Sat, Apr 27, 2024
Volume 4, Issue 2 (Spring 2018)
Caspian J Neurol Sci 2018, 4(2): 64-70 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezapour P, Borjali A, Hatamian H, Shafaei F, Janalipour K. Effectiveness of Acceptance and Commitment Therapy in Pain Control in Multiple Sclerotic Women. Caspian J Neurol Sci 2018; 4 (2) :64-70
URL: http://cjns.gums.ac.ir/article-1-153-en.html
URL: http://cjns.gums.ac.ir/article-1-153-en.html
1- Department of Psychology, Faculty of Clinical Psychology, Allameh Tabataba’i University, Tehran, Iran , rezapour.info@gmail.com
2- Associate Professor of Psychology, Department of Psychology, Faculty of Clinical Psychology, Allameh Tabataba’i University, Tehran, Iran
3- Department of Neurology, Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
4- Neuroscience Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran
5- Department of Psychology, Faculty of Literature and Humanities, Urmia University, Urmia, Iran
2- Associate Professor of Psychology, Department of Psychology, Faculty of Clinical Psychology, Allameh Tabataba’i University, Tehran, Iran
3- Department of Neurology, Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
4- Neuroscience Research Center, Poursina Hospital, Guilan University of Medical Sciences, Rasht, Iran
5- Department of Psychology, Faculty of Literature and Humanities, Urmia University, Urmia, Iran
Full-Text [PDF 913 kb]
(895 Downloads)
| Abstract (HTML) (3172 Views)
Full-Text: (855 Views)
Introduction
Multiple Sclerosis (MS) is a common chronic condition that involves the central nervous system [1]. It typically causes the inflammation and damage of the myelin sheath surrounding the nerve fibers in the brain and spinal cord [2]. Mostly occurs in individuals of 20-40 years old and afflicts two to threefold more women as men [3]. In addition to the sensory, motor and cognitive symptoms of MS, emotional ones are also the symptoms of the disease [4]. This immensely affects the patient’s social activities and their quality of life. Functional changes, including movement disorders, early fatigue and tension headaches, cause MS patients to withdraw from many social and work activities and negatively affects their social relationships.
Pain is a common MS symptom that plays a key role in the mental health and quality of life of the patients [5]. Pain that lasts more than three to six months is called chronic pain. Chronic pain in these patients is due to continuous accumulation of injury and incomplete return injury to the previous attack. Chronic pain is associated with poor compatibility, which involves depression and poor self-esteem. Pain, including tension headaches, is common in the MS patients and has recently been known to play a key role in their mental health and quality of life [6]. Therefore, this disease is harmful to both the active populations of the society. Severe pain is associated with a poorer score in most of the subscales for the Short-Form health survey (SF-36), such as general health, vitality, mental health and social function [7].
Pharmacological pain control is challenging in the MS patients. Even persistent efforts have failed to control pain in these patients; e.g. although carbamazepine may affect in the first stage of neuralgia, it loses its effectiveness in due course of time. Controlling chronic pain is particularly complicated, as there are no definite guidelines for their pharmacological treatment. Despite, the growing evidence that confirms the effectiveness of several categories of the medicines, persistent and progressive pain are yet common in MS patients. In addition to the imposed costing over the patients, chronic pain causes sides effects like hypoventilation, nausea and gastrointestinal bleeding [8]. To relieve the pain in these patients, four groups of medicines are used, including analgesics, opiates, MS medications and antidepressants [5]. Moreover, compelling evidences suggest that the psychological component of pain can significantly contribute in determining the pain perception, experiencing the pain intensity, functional effects of the pain, emotional well-being and response to the treatment [9].
Pain is associated with negative emotions, which in turn causes the pain persistence [10]; nevertheless, all the patients with chronic pain do not present the psychological problems [11]. Research suggests that patients with chronic pain, even with seemingly similar clinical symptoms, may present totally different degrees of the psychological dysfunction. The experience of chronic pain is often associated with substantial distress and disability. There is now a well-established database indicating that psychological and behavioral processes are strongly related to the patient physical and emotional functioning.
Psychological approaches to the chronic pain management target the behavioral, emotional and cognitive elements of chronic pain and its preserver agents. It involves interventions which aim to improve the self-management and modify behavior and cognition rather than directly eliminating the pain [12]. The psychological interventions frequently applied so far included psycho-physical techniques (i.e. biofeedback), behavioral approaches, cognitive behavioral therapies and acceptance-based interventions [13].
ACT is the most common acceptance-based treatment that aims to help clients achieve a more valuable and satisfactory life by improving the psychological flexibility. This will be achieved by promoting the ability to contact with the present moment and choose the most appropriate action among the different alternatives, not for avoiding turbulent thoughts, feelings, memories and inclinations. This therapeutic method involves six core processes that cause psychological flexibility, namely acceptance, cognitive defusing, being present, self as context, values and committed actions [14]. In other words, ACT is an approach that combines mindfulness-associated processes with behavior change methods [15].
According to acceptance and commitment theory, by chronic pain, patients’ reaction to the pain deprives them of the healthy life. These patients may anxiously approach to their pain and move away from valuable and important aspects of their life and generally turn to control or avoid terrible experiences, while these behaviors do not exert any positive effects [16]. ACT targets inefficient control and avoidance strategies by developing techniques that cause psychological flexibility [17]. This method helps the patients to accept and experience the pain, undesirable events and pain-associated thoughts and improve meaningful aspects of life while encouraging them to perform valuable activities instead of making useless attempts against the pain [18].
Some studies suggest the effectiveness of ACT on the pain-related anxiety and depression, feeling disabled, occupational performance and the frequency of doctor visit [18]. Some other studies also reported the effects of intervening variables of pain such as beliefs about pain-associated damage and self-efficacy [19]. Furthermore, several controlled studies supported the effect of ACT on alleviating chronic pains [20, 21]. Comparing the ACT with interdisciplinary therapies indicated the preference of ACT for improving pain-associated functional abilities and quality of life, overcoming the fear of movement and reducing the pains complaints [22].
The effectiveness of ACT in pain acceptance, pain-related anxiety and pain intensity has been demonstrated in patients with chronic pains by the few studies conducted in Iran [23-25]. The ACT-based group therapy has shown to significantly increase the quality of life and self-efficacy in MS patients [26]. Given the lack of definitive treatment for MS, ACT can be considered as a proper alternative for enhancing the skills of dealing with and accepting the disease. Furthermore, given the prevalence of MS in Iran [27], particularly in women and the lack of research resources, further studies are recommended on the effectiveness of the newly-found ACT in the Iranian population. The present study was therefore performed to examine the effectiveness of the acceptance and commitment-based group therapy in pain control in the women with MS.
Materials and Methods
The research was designed such that all the patients in the two groups were identical in terms of use of anesthesia and sedation. The present semi-experimental study was conducted on control and experimental group in 2014-2015. The statistical population comprised of only women with MS. Convenience sampling was used to select the subjects from the volunteers who gathered in Sari MS Society in the north of Iran, following an announcement. Eighteen subjects were randomly assigned to the experimental group (n=9) and the control group (n=9) by using the random sampling table.
The inclusion criteria consisted of Relapsing-Remitting (RR) type of MS, age between 20-30 years, the disease was diagnosed at least one year before the study and the level of education was between high-school diploma and bachelor’s degree. The exclusion criteria comprised of having a history of receiving stress management or relaxation training, presenting severe symptoms of the disease during the program and being absent for more than two sessions.
Data collection tools
The 10-item Pain Self-Efficacy Questionnaire (PSEQ) of the Nicholas was a self-report instrument developed in 1989 to automatically assess the patients with chronic pain. The items were scored on a 7-point Likert scale from 0=not at all confident to 6=completely confident based on the patient’s self-assessment of their ability to perform a group of activities despite their pain [28]. Nicholas reported the internal consistency of the question was 0.92 by Cronbach’s alpha method. In another study by Asghari and Nicholas, Cronbach’s Alpha was 0.94 [29]. Cronbach’s alpha of 0.89 in this study confirmed the reliability of this tool.
Therapeutic sessions
The therapeutic protocol of the present study intervention was developed by Abedi [23] based on the work and therapy method of Hayes [14] and involves eight 2-hour sessions.
Session 1: Established the therapeutic relationship, familiarized the patients with the study subject and treatment, completed the questionnaire and signed the therapeutic contract.
Session 2: Identified and examined the therapeutic methods that suited the patients, evaluated their effectiveness, discussed their temporary nature and insignificant effects.
Session 3: Helped the clients identify the inefficient control strategies, realized their uselessness and accepted the terrible personal events while avoided to struggle with them.
Session 4: Explained how to avoid terrible experiences and become aware of their consequences, taught the acceptance steps, changed the language concepts using allegory, taught relaxation, received feedbacks and gave homework.
Session 5: Introduced a three-dimensional model to express the common relationship among behavior, feelings, psychological functions and observable behavior and discussed how to attempt to modify behavior accordingly, received feedbacks and gave homework.
Session 6: Explained the implications of the role and context, perceived self as a context and made contact with him, understood different sensory sensations and separated from senses that were a part of the mental content, received feedbacks and gave homework.
Session 7: Explained the concept of values, encouraged the change and enabled the clients to have a better life, the core practice, received feedbacks and gave homework.
Session 8: Taught commitment towards action, identified the behavior models based on the values and supported commitment to follow them, summarized the sessions and performed the post-test.
Method of implementation
Convenience sampling method was used to select the samples. After investigating the subjects’ profiles, the researchers selected 18 participants from the volunteers and randomly assigned them to the control and experimental groups. The main purpose of examining the profiles was to achieve a homogenous group. After presenting to the MS Society in Sari, a notice was put up in this center containing brief information about ACT, MS and the effective factors. The participants were asked to make the necessary coordination with the person in charge of the public relations.
In the enrollment stage, the applicants were asked to provide public relations with their details, including age, level of education, duration of the disease and their cell phone number, so that the researcher could contact the subjects in the following stages. In this stage, the patients were not allowed to examine the profiles. After the number of subjects reached the desired limit, their names were divided into a waiting list and an experimental list. After selecting the samples, the post-test was performed, their results were analyzed, and the patients admitted their pain. The subjects were then assigned to the control and experimental groups. The experimental group then attended 8 sessions of ACT. Both groups ultimately took the post-test and were followed up after 1.5 months.
Results
Participants with a mean age of 26.93±6.35 years participated in this study, in two groups of experimental and control, with this conditional statement; a person with MS. Six member of the participants had a diploma, two had an undergraduate degree and six had bachelor’s degree.
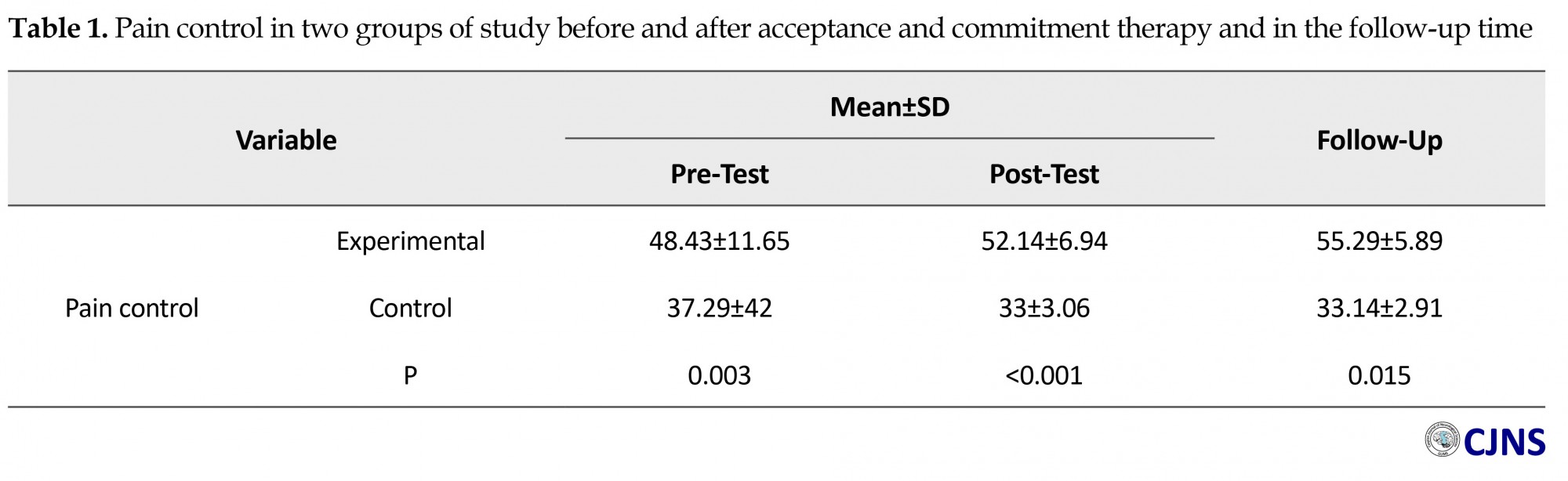
Due to the need for a proper understanding of the topic presented to the subjects and the ability of the subjects to perform the assignments, creating more homogeneity in the group, at least the education of the participants was considered to be the diploma or the bachelor’s degree. Another criterion was the duration of the disease, which was considered to be at least one year. The compatibility crisis is likely to be resolved or reduced early, and it is a part of the patient’s life, the usual course of the patient’s prescribed drug was well established. The cognitive function of the patient has not been severely damaged. The person has to be in the RR stage and has the ability to attend meetings and carry out the assignments. Table 1 presents the descriptive findings associated with the pain control in the two groups of study, before and after the intervention and in the follow-up time.
Multiple Sclerosis (MS) is a common chronic condition that involves the central nervous system [1]. It typically causes the inflammation and damage of the myelin sheath surrounding the nerve fibers in the brain and spinal cord [2]. Mostly occurs in individuals of 20-40 years old and afflicts two to threefold more women as men [3]. In addition to the sensory, motor and cognitive symptoms of MS, emotional ones are also the symptoms of the disease [4]. This immensely affects the patient’s social activities and their quality of life. Functional changes, including movement disorders, early fatigue and tension headaches, cause MS patients to withdraw from many social and work activities and negatively affects their social relationships.
Pain is a common MS symptom that plays a key role in the mental health and quality of life of the patients [5]. Pain that lasts more than three to six months is called chronic pain. Chronic pain in these patients is due to continuous accumulation of injury and incomplete return injury to the previous attack. Chronic pain is associated with poor compatibility, which involves depression and poor self-esteem. Pain, including tension headaches, is common in the MS patients and has recently been known to play a key role in their mental health and quality of life [6]. Therefore, this disease is harmful to both the active populations of the society. Severe pain is associated with a poorer score in most of the subscales for the Short-Form health survey (SF-36), such as general health, vitality, mental health and social function [7].
Pharmacological pain control is challenging in the MS patients. Even persistent efforts have failed to control pain in these patients; e.g. although carbamazepine may affect in the first stage of neuralgia, it loses its effectiveness in due course of time. Controlling chronic pain is particularly complicated, as there are no definite guidelines for their pharmacological treatment. Despite, the growing evidence that confirms the effectiveness of several categories of the medicines, persistent and progressive pain are yet common in MS patients. In addition to the imposed costing over the patients, chronic pain causes sides effects like hypoventilation, nausea and gastrointestinal bleeding [8]. To relieve the pain in these patients, four groups of medicines are used, including analgesics, opiates, MS medications and antidepressants [5]. Moreover, compelling evidences suggest that the psychological component of pain can significantly contribute in determining the pain perception, experiencing the pain intensity, functional effects of the pain, emotional well-being and response to the treatment [9].
Pain is associated with negative emotions, which in turn causes the pain persistence [10]; nevertheless, all the patients with chronic pain do not present the psychological problems [11]. Research suggests that patients with chronic pain, even with seemingly similar clinical symptoms, may present totally different degrees of the psychological dysfunction. The experience of chronic pain is often associated with substantial distress and disability. There is now a well-established database indicating that psychological and behavioral processes are strongly related to the patient physical and emotional functioning.
Psychological approaches to the chronic pain management target the behavioral, emotional and cognitive elements of chronic pain and its preserver agents. It involves interventions which aim to improve the self-management and modify behavior and cognition rather than directly eliminating the pain [12]. The psychological interventions frequently applied so far included psycho-physical techniques (i.e. biofeedback), behavioral approaches, cognitive behavioral therapies and acceptance-based interventions [13].
ACT is the most common acceptance-based treatment that aims to help clients achieve a more valuable and satisfactory life by improving the psychological flexibility. This will be achieved by promoting the ability to contact with the present moment and choose the most appropriate action among the different alternatives, not for avoiding turbulent thoughts, feelings, memories and inclinations. This therapeutic method involves six core processes that cause psychological flexibility, namely acceptance, cognitive defusing, being present, self as context, values and committed actions [14]. In other words, ACT is an approach that combines mindfulness-associated processes with behavior change methods [15].
According to acceptance and commitment theory, by chronic pain, patients’ reaction to the pain deprives them of the healthy life. These patients may anxiously approach to their pain and move away from valuable and important aspects of their life and generally turn to control or avoid terrible experiences, while these behaviors do not exert any positive effects [16]. ACT targets inefficient control and avoidance strategies by developing techniques that cause psychological flexibility [17]. This method helps the patients to accept and experience the pain, undesirable events and pain-associated thoughts and improve meaningful aspects of life while encouraging them to perform valuable activities instead of making useless attempts against the pain [18].
Some studies suggest the effectiveness of ACT on the pain-related anxiety and depression, feeling disabled, occupational performance and the frequency of doctor visit [18]. Some other studies also reported the effects of intervening variables of pain such as beliefs about pain-associated damage and self-efficacy [19]. Furthermore, several controlled studies supported the effect of ACT on alleviating chronic pains [20, 21]. Comparing the ACT with interdisciplinary therapies indicated the preference of ACT for improving pain-associated functional abilities and quality of life, overcoming the fear of movement and reducing the pains complaints [22].
The effectiveness of ACT in pain acceptance, pain-related anxiety and pain intensity has been demonstrated in patients with chronic pains by the few studies conducted in Iran [23-25]. The ACT-based group therapy has shown to significantly increase the quality of life and self-efficacy in MS patients [26]. Given the lack of definitive treatment for MS, ACT can be considered as a proper alternative for enhancing the skills of dealing with and accepting the disease. Furthermore, given the prevalence of MS in Iran [27], particularly in women and the lack of research resources, further studies are recommended on the effectiveness of the newly-found ACT in the Iranian population. The present study was therefore performed to examine the effectiveness of the acceptance and commitment-based group therapy in pain control in the women with MS.
Materials and Methods
The research was designed such that all the patients in the two groups were identical in terms of use of anesthesia and sedation. The present semi-experimental study was conducted on control and experimental group in 2014-2015. The statistical population comprised of only women with MS. Convenience sampling was used to select the subjects from the volunteers who gathered in Sari MS Society in the north of Iran, following an announcement. Eighteen subjects were randomly assigned to the experimental group (n=9) and the control group (n=9) by using the random sampling table.
The inclusion criteria consisted of Relapsing-Remitting (RR) type of MS, age between 20-30 years, the disease was diagnosed at least one year before the study and the level of education was between high-school diploma and bachelor’s degree. The exclusion criteria comprised of having a history of receiving stress management or relaxation training, presenting severe symptoms of the disease during the program and being absent for more than two sessions.
Data collection tools
The 10-item Pain Self-Efficacy Questionnaire (PSEQ) of the Nicholas was a self-report instrument developed in 1989 to automatically assess the patients with chronic pain. The items were scored on a 7-point Likert scale from 0=not at all confident to 6=completely confident based on the patient’s self-assessment of their ability to perform a group of activities despite their pain [28]. Nicholas reported the internal consistency of the question was 0.92 by Cronbach’s alpha method. In another study by Asghari and Nicholas, Cronbach’s Alpha was 0.94 [29]. Cronbach’s alpha of 0.89 in this study confirmed the reliability of this tool.
Therapeutic sessions
The therapeutic protocol of the present study intervention was developed by Abedi [23] based on the work and therapy method of Hayes [14] and involves eight 2-hour sessions.
Session 1: Established the therapeutic relationship, familiarized the patients with the study subject and treatment, completed the questionnaire and signed the therapeutic contract.
Session 2: Identified and examined the therapeutic methods that suited the patients, evaluated their effectiveness, discussed their temporary nature and insignificant effects.
Session 3: Helped the clients identify the inefficient control strategies, realized their uselessness and accepted the terrible personal events while avoided to struggle with them.
Session 4: Explained how to avoid terrible experiences and become aware of their consequences, taught the acceptance steps, changed the language concepts using allegory, taught relaxation, received feedbacks and gave homework.
Session 5: Introduced a three-dimensional model to express the common relationship among behavior, feelings, psychological functions and observable behavior and discussed how to attempt to modify behavior accordingly, received feedbacks and gave homework.
Session 6: Explained the implications of the role and context, perceived self as a context and made contact with him, understood different sensory sensations and separated from senses that were a part of the mental content, received feedbacks and gave homework.
Session 7: Explained the concept of values, encouraged the change and enabled the clients to have a better life, the core practice, received feedbacks and gave homework.
Session 8: Taught commitment towards action, identified the behavior models based on the values and supported commitment to follow them, summarized the sessions and performed the post-test.
Method of implementation
Convenience sampling method was used to select the samples. After investigating the subjects’ profiles, the researchers selected 18 participants from the volunteers and randomly assigned them to the control and experimental groups. The main purpose of examining the profiles was to achieve a homogenous group. After presenting to the MS Society in Sari, a notice was put up in this center containing brief information about ACT, MS and the effective factors. The participants were asked to make the necessary coordination with the person in charge of the public relations.
In the enrollment stage, the applicants were asked to provide public relations with their details, including age, level of education, duration of the disease and their cell phone number, so that the researcher could contact the subjects in the following stages. In this stage, the patients were not allowed to examine the profiles. After the number of subjects reached the desired limit, their names were divided into a waiting list and an experimental list. After selecting the samples, the post-test was performed, their results were analyzed, and the patients admitted their pain. The subjects were then assigned to the control and experimental groups. The experimental group then attended 8 sessions of ACT. Both groups ultimately took the post-test and were followed up after 1.5 months.
Results
Participants with a mean age of 26.93±6.35 years participated in this study, in two groups of experimental and control, with this conditional statement; a person with MS. Six member of the participants had a diploma, two had an undergraduate degree and six had bachelor’s degree.
Due to the need for a proper understanding of the topic presented to the subjects and the ability of the subjects to perform the assignments, creating more homogeneity in the group, at least the education of the participants was considered to be the diploma or the bachelor’s degree. Another criterion was the duration of the disease, which was considered to be at least one year. The compatibility crisis is likely to be resolved or reduced early, and it is a part of the patient’s life, the usual course of the patient’s prescribed drug was well established. The cognitive function of the patient has not been severely damaged. The person has to be in the RR stage and has the ability to attend meetings and carry out the assignments. Table 1 presents the descriptive findings associated with the pain control in the two groups of study, before and after the intervention and in the follow-up time.
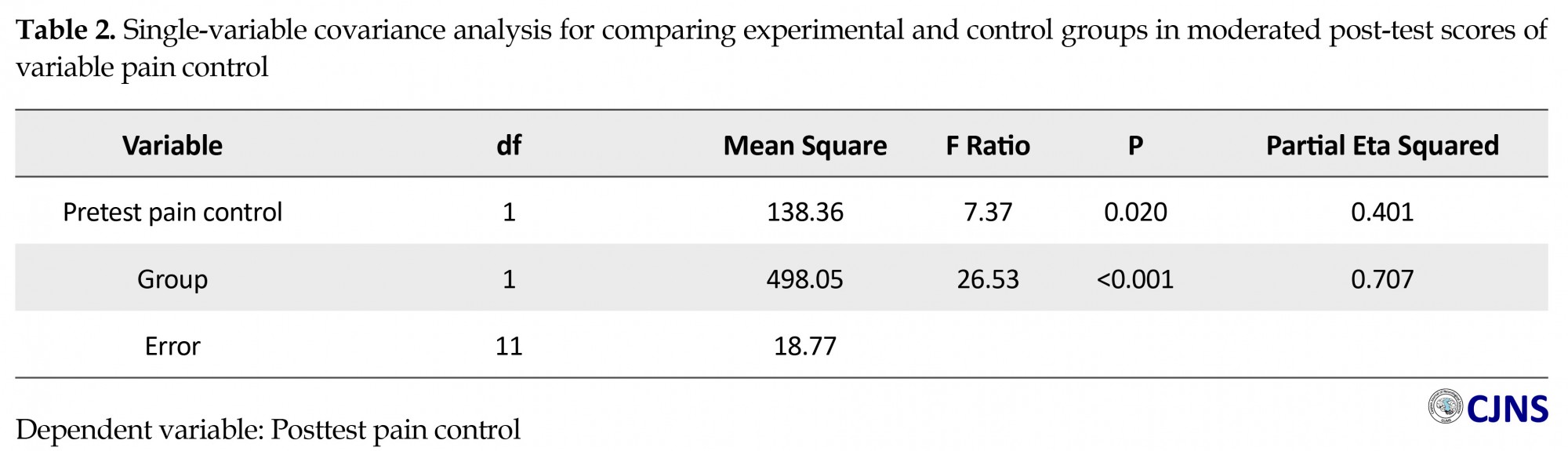
Does ACT affect the post-test pain control in the women with MS as compared to the control group? ANCOVA was used to investigate the effectiveness of ACT in pain control in the MS patients. Regression slopes and Levene’s test were first analyzed. Given that this interaction was statistically insignificant (P>0.05), the hypotheses of the homogeneity of the regression slopes and homogeneity of the variance were confirmed, this depicted the reliability of the following results.
As seen in Table 2, the auxiliary random variables were significantly associated with the dependent variable. The significant levels obtained suggested the main group effect (F(1, 11)=26.53, P<0.001, µ2=0.71).
As seen in Table 2, the auxiliary random variables were significantly associated with the dependent variable. The significant levels obtained suggested the main group effect (F(1, 11)=26.53, P<0.001, µ2=0.71).
Does ACT affect pain control in the MS women after one-month follow-up as compared to the control group? Table 3 presents the Results of single-variable covariance analysis for comparing experimental and control groups in moderated follow-up scores of variable pain control and it is a part of the patient’s life, the usual course of the patient’s prescribed drug was well established. ANCOVA was used. Slopes of regression and Levene’s test were first examined for the homogeneity of the variance. Given that this interaction was statistically insignificant (P>0.05), the hypotheses of homogeneity of the regression slopes and homogeneity of variance were confirmed, this depicted the reliability of the upcoming results. The significant levels obtained suggested the main group effect (F(1, 11)=56.55, P=0.001, µ2=0.84).
Discussion
The present findings showed that the ACT caused significant differences between the two groups in terms of pain control. These differences persisted for 1.5 months. The findings obtained by Wicksell et al. [19, 21], Buhrman et al. [20], Anvari et al. [23], Irandoost et al. [23, 24], who confirmed the effectiveness of ACT in relieving the pain, were consistent with those obtained in the present study.
The study conducted by Anvari et al. [23] suggested the effectiveness of acceptance and commitment group therapy in accepting and alleviating pain in the male patients with chronic pain. Irandoost et al. [24] confirmed the effectiveness of ACT in reducing the pain experienced by women with chronic low back pain. To explain this finding, Wicksell et al. argued that ACT therapists help patients and make efforts to identify their personal values as a major path in their life, while considering the exposure to the previously avoided personal experiences the core of intervention with an emphasis on a more extended and flexible set of behaviors [22].
According to Hayes, ideas such as ‘If I work, my pain will intensify” are strong and emphasized the routes which were far from the expressed values such as ‘playing football and being a team member’ [14]. By helping the patient with the comprehension and recognition of the personal experiences with pain as they were, the therapist functionally analyzed the action consequences based on the thoughts and helped the patients to avoid or nullify these thoughts, while refrained from discussing about the correctness of these thoughts.
The program taught the patients to be more mindful, gradually learn to observe and recognize undesirable experiences by avoiding judgment and details. Learning these skills help the patients to properly identify and follow their goals rather than being like a person who is controlled by psychological events such as pain and fear of the predicted pain. Therefore, they adapted to their problems more effectively and experienced less physical pain and discomfort. Regarding the prolongation of the effect of this therapeutic method, McCracken & Vowles argued that accepting chronic pain can be considered as a behavior domain with two components. The first component is associated with the normal pursuit of daily activities even in the presence of pain. This type of concentration is beyond a psychological process, as it requires the patient to get involved in positive functional activities irrespective of the pain. The second component involves admitting that pain avoidance and control are inefficient solutions, whereas being present is an alternative that helps patients continuously move away from fighting for pain control towards their desired lifestyle and valuable aims [18].
The effectiveness of ACT can be explained by the processes governing this therapy, which involved mindfulness as an important technique. Numerous studies have confirmed the effect of mindfulness by improving the patients with chronic pain. For instance, Mc Cracken et al. investigated the role of mindfulness in chronic pain-associated suffering and disability and concluded that, after controlling demographic variables, pain intensity and pain acceptance, mindfulness can explain the variance of anxiety scores associated with pain and psychophysical disabilities. Cho et al. showed that mindfulness-based methods positively affect the patients with pain-related anxiety and disability. Schutzeet et al. demonstrated that mindfulness significantly and negatively predicts the negative emotions of pain debilitating, pain-related fear, pain hyper-viGuilance and functional disability which accounted for 17-41% of their variance [23].
Conclusion
The findings obtained from the present study suggested the increased post-test and follow-up scores of the pain control in MS patients; this indicated the effectiveness of this type of treatment. This therapeutic method broadens the horizon of clinical interventions and can be applied as a useful intervention. Despite the many efforts made, the present study has some limitations, including the small sample size and the use of convenience sampling, focusing on single gender and impossibility of generalization. Furthermore, given the relatively short follow-up, the stability of treatment effects cannot be guaranteed for longer periods.
Given the effect of ACT on pain control, future studies are recommended to focus on the effectiveness of ACT in other diseases, especially those associated with chronic pain. Given that the present study addresses only women with MS in Sari, further research is recommended on male patients and also in the different regions. To determine the extension of the treatment effects, long-term follow-up tests are proposed to be carried out. The consequences of ACT should also be compared with those of other treatment methods. Given the effect of ACT on pain control, institutions supporting MS patients and other associated organizations are recommended to provide the patients with the opportunity of using this type of treatment.
Ethical Considerations
Compliance with ethical guidelines
All participants were assured that their information would be confidential. The research process was also explained to them.
Funding
This article is derived from the MA thesis of Parisa Rezapour at Faculty of Psychology and Educational Sciences, Allame Tabatabaie University, Tehran, Iran.
Conflict of interest
The authors have no conflict of interest.
References
The present findings showed that the ACT caused significant differences between the two groups in terms of pain control. These differences persisted for 1.5 months. The findings obtained by Wicksell et al. [19, 21], Buhrman et al. [20], Anvari et al. [23], Irandoost et al. [23, 24], who confirmed the effectiveness of ACT in relieving the pain, were consistent with those obtained in the present study.
The study conducted by Anvari et al. [23] suggested the effectiveness of acceptance and commitment group therapy in accepting and alleviating pain in the male patients with chronic pain. Irandoost et al. [24] confirmed the effectiveness of ACT in reducing the pain experienced by women with chronic low back pain. To explain this finding, Wicksell et al. argued that ACT therapists help patients and make efforts to identify their personal values as a major path in their life, while considering the exposure to the previously avoided personal experiences the core of intervention with an emphasis on a more extended and flexible set of behaviors [22].
According to Hayes, ideas such as ‘If I work, my pain will intensify” are strong and emphasized the routes which were far from the expressed values such as ‘playing football and being a team member’ [14]. By helping the patient with the comprehension and recognition of the personal experiences with pain as they were, the therapist functionally analyzed the action consequences based on the thoughts and helped the patients to avoid or nullify these thoughts, while refrained from discussing about the correctness of these thoughts.
The program taught the patients to be more mindful, gradually learn to observe and recognize undesirable experiences by avoiding judgment and details. Learning these skills help the patients to properly identify and follow their goals rather than being like a person who is controlled by psychological events such as pain and fear of the predicted pain. Therefore, they adapted to their problems more effectively and experienced less physical pain and discomfort. Regarding the prolongation of the effect of this therapeutic method, McCracken & Vowles argued that accepting chronic pain can be considered as a behavior domain with two components. The first component is associated with the normal pursuit of daily activities even in the presence of pain. This type of concentration is beyond a psychological process, as it requires the patient to get involved in positive functional activities irrespective of the pain. The second component involves admitting that pain avoidance and control are inefficient solutions, whereas being present is an alternative that helps patients continuously move away from fighting for pain control towards their desired lifestyle and valuable aims [18].
The effectiveness of ACT can be explained by the processes governing this therapy, which involved mindfulness as an important technique. Numerous studies have confirmed the effect of mindfulness by improving the patients with chronic pain. For instance, Mc Cracken et al. investigated the role of mindfulness in chronic pain-associated suffering and disability and concluded that, after controlling demographic variables, pain intensity and pain acceptance, mindfulness can explain the variance of anxiety scores associated with pain and psychophysical disabilities. Cho et al. showed that mindfulness-based methods positively affect the patients with pain-related anxiety and disability. Schutzeet et al. demonstrated that mindfulness significantly and negatively predicts the negative emotions of pain debilitating, pain-related fear, pain hyper-viGuilance and functional disability which accounted for 17-41% of their variance [23].
Conclusion
The findings obtained from the present study suggested the increased post-test and follow-up scores of the pain control in MS patients; this indicated the effectiveness of this type of treatment. This therapeutic method broadens the horizon of clinical interventions and can be applied as a useful intervention. Despite the many efforts made, the present study has some limitations, including the small sample size and the use of convenience sampling, focusing on single gender and impossibility of generalization. Furthermore, given the relatively short follow-up, the stability of treatment effects cannot be guaranteed for longer periods.
Given the effect of ACT on pain control, future studies are recommended to focus on the effectiveness of ACT in other diseases, especially those associated with chronic pain. Given that the present study addresses only women with MS in Sari, further research is recommended on male patients and also in the different regions. To determine the extension of the treatment effects, long-term follow-up tests are proposed to be carried out. The consequences of ACT should also be compared with those of other treatment methods. Given the effect of ACT on pain control, institutions supporting MS patients and other associated organizations are recommended to provide the patients with the opportunity of using this type of treatment.
Ethical Considerations
Compliance with ethical guidelines
All participants were assured that their information would be confidential. The research process was also explained to them.
Funding
This article is derived from the MA thesis of Parisa Rezapour at Faculty of Psychology and Educational Sciences, Allame Tabatabaie University, Tehran, Iran.
Conflict of interest
The authors have no conflict of interest.
References
- Elliott DG. Migraine in multiple sclerosis. Int Rev Neurobiol. 2007; 79:281-302. [DOI:10.1016/S0074-7742(07)79012-8] [PMID]
- Burks JS. A review of the current medical aspects of multiple sclerosis. J Neuro Rehab. 1992; 6(3):131-9. [DOI:10.1177/136140969200600302]
- D’Amico D, La Mantia L, Rigamonti A, Usai S, Mascoli N, Milanese C, et al. Prevalence of primary headaches in people with multiple sclerosis. Cephalalgia. 2004; 24(11):980-4. [DOI:10.1111/j.1468-2982.2004.00790.x] [PMID]
- Santrock J. Psychology Training Guide context of Santrock. [M. Firoozbakht, Persian Trans.]. Tehran: Resa; 2003.
- Kenner M, Menon U, Elliott DG. Multiple sclerosis as a painful disease. Int Rev Neurobiol 2007; 79:303-21. [DOI:10.1016/S0074-7742(07)79013-X] [PMID]
- Gatchel RJ, Turk DC. Psychosocial factors in pain: Critical perspectives. New York: Guilford Press; 1999.
- Büssing A, Heusser P, Mundle G. Course of life satisfaction in patients with depressive and addictive disorders after therapeutic intervention. Int J Soc Psychiatry. 2012; 58(3):239-45. [DOI:10.1177/0020764010390498] [PMID]
- Clifford DB, Trotter JL. Pain in multiple sclerosis. Int J Soc Psychiatry. 1984; 41(12):1270-2. [DOI:10.1001/archneur.1984.04050230052017]
- Jensen MP, Turner JA, Romano JM. Chronic pain coping measures: Individual vs. composite scores. Pain. 1992; 51(3):273-80. [DOI:10.1016/0304-3959(92)90210-3] [PMID]
- Nash JM, Williams DM, Nicholson R, Trask PC. The contribution of pain-related anxiety to disability from headache. J Behav Med. 2006; 29(1):61-7. [DOI:10.1007/s10865-005-9033-4] [PMID]
- McCracken LM, Gauntlett-Gilbert J, Eccleston C. Acceptance of pain in adolescents with chronic pain: Validation of an adapted assessment instrument and preliminary correlation analyses. Eur J Pain. 2010; 14(3):316-20. [DOI:10.1016/j.ejpain.2009.05.002] [PMID]
- Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag. 2011; 4:41-9. [DOI:10.2147/PRBM.S15375] [PMID] [PMCID]
- Rudy TE, Turk DC, Zaki HS, Curtin HD. An empirical taxometric alternative to traditional classification of temporomandibular disorders. Pain. 1989; 36(3):311-20. [DOI:10.1016/0304-3959(89)90090-0] [PMID]
- Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies–republished article. Behav Ther. 2016; 47(6):869-85. [DOI:10.1016/j.beth.2016.11.006] [PMID]
- McCracken LM. Committed action: An application of the psychological flexibility model to activity patterns in chronic pain. J Pain. 2013; 14(8):828-35. [DOI:10.1016/j.jpain.2013.02.009] [PMID]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: The process and practice of mindful change. New York: Guilford Press; 2012.
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, Processes and outcomes. Behav Res Ther. 2006; 44:1-28. [DOI:10.1016/j.brat.2005.06.006] [PMID]
- McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Health Psychol. 2008; 27(2):215-20. [DOI:10.1037/0278-6133.27.2.215] [PMID]
- Wicksell RK, Olsson GL, Hayes SC. Mediators of change in acceptance and commitment therapy for pediatric chronic pain. Pain. 2011; 152(12):2792-801. [DOI:10.1016/j.pain.2011.09.003] [PMID]
- Buhrman M, Skoglund A, Husell J, Bergström K, Gordh T, Hursti T, et al. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: A randomized controlled trial. Behav Res Ther. 2013; 51(6):307-15. [DOI:10.1016/j.brat.2013.02.010] [PMID]
- Wicksell RK, Kemani M, Jensen K, Kosek E, Kadetoff D, Sorjonen K, et al. Acceptance and commitment therapy for fibromyalgia: a randomized controlled trial. Eur J Pain. 2013; 17(4):599-611. [DOI:10.1002/j.1532-2149.2012.00224.x] [PMID]
- Wicksell RK, Ahlqvist J, Bring A, Melin L, Olsson GL. Can exposure and acceptance strategies improve functioning and life satisfaction in people with chronic pain and Whiplash-Associated Disorders (WAD)? A randomized controlled trial. Cogn Behav Ther. 2008; 37(3):169-82. [DOI:10.1080/16506070802078970] [PMID]
- Anvari MH, Ebrahimi A, Neshatdoost HT, Afshar H Abedi A. [The effectiveness of group-based Acceptance and Commitment Therapy on pain-related anxiety, acceptance of pain and pain intensity in patients with chronic pain (Persian)]. J Isfahan Med Sch. 2014; 32(259):1-10.
- Irandoost F, Taher-Neshatdoost H, Nadi MA, Safary S. [The effectiveness of Acceptance and Commitment Therapy on the rate of pain intensity in women with chronic low backpain (Persian)]. J Clin Psychol. 2014; 6(2):75-84.
- Irandoost F, Safari S, Taher-Neshatdoost H, Nadi MA. [The effectiveness of group Acceptance and Commitment Therapy (ACT) on pain-related anxity and depression in women with chronic low back pain (Persian)]. Int J Behav Sci. 2015; 9(1):1-8.
- Monfared AR. [The effect of acceptance and commitment therapy on reducing anxity, depression and increase life quality, self-efficacy of Multiple Sclerosis patients (Persian)] [Master Thesis]. Rasht: Islamic Azad University; 2015.
- Etemadifar M. [Diagnosis and treatment of patients with multiple sclerosis (Persian)]. Isfahan: Chahar Bagh; 2006.
- Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. Eur J Pain. 2007; 11(2):153-63. [DOI:10.1016/j.ejpain.2005.12.008] [PMID]
- Asghari A, Nicholas MK. Pain self-efficacy beliefs and pain behaviour: A prospective study. Pain. 2001; 94(1):85-100. [DOI:10.1016/S0304-3959(01)00344-X] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2017/04/9 | Accepted: 2017/10/10 | Published: 2018/04/1
Received: 2017/04/9 | Accepted: 2017/10/10 | Published: 2018/04/1
References
1. Elliott DG. Migraine in multiple sclerosis. Int Rev Neurobiol. 2007; 79:281-302. [DOI:10.1016/S0074-7742(07)79012-8] [PMID] [DOI:10.1016/S0074-7742(07)79012-8]
2. Burks JS. A review of the current medical aspects of multiple sclerosis. J Neuro Rehab. 1992; 6(3):131-9. [DOI:10.1177/136140969200600302] [DOI:10.1177/136140969200600302]
3. D'Amico D, La Mantia L, Rigamonti A, Usai S, Mascoli N, Milanese C, et al. Prevalence of primary headaches in people with multiple sclerosis. Cephalalgia. 2004; 24(11):980-4. [DOI:10.1111/j.1468-2982.2004.00790.x] [PMID] [DOI:10.1111/j.1468-2982.2004.00790.x]
4. Santrock J. Psychology Training Guide context of Santrock. [M. Firoozbakht, Persian Trans.]. Tehran: Resa; 2003. [PMID]
5. Kenner M, Menon U, Elliott DG. Multiple sclerosis as a painful disease. Int Rev Neurobiol 2007; 79:303-21. [DOI:10.1016/S0074-7742(07)79013-X] [PMID] [DOI:10.1016/S0074-7742(07)79013-X]
6. Gatchel RJ, Turk DC. Psychosocial factors in pain: Critical perspectives. New York: Guilford Press; 1999.
7. Büssing A, Heusser P, Mundle G. Course of life satisfaction in patients with depressive and addictive disorders after therapeutic intervention. Int J Soc Psychiatry. 2012; 58(3):239-45. [DOI:10.1177/0020764010390498] [PMID] [DOI:10.1177/0020764010390498]
8. Clifford DB, Trotter JL. Pain in multiple sclerosis. Int J Soc Psychiatry. 1984; 41(12):1270-2. [DOI:10.1001/archneur.1984.04050230052017] [DOI:10.1001/archneur.1984.04050230052017]
9. Jensen MP, Turner JA, Romano JM. Chronic pain coping measures: Individual vs. composite scores. Pain. 1992; 51(3):273-80. [DOI:10.1016/0304-3959(92)90210-3] [PMID] [DOI:10.1016/0304-3959(92)90210-3]
10. Nash JM, Williams DM, Nicholson R, Trask PC. The contribution of pain-related anxiety to disability from headache. J Behav Med. 2006; 29(1):61-7. [DOI:10.1007/s10865-005-9033-4] [PMID] [DOI:10.1007/s10865-005-9033-4]
11. McCracken LM, Gauntlett-Gilbert J, Eccleston C. Acceptance of pain in adolescents with chronic pain: Validation of an adapted assessment instrument and preliminary correlation analyses. Eur J Pain. 2010; 14(3):316-20. [DOI:10.1016/j.ejpain.2009.05.002] [PMID] [DOI:10.1016/j.ejpain.2009.05.002]
12. Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychol Res Behav Manag. 2011; 4:41-9. [DOI:10.2147/PRBM.S15375] [PMID] [PMCID] [DOI:10.2147/PRBM.S15375]
13. Rudy TE, Turk DC, Zaki HS, Curtin HD. An empirical taxometric alternative to traditional classification of temporomandibular disorders. Pain. 1989; 36(3):311-20. [DOI:10.1016/0304-3959(89)90090-0] [PMID] [DOI:10.1016/0304-3959(89)90090-0]
14. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies–republished article. Behav Ther. 2016; 47(6):869-85. [DOI:10.1016/j.beth.2016.11.006] [PMID] [DOI:10.1016/j.beth.2016.11.006]
15. McCracken LM. Committed action: An application of the psychological flexibility model to activity patterns in chronic pain. J Pain. 2013; 14(8):828-35. [DOI:10.1016/j.jpain.2013.02.009] [PMID] [DOI:10.1016/j.jpain.2013.02.009]
16. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: The process and practice of mindful change. New York: Guilford Press; 2012.
17. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, Processes and outcomes. Behav Res Ther. 2006; 44:1-28. [DOI:10.1016/j.brat.2005.06.006] [PMID] [DOI:10.1016/j.brat.2005.06.006]
18. McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Health Psychol. 2008; 27(2):215-20. [DOI:10.1037/0278-6133.27.2.215] [PMID] [DOI:10.1037/0278-6133.27.2.215]
19. Wicksell RK, Olsson GL, Hayes SC. Mediators of change in acceptance and commitment therapy for pediatric chronic pain. Pain. 2011; 152(12):2792-801. [DOI:10.1016/j.pain.2011.09.003] [PMID] [DOI:10.1016/j.pain.2011.09.003]
20. Buhrman M, Skoglund A, Husell J, Bergström K, Gordh T, Hursti T, et al. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: A randomized controlled trial. Behav Res Ther. 2013; 51(6):307-15. [DOI:10.1016/j.brat.2013.02.010] [PMID] [DOI:10.1016/j.brat.2013.02.010]
21. Wicksell RK, Kemani M, Jensen K, Kosek E, Kadetoff D, Sorjonen K, et al. Acceptance and commitment therapy for fibromyalgia: a randomized controlled trial. Eur J Pain. 2013; 17(4):599-611. [DOI:10.1002/j.1532-2149.2012.00224.x] [PMID] [DOI:10.1002/j.1532-2149.2012.00224.x]
22. Wicksell RK, Ahlqvist J, Bring A, Melin L, Olsson GL. Can exposure and acceptance strategies improve functioning and life satisfaction in people with chronic pain and Whiplash-Associated Disorders (WAD)? A randomized controlled trial. Cogn Behav Ther. 2008; 37(3):169-82. [DOI:10.1080/16506070802078970] [PMID] [DOI:10.1080/16506070802078970]
23. Anvari MH, Ebrahimi A, Neshatdoost HT, Afshar H Abedi A. [The effectiveness of group-based Acceptance and Commitment Therapy on pain-related anxiety, acceptance of pain and pain intensity in patients with chronic pain (Persian)]. J Isfahan Med Sch. 2014; 32(259):1-10.
24. Irandoost F, Taher-Neshatdoost H, Nadi MA, Safary S. [The effectiveness of Acceptance and Commitment Therapy on the rate of pain intensity in women with chronic low backpain (Persian)]. J Clin Psychol. 2014; 6(2):75-84.
25. Irandoost F, Safari S, Taher-Neshatdoost H, Nadi MA. [The effectiveness of group Acceptance and Commitment Therapy (ACT) on pain-related anxity and depression in women with chronic low back pain (Persian)]. Int J Behav Sci. 2015; 9(1):1-8.
26. Monfared AR. [The effect of acceptance and commitment therapy on reducing anxity, depression and increase life quality, self-efficacy of Multiple Sclerosis patients (Persian)] [Master Thesis]. Rasht: Islamic Azad University; 2015.
27. Etemadifar M. [Diagnosis and treatment of patients with multiple sclerosis (Persian)]. Isfahan: Chahar Bagh; 2006.
28. Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. Eur J Pain. 2007; 11(2):153-63. [DOI:10.1016/j.ejpain.2005.12.008] [PMID] [DOI:10.1016/j.ejpain.2005.12.008]
29. Asghari A, Nicholas MK. Pain self-efficacy beliefs and pain behaviour: A prospective study. Pain. 2001; 94(1):85-100. [DOI:10.1016/S0304-3959(01)00344-X] [PMID] [DOI:10.1016/S0304-3959(01)00344-X]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |