distress tolerance, such as emotion regulation and its assessment well. Therefore, training and its stages can reduce, regulate, and control negative emotions [30].
Emotion regulation also has a significant impact on the pathology of mental disorders when it occurs inconsistently. Emotional dysregulation has a great impact on psychiatric disorders Axis one and two. Emotion regulation can be an effective factor in mental health [32]. If we want to divide emotion regulation into regular steps, the first step is identification and awareness of emotions. To be able to regulate his emotions, the individual must first know them and be able to express them to himself and others. This relationship is so important so that a person who cannot recognize his emotions and describe them, has difficulty in regulating his emotions [33]. Inability to identify emotions not only affects the final process of dealing with emotions, i.e., emotion regulation but also affects the person’s positive emotions, as it reduces pleasure, effective communication with people, and life satisfaction, as well [13]. Moreover, the difficulty in identifying feelings operates as a measure of one’s capabilities in the eyes of the individual himself, and for the person who can properly recognize his emotions, this insight leads to a kind of self-esteem and satisfaction with this capability, which consequently is effective in his mental health [34]. This ambiguity in the emotions or the difficulty in identifying feelings can even appear as the effective factor in recognizing bodily sensations and emotions as well; for example, the individual cannot distinguish between gastrointestinal dysfunction and the emotions of stress and anxiety, which this factor has been confirmed in previous research [8].
Both difficulty in describing emotions and difficulty in regulating emotion are less associated with empathy. The person who has difficulty in recognizing emotions cannot properly empathize with others, and this relationship is unfortunately mutual and exacerbate the problems. Emotional dysregulation does not allow the person to be aware of the emotions, because before he can know the nature of his emotions, he confronts the emotion using an inconsistent strategy and removes the emotion in a very short time [35]. People with emotional dysregulation have also weaknesses in the ability of mindfulness. The ability of mindfulness can be seen as the power to observe emotions, describe them, and understand mental experiences in the present time; this ability is the opposite point of some mothers of children with autism. Weakness in this ability leads to the individual’s inability to be in the present time and pay attention to his/her current feelings, and the result is nothing except an inability to describe emotions [36]. Mindfulness techniques are effective in increasing muscle relaxation and stress reduction. These techniques help the person perceive the events as less distressing than they are. This type of treatment is about correcting, controlling, and processing thoughts. It seems that the main mechanism of mindfulness is self-control of attention because frequent focusing on a neutral stimulus, such as breathing creates a good attention environment. Also, mindfulness teaches the mothers of children with autism to understand the fact that although negative thoughts and emotions occur, they are not a stable part of one’s identity. Hence, in this technique, one learns to respond to events more flexibly [37].
Meditation and mindfulness exercises increase the ability of self-awareness and self-acceptance in patients. Mindfulness is not a method or technique, although many different methods and techniques have been used to do it. Mindfulness can be described as a way of “being” or a way of “knowing” that involves understanding personal feelings. The field of mindfulness experience is very broad and includes feelings, perceptions, impulses, emotions, thoughts, speech, action, and communication; therefore, it can help a person who is suffering from a lack of flexibility. A series of learned attention control skills in mindfulness meditation can be effective in accepting the problem, not judging and emotionally engaging in it, and can lead the mind to flexibility. Flexibility is avoiding rumination and previous solutions, and it is the route, which is the main goal of mindfulness. A person who deals with and learns the techniques of mindfulness learns the mental, emotional, and behavioral patterns to make choices by acceptance, non-judgment, and awareness of all aspects; all of which are the very definition of cognitive flexibility [38].
Mindfulness exercises that are combined with cognitive-behavioral therapy require special behavioral, cognitive, and metacognitive strategies, for focusing on the attention process, which in turn leads to prevention from the factors causing negative mood and thought and tendency to anxious responses and also, leads to the growth of new perspectives and formation of pleasant thoughts and emotions. This type of treatment includes various meditations, stretching yoga, body scanning practice, and several practices that show the relationship between mood, thoughts, emotions, and physical sensations [39]. In mindfulness training, mothers of autistic children learn how to communicate with their irrational thoughts and feelings about caring for their child and how to focus on changing the content of thoughts, change them, and see thoughts and feelings in a broader perspective [40].
One of the limitations of this study is that it was performed on mothers of autistic children. Also, this study was performed only on mothers. The use of self-reporting tools and the lack of a follow-up stage are other limitations of the present study that should be considered. It is suggested that to generalize the results, this research should be done in other cities and on the fathers of these children, as well. Also, for assurance of the results and stability of training, it is suggested that the follow-up stage be implemented. It is also recommended that autism treatment centers provide the conditions to implement these kinds of strategies to improve the quality of life of families who have autistic children.
Conclusion
Based on the results, the pervasive and severe disabilities of children with autism are a difficult experience for their parents and families and are often associated with a range of challenges for caregivers. The results of this study showed that mindfulness training increased distress tolerance and reduced alexithymia. By designing appropriate programs for improving their distress tolerance and reducing alexithymia in the priority of health care plans, it is possible to help mothers as well as other family members and caregivers of these children remarkably.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Islamic Azad University, Rasht Branch (No. IR.IAU.RASHT.REC.1400.003). All study procedures complied with the ethical guidelines of the Declaration of Helsinki 2013.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, and supervision: Leila Moghtader; Resources and funding acquisition: Sara Razzaghi; Writing the original draft: Leila Moghtader; Writing, reviewing, editing and investigation: both authors.
Conflict of interest
The authors declared no conflicts of interests.
Refrences:
Autism is a developmental disorder that occurs in the first three years of a child’s life and affects normal brain development and social interactions, as well as speech and communication skills. This disease, which is accompanied by some special behaviors, can be considered as a disorder with a spectrum that manifests itself in different forms and different intensities in affected children [1]. Autism is the most famous type of disorder that affects all four areas of development, including sensory, social, language, and cognitive areas [2]. In a study conducted on 8-year-old children, it was reported that, in general, one in every 150 children had some forms of the disorder [3].
It has been found that parents of children with developmental and psychiatric problems compared with parents of normal children experience more distress [4]. A lower level of psychological distress tolerance is one of the important psychological signs in families with autistic children, which are manifested in relation to the ability to analyze psychological situations. Distress may be the result of physical and cognitive processes, but its representation is in the form of a negative emotional state that is often manifested by a tendency to react to get rid of negative emotional experiences [5]. Mothers with low levels of distress tolerance evaluate emotional distress experienced as exhausting and unacceptable. As a result, they try to alleviate this negative emotional state but are often unable to focus their attention on something other than their distress [6].
On the other hand, alexithymia is one of the problems that mothers with autistic children always suffer from. The presence of a difficult child in the family affects the whole family system and the parents of these children feel themselves immersed in their child’s problems [7]. Research has shown that family relationships affect the other aspects of a teenager’s life, like emotional features. People with alexithymia magnify normal physical arousals and seek treatment for physical symptoms in therapeutic measures [8]. Alexithymia is a type of defect and failure that causes an inability in cognitive processing of emotional information and emotion regulation [9]. Alexithymia causes disability in the use of emotions as a sign of emotional problems, hinders abstract thinking and reduces dream recall, causes difficulty in distinguishing between emotional states and body feelings, creates poker face, lack of emotional effects on the face, and limited capacity for empathy and self-awareness [10]
The treatment widely used today for alexithymia, distress tolerance, and problems arising from them is mindfulness therapy [11, 12]. Mindfulness is unbiased, indescribable, and present-based awareness about an experience that a person at a certain moment concentrates on it. In addition, this concept includes acknowledging and accepting the mentioned experience [13]. Mindfulness techniques are effective in increasing muscle relaxation and reducing worry, stress, and anxiety. It seems that the main mechanism of self-controlled mindfulness is attention because repetitive concentration on a neutral stimulus, such as breathing creates a proper environment for attention [14]. Thao (2014) considered mindfulness-based training to be effective in improving and regulating emotion and increasing the quality of life [15-18]. Bergsma et al. (2012) in a study on the effectiveness of mindfulness exercises on children with Attention Deficit Hyperactivity Disorder (ADHD) and mindful parenting for their parents in 24 participating families, found that an 8-week mindfulness training had a significant effect on distress tolerance of mothers of children with autism [19].
Statistics show an increase in the prevalence of autism in Iran and it is estimated that one in every 158 people has this disorder and on the other hand, the birth of a child with autism is difficult for families (especially for mothers) [20]. In addition, a few studies have been done on the effect of mindfulness training on the characteristics of mothers with autistic children, and no research has examined the effect of mindfulness training on their distress tolerance and alexithymia, which is a research gap in this area.
The results of this research can be helpful in prevention and helping these mothers to reduce alexithymia in the face of difficulties ahead and increase distress tolerance. Moreover, the results of this study can be applied in family counseling centers and couple therapy. Therefore, it is necessary to consider this issue. The aim of this study was to evaluate the effect of mindfulness training on distress tolerance and alexithymia of mothers with autistic children. Accordingly, in this study, we intend to address this question: Does mindfulness training affect distress tolerance and alexithymia of mothers with autistic children?
Materials and Methods
This quasi-experimental research with the pretest-posttest design was performed with a control group. The research population consisted of all mothers of children with autism spectrum in Rasht City, Guilan, Iran, in 2019, who referred to the “Negah-e No” Counseling Center. In this study, 30 people were selected by convenience sampling method and were randomly assigned to the experimental and control groups (15 cases in each group).
For behavioral sciences studies, about 15 subjects for each variable are required. In experimental research, the Cohen method has recently been used to determine the adequacy of sample size in statistical analysis. In this study, considering the alpha level of 0.05 and the effect size equal to 0.50 with a test power of 0.76, 15 people were selected for each group.
The experimental group received eight 90-minute sessions of Mindfulness-Based Cognitive Therapy (MBCT). Inclusion and exclusion criteria were used to select the subjects. Inclusion criteria were mothers with autistic children, lack of history of receiving the medical intervention, and willingness to participate in this educational program. Exclusion criteria were the absence of more than two training sessions, the use of other training methods to treat autism, and the emergence of unpredictable problems for mothers leading to interruption or disruption of treatment sessions.
Study instruments
Distress Tolerance Scale (DTS)
This scale is a self-report index to assess distress tolerance developed by Simmons and Gauher (2005) [21]. Items of this scale evaluate distress tolerance based on individual abilities for tolerating emotional distress, mental evaluation of distress, the degree of attention to negative emotions in the case of occurrence, and regulating actions for distress relief. The scale has 15 items and four subscales, namely the emotional distress tolerance (questions 1, 3, 5), attraction by negative emotions (questions 2, 4, 14), the mental evaluation of distress (questions 6, 7, 9-12), and regulating the efforts to relieve distress (questions 8, 13, 15). Items of the scale were scored based on a five-point Likert scale, ranging from strongly disagree (score: 1) to strongly agree (score: 5). High scores on this scale indicated high distress tolerance. The content validity of the tool was confirmed by the experts and regarding the reliability of the questionnaire, Cronbach’s alpha of subscales of the questionnaire was calculated as 0.72, 0.82, 0.78, and 0.70, respectively, and for the entire scale, it was equal to 0.82. In Iran, Azizi et al. (2010) stated that the Cronbach’s alpha value of this questionnaire was equal to 0.67 and the retest validity of this questionnaire was 0.79 [22].
Persian version of Toronto Alexithymia Scale (FTAS-20)
This scale was designed by Bagby, Parker, and Taylor in 1994 and consists of three subscales of difficulty in identifying emotions, difficulty in describing emotions, and externally-oriented thinking [23]. These researchers calculated the reliability of the scale using Cronbach’s alpha coefficient (0.81) and test-retest reliability (0.77) as optimum [24]. In Iran, the 20-item alexithymia scale, in two separate studies, was translated and validated to be used on a group of drug abusers, as well as clinical and non-clinical groups [25]. The first subscale consists of 7 items (1, 3, 6, 7, 9, 13, and 14), which evaluates the subject’s ability in identifying his/her emotions and distinguishing between emotions and physical sensations. The second subscale has 5 items (2, 4, 11, 12, and 17), which assesses the subject’s ability in expressing emotions and whether he or she is able to express his/her feelings in words. The third subscale has 8 items (5, 8, 10, 15, 16, 18, 19, and 20) and examines the extent to which a person is introverted and deepened in his/her and others’ inner feelings.
The range of responses to each item varies from strongly disagree (score: 1) to strongly agree (score 5) based on a 5-point Likert scale. Items 4, 5, 10, 18, and 19 are scored in the reverse method, i.e., “strongly disagree” gets a score of 5, and “strongly agree” gets a score of 1. On this scale, higher scores indicate higher alexithymia. The content validity of the questionnaire was accepted by the experts. The concurrent validity of FTAS-20 was evaluated and confirmed in terms of the correlation between the subscales of this test and the emotional intelligence, psychological well-being, and psychological helplessness scales. Moreover, the Cronbach’s alpha coefficients of FATS-20 and its three subscales of difficulty in recognizing emotions, difficulty in describing emotions, and externally-oriented thinking were calculated at 0.85, 0.82, 0.75, and 0.72, respectively, indicating good internal consistency of the scale [25].
Subjects were first evaluated for diagnosis of the disorder. Then, detailed studies were performed and after an exclusive interview with the mothers and identifying the study subjects, the baseline of each subject was determined through clinical observations during three sessions. Training sessions were regulated according to a pre-determined schedule (a plan that was prepared before the start of training sessions) and using the theoretical foundations and training prepared with the help of experts and professors in the field of autism treatment. Training sessions were performed by the researcher as follows:
Mindfulness treatment plan
The treatment plan for subjects exposed to group mindfulness training was presented in eight sessions in group form. Each session consisted of 90 minutes and included doing the exercises, talking about the exercises, and assessing the assignments of each session. For headlines, topics, exercises, and assignments of each session, the Practical Guide to Mindfulness-Based Cognitive Therapy [26] was used.
Summary of mindfulness-based training sessions:
Session 1: Communicating, defining and conceptualizing, and the necessity of using mindfulness training;
Session 2: Introduction to relaxation, relaxation training for 12 muscle groups, including the forearm, arm, back leg muscles, thighs, abdomen, chest, shoulders, neck, lips, eyes, jaws, and forehead;
Session 3: Relaxation training for 7 muscle groups, including arms and legs, legs and thighs, abdomen and chest, neck and shoulders, jaws, forehead, and lips, and relaxation homework;
Session 4: Breathing mindfulness training: A brief overview of the previous session, familiarity with how to breathe mindfully, teaching the technique of relaxed inhaling and exhaling without thinking about anything else, as well as teaching the technique of watching breathing and homework of mindful breathing before going to bed for 20 minutes;
Session 5: Teaching body scanning technique: Teaching the technique of paying attention to body movement when breathing, focusing on body parts and their movement and searching for physical senses (hearing, taste, etc.), homework of mindful eating (eating calmly and paying attention to the taste and appearance of food);
Session 6: Teaching mindfulness: teaching paying attention to mind, negative and positive thoughts, pleasant and unpleasant thoughts, allowing negative and positive thoughts to enter the mind and easily take them out of the mind without judgment and deep attention to them, and homework of writing negative and positive daily experiences without judging them;
Session 7: Full mindfulness: Repeating the training sessions 4, 5, and 6 each for 20 to 30 minutes;
Session 8: Reviewing and summarizing the previous sessions and performing the post-test.
In order to test the research hypotheses and analyze the data, descriptive statistics [chart, Mean±SD] and inferential statistics [multivariate analysis of covariance (MANCOVA)] were used by IBM SPSS Statistics for Windows, v. 24.0 (IBM Corp., Armonk, NY, USA).
Results
The Mean±SD age of mothers with autistic and healthy children was 38.25±2.21 and 40.32±2.01, respectively. The frequency of age in the two study groups can be seen in Table 1.
The mean scores of distress tolerance and alexithymia in pre-test and post-test in both experimental and control groups are shown in Table 2. MANCOVA was used to evaluate the effectiveness of mindfulness training on research variables.
_autism.PNG)
Given that the implementation of this analysis requires the existence of conditions or assumptions, at first, to check the normality of the data, the Kolmogorov-Smirnov test was used and due to the lack of significance of the variables, the normality of the data was confirmed. Also, the Box’s M test was used to examine the default homogeneity of the variance matrix, and the results of this test showed that the relevant condition was well observed. Therefore, in Table 2, the results of MANCOVA are presented to investigate the effect of independent variables on research variables.
Examination of outliers is also a critical part of the parametric analysis. Mahalanobis distance is one of the methods for examining outlier data. In determining the value of the critical Chi-square using the number of dependent variables as degrees of freedom (df) for identifying the outlier data, the results showed that the maximum value in the data file was 12.38, which was not outside the critical value range (20.52).
Checking the assumption of homogeneity of covariance matrix
In examining the assumption of homogeneity of the covariance matrix using the Box’s M test, the test results in the Table 1 showed that the significance level of the Box’s M test was greater than the alpha level of 0.05. Therefore, it can be said that this assumption was valid and was not violated (F(3, 141120)= 0.83, Box’s M=0.64, P>0.05).
Investigation of the assumption of homogeneity of variance of groups
Findings from Levene’s test with degrees of freedom (df) of 1 and 38 in Table 3 showed that Levene’s test calculated for the post-test of distress tolerance was not statistically significant. Therefore, the assumption of homogeneity of variances was confirmed (P<0.05). Regarding the establishment of the underlying assumptions of the MANCOVA, the findings from the main purpose of the research are reported below.
As can be seen in Table 4, the findings of the MANCOVA showed that there was a significant difference between the subjects in the experimental and control groups in the new combined variable resulting from distress tolerance and alexithymia (F(2,25)=31.15, P<0.001, Pillai’s trace= 0.71). In other words, according to this finding, it can be said that there was a significant difference between the subjects of the experimental and control groups in at least one of the variables in the post-test.
In order to investigate that the difference between the two groups in distress tolerance or alexithymia, the findings of One-way Analysis of Covariance (ANCOVA) are reported in Table 5. According to the findings of the ANCOVA in Table 5, a significant difference was observed between the post-test scores of distress tolerance (F(1,26)= 59.45, P<0.001, η2= 0.69) and alexithymia (F(1,26)= 20.52, P<0.001, η2= 0.44) of the subjects in the experimental and control groups. As can be seen in Table 2, the mean score of distress tolerance of the subjects in the experimental group in the post-test was higher than the mean scores of the subjects in the control group. Also, the mean score of alexithymia of the subjects in the experimental group in the post-test was lower than the mean scores of the subjects in the control group. Therefore, according to this finding, mindfulness training was effective on distress tolerance and alexithymia of mothers with autistic children.
Discussion
According to the results of the present study, mindfulness training was effective in increasing distress tolerance and reducing alexithymia. The findings of the present study are consistent with some studies [2, 3, 27-30] that have shown the effectiveness of mindfulness training on distress tolerance and alexithymia in relatives, including mothers of patients and children with different chronic diseases. Using mindfulness techniques and proverbs and metaphors helps mothers try to improve their lives in different ways instead of arguing without avoiding the upsetting feelings and without previous controls by acceptance and practice of being in the present time. Moreover, mindfulness can help mothers of autistic children who have a low level of distress tolerance recognize improper thoughts and evaluations and be aware of the present time without judgment [28]. In addition, mindfulness also helped them reinforce attitudes accompanying the presence of their mind, such as reassurance, patience, and acceptance, and change their relationship with the problem they are dealing with, because mindfulness involves a receptive awareness, without judgment of what is happening now. Mindful people perceive internal and external realities freely and without distortion and have a great ability to face a wide range of thoughts, emotions, and experiences (both pleasant and unpleasant) [29]. Therefore, mindfulness can cause women to accept the experience of the negative emotion without perception and judgment, take steps to absorb emotions with the acceptance they have acquired, and by avoiding or undermining the immediate experiences of their life, pay more attention to the present time. It leads to distress tolerance and improves emotional evaluation and regulation according to Simmons and Gauher (2005) [21]. According to Williams and Penman (2011) [31], when the mind is observed in practice, thoughts and emotions spontaneously disappear. Therefore, the mothers of children with autism who have low distress tolerance realize their personal values and abilities and improve their distress tolerance.
Mothers of children with autism find out that other mothers have similar problems during meetings and in interaction with the group, and in this regard, the relationship between members becomes wider. This causes emotional externalization and the exchange of emotions between group members leads to the discharge of negative emotions. Because distress tolerance depends on how you respond to negative emotions, mothers by doing homework in the next sessions, learn the strategies of increasing distress tolerance, such as emotion regulation and its assessment well. Therefore, training and its stages can reduce, regulate, and control negative emotions [30].
Emotion regulation also has a significant impact on the pathology of mental disorders when it occurs inconsistently. Emotional dysregulation has a great impact on psychiatric disorders Axis one and two. Emotion regulation can be an effective factor in mental health [32]. If we want to divide emotion regulation into regular steps, the first step is identification and awareness of emotions. To be able to regulate his emotions, the individual must first know them and be able to express them to himself and others. This relationship is so important so that a person who cannot recognize his emotions and describe them, has difficulty in regulating his emotions [33]. Inability to identify emotions not only affects the final process of dealing with emotions, i.e., emotion regulation but also affects the person’s positive emotions, as it reduces pleasure, effective communication with people, and life satisfaction, as well [13]. Moreover, the difficulty in identifying feelings operates as a measure of one’s capabilities in the eyes of the individual himself, and for the person who can properly recognize his emotions, this insight leads to a kind of self-esteem and satisfaction with this capability, which consequently is effective in his mental health [34]. This ambiguity in the emotions or the difficulty in identifying feelings can even appear as the effective factor in recognizing bodily sensations and emotions as well; for example, the individual cannot distinguish between gastrointestinal dysfunction and the emotions of stress and anxiety, which this factor has been confirmed in previous research [8].
Both difficulty in describing emotions and difficulty in regulating emotion are less associated with empathy. The person who has difficulty in recognizing emotions cannot properly empathize with others, and this relationship is unfortunately mutual and exacerbate the problems. Emotional dysregulation does not allow the person to be aware of the emotions, because before he can know the nature of his emotions, he confronts the emotion using an inconsistent strategy and removes the emotion in a very short time [35]. People with emotional dysregulation have also weaknesses in the ability of mindfulness. The ability of mindfulness can be seen as the power to observe emotions, describe them, and understand mental experiences in the present time; this ability is the opposite point of some mothers of children with autism. Weakness in this ability leads to the individual’s inability to be in the present time and pay attention to his/her current feelings, and the result is nothing except an inability to describe emotions [36]. Mindfulness techniques are effective in increasing muscle relaxation and stress reduction. These techniques help the person perceive the events as less distressing than they are. This type of treatment is about correcting, controlling, and processing thoughts. It seems that the main mechanism of mindfulness is self-control of attention because frequent focusing on a neutral stimulus, such as breathing creates a good attention environment. Also, mindfulness teaches the mothers of children with autism to understand the fact that although negative thoughts and emotions occur, they are not a stable part of one’s identity. Hence, in this technique, one learns to respond to events more flexibly [37].
Meditation and mindfulness exercises increase the ability of self-awareness and self-acceptance in patients. Mindfulness is not a method or technique, although many different methods and techniques have been used to do it. Mindfulness can be described as a way of “being” or a way of “knowing” that involves understanding personal feelings. The field of mindfulness experience is very broad and includes feelings, perceptions, impulses, emotions, thoughts, speech, action, and communication; therefore, it can help a person who is suffering from a lack of flexibility. A series of learned attention control skills in mindfulness meditation can be effective in accepting the problem, not judging and emotionally engaging in it, and can lead the mind to flexibility. Flexibility is avoiding rumination and previous solutions, and it is the route, which is the main goal of mindfulness. A person who deals with and learns the techniques of mindfulness learns the mental, emotional, and behavioral patterns to make choices by acceptance, non-judgment, and awareness of all aspects; all of which are the very definition of cognitive flexibility [38].
Mindfulness exercises that are combined with cognitive-behavioral therapy require special behavioral, cognitive, and metacognitive strategies, for focusing on the attention process, which in turn leads to prevention from the factors causing negative mood and thought and tendency to anxious responses and also, leads to the growth of new perspectives and formation of pleasant thoughts and emotions. This type of treatment includes various meditations, stretching yoga, body scanning practice, and several practices that show the relationship between mood, thoughts, emotions, and physical sensations [39]. In mindfulness training, mothers of autistic children learn how to communicate with their irrational thoughts and feelings about caring for their child and how to focus on changing the content of thoughts, change them, and see thoughts and feelings in a broader perspective [40].
One of the limitations of this study is that it was performed on mothers of autistic children. Also, this study was performed only on mothers. The use of self-reporting tools and the lack of a follow-up stage are other limitations of the present study that should be considered. It is suggested that to generalize the results, this research should be done in other cities and on the fathers of these children, as well. Also, for assurance of the results and stability of training, it is suggested that the follow-up stage be implemented. It is also recommended that autism treatment centers provide the conditions to implement these kinds of strategies to improve the quality of life of families who have autistic children.
Conclusion
Based on the results, the pervasive and severe disabilities of children with autism are a difficult experience for their parents and families and are often associated with a range of challenges for caregivers. The results of this study showed that mindfulness training increased distress tolerance and reduced alexithymia. By designing appropriate programs for improving their distress tolerance and reducing alexithymia in the priority of health care plans, it is possible to help mothers as well as other family members and caregivers of these children remarkably.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Islamic Azad University, Rasht Branch (No. IR.IAU.RASHT.REC.1400.003). All study procedures complied with the ethical guidelines of the Declaration of Helsinki 2013.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, methodology, and supervision: Leila Moghtader; Resources and funding acquisition: Sara Razzaghi; Writing the original draft: Leila Moghtader; Writing, reviewing, editing and investigation: both authors.
Conflict of interest
The authors declared no conflicts of interests.
Refrences:
- Samadi SA, McConkey R. Screening for autism in Iranian preschoolers: Contrasting M-CHAT and a scale developed in Iran. J Autism Dev Disord. 2015; 45(9):2908-16. [DOI:10.1007/s10803-015-2454-1] [PMID]
- Soltanzadeh M. [Evaluation of the effectiveness of mindfulness-based techniques on reducing post-traumatic stress symptoms, increasing turbulence tolerance and reducing dysfunctional attitudes in mothers of children with cancer in Mashhad (Persian)]. [MA. Thesis]. Gorgan: University College Gorgan; 2019.
- Ahmadi A, Raeesi Z. [The effect of acceptance and commitment therapy on distress tolerance in mothers of children with autism (Persian)]. J Child Ment Health. 2018; 5(3):69-79. http://childmentalhealth.ir/article-1-349-fa.html
- Hauser-Cram P, Warfield ME, Shonkoff JP, Krauss MW, Sayer A, Upshur CC. Children with disabilities: A longitudinal study of child development and parent well-being. Monogr Soc Res Child Dev. 2001; 66(3):i-viii, 1-114; discussion 115-26. [PMID]
- Banducci AN, Bujarski SJ, Bonn-Miller MO, Patel A, Connolly KM. The impact of intolerance of emotional distress and uncertainty on veterans with co-occurring PTSD and substance use disorders. J Anxiety Disord. 41:73-81. [DOI:10.1016/j.janxdis.2016.03.003] [PMID]
- Kelishadi F, Yazdkhasti F. [Impact of perception of parental rejection-acceptance and control on moral intelligence and distress tolerance (Persian)]. Culture Strategy. 2016; 9(33):155-69. http://www.jsfc.ir/article_15196_en.html
- Khanna R, Jariwala K, Bentley JP. Psychometric properties of the euroqol five dimensional questionnaire (EQ-5D) in caregivers of autistic children. Qual Life Res. 2013; 22(10):2909-20. [DOI:10.1007/s11136-013-0423-8] [PMID]
- Picardi A, Toni A, Caroppo E. Stability of alexithymia and its relationships with the ‘big five’factors, temperament, character, and attachment style. Psychother Psychosom. 2005; 74(6):371-8. [DOI:10.1159/000087785] [PMID]
- Stasiewicz PR, Bradizza CM, Gudleski GD, Coffey SF, Schlauch RC, Bailey ST, et al. The relationship of alexithymia to emotional dysregulation within an alcohol dependent treatment sample. Addict Behav. 2012; 37(4):469-76. [DOI:10.1016/j.addbeh.2011.12.011] [PMID] [PMCID]
- Mottaghi S, Ramak, N. [Comparison of action flexibility, quality of life and mood apnea in mothers of autistic children and mothers of children with Down syndrome (Persian)]. First International Congress and Fifth National Congress of Preschool Education and Health. 18 June 2018; Tehran, Iran. https://civilica.com/doc/786432/
- Forkmann T, Brakemeier EL, Teismann T, Schramm E, Michalak J. The effects of mindfulness‐based cognitive therapy and cognitive behavioral analysis system of psychotherapy added to treatment as usual on suicidal ideation in chronic depression: Results of a randomized-clinical trial. J Affect Disord. 2016; 200:51-7. [DOI:10.1016/j.jad.2016.01.047] [PMID]
- Huijbers MJ, Spinhoven P, van Schaik DJ, Nolen WA, Speckens AE. Patients with a preference for medication do equally well in mindfulness-based cognitive therapy for recurrent depression as those preferring mindfulness. J Affect Disord. 2016; 195:32-9. [DOI:10.1016/j.jad.2016.01.041] [PMID]
- Bylsma LM, Rottenberg J. Uncovering the dynamics of emotion regulation and dysfunction in daily life with ecological momentary assessment. In: Nykliček I, Vingerhoets A, Zeelenberg M, editors. Emotion regulation and well-being. New York: NY Springer; 2011. [DOI:10.1007/978-1-4419-6953-8_14]
- Semple RJ, Reid EF, Miller L. Treating anxiety with mindfulness: An open trial of mindfulness training for anxious children. J Cogn Psychother. 2005; 19(4):379-92. [DOI:10.1891/jcop.2005.19.4.379]
- Le TN. Mindfulness-based adventure camp for military youth. J Ext. 2014; 52(2). https://archives.joe.org/joe/2014april/a5.php
- Shakernejad S, Alilou M. Effectiveness of mindfulness in decreasing the anxiety and depression of patients suffering from irritable bowel syndrome. Caspian J Neurol Sci. 2016; 2(4):32-40 [DOI:10.18869/acadpub.cjns.2.7.32]
- Abdolghaderi M, Kafi S, Saberi A, Ariaporan S. Effectiveness of mindfulness-based cognitive therapy on hope and pain beliefs of patients with chronic low back pain. Caspian J Neurol Sci. 2018; 4(1):18-23 [DOI:10.29252/nirp.cjns.4.12.18]
- Shayegh Borojeni B, Manshaee G, Sajjadian I. The effectiveness of adolescent-centered mindfulness training and cognitive behavioral therapy on depression and suicidal ideation in adolescent girls with bipolar II disorder. Caspian J Neurol Sci. 2019; 5(4):175-84. [DOI:10.32598/CJNS.5.19.175]
- Van de Weijer-Bergsma E, Formsma AR, de Bruin EI, Bögels SM. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J Child Fam Stud. 2012; 21(5):775-87. [DOI:10.1007/s10826-011-9531-7] [PMID] [PMCID]
- Ajirak Z, Zavvar M, Shahsavar M. Effects of positive couple therapy on hope of mothers of children with special needs. Eur J Psychol Educ Stud. 2015; 2(3):95-8. [DOI:10.4103/2395-2555.190479]
- Simons JS, Gaher RM. The distress tolerance scale: Development and validation of a self-report measure. Motiv Emot. 2005; 29(2):83-102. [DOI:10.1007/s11031-005-7955-3]
- Azizi A, Borjali A, Golzari M. The effectiveness of emotion regulation training and cognitive therapy on the emotional and addictional problems of substance abusers. Iran J Psychiatry. 2010; 5(2):60-5. [PMCID]
- Bagby RM, Taylor GJ, Parker JD. The twenty-item Toronto Alexithymia Scale-II. Convergent, discriminant, and concurrent validity. J Psychosom Res 1994; 38(1):33-40. [DOI:10.1016/0022-3999(94)90006-X]
- Palmer BR, Gignac G, Manocha R, Stough C. A psychometric evaluation of the Mayer-Salovey-Caruso emotional intelligence test version 2.0. Intelligence. 2005; 33(3):285-305. [DOI:10.1016/j.intell.2004.11.003]
- Besharat MA. Reliability and factorial validity of a Farsi version of the 20-item Toronto Alexithymia Scale with a sample of Iranian students. Psychol Rep. 2007; 101(1):209- 20. [DOI:10.2466/PR0.101.5.209-220] [PMID]
- Mansouri M, Nazemipour H. [Effectiveness of parental training with Adlerian psychological well-being and parenting stress in mothers of children with Avtbysm (Persian)]. First National Congress of community empowerment in the social sciences Psychology and Educational Sciences. 04 March 2015; Tehran, Iran. https://civilica.com/doc/474993/
- Ghassem Boroujerdi F, Safa M, Karamlou S, Masjedi MR. [The effectiveness of mindfulness-based cognitive therapy on distress tolerance and dysfunctional attitudes in families of patients with chronic lung diseases (Persian)]. J Res Psychol Health. 2014; 8(4):6-7. https://rph.khu.ac.ir/article-1-2384-fa.html
- Sabouri F. [The effectiveness of mindfulness training on tolerating confusion and dysfunctional communication beliefs of mothers of children with the syndrome (Persian)]. [MA thesis]. Marvdasht: Islamic Azad University of Marvdasht; 2016.
- Ghadernezhad L. [The effectiveness of mindfulness-based cognitive therapy on psychological well-being of mothers with children with autism spectrum disorder (Persian)]. Paper presented at 5th National Conference on Recent Innovations in Psychology, Applications and Empowerment with a focus on psychotherapy. 20 June 2019; Tehran, Iran. https://civilica.com/doc/922513/
- Williams M, Penman D. Mindfulness: A practical guide to finding peace in a frantic world. France: Hachette UK; 2011. https://www.hachette.com.au/mark-williams-danny-penman/mindfulness-a-practical-guide-to-finding-peace-in-a-frantic-world
- Foody C, James JE, Leader G. Parenting stress, salivary biomarkers, and ambulatory blood pressure: A comparison between mothers and fathers of children with autism spectrum disorders. J Autism Dev Disord. 2015; 45(4):1084-95. [DOI:10.1007/s10803-014-2263-y] [PMID]
- Roche LT, Barrachina MT, Fernández II. Effect of ‘Exercise without Movement’yoga method on mindfulness, anxiety and depression. Complement Ther Clin Pract. 2016; 25:136-41. [DOI:10.1016/j.ctcp.2016.09.008] [PMID]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004; 26(1):41-54. [DOI:10.1023/B:JOBA.0000007455.08539.94]
- Lundh LG, Broman JE. Alexithymia and insomnia. Pers Individ Differ. 40(8):1615-24. [DOI:10.1016/j.paid.2005.11.026]
- Jonason PK, Krause L. The emotional deficits associated with the Dark Triad traits: Cognitive empathy, affective empathy, and alexithymia. Pers Individ Differ. 2013; 55(5):532-7. [DOI:10.1016/j.paid.2013.04.027]
- Connelly M, Denney DR. Regulation of emotions during experimental stress in alexithymia. J Psychosom Res. 2007; 62(6):649-56. [DOI:10.1016/j.jpsychores.2006.12.008] [PMID]
- Rashidi Shiraz A. [Principles of mindfulness: Twenty-first century meditation (Persian)]. Tehran: Savalan Publications, 2019. http://opac.nlai.ir/opac-prod/search/briefListSearch.do?command=FULL_VIEW&id=3376596&pageStatus
- Curtiss J, Klemanski DH. Teasing apart low mindfulness: Differentiating deficits in mindfulness and in psychological flexibility in predicting symptoms of generalized anxiety disorder and depression. J Affect Disord. 2014; 166:41-7. [DOI:10.1016/j.jad.2014.04.062] [PMID]
- Kangasniemi A, Lappalainen R, Kankaanpää A, et al. Mindfulness skills, psychological flexibility, and psychological symptoms among physically less active and active adults. Ment Health Phys Act. 2014; 7(3):121-7. [DOI:10.1016/j.mhpa.2014.06.005]
- Lee JK, Orsillo SM. Investigating cognitive flexibility as a potential mechanism of mindfulness in generalized anxiety disorder. J Behav Ther Exp Psychiatry. 2014; 45(1):208-16. [DOI:10.1016/j.jbtep.2013.10.008] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2021/03/10 | Accepted: 2021/08/12 | Published: 2021/10/1
Received: 2021/03/10 | Accepted: 2021/08/12 | Published: 2021/10/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |