Fri, Apr 26, 2024
Volume 7, Issue 2 (Spring 2021)
Caspian J Neurol Sci 2021, 7(2): 104-117 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rafiee S H, Taklavi S, Abolghasemi A, Hatamian H. Comparing the Effectiveness of Reality Therapy and Positive Psychotherapy on Sleep Quality in Patients With Multiple Sclerosis. Caspian J Neurol Sci 2021; 7 (2) :104-117
URL: http://cjns.gums.ac.ir/article-1-419-en.html
URL: http://cjns.gums.ac.ir/article-1-419-en.html
1- Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil, Iran.
2- Department of Psychology, University of Guilan, Rasht, Iran.
3- Department of Neurology, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Psychology, University of Guilan, Rasht, Iran.
3- Department of Neurology, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 1903 kb]
(691 Downloads)
| Abstract (HTML) (1568 Views)
Full-Text: (850 Views)
Introduction
ultiple Sclerosis (MS) is one of the most common neurological diseases [1], causing inflammation and demyelination of the central nervous system. Damage to the myelin sheath in the nerve cell creates specific symptoms of the disease [2]. MS is one of the most significant life-changing diseases, as it usually affects the best part of a person’s life and gradually progresses to disability and has no definitive cure. As a result, this disease has damaged the productive forces of society [3]. The prevalence of this disease is rapidly increasing. Atlas of MS (2016) has estimated its prevalence worldwide to be about two and a half million people [4]. In Iran, 5.78 out of every 100 people have been reported with MS [5].
MS causes many physical problems for people with the disease, including balance disorder, one of the most debilitating symptoms of this disease, muscle cramps, extreme fatigue, bladder dysfunction, disability, sexual dysfunction, etc. These complications always reduce the ability to perform daily activities in MS patients [6]. In addition to physical problems, these patients have always reported many sleep problems [7, 8].
In general, almost any physical illness that produces significant pain or discomfort can negatively affect the quantity and quality of sleep [9]. Sleep is a dynamic and highly organized biological process that is an essential part of life, and the quantity of sleep is known to be related to the quality of social interaction. The importance of sleep in health and disease has been considered since Hippocrates, and disturbed sleep is considered a significant cause of suffering and illness of human beings at any age [10]. During sleep, the body restores its energy, and nerve cells are regenerated. Sleep protects the body against extreme fatigue. However, sleep is not just a neuro-physiological component. Psychologically, sleep, through its restorative effect, treats stressed and nervous people. When the sleep nuclei in the brain are damaged, the Circadian Rhythm (CR) of sleep is disrupted, and sleep quality is impaired [11]. Inadequate sleep quality can cause psychological problems and consequently the deterioration of the patients’ condition [12]. Because of sleep quality problems in patients with MS, psychological interventions can be an essential and effective step in reducing their psychological problems and improving their sleep quality. In particular, evidence suggests that traditional cognitive-behavioral therapy does not improve cognitive function in these patients [13].
The development of psychological therapies over the past few decades has led to the development of new approaches to maladaptive cognitions that target broad, contextual goals. Treatments of insomnia have evolved similarly, and several therapies, including reality therapy, have begun to gather evidence as effective therapies for sleep-related processes over the past few decades. Reality therapy is a method of psychotherapy that is based on the Choice Theory and was founded by Glasser. This treatment is based on the principle that people choose their behaviors and are responsible for their lives and what they do, feel, and think [14]. This approach helps people control their behavior and make better choices and emphasizes that having a successful identity is achieved through successful work and the power of choice is an essential factor in their mental health [15, 16]. In other words, its primary goal is to help clients learn better ways to satisfy all their psychological needs [17]. Researchers have examined and confirmed the effect of reality therapy on a wide range of psychological symptoms [18, 19, 20].
Although sleep is a powerful and highly regulated biological stimulus, the ability to fall asleep at any time and maintain sleep without waking up is very fragile and is affected by several factors. Identification of these factors is the key to insomnia treatment [21]. Positive psychological structures (e.g., optimism and hope) have been associated with better sleep quality in previous work [22]. However, such studies have not examined the effect of a wide range of positive psychological structures or the effectiveness of positive psychotherapy on sleep-related health behaviors. Positive psychotherapy originates from the positive psychology approach and is a multi-component model that enhances therapeutic change by creating interaction, pleasure, and meaning [23]. This approach, which is a combination of Beck’s cognitive approach in clinical practice, the Mihaly cognitive-attention syndrome, and Seligman’s positive psychology, teaches clients to be more optimistic. The main goal of this therapy is to extend the psychologist’s focus beyond the disease and its direct relief. The exercises used and suggested in this therapy directly target patients’ interpersonal relationships. Also, in some therapy sessions, patients are trained to use their abilities and strengths, which also helps them reduce their psychological problems by strengthening their self-confidence [24]. In addition, Lyubomirsky and Laius believed that positive interventions reduce depression and increase happiness and psychological wellbeing by increasing positive emotions, positive thoughts, and satisfying basic needs such as autonomy, love, belonging, and communication [25]. Cucarella and Perza showed that positivist psychology was effective in reducing stress in female patients [26]. In addition, other separate studies have shown that positive psychotherapy reduces patients’ emotional and mental memory problems [27, 28].
Glasser’s view of psychopathology in the reality therapy approach does not address the patient or a defect in behavior. In this view, to change the clients’ mental state, the choice of useful and effective behavior is considered instead of ineffective behavior, and by increasing the power of choice and behavior based on reality, the patient’s mental function is improved. On the other hand, positive psychotherapy is a different approach from other therapy models because it focuses on positive emotions and relationships, and wellbeing. According to what was said, the goals and techniques in the above two therapies are different. In reality therapy, selection, control, and internal factors are considered, and in positive psychotherapy, capabilities are. So it seems that comparing the effectiveness of these two therapeutic approaches should help select a more appropriate approach to improve sleep quality in patients with MS. Also, the researcher’s investigation on internal and external studies in the field of reality therapy and positive psychotherapy indicates that the effectiveness of these two treatment models has been studied on populations with various problems, and useful results have been obtained. However, the effectiveness of these two approaches on sleep quality in patients with MS has not been studied so far. Therefore, the present study aimed to compare the effectiveness of reality therapy and positive psychotherapy on sleep quality in women with MS.
Materials and Methods
This study was quasi-experimental research with a pre-test, post-test design and a control group. The study population included all female patients with MS referred to Guilan MS Association, Iran, in the summer and fall of 2019 (1197 people). Of them, 45 patients from the mentioned community were selected by purposive sampling method (taking into account the inclusion criteria) and randomly placed into three groups: reality therapy training (15 people), positive psychotherapy (15 people), and control group (15 people). This number was selected based on the sample size proposed for the experimental and quasi-experimental studies (at least 15 people for each group) [29]. The inclusion criteria include completing the consent form to participate in the training program, not suffering from acute psychological problems by the psychiatrist’s discretion, and the literacy level of at least third grade of guidance school to answer the questionnaires. Considering that the condition for membership in the MS association was the definitive confirmation of the disease by trusted experts, the criterion of the disease was membership in this association. The exclusion criteria included participation in other treatment programs, unwillingness to participate in the program, and two consecutive absences from intervention sessions.
After selecting the statistical subjects, both experimental groups received eight 90-minute sessions of intervention treatment, and the control group remained without any intervention. Because of the follow-up and encouragement of researchers, there was no subject withdrawal, and if any of the subjects missed only one training session, the researcher held extra programs to her catching up with the group.
Finally, after 4 weeks of holding training sessions, a post-test was taken from all three groups, and the data were analyzed with descriptive statistics (including mean and standard deviation) and Multivariate Analysis of Covariance (MANCOVA) in SPSS v. 22.
Research tools
Pittsburgh Sleep Quality Index (PSQI)
Pittsburgh Sleep Quality Index (PSQI) was developed by Buysse et al. to measure sleep quality and help diagnose the people who have good or bad sleep [30]. It consists of 18 items that determine people’s sleep quality by evaluating 7 characteristics during the last month. These characteristics include sleep quality in terms of the individual, the time it takes for the person to fall asleep, the duration of sleep, sleep efficiency, problems during sleep time, use of sleeping medication, and dysfunction of daily performance. Each of the 7 subscales in this questionnaire has a score of 0 to 3, where high scores indicate poor sleep. A total score greater than 5 indicates that the participant has poor sleep quality and severe problems in at least two areas. The reliability of this scale was calculated as 0.83, and its validity by a sensitivity of 89.6% and a specificity of 86.5% is at an appropriate level [30]. In Iran, the validity of this questionnaire for the Iranian population has been confirmed at the Tehran Psychiatric Institute. Also, the reliability coefficient of the questionnaire through Cronbach alpha was calculated as 0.81 [31]. Heidari et al. also reported validity of 0.86 and a reliability of 0.89 for this questionnaire [32].
Protocol of group reality therapy sessions
In this study, the reality therapy intervention was based on Glasser’s reality therapy training package [33], held during eight 90-minute sessions, one session per week for the study participants (experimental group). Details and summaries of the sessions are provided in Table 1.
.jpg)
Protocol of positive psychotherapy training sessions
In this study, a positive psychotherapy intervention was based on the reality therapy training package [34], was held during eight 90-minute sessions and one weekly session for study participants (experimental group 1). Details of the sessions are provided in Table 2.
.jpg)
Results
In the present study, 45 female patients with MS were studied in 3 groups: reality therapy training (15 patients), positive psychotherapy (15 patients), and a control group (15 patients). Demographic characteristics is shown in Table 3.
.jpg)
According to Table 4, the average quality of sleep and its components in the control group in the pre-test and post-test phase do not show any change.
.jpg)
But in the experimental group, it decreased in the post-test stage compared to the pre-test stage. The results of the Shapiro-Wilk test indicate that the distribution of data is normal in sleep quality variables and its components (P>0.05), and the premise of the normal distribution of data for covariance analysis is thus established. Also, the assumed results of homogeneity of covariance matrices of variance (M-Box test) indicate no difference between the variances (M-Box=62.690, F=1.731, P=0.079). Default homogeneity of regression line slope and the existence of a linear relationship between the covariate and the dependent variable for sleep quality and its dimensions was also investigated, which showed that these two assumptions were established. Following are the results related to the validity indicators of multivariate analysis of covariance (Table 5).
.jpg)
The results of validity indicators of multivariate analysis of covariance (Table 5) showed that the effect of group on the composition of the studied components is significant (P<0.05). Accordingly, the square of Eta shows that the difference between the two groups is generally significant with respect to the components of the dependent variable. To determine the more accurate effects of treatments on sleep quality subscales in women with MS, the results of adjusted means and Bonferroni post hoc test have been reported (Table 6).
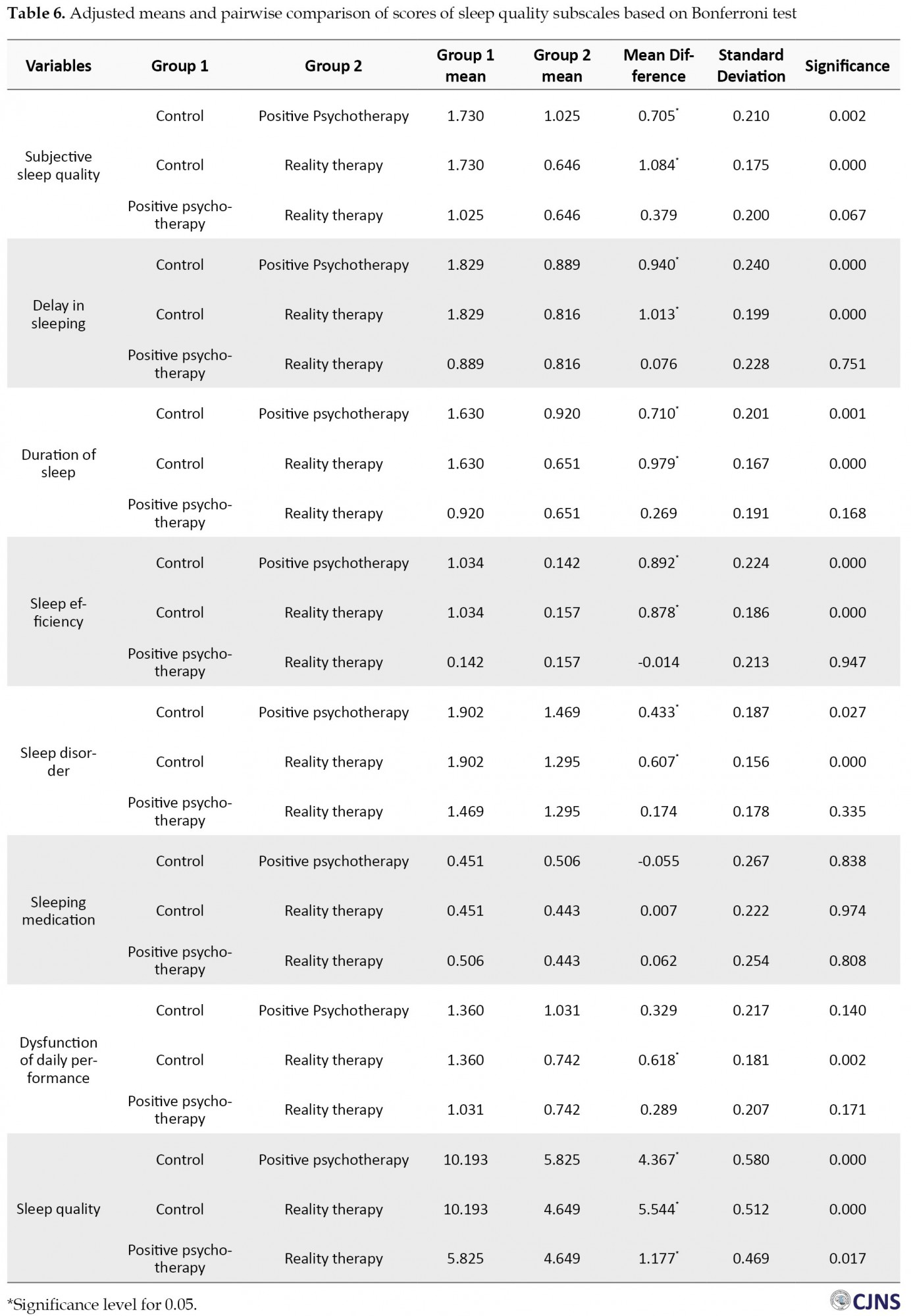
According to Table 6, the sleep quality in the reality therapy group showed a more appropriate and significant improvement compared to the positive treatment (P<0.05). But in all sleep quality subscales, there is no significant difference between reality therapy and positive psychotherapy (P>0.05).
Discussion
This study aimed to compare the effectiveness of reality therapy and positive psychotherapy on sleep quality in women with MS. The results showed that reality therapy significantly affected sleep quality and its components in women with MS. The result was consistent with the findings of Lee et al., [35] Willie et al. [36]. In explaining this finding, based on the opinion of researchers, the emotional reaction to illness and physical pain affect the quality and quantity of sleep [37]. Therefore, when MS patients underwent this intervention, they could improve their sleep quality by controlling emotional reactions such as anxiety, stress, and depression. In particular, there is a significant correlation between sleep quality and reduced emotional disturbance [38]. It is also noteworthy that sleep is a bio-cognitive process, and reality therapy intervention based on selection theory refers to explaining how and why the brain works. Therefore, from the point of view of this theory, providing education based on reality therapy paves the way for improving the biological process. According to the theory of neuroplasticity, neural pathways and synapses can be altered by changes in behavior, environmental processes, and neural processes. The reorganization of the views of different parts of the body in the cerebral cortex constantly occurs in response to activities, behaviors, and skill learning, so neural processes have flexibility. Reality therapy can make a difference in people’s biological processes by changing their thoughts, feelings, and actions [39].
Reality therapy has techniques to help people change their inefficient behaviors to efficient ones, destructive styles into wise alternatives, and above all, their unhealthy lifestyle to a healthy one [38]. In choice theory, behavior consists of four components: thinking, action, feeling, and physiology. Glasser suggested that we have considerable control or choice over the first two: thinking and acting. However, we have little ability to directly select the components of emotion and physiology because they are deeply unconscious. These four components are closely intertwined, and the choices we make in our thinking and acting indirectly and significantly affect our feelings and physiology [40]. Sleep involves a sequence of neurophysiological changes in the brain. Proper sleep involves a dynamic interaction between voluntary decisions and involuntary biological activity. Turning off the lights, reducing the noise, and lying down are voluntary behavior, but the result is an involuntary increase in melatonin and a series of changes in brain activity patterns during the night. Sleeping ultimately depends on cooperation between behavior and biology, and the defect in any of them causes sleep disorders [41]. Therefore, reality therapy can make significant changes in the patient’s feelings and physiology and provide a basis for improving the quality of sleep in MS patients through cognitive evaluation and training to stop rumination, change attention and provide a distraction. It changes the individual’s knowledge about the disease and sleep quality problems by manipulating the patient’s thinking and action [42].
Consistent with the above argument in the reality therapy intervention, the therapist asks the client: what options do you have to deal with your problem? The client should use the brainstorming method. The therapist challenges the patient’s irrational thoughts by offering several options as well as questions. In other words, the patient’s enjoyment and satisfaction with life are enhanced by creating a positive view of the disease, changing negative perceptions, and emphasizing the patient’s different roles in life (for example, the patient is told that you aren’t a prisoner of your MS and sleep problems, starting now you can have a better life by choosing a healthy lifestyle and changing your thoughts and attitudes) [43]. Therefore, based on Glasser’s point of view, people are in any given situation because of their individual choices and because they have not been able to satisfy their basic needs in a right and reasonable way. Humans can create a better situation by choosing an effective and appropriate way to meet their needs and positively affect their physiological processes, such as sleep quality [44].
The other part of the results showed that positive psychotherapy significantly affected sleep quality and its components in women with MS. The results obtained were consistent with the findings of Kim et al., [45] Pahlavan et al., [46] and Saghebi Saeedi et al. [47]. In this regard, Kim et al. suggested in a study that positive psychology has a significant mediating effect on the relationship between sleep disorders and depressive symptoms and can reduce the symptoms of sleep disorders and depression caused by sleep disorders [45]. The present study findings are consistent with McEwen’s theory of allostatic load. This theory interprets the individual’s attempt to adapt to the demands of life as a cumulative physiological load imposed on the body. Accordingly, patients with MS who experience insomnia may experience increased stress and inability to participate in enjoyable activities, making them more vulnerable to sleep disorders [45]. Previous research findings have confirmed this finding. In a large study, Hamilton et al. reported that participants with low levels of psychological wellbeing showed more sleep disorders independent of age, gender, physical symptoms, and cognitive disorders [48]. Therefore, experiencing high levels of chronic stress in patients with MS leads to activation of the Hypothalamic-Pituitary-Adrenal (HPA) axis, an essential neuroendocrine mediator of the stress response. HPA axis hyperactivity, which leads to increased cortisol levels, may stimulate poor sleep in these patients and is associated with an increased risk of insomnia.
Conversely, the symptoms of insomnia in patients may also increase cortisol levels, causing a vicious cycle [49]. Therefore, it seems that the psychological resources and positive cognitions generated by positive psychotherapy create a strong protective function in response to stress and improve the sleep quality of patients by modulating HPA-based activity and reducing overall cortisol levels. Previous studies have also supported this conceptualization, and research has shown that people with more psychological resources do not show an HPA response to crucial negative life events and daily stress [50, 51]. The broaden-and-build theory suggests that positive emotions associated with positive cognitions enhance patients’ physical, intellectual, and social resources by expanding the action-thought repertoire [52]. Examples of these resources include the quality of social relationships and resilience, both of which have been suggested to improve sleep quality [53, 54]. In this regard, Solberg and Segerstrom argue that people with positive cognitions are often more flexible in using coping strategies and are more successful in dealing with controlled and uncontrollable stressors. Therefore, the positive cognition developed in a person following positive psychotherapy is likely to affect sleep quality through a combination of psychological, behavioral, and biological pathways [55].
In explaining this finding, we can refer to the techniques and exercises used in positivity intervention. Positive gratitude exercises seem to have been effective in this regard [56]. The development and construction of positive emotion models and cognitive sleep models are especially important for study [57]. The content of pre-sleep cognitions is also essential. Cognitive sleep patterns reflect the biases of people who have lower sleep quality in sensitive periods before going to sleep and cannot interpret this low quality (such as focusing on negative events or the idea that I cannot sleep well). This condition happens because schemes and hypotheses activate the information processing system. A clear explanation for this is that rumination about sleep problems can intensify sleep problems, which is, in fact, one of the best predictors of delayed sleep [57]. Gratitude exercises may encourage individuals to shift their focus from stressful topics to more adaptive and flexible plans, and this is related to the cognitive theory presented above. Positive psychotherapy may also be effective through processes that can build strong attitudes such as hope and optimism. Sleep seems to be a process through which positive emotions can show their effects on mental satisfaction [58].
It can also be stated that in patients with MS whose main symptoms are fatigue and insomnia, positive thinking training provides a general approach to life and something beyond the usual thoughts for the patient. Positive thinking enables them to focus on the positives rather than the negatives in all aspects of life. Good thoughts and feelings about oneself replace constant self-humiliation, make them think well about others and establish a good relationship with them, increases the expectation of the best in the world, and ultimately adds confidence in receiving the best of the world to one’s beliefs. These positive changes will undoubtedly reduce negative thoughts and lead to improved sleep quality [52].
The results also showed a significant difference between the effectiveness of the two intervention methods on sleep quality scores. Reality therapy intervention had a more significant impact on sleep quality compared to the positive intervention. But there was no significant difference between sleep quality components. No research has been found inside the country or abroad to compare the effectiveness of these two therapeutic approaches on sleep quality in MS patients. Therefore, we mentioned studies that are approximate or similar to this study or studies that only consider the effectiveness of one of the interventions. Therefore, the results of this finding are consistent with parts of the findings of Lee et al., [35] Wiley et al., [36] Pahlavan and Ahi [45]; Kim et al., [45] and Saghebi Saeedi et al. [47]. In this regard, BaniHashemi et al. suggested that reality therapy and treatment based on acceptance and commitment to the quality of life (physical dimension of sleep) have the same effectiveness [59]. In explaining this finding, it can be said that reality therapists believe that responsibility and selection are effective on thoughts, excitement, behavior, and proper control and satisfaction of needs and causes positive thinking and positive mood [60].
During treatment, the reality therapy approach helps patients choose the theory of choice or the internal control instead of external control. They accept that only the individual can do something for himself or herself, and with behavioral activation, setting objective goals and personal aspirations, and behaving in a committed manner to achieve them, the more positive emotions will emerge [61]. Reality therapy techniques such as living in the present, responsibility, fruitful relationships, and internal control can improve patients’ happiness and achieve positive emotions and feelings [60, 61]. Because of this, reality therapy can make a difference in the thoughts and attitudes of MS patients towards life by increasing positive emotions. Langer and Rodin also state that by emphasizing control, responsibility, feeling, and the attitude that everything is under our control, reality therapy can help patients change their attitudes and make them optimistic and positively redefine their lives and situations [62]. Therefore, in justifying the effectiveness of reality therapy, compared to positive psychotherapy, reality therapy is an intervention that uses positivity-related training in some sessions (the-7-habits techniques, destructive measures, etc.) (e.g., the sixth training session in the present study, which taught the identification of a quality world and a desirable world), in addition to the concepts related to the choice theory as well as acceptance of commitment therapy. In other words, the client, with the help of the therapist, tries to reduce destructive habits and cultivate good habits instead. Also, in the intervention process, the therapist seeks to moderate the contradiction between the patient’s quality world and the patient’s desired world and replace the negative emotions with positive emotions, which seems to justify the effectiveness of this therapeutic approach to a greater degree. This is because reality therapy intervention can consider more aspects of the mental health of MS patients, and this multidimensionality of the intervention also adds to its effectiveness. In terms of reality therapy, if people have a positive and realistic image of themselves and take responsibility for their actions, they will experience a sense of worth and feel better, and as a result, it will have a positive effect on their physical and mental health (sleep quality) and adaptation [63].
Because no research has so far compared the effectiveness of these two intervention methods, it was impossible to compare ours with the results of other studies. It can be said that reality therapy intervention is based on the principle that people choose their behaviors and are responsible for their own lives and what they do, feel, and think [14]. This approach helps people control their behavior and make better choices in their lives and emphasizes that having a successful identity is achieved through successful work and the power of choice is an important factor in their mental health [59, 60, 61, 62, 63, 64]. Accordingly, such assistance to MS patients through reality therapy intervention makes them feel responsible for all their behaviors and thoughts. Therefore, such thinking can reduce emotional disturbance and improve mental health and sleep quality by preparing the ground for accepting the disease.
Considering the effects of both therapeutic and educational methods on improving sleep quality in women with MS, both methods have good practical capabilities for clinical interventions to improve sleep quality. In addition, based on the results of the additional impact of reality therapy on sleep quality compared to positive intervention, it is suggested that this treatment method be used more by counselors and psychologists of medical centers and MS associations to improve the sleep quality of patients with MS. The specificity of the statistical population to the female gender was the main limitations of the present study. Therefore, it is suggested that future studies are done with a control group, and also a similar study should be performed on both genders to make the results more powerful.
Conclusion
The results showed that reality therapy and positive psychotherapy are effective on the sleep quality of women with MS. Reality therapy also showed greater effectiveness on sleep quality in women with MS. The psychological resources and positive cognitions created by positive psychotherapy create a strong protective function in response to the stress of the disease and thus improve the sleep quality of patients. Also, according to the theory of neuroplasticity, reality therapy can make changes in the biological process of women with MS by changing the thoughts, feelings, and actions of patients, thus improving the quality of sleep of patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (No.IR.GUMS.REC.1399.067) and the Iranian Registry of Clinical Trial (IRCT20200616047804N1). All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This article is derived from the PhD dissertation of first author at the Faculty of Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil (No. 1194860396442731398162255936).
Authors contributions
Conceptualization, supervision, and writing the original draft: Somayyeh Taklavi; Methodology, investigation: All authors; Writing, review, and editing: Abbas Abolghasemi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank Mrs Qutbzadeh (Director of MS Guilan Association), Mrs Fathi Moghadam (Director of Mehr-Ara Clinic), Miss Alidastan, and other loved ones who helped us in completing this research.
References
ultiple Sclerosis (MS) is one of the most common neurological diseases [1], causing inflammation and demyelination of the central nervous system. Damage to the myelin sheath in the nerve cell creates specific symptoms of the disease [2]. MS is one of the most significant life-changing diseases, as it usually affects the best part of a person’s life and gradually progresses to disability and has no definitive cure. As a result, this disease has damaged the productive forces of society [3]. The prevalence of this disease is rapidly increasing. Atlas of MS (2016) has estimated its prevalence worldwide to be about two and a half million people [4]. In Iran, 5.78 out of every 100 people have been reported with MS [5].
MS causes many physical problems for people with the disease, including balance disorder, one of the most debilitating symptoms of this disease, muscle cramps, extreme fatigue, bladder dysfunction, disability, sexual dysfunction, etc. These complications always reduce the ability to perform daily activities in MS patients [6]. In addition to physical problems, these patients have always reported many sleep problems [7, 8].
In general, almost any physical illness that produces significant pain or discomfort can negatively affect the quantity and quality of sleep [9]. Sleep is a dynamic and highly organized biological process that is an essential part of life, and the quantity of sleep is known to be related to the quality of social interaction. The importance of sleep in health and disease has been considered since Hippocrates, and disturbed sleep is considered a significant cause of suffering and illness of human beings at any age [10]. During sleep, the body restores its energy, and nerve cells are regenerated. Sleep protects the body against extreme fatigue. However, sleep is not just a neuro-physiological component. Psychologically, sleep, through its restorative effect, treats stressed and nervous people. When the sleep nuclei in the brain are damaged, the Circadian Rhythm (CR) of sleep is disrupted, and sleep quality is impaired [11]. Inadequate sleep quality can cause psychological problems and consequently the deterioration of the patients’ condition [12]. Because of sleep quality problems in patients with MS, psychological interventions can be an essential and effective step in reducing their psychological problems and improving their sleep quality. In particular, evidence suggests that traditional cognitive-behavioral therapy does not improve cognitive function in these patients [13].
The development of psychological therapies over the past few decades has led to the development of new approaches to maladaptive cognitions that target broad, contextual goals. Treatments of insomnia have evolved similarly, and several therapies, including reality therapy, have begun to gather evidence as effective therapies for sleep-related processes over the past few decades. Reality therapy is a method of psychotherapy that is based on the Choice Theory and was founded by Glasser. This treatment is based on the principle that people choose their behaviors and are responsible for their lives and what they do, feel, and think [14]. This approach helps people control their behavior and make better choices and emphasizes that having a successful identity is achieved through successful work and the power of choice is an essential factor in their mental health [15, 16]. In other words, its primary goal is to help clients learn better ways to satisfy all their psychological needs [17]. Researchers have examined and confirmed the effect of reality therapy on a wide range of psychological symptoms [18, 19, 20].
Although sleep is a powerful and highly regulated biological stimulus, the ability to fall asleep at any time and maintain sleep without waking up is very fragile and is affected by several factors. Identification of these factors is the key to insomnia treatment [21]. Positive psychological structures (e.g., optimism and hope) have been associated with better sleep quality in previous work [22]. However, such studies have not examined the effect of a wide range of positive psychological structures or the effectiveness of positive psychotherapy on sleep-related health behaviors. Positive psychotherapy originates from the positive psychology approach and is a multi-component model that enhances therapeutic change by creating interaction, pleasure, and meaning [23]. This approach, which is a combination of Beck’s cognitive approach in clinical practice, the Mihaly cognitive-attention syndrome, and Seligman’s positive psychology, teaches clients to be more optimistic. The main goal of this therapy is to extend the psychologist’s focus beyond the disease and its direct relief. The exercises used and suggested in this therapy directly target patients’ interpersonal relationships. Also, in some therapy sessions, patients are trained to use their abilities and strengths, which also helps them reduce their psychological problems by strengthening their self-confidence [24]. In addition, Lyubomirsky and Laius believed that positive interventions reduce depression and increase happiness and psychological wellbeing by increasing positive emotions, positive thoughts, and satisfying basic needs such as autonomy, love, belonging, and communication [25]. Cucarella and Perza showed that positivist psychology was effective in reducing stress in female patients [26]. In addition, other separate studies have shown that positive psychotherapy reduces patients’ emotional and mental memory problems [27, 28].
Glasser’s view of psychopathology in the reality therapy approach does not address the patient or a defect in behavior. In this view, to change the clients’ mental state, the choice of useful and effective behavior is considered instead of ineffective behavior, and by increasing the power of choice and behavior based on reality, the patient’s mental function is improved. On the other hand, positive psychotherapy is a different approach from other therapy models because it focuses on positive emotions and relationships, and wellbeing. According to what was said, the goals and techniques in the above two therapies are different. In reality therapy, selection, control, and internal factors are considered, and in positive psychotherapy, capabilities are. So it seems that comparing the effectiveness of these two therapeutic approaches should help select a more appropriate approach to improve sleep quality in patients with MS. Also, the researcher’s investigation on internal and external studies in the field of reality therapy and positive psychotherapy indicates that the effectiveness of these two treatment models has been studied on populations with various problems, and useful results have been obtained. However, the effectiveness of these two approaches on sleep quality in patients with MS has not been studied so far. Therefore, the present study aimed to compare the effectiveness of reality therapy and positive psychotherapy on sleep quality in women with MS.
Materials and Methods
This study was quasi-experimental research with a pre-test, post-test design and a control group. The study population included all female patients with MS referred to Guilan MS Association, Iran, in the summer and fall of 2019 (1197 people). Of them, 45 patients from the mentioned community were selected by purposive sampling method (taking into account the inclusion criteria) and randomly placed into three groups: reality therapy training (15 people), positive psychotherapy (15 people), and control group (15 people). This number was selected based on the sample size proposed for the experimental and quasi-experimental studies (at least 15 people for each group) [29]. The inclusion criteria include completing the consent form to participate in the training program, not suffering from acute psychological problems by the psychiatrist’s discretion, and the literacy level of at least third grade of guidance school to answer the questionnaires. Considering that the condition for membership in the MS association was the definitive confirmation of the disease by trusted experts, the criterion of the disease was membership in this association. The exclusion criteria included participation in other treatment programs, unwillingness to participate in the program, and two consecutive absences from intervention sessions.
After selecting the statistical subjects, both experimental groups received eight 90-minute sessions of intervention treatment, and the control group remained without any intervention. Because of the follow-up and encouragement of researchers, there was no subject withdrawal, and if any of the subjects missed only one training session, the researcher held extra programs to her catching up with the group.
Finally, after 4 weeks of holding training sessions, a post-test was taken from all three groups, and the data were analyzed with descriptive statistics (including mean and standard deviation) and Multivariate Analysis of Covariance (MANCOVA) in SPSS v. 22.
Research tools
Pittsburgh Sleep Quality Index (PSQI)
Pittsburgh Sleep Quality Index (PSQI) was developed by Buysse et al. to measure sleep quality and help diagnose the people who have good or bad sleep [30]. It consists of 18 items that determine people’s sleep quality by evaluating 7 characteristics during the last month. These characteristics include sleep quality in terms of the individual, the time it takes for the person to fall asleep, the duration of sleep, sleep efficiency, problems during sleep time, use of sleeping medication, and dysfunction of daily performance. Each of the 7 subscales in this questionnaire has a score of 0 to 3, where high scores indicate poor sleep. A total score greater than 5 indicates that the participant has poor sleep quality and severe problems in at least two areas. The reliability of this scale was calculated as 0.83, and its validity by a sensitivity of 89.6% and a specificity of 86.5% is at an appropriate level [30]. In Iran, the validity of this questionnaire for the Iranian population has been confirmed at the Tehran Psychiatric Institute. Also, the reliability coefficient of the questionnaire through Cronbach alpha was calculated as 0.81 [31]. Heidari et al. also reported validity of 0.86 and a reliability of 0.89 for this questionnaire [32].
Protocol of group reality therapy sessions
In this study, the reality therapy intervention was based on Glasser’s reality therapy training package [33], held during eight 90-minute sessions, one session per week for the study participants (experimental group). Details and summaries of the sessions are provided in Table 1.
.jpg)
Protocol of positive psychotherapy training sessions
In this study, a positive psychotherapy intervention was based on the reality therapy training package [34], was held during eight 90-minute sessions and one weekly session for study participants (experimental group 1). Details of the sessions are provided in Table 2.
.jpg)
Results
In the present study, 45 female patients with MS were studied in 3 groups: reality therapy training (15 patients), positive psychotherapy (15 patients), and a control group (15 patients). Demographic characteristics is shown in Table 3.
.jpg)
According to Table 4, the average quality of sleep and its components in the control group in the pre-test and post-test phase do not show any change.
.jpg)
But in the experimental group, it decreased in the post-test stage compared to the pre-test stage. The results of the Shapiro-Wilk test indicate that the distribution of data is normal in sleep quality variables and its components (P>0.05), and the premise of the normal distribution of data for covariance analysis is thus established. Also, the assumed results of homogeneity of covariance matrices of variance (M-Box test) indicate no difference between the variances (M-Box=62.690, F=1.731, P=0.079). Default homogeneity of regression line slope and the existence of a linear relationship between the covariate and the dependent variable for sleep quality and its dimensions was also investigated, which showed that these two assumptions were established. Following are the results related to the validity indicators of multivariate analysis of covariance (Table 5).
.jpg)
The results of validity indicators of multivariate analysis of covariance (Table 5) showed that the effect of group on the composition of the studied components is significant (P<0.05). Accordingly, the square of Eta shows that the difference between the two groups is generally significant with respect to the components of the dependent variable. To determine the more accurate effects of treatments on sleep quality subscales in women with MS, the results of adjusted means and Bonferroni post hoc test have been reported (Table 6).
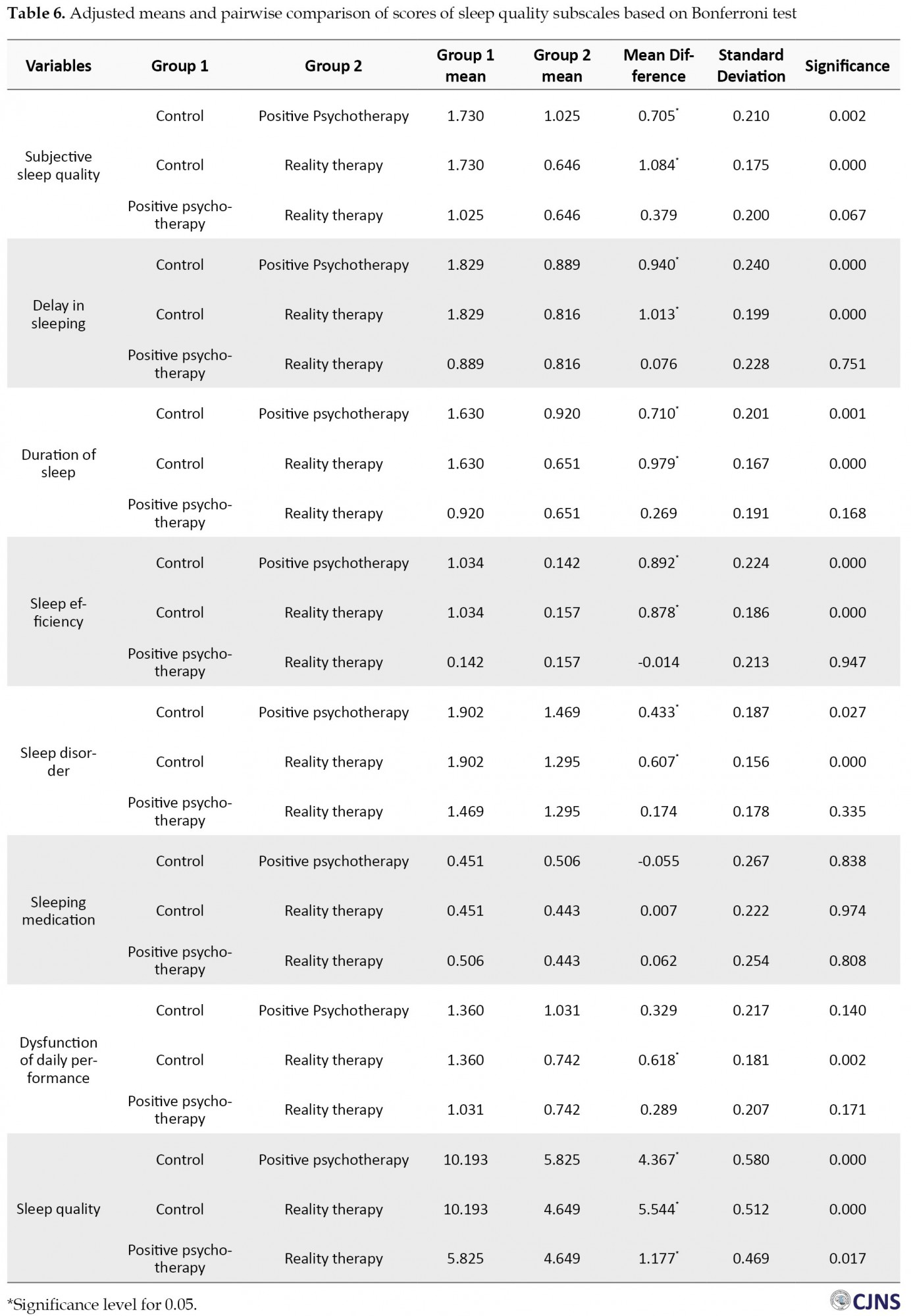
According to Table 6, the sleep quality in the reality therapy group showed a more appropriate and significant improvement compared to the positive treatment (P<0.05). But in all sleep quality subscales, there is no significant difference between reality therapy and positive psychotherapy (P>0.05).
Discussion
This study aimed to compare the effectiveness of reality therapy and positive psychotherapy on sleep quality in women with MS. The results showed that reality therapy significantly affected sleep quality and its components in women with MS. The result was consistent with the findings of Lee et al., [35] Willie et al. [36]. In explaining this finding, based on the opinion of researchers, the emotional reaction to illness and physical pain affect the quality and quantity of sleep [37]. Therefore, when MS patients underwent this intervention, they could improve their sleep quality by controlling emotional reactions such as anxiety, stress, and depression. In particular, there is a significant correlation between sleep quality and reduced emotional disturbance [38]. It is also noteworthy that sleep is a bio-cognitive process, and reality therapy intervention based on selection theory refers to explaining how and why the brain works. Therefore, from the point of view of this theory, providing education based on reality therapy paves the way for improving the biological process. According to the theory of neuroplasticity, neural pathways and synapses can be altered by changes in behavior, environmental processes, and neural processes. The reorganization of the views of different parts of the body in the cerebral cortex constantly occurs in response to activities, behaviors, and skill learning, so neural processes have flexibility. Reality therapy can make a difference in people’s biological processes by changing their thoughts, feelings, and actions [39].
Reality therapy has techniques to help people change their inefficient behaviors to efficient ones, destructive styles into wise alternatives, and above all, their unhealthy lifestyle to a healthy one [38]. In choice theory, behavior consists of four components: thinking, action, feeling, and physiology. Glasser suggested that we have considerable control or choice over the first two: thinking and acting. However, we have little ability to directly select the components of emotion and physiology because they are deeply unconscious. These four components are closely intertwined, and the choices we make in our thinking and acting indirectly and significantly affect our feelings and physiology [40]. Sleep involves a sequence of neurophysiological changes in the brain. Proper sleep involves a dynamic interaction between voluntary decisions and involuntary biological activity. Turning off the lights, reducing the noise, and lying down are voluntary behavior, but the result is an involuntary increase in melatonin and a series of changes in brain activity patterns during the night. Sleeping ultimately depends on cooperation between behavior and biology, and the defect in any of them causes sleep disorders [41]. Therefore, reality therapy can make significant changes in the patient’s feelings and physiology and provide a basis for improving the quality of sleep in MS patients through cognitive evaluation and training to stop rumination, change attention and provide a distraction. It changes the individual’s knowledge about the disease and sleep quality problems by manipulating the patient’s thinking and action [42].
Consistent with the above argument in the reality therapy intervention, the therapist asks the client: what options do you have to deal with your problem? The client should use the brainstorming method. The therapist challenges the patient’s irrational thoughts by offering several options as well as questions. In other words, the patient’s enjoyment and satisfaction with life are enhanced by creating a positive view of the disease, changing negative perceptions, and emphasizing the patient’s different roles in life (for example, the patient is told that you aren’t a prisoner of your MS and sleep problems, starting now you can have a better life by choosing a healthy lifestyle and changing your thoughts and attitudes) [43]. Therefore, based on Glasser’s point of view, people are in any given situation because of their individual choices and because they have not been able to satisfy their basic needs in a right and reasonable way. Humans can create a better situation by choosing an effective and appropriate way to meet their needs and positively affect their physiological processes, such as sleep quality [44].
The other part of the results showed that positive psychotherapy significantly affected sleep quality and its components in women with MS. The results obtained were consistent with the findings of Kim et al., [45] Pahlavan et al., [46] and Saghebi Saeedi et al. [47]. In this regard, Kim et al. suggested in a study that positive psychology has a significant mediating effect on the relationship between sleep disorders and depressive symptoms and can reduce the symptoms of sleep disorders and depression caused by sleep disorders [45]. The present study findings are consistent with McEwen’s theory of allostatic load. This theory interprets the individual’s attempt to adapt to the demands of life as a cumulative physiological load imposed on the body. Accordingly, patients with MS who experience insomnia may experience increased stress and inability to participate in enjoyable activities, making them more vulnerable to sleep disorders [45]. Previous research findings have confirmed this finding. In a large study, Hamilton et al. reported that participants with low levels of psychological wellbeing showed more sleep disorders independent of age, gender, physical symptoms, and cognitive disorders [48]. Therefore, experiencing high levels of chronic stress in patients with MS leads to activation of the Hypothalamic-Pituitary-Adrenal (HPA) axis, an essential neuroendocrine mediator of the stress response. HPA axis hyperactivity, which leads to increased cortisol levels, may stimulate poor sleep in these patients and is associated with an increased risk of insomnia.
Conversely, the symptoms of insomnia in patients may also increase cortisol levels, causing a vicious cycle [49]. Therefore, it seems that the psychological resources and positive cognitions generated by positive psychotherapy create a strong protective function in response to stress and improve the sleep quality of patients by modulating HPA-based activity and reducing overall cortisol levels. Previous studies have also supported this conceptualization, and research has shown that people with more psychological resources do not show an HPA response to crucial negative life events and daily stress [50, 51]. The broaden-and-build theory suggests that positive emotions associated with positive cognitions enhance patients’ physical, intellectual, and social resources by expanding the action-thought repertoire [52]. Examples of these resources include the quality of social relationships and resilience, both of which have been suggested to improve sleep quality [53, 54]. In this regard, Solberg and Segerstrom argue that people with positive cognitions are often more flexible in using coping strategies and are more successful in dealing with controlled and uncontrollable stressors. Therefore, the positive cognition developed in a person following positive psychotherapy is likely to affect sleep quality through a combination of psychological, behavioral, and biological pathways [55].
In explaining this finding, we can refer to the techniques and exercises used in positivity intervention. Positive gratitude exercises seem to have been effective in this regard [56]. The development and construction of positive emotion models and cognitive sleep models are especially important for study [57]. The content of pre-sleep cognitions is also essential. Cognitive sleep patterns reflect the biases of people who have lower sleep quality in sensitive periods before going to sleep and cannot interpret this low quality (such as focusing on negative events or the idea that I cannot sleep well). This condition happens because schemes and hypotheses activate the information processing system. A clear explanation for this is that rumination about sleep problems can intensify sleep problems, which is, in fact, one of the best predictors of delayed sleep [57]. Gratitude exercises may encourage individuals to shift their focus from stressful topics to more adaptive and flexible plans, and this is related to the cognitive theory presented above. Positive psychotherapy may also be effective through processes that can build strong attitudes such as hope and optimism. Sleep seems to be a process through which positive emotions can show their effects on mental satisfaction [58].
It can also be stated that in patients with MS whose main symptoms are fatigue and insomnia, positive thinking training provides a general approach to life and something beyond the usual thoughts for the patient. Positive thinking enables them to focus on the positives rather than the negatives in all aspects of life. Good thoughts and feelings about oneself replace constant self-humiliation, make them think well about others and establish a good relationship with them, increases the expectation of the best in the world, and ultimately adds confidence in receiving the best of the world to one’s beliefs. These positive changes will undoubtedly reduce negative thoughts and lead to improved sleep quality [52].
The results also showed a significant difference between the effectiveness of the two intervention methods on sleep quality scores. Reality therapy intervention had a more significant impact on sleep quality compared to the positive intervention. But there was no significant difference between sleep quality components. No research has been found inside the country or abroad to compare the effectiveness of these two therapeutic approaches on sleep quality in MS patients. Therefore, we mentioned studies that are approximate or similar to this study or studies that only consider the effectiveness of one of the interventions. Therefore, the results of this finding are consistent with parts of the findings of Lee et al., [35] Wiley et al., [36] Pahlavan and Ahi [45]; Kim et al., [45] and Saghebi Saeedi et al. [47]. In this regard, BaniHashemi et al. suggested that reality therapy and treatment based on acceptance and commitment to the quality of life (physical dimension of sleep) have the same effectiveness [59]. In explaining this finding, it can be said that reality therapists believe that responsibility and selection are effective on thoughts, excitement, behavior, and proper control and satisfaction of needs and causes positive thinking and positive mood [60].
During treatment, the reality therapy approach helps patients choose the theory of choice or the internal control instead of external control. They accept that only the individual can do something for himself or herself, and with behavioral activation, setting objective goals and personal aspirations, and behaving in a committed manner to achieve them, the more positive emotions will emerge [61]. Reality therapy techniques such as living in the present, responsibility, fruitful relationships, and internal control can improve patients’ happiness and achieve positive emotions and feelings [60, 61]. Because of this, reality therapy can make a difference in the thoughts and attitudes of MS patients towards life by increasing positive emotions. Langer and Rodin also state that by emphasizing control, responsibility, feeling, and the attitude that everything is under our control, reality therapy can help patients change their attitudes and make them optimistic and positively redefine their lives and situations [62]. Therefore, in justifying the effectiveness of reality therapy, compared to positive psychotherapy, reality therapy is an intervention that uses positivity-related training in some sessions (the-7-habits techniques, destructive measures, etc.) (e.g., the sixth training session in the present study, which taught the identification of a quality world and a desirable world), in addition to the concepts related to the choice theory as well as acceptance of commitment therapy. In other words, the client, with the help of the therapist, tries to reduce destructive habits and cultivate good habits instead. Also, in the intervention process, the therapist seeks to moderate the contradiction between the patient’s quality world and the patient’s desired world and replace the negative emotions with positive emotions, which seems to justify the effectiveness of this therapeutic approach to a greater degree. This is because reality therapy intervention can consider more aspects of the mental health of MS patients, and this multidimensionality of the intervention also adds to its effectiveness. In terms of reality therapy, if people have a positive and realistic image of themselves and take responsibility for their actions, they will experience a sense of worth and feel better, and as a result, it will have a positive effect on their physical and mental health (sleep quality) and adaptation [63].
Because no research has so far compared the effectiveness of these two intervention methods, it was impossible to compare ours with the results of other studies. It can be said that reality therapy intervention is based on the principle that people choose their behaviors and are responsible for their own lives and what they do, feel, and think [14]. This approach helps people control their behavior and make better choices in their lives and emphasizes that having a successful identity is achieved through successful work and the power of choice is an important factor in their mental health [59, 60, 61, 62, 63, 64]. Accordingly, such assistance to MS patients through reality therapy intervention makes them feel responsible for all their behaviors and thoughts. Therefore, such thinking can reduce emotional disturbance and improve mental health and sleep quality by preparing the ground for accepting the disease.
Considering the effects of both therapeutic and educational methods on improving sleep quality in women with MS, both methods have good practical capabilities for clinical interventions to improve sleep quality. In addition, based on the results of the additional impact of reality therapy on sleep quality compared to positive intervention, it is suggested that this treatment method be used more by counselors and psychologists of medical centers and MS associations to improve the sleep quality of patients with MS. The specificity of the statistical population to the female gender was the main limitations of the present study. Therefore, it is suggested that future studies are done with a control group, and also a similar study should be performed on both genders to make the results more powerful.
Conclusion
The results showed that reality therapy and positive psychotherapy are effective on the sleep quality of women with MS. Reality therapy also showed greater effectiveness on sleep quality in women with MS. The psychological resources and positive cognitions created by positive psychotherapy create a strong protective function in response to the stress of the disease and thus improve the sleep quality of patients. Also, according to the theory of neuroplasticity, reality therapy can make changes in the biological process of women with MS by changing the thoughts, feelings, and actions of patients, thus improving the quality of sleep of patients.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Guilan University of Medical Sciences (No.IR.GUMS.REC.1399.067) and the Iranian Registry of Clinical Trial (IRCT20200616047804N1). All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This article is derived from the PhD dissertation of first author at the Faculty of Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil (No. 1194860396442731398162255936).
Authors contributions
Conceptualization, supervision, and writing the original draft: Somayyeh Taklavi; Methodology, investigation: All authors; Writing, review, and editing: Abbas Abolghasemi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We would like to thank Mrs Qutbzadeh (Director of MS Guilan Association), Mrs Fathi Moghadam (Director of Mehr-Ara Clinic), Miss Alidastan, and other loved ones who helped us in completing this research.
References
- Pompili M, Forte A, Palermo M, Stefani H, Lamis DA, Serafini G, et al. Suicide risk in multiple sclerosis: A systematic review of current literature. J Psychosom Res. 2012; 73(6):411-7. [DOI:10.1016/j.jpsychores.2012.09.011] [PMID]
- Hughes N, Locock L, Ziebland S. Personal identity and the role of ‘carer’ among relatives and friends of people with multiple sclerosis. Soc Sci Med. 2013; 96:78-85. [DOI:10.1016/j.socscimed.2013.07.023] [PMID] [PMCID]
- Holland NJ, Madonna M. Nursing grand rounds: Multiple sclerosis. J Neurosci Nurs. 2005; 37(1):15-9. [DOI:10.1097/01376517-200502000-00003]
- Biernacki, T, Sandi, D, Zsanett, F, Tamás, K, Rózsa, L, Zsófia, K. Epidemiology of multiple sclerosis in Central Europe, update from Hungary. Brain Behav. 2020; 10(5):e01598. [DOI:10.1002/brb3.1598] [PMID] [PMCID]
- Nasiri M, Hosseini SH, Sakhaei SY, Tabrizi N, Yazdani Cherati J, Abedini M. [Prevalence of psychiatric disorders in patients with multiple sclerosis in Mazandaran, Iran (Persian)]. J Mazandaran Univ Med Sci. 2016; 26(140):60-70. http://jmums.mazums.ac.ir/article-1-8549-en.html
- Doumas M, Smolders C, Krampe RT. Task prioritization in aging: Effects of sensory information on concurrent posture and memory performance. Exp Brain Res. 2008; 187(2):275-81. [DOI:10.1007/s00221-008-1302-3] [PMID]
- Razazian N, Najafi F, Mahdavi P, Aghaie A. [Prevalence of sleep disorders in patients with multiple sclerosis (Persian)]. J Mazandaran Univ Med Sci. 2014; 23(110):219-24. http://jmums.mazums.ac.ir/article-1-3384-en.html
- Fogelberg, DJ, Hughes, AJ, Vitiello, MV. Hoffman, JM. & Amtmann, D. Comparison of sleep problems in individuals with spinal cord injury and multiple sclerosis. J Clin Sleep Med. 2016; 12(5):695-701. [DOI:10.5664/jcsm.5798] [PMID] [PMCID]
- Shalileh K, Purpak Z, Harirchian MH, Negar F. [Multiple Sclerosis. (Persian)]. Tehran: Hayan Publishing; 2007. https://www.gisoom.com/book/1419379
- Gleason K, McCall, WV. Current concepts in the diagnosis and treatment of sleep disorders in the elderly. Curr Psychiatry Rep. 2015; 17(6):45. [DOI:10.1007/s11920-015-0583-z] [PMID]
- Motavakel N, Maghsoudi Z, Mohammadi Y, Oshvandi K. [The effect of spiritual care on sleep quality in patients with Multiple Sclerosis referred to the MS Society of Hamadan City in 2018 (Persian)]. Avicenna J Nurs Midwifery Care. 2020; 28(1):36-45. [DOI:10.30699/ajnmc.28.1.36]
- Karimi S, Jalilian M, Abdi A, Khazaie H, Sarbarzeh PA. [Surveying sleep quality and fatigue in multiple sclerosis patients at a multiple sclerosis center in Kermanshah, Iran, in 2017 (Persian)]. Neurobiol Sleep Circadian Rhythms. 2020; 8:100050. [DOI:10.1016/j.nbscr.2020.100050] [PMID] [PMCID]
- Jackson H, Hannah, MacLeod AK. Well-being in chronic fatigue syndrome: Relationship to symptoms and psychological distress. Clin Psychol Psychother. 2017; 24(4):859-69. [DOI:10.1002/cpp.2051] [PMID]
- Abbott WJ. The effect of reality therapy-based group counseling on the self esteem of learning disabled sixth, seventh, and eighth graders. Virginia: University of Virginia; 1983. https://books.google.com/books?id
- Palmer Mason C, Duba JD. Using reality therapy in schools :Its potential impact on the effectiveness of the ASCA national model. Int J Reality Ther. 2009; 29(2):5-12. https://digitalcommons.wku.edu/cgi/viewcontent.cgi?article=1036&context=csa_fac_pub
- Sedaghat M, Sahebi A, Shahabi Moghaddam S. [The effectiveness of individualized reality therapy on major depression patients with suicide attempt history (Persian)]. J Police Med. 2017; 5(5):371-8. http://teb.police.ir/teb/article-1-481-en.html
- Arefi M, Ganjoori M. [Effectiveness of reality therapy training on psychological well-being of deaf students. J Journal of Social Work (Persian)]. 2017; 6(1):21-8. http://socialworkmag.ir/browse.php?a_id=286&sid=1&slc_lang=fa
- Bhargava R. The use of reality therapy with a depressed deaf adult. Clin Case Stud. 2013; 12(5):388-96. [DOI:10.1177/1534650113496869]
- Klingler LK, Gray ND. Reality therapy/choice theory today: An interview with Dr. Robert E. Wubbolding. Canadian J Counsel Psychother. 2015; 49(2):185–97. https://cjc-rcc.ucalgary.ca/article/view/61040
- Sauerheber JD, Graham MA, Britzman MJ, Jenkins C. Using reality therapy to facilitate successful aging in clinical practice. Family J. 2016; 24(2):174-81. [DOI:10.1177/1066480716628630]
- Veauthier C, Paul F. Sleep disorders in multiple sclerosis and their relationship to fatigue. Sleep Med. 2014; 15(1):5-14. [DOI:10.1016/j.sleep.2013.08.791] [PMID]
- Lemola S, Räikkönen K, Scheier MF, Matthews KA, Pesonen AK, Heinonen K, et al. Sleep quantity, quality and optimism in children. J Sleep Res. 2011; 20(1 Pt 1):12-20. [DOI:10.1111/j.1365-2869.2010.00856.x] [PMID] [PMCID]
- Amonoo HL, Brown LA, Scheu CF, et al. Positive psychological experiences in allogeneic hematopoietic stem cell transplantation. Psychooncology. 2019; 28(8):1633-9. [DOI:10.1002/pon.5128] [PMID]
- Seligmon MEP. Flourish: A visionary new understanding of happiness and well-being. New York: Free Press; 2011. https://psycnet.apa.org/record/2010-25554-000
- Lyubomirsky S, Layous K. How do simple positive activities increase well-being? Curr Dir Psychol Sci. 2013; 22(1):57-62. [DOI:10.1177/0963721412469809]
- Cucarella SP, Pereza MAC. Positive psychology in women with breast cancer. Eur Proc Social Beh Sci (EpSBS). 2015; 12-21. [DOI:10.15405/epsbs.2015.07.3]
- Fisher PL, Byrne A, Salmon P. Metacognitive therapy for emotional distress in adult cancer survivors: A case series. Cognit Ther Res. 2017; 41(6):891-901. [DOI:10.1007/s10608-017-9862-9] [PMID] [PMCID]
- Jacobsen HB, Aasvik JK, Borchgrevink PC, Landrø NI, Stiles TC. Metacognitions are associated with subjective memory problems in individuals on sick leave due to chronic fatigue. Front Psychol. 2016; 7:729. https://doi.org/10.3389/fpsyg.2016.00729
- Delawar A. Research Methods in Psychology and Educational Sciences. Tehran: Virayesh Publishing; 2012. https://www.gisoom.com/book/11018856/
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatr Res. 1989; 28(2):193-213. [DOI:10.1016/0165-1781(89)90047-4]
- Afkham Ebrahimi A, Ghale Bandi M, Salehi M, Kafian Tafti A, Vakili Y, Akhlaghi Farsi E. [Sleep parameters and the factors affecting the quality of sleep in patients attending selected clinics of Rasoul-e-Akram hospital (Persian)]. Razi J Med Sci (RJMS). 2008; 15:31-8. http://rjms.iums.ac.ir/index.php?&slct_pg_id=10&sid=1&slc_lang=en
- Heidari ARP, Ehteshamzadeh, and M. Marashi. [The relationship between insomnia intensity, sleep quality, sleepiness and mental health disorder with educational performance in female adolescences of Ahwaz City (Persian)]. Woman Cult. 2010; 1(4):65-76. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=258950
- Glasser, W. Choice Theory: A new psychology of personal freedom. New York: Harper Collins; 1999. https://www.amazon.com/Choice-Theory-Psychology-Personal-Freedom/dp/0060930144
- Coniliam S. Positive thinking and applied positivism [Barati Sedeh F, Sadeghi A, Persian trans.]. Tehran: Roshd; 2016. https://www.fadakbook.ir/product/11793/
- Lee SY, Kang J. Effect of virtual reality meditation on sleep quality of intensive care unit patients: A randomised controlled trial. Intensive Crit Care Nurs. 2020; 59:102849. [DOI:10.1016/j.iccn.2020.102849] [PMID]
- Wiley E, Khattab S, Tang A. Examining the effect of virtual reality therapy on cognition post-stroke: A systematic review and meta-analysis. Disabil Rehabil Assist Technol. 2020; 1-11. [DOI:10.1080/17483107.2020.1755376] [PMID]
- Bamer AM, Johnson KL, Amtmann D, Kraft GH. Prevalence of sleep problems in individuals with Multiple Sclerosis. Mult Scler. 2008; 14(8):1127-30. [DOI:10.1177/1352458508092807] [PMID] [PMCID]
- Casstevens WJ. Using reality therapy and choice theory in health and wellness program development within psychiatric psychosocial rehabilitation agencies. Int J Choice Theory Real Ther. 2010; 29(2):55-8. Using reality therapy and choice theory in health and wellness program development within psychiatric psychosocial rehabilitation agencies
- Dehghan L, Dalvand H. Neuroplasticity after injury. J Mod Rehabil. 2008; 1(4):13-9. htpp://mrj.tums.ac.ir/article-1-154-fa.htmi
- Broda A, Krüger J, Schinke S, Weber A. Determinants of choice of delivery place: Testing rational choice theory and habitus theory. Midwifery. 2018; 63:33-8. [DOI:10.1016/j.midw.2018.04.023] [PMID]
- Tubbs AS, Dollish HK, Fernandez F, Grandner MA. Chapter 1 - The basics of sleep physiology and behavior. In: MA Grandner (ed.), Sleep and Health (pp. 3-10): Academic Press. [DOI:10.1016/B978-0-12-815373-4.00001-0]
- Greenberg LS. Emotion-focused therapy: A synopsis. J Contemp Psychother. 2006; 36(2):87-93. [DOI:10.1007/s10879-006-9011-3]
- Dehnavi H, Sadeghi M, Sepahvandi M. The effectiveness of the integrative approach of reality: Emotion-focused therapy on the quality of sleep and sexual self-efficacy in women with hypothyroidism. Sadra Med J. 2020; 8(2):91-102. [DOI:10.30476/smsj.2020.82889.1039]
- Greenberg LS, Elliott R, Pos A. Special topic: Emotion-focused therapy. Eur Psychother. 2007; 7:87-93. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.458.7814&rep=rep1&type=pdf
- Kim SH, Park SH, Choo IH, Kim SG, Yoon HJ. The relationship between sleep disturbance and depressive symptoms among Korean university students: moderating effect of the positive psychology. Eur Neuropsychopharmacol. 2019; 29(1):S292. [DOI:10.1016/j.euroneuro.2018.11.458]
- Pahlavan A, AHI Q. [Effectiveness of positive psychology interventions on death anxiety and sleep quality of female patients with Multiple Sclerosis (MS) (Persian)]. Res Clin Psychol Counsel. 2019-2020; 9(2):28-42. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=733539
- Saghebi Saeedi K, Abolghasem A, Akbari B. [The effectiveness of self-compassion training and positive thinking on sleep quality and decrease of pain intensity in girl with primary dysmenorrhea (Persian)]. Complemen Med J (CMJA). 2020; 9(4):3914-29. [DOI:10.32598/cmja.9.4.942.1]
- Hamilton NA, Gallagher MW, Preacher KJ, Stevens N, Nelson CA, Karlson C, et al. Insomnia and well-being. J Consult Clin Psychol. 75(6):939-46. [DOI:10.1037/0022-006X.75.6.939] [PMID]
- Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010; 2010:759234. [DOI:10.1155/2010/759234] [PMID] [PMCID]
- Chiang JJ, Ko A, Bower JE, Taylor SE, Irwin MR, Fuligni AJ. Stress, psychological resources, and HPA and inflammatory reactivity during late adolescence. Dev Psychopathol. 2019; 31(2):699-712. [DOI:10.1017/S0954579418000287] [PMID] [PMCID]
- Lau EY, Hui CH, Lam J, Cheung SF. Sleep and optimism: A longitudinal study of bidirectional causal relationship and its mediating and moderating variables in a Chinese Student Sample. Chronobiol Int. 2017; 34(3):360-72. [DOI:10.1080/07420528.2016.1276071] [PMID]
- Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychol. 2001; 56, 218-26. [DOI:10.1037/0003-066X.56.3.218]
- Kent RG, Uchino BN, Cribbet MR, Bowen K, Smith TW. Social relationships and sleep quality. Ann Behav Med. 2015; 49(6):912-7. [DOI:10.1007/s12160-015-9711-6] [PMID] [PMCID]
- Li Y, Gu S, Wang Z, Li H, Xu X, Zhu H, et al. Relationship between stressful life events and sleep quality: Rumination as a mediator and resilience as a moderator. Front Psychiatr. 2019; 10:348. [DOI:10.3389/fpsyt.2019.00348] [PMID] [PMCID]
- Nes LS, Segerstrom SC. Dispositional optimism and coping: A meta-analytic review. Pers Soc Psychol Rev. 2006; 10(3):235-51. [DOI:10.1207/s15327957pspr1003_3] [PMID]
- Amonoo HL, Barclay ME, El-Jawahri A, Traeger LN, Lee SJ, Huffman JC. Positive psychological constructs and health outcomes in hematopoietic stem cell transplantation patients: A systematic review. Biol Blood Marrow Transplant. 2019; 25(1):e5-e16. [DOI:10.1016/j.bbmt.2018.09.030] [PMID]
- Mitchell AJ, Benito-León J, Morales González JM, Rivera- Navarro J. Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. Lancet Neurol. 2005; 4(9):556-66. [DOI:10.1016/S1474-4422(05)70166-6]
- Seligman MEP. Authentic happiness: Using the new positive psychology to realize your potential for lasting fulfilment. New York: Free Press. https://books.google.com/books?id=3L0BCCoFMRgC&dq
- Bani Hashemi S, Hatami M, Hasani J, Sahebi A. Comparing effectiveness of the cognitive-behavioral therapy, reality therapy, and acceptance and commitment therapy on quality of life, general health, and coping strategies of chronic patient’s caregivers. J Clin Psychol. 2020; 12(1):63-76. [DOI:10.22075/jcp.2020.18992.1757]
- Barness R, Parish TS. Drugs” versus” reality therapy. Int J Reality Ther. 25(2):43-54. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.604.7999&rep=rep1&type=pdf
- Wubbolding RE, Brickell J. The work of brandiroth. Int J Choice Theory and Reality Ther. 2014; 33(2):7-12. https://www.sid.ir/en/journal/ViewPaper.aspx?ID=517536
- Goldstein S, Naglieri JA. Assessing impairment: From theory to practice. Springer Nature Switzerland; 2016. [DOI:10.1007/978-1-4899-7996-4]
- Corey G. Theory and practice of counseling and psychotherapy. Boston, Massachusetts: Cengage Learning; 2015. https://www.amazon.com/Theory-Practice-Counseling-Psychotherapy-Gerald/dp/1305263723
- Mason D, Palmer C, Duba D, Jill D. Using reality therapy in schools: Its potential impact on the effectiveness of the ASCA national model. Int J Real Ther. 2009; 29(2):5-12. https://digitalcommons.wku.edu/csa_fac_pub/33/
Type of Study: Research |
Subject:
Special
Received: 2021/07/1 | Accepted: 2021/04/30 | Published: 2021/04/30
Received: 2021/07/1 | Accepted: 2021/04/30 | Published: 2021/04/30
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |