Sat, Sep 21, 2024
Volume 7, Issue 1 (Winter 2021)
Caspian J Neurol Sci 2021, 7(1): 22-29 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rangrazian F, Kiamarsi A, Kazemi R. Effectiveness of Illness Management Program on Positive/Negative Symptoms, and Insight of Schizophrenic Patients. Caspian J Neurol Sci 2021; 7 (1) :22-29
URL: http://cjns.gums.ac.ir/article-1-385-en.html
URL: http://cjns.gums.ac.ir/article-1-385-en.html
1- Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil, Iran.
2- Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil, Iran. ,a.kiamarsi52@gmail.com
2- Department of Psychology, Ardabil Branch, Islamic Azad University, Ardabil, Iran. ,
Full-Text [PDF 1398 kb]
(692 Downloads)
| Abstract (HTML) (1799 Views)
Full-Text: (975 Views)
Introduction
chizophrenia is a complex neuropsychological disorder affecting approximately 1% of the global population. The disease is characterized by hallucinations, delusions, disorganized behavior, and progressive cognitive impairments [1]. The outbreak of schizophrenia is similar among women and men, with women having a better prognosis and usually have a better social functioning before the disease onset [2]. The negative symptoms include affective flattening or blunting, poverty of speech or content of speech, thinking blocking or dysfunction, inappropriate grooming and hygiene, lack of motivation, lack of pleasure, social inattentiveness, cognitive impairments, and lack of attention. The positive symptoms include impaired perception, thinking, and behavior such as loosening of associations, hallucinations, bizarre behavior, and tangentially. Patients with positive symptoms usually have a better prognosis than patients with negative symptoms [3].
According to various studies, negative symptoms have a more severe effect on reducing the quality of life and functional disability in these patients than the positive symptoms [4]. Lack of insight into the disease is one of the most common symptoms of schizophrenia. The insight into the disease ranges from the initial awareness of the condition to a deep and reasonable understanding and emotional touch of the disease. Lack of insight is more common in schizophrenia than in other disorders. Also, it is highly involved in the disease prognosis and can lead to disease recurrence and an increased number of hospital admissions [5]. Impaired insight is associated with impairments in cognitive functions, self-awareness, empathy, and self-control, and poor cooperation for treatment, and subsequently forced hospitalization. Decreased insight is correlated with the psychopathology of the disease. The lack of insight leads to a lack of cooperation in treatment and subsequently persistence of the patients’ problems and the family/friends [6]. There is significant evidence that schizophrenic patients not only lack insight into their psychotic symptoms but also have neurocognitive disorders. The patients likely show low metacognitive awareness of the cognitive functions involved in the delusional symptoms [7]. Akbari and Saeidi found that psychosocial rehabilitation had a significant effect on reducing the negative symptoms and improving the social skills in patients with chronic schizophrenia [8]. Esmkhani et al. showed that the interventional programs aimed at improving treatment adherence could enhance the quality of life in schizophrenic patients [9]. Haji Aghaei et al. showed that psychological education of the family was effective in decreasing the symptom severity and recurrence of schizophrenia [10].
Illness management is a program with a combination of psychosocial interventions that helps patients have more control over their problems and also helps in disease management and supports recovery [11]. In general, self-management is a new type of education in caregiving for patients with chronic diseases. In this therapeutic method, the process of problem-solving is done by the patient, and the necessary coping skills are taught to the patient by the treatment team. Therefore, patients learn to control the complications by relying on their skills and self-confidence using problem-solving skills. Finally, the main goal in the self-management educational program is managing the illness by the patients themselves [12]. A study by Burlingame et al. showed that group therapy was effective in treating schizophrenic patients [13].
It seems that teaching illness management to schizophrenic patients needs further attention. Also, limited education has been provided to these patients in Iran. Few studies have been conducted on the Iranian society focusing on the illness management education among these patients, and there is a need for such research in this field. Therefore, the present study aimed to investigate the effectiveness of the illness management program on the positive symptoms, negative symptoms, and insight of schizophrenic patients.
Materials and Methods
This present study was a quasi-experimental study with a pre-test, post-test design and a control group. The study population consisted of all the schizophrenic patients (n=796) admitted to the Shafa Hospital, Rasht City, from March 2019 to April 2020. A total of 30 patients were selected using the convenient sampling method in a purposeful manner and randomly divided into 2 groups of the experimental group and the control group, with 15 patients in each group. The pre-test was performed in both groups. Then, the experimental group underwent the intervention of illness management in 20 sessions, each with 90 minutes duration (Table 1), twice a week as group therapy in the hospital.
.jpg)
During this time, both groups received medication as directed by a psychiatrist, while the control group did not undergo any psychological interventions. Finally, both groups underwent the post-test after the treatment course. A 4-question questionnaire on the precision of illness management therapy was prepared with yes/no answers to examine the validity of the illness management therapy, and 6 assessors (therapists) answered the questions. The coefficient of agreement between the answers of the 6 assessors was then calculated as being 0.894 (P<0.05).
The inclusion criteria included the diagnosis of schizophrenia by a psychiatrist, being in the schizophrenia chronic phase, being affected by the disease for at least 2 years, and age from 20 to 45 years old. Also, the exclusion criteria included receiving another type of psychotherapy simultaneously, being absent for more than 3 sessions, and treatment cessation.
Study tools
The Scale for the Assessment of Negative Symptoms (SANS)
It is designed and standardized by Andreasen et al. The Scale for the Assessment of Negative Symptoms (SANS) scale has 24 items assessing 5 classes of negative symptoms of schizophrenia, including affective flattening or blunting, poverty of speech, avolition, apathy, lack of pleasure, social inattentiveness, and lack of attention [14]. A general question assesses the set of related symptoms at the end of each group. The answers are scored on a 6-point scale ranging from 0 for the absence of symptoms to 5 states of symptom severity. The higher the score of the patients, the severer their symptoms would be. The questionnaire is filled by the researcher using the information obtained from questioning the patient. The reliability values of the Persian version of the scale using the methods of internal consistency, test-retest, and inter-rater reliability were found as 0.94, 0.92, and 0.89, respectively [15]. The reliability of the negative symptoms in the Iranian culture was calculated to be 0.78 using the methods test-retest [16]. The Cronbach alpha was calculated to be 0.81 for the internal consistency of the negative symptoms [17].
The Scale for the Assessment of Positive Symptoms (SAPS)
It is also designed by Andreasen et al. The scale has 30 items assessing 4 groups of positive symptoms: hallucinations, delusions, bizarre behaviors, and formal thought disorder [18]. This tool can also cover the months before the time of evaluation by considering a suitable duration. The questionnaire is filled by the researcher using a standard clinical interview, in which there should be a 5-10-minute conversation about a neutral topic with the patient for evaluating the speech and response style to find a significant abstract thought disorder. Also, other sources such as direct observation and reports of the family and nurses can be used. The answers are scored on a 6-point scale ranging from 0 for the absence of the symptoms to 5 as the most severe. The higher the scores of the patients, the severer their symptoms would be. The last item of each group needs an overall score on the nature and severity of the certain symptom type. The reliability of the Persian version of the scale using the methods of internal consistency, test-retest, and inter-rater reliability were 0.83, 0.88, and 0.87, respectively [15]. The reliability of the positive symptoms in the Iranian culture was calculated to be 0.77 using the test-retest method [16]. The Cronbach alpha was calculated to be 0.83 for the internal consistency of the positive symptoms [17].
The Scale to Assess Unawareness of Mental Disorders (SUMD)
It is designed by Ghaemi et al. with 9 items assessing 3 components of 1. insight into the symptoms of mental illness; 2. insight into the need for treatment; and 3. insight into the social consequences of the mental disorder symptoms [19]. The reliability and validity of the SUMD and its abridged version have been reported to be acceptable [20]. On this scale, the patients with better insight have lower scores. The Cronbach alpha was calculated to be 0.85 for the internal consistency of the SUMD, and the internal consistency coefficient was between 0.81 to 0.90 [21]. The inter-rater reliability coefficient in Iran was in the range of 0.73-0.93, and the improvement in the patients’ insight in the acute and recovery phases showed the construct validity of the scale [22].
The study protocol was approved by the Ethics Committee of Ardabil branch, Islamic Azad University presented to the Shafa Hospital, Rasht City, Iran. A total of 30 patients of the said center with schizophrenia were selected using the purposive sampling method and were divided into 2 groups of the experimental group and the control group using simple randomization. In the present study, the researcher played the roles of an influencer, participator in the therapeutic sessions, and observer. Then, the researcher provided necessary and clear explanations about the study objectives, method, and data confidentiality, and the patients’ main caregivers (parents, spouses) gave written informed consent. Following the establishment of the initial therapeutic relationship, the researcher explained the questionnaires to the participants. In the next step, the experimental group underwent collective trainings by the researcher twice a week at the hospital. At the same time, the control group did not receive any intervention. The medication was similar in both groups according to the instructions of the psychiatrist.
Then, both groups underwent a post-test after the end of the treatment course. To avoid sample drop in this study, efforts were made to increase the patients’ motives of increased function level, returning to the society, developing communication skills, reducing stress, increasing the ability to confront the illness symptoms, and preventing its recurrence, and there was no sample drop in this study due to the therapeutic relationship between the researcher and the patients. Data analysis was performed in SPSS software version 24 using the univariate analysis of variance in normal distribution and the non-parametric Kruskal-Wallis test for the variable which didn't follow the normal distribution.
Data analysis was performed in SPSS software version 24 using the univariate analysis of variance in normal distribution and the non-parametric Kruskal-Wallis test for the variable which didn't follow the normal distribution.
Results
Descriptive indices of demographic variables of the research groups are explained in Table 2.

In Table 3, mean and standard deviation indices of the positive/negative symptoms and insight total scores are presented separately for pre-test and post-test of illness management and control groups.
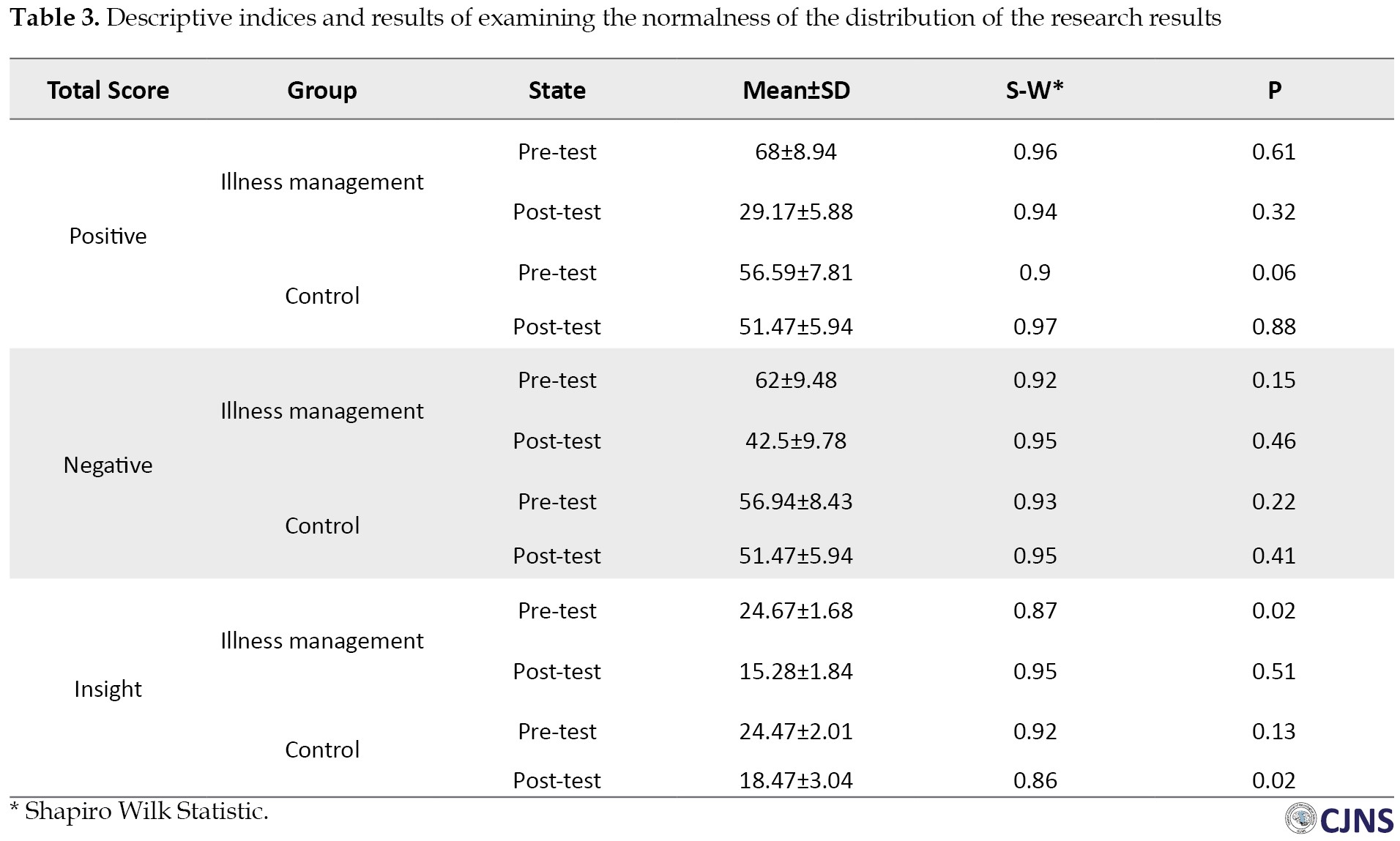
The Shapiro-Wilk test was used to test the normality of distribution. The results of this test indicate that the distribution of positive and negative symptoms total score is normal (P<0.05), and the total insight score does not follow the normal distribution (P<0.05).
Univariate analysis of variance was used to evaluate the total score of positive and negative symptoms, assuming homogeneity of groups. Because the distribution of total score of positive and negative symptoms in pre-test and post-test during Shapiro-Wilk test was normal and the slope of pre-test and post-test regression of the total score of positive and negative symptoms was obtained homogenous according to the significance of F statistic (P<0.05). Also, the variance of the dependent variable in the experimental and control groups was equal due to the insignificance of Levene’s statistic (P>0.05, F = 2.81 for positive symptoms and P>0.05, F = 0.91 for negative symptoms).
The results of univariate Analysis of Variance (ANOVA) to examine the difference between the experimental and control groups in terms of positive and negative symptoms are presented in Table 4.

The Eta squared shows that the difference between the two groups in these variables is 0.546 for positive symptoms and 0.538 for negative symptoms. This means that experimental conditions have been effective in improving these variables.
Also, the modified means in Table 5 shows that experimental condition within 95% confidence is effective in reducing the positive and negative symptoms of patients.

Because of the non-normal distribution of total insight scores, the non-parametric Kruskal-Wallis test was used and the post-test results (Table 6) showed a significant difference between the two groups in the average rank of insight to positive and negative symptoms and total insight score components (P<0.05).

Discussion
The present study aimed to determine the effectiveness of illness management program on positive and negative symptoms in schizophrenic patients. The results indicated that illness management effectively decreased the positive and negative symptoms and improved insight into the disease of schizophrenic patients. Results of the present study are in line with findings of Nakamura et al. [24], Färdig et al. [25], Lin et al. [26], Bartels et al. [27], Egeland et al. [28], and Liberman and Kopelowicz [29]. In all of these studies, the illness management program for schizophrenic patients improved performance, reduced positive and negative symptoms, improved insight, reduced recurrence rates, and improved quality of life.
Various studies showed that self-management behaviors improved the therapeutic outcomes and treatment acceptance by helping patients in disease understanding and treatment and increasing the knowledge and skills of the patients and their caregivers for health maintaining and promotion. These behaviors include changes in lifestyle, decision-making on the present therapeutic methods that are appropriate to the social context of the patient, monitoring the activities, management of the signs and symptoms of the disease, and cooperation with the healthcare team. We can explain these findings by stating that the illness management program educated the patients to use their best ability to seek help from others in case of warning signs of the onset of a disease episode or recurrence. They learned that they could not diagnose the recurrence symptoms independently and seek help from a healthy person for timely diagnosis and subsequent discussion with the physician. These results suggest that the self-management program can decrease the positive symptoms, negative symptoms, and stress and prevent a recurrence. Since schizophrenia is a social disease, improvement of the patients’ insight into the condition leads to better treatment, reduced prevalence in the community, and decrease the destructive physical, mental, familial, social, and economic burden of the disease. Also, this study was performed in patients with extended hospital stays, so the generalization of the findings to the outpatients should be made with caution.
Conclusion
Illness management reduced the positive and negative symptoms of schizophrenic patients. This program enables the patient to be active in the treatment process, which reduces the treatment costs and increase the beneficial effects of the healing process. Therefore, it is suggested to provide illness management education to enhance the patients’ health after their release to improve their life quality.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Ardabil branch, Islamic Azad University (IR.IAU.ARDABIL.REC.1399.045). All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This article was extracted from the PhD. dissertation of first author at the Department of Psychology, Ardabil branch, Islamic Azad University (Code No. :119481960923099139891662).
Authors contributions
Investigation: Fatemeh Rangrazian and Azar Kiamarsi; Writing the original draft: Fatemeh Rangrazian; Supervision, writing, review, and editing: Azar Kiamarsi, Reza Kazemi; Methodology and final approval of the version to be submitted: Fatemeh Rangrazian, Azar Kiamarsi, and Reza Kazemi.
Conflict of interest
The authors declared no conflict of interest.
References
chizophrenia is a complex neuropsychological disorder affecting approximately 1% of the global population. The disease is characterized by hallucinations, delusions, disorganized behavior, and progressive cognitive impairments [1]. The outbreak of schizophrenia is similar among women and men, with women having a better prognosis and usually have a better social functioning before the disease onset [2]. The negative symptoms include affective flattening or blunting, poverty of speech or content of speech, thinking blocking or dysfunction, inappropriate grooming and hygiene, lack of motivation, lack of pleasure, social inattentiveness, cognitive impairments, and lack of attention. The positive symptoms include impaired perception, thinking, and behavior such as loosening of associations, hallucinations, bizarre behavior, and tangentially. Patients with positive symptoms usually have a better prognosis than patients with negative symptoms [3].
According to various studies, negative symptoms have a more severe effect on reducing the quality of life and functional disability in these patients than the positive symptoms [4]. Lack of insight into the disease is one of the most common symptoms of schizophrenia. The insight into the disease ranges from the initial awareness of the condition to a deep and reasonable understanding and emotional touch of the disease. Lack of insight is more common in schizophrenia than in other disorders. Also, it is highly involved in the disease prognosis and can lead to disease recurrence and an increased number of hospital admissions [5]. Impaired insight is associated with impairments in cognitive functions, self-awareness, empathy, and self-control, and poor cooperation for treatment, and subsequently forced hospitalization. Decreased insight is correlated with the psychopathology of the disease. The lack of insight leads to a lack of cooperation in treatment and subsequently persistence of the patients’ problems and the family/friends [6]. There is significant evidence that schizophrenic patients not only lack insight into their psychotic symptoms but also have neurocognitive disorders. The patients likely show low metacognitive awareness of the cognitive functions involved in the delusional symptoms [7]. Akbari and Saeidi found that psychosocial rehabilitation had a significant effect on reducing the negative symptoms and improving the social skills in patients with chronic schizophrenia [8]. Esmkhani et al. showed that the interventional programs aimed at improving treatment adherence could enhance the quality of life in schizophrenic patients [9]. Haji Aghaei et al. showed that psychological education of the family was effective in decreasing the symptom severity and recurrence of schizophrenia [10].
Illness management is a program with a combination of psychosocial interventions that helps patients have more control over their problems and also helps in disease management and supports recovery [11]. In general, self-management is a new type of education in caregiving for patients with chronic diseases. In this therapeutic method, the process of problem-solving is done by the patient, and the necessary coping skills are taught to the patient by the treatment team. Therefore, patients learn to control the complications by relying on their skills and self-confidence using problem-solving skills. Finally, the main goal in the self-management educational program is managing the illness by the patients themselves [12]. A study by Burlingame et al. showed that group therapy was effective in treating schizophrenic patients [13].
It seems that teaching illness management to schizophrenic patients needs further attention. Also, limited education has been provided to these patients in Iran. Few studies have been conducted on the Iranian society focusing on the illness management education among these patients, and there is a need for such research in this field. Therefore, the present study aimed to investigate the effectiveness of the illness management program on the positive symptoms, negative symptoms, and insight of schizophrenic patients.
Materials and Methods
This present study was a quasi-experimental study with a pre-test, post-test design and a control group. The study population consisted of all the schizophrenic patients (n=796) admitted to the Shafa Hospital, Rasht City, from March 2019 to April 2020. A total of 30 patients were selected using the convenient sampling method in a purposeful manner and randomly divided into 2 groups of the experimental group and the control group, with 15 patients in each group. The pre-test was performed in both groups. Then, the experimental group underwent the intervention of illness management in 20 sessions, each with 90 minutes duration (Table 1), twice a week as group therapy in the hospital.
.jpg)
During this time, both groups received medication as directed by a psychiatrist, while the control group did not undergo any psychological interventions. Finally, both groups underwent the post-test after the treatment course. A 4-question questionnaire on the precision of illness management therapy was prepared with yes/no answers to examine the validity of the illness management therapy, and 6 assessors (therapists) answered the questions. The coefficient of agreement between the answers of the 6 assessors was then calculated as being 0.894 (P<0.05).
The inclusion criteria included the diagnosis of schizophrenia by a psychiatrist, being in the schizophrenia chronic phase, being affected by the disease for at least 2 years, and age from 20 to 45 years old. Also, the exclusion criteria included receiving another type of psychotherapy simultaneously, being absent for more than 3 sessions, and treatment cessation.
Study tools
The Scale for the Assessment of Negative Symptoms (SANS)
It is designed and standardized by Andreasen et al. The Scale for the Assessment of Negative Symptoms (SANS) scale has 24 items assessing 5 classes of negative symptoms of schizophrenia, including affective flattening or blunting, poverty of speech, avolition, apathy, lack of pleasure, social inattentiveness, and lack of attention [14]. A general question assesses the set of related symptoms at the end of each group. The answers are scored on a 6-point scale ranging from 0 for the absence of symptoms to 5 states of symptom severity. The higher the score of the patients, the severer their symptoms would be. The questionnaire is filled by the researcher using the information obtained from questioning the patient. The reliability values of the Persian version of the scale using the methods of internal consistency, test-retest, and inter-rater reliability were found as 0.94, 0.92, and 0.89, respectively [15]. The reliability of the negative symptoms in the Iranian culture was calculated to be 0.78 using the methods test-retest [16]. The Cronbach alpha was calculated to be 0.81 for the internal consistency of the negative symptoms [17].
The Scale for the Assessment of Positive Symptoms (SAPS)
It is also designed by Andreasen et al. The scale has 30 items assessing 4 groups of positive symptoms: hallucinations, delusions, bizarre behaviors, and formal thought disorder [18]. This tool can also cover the months before the time of evaluation by considering a suitable duration. The questionnaire is filled by the researcher using a standard clinical interview, in which there should be a 5-10-minute conversation about a neutral topic with the patient for evaluating the speech and response style to find a significant abstract thought disorder. Also, other sources such as direct observation and reports of the family and nurses can be used. The answers are scored on a 6-point scale ranging from 0 for the absence of the symptoms to 5 as the most severe. The higher the scores of the patients, the severer their symptoms would be. The last item of each group needs an overall score on the nature and severity of the certain symptom type. The reliability of the Persian version of the scale using the methods of internal consistency, test-retest, and inter-rater reliability were 0.83, 0.88, and 0.87, respectively [15]. The reliability of the positive symptoms in the Iranian culture was calculated to be 0.77 using the test-retest method [16]. The Cronbach alpha was calculated to be 0.83 for the internal consistency of the positive symptoms [17].
The Scale to Assess Unawareness of Mental Disorders (SUMD)
It is designed by Ghaemi et al. with 9 items assessing 3 components of 1. insight into the symptoms of mental illness; 2. insight into the need for treatment; and 3. insight into the social consequences of the mental disorder symptoms [19]. The reliability and validity of the SUMD and its abridged version have been reported to be acceptable [20]. On this scale, the patients with better insight have lower scores. The Cronbach alpha was calculated to be 0.85 for the internal consistency of the SUMD, and the internal consistency coefficient was between 0.81 to 0.90 [21]. The inter-rater reliability coefficient in Iran was in the range of 0.73-0.93, and the improvement in the patients’ insight in the acute and recovery phases showed the construct validity of the scale [22].
The study protocol was approved by the Ethics Committee of Ardabil branch, Islamic Azad University presented to the Shafa Hospital, Rasht City, Iran. A total of 30 patients of the said center with schizophrenia were selected using the purposive sampling method and were divided into 2 groups of the experimental group and the control group using simple randomization. In the present study, the researcher played the roles of an influencer, participator in the therapeutic sessions, and observer. Then, the researcher provided necessary and clear explanations about the study objectives, method, and data confidentiality, and the patients’ main caregivers (parents, spouses) gave written informed consent. Following the establishment of the initial therapeutic relationship, the researcher explained the questionnaires to the participants. In the next step, the experimental group underwent collective trainings by the researcher twice a week at the hospital. At the same time, the control group did not receive any intervention. The medication was similar in both groups according to the instructions of the psychiatrist.
Then, both groups underwent a post-test after the end of the treatment course. To avoid sample drop in this study, efforts were made to increase the patients’ motives of increased function level, returning to the society, developing communication skills, reducing stress, increasing the ability to confront the illness symptoms, and preventing its recurrence, and there was no sample drop in this study due to the therapeutic relationship between the researcher and the patients. Data analysis was performed in SPSS software version 24 using the univariate analysis of variance in normal distribution and the non-parametric Kruskal-Wallis test for the variable which didn't follow the normal distribution.
Data analysis was performed in SPSS software version 24 using the univariate analysis of variance in normal distribution and the non-parametric Kruskal-Wallis test for the variable which didn't follow the normal distribution.
Results
Descriptive indices of demographic variables of the research groups are explained in Table 2.

In Table 3, mean and standard deviation indices of the positive/negative symptoms and insight total scores are presented separately for pre-test and post-test of illness management and control groups.
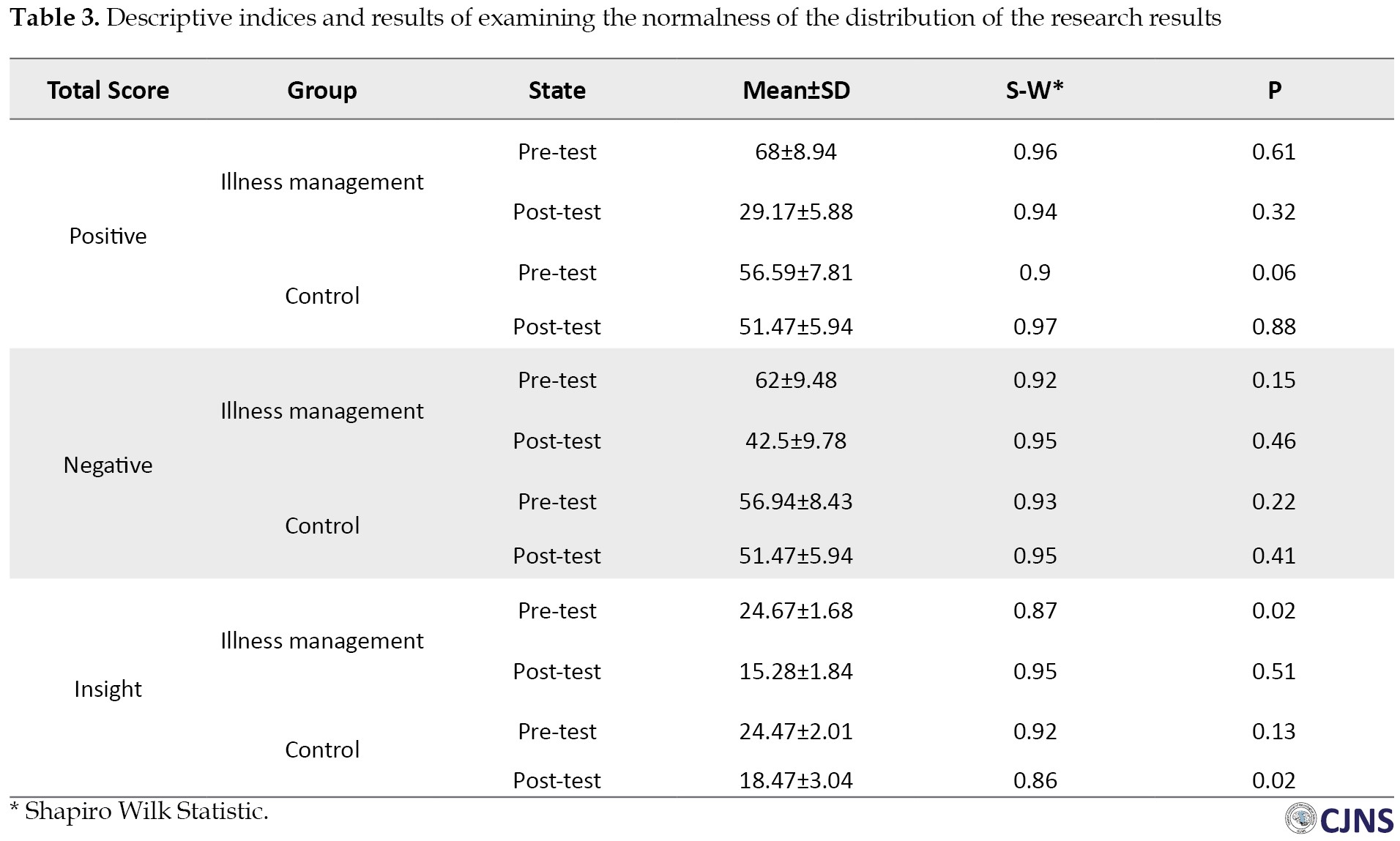
The Shapiro-Wilk test was used to test the normality of distribution. The results of this test indicate that the distribution of positive and negative symptoms total score is normal (P<0.05), and the total insight score does not follow the normal distribution (P<0.05).
Univariate analysis of variance was used to evaluate the total score of positive and negative symptoms, assuming homogeneity of groups. Because the distribution of total score of positive and negative symptoms in pre-test and post-test during Shapiro-Wilk test was normal and the slope of pre-test and post-test regression of the total score of positive and negative symptoms was obtained homogenous according to the significance of F statistic (P<0.05). Also, the variance of the dependent variable in the experimental and control groups was equal due to the insignificance of Levene’s statistic (P>0.05, F = 2.81 for positive symptoms and P>0.05, F = 0.91 for negative symptoms).
The results of univariate Analysis of Variance (ANOVA) to examine the difference between the experimental and control groups in terms of positive and negative symptoms are presented in Table 4.

The Eta squared shows that the difference between the two groups in these variables is 0.546 for positive symptoms and 0.538 for negative symptoms. This means that experimental conditions have been effective in improving these variables.
Also, the modified means in Table 5 shows that experimental condition within 95% confidence is effective in reducing the positive and negative symptoms of patients.

Because of the non-normal distribution of total insight scores, the non-parametric Kruskal-Wallis test was used and the post-test results (Table 6) showed a significant difference between the two groups in the average rank of insight to positive and negative symptoms and total insight score components (P<0.05).

Discussion
The present study aimed to determine the effectiveness of illness management program on positive and negative symptoms in schizophrenic patients. The results indicated that illness management effectively decreased the positive and negative symptoms and improved insight into the disease of schizophrenic patients. Results of the present study are in line with findings of Nakamura et al. [24], Färdig et al. [25], Lin et al. [26], Bartels et al. [27], Egeland et al. [28], and Liberman and Kopelowicz [29]. In all of these studies, the illness management program for schizophrenic patients improved performance, reduced positive and negative symptoms, improved insight, reduced recurrence rates, and improved quality of life.
Various studies showed that self-management behaviors improved the therapeutic outcomes and treatment acceptance by helping patients in disease understanding and treatment and increasing the knowledge and skills of the patients and their caregivers for health maintaining and promotion. These behaviors include changes in lifestyle, decision-making on the present therapeutic methods that are appropriate to the social context of the patient, monitoring the activities, management of the signs and symptoms of the disease, and cooperation with the healthcare team. We can explain these findings by stating that the illness management program educated the patients to use their best ability to seek help from others in case of warning signs of the onset of a disease episode or recurrence. They learned that they could not diagnose the recurrence symptoms independently and seek help from a healthy person for timely diagnosis and subsequent discussion with the physician. These results suggest that the self-management program can decrease the positive symptoms, negative symptoms, and stress and prevent a recurrence. Since schizophrenia is a social disease, improvement of the patients’ insight into the condition leads to better treatment, reduced prevalence in the community, and decrease the destructive physical, mental, familial, social, and economic burden of the disease. Also, this study was performed in patients with extended hospital stays, so the generalization of the findings to the outpatients should be made with caution.
Conclusion
Illness management reduced the positive and negative symptoms of schizophrenic patients. This program enables the patient to be active in the treatment process, which reduces the treatment costs and increase the beneficial effects of the healing process. Therefore, it is suggested to provide illness management education to enhance the patients’ health after their release to improve their life quality.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Ardabil branch, Islamic Azad University (IR.IAU.ARDABIL.REC.1399.045). All study procedures were done in compliance with the ethical guidelines of the 2013 version of the Declaration of Helsinki.
Funding
This article was extracted from the PhD. dissertation of first author at the Department of Psychology, Ardabil branch, Islamic Azad University (Code No. :119481960923099139891662).
Authors contributions
Investigation: Fatemeh Rangrazian and Azar Kiamarsi; Writing the original draft: Fatemeh Rangrazian; Supervision, writing, review, and editing: Azar Kiamarsi, Reza Kazemi; Methodology and final approval of the version to be submitted: Fatemeh Rangrazian, Azar Kiamarsi, and Reza Kazemi.
Conflict of interest
The authors declared no conflict of interest.
References
- Mohammadi A, Bahrami E, Hatef B, Kargar M. [Effectiveness of neurofeedback treatment on empathy and delusional beliefs in patients with Schizophrenia and Bipolar Disorder (Persian)]. J Mil Med. 2018; 20(2):231-41. http://militarymedj.ir/article-1-1859-en.html
- Sadeghi Babokani Z, Ghazanfari A, Ahmadi R, Chorami M. [The Comparison of the effectiveness of behavioral activation and psychosocial rehabilitation on verbal mental cognitive functions, abstraction and attention in women with Chronic Schizophrenia (Persian)]. Psychol Stud. 2020; 15(4):91-108. https://psychstudies.alzahra.ac.ir/article_4661_af9b542b083a00c3914ec0d52194036c.pdf
- Sadock BJ, Sadock VA. Kaplan & Sadock’s pocket handbook of clinical psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. https://www.amazon.com/Kaplan-Sadocks-Handbook-Clinical-Psychiatry/dp/1605472646
- Mojtabaei M, Hematyar Naghne M. [Effectiveness of cognitive behavioral group therapy in reducing positive and negative symptoms of Schizophrenia (Persian)]. J Appl EnvironBiol Sci. 2015; 5(8):304-13. http://www.textroad.com/pdf/JAEBS/J.%20Appl.%20Environ.%20Biol.%20Sci.,%205(8)304-313,%202015.pdf
- Ebrahimi H, Namdar H. [Relationship between insights into the disease with compliance in schizophrenic patients (Persian)]. Nurs Midwifery J. 2014; 12(5):354-60. http://unmf.umsu.ac.ir/article-1-1637-en.html
- Sadock BJ, Sadocks VA, Ruiz P. Summary of Kaplan and Zadok Psychiatry Volume 1 [F Rzaee, Persian trans.]. Tehran: Arjmand publisher; 2015. https://www.arjmandpub.com/Book/1209
- Krężołek M, Pionke R, Banaszak B, Kokoszka A, Gawęda Ł. The relationship between jumping to conclusions and neuropsychological functioning in schizophrenia. Psychiatry Res. 2019; 273:443-9. [DOI:10.1016/j.psychres.2019.01.035] [PMID]
- Akbari M, saeidi S. [The effectiveness of psychosocial rehabilitation in reducing negative symptoms and improving social skills of chronic Schizophrenia Patients (Persian)]. Shenakht J Psychol Psychiatr. 2017; 4(3):21-35. http://shenakht.muk.ac.ir/article-1-319-fa.html
- Esmkhani M, Ahangarzadeh Rezaei S, khalkhali H. [the effect of adherence to treatment intervention porgram on the quality of life of schizophrenia patients (Persian)]. Nurs Midwifery J. 2017; 15(8):595-604. http://unmf.umsu.ac.ir/article-1-3157-fa.html
- Haji Aghaei N, Sheikhi MR, Zeighami R, Alipour M. [Follow up of the impact of family-centered psychoeducation based on Atkinson and Coia’s model on the relapse and severity of symptoms in Schizophrenia (Persian)]. Iran J Psychiatr Nurs. 2017; 5(4):27-33. [DOI:10.21859/ijpn-05044]
- Roosenschoon BJ, Mulder CL, Deen ML, van Weeghel J. Effectiveness of Illness Management and Recovery (IMR) in the Netherlands: a randomised clinical trial. BMC Psychiatry. 2016; 16:73. [DOI:10.1186/s12888-016-0774-0] [PMID] [PMCID]
- Jamshidi F, Tohidi S, Shayan A. [Comparison of the effect of Community Re-entry Program (CRP) and conventional psychotherapy programs on symptoms severity and communication and interaction skills of Persons with Severe Mental Disorders (Persian)]. Iran J Rehabil Res. 2017; 3(4):21-8. [DOI:10.21859/ijrn-03043]
- Burlingame GM, Svien H, Hoppe L, Hunt I, Rosendahl J. Group therapy for schizophrenia: A meta-analysis. Psychotherapy (Chic). 2020; 57(2):219-36. [DOI:10.1037/pst0000293] [PMID]
- Andreasen NC, Flaum M, Swayze VW, Tyrrell G, Arndt S. Positive and negative symptoms in schizophrenia. A critical reappraisal. Arch Gen Psychiatry 1990; 47(7):615-21. [DOI:10.1001/archpsyc.1990.01810190015002] [PMID]
- Yasrebi K, Jazayeri AR, Pourshahbaz A, Dolatshahi B. [The effectiveness of psychosocial rehabilitation in reducing negative symptoms and improving social skills of Chronic Schizophrenia Patients (Persian)]. Iran J psychiatr Clin Psychol. 2009; 14(4):363-70. http://ijpcp.iums.ac.ir/browse.php?a_code=A-10-1-315&sid=1&slc_lang=en
- Zad Mohammadi A, Haidari M, Majd Timure M. [The effect of music therapy on the negative and positive symptoms of Mentally Ill Patients (Persian)]. Psychology. 2002; 3(5):231-249. https://www.sid.ir/fa/journal/ViewPaper.aspx?id=21352
- Hasani J, Hadianfard H. [The relationship between positive and negative symptoms of schizophrenia with the maintenance of attention (Persian)]. Adv Cogn Sci. 2003; 5(3):24-33. http://icssjournal.ir/article-1-245-fa.html
- Andreasen NC. Positive versus negative schizophrenia: criteria and validation. In Clinical Psychopathology Nomenclature and Classification. Boston, MA: Springer; 1985. [DOI:10.1007/978-1-4899-5049-9_79]
- Ghaemi SN, Boiman E, Goodwin FK. [Insight and outcome in bipolar, unipolar, and anxiety disorders (Persian)]. Compr Psychiatry. 2000; 41(3):167-71. [DOI:10.1016/S0010-440X(00)90043-9]
- Shad MU, Tamminga CA, Cullum M, Haas GL, Keshavan MS. Insight and frontal cortical function in schizophrenia: a review. Schizophr Res. 2006; 86(1-3):54-70. [DOI:10.1016/j.schres.2006.06.006] [PMID]
- Michel P, Baumstarck K, Auquier P, Amador X, Dumas R, Fernandez J, et al. Psychometric properties of the abbreviated version of the Scale to Assess Unawareness in Mental Disorder in schizophrenia. BMC Psychiatry. 2013; 13:229. [DOI:10.1186/1471-244X-13-229] [PMID] [PMCID]
- Mokhtarzadeh A, Ghoreishizadeh S, Pezeshki MZ, Ranjbar KF, Mohammadi R, Mousavi A, et al. [Reliability and validity of abridged version of the farsi version of scale to Assess Unawareness of Mental Disorders (SUMD) in psychotic mania (Persian)]. Iran J Psychiatry Clinical Psychology. 2010; 16(3):181-6. http://ijpcp.iums.ac.ir/article-1-1082-en.html
- Mueser KT, Meyer PS, Penn DL, Clancy R, Clancy DM, Salyers MP. The illness management and recovery program: rationale, development, and preliminary findings. Schizophr Bull. 2006; 32 (Suppl 1):S32-43. [DOI:10.1093/schbul/sbl022] [PMID] [PMCID]
- Nakamura R, Asami T, Yoshimi A, Kato D, Fujita E, Takaishi M, et al. Clinical and brain structural effects of the Illness Management and Recovery program in middle-aged and older patients with schizophrenia. Psychiatry Clin Neurosci. 2019; 73(12):731-7. [DOI:10.1111/pcn.12919] [PMID]
- Färdig R, Fredriksson A, Lewander T, Melin L, Mueser KT. Neurocognitive functioning and outcome of the Illness Management and Recovery Program for clients with schizophrenia and schizoaffective disorder. Nord J Psychiatry. 2016; 70(6):430-5. [DOI:10.3109/08039488.2016.1146797] [PMID]
- Lin EC, Shao WC, Chan CH, Shiau S, Wang HS, Huang SC. A pilot study of an illness management and recovery program in discharged patients with schizophrenia. J Nurs Res. 2013; 21(4):270-7. [DOI:10.1097/jnr.0000000000000004] [PMID]
- Bartels SJ, Pratt SI, Mueser KT, Naslund JA, Wolfe RS, Santos M, et al. Integrated IMR for psychiatric and general medical illness for adults aged 50 or older with serious mental illness. Psychiatr Serv. 2014; 65(3):330-7. [DOI:10.1176/appi.ps.201300023] [PMID] [PMCID]
- Egeland KM, Ruud T, Ogden T, Färdig R, Lindstrøm JC, Heiervang KS. How to implement Illness Management and Recovery (IMR) in mental health service settings: evaluation of the implementation strategy. Int J Ment Health Syst. 2017; 11(1):1-11. [DOI:10.1186/s13033-017-0120-z] [PMID] [PMCID]
- Liberman RP, Kopelowicz A. Training skills for illness self-management in the rehabilitation of schizophrenia: a family-assisted program for Latinos in California. Salud Mental. 2009; 32(2):93-105. http://www.scielo.org.mx/scielo.php?pid=S0185-33252009000200002&script=sci_arttext&tlng=en
Type of Study: Research |
Subject:
Special
Received: 2021/03/14 | Accepted: 2021/01/21 | Published: 2021/01/21
Received: 2021/03/14 | Accepted: 2021/01/21 | Published: 2021/01/21
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |