Sat, Apr 27, 2024
Volume 4, Issue 4 (Autumn 2018)
Caspian J Neurol Sci 2018, 4(4): 159-168 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yousefzadeh-Chabok S, Khodadadi-Hassankiadeh N, Saberi A, Ghanbari Khanghah A, Zarrabi H, Yeganeh M R, et al . Anxiety, Depression, and Their Related Factors in Patients Admitted to Intensive Care Units. Caspian J Neurol Sci 2018; 4 (4) :159-168
URL: http://cjns.gums.ac.ir/article-1-246-en.html
URL: http://cjns.gums.ac.ir/article-1-246-en.html
Shahrokh Yousefzadeh-Chabok1 

 , Naema Khodadadi-Hassankiadeh *
, Naema Khodadadi-Hassankiadeh * 

 2, Alia Saberi1
2, Alia Saberi1 

 , Atefeh Ghanbari Khanghah3
, Atefeh Ghanbari Khanghah3 

 , Homa Zarrabi4
, Homa Zarrabi4 

 , Mohammad Reza Yeganeh5
, Mohammad Reza Yeganeh5 
 , Hamideh Hakimi6
, Hamideh Hakimi6 

 , Anoush Dehnadi Moghadam4
, Anoush Dehnadi Moghadam4 




 , Naema Khodadadi-Hassankiadeh *
, Naema Khodadadi-Hassankiadeh * 

 2, Alia Saberi1
2, Alia Saberi1 

 , Atefeh Ghanbari Khanghah3
, Atefeh Ghanbari Khanghah3 

 , Homa Zarrabi4
, Homa Zarrabi4 

 , Mohammad Reza Yeganeh5
, Mohammad Reza Yeganeh5 
 , Hamideh Hakimi6
, Hamideh Hakimi6 

 , Anoush Dehnadi Moghadam4
, Anoush Dehnadi Moghadam4 


1- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran
2- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran , n_khodadady@yahoo.com
3- Determinants of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), School of Nursing, Guilan University of Medical Sciences, Rasht, Iran
4- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
5- Instructor of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
6- Instructor, Department of Nursing, Lahijan Branch, Islamic Azad university, Lahijan, Iran
2- Neuroscience Research Center, Guilan University of Medical Sciences, Rasht, Iran , n_khodadady@yahoo.com
3- Determinants of Health Research Center (SDHRC), Department of Nursing (Medical-Surgical), School of Nursing, Guilan University of Medical Sciences, Rasht, Iran
4- Guilan Road Trauma Research Center, Guilan University of Medical Sciences, Rasht, Iran
5- Instructor of Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran
6- Instructor, Department of Nursing, Lahijan Branch, Islamic Azad university, Lahijan, Iran
Full-Text [PDF 1480 kb]
(840 Downloads)
| Abstract (HTML) (2685 Views)
Full-Text: (968 Views)
Introduction
Disease crisis and necessary medical care in the Intensive Care Units (ICUs) are psychological stressors for patients. Many patients often recall the frightening events they experienced in ICUs and call it a stressful experience [1]. Severe stresses, in addition to the physical consequences, cause psychological complications including stress due to the cessation of mechanical ventilation, transfer to the general department, and discharge that are reported in various studies [2-4]. Diseases requiring special care are called critical illnesses. Such life-threatening diseases cause anxiety [1, 5, 6].
Studies on the incidence of anxiety in patients hospitalized in ICUs reported the relevant anxiety as 12-43% [5, 6]. The challenge to determine the anxiety of such patients is the administration of sedatives, opioids, corticosteroids, and anticonvulsants. They can hide anxiety or show a lower level of anxiety in the patients [7]. The short-term and long-term physiological consequences of anxiety induced in patients hospitalized in ICUs are of great important so that can lead to an increase in mortality rate [7]. The immediate physiological response of body to anxiety, and complex changes in neuroendocrine and immune function can delay wound healing, myocardial ischemia, diastolic dysfunction, and the development of postoperative delirium [8]. On the other hand, anxiety persists a long time after the treatment and discharge from the ICU.
A study showed that a significant rate of such patients experience anxiety even one year after discharge from ICUs [9]. Persisted anxiety, causing disability in various functions in addition to affecting the quality of life of patients [10] and their caregivers [11], accounts for a large part of health care services [12], and the severity of anxiety in such patients is related to the history of mental illness, duration of hospitalization, and the severity of the stressful accident [13].
Some studies reported that depression rate in ICU-admitted patients is five times greater than those of other complications such as posttraumatic stress disorder [14]. The studies conducted in Iran reported that delirium had a relationship with depression in ICU-admitted patients [2]; the incidence of depression at the time of discharge from the ICU was 57.8% [15]; depressive symptoms occurred in approximately one-third of ICU survivors, which persisted for one year after discharge [16]. According to the results of a study by Haines et al. [17], starting antidepressant medication immediately after admission to the ICU did not affect the rate of depression after discharge. In another study, after initiation of antidepressants, African-American youth were more likely to have depressive symptoms [18].
Experiences related to treatment in the ICUs are very specific. Some of these experiences are: pain and a feeling of loss of self-control, excessive noises, disability to communicate adequately [19], continuous and disturbing light, ineffective communication, long duration of mechanical ventilation, pulmonary artery catheter insertion [3], suction, and the length of stay. These factors are considered as psychological stressors that increase the risk of mental disorders such as anxiety, posttraumatic stress, and depression after discharge. The female patients with a permanent facial scar and a past psychiatric history are more exposed to these risk factors [20].
ICU-admitted patients have limitations to verbally respond to the questionnaires. One of the reasons for this limitation is the presence of Pulmonary Artery Catheter (PAC), which does not allow the patient to speak. Hospital Anxiety and Depression Scale (HADS) is a questionnaire that can be easily used to assess anxiety incidence in the ICU, although these studies are conducted on patients with the ability to communicate verbally [7].
In Iran, there are few studies on the incidence of anxiety and depression and their related factors in patients admitted to the ICUs. Due to the increase in the number of patients that need intensive care in Iran, more studies should be conducted on mental disorders and related factors in such patients [1, 21], since early detection can provide timely supportive interventions for the patients and reduce short-term [8] and long-term [22, 23] outcomes. In this regard, the current study aimed at screening anxiety and depression as well as their related factors in ICU-admitted patients in Iran.
Materials and Methods
The current analytical, cross sectional study was conducted from 2012 to 2014. The study population consisted of patients admitted to the two ICUs of a medical education center in Northern Iran. Convenience sampling method was employed to select 133 subjects, according to the study by McKinley et al. that reported anxiety rate of 85% in ICU-admitted patients considering 99% confidence interval, and the error rate of 0.08; the final sample size was set to 135 after consulting with a statistician [7].
Inclusion criteria were: being literate, age >15 years, at least 24 hours of hospitalization in ICU, Glasgow Coma Scale (GCS) >13 according to the nurses diagnosis, having vital signs, no pain and respiratory distress, and having ability to interact (i.e. to be able to answer questions with their eyes open, read, and understand the Persian language, and read the written words). The subjects with PAC for mechanical ventilation or receiving non-invasive positive-pressure mechanical ventilation were entered into the study if they had willingness to participate. Unwillingness to participate and fatigue to continue the interview were considered as exclusion criteria.
Sampling was conducted by a trained nurse working in the ICU through interviewing. The interview was performed at 10:00 am and 4:00 pm when the patients were awake. To show their willingness or unwillingness to participate in the study, patients acted non-verbally by moving hands or head up and down to say yes or no. They were informed about the freedom to quit the study whenever they could not continue. Data collection tool was a two-part questionnaire. The first part was a researcher-made checklist surveying demographic (age, gender, occupation, marital status, education), clinical (diagnosis, duration of hospitalization, type of ICU, ventilation status, sedative and narcotic drugs use), and psychosocial (history of mental disorders; i.e. admission to a psychiatric hospital and history of substance abuse) characteristics of patients. All information was obtained from the patients` medical records. The checklist was designed according to similar studies [7, 24-27].
The second part was HADS questionnaire. It has 14 items, 7 assess anxiety level and 7 are related to depression. For its Persian version, Kaviani et al. recommended the clinical cut off point of 20. This point for Beck’s depression inventory and Beck’s anxiety inventory were 15 and 11, respectively. Hence, for both anxiety and depression subscales of HADS, the clinical cut off point was 6. The correlation of HADS subscales with BDI and BAI were significant (r=0.77 and 0.76, respectively). In their study, the t-test results between the two groups showed that both sub-scales of depression and anxiety could distinguish between the two groups of healthy subjects and the patients. They also examined test-retest reliability of HADS for depression subscale (r=0.77) and anxiety subscale (r=0.81), which indicated acceptable reliability of its Persian version. Moreover, internal consistency for depression and anxiety subscales were α=0.70 and 0.85 respectively, which indicated its acceptable validity [28]. In another study, its Cronbach’s alpha for depression and anxiety subscales in Iranian patients were reported 0.86 and 0.78, respectively [29].
HADS is a self-reporting scale that measures anxiety and depression in patients. Its completion by the subjects takes less than five minutes. The questionnaire items are scored based on a four-point Likert scale from 0 to 3. Hence, the total score ranges 0 to 42. For anxiety scale, scores 0-6 indicate no sign of anxiety, 7-9 low anxiety, 10-13 moderate anxiety, and scores ≥14 show high level of anxiety. For depression scale, scores 0-6 indicate no sign of depression, 7-9 low depression, 10-11 moderate depression, and scores ≥11 show high level of depression. In the current study, scores ≥11 for both subscales were considered as clinical cut off point [29, 30].
To minimize the patient’s attempt to answer questions, each item of HADS was clearly written on a A4-size cardboard with a font size of 18 to read and answer with pointing fingers; one finger if they had no anxiety/depression, two fingers if they had low anxiety/depression, three fingers if they had moderate anxiety/depression and four figures if they had high anxiety/depression.
The collected data were analyzed with SPSS V. 18 using descriptive statistics (frequency, mean, and standard deviation) and statistical tests. The variables were once evaluated with anxiety variable and once with depression variable using the Kolmogorov-Smirnov Test (due to sample size of >100, the Shapiro–Wilk Test was not used) to test the normality of distribution. Since the obtained P-value was less than 0.05, the distribution was not normal and accordingly, non-parametric tests (the Mann-Whitney U and the Kruskal–Wallis) were employed.
Results
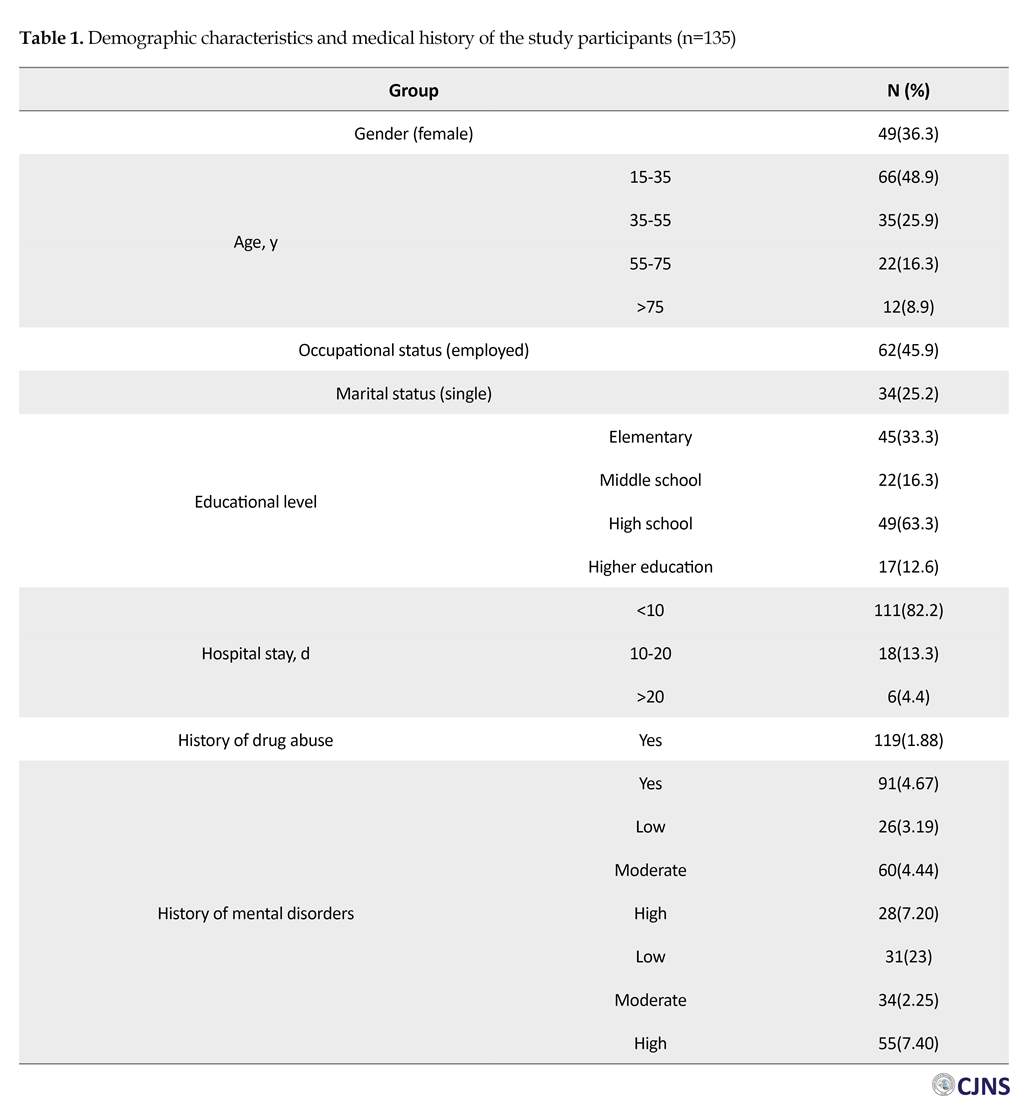
Demographic characteristics and medical history of the 135 study subjects are shown in Table 1. Most of them were male (63.7%), aged 15-35 years (48.9%), married (74.8%), and unemployed (54.1%). Most of them had no history of drug abuse (88.1%). Majority of the patients reported high anxiety (40.7%) and moderate depression (44.4%) based on HADS.
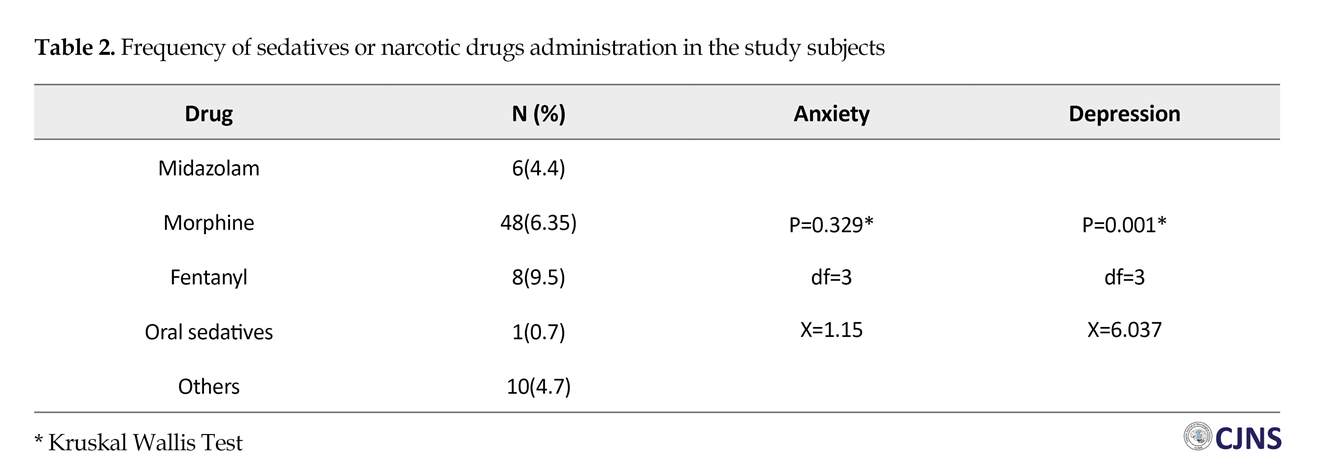
According to Table 2, more than two-thirds of patients (67.4%) received sedative or narcotic drug 24 hours prior to the study onset. In total, 91 patients received at least a single dose of sedative, and the most commonly used drug was morphine (n=48 or 35.6%), followed by fentanyl (n=8 or 5.9%), and midazolam (n=6 or 4.4%). A number of patients simultaneously received both sedative and narcotic drugs: both morphine and midazolam (n=14; 10.4%), fentanyl and midazolam (n=2; 1.5%), and morphine plus an oral sedative (n=2; 1.5%). Morphine was mostly used in combination with other drugs. There was no significant relationship between the level of anxiety and the administration of sedatives, but the level of depression had significant relationship with the use of sedatives (X=6.037, df=3, P=0.001) (Table 2).
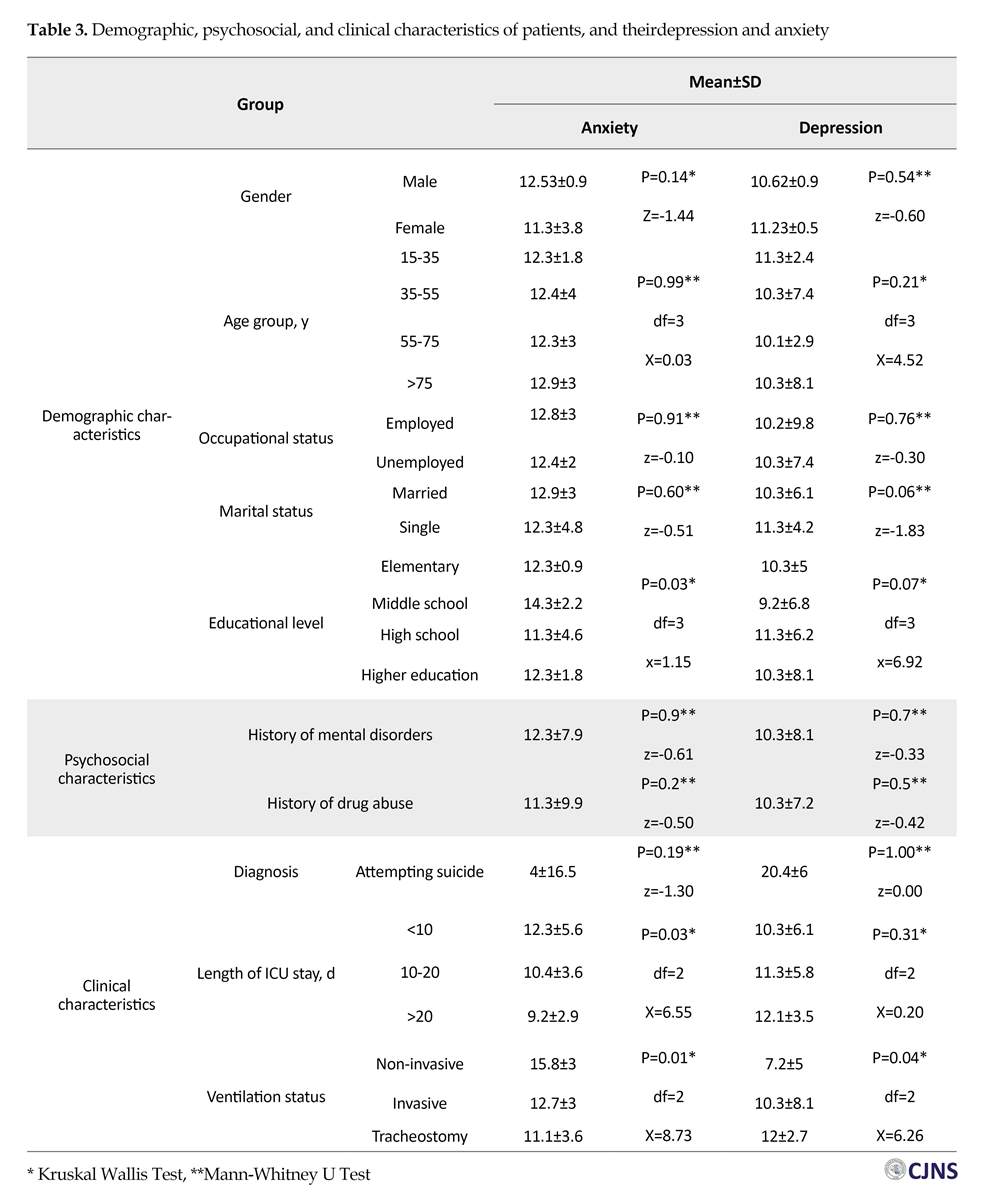
As can be observed in Table 3, the Mean anxiety score of patients was 12.06±3.9 and their mean depression score was 10.7±3.2. Anxiety and depression scores of 89 (65.9%) and 87 (64.4%) subjects, respectively, were above the cut off point. There was no statistically significant difference between the mean scores of anxiety and depression in terms of gender as well as occupational and marital status. Regarding educational level, the highest mean of anxiety was observed in subjects with middle school education and its relationship was statistically significant (X=1.15, df=2, P=0.03), while the highest mean of depression (11.3±6.2) was observed in subjects with high school education, and the relationship was statistically insignificant.
Regarding the ICU stay, the highest mean of anxiety (12.3±5.6) was observed in subjects with short-term hospitalization (<10 days). A significant correlation was observed between short-term hospitalization and anxiety (X=6.55, df=2, P=0.03), but other lengths of ICU stay had no significant relationship with anxiety (X=0.20, df=2, P=0.31). Moreover, there was no significant difference between the age groups in terms of anxiety and depression.
There was no statistically significant difference between the mean scores of anxiety and depression in terms of having a history of mental disorders and substance abuse. The highest mean of anxiety was found with the subjects hospitalized for suicide attempt (16.5±4), and the highest mean of depression was observed in subjects hospitalized for other reasons (11.1±3). There was no significant relationship between attempting suicide and anxiety (P=0.19) and depression (P=1) in ICU-admitted patients.
Regarding the treatment with mechanical ventilation, the highest mean of anxiety was observed in subjects with non-invasive mechanical ventilation (15.8±3), and the relationship was significant (X=8.731, df=2, P=0.01). The highest mean of depression was observed in subjects with tracheostomy (12±2.7), and its relationship was also significant (X=6.26, df=2, P=0.04).
Disease crisis and necessary medical care in the Intensive Care Units (ICUs) are psychological stressors for patients. Many patients often recall the frightening events they experienced in ICUs and call it a stressful experience [1]. Severe stresses, in addition to the physical consequences, cause psychological complications including stress due to the cessation of mechanical ventilation, transfer to the general department, and discharge that are reported in various studies [2-4]. Diseases requiring special care are called critical illnesses. Such life-threatening diseases cause anxiety [1, 5, 6].
Studies on the incidence of anxiety in patients hospitalized in ICUs reported the relevant anxiety as 12-43% [5, 6]. The challenge to determine the anxiety of such patients is the administration of sedatives, opioids, corticosteroids, and anticonvulsants. They can hide anxiety or show a lower level of anxiety in the patients [7]. The short-term and long-term physiological consequences of anxiety induced in patients hospitalized in ICUs are of great important so that can lead to an increase in mortality rate [7]. The immediate physiological response of body to anxiety, and complex changes in neuroendocrine and immune function can delay wound healing, myocardial ischemia, diastolic dysfunction, and the development of postoperative delirium [8]. On the other hand, anxiety persists a long time after the treatment and discharge from the ICU.
A study showed that a significant rate of such patients experience anxiety even one year after discharge from ICUs [9]. Persisted anxiety, causing disability in various functions in addition to affecting the quality of life of patients [10] and their caregivers [11], accounts for a large part of health care services [12], and the severity of anxiety in such patients is related to the history of mental illness, duration of hospitalization, and the severity of the stressful accident [13].
Some studies reported that depression rate in ICU-admitted patients is five times greater than those of other complications such as posttraumatic stress disorder [14]. The studies conducted in Iran reported that delirium had a relationship with depression in ICU-admitted patients [2]; the incidence of depression at the time of discharge from the ICU was 57.8% [15]; depressive symptoms occurred in approximately one-third of ICU survivors, which persisted for one year after discharge [16]. According to the results of a study by Haines et al. [17], starting antidepressant medication immediately after admission to the ICU did not affect the rate of depression after discharge. In another study, after initiation of antidepressants, African-American youth were more likely to have depressive symptoms [18].
Experiences related to treatment in the ICUs are very specific. Some of these experiences are: pain and a feeling of loss of self-control, excessive noises, disability to communicate adequately [19], continuous and disturbing light, ineffective communication, long duration of mechanical ventilation, pulmonary artery catheter insertion [3], suction, and the length of stay. These factors are considered as psychological stressors that increase the risk of mental disorders such as anxiety, posttraumatic stress, and depression after discharge. The female patients with a permanent facial scar and a past psychiatric history are more exposed to these risk factors [20].
ICU-admitted patients have limitations to verbally respond to the questionnaires. One of the reasons for this limitation is the presence of Pulmonary Artery Catheter (PAC), which does not allow the patient to speak. Hospital Anxiety and Depression Scale (HADS) is a questionnaire that can be easily used to assess anxiety incidence in the ICU, although these studies are conducted on patients with the ability to communicate verbally [7].
In Iran, there are few studies on the incidence of anxiety and depression and their related factors in patients admitted to the ICUs. Due to the increase in the number of patients that need intensive care in Iran, more studies should be conducted on mental disorders and related factors in such patients [1, 21], since early detection can provide timely supportive interventions for the patients and reduce short-term [8] and long-term [22, 23] outcomes. In this regard, the current study aimed at screening anxiety and depression as well as their related factors in ICU-admitted patients in Iran.
Materials and Methods
The current analytical, cross sectional study was conducted from 2012 to 2014. The study population consisted of patients admitted to the two ICUs of a medical education center in Northern Iran. Convenience sampling method was employed to select 133 subjects, according to the study by McKinley et al. that reported anxiety rate of 85% in ICU-admitted patients considering 99% confidence interval, and the error rate of 0.08; the final sample size was set to 135 after consulting with a statistician [7].
Inclusion criteria were: being literate, age >15 years, at least 24 hours of hospitalization in ICU, Glasgow Coma Scale (GCS) >13 according to the nurses diagnosis, having vital signs, no pain and respiratory distress, and having ability to interact (i.e. to be able to answer questions with their eyes open, read, and understand the Persian language, and read the written words). The subjects with PAC for mechanical ventilation or receiving non-invasive positive-pressure mechanical ventilation were entered into the study if they had willingness to participate. Unwillingness to participate and fatigue to continue the interview were considered as exclusion criteria.
Sampling was conducted by a trained nurse working in the ICU through interviewing. The interview was performed at 10:00 am and 4:00 pm when the patients were awake. To show their willingness or unwillingness to participate in the study, patients acted non-verbally by moving hands or head up and down to say yes or no. They were informed about the freedom to quit the study whenever they could not continue. Data collection tool was a two-part questionnaire. The first part was a researcher-made checklist surveying demographic (age, gender, occupation, marital status, education), clinical (diagnosis, duration of hospitalization, type of ICU, ventilation status, sedative and narcotic drugs use), and psychosocial (history of mental disorders; i.e. admission to a psychiatric hospital and history of substance abuse) characteristics of patients. All information was obtained from the patients` medical records. The checklist was designed according to similar studies [7, 24-27].
The second part was HADS questionnaire. It has 14 items, 7 assess anxiety level and 7 are related to depression. For its Persian version, Kaviani et al. recommended the clinical cut off point of 20. This point for Beck’s depression inventory and Beck’s anxiety inventory were 15 and 11, respectively. Hence, for both anxiety and depression subscales of HADS, the clinical cut off point was 6. The correlation of HADS subscales with BDI and BAI were significant (r=0.77 and 0.76, respectively). In their study, the t-test results between the two groups showed that both sub-scales of depression and anxiety could distinguish between the two groups of healthy subjects and the patients. They also examined test-retest reliability of HADS for depression subscale (r=0.77) and anxiety subscale (r=0.81), which indicated acceptable reliability of its Persian version. Moreover, internal consistency for depression and anxiety subscales were α=0.70 and 0.85 respectively, which indicated its acceptable validity [28]. In another study, its Cronbach’s alpha for depression and anxiety subscales in Iranian patients were reported 0.86 and 0.78, respectively [29].
HADS is a self-reporting scale that measures anxiety and depression in patients. Its completion by the subjects takes less than five minutes. The questionnaire items are scored based on a four-point Likert scale from 0 to 3. Hence, the total score ranges 0 to 42. For anxiety scale, scores 0-6 indicate no sign of anxiety, 7-9 low anxiety, 10-13 moderate anxiety, and scores ≥14 show high level of anxiety. For depression scale, scores 0-6 indicate no sign of depression, 7-9 low depression, 10-11 moderate depression, and scores ≥11 show high level of depression. In the current study, scores ≥11 for both subscales were considered as clinical cut off point [29, 30].
To minimize the patient’s attempt to answer questions, each item of HADS was clearly written on a A4-size cardboard with a font size of 18 to read and answer with pointing fingers; one finger if they had no anxiety/depression, two fingers if they had low anxiety/depression, three fingers if they had moderate anxiety/depression and four figures if they had high anxiety/depression.
The collected data were analyzed with SPSS V. 18 using descriptive statistics (frequency, mean, and standard deviation) and statistical tests. The variables were once evaluated with anxiety variable and once with depression variable using the Kolmogorov-Smirnov Test (due to sample size of >100, the Shapiro–Wilk Test was not used) to test the normality of distribution. Since the obtained P-value was less than 0.05, the distribution was not normal and accordingly, non-parametric tests (the Mann-Whitney U and the Kruskal–Wallis) were employed.
Results
Demographic characteristics and medical history of the 135 study subjects are shown in Table 1. Most of them were male (63.7%), aged 15-35 years (48.9%), married (74.8%), and unemployed (54.1%). Most of them had no history of drug abuse (88.1%). Majority of the patients reported high anxiety (40.7%) and moderate depression (44.4%) based on HADS.
According to Table 2, more than two-thirds of patients (67.4%) received sedative or narcotic drug 24 hours prior to the study onset. In total, 91 patients received at least a single dose of sedative, and the most commonly used drug was morphine (n=48 or 35.6%), followed by fentanyl (n=8 or 5.9%), and midazolam (n=6 or 4.4%). A number of patients simultaneously received both sedative and narcotic drugs: both morphine and midazolam (n=14; 10.4%), fentanyl and midazolam (n=2; 1.5%), and morphine plus an oral sedative (n=2; 1.5%). Morphine was mostly used in combination with other drugs. There was no significant relationship between the level of anxiety and the administration of sedatives, but the level of depression had significant relationship with the use of sedatives (X=6.037, df=3, P=0.001) (Table 2).
As can be observed in Table 3, the Mean anxiety score of patients was 12.06±3.9 and their mean depression score was 10.7±3.2. Anxiety and depression scores of 89 (65.9%) and 87 (64.4%) subjects, respectively, were above the cut off point. There was no statistically significant difference between the mean scores of anxiety and depression in terms of gender as well as occupational and marital status. Regarding educational level, the highest mean of anxiety was observed in subjects with middle school education and its relationship was statistically significant (X=1.15, df=2, P=0.03), while the highest mean of depression (11.3±6.2) was observed in subjects with high school education, and the relationship was statistically insignificant.
Regarding the ICU stay, the highest mean of anxiety (12.3±5.6) was observed in subjects with short-term hospitalization (<10 days). A significant correlation was observed between short-term hospitalization and anxiety (X=6.55, df=2, P=0.03), but other lengths of ICU stay had no significant relationship with anxiety (X=0.20, df=2, P=0.31). Moreover, there was no significant difference between the age groups in terms of anxiety and depression.
There was no statistically significant difference between the mean scores of anxiety and depression in terms of having a history of mental disorders and substance abuse. The highest mean of anxiety was found with the subjects hospitalized for suicide attempt (16.5±4), and the highest mean of depression was observed in subjects hospitalized for other reasons (11.1±3). There was no significant relationship between attempting suicide and anxiety (P=0.19) and depression (P=1) in ICU-admitted patients.
Regarding the treatment with mechanical ventilation, the highest mean of anxiety was observed in subjects with non-invasive mechanical ventilation (15.8±3), and the relationship was significant (X=8.731, df=2, P=0.01). The highest mean of depression was observed in subjects with tracheostomy (12±2.7), and its relationship was also significant (X=6.26, df=2, P=0.04).
Discussion
The results of the current study showed a significant level of anxiety and depression in the ICU-admitted patients, which was consistent to the findings of other similar studies [7, 24-27]. The incidence of high anxiety in the current study subjects was high, which was consistent with the results of McKinley et al. where the incidence of anxiety was higher than average in hospitalized patients [7]. However, the reported anxiety rate in the current study was higher than that of patients admitted for cardiovascular and respiratory diseases that were candidates for bypass surgery with anxiety scores of respectively 5.2 and 6.6, based on HADS [31].
In the current study, 89 patients (65.9%) had anxiety scores higher than cut off point (≥10) and 87 (64.4%) had depression scores above the cut off point. In the study by Scragg et al. 24 (30%) subjects scored above 8 on the depression subscale and 34 (43%) scored above 8 on the anxiety subscale [31]. The reason for the higher levels of anxiety and depression in their study compared with the studies conducted in the developed countries is that in such countries, supportive and psychological interventions begin immediately after admission to the ICUs, and patients feel more secure, resulting in a low level of anxiety and depression [32, 33]. Other factors such as different sampling methods and assessment days may also be ineffective.
In the current study, the ventilation status and length of ICU stay had a statistically significant correlation with anxiety rate. This fact is well known either through prospective or retrospective studies that anxiety is a persistent and constant problem for patients admitted to ICUs. The anxiety level in the current study was high in patients underwent non-invasive ventilation. It was expected because patients receiving mechanical (invasive) ventilation consume more sedative and anti-anxiety medication that can hide their anxiety and accordingly, were less anxious. However, McKinley and Madronio reported that anxiety of ICU-admitted patients receiving non-invasive mechanical ventilation was at low or moderate level [27], although physiological demands and greater dependence observed in mechanical ventilation are expected to increase anxiety.
In the current study, depression was significantly related to undergoing mechanical ventilation and patients with tracheostomy were more depressed. It is reported that patients with tracheostomy and their families are significantly depressed [34]. The incidence of depression is reported in patients undergoing tracheostomy due to speaking barriers and subsequent communication problems [35]. In the current study, depression in patients receiving more sedatives was also significantly higher, which may be due to the presence of tracheostomy. In a study with consistent results, there was a significant difference between non-invasive and invasive ventilation in patients with neuromuscular disease, and it was reported that anxiety contributed to respiratory difficulty, sleep impediment, and depression [36].
Anxiety had significant relationship with short-term hospitalization (less than 10 days). In other words, the level of anxiety was higher in patient who stayed less than 10 days in ICU and, in contrary, was lower in the ones stayed more than 10 days in this unit. Perhaps this is due to the patient’s acclimation to the environment and conditions of the ICU and accepting the conditions in such critical situation. However, some studies reported that the short stay in ICU could be associated with physical recovery and low anxiety [37]. Patients who stay in the ICU for a longer time are accustomed to the conditions of the unit, and sometimes they themselves ask to stay more in ICU due to its better care and facilities, and their anxiety intensifies when they are informed that they are going to be discharged and transferred to general wards [38].
There was no statistically significant relationship between anxiety and administration of anti-anxiety and sedative medications in ICU-admitted patients. The administration of these drugs in the current study could not reduce anxiety in ICU-admitted patients. This result was in agreement with those of other studies. For example, McKinley et al. [7] reported that during data collection process, patients regularly received sedatives or opioids, but they were still anxious.
It is very difficult to diagnose and manage anxiety in ICU-admitted patients, especially in the ones receiving invasive ventilation where it is very difficult to communicate. In the current study, it took 18 months to get samples that could communicate with authors. Despite the fact that most of the study patients received sedatives, they still had a significant degree of anxiety. Therefore, it is important to be checked and diagnosed by the nurse, although unfortunately the patients were not routinely asked if they were anxious. To reduce anxiety, patient-centered approaches such as family meeting and training sessions are recommended [39]. Non-pharmacological interventions to reduce anxiety by nurses are also recommended. Music therapy [40] and sound interventions can reduce heart rate, blood pressure, and respiratory rate, and consequently, reduce the anxiety in ICU-admitted patients [33].
One of the limitations of the current study was its small sample size that was attributed to the high amount of time needed to find eligible samples. With a larger sample size, the findings would be different. A larger sample can better show changes in anxiety based on the causes of hospitalization. In most of the patients, anxiety could not be assessed due to lack of communication (because of low level of consciousness, instable physical conditions, or receiving high doses of sedatives). A one-item questionnaire is probably a good idea.
Another limitation was the absence of a psychiatrist to diagnose mental disorders and drug abuse. Therefore, it is suggested to assess mental disorders in future studies using structured clinical interviews based on Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Also, patients with history of mood disorders, anxiety, and depression were included in the study due to the low sample size, which may affect the results.
Conclusion
Anxiety and depression (symptoms of mood disorders) in the ICU-admitted patients were relatively high; the duration of hospitalization was significantly associated with anxiety and administration of sedatives had a significant correlation with depression. Also, the type of received mechanical ventilation was associated with both disorders. Based on the obtained results, routine screening of anxiety and depression by nurses in ICUs is useful for early diagnosis and treatment, which can prevent long-term complications of such disorders.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; They were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
The present research program was Financial supported by the Research Committee of Guilan University of Medical Sciences, Rasht, Iran.
Authors contributions
The authors contributions is as follows: Conceptualization: Shahrokh Yousefzadeh-Chabok; Methodology: Naema Khodadadi-Hassankiadeh; Investigation: Alia Saberi; Writing–original draft: Atefeh Ghanbari khanghah; Writing–review & editing: Homa Zarrabi; Funding Acquisition: Mohammad Reza Yeganeh; Resources: Hamideh Hakimi; and Supervision: Anoush Dehnadi Moghadam.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to express our gratitude to the patients and the staff of Poorsina Hospital. We also would like to thank Ms. Kazemi for translating the manuscript.
References
The results of the current study showed a significant level of anxiety and depression in the ICU-admitted patients, which was consistent to the findings of other similar studies [7, 24-27]. The incidence of high anxiety in the current study subjects was high, which was consistent with the results of McKinley et al. where the incidence of anxiety was higher than average in hospitalized patients [7]. However, the reported anxiety rate in the current study was higher than that of patients admitted for cardiovascular and respiratory diseases that were candidates for bypass surgery with anxiety scores of respectively 5.2 and 6.6, based on HADS [31].
In the current study, 89 patients (65.9%) had anxiety scores higher than cut off point (≥10) and 87 (64.4%) had depression scores above the cut off point. In the study by Scragg et al. 24 (30%) subjects scored above 8 on the depression subscale and 34 (43%) scored above 8 on the anxiety subscale [31]. The reason for the higher levels of anxiety and depression in their study compared with the studies conducted in the developed countries is that in such countries, supportive and psychological interventions begin immediately after admission to the ICUs, and patients feel more secure, resulting in a low level of anxiety and depression [32, 33]. Other factors such as different sampling methods and assessment days may also be ineffective.
In the current study, the ventilation status and length of ICU stay had a statistically significant correlation with anxiety rate. This fact is well known either through prospective or retrospective studies that anxiety is a persistent and constant problem for patients admitted to ICUs. The anxiety level in the current study was high in patients underwent non-invasive ventilation. It was expected because patients receiving mechanical (invasive) ventilation consume more sedative and anti-anxiety medication that can hide their anxiety and accordingly, were less anxious. However, McKinley and Madronio reported that anxiety of ICU-admitted patients receiving non-invasive mechanical ventilation was at low or moderate level [27], although physiological demands and greater dependence observed in mechanical ventilation are expected to increase anxiety.
In the current study, depression was significantly related to undergoing mechanical ventilation and patients with tracheostomy were more depressed. It is reported that patients with tracheostomy and their families are significantly depressed [34]. The incidence of depression is reported in patients undergoing tracheostomy due to speaking barriers and subsequent communication problems [35]. In the current study, depression in patients receiving more sedatives was also significantly higher, which may be due to the presence of tracheostomy. In a study with consistent results, there was a significant difference between non-invasive and invasive ventilation in patients with neuromuscular disease, and it was reported that anxiety contributed to respiratory difficulty, sleep impediment, and depression [36].
Anxiety had significant relationship with short-term hospitalization (less than 10 days). In other words, the level of anxiety was higher in patient who stayed less than 10 days in ICU and, in contrary, was lower in the ones stayed more than 10 days in this unit. Perhaps this is due to the patient’s acclimation to the environment and conditions of the ICU and accepting the conditions in such critical situation. However, some studies reported that the short stay in ICU could be associated with physical recovery and low anxiety [37]. Patients who stay in the ICU for a longer time are accustomed to the conditions of the unit, and sometimes they themselves ask to stay more in ICU due to its better care and facilities, and their anxiety intensifies when they are informed that they are going to be discharged and transferred to general wards [38].
There was no statistically significant relationship between anxiety and administration of anti-anxiety and sedative medications in ICU-admitted patients. The administration of these drugs in the current study could not reduce anxiety in ICU-admitted patients. This result was in agreement with those of other studies. For example, McKinley et al. [7] reported that during data collection process, patients regularly received sedatives or opioids, but they were still anxious.
It is very difficult to diagnose and manage anxiety in ICU-admitted patients, especially in the ones receiving invasive ventilation where it is very difficult to communicate. In the current study, it took 18 months to get samples that could communicate with authors. Despite the fact that most of the study patients received sedatives, they still had a significant degree of anxiety. Therefore, it is important to be checked and diagnosed by the nurse, although unfortunately the patients were not routinely asked if they were anxious. To reduce anxiety, patient-centered approaches such as family meeting and training sessions are recommended [39]. Non-pharmacological interventions to reduce anxiety by nurses are also recommended. Music therapy [40] and sound interventions can reduce heart rate, blood pressure, and respiratory rate, and consequently, reduce the anxiety in ICU-admitted patients [33].
One of the limitations of the current study was its small sample size that was attributed to the high amount of time needed to find eligible samples. With a larger sample size, the findings would be different. A larger sample can better show changes in anxiety based on the causes of hospitalization. In most of the patients, anxiety could not be assessed due to lack of communication (because of low level of consciousness, instable physical conditions, or receiving high doses of sedatives). A one-item questionnaire is probably a good idea.
Another limitation was the absence of a psychiatrist to diagnose mental disorders and drug abuse. Therefore, it is suggested to assess mental disorders in future studies using structured clinical interviews based on Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Also, patients with history of mood disorders, anxiety, and depression were included in the study due to the low sample size, which may affect the results.
Conclusion
Anxiety and depression (symptoms of mood disorders) in the ICU-admitted patients were relatively high; the duration of hospitalization was significantly associated with anxiety and administration of sedatives had a significant correlation with depression. Also, the type of received mechanical ventilation was associated with both disorders. Based on the obtained results, routine screening of anxiety and depression by nurses in ICUs is useful for early diagnosis and treatment, which can prevent long-term complications of such disorders.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed about the purpose of the research and its implementation stages; They were also assured about the confidentiality of their information; Moreover, They were allowed to leave the study whenever they wish, and if desired, the results of the research would be available to them.
Funding
The present research program was Financial supported by the Research Committee of Guilan University of Medical Sciences, Rasht, Iran.
Authors contributions
The authors contributions is as follows: Conceptualization: Shahrokh Yousefzadeh-Chabok; Methodology: Naema Khodadadi-Hassankiadeh; Investigation: Alia Saberi; Writing–original draft: Atefeh Ghanbari khanghah; Writing–review & editing: Homa Zarrabi; Funding Acquisition: Mohammad Reza Yeganeh; Resources: Hamideh Hakimi; and Supervision: Anoush Dehnadi Moghadam.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to express our gratitude to the patients and the staff of Poorsina Hospital. We also would like to thank Ms. Kazemi for translating the manuscript.
References
- Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: A systematic review. Gen Hosp Psychiatry. 2008; 30(5):421-34. [DOI:10.1016/j.genhosppsych.2008.05.006] [PMID] [PMCID]
- Bashar FR, Vahedian Azimi A, Hajiesmaeili M, Salesi M, Farzanegan B, Shojaei S, et al. Post-ICU psychological morbidity in very long ICU stay patients with ARDS and delirium. Heart Lung. 2018; 43:88-94. [DOI:10.1016/j.jcrc.2017.08.034] [PMID]
- Davydow DS, Zatzick DF, Rivara FP, Jurkovich GJ, Wang J, Roy Byrne PP, et al. Predictors of posttraumatic stress disorder and return to usual major activity in traumatically injured intensive care unit survivors. Ann Gen Hosp Psychiatry. 2009; 31(5):428-35. [DOI:10.1016/j.genhosppsych.2009.05.007] [PMID] [PMCID]
- Granja C, Lopes A, Moreira S, Dias C, Costa Pereira A, Carneiro A. Patients’ recollections of experiences in the intensive care unit may affect their quality of life. Crit Care. 2005; 9(2):R96. [DOI:10.1186/cc3026] [PMID] [PMCID]
- Griffiths JA, Morgan K, Barber VS, Young JD. Study protocol: The Intensive Care Outcome Network (‘ICON’) study. BMC Health Serv Res. 2008; 8(1):132. [DOI:10.1186/1472-6963-8-132] [PMID] [PMCID]
- Myhren H, Ekeberg O, Toien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010; 14(1):R14. [DOI:10.1186/cc8870] [PMID] [PMCID]
- McKinley S, Stein Parbury J, Chehelnabi A, Lovas J. Assessment of anxiety in intensive care patients by using the Faces Anxiety Scale. Am J Crit Care. 2004; 13(2):146-52. [PMID]
- Frazier SK, Moser DK, Daley LK, McKinley S, Riegel B, Garvin BJ, et al. Critical care nurses’ beliefs about and reported management of anxiety. Am J Crit Care. 2003; 12(1):19-27. [PMID]
- O’donnell ML, Holmes AC, Creamer MC, Ellen S, Judson R, McFarlane AC, et al. The role of post-traumatic stress disorder and depression in predicting disability after injury. Med J Aust. 2009; 190(7):S71. [PMID]
- Stoll C, Schelling G, Goetz AE, Kilger E, Bayer A, Kapfhammer HP, et al. Health-related quality of life and post-traumatic stress disorder in patients after cardiac surgery and intensive care treatment. J Thorac Cardiovasc Surg. 2000; 120(3):505-12. [DOI:10.1067/mtc.2000.108162] [PMID]
- Beesley SJ, Hopkins RO, Holt Lunstad J, Wilson EL, Butler J, Kuttler KG, et al. Acute physiologic stress and subsequent anxiety among family members of ICU patients. Crit Care Med. 2018; 46(2):229-35. [DOI:10.1097/CCM.0000000000002835] [PMID] [PMCID]
- Wallen K, Chaboyer W, Thalib L, Creedy DK. Symptoms of acute posttraumatic stress disorder after intensive care. Am J Crit Care. 2008; 17(6):534-43. [PMID]
- Wang CH, Tsay SL, Elaine Bond A. Post‐traumatic stress disorder, depression, anxiety and quality of life in patients with traffic‐related injuries. J Adv Nurs. 2005; 52(1):22-30. [DOI:10.1111/j.1365-2648.2005.03560.x] [PMID]
- Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: A longitudinal cohort study. Lancet Resp Med. 2014; 2(5):369-79. [DOI:10.1016/S2213-2600(14)70051-7]
- Momennasab M, Ghahramani T, Yektatalab S, Zand F. Physical and mental health of patients immediately after discharge from intensive care unit and 24 hours later. Trauma Mon. 2016; 21(1):e29231. [DOI:10.5812/traumamon.29231] [PMID] [PMCID]
- Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. Depressive symptoms after critical illness: A systematic review and meta-analysis. Crit Care Med. 2016; 44(9):1744-53. [DOI:10.1097/CCM.0000000000001811] [PMID]
- Haines D, Hild J, He J, Stun L, Ballew A, Green JL, et al. A retrospective, pilot study of de novo antidepressant medication initiation in intensive care unit patients and oost-ICU depression. Crit Care Res Pract. 2017; 2017:5804860. [DOI:10.1155/2017/5804860]
- Wang S, Mosher C, Gao S, Kirk K, Lasiter S, Khan S, et al. Antidepressant use and depressive symptoms in intensive care unit survivors. Br J Hosp Med. 2017; 12(9):731-4. [DOI:10.12788/jhm.2814.] [PMID]
- Gómez Carretero P, Monsalve V, Soriano J, De Andrés J. [Emotional disorders and psychological needs of patients in an Intensive Care Unit (Spanish)]. Med Intensiva. 2006; 31(6):318-25. [DOI:10.1016/S0210-5691(07)74830-1]
- Islam S, Ahmed M, Walton GM, Dinan TG, Hoffman GR. The association between depression and anxiety disorders following facial trauma-A comparative study. Injury. 2010; 41(1):92-6. [DOI:10.1016/j.injury.2009.07.012] [PMID]
- Davydow DS, Desai SV, Needham DM, Bienvenu OJ. Psychiatric morbidity in survivors of the acute respiratory distress syndrome: A systematic review. Psychosom Med. 2008; 70(4):512-9. [DOI:10.1097/PSY.0b013e31816aa0dd] [PMID]
- Andersen FH, Flaatten H, Klepstad P, Follestad T, Strand K, Krüger AJ, et al. Long-term outcomes after ICU admission triage in octogenarians. Crit. Care Med. 2017; 45(4):e363-e71. [DOI:10.1097/CCM.0000000000002098] [PMID]
- Gayat E, Cariou A, Deye N, Vieillard Baron A, Jaber S, Damoisel C, et al. Determinants of long-term outcome in ICU survivors: Results from the FROG-ICU study. Crit Care. 2018; 22(1):8. [DOI:10.1186/s13054-017-1922-8] [PMID] [PMCID]
- Cardoso G, Alexandre J, Rosa A. Depression, anxiety and alcohol abuse in a gastroenterology intensive care unit: Prevalence and detection. Clin Pract Epidemiol Ment Health. 2010; 6:47-52. [DOI:10.2174/17450179010060100047] [PMID] [PMCID]
- Chlan LL. Relationship between two anxiety instruments in patients receiving mechanical ventilatory support. J Adv Nurs. 2004; 48(5):493-9. [DOI:10.1111/j.1365-2648.2004.03231.x] [PMID]
- Rattray J, Johnston M, Wildsmith J. Predictors of emotional outcomes of intensive care. Anaesth. 2005; 60(11):1085-92. [DOI:10.1111/j.1365-2044.2005.04336.x] [PMID]
- McKinley S, Madronio C. Validity of the faces anxiety scale for the assessment of state anxiety in intensive care patients not receiving mechanical ventilation. J Psychosom Res. 2008; 64(5):503-7. [DOI:10.1016/j.jpsychores.2008.02.002] [PMID]
- Bagherian R, Maroofi M, Gol MF, Zare F. [Prevalence of anxiety, depression and coping styles in myocardial infarction patients hospitalized in Isfahan hospitals (Persian)]. J Mazandaran Uni Med Sci. 2010; 20(77):36-45.
- Kaviani H, Seifourian H, Sharifi V, Ebrahimkhani N. [Reliability and validity of anxiety and depression hospital scales (HADS): Iranian patients with anxiety and depression disorders (Persian)]. Teh Uni Med J. 2009; 67(5):379-85.
- Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003; 1:14. [DOI:10.1186/1477-7525-1-19] [PMID] [PMCID]
- Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesth. 2001; 56(1):9-14. [DOI:10.1046/j.1365-2044.2001.01714.x] [PMID]
- Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, et al. Poverty and mental disorders: Breaking the cycle in low-income and middle-income countries. Lancet. 2011; 378(9801):1502-14. [DOI:10.1016/S0140-6736(11)60754-X]
- Saadatmand V, Rejeh N, Heravi Karimooi M, Tadrisi SD, Zayeri F, Vaismoradi M, et al. Effect of nature-based sounds’ intervention on agitation, anxiety, and stress in patients under mechanical ventilator support: A randomised controlled trial. Int J Nurs Stud. 2013; 50(7):895-904. [DOI:10.1016/j.ijnurstu.2012.11.018] [PMID]
- Pelosi P, Ball L, Brunetti I, Vargas M, Patroniti N. Tracheostomy in intensive care: Patients and families will never walk alone! Anaesth Crit Care Pain Med. 2018; 37(3):197-9. [DOI:10.1016/j.accpm.2018.04.001] [PMID]
- Mitate E, Kubota K, Ueki K, Inoue R, Inoue R, Momii K, et al. Speaking tracheostomy tube and modified mouthstick stylus in a ventilator-dependent patient with spinal cord injury. Case Rep Emerg Med. 2015; 2015:320357.
- Hwang MS, Lee MK, Song JR. Survey on self care, respiratory difficulty, sleep impediment, anxiety and depression among patients with neuromuscular disease dependent on home mechanical ventilator. Korean J Adult Nur. 2016; 28(5):595-606. [DOI:10.7475/kjan.2016.28.5.595]
- Székely A, Balog P, Benkö E, Breuer T, Székely J, Kertai MD, et al. Anxiety predicts mortality and morbidity after coronary artery and valve surgery-A 4-year follow-up study. Psychosom Med. 2007; 69(7):625-31. [DOI:10.1097/PSY.0b013e31814b8c0f] [PMID]
- Enger R, Andershed B. Nurses’ experience of the transfer of ICU patients to general wards: A great responsibility and a huge challenge. J Clin Nurs. 2018; 27(1-2):e186-e94. [DOI:10.1111/jocn.13911] [PMID]
- Brooke J, Hasan N, Slark J, Sharma P. Efficacy of information interventions in reducing transfer anxiety from a critical care setting to a general ward: A systematic review and meta-analysis. J Crit Care. 2012; 27(4):425. e9-15.
- Beaulieu Boire G, Bourque S, Chagnon F, Chouinard L, Gallo Payet N, Lesur O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward-a prospective interventional randomized crossover trial. J Crit Care. 2013; 28(4):442-50. [DOI:10.1016/j.jcrc.2013.01.007] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2018/01/17 | Accepted: 2018/09/27 | Published: 2018/10/1
Received: 2018/01/17 | Accepted: 2018/09/27 | Published: 2018/10/1
References
1. Davydow DS, Gifford JM, Desai SV, Needham DM, Bienvenu OJ. Posttraumatic stress disorder in general intensive care unit survivors: A systematic review. Gen Hosp Psychiatry. 2008; 30(5):421-34. [DOI:10.1016/j.genhosppsych.2008.05.006] [PMID] [PMCID] [DOI:10.1016/j.genhosppsych.2008.05.006]
2. Bashar FR, Vahedian Azimi A, Hajiesmaeili M, Salesi M, Farzanegan B, Shojaei S, et al. Post-ICU psychological morbidity in very long ICU stay patients with ARDS and delirium. Heart Lung. 2018; 43:88-94. [DOI:10.1016/j.jcrc.2017.08.034] [PMID] [DOI:10.1016/j.jcrc.2017.08.034]
3. Davydow DS, Zatzick DF, Rivara FP, Jurkovich GJ, Wang J, Roy Byrne PP, et al. Predictors of posttraumatic stress disorder and return to usual major activity in traumatically injured intensive care unit survivors. Ann Gen Hosp Psychiatry. 2009; 31(5):428-35. [DOI:10.1016/j.genhosppsych.2009.05.007] [PMID] [PMCID] [DOI:10.1016/j.genhosppsych.2009.05.007]
4. Granja C, Lopes A, Moreira S, Dias C, Costa Pereira A, Carneiro A. Patients' recollections of experiences in the intensive care unit may affect their quality of life. Crit Care. 2005; 9(2):R96. [DOI:10.1186/cc3026] [PMID] [PMCID] [DOI:10.1186/cc3026]
5. Griffiths JA, Morgan K, Barber VS, Young JD. Study protocol: The Intensive Care Outcome Network ('ICON') study. BMC Health Serv Res. 2008; 8(1):132. [DOI:10.1186/1472-6963-8-132] [PMID] [PMCID] [DOI:10.1186/1472-6963-8-132]
6. Myhren H, Ekeberg O, Toien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010; 14(1):R14. [DOI:10.1186/cc8870] [PMID] [PMCID] [DOI:10.1186/cc8870]
7. McKinley S, Stein Parbury J, Chehelnabi A, Lovas J. Assessment of anxiety in intensive care patients by using the Faces Anxiety Scale. Am J Crit Care. 2004; 13(2):146-52. [PMID] [PMID]
8. Frazier SK, Moser DK, Daley LK, McKinley S, Riegel B, Garvin BJ, et al. Critical care nurses' beliefs about and reported management of anxiety. Am J Crit Care. 2003; 12(1):19-27. [PMID] [PMID]
9. O'donnell ML, Holmes AC, Creamer MC, Ellen S, Judson R, McFarlane AC, et al. The role of post-traumatic stress disorder and depression in predicting disability after injury. Med J Aust. 2009; 190(7):S71. [PMID] [PMID]
10. Stoll C, Schelling G, Goetz AE, Kilger E, Bayer A, Kapfhammer HP, et al. Health-related quality of life and post-traumatic stress disorder in patients after cardiac surgery and intensive care treatment. J Thorac Cardiovasc Surg. 2000; 120(3):505-12. [DOI:10.1067/mtc.2000.108162] [PMID] [DOI:10.1067/mtc.2000.108162]
11. Beesley SJ, Hopkins RO, Holt Lunstad J, Wilson EL, Butler J, Kuttler KG, et al. Acute physiologic stress and subsequent anxiety among family members of ICU patients. Crit Care Med. 2018; 46(2):229-35. [DOI:10.1097/CCM.0000000000002835] [PMID] [PMCID] [DOI:10.1097/CCM.0000000000002835]
12. Wallen K, Chaboyer W, Thalib L, Creedy DK. Symptoms of acute posttraumatic stress disorder after intensive care. Am J Crit Care. 2008; 17(6):534-43. [PMID] [PMID]
13. Wang CH, Tsay SL, Elaine Bond A. Post‐traumatic stress disorder, depression, anxiety and quality of life in patients with traffic‐related injuries. J Adv Nurs. 2005; 52(1):22-30. [DOI:10.1111/j.1365-2648.2005.03560.x] [PMID] [DOI:10.1111/j.1365-2648.2005.03560.x]
14. Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: A longitudinal cohort study. Lancet Resp Med. 2014; 2(5):369-79. [DOI:10.1016/S2213-2600(14)70051-7] [DOI:10.1016/S2213-2600(14)70051-7]
15. Momennasab M, Ghahramani T, Yektatalab S, Zand F. Physical and mental health of patients immediately after discharge from intensive care unit and 24 hours later. Trauma Mon. 2016; 21(1):e29231. [DOI:10.5812/traumamon.29231] [PMID] [PMCID] [DOI:10.5812/traumamon.29231]
16. Rabiee A, Nikayin S, Hashem MD, Huang M, Dinglas VD, Bienvenu OJ, et al. Depressive symptoms after critical illness: A systematic review and meta-analysis. Crit Care Med. 2016; 44(9):1744-53. [DOI:10.1097/CCM.0000000000001811] [PMID] [DOI:10.1097/CCM.0000000000001811]
17. Haines D, Hild J, He J, Stun L, Ballew A, Green JL, et al. A retrospective, pilot study of de novo antidepressant medication initiation in intensive care unit patients and oost-ICU depression. Crit Care Res Pract. 2017; 2017:5804860. [DOI:10.1155/2017/5804860] [DOI:10.1155/2017/5804860]
18. Wang S, Mosher C, Gao S, Kirk K, Lasiter S, Khan S, et al. Antidepressant use and depressive symptoms in intensive care unit survivors. Br J Hosp Med. 2017; 12(9):731-4. [DOI:10.12788/jhm.2814.] [PMID] [DOI:10.12788/jhm.2814]
19. Gómez Carretero P, Monsalve V, Soriano J, De Andrés J. [Emotional disorders and psychological needs of patients in an Intensive Care Unit (Spanish)]. Med Intensiva. 2006; 31(6):318-25. [DOI:10.1016/S0210-5691(07)74830-1] [DOI:10.1016/S0210-5691(07)74830-1]
20. Islam S, Ahmed M, Walton GM, Dinan TG, Hoffman GR. The association between depression and anxiety disorders following facial trauma-A comparative study. Injury. 2010; 41(1):92-6. [DOI:10.1016/j.injury.2009.07.012] [PMID] [DOI:10.1016/j.injury.2009.07.012]
21. Davydow DS, Desai SV, Needham DM, Bienvenu OJ. Psychiatric morbidity in survivors of the acute respiratory distress syndrome: A systematic review. Psychosom Med. 2008; 70(4):512-9. [DOI:10.1097/PSY.0b013e31816aa0dd] [PMID] [DOI:10.1097/PSY.0b013e31816aa0dd]
22. Andersen FH, Flaatten H, Klepstad P, Follestad T, Strand K, Krüger AJ, et al. Long-term outcomes after ICU admission triage in octogenarians. Crit. Care Med. 2017; 45(4):e363-e71. [DOI:10.1097/CCM.0000000000002098] [PMID] [DOI:10.1097/CCM.0000000000002098]
23. Gayat E, Cariou A, Deye N, Vieillard Baron A, Jaber S, Damoisel C, et al. Determinants of long-term outcome in ICU survivors: Results from the FROG-ICU study. Crit Care. 2018; 22(1):8. [DOI:10.1186/s13054-017-1922-8] [PMID] [PMCID] [DOI:10.1186/s13054-017-1922-8]
24. Cardoso G, Alexandre J, Rosa A. Depression, anxiety and alcohol abuse in a gastroenterology intensive care unit: Prevalence and detection. Clin Pract Epidemiol Ment Health. 2010; 6:47-52. [DOI:10.2174/17450179010060100047] [PMID] [PMCID] [DOI:10.2174/17450179010060100047]
25. Chlan LL. Relationship between two anxiety instruments in patients receiving mechanical ventilatory support. J Adv Nurs. 2004; 48(5):493-9. [DOI:10.1111/j.1365-2648.2004.03231.x] [PMID] [DOI:10.1111/j.1365-2648.2004.03231.x]
26. Rattray J, Johnston M, Wildsmith J. Predictors of emotional outcomes of intensive care. Anaesth. 2005; 60(11):1085-92. [DOI:10.1111/j.1365-2044.2005.04336.x] [PMID] [DOI:10.1111/j.1365-2044.2005.04336.x]
27. McKinley S, Madronio C. Validity of the faces anxiety scale for the assessment of state anxiety in intensive care patients not receiving mechanical ventilation. J Psychosom Res. 2008; 64(5):503-7. [DOI:10.1016/j.jpsychores.2008.02.002] [PMID] [DOI:10.1016/j.jpsychores.2008.02.002]
28. Bagherian R, Maroofi M, Gol MF, Zare F. [Prevalence of anxiety, depression and coping styles in myocardial infarction patients hospitalized in Isfahan hospitals (Persian)]. J Mazandaran Uni Med Sci. 2010; 20(77):36-45.
29. Kaviani H, Seifourian H, Sharifi V, Ebrahimkhani N. [Reliability and validity of anxiety and depression hospital scales (HADS): Iranian patients with anxiety and depression disorders (Persian)]. Teh Uni Med J. 2009; 67(5):379-85.
30. Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003; 1:14. [DOI:10.1186/1477-7525-1-19] [PMID] [PMCID] [DOI:10.1186/1477-7525-1-19]
31. Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesth. 2001; 56(1):9-14. [DOI:10.1046/j.1365-2044.2001.01714.x] [PMID] [DOI:10.1046/j.1365-2044.2001.01714.x]
32. Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, et al. Poverty and mental disorders: Breaking the cycle in low-income and middle-income countries. Lancet. 2011; 378(9801):1502-14. [DOI:10.1016/S0140-6736(11)60754-X] [DOI:10.1016/S0140-6736(11)60754-X]
33. Saadatmand V, Rejeh N, Heravi Karimooi M, Tadrisi SD, Zayeri F, Vaismoradi M, et al. Effect of nature-based sounds' intervention on agitation, anxiety, and stress in patients under mechanical ventilator support: A randomised controlled trial. Int J Nurs Stud. 2013; 50(7):895-904. [DOI:10.1016/j.ijnurstu.2012.11.018] [PMID] [DOI:10.1016/j.ijnurstu.2012.11.018]
34. Pelosi P, Ball L, Brunetti I, Vargas M, Patroniti N. Tracheostomy in intensive care: Patients and families will never walk alone! Anaesth Crit Care Pain Med. 2018; 37(3):197-9. [DOI:10.1016/j.accpm.2018.04.001] [PMID] [DOI:10.1016/j.accpm.2018.04.001]
35. Mitate E, Kubota K, Ueki K, Inoue R, Inoue R, Momii K, et al. Speaking tracheostomy tube and modified mouthstick stylus in a ventilator-dependent patient with spinal cord injury. Case Rep Emerg Med. 2015; 2015:320357. [DOI:10.1155/2015/320357]
36. Hwang MS, Lee MK, Song JR. Survey on self care, respiratory difficulty, sleep impediment, anxiety and depression among patients with neuromuscular disease dependent on home mechanical ventilator. Korean J Adult Nur. 2016; 28(5):595-606. [DOI:10.7475/kjan.2016.28.5.595] [DOI:10.7475/kjan.2016.28.5.595]
37. Székely A, Balog P, Benkö E, Breuer T, Székely J, Kertai MD, et al. Anxiety predicts mortality and morbidity after coronary artery and valve surgery-A 4-year follow-up study. Psychosom Med. 2007; 69(7):625-31. [DOI:10.1097/PSY.0b013e31814b8c0f] [PMID] [DOI:10.1097/PSY.0b013e31814b8c0f]
38. Enger R, Andershed B. Nurses' experience of the transfer of ICU patients to general wards: A great responsibility and a huge challenge. J Clin Nurs. 2018; 27(1-2):e186-e94. [DOI:10.1111/jocn.13911] [PMID] [DOI:10.1111/jocn.13911]
39. Brooke J, Hasan N, Slark J, Sharma P. Efficacy of information interventions in reducing transfer anxiety from a critical care setting to a general ward: A systematic review and meta-analysis. J Crit Care. 2012; 27(4):425. e9-15.
40. Beaulieu Boire G, Bourque S, Chagnon F, Chouinard L, Gallo Payet N, Lesur O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward-a prospective interventional randomized crossover trial. J Crit Care. 2013; 28(4):442-50. [DOI:10.1016/j.jcrc.2013.01.007] [PMID] [DOI:10.1016/j.jcrc.2013.01.007]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |