Mon, Feb 16, 2026
Volume 5, Issue 3 (Summer 2019)
Caspian J Neurol Sci 2019, 5(3): 118-126 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mousavi S M, Shabahang R, Khodadadi-Hassankiadeh N. The Effects of Acceptance and Commitment Therapy and Biofeedback on Chronic Psychosomatic Low Back Pain. Caspian J Neurol Sci 2019; 5 (3) :118-126
URL: http://cjns.gums.ac.ir/article-1-268-en.html
URL: http://cjns.gums.ac.ir/article-1-268-en.html
1- Department of Nursing and Midwifery, Faculty of nursing and midwifery, Rasht Branch, Islamic Azad University, Rasht, Iran
2- Department of Psychology, Faculty of Psychology and Educational Sciences, University of Tehran, Tehran, Iran
3- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.; Social Determinants of Health Research Center, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Psychology, Faculty of Psychology and Educational Sciences, University of Tehran, Tehran, Iran
3- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran.; Social Determinants of Health Research Center, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 1205 kb]
(1254 Downloads)
| Abstract (HTML) (3543 Views)
Full-Text: (1710 Views)
Introduction
ain is among the main causes of seeking medical help [1]. According to the International Association of Pain Studies, pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage”. Chronic pain is also defined as a pain with a duration of more than six months. The prevalence of chronic pain in the world is 5-33% [1-2]. Low back pain (LBP) is among the most common types of chronic pain. It is among the main causes of disability and absence from work and hence, imposes heavy financial burden on patients, healthcare systems, and communities [3]. It dramatically affects all aspects of life including daily activities, independence, cognitive and physical functions, work, relationships, parenting, and emotional and psychological well-being.
These problems, in turn, can cause confusion, restlessness, social isolation, social stigma, hopelessness, and anxiety even among people with good health and functional status [4]. Moreover, pain is associated with reduced quality of life (QOL) and depressive symptoms [5]. Psychosomatic form of low back pain is one of the prominent kind of low back pain. In fact, psychosomatic low back pain is used to mean a low back pain that is thought to be caused, or made worse, by mental factors [6].
There are different cognitive therapies for chronic pain management. These therapies include, but are not limited to, mind-body interventions, behavioral techniques, cognitive behavioral techniques, and acceptance and commitment therapy [7]. These therapies aim to help clients acquire abilities such as greater self-management, behavioral modification, and cognitive modification rather than direct pain eradication.
Acceptance and commitment therapy (ACT) is one of the cognitive therapies. It aims at helping clients develop greater psychological flexibility and thereby, have more valuable and satisfactory lives. ACT improves psychological flexibility through the six core processes of acceptance, cognitive defusion, contact with present moment, self as a context, values, and committed action.
Studies showed that the acceptance of pain was associated with better QOL among patients with LBP, better functional status among patients with rheumatoid arthritis, greater involvement in personal activities, better maintenance of functioning, high levels of psychological well-being, and lower levels of pain, pain-related distress, and disability [8-13].
Electromyographic (EMG) biofeedback is another psychological therapy. In this therapy, data about nerves, muscles, and autonomic activities are collected and processed using electronic devices and are provided to patients and physicians as audio or visual feedbacks. This method is used to manage LBP, headache, anxiety disorders, muscular injuries, and urinary incontinence [14].
Unlike most medical treatments, this method helps clients acquire greater knowledge about autonomic activities of the body and hence, helps them develop greater control over their bodies and functions [15]. Previous studies reported the effectiveness of biofeedback in reducing non-cardiac chest pain and managing regional pain syndrome and phantom pain [16-18].
However, there is a paucity of information regarding the effectiveness of ACT and biofeedback in managing chronic LBP. Thus, the present study was conducted to investigate and compare the effects of ACT and EMG biofeedback on pain severity and duration and QOL among women with chronic psychosomatic LBP.
Materials and Methods
This was a three-group Pre-test and post-test controlled quasi-experimental study. Study population consisted of all women with chronic psychosomatic LBP who referred from September 2016 to June 2017 to Rasht pain clinic, Rasht, Iran. According to the more prevalence and more presentation of low back pain in women [19], the study population consisted women with chronic psychosomatic LBP.
Moreover, lack of sufficient researches on women with chronic psychosomatic LBP is another reason for studying women population specifically. In this regard, thirty women with LBP were conveniently recruited and randomly allocated to three ten-person groups, namely an ACT group, a biofeedback group, and a control group.
Inclusion criteria were diagnosis of chronic psychosomatic LBP by an orthopedist or neurologist based on the criteria of the International Association of Pain Studies and considering psychological aspects of LBP [6, 20], an age of 23-34, educational level of secondary diploma or higher. Exclusion criteria were comorbid serious physical or mental problems [21], use of any psychological or counseling techniques during the study, use of psychiatric medications, history of referring to behavioral therapist during the last six months, and history of spinal cancer, spinal rheumatoid arthritis, spinal surgery, or other pathologic spinal conditions.
Study tools
Four instruments were used for data collection. The first was a demographic questionnaire with items on age, educational level, marital status, and the duration of suffering from LBP. The second instrument was the modified McGill pain questionnaire (MPQ). MPQ includes twenty sets of pain-related words in the four main dimensions of pain, namely sensory perception of pain, emotional perception of pain, cognitive evaluation of pain, and different types of pain. The modified version of MPQ includes three main parts.
The first part contains fifteen verbal descriptors of pain in two main groups of sensory (eleven items) and emotional (four items) descriptors. Each descriptor is rated as “No pain” (scored 0), “Mild pain” (scored 1), “Moderate pain” (scored 2), and “Severe pain” (scored 3). The second part of this questionnaire is a visual analogue scale for pain assessment.
Each intended client is asked to rate his/her pain from “No pain” (scored 0) to “Severest possible pain” or “Intolerable pain” (scored 10). The third part of MPQ relates to the present pain intensity which is rated as “No pain” (scored 0), “Mild” (scored 1), “Discomforting” (scored 2), “Distressing” (scored 3), “Horrible” (scored 4), and “Excruciating” (scored 5). The total score of the questionnaire is calculated through adding up the scores of these three main parts [22].
The SF-MPQ has been validated and appears to correlate well with the original long-form MPQ. SF-MPQ able to discriminate between different types of pain syndromes and it is sensitive to changes in pain brought about by therapies [23]. In the research of Dworkin et al. Cronbach’s alpha for SF-MPQ was 0.95 [22]. In Iran, the study of Tanhaee et al. provided evidence that supported the validity and reliability of the questionnaire [24].
The third study instrument was the world health organization quality of life-BREF (WHOQOL-BREF). This survey contains 26 items in four main domains of QOL, namely physical health (seven items), psychological health (six items), social health (three items), and environmental health (eight items) as well as two general items on QOL. Items 3, 4, and 26 are reversely scored. Higher scores indicate higher health [25].
Skevington, Lotfy, Connell, & WHOQOL group demonstrated the appropriate reliability and validity of the questionnaire. In the study of the Skevington et al. internal consistency by Cronbach’s alphas’ for domains and centers were 0.68 to 0.82 [26]. WHOQOL-BREF has been translated into nineteen languages and is used in different countries for QOL assessment. Nejat et al. translated it into Persian and confirmed that the Persian version has acceptable validity and reliability. The results of Nejat et al.’s study showed that the Cronbach’s alpha for physical health, psychological health, social health, and environmental health were 0.77, 0.77, 0.75, and 0.84, respectively [25].
The fourth study instrument was an EMG device (Biofeedback Procomb) used for EMG feedback. EMG turns electrical signals of motor neurons which induce muscle contraction into interpretable sounds or images. It is considered as a diagnostic method for evaluating the health status of both muscles and nerves. During electromyography, needle electrodes are inserted into a muscle in order to detect and transfer electrical signals and thereby, to record the electrical activity of the muscle.
In neural conduction test, a subtype of EMG, surface electrodes are attached to the skin in order to measure the velocity and the strength of the signals transmitted between two or more points. EMG findings are used to diagnose the different types of functional disorders of nerves, muscles, or neuromuscular junctions [27].
Procedure
The ACT intervention was individually provided to each participant in the ACT group in eight one-hour weekly sessions. The ACT protocol was developed based on Vowles and Sorrell’s book entitled, “Life with chronic pain: an acceptance-based approach (therapist guide and patient workbook)” [28, 29]. On the other hand, the EMG biofeedback protocol was provided to participants in the biofeedback group based on the protocol developed by the Biofeedback Society of California.
Accordingly, twelve twice-weekly 45-minutes biofeedback sessions were held for each participant. Thus, EMG biofeedback training to the back muscles was completed in six successive weeks. Besides ACT or biofeedback, participants in the two intervention groups received routine care services provided to all patients in the study setting which included physical exercise, corrective exercises, physical therapy, massage, and laser therapy. Participants in the control group received the same routine care services without any ACT or biofeedback interventions. Data collection was done for all participants in all three groups both before and after the study intervention.
Data analysis
The SPSS software V. 21 was used for data collection. Within-group comparisons were made through the paired-sample t-test, while between-group comparisons were made using the one-way analysis of variance as well as the Chi-square and Scheffe’s tests.
Results
The Mean±SD of participants’ age in the ACT, biofeedback, and control groups were 24.71±6.85, 27.43±11.54, and 33.43±14.81, respectively. Most participants in these groups were married. The duration of their LBP was 6.5±3.4 months, on average. There were no statistically significant differences among the study groups in terms of their demographic characteristics (P>0.05).
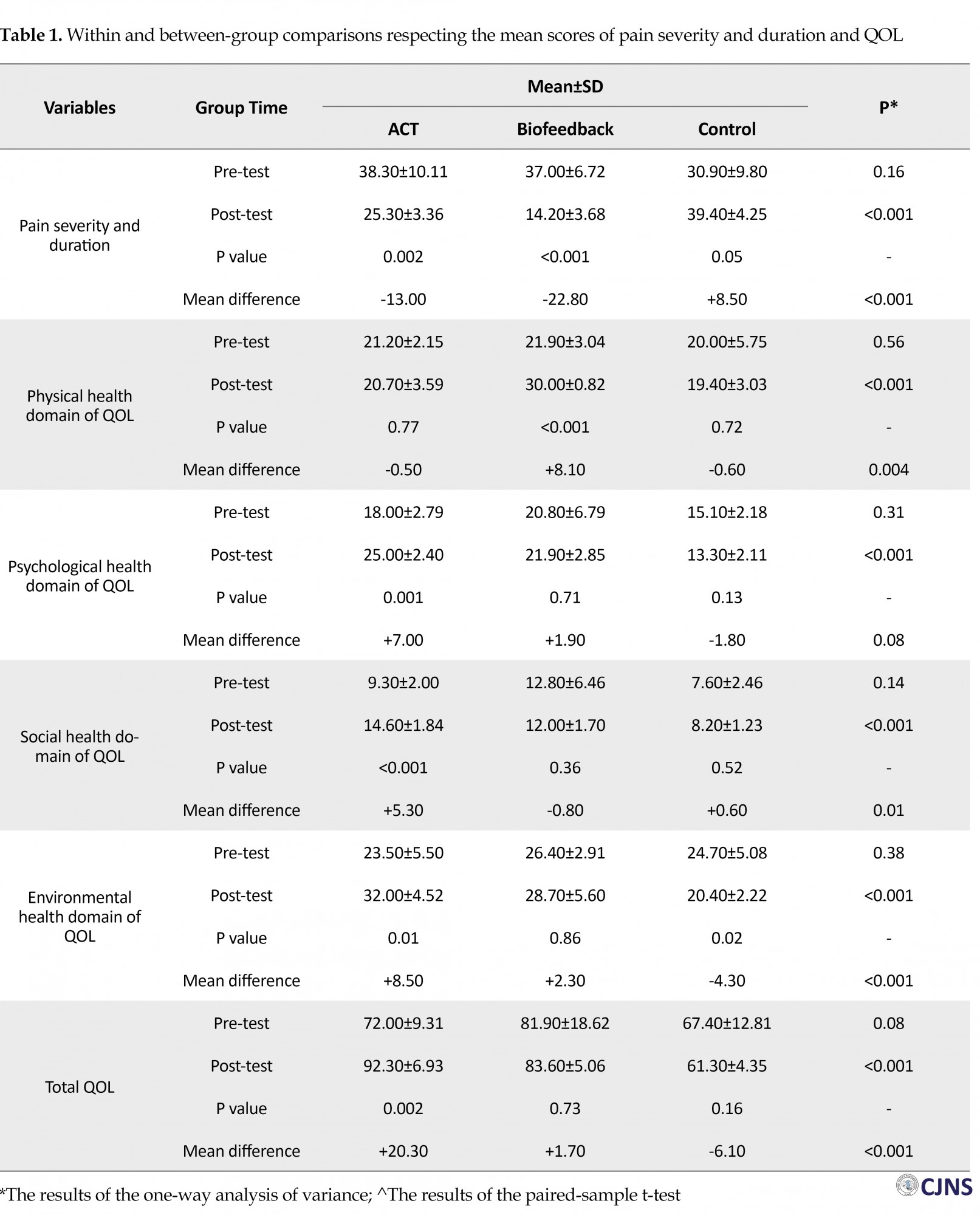
At pre-test, the groups did not significantly differ from each other in terms of the mean scores of pain severity and duration, physical health, psychological health, social health, environmental health, and total QOL (P>0.05). However, during the study, the mean score of pain severity and duration significantly decreased in the ACT (P=0.002) and the biofeedback (P<0.001) groups and significantly increased in the control group (P=0.05).
The post-test mean score of pain severity and duration in the biofeedback group (14.20±3.68) was significantly less than the ACT (25.30±3.36) and the control (39.40±4.25) groups (P<0.001). Moreover, the pre-test and post-test mean difference of pain severity and duration in the biofeedback group (-22.80) was significantly greater than the ACT (-13.0) and the control (+8.50) groups (P<0.001; Table 1). Thus, both ACT and biofeedback were effective in significantly reducing pain severity and duration though the effects of biofeedback on pain severity and duration were stronger than ACT.
ain is among the main causes of seeking medical help [1]. According to the International Association of Pain Studies, pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage”. Chronic pain is also defined as a pain with a duration of more than six months. The prevalence of chronic pain in the world is 5-33% [1-2]. Low back pain (LBP) is among the most common types of chronic pain. It is among the main causes of disability and absence from work and hence, imposes heavy financial burden on patients, healthcare systems, and communities [3]. It dramatically affects all aspects of life including daily activities, independence, cognitive and physical functions, work, relationships, parenting, and emotional and psychological well-being.
These problems, in turn, can cause confusion, restlessness, social isolation, social stigma, hopelessness, and anxiety even among people with good health and functional status [4]. Moreover, pain is associated with reduced quality of life (QOL) and depressive symptoms [5]. Psychosomatic form of low back pain is one of the prominent kind of low back pain. In fact, psychosomatic low back pain is used to mean a low back pain that is thought to be caused, or made worse, by mental factors [6].
There are different cognitive therapies for chronic pain management. These therapies include, but are not limited to, mind-body interventions, behavioral techniques, cognitive behavioral techniques, and acceptance and commitment therapy [7]. These therapies aim to help clients acquire abilities such as greater self-management, behavioral modification, and cognitive modification rather than direct pain eradication.
Acceptance and commitment therapy (ACT) is one of the cognitive therapies. It aims at helping clients develop greater psychological flexibility and thereby, have more valuable and satisfactory lives. ACT improves psychological flexibility through the six core processes of acceptance, cognitive defusion, contact with present moment, self as a context, values, and committed action.
Studies showed that the acceptance of pain was associated with better QOL among patients with LBP, better functional status among patients with rheumatoid arthritis, greater involvement in personal activities, better maintenance of functioning, high levels of psychological well-being, and lower levels of pain, pain-related distress, and disability [8-13].
Electromyographic (EMG) biofeedback is another psychological therapy. In this therapy, data about nerves, muscles, and autonomic activities are collected and processed using electronic devices and are provided to patients and physicians as audio or visual feedbacks. This method is used to manage LBP, headache, anxiety disorders, muscular injuries, and urinary incontinence [14].
Unlike most medical treatments, this method helps clients acquire greater knowledge about autonomic activities of the body and hence, helps them develop greater control over their bodies and functions [15]. Previous studies reported the effectiveness of biofeedback in reducing non-cardiac chest pain and managing regional pain syndrome and phantom pain [16-18].
However, there is a paucity of information regarding the effectiveness of ACT and biofeedback in managing chronic LBP. Thus, the present study was conducted to investigate and compare the effects of ACT and EMG biofeedback on pain severity and duration and QOL among women with chronic psychosomatic LBP.
Materials and Methods
This was a three-group Pre-test and post-test controlled quasi-experimental study. Study population consisted of all women with chronic psychosomatic LBP who referred from September 2016 to June 2017 to Rasht pain clinic, Rasht, Iran. According to the more prevalence and more presentation of low back pain in women [19], the study population consisted women with chronic psychosomatic LBP.
Moreover, lack of sufficient researches on women with chronic psychosomatic LBP is another reason for studying women population specifically. In this regard, thirty women with LBP were conveniently recruited and randomly allocated to three ten-person groups, namely an ACT group, a biofeedback group, and a control group.
Inclusion criteria were diagnosis of chronic psychosomatic LBP by an orthopedist or neurologist based on the criteria of the International Association of Pain Studies and considering psychological aspects of LBP [6, 20], an age of 23-34, educational level of secondary diploma or higher. Exclusion criteria were comorbid serious physical or mental problems [21], use of any psychological or counseling techniques during the study, use of psychiatric medications, history of referring to behavioral therapist during the last six months, and history of spinal cancer, spinal rheumatoid arthritis, spinal surgery, or other pathologic spinal conditions.
Study tools
Four instruments were used for data collection. The first was a demographic questionnaire with items on age, educational level, marital status, and the duration of suffering from LBP. The second instrument was the modified McGill pain questionnaire (MPQ). MPQ includes twenty sets of pain-related words in the four main dimensions of pain, namely sensory perception of pain, emotional perception of pain, cognitive evaluation of pain, and different types of pain. The modified version of MPQ includes three main parts.
The first part contains fifteen verbal descriptors of pain in two main groups of sensory (eleven items) and emotional (four items) descriptors. Each descriptor is rated as “No pain” (scored 0), “Mild pain” (scored 1), “Moderate pain” (scored 2), and “Severe pain” (scored 3). The second part of this questionnaire is a visual analogue scale for pain assessment.
Each intended client is asked to rate his/her pain from “No pain” (scored 0) to “Severest possible pain” or “Intolerable pain” (scored 10). The third part of MPQ relates to the present pain intensity which is rated as “No pain” (scored 0), “Mild” (scored 1), “Discomforting” (scored 2), “Distressing” (scored 3), “Horrible” (scored 4), and “Excruciating” (scored 5). The total score of the questionnaire is calculated through adding up the scores of these three main parts [22].
The SF-MPQ has been validated and appears to correlate well with the original long-form MPQ. SF-MPQ able to discriminate between different types of pain syndromes and it is sensitive to changes in pain brought about by therapies [23]. In the research of Dworkin et al. Cronbach’s alpha for SF-MPQ was 0.95 [22]. In Iran, the study of Tanhaee et al. provided evidence that supported the validity and reliability of the questionnaire [24].
The third study instrument was the world health organization quality of life-BREF (WHOQOL-BREF). This survey contains 26 items in four main domains of QOL, namely physical health (seven items), psychological health (six items), social health (three items), and environmental health (eight items) as well as two general items on QOL. Items 3, 4, and 26 are reversely scored. Higher scores indicate higher health [25].
Skevington, Lotfy, Connell, & WHOQOL group demonstrated the appropriate reliability and validity of the questionnaire. In the study of the Skevington et al. internal consistency by Cronbach’s alphas’ for domains and centers were 0.68 to 0.82 [26]. WHOQOL-BREF has been translated into nineteen languages and is used in different countries for QOL assessment. Nejat et al. translated it into Persian and confirmed that the Persian version has acceptable validity and reliability. The results of Nejat et al.’s study showed that the Cronbach’s alpha for physical health, psychological health, social health, and environmental health were 0.77, 0.77, 0.75, and 0.84, respectively [25].
The fourth study instrument was an EMG device (Biofeedback Procomb) used for EMG feedback. EMG turns electrical signals of motor neurons which induce muscle contraction into interpretable sounds or images. It is considered as a diagnostic method for evaluating the health status of both muscles and nerves. During electromyography, needle electrodes are inserted into a muscle in order to detect and transfer electrical signals and thereby, to record the electrical activity of the muscle.
In neural conduction test, a subtype of EMG, surface electrodes are attached to the skin in order to measure the velocity and the strength of the signals transmitted between two or more points. EMG findings are used to diagnose the different types of functional disorders of nerves, muscles, or neuromuscular junctions [27].
Procedure
The ACT intervention was individually provided to each participant in the ACT group in eight one-hour weekly sessions. The ACT protocol was developed based on Vowles and Sorrell’s book entitled, “Life with chronic pain: an acceptance-based approach (therapist guide and patient workbook)” [28, 29]. On the other hand, the EMG biofeedback protocol was provided to participants in the biofeedback group based on the protocol developed by the Biofeedback Society of California.
Accordingly, twelve twice-weekly 45-minutes biofeedback sessions were held for each participant. Thus, EMG biofeedback training to the back muscles was completed in six successive weeks. Besides ACT or biofeedback, participants in the two intervention groups received routine care services provided to all patients in the study setting which included physical exercise, corrective exercises, physical therapy, massage, and laser therapy. Participants in the control group received the same routine care services without any ACT or biofeedback interventions. Data collection was done for all participants in all three groups both before and after the study intervention.
Data analysis
The SPSS software V. 21 was used for data collection. Within-group comparisons were made through the paired-sample t-test, while between-group comparisons were made using the one-way analysis of variance as well as the Chi-square and Scheffe’s tests.
Results
The Mean±SD of participants’ age in the ACT, biofeedback, and control groups were 24.71±6.85, 27.43±11.54, and 33.43±14.81, respectively. Most participants in these groups were married. The duration of their LBP was 6.5±3.4 months, on average. There were no statistically significant differences among the study groups in terms of their demographic characteristics (P>0.05).
At pre-test, the groups did not significantly differ from each other in terms of the mean scores of pain severity and duration, physical health, psychological health, social health, environmental health, and total QOL (P>0.05). However, during the study, the mean score of pain severity and duration significantly decreased in the ACT (P=0.002) and the biofeedback (P<0.001) groups and significantly increased in the control group (P=0.05).
The post-test mean score of pain severity and duration in the biofeedback group (14.20±3.68) was significantly less than the ACT (25.30±3.36) and the control (39.40±4.25) groups (P<0.001). Moreover, the pre-test and post-test mean difference of pain severity and duration in the biofeedback group (-22.80) was significantly greater than the ACT (-13.0) and the control (+8.50) groups (P<0.001; Table 1). Thus, both ACT and biofeedback were effective in significantly reducing pain severity and duration though the effects of biofeedback on pain severity and duration were stronger than ACT.
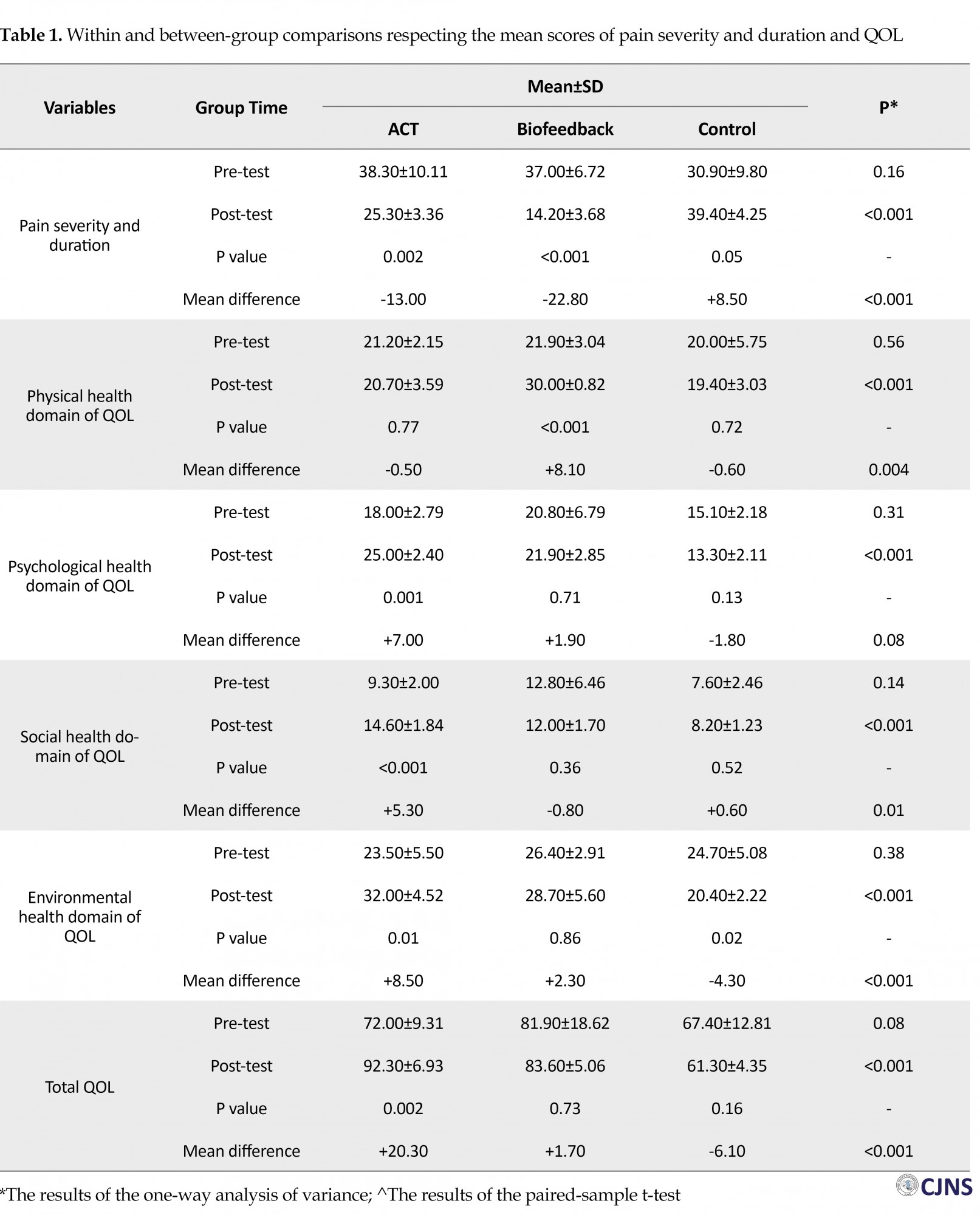
The meanscore of the physical health domain of QOL in the biofeedback group significantly increased during the study (P<0.001), while it did not significantly change in the ACT (P=0.77) and the control (P=0.72) groups. Therefore, the post-test Mean±SD score of physical health in the biofeedback group (30.00±0.82) was significantly greater than the ACT (20.70±3.59) and the control (19.40±3.03) groups (P<0.001).
The pre-tes and post-test mean difference of physical health in the biofeedback group (+8.10) was significantly greater than the ACT (-0.50) and the control (-0.60) groups (P = 0.004; Table 1). These findings denote that biofeedback had significant positive effects on the physical health domain of QOL, while ACT had no significant effects on it.
The mean score of the psychological health domain of QOL significantly increased in the ACT group (P=0.001), while it did not significantly change in the biofeedback (P=0.71) and the control (P=0.13) groups. Thus, the post-test Mean±SD score of psychological health in the ACT group (25.00±2.40) was significantly greater than the biofeedback (21.90±2.85) and the control (13.30±2.11) groups (P<0.001). However, there was no statistically significant difference among the groups in terms of the pre-test and post-test mean difference of psychological health mean score (P=0.08; Table 1).
These findings imply the effectiveness of ACT and the ineffectiveness of biofeedback in improving the psychological health domain of QOL among women with chronic LBP. The mean score of the social health domain of QOL significantly increased in the ACT group (P<0.001), but did not significantly change in the biofeedback (P=0.36) and the control (P=0.52) groups. Hence, the post-test mean score of social health in the ACT group (14.60±1.84) was significantly greater than the biofeedback (P=12.00±1.70) and the control (8.20±1.23) groups.
Moreover, the pre-test and post-test mean difference of the social health mean score in the ACT group (+5.30) was significantly greater than the biofeedback (-0.80) and the control (+0.60) groups (P=0.01; Table 1). These findings altogether denote the positive effects of ACT and the insignificant effects of biofeedback on the social health domain of QOL.
The mean score of the environmental health domain of QOL significantly increased in the ACT group (P=0.01); however, it did not significantly change in the biofeedback group (P=0.86) and significantly decreased in the control group (P=0.02). The post-test mean score of environmental health in the ACT group (32.00±4.52) was significantly greater than the biofeedback (28.70±5.60) and the control (20.40±2.22) groups (P<0.001).
The pre-test and post-test mean difference of the mean score of environmental health in the ACT group (+8.50) was also significantly greater than the biofeedback (+2.30) and the control (-4.30) groups (P<0.001; Table 1). Based on these findings, ACT was effective and biofeedback was ineffective in significantly improving the environmental health domain of QOL among women with chronic LBP.
Although the total mean score of QOL significantly increased in the ACT group (P=0.002), it showed no statistically significant change in the biofeedback (P=0.73) and the control (P=0.16) groups. Consequently, the post-test mean score of QOL in the ACT group (92.30±6.93) was significantly greater than the biofeedback (83.60±5.06) and the control (61.30±4.35) groups (P<0.001).
In addition, the Pre-test and post-test mean score of the QOL mean score in the ACT group (+20.30) was significantly greater than the biofeedback (+1.70) and the control (-6.10) groups (P < 0.001; Table 1). These findings indicate that ACT had significant effects and biofeedback had insignificant effects on QOL among women with chronic LBP.
Discussion
The aim of this study was to investigate the effects of ACT and biofeedback on pain severity and duration and QOL among women with chronic psychosomatic LBP. Findings revealed that both ACT and biofeedback significantly reduced pain severity and duration among these women. Of course, there was no significant difference between these two therapies respecting their effects on pain severity and duration.
In line with these findings, a former study reported that ACT significantly reduced pain among women with chronic headache [30]. One reason behind the positive effects of biofeedback is that it contains a relaxation component. Relaxation techniques such as diaphragmatic breathing and progressive muscular relaxation can significantly reduce pain. Besides, during biofeedback, patients learn how to deliberately identify and manage LBP symptoms and prevent their exacerbation.
Study findings also indicated the positive effects of both ACT and biofeedback on QOL among women with chronic psychosomatic LBP. Our literature search revealed that none of the previous studies had compared the effects of these two therapies on QOL among patients with LBP. However, several studies had investigated the effects of either ACT or biofeedback on QOL.
For instance, a study reported that the acceptance of LBP following ACT use significantly improved QOL among patients with chronic LBP [8]. Several other studies also reported the positive effects of ACT on QOL [31-34], anxiety symptoms, psychological strains and distress [32-34], and depression [24]. Other studies revealed that mindfulness-based stress reduction was effective in alleviating stress and improving QOL and physical, subjective, spiritual, and emotional well-being [35-37].
Therapies like ACT and biofeedback help patients evaluate physiologic reactions inside their bodies and then, attempt to control them [36]. ACT also exerts its positive effects on different patient outcomes, such as anxiety and depression, through improving psychological flexibility and deliberate attention to the present moment [32, 39]. ACT contains six core processes which can promote psychological flexibility and committed behavioral performance.
Self as a context is one of these processes. It makes clients aware of their thoughts, feelings, and desires and requires them to avoid controlling or avoiding them. After using this process, clients are subjected to another core process of ACT, i.e. cognitive defusion, which helps modify reactions to behaviors. In fact, instead of focusing on the validation or challenging of the thoughts, ACT focuses on performances.
Another core process of ACT is the acceptance of unavoidable situations like pain. Contact with present moment, determination of personal values, and committed action are the other core processes of ACT. Contact with present moment helps clients focus on the present moment instead of struggling with the past or probable events in the future. These six core processes improve psychological flexibility and QOL [8].
Patients with chronic LBP usually have limitations in doing their activities; thus, they may experience mood problems, reduced self-confidence, loss of employment, concerns over poor health status, and fear over attending social events. These problems can eventually lead to anxiety. Anxiety, in turn, aggravates patients’ physical conditions and reduces QOL [14].
On the other hand, chronic LBP negatively affects sleep quality, psycho-emotional status, and social relationships [39-42]. Given the association of LBP with these psychological conditions, pure biomedical approach may be ineffective in the successful management of LBP and its associated problems and hence, psychological therapies must be taken into account for LBP management [40]. Psychological therapies such as ACT and biofeedback improve psychological flexibility and thereby, alleviate chronic pain, enhance physical health status, improve QOL, and help people have more satisfactory lives [8, 43].
Another justification for the positive effects of biofeedback on pain and QOL among patients with LBP is the positive effects of this therapy on stress. Psychological and environmental stresses are among the predictors of LBP and its associated problems. Therefore, stress management and relaxation techniques can contribute to LBP management.
Effective management of stress not only reduces physical symptoms of LBP (such as pain severity and duration), but also improves QOL and physical and psychological well-being. During biofeedback, clients learn different stress management strategies and learn how to use them for managing psychological and environmental stressors during daily life and how to develop their resistance to such stressors.
One of the study limitation was sampling from female patients with psychosomatic LBP in only one city in Iran. Thus, findings may have limited generalizability to male patients and patients with other types of LBP and other types of pain. Further studies are needed to compare the effects of ACT and biofeedback on other disorders and on patients from different age and gender groups. The strength of this study was the comparison of the effects of ACT and biofeedback on chronic LBP for the first time.
Conclusion
This study shows the effectiveness of both ACT and biofeedback in significantly reducing pain severity and duration and improving QOL among female patients with chronic psychosomatic LBP. Of course, while biofeedback has significant effects on the physical health aspect of QOL, it has no significant effects on the other aspects of QOL.
Contrarily, ACT significantly improves all aspects of QOL, except for the physical health aspect. These therapies can be used in specialty clinics and psychological services centers to manage symptoms and improve QOL among patients with chronic psychosomatic LBP. The findings of the present study highlight the necessity of using interdisciplinary approaches for managing chronic health problems caused by different physical and psychosocial etiologies.
Ethical Considerations
Compliance with ethical guidelines
The study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 1957. Moreover, this study was approved by the Ethics Committee of Rasht Islamic Azad University, Rasht, Iran (Code: IR.IAU.RASHT.REC.1395.70). All participants were ensured that their data would be confidentially managed and solely used for the purposes of the present study
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors contributions
Draft: Seyedeh Maryam Mousavi, Reza Shabahang, Naema Khodadadi-Hassankiadeh; Writing review and editing: Seyedeh Maryam Mousavi, Reza Shabahang; Resources: Seyedeh Maryam Mousavi, Reza Shabahang, Naema Khodadadi-Hassankiadeh; Supervision: Seyedeh Maryam Mousavi, Naema Khodadadi-Hassankiadeh; Data collecting: Reza Shabahang.
Conflict of interest
The authors have no conflict of interest.
References
The pre-tes and post-test mean difference of physical health in the biofeedback group (+8.10) was significantly greater than the ACT (-0.50) and the control (-0.60) groups (P = 0.004; Table 1). These findings denote that biofeedback had significant positive effects on the physical health domain of QOL, while ACT had no significant effects on it.
The mean score of the psychological health domain of QOL significantly increased in the ACT group (P=0.001), while it did not significantly change in the biofeedback (P=0.71) and the control (P=0.13) groups. Thus, the post-test Mean±SD score of psychological health in the ACT group (25.00±2.40) was significantly greater than the biofeedback (21.90±2.85) and the control (13.30±2.11) groups (P<0.001). However, there was no statistically significant difference among the groups in terms of the pre-test and post-test mean difference of psychological health mean score (P=0.08; Table 1).
These findings imply the effectiveness of ACT and the ineffectiveness of biofeedback in improving the psychological health domain of QOL among women with chronic LBP. The mean score of the social health domain of QOL significantly increased in the ACT group (P<0.001), but did not significantly change in the biofeedback (P=0.36) and the control (P=0.52) groups. Hence, the post-test mean score of social health in the ACT group (14.60±1.84) was significantly greater than the biofeedback (P=12.00±1.70) and the control (8.20±1.23) groups.
Moreover, the pre-test and post-test mean difference of the social health mean score in the ACT group (+5.30) was significantly greater than the biofeedback (-0.80) and the control (+0.60) groups (P=0.01; Table 1). These findings altogether denote the positive effects of ACT and the insignificant effects of biofeedback on the social health domain of QOL.
The mean score of the environmental health domain of QOL significantly increased in the ACT group (P=0.01); however, it did not significantly change in the biofeedback group (P=0.86) and significantly decreased in the control group (P=0.02). The post-test mean score of environmental health in the ACT group (32.00±4.52) was significantly greater than the biofeedback (28.70±5.60) and the control (20.40±2.22) groups (P<0.001).
The pre-test and post-test mean difference of the mean score of environmental health in the ACT group (+8.50) was also significantly greater than the biofeedback (+2.30) and the control (-4.30) groups (P<0.001; Table 1). Based on these findings, ACT was effective and biofeedback was ineffective in significantly improving the environmental health domain of QOL among women with chronic LBP.
Although the total mean score of QOL significantly increased in the ACT group (P=0.002), it showed no statistically significant change in the biofeedback (P=0.73) and the control (P=0.16) groups. Consequently, the post-test mean score of QOL in the ACT group (92.30±6.93) was significantly greater than the biofeedback (83.60±5.06) and the control (61.30±4.35) groups (P<0.001).
In addition, the Pre-test and post-test mean score of the QOL mean score in the ACT group (+20.30) was significantly greater than the biofeedback (+1.70) and the control (-6.10) groups (P < 0.001; Table 1). These findings indicate that ACT had significant effects and biofeedback had insignificant effects on QOL among women with chronic LBP.
Discussion
The aim of this study was to investigate the effects of ACT and biofeedback on pain severity and duration and QOL among women with chronic psychosomatic LBP. Findings revealed that both ACT and biofeedback significantly reduced pain severity and duration among these women. Of course, there was no significant difference between these two therapies respecting their effects on pain severity and duration.
In line with these findings, a former study reported that ACT significantly reduced pain among women with chronic headache [30]. One reason behind the positive effects of biofeedback is that it contains a relaxation component. Relaxation techniques such as diaphragmatic breathing and progressive muscular relaxation can significantly reduce pain. Besides, during biofeedback, patients learn how to deliberately identify and manage LBP symptoms and prevent their exacerbation.
Study findings also indicated the positive effects of both ACT and biofeedback on QOL among women with chronic psychosomatic LBP. Our literature search revealed that none of the previous studies had compared the effects of these two therapies on QOL among patients with LBP. However, several studies had investigated the effects of either ACT or biofeedback on QOL.
For instance, a study reported that the acceptance of LBP following ACT use significantly improved QOL among patients with chronic LBP [8]. Several other studies also reported the positive effects of ACT on QOL [31-34], anxiety symptoms, psychological strains and distress [32-34], and depression [24]. Other studies revealed that mindfulness-based stress reduction was effective in alleviating stress and improving QOL and physical, subjective, spiritual, and emotional well-being [35-37].
Therapies like ACT and biofeedback help patients evaluate physiologic reactions inside their bodies and then, attempt to control them [36]. ACT also exerts its positive effects on different patient outcomes, such as anxiety and depression, through improving psychological flexibility and deliberate attention to the present moment [32, 39]. ACT contains six core processes which can promote psychological flexibility and committed behavioral performance.
Self as a context is one of these processes. It makes clients aware of their thoughts, feelings, and desires and requires them to avoid controlling or avoiding them. After using this process, clients are subjected to another core process of ACT, i.e. cognitive defusion, which helps modify reactions to behaviors. In fact, instead of focusing on the validation or challenging of the thoughts, ACT focuses on performances.
Another core process of ACT is the acceptance of unavoidable situations like pain. Contact with present moment, determination of personal values, and committed action are the other core processes of ACT. Contact with present moment helps clients focus on the present moment instead of struggling with the past or probable events in the future. These six core processes improve psychological flexibility and QOL [8].
Patients with chronic LBP usually have limitations in doing their activities; thus, they may experience mood problems, reduced self-confidence, loss of employment, concerns over poor health status, and fear over attending social events. These problems can eventually lead to anxiety. Anxiety, in turn, aggravates patients’ physical conditions and reduces QOL [14].
On the other hand, chronic LBP negatively affects sleep quality, psycho-emotional status, and social relationships [39-42]. Given the association of LBP with these psychological conditions, pure biomedical approach may be ineffective in the successful management of LBP and its associated problems and hence, psychological therapies must be taken into account for LBP management [40]. Psychological therapies such as ACT and biofeedback improve psychological flexibility and thereby, alleviate chronic pain, enhance physical health status, improve QOL, and help people have more satisfactory lives [8, 43].
Another justification for the positive effects of biofeedback on pain and QOL among patients with LBP is the positive effects of this therapy on stress. Psychological and environmental stresses are among the predictors of LBP and its associated problems. Therefore, stress management and relaxation techniques can contribute to LBP management.
Effective management of stress not only reduces physical symptoms of LBP (such as pain severity and duration), but also improves QOL and physical and psychological well-being. During biofeedback, clients learn different stress management strategies and learn how to use them for managing psychological and environmental stressors during daily life and how to develop their resistance to such stressors.
One of the study limitation was sampling from female patients with psychosomatic LBP in only one city in Iran. Thus, findings may have limited generalizability to male patients and patients with other types of LBP and other types of pain. Further studies are needed to compare the effects of ACT and biofeedback on other disorders and on patients from different age and gender groups. The strength of this study was the comparison of the effects of ACT and biofeedback on chronic LBP for the first time.
Conclusion
This study shows the effectiveness of both ACT and biofeedback in significantly reducing pain severity and duration and improving QOL among female patients with chronic psychosomatic LBP. Of course, while biofeedback has significant effects on the physical health aspect of QOL, it has no significant effects on the other aspects of QOL.
Contrarily, ACT significantly improves all aspects of QOL, except for the physical health aspect. These therapies can be used in specialty clinics and psychological services centers to manage symptoms and improve QOL among patients with chronic psychosomatic LBP. The findings of the present study highlight the necessity of using interdisciplinary approaches for managing chronic health problems caused by different physical and psychosocial etiologies.
Ethical Considerations
Compliance with ethical guidelines
The study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 1957. Moreover, this study was approved by the Ethics Committee of Rasht Islamic Azad University, Rasht, Iran (Code: IR.IAU.RASHT.REC.1395.70). All participants were ensured that their data would be confidentially managed and solely used for the purposes of the present study
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Authors contributions
Draft: Seyedeh Maryam Mousavi, Reza Shabahang, Naema Khodadadi-Hassankiadeh; Writing review and editing: Seyedeh Maryam Mousavi, Reza Shabahang; Resources: Seyedeh Maryam Mousavi, Reza Shabahang, Naema Khodadadi-Hassankiadeh; Supervision: Seyedeh Maryam Mousavi, Naema Khodadadi-Hassankiadeh; Data collecting: Reza Shabahang.
Conflict of interest
The authors have no conflict of interest.
References
- Mason VL, Skevington SM, Osborn M. Development of a pain and discomfort module for use with the WHOQOL-100. Qual Life Res 2004; 13(6):1139-52. [DOI:10.1023/B:QURE.0000031344.53009.eb] [PMID]
- Lindberg J, Bluestein BW. Chronic pain management. In: Brodwin MG, Tellez F, Brodwin SK, editors. Medical, psychosocial, and vocational aspects of disability. 2nd ed. Georgia: Elliott and Fitzpatrick; 2000.
- Gracey JH, McDonough SM, Baxter GD. Physiotherapy management of low back pain: A survey of current practice in Northern Ireland. Spine (Phila Pa 1976) 2002; 27(4):406-17. [DOI:10.1097/00007632-200202150-00017]
- Khani H, Majdi MR, Azad Marzabadi E, Montazeri A, Ghorbani A, Ramezani M. Quality of life in Iranian Beta-thalassemia major patients of southern coastwise of the Caspian Sea. East Mediterr Health J 2012; 18(5):539-45. [DOI:10.26719/2012.18.5.539] [PMID]
- Munoz RA, McBride ME, Brnabic AJM, Lopez CJ, Hetem LAB, Secin R, et al. Major depressive disorder in Latin America: The relationship between depression severity, painful somatic symptoms, and quality of life. J Affect Disord 2005; 86(1):93-8. [DOI:10.1016/j.jad.2004.12.012] [PMID]
- Smite D, Ancâne G. Psychosomatic aspects of chronic low back pain syndrome. Proceedings of the Latvian Academy of Sciences. 2010; 64:202-208. [DOI:10.2478/v10046-011-0005-5]
- Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag 2011; 4:41-9. [DOI:10.2147/PRBM.S15375] [PMID] [PMCID]
- Mason VL, Mathias B, Skevington SM. Accepting low back pain: is it related to a good quality of life? Clin J Pain 2008; 24(1):22-9. [DOI:10.1097/AJP.0b013e318156d94f] [PMID]
- Kratz AL, Davis MC, Zautra AJ. Pain acceptance moderates the relation between pain and negative affect in female osteoarthritis and fibromyalgia patients. Ann Behav Med 2007; 33(3): 291-301. [DOI:10.1007/BF02879911] [PMID] [PMCID]
- McCracken LM, Sato A, Taylor GJ. A Trial of a Brief Group-Based Form of Acceptance and Commitment Therapy (ACT) for Chronic Pain in General Practice: Pilot Outcome and Process Results. J Pain 2013; 14(11):1398-406. [DOI:10.1016/j.jpain.2013.06.011] [PMID] [PMCID]
- Esteve R, Ramirez-Maestre C, Lopez-Marinez AE. Adjustment to chronic pain: the role of pain acceptance, coping strategies, and pain-related cognitions. Ann Behav Med 2007; 33(2): 179-88. [DOI:10.1007/BF02879899] [PMID]
- Lame IE, Peters ML, Vlaeyen JWS, Kleef MV, Patijn J. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. Eur J Pain 2005; 9(1): 15-24. [DOI:10.1016/j.ejpain.2004.02.006] [PMID]
- McCracken LM, Zhao-O’Brien J. General psychological acceptance and chronic pain: There is more to accept than the pain itself. Eur J Pain 2010; 14(2): 170-5. [DOI:10.1016/j.ejpain.2009.03.004] [PMID]
- Sielski R, Rief W, Glombiewski JA. Efficacy of biofeedback in chronic back pain: a meta-analysis. Int J Behav Med 2017; 24(1):25-41. [DOI:10.1007/s12529-016-9572-9] [PMID]
- Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-Analysis of Psychological Interventions for Chronic Low Back Pain. Health Psychol 2007; 26(1): 1-9. [DOI:10.1037/0278-6133.26.1.1] [PMID]
- Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness Training as an intervention for Fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychother Psychosom 2012; 76(4): 226-33. [DOI:10.1159/000101501] [PMID]
- Rossiter T. The Effectiveness of neurofeedbackand stimulant drugs in treating AD/HD. Appl Psychophysiol Biofeedback 2004; 29 (4):233-43. [DOI:10.1007/s10484-004-0383-4] [PMID]
- Shakeri R, Shaeiri MR, Roshan R. [The effect of biofeedback training on experimental pain according to perfectionism]. Journal of Bulletin of Environment, Pharmacology and Life Sciences 2007; 11(1):43-59.
- Sheffer CE, Cassis JE, Ferraresi LM, Lofland KR, McCracken LM. Sex Differences in the Presentation of Chronic Low Back Pain. Psychol Women Q 2003; 26(4):329-40. [DOI:10.1111/1471-6402.00072]
- Chenot J-F, Greitemann B, Kladny B, Petzke F, Pfingsten N, Schorr SG. Non-Specific Low Back Pain. Dtsch Arztebl Int 2017; 114(51-52):883-90. [DOI:10.3238/arztebl.2017.0883] [PMID] [PMCID]
- Goldberg D. Manual of the general health questionnaire. NFER-Nelson, Windsor; 1978.
- Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain 2009; 144(1-2):35-42. [DOI:10.1016/j.pain.2009.02.007] [PMID]
- Correll, DJ. The Measurement of Pain: Objectifying the Subjective. Pain Manag 2007;1:197-211. [DOI:10.1016/B978-0-7216-0334-6.50022-4]
- Tanhaee Z, Fathi-Ashtiani A , Amini M, Vahedi H, Shaghaghi F. [Validation of a Revised Version of the Short-form Mc-Gill Pain Questionnaire (SF-MPQ-2) for IBS Patients]. Govaresh 2012; 17:91-7.
- Nejat S, Montazeri A, Holakouie Naieni K, Mohammad K, Majdzadeh S. [The World Health Organization quality of Life (WHOQOL-BREF) questionnaire: Translation and validation study of the Iranian version]. Journal of School of Public Health and Institute of Public Health Research 2006; 4 (4):1-12.
- Skevington SM, Lotfy M, O’Connell KA, WHOQOL Group. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 2004; 13(2):299-310. [DOI:10.1023/B:QURE.0000018486.91360.00] [PMID]
- Mills KR. The basics of electromyography. J Neurol Neurosurg Psychiatry 2005; 76 (Suppl 2): 32-5. [DOI:10.1136/jnnp.2005.069211] [PMID] [PMCID]
- Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: A study of treatment effectiveness and process: J Consult Clin Psychol 2008; 76(3):397-407. [DOI:10.1037/0022-006X.76.3.397] [PMID]
- Vowles, KE, Thompson M. Acceptance and commitment therapy for chronic pain. In L. M. McCracken (Ed.), Mindfulness and acceptance in behavioral medicine: Current theory and. Oakland: New Harbinger Press; 2011.
- Tamannaeifar S, Gharraee B, Birashk B, Habibi MA [Comparative effectiveness of acceptance and commitment therapy and group cognitive therapy for major depressive disorder]. Zahedan Journal of Research in Medical Sciences 2014; 16(10):60-3.
- Mohabbat-Bahar S, Maleki-Rizi F, Akbari ME, Moradi-Joo M. Effectiveness of group training based on acceptance and commitment therapy on anxiety and depression of women with breast cancer. Iran J Cancer Prev 2015; 8(2):71-6.
- Veehof MM, Oskam M-J, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: a systematic review and meta-analysis. Pain 2011; 152(3):533-42. [DOI:10.1016/j.pain.2010.11.002] [PMID]
- Veehof M, Trompetter H, Bohlmeijer ET, Schreurs KMG. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther 2016; 45(1):5-31. [DOI:10.1080/16506073.2015.1098724] [PMID]
- Chisholm D, Sweeny K, Sheehan P, Rasmussen B, Smit F, Cuijpers P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry 2016; 3(5):415-24. [DOI:10.1016/S2215-0366(16)30024-4]
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007; 133(4):581-624. [DOI:10.1037/0033-2909.133.4.581] [PMID]
- Banth S, Ardebil MD. Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic low back pain. Int J Yoga 2015; 8(2):128-33. [DOI:10.4103/0973-6131.158476] [PMID] [PMCID]
- Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10(4):287-333. [DOI:10.1016/j.ejpain.2005.06.009] [PMID]
- Andersson HI. The course of non‐malignant chronic pain: A 12‐year follow‐up of a cohort from the general population. Eur J Pain 2004; 8(1):47-53. [DOI:10.1016/S1090-3801(03)00064-8]
- Wicksell RK, Melin L, Lekander M, Olsson GL. Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain-a randomized controlled trial. Pain 2009; 141(3):248-57. [DOI:10.1016/j.pain.2008.11.006] [PMID]
- Carlesso LC, Rampersaud YR, Davis AM. Clinical classes of injured workers with chronic low back pain: a latent class analysis with relationship to working status. Eur Spine J 2017:117-24. [DOI:10.1007/s00586-017-4966-1] [PMID]
- Heidari J, Hasenbring M, Kleinert J, Kellmann M. Stress-related psychological factors for back pain among athletes: Important topic with scarce evidence. Eur J Sport Sci 2017; 17(3):351-9. [DOI:10.1080/17461391.2016.1252429] [PMID]
- Sturgeon JA, Zautra AJ. Resilience to chronic arthritis pain is not about stopping pain that will not stop: development of a dynamic model of effective pain adaptation. Psychosocial Factors in Arthritis 2016; 133-49. [DOI:10.1007/978-3-319-22858-7_8]
- Johnston M, Foster M, Shennan J, Starkey NJ, Johnson A. The effectiveness of an acceptance and commitment therapy self-help intervention for chronic pain. Clin J Pain 2010; 26(5):393-402. [DOI:10.1097/AJP.0b013e3181cf59ce] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2019/05/4 | Accepted: 2019/06/6 | Published: 2019/07/1
Received: 2019/05/4 | Accepted: 2019/06/6 | Published: 2019/07/1
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |