Wed, Apr 24, 2024
Volume 8, Issue 4 (Autumn 2022)
Caspian J Neurol Sci 2022, 8(4): 252-267 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nikbakht H, Shojaie L, Niknejad N, Hassanipour S, Soleimanpour H, Heidari S, et al . Mortality Rate of Acute Stroke in Iran: A Systematic Review and Meta-Analysis. Caspian J Neurol Sci 2022; 8 (4) :252-267
URL: http://cjns.gums.ac.ir/article-1-568-en.html
URL: http://cjns.gums.ac.ir/article-1-568-en.html
Hossein-Ali Nikbakht * 

 1, Layla Shojaie2
1, Layla Shojaie2 

 , Nasim Niknejad3
, Nasim Niknejad3 

 , Soheil Hassanipour4
, Soheil Hassanipour4 

 , Hassan Soleimanpour5
, Hassan Soleimanpour5 

 , Sohrab Heidari6
, Sohrab Heidari6 

 , Sima Afrashteh7
, Sima Afrashteh7 

 , Ehsan Sarbazi8
, Ehsan Sarbazi8 

 , Saber Ghaffari-fam6
, Saber Ghaffari-fam6 




 1, Layla Shojaie2
1, Layla Shojaie2 

 , Nasim Niknejad3
, Nasim Niknejad3 

 , Soheil Hassanipour4
, Soheil Hassanipour4 

 , Hassan Soleimanpour5
, Hassan Soleimanpour5 

 , Sohrab Heidari6
, Sohrab Heidari6 

 , Sima Afrashteh7
, Sima Afrashteh7 

 , Ehsan Sarbazi8
, Ehsan Sarbazi8 

 , Saber Ghaffari-fam6
, Saber Ghaffari-fam6 


1- Social Determinants of Health Research Center of Babol University of Medical Sciences, Babol University of Medical Sciences, Babol, Iran
2- Department of Medicine, Keck School of Medicine, University of Southern California, Los Angeles, United States
3- Department of Population and Public Health, School of Population and Public Health, The University of British Columbia, Vancouver, Canada
4- Department of Cardiology, Cardiovascular Diseases Research Center, School of Medicine, Heshmat Hospital, Guilan University of Medical Sciences, Rasht, Iran
5- Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
6- Nursing School of Miyandoab, Urmia University of Medical Sciences, Urmia, Iran
7- Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
8- Student Research Committee, Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Medicine, Keck School of Medicine, University of Southern California, Los Angeles, United States
3- Department of Population and Public Health, School of Population and Public Health, The University of British Columbia, Vancouver, Canada
4- Department of Cardiology, Cardiovascular Diseases Research Center, School of Medicine, Heshmat Hospital, Guilan University of Medical Sciences, Rasht, Iran
5- Aging Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
6- Nursing School of Miyandoab, Urmia University of Medical Sciences, Urmia, Iran
7- Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
8- Student Research Committee, Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Full-Text [PDF 4015 kb]
(460 Downloads)
| Abstract (HTML) (963 Views)
Full-Text: (565 Views)
Introduction
Stroke is the second leading cause of mortality worldwide and the leading cause of acquired disability in adults. Also, two-thirds of the stroke-induced burden occurs in developing countries [1, 2]. Identifying patients’ mortality risk at admission can contribute to valuable clinical care modifications by identifying high-risk patients with poor outcomes who require more intensive resources. There is also an incremental course in the need to evolve well-validated models in predicting patients’ mortality risk. The objective is to reduce the overall burden of stroke on developing societies and establish an organized and classified protocol in acute stroke management [3, 4].
Stroke has many personal and social consequences; hence, it has been recognized as one of the most prioritized non-communicable diseases by the World Health Organization, a specialized agency of the United Nations responsible for international public health [5]. Blood pressure, type 2 diabetes, and heart disease are the most cardinal yet modifiable risk factors for stroke [6]. Independent predictors of stroke’s poor prognosis included the onset of stroke (whether acute or chronic), age over 70, deterioration during the first 48 hours of hospitalization, decreased consciousness, complete motor deficit, major cognitive syndrome, hyperglycemia, and female gender. Most ischemic strokes occur between 71 and 80, while most cases of hemorrhagic strokes occur between the age range of 60 and 70 [7, 8].
Recent estimates of the Global Burden of Disease Study clarified that the prevalence and incidence of stroke worldwide in 2016 were estimated to be 83 and 13.6 million, respectively [9]. Due to aging and population growth, the global burden of stroke is rising steadily [10]. The world has witnessed that the largest stroke burden pertains to low and middle-income countries [11]. In high-income countries, over the past two decades, the incidence of ischemic stroke has decreased by 13% and the mortality rate by 37%. Moreover, DALY (the disability-adjusted life year) and the mortality ratio to incidence decreased by 34% and 21%, respectively [12].
There is no national stroke registry in Iran. Therefore, there was a discrepancy among the recorded stroke incidence from 22 to 140 strokes per 100000 people between different regions of the country [10]. Studies show that stroke resulted in 12.3% mortality with a median of 5.5 months after discharge, mostly due to recurrence or complications of stroke [13].
Stroke mortality can be an excellent indicator of stroke care and control. Several studies have been conducted to estimate the mortality rate of stroke in hospitals, including 30 days post-stroke [14, 15], six months post-stroke [16], and long periods with different sample sizes and different follow-up lengths in several provinces of Iran [17]. Identification of mortality predictors at the time of hospitalization can be beneficial in reducing post-stroke mortality rates. Therefore, the present study aimed to systematically review and meta-analysis the available evidence to assess the short-term mortality rate of stroke in Iran.
Materials and Methods
This review study is a systematic and meta-analysis of short-term stroke mortality rates in Iran. This study’s reporting method is based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) checklist [18].
Search strategy
We applied the following terms, and our search was based on international electronic databases, including Scopus, PubMed, Web of Science, and national databases of Iranian Research Institute for Information Science and Technology (IranDoc), Magiran , Scientific Information Database (SID) Gray Literature, reference lists check, and manual journal searching from January 1990 to March 2020. The key search terms were “Stroke,” or “Ischemic stroke,” or” Hemorrhagic stroke,” “Intracerebral hemorrhage,” or “Intracerebral stroke,” or “subarachnoid hemorrhage,” or“Dead,” or “Fatality Rate,” or “Mortality Rate,” or “Survival,” or “Survival Analysis,” or “ Survival Rate” plus “Cohort Studies” or “Retrospective Studies” or “Prospective Studies” or “Longitudinal Studies” or “Cross-sectional studies” or “Observational studies” and “Iran.”
We additionally examined resource references from retrieval articles to guarantee that none of the relevant articles were missed. The collected data were entered into EndNote, X7 software, and duplicate articles were automatically deleted. It is worth noting that two researchers reviewed the articles independently.
Eligibility criteria
All observational studies (cross-sectional and cohort) referred to 1-month and 1-year stroke mortality related to Iran were entered into the review study without time limits. The included studies were necessitated to have a lethality rate or a mortality rate.
Death was defined as the permanent cessation of all vital signs, and its causes were classified according to the 10th version of the International Classification of Diseases (ICD-10). The causes of death in this study were stroke (ICD-10 I60-I69).
Quality assessment
Newcastle-Ottawa’s quality assessment checklist was utilized to evaluate the quality of the articles. This tool consists of three parts: selection (4 questions), comparison (1 question), and result (3 questions). Furthermore, based on the final score, the score was classified into three categories: good group (3 or 4 stars in the selection section, 1 or 2 stars in the comparison part, and 2 or 3 stars in the result section), fair (2 stars in the selection section, 1 or 2 stars in the comparison part and 2 or 3 stars in the result section), and poor (0 or 1 star in the selection section, 0 stars in the comparison part and 0 or 1 star in the result section) [2]. The results of the qualitative evaluation are presented in Appendix 1.

Screening of studies
Two researchers conducted initial exploration and assessed the studies’ qualities; in case of a discrepancy, the supervisor had the final word.
Data extraction form
A previously prepared checker extracted all ultimate articles that entered the study process. The checklist included the author’s name, publication year, study timeframe, sample size, study location, gender, mean age, stroke type, and mortality rate at distinct intervals.
Statistical analysis
Heterogeneity between studies was investigated by the Cochran test (with a significance level less than 0.1) and a combination employing I2 statistics. In a case with heterogeneity, the random-effects model was applied by the inverse-variance method, and in the case of no heterogeneity, the fixed effects model was adopted. In the case of heterogeneity amidst studies, methods such as meta-regression and subgroup analysis were practiced. All analyses were performed by STATA software v. 13.
Additional analysis
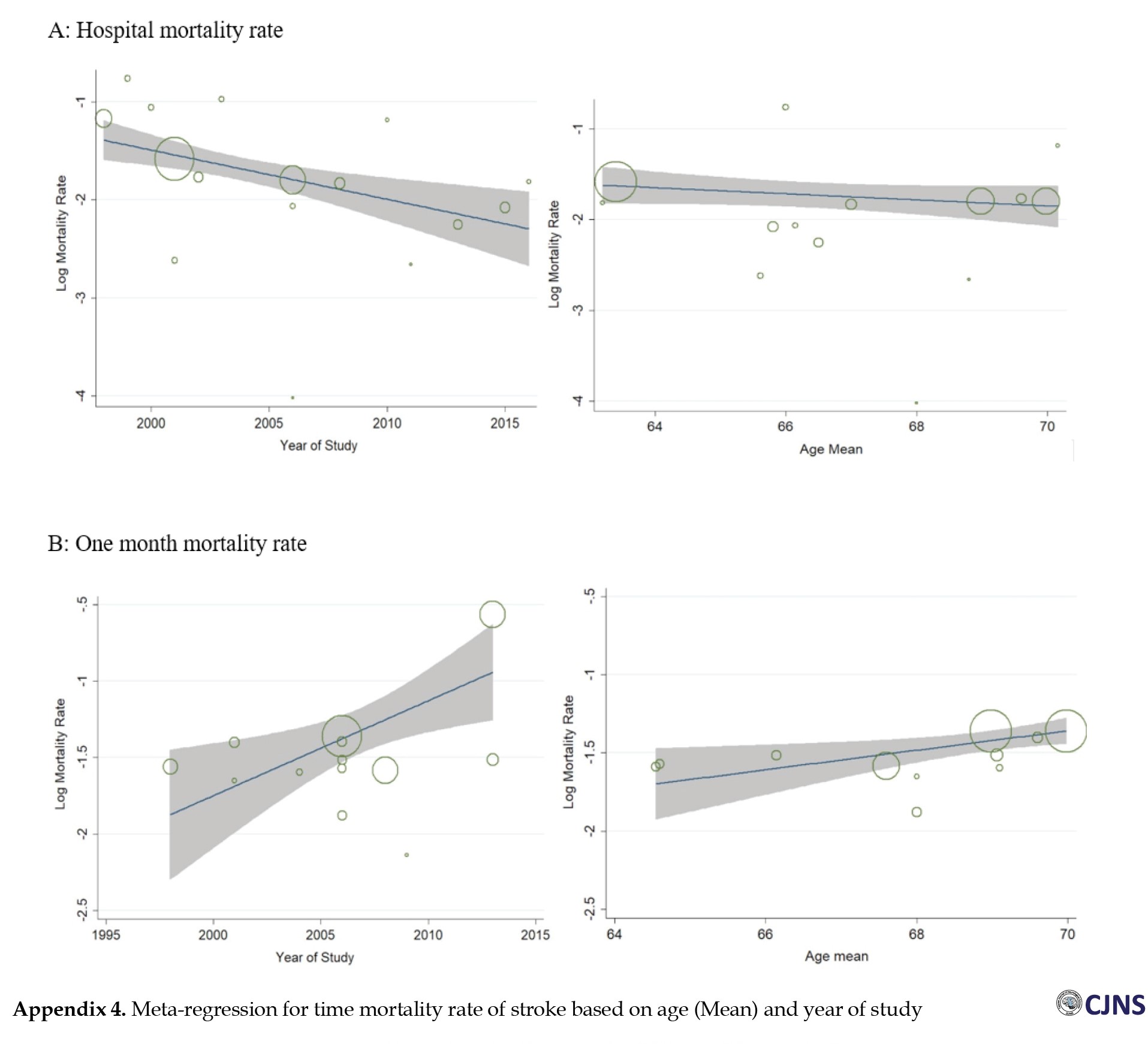
Due to the high heterogeneity of the studies, meta-regression analysis was practiced. Meta-regression analysis was conducted based on the year of the study and the mean age of the patients. Also, the subgroup analysis was performed only based on provinces to show more reliable stroke mortality status in the country for other variables such as stroke type, gender, the prevalence of hypertension, diabetes, etc. Due to the insufficient number of reports, meta-regression analysis and subgroup analysis were not preparatory.
Publication bias
The random-effects model was utilized to lessen the chance of bias in studies [19, 20]. Egger emission bias assessment test was also practiced to estimate the risk of bias [21].
Results
Study selection
Of 143 retrieved records, 33 were withdrawn due to duplication, and 82 due to a lack of responses to the study questions. Finally, 28 articles were incorporated into the meta-analysis. The study design consisted of 11 cohort studies and 17 cross-sectional studies. It should be noted that the references of the entered articles were also reviewed to supplement relevant studies. The selection process of included studies is presented in Figure 1. Study characteristics
The incorporated studies were from 1998 to 2018, and only 13 provinces had at least one eligible study. Based on the geographical location of the province, out of 28 studies included, six were in Khorasan Razavi [22, 23, 24, 25, 26, 27], 6 in East Azerbaijan [14, 16, 17, 28, 29, 30], 3 in Isfahan [31, 32, 33], 2 in Tehran [34, 35], 2 in Qom [13, 36], and 2 in Ardabil [34, 35, 37, 38]. Guilan [39], Kermanshah [40], South Khorasan [41], Mazandaran [42], Fars [15], Urmia [43], and Zahedan [44] Semnan [45] each had 1 study. One study was conducted on the entire population in Iran [46]. The characteristics of the studies are pitched in Table 1.
.jpg)
Quality assessment
The articles’ quality assessment results are shown in appendixes 1 and 2. Based on our review using the relevant checklist, 18 studies had good quality, and ten articles had moderate quality.
Heterogeneity
The results of the Chi-squared test and I2 index revealed significant heterogeneity between studies in mortality analysis for stroke and hospital mortality (I2=99.1%, P<0.001) and monthly mortality (I2=97.8%, P<0.001), so for these two, the random-effects model was adopted. The fixed-effects model was then used to analyze 1-year mortality (I2=44.6%, P=0.125) because the studies were homogeneous.
Results of the meta-analysis
First, the articles were classified based on the year of publication of the study. The obtained mortality rate was determined according to the following: hospital mortality rate, 1-month, and 1-year mortality rate. The mortality rates were conducted independently by provinces. Moreover, meta-regression was performed based on the study’s year and the patients’ mean age.
Hospital mortality rate
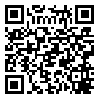
Out of the ultimate articles, 17 studies published stroke hospital mortality. Based on the random-effect model, the study results recorded that the hospital mortality rate in Iran is 18.71% (95% CI: 15.09%-22.34%) among 47961 patients (Figure 2 and Appendix 3). One-month mortality
Out of the final articles, 15 studies listed one-month-long stroke mortality. Based on the random-effect model, the results revealed that the 1-month mortality rate in Iran was 23.43% (95% CI: 20.08%-26.78%) (Figure 3). One-year mortality
Out of the final articles, five studies reported one-year stroke mortality. The results revealed that one-year mortality in Iran based on the fixed-effects model was 34.44% (95% CI: 32.02%-36.85%) (Figure 4). Mortality rate based on provinces
Overall, the results of stroke mortality in 13 provinces in Iran, based on the studies included, are shown in Table 2.
.jpg)
In general, 12 provinces reported at least one hospital mortality study, 7 reported one-month mortality rates, and three provinces proclaimed one-year mortality. Moreover, the highest and lowest prevalence in the provinces for hospital mortality was 37.60% (30.02%-45.18%) for Ardebil and 1.80% (0.96%-2.64%) for Qom; for one month, the same index was for East Azerbaijan as 33.06% (13.63%-52.49%) and Mazandaran as 19.20% (14.32%-24.08%).
Meta-regression
The meta-regression results were based on the variables of the year of study and the mean age of the patients. There was no significant relationship between these two variables and mortality for years of study and mean age, although having risen in the year of study (Reg Coef=0.048, P=0.162 and increase in one unit mean age (Reg Coef=-0.017, P=0.585) and decrease hospital mortality, but these relationships were not statistically significant. Of course, although these two relationships were not statistically significant for one-month mortality, the results were somewhat different, with an increase in the year of the study (Reg Coef=0.025, P=0.260) and an increase in one unit of mean age (Reg Coef=0.030, P=0.232) and increased monthly mortality (Appendix 4). Publication bias
Ultimately, we utilized funnel plots to check the propagation bias for stroke mortality; the Egger test results did not confirm this bias (P=0.479). These studies were scattered almost on both sides of the horizontal line, indicating the absence of publication bias (Appendix 5). Discussion
Based on our findings, the stroke in-hospital mortality rate in Iran was estimated to be 18.71%. This is the first study to determine the in-hospital mortality rate in Iran, and it provides a baseline figure to evaluate the subsequent changes in the trend of stroke mortality rate. Our results were lower than the seven countries that reported their stroke mortality rates to World Health Organization (WHO): Russian Federation, Ukraine, Belarus, Turkmenistan, Kazakhstan, Seychelles, and Oman. Their rates varied from 26 in Oman to 233 per 100000 population in Russian Federation [47]. The rate of hospital mortality in Germany reported by the stroke registry system in 2000 was estimated to be 4.9% [48]. In Mashhad, a province in Iran, the in-hospital stroke mortality rate from March 2018 to March 2019 was 14.2% [49]. This case fatality rate was lower than reported in Tanzania, 33.3% [50]. Based on our data, age increased monthly mortality. The overall case fatality rate and reported case fatality rate in each gender demonstrated a non-significant increasing trend by age [51]. Furthermore, our study differed from a study in Tanzania, which described a significant increase of case fatality over the age of 65 [50].
Reedwong et al. [52] demonstrated that elderly patients have a higher mortality risk. This higher mortality risk is possibly due to transitional patients with medical emergencies and higher severity of stroke symptoms [53]. History of stroke, carotid stenosis, hypertension, dyslipidemia, and smoking are associated with low stroke mortality, probably because these risk factors are associated with non-cardioembolic stroke [54, 55]. Although significant studies have been published to predict stroke mortality, most have been convoyed when specific parts of stroke management and treatments have not yet been established or implemented on heterogeneous cohorts, such as ischemic and hemorrhagic strokes.
In the Middle East, the results of a recent systematic review revealed a significant positive correlation between age and mortality rate [56]. Age is an important risk factor for death, and each additional year in age is correlated with a 3% relative increase in in-hospital stroke mortality [49]. Age seems to be the most important predictor of the 1-year mortality of stroke. According to several previous studies [57], age ≥70 years is associated with stroke risk (P<0.05) [58]. Although many studies have mentioned that increasing age is an important risk factor for in-hospital death, some studies have considered the effect of age more, especially for the elderly (≥ 65 years). Also, it could not be independently correlated with poor outcomes (modified ranking scale ≥3) assessed through modified ranking scale at discharge [59, 60].
Based on our data, the 1-month stroke mortality rate in Iran was estimated to be 23.43%. The 30-day fatality rate in other demographic studies was estimated to be 23.43%, which was registered to be from 11.8% to 56.8% [61]. Recent studies have reported comparable results for 30-day lethality rates, such as ischemic stroke for 14.9% in Italy’s Lazio regions in 2011-2012 [59] and 7.9% in Scotland in 2013 [62]. Moreover, in a review, the 28-day-old lethality rate varied from 17% to 33% and was estimated to be 22.9% [63]. Kumral reported that the overall 30-day mortality rate was 19.7%, which was higher for hemorrhagic stroke patients (29%) compared to ischemic stroke (17%) [64]. The 28-day lethality rate for all types of stroke was 24%, while in the Oxfordshire Community Stroke project, the overall 30-day lethality rate was estimated at 19% [65]. Although in high-income countries, the lethality rate has decreased or remained steady for 28 days after stroke [66]. One of the reasons for this decline can be the improvement of care in the acute phase of the disease and management [67]. This finding might be relevant to Iran, which has undergone major political and socioeconomic changes after the Islamic revolution.
The 1-year mortality rate in Iran was 34.44%. In a separate study, independent predictors of stroke were considered age, pre-stroke functional status (MRS score more than 0), the severity of stroke (NIHSS), history of diabetes mellitus, heart disease, posterior circulation stroke syndrome (compared to anterior circulation stroke syndromes), and non-lacunar stroke causes [68]. In a population-based study in Greece on hemorrhagic patients, the 1-year mortality rate was estimated to be 36.8% [69]. The Danish MONICA study reported a 1-year mortality rate of 41% [70]. These mortality rates are considerably lower than those reported in previous older studies from Germany (58.3% between 1994 and 1996) [71] and New Zealand (57% between 1981-1982 and 1983) [72]. These differences may be associated with omitting cases that died before reaching the hospital.
Limitations of the study
Among the constraints of this study are the type and quality of studies included in our study, the sample size of studies, and the number of studies conducted in each province that can affect this study’s results. Another limitation of this review was that many studies had results based on critical variables such as gender, stroke typing, etc. Therefore, the researchers could not perform subgroup analysis and meta-regression based on these variables. These factors can also justify significant heterogeneity between studies. Moreover, it needs to be noted that the more distant cohort studies have higher mortality levels. It is inescapable to recognize the cohort effect and age in future research projects using demographic data and not look at cross-sectional data.
Study suggestions
Lastly, the quantity of mortality for a time period and type of stroke was not plausible. A few studies reported this rate; however, there is a necessity for more prospective studies in this field in the future. Besides, no study was published in numerous geographic areas, and more studies are necessary, especially in deprived provinces, to have a more accurate approximation in the country.
Conclusion
Our study’s findings revealed that the short-term mortality rate amongst stroke patients is about one-fifth in the hospital after death designation. This mortality rate increases in 1-month and 1-year periods, which increases by one-third in a 1-year mortality rate. Furthermore, it is essential to adjust programs to reduce mortality in short-term outcomes after stroke by performing specific primary treatments on these patients.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was approved and supported by the Student Research Committee, Tabriz University of Medical Sciences (Code: IR.TBZMED.VCR.REC.1398.355).
Funding
The study was funded by Tabriz University of Medical Sciences, Tabriz, Iran. (Grant number: 1398.355).
Authors contributions
Study conception and design: Hossein-Ali Nikbakht, Soheil Hassanipour, and Saber Ghaffari-fam; Acquisition of data: Hassan Soleimanpour, Layla Shojaieand, and Sohrab Heidari; Statistical analysis: Hossein-Ali Nikbakht, Soheil Hassanipour, Sima Afrashteh, and Ehsan Sarbazi; Interpretation of results: Hossein-Ali Nikbakht, Soheil Hassanipour, Layla Shojaie, and Saber Ghaffari-fam; Drafting of manuscript, approval of the article’s final version, including the authorship list: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Stroke is the second leading cause of mortality worldwide and the leading cause of acquired disability in adults. Also, two-thirds of the stroke-induced burden occurs in developing countries [1, 2]. Identifying patients’ mortality risk at admission can contribute to valuable clinical care modifications by identifying high-risk patients with poor outcomes who require more intensive resources. There is also an incremental course in the need to evolve well-validated models in predicting patients’ mortality risk. The objective is to reduce the overall burden of stroke on developing societies and establish an organized and classified protocol in acute stroke management [3, 4].
Stroke has many personal and social consequences; hence, it has been recognized as one of the most prioritized non-communicable diseases by the World Health Organization, a specialized agency of the United Nations responsible for international public health [5]. Blood pressure, type 2 diabetes, and heart disease are the most cardinal yet modifiable risk factors for stroke [6]. Independent predictors of stroke’s poor prognosis included the onset of stroke (whether acute or chronic), age over 70, deterioration during the first 48 hours of hospitalization, decreased consciousness, complete motor deficit, major cognitive syndrome, hyperglycemia, and female gender. Most ischemic strokes occur between 71 and 80, while most cases of hemorrhagic strokes occur between the age range of 60 and 70 [7, 8].
Recent estimates of the Global Burden of Disease Study clarified that the prevalence and incidence of stroke worldwide in 2016 were estimated to be 83 and 13.6 million, respectively [9]. Due to aging and population growth, the global burden of stroke is rising steadily [10]. The world has witnessed that the largest stroke burden pertains to low and middle-income countries [11]. In high-income countries, over the past two decades, the incidence of ischemic stroke has decreased by 13% and the mortality rate by 37%. Moreover, DALY (the disability-adjusted life year) and the mortality ratio to incidence decreased by 34% and 21%, respectively [12].
There is no national stroke registry in Iran. Therefore, there was a discrepancy among the recorded stroke incidence from 22 to 140 strokes per 100000 people between different regions of the country [10]. Studies show that stroke resulted in 12.3% mortality with a median of 5.5 months after discharge, mostly due to recurrence or complications of stroke [13].
Stroke mortality can be an excellent indicator of stroke care and control. Several studies have been conducted to estimate the mortality rate of stroke in hospitals, including 30 days post-stroke [14, 15], six months post-stroke [16], and long periods with different sample sizes and different follow-up lengths in several provinces of Iran [17]. Identification of mortality predictors at the time of hospitalization can be beneficial in reducing post-stroke mortality rates. Therefore, the present study aimed to systematically review and meta-analysis the available evidence to assess the short-term mortality rate of stroke in Iran.
Materials and Methods
This review study is a systematic and meta-analysis of short-term stroke mortality rates in Iran. This study’s reporting method is based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) checklist [18].
Search strategy
We applied the following terms, and our search was based on international electronic databases, including Scopus, PubMed, Web of Science, and national databases of Iranian Research Institute for Information Science and Technology (IranDoc), Magiran , Scientific Information Database (SID) Gray Literature, reference lists check, and manual journal searching from January 1990 to March 2020. The key search terms were “Stroke,” or “Ischemic stroke,” or” Hemorrhagic stroke,” “Intracerebral hemorrhage,” or “Intracerebral stroke,” or “subarachnoid hemorrhage,” or“Dead,” or “Fatality Rate,” or “Mortality Rate,” or “Survival,” or “Survival Analysis,” or “ Survival Rate” plus “Cohort Studies” or “Retrospective Studies” or “Prospective Studies” or “Longitudinal Studies” or “Cross-sectional studies” or “Observational studies” and “Iran.”
We additionally examined resource references from retrieval articles to guarantee that none of the relevant articles were missed. The collected data were entered into EndNote, X7 software, and duplicate articles were automatically deleted. It is worth noting that two researchers reviewed the articles independently.
Eligibility criteria
All observational studies (cross-sectional and cohort) referred to 1-month and 1-year stroke mortality related to Iran were entered into the review study without time limits. The included studies were necessitated to have a lethality rate or a mortality rate.
Death was defined as the permanent cessation of all vital signs, and its causes were classified according to the 10th version of the International Classification of Diseases (ICD-10). The causes of death in this study were stroke (ICD-10 I60-I69).
Quality assessment
Newcastle-Ottawa’s quality assessment checklist was utilized to evaluate the quality of the articles. This tool consists of three parts: selection (4 questions), comparison (1 question), and result (3 questions). Furthermore, based on the final score, the score was classified into three categories: good group (3 or 4 stars in the selection section, 1 or 2 stars in the comparison part, and 2 or 3 stars in the result section), fair (2 stars in the selection section, 1 or 2 stars in the comparison part and 2 or 3 stars in the result section), and poor (0 or 1 star in the selection section, 0 stars in the comparison part and 0 or 1 star in the result section) [2]. The results of the qualitative evaluation are presented in Appendix 1.

Screening of studies
Two researchers conducted initial exploration and assessed the studies’ qualities; in case of a discrepancy, the supervisor had the final word.
Data extraction form
A previously prepared checker extracted all ultimate articles that entered the study process. The checklist included the author’s name, publication year, study timeframe, sample size, study location, gender, mean age, stroke type, and mortality rate at distinct intervals.
Statistical analysis
Heterogeneity between studies was investigated by the Cochran test (with a significance level less than 0.1) and a combination employing I2 statistics. In a case with heterogeneity, the random-effects model was applied by the inverse-variance method, and in the case of no heterogeneity, the fixed effects model was adopted. In the case of heterogeneity amidst studies, methods such as meta-regression and subgroup analysis were practiced. All analyses were performed by STATA software v. 13.
Additional analysis
Due to the high heterogeneity of the studies, meta-regression analysis was practiced. Meta-regression analysis was conducted based on the year of the study and the mean age of the patients. Also, the subgroup analysis was performed only based on provinces to show more reliable stroke mortality status in the country for other variables such as stroke type, gender, the prevalence of hypertension, diabetes, etc. Due to the insufficient number of reports, meta-regression analysis and subgroup analysis were not preparatory.
Publication bias
The random-effects model was utilized to lessen the chance of bias in studies [19, 20]. Egger emission bias assessment test was also practiced to estimate the risk of bias [21].
Results
Study selection
Of 143 retrieved records, 33 were withdrawn due to duplication, and 82 due to a lack of responses to the study questions. Finally, 28 articles were incorporated into the meta-analysis. The study design consisted of 11 cohort studies and 17 cross-sectional studies. It should be noted that the references of the entered articles were also reviewed to supplement relevant studies. The selection process of included studies is presented in Figure 1. Study characteristics
The incorporated studies were from 1998 to 2018, and only 13 provinces had at least one eligible study. Based on the geographical location of the province, out of 28 studies included, six were in Khorasan Razavi [22, 23, 24, 25, 26, 27], 6 in East Azerbaijan [14, 16, 17, 28, 29, 30], 3 in Isfahan [31, 32, 33], 2 in Tehran [34, 35], 2 in Qom [13, 36], and 2 in Ardabil [34, 35, 37, 38]. Guilan [39], Kermanshah [40], South Khorasan [41], Mazandaran [42], Fars [15], Urmia [43], and Zahedan [44] Semnan [45] each had 1 study. One study was conducted on the entire population in Iran [46]. The characteristics of the studies are pitched in Table 1.
.jpg)
Quality assessment
The articles’ quality assessment results are shown in appendixes 1 and 2. Based on our review using the relevant checklist, 18 studies had good quality, and ten articles had moderate quality.
Heterogeneity
The results of the Chi-squared test and I2 index revealed significant heterogeneity between studies in mortality analysis for stroke and hospital mortality (I2=99.1%, P<0.001) and monthly mortality (I2=97.8%, P<0.001), so for these two, the random-effects model was adopted. The fixed-effects model was then used to analyze 1-year mortality (I2=44.6%, P=0.125) because the studies were homogeneous.
Results of the meta-analysis
First, the articles were classified based on the year of publication of the study. The obtained mortality rate was determined according to the following: hospital mortality rate, 1-month, and 1-year mortality rate. The mortality rates were conducted independently by provinces. Moreover, meta-regression was performed based on the study’s year and the patients’ mean age.
Hospital mortality rate
Out of the ultimate articles, 17 studies published stroke hospital mortality. Based on the random-effect model, the study results recorded that the hospital mortality rate in Iran is 18.71% (95% CI: 15.09%-22.34%) among 47961 patients (Figure 2 and Appendix 3). One-month mortality
Out of the final articles, 15 studies listed one-month-long stroke mortality. Based on the random-effect model, the results revealed that the 1-month mortality rate in Iran was 23.43% (95% CI: 20.08%-26.78%) (Figure 3). One-year mortality
Out of the final articles, five studies reported one-year stroke mortality. The results revealed that one-year mortality in Iran based on the fixed-effects model was 34.44% (95% CI: 32.02%-36.85%) (Figure 4). Mortality rate based on provinces
Overall, the results of stroke mortality in 13 provinces in Iran, based on the studies included, are shown in Table 2.
.jpg)
In general, 12 provinces reported at least one hospital mortality study, 7 reported one-month mortality rates, and three provinces proclaimed one-year mortality. Moreover, the highest and lowest prevalence in the provinces for hospital mortality was 37.60% (30.02%-45.18%) for Ardebil and 1.80% (0.96%-2.64%) for Qom; for one month, the same index was for East Azerbaijan as 33.06% (13.63%-52.49%) and Mazandaran as 19.20% (14.32%-24.08%).
Meta-regression
The meta-regression results were based on the variables of the year of study and the mean age of the patients. There was no significant relationship between these two variables and mortality for years of study and mean age, although having risen in the year of study (Reg Coef=0.048, P=0.162 and increase in one unit mean age (Reg Coef=-0.017, P=0.585) and decrease hospital mortality, but these relationships were not statistically significant. Of course, although these two relationships were not statistically significant for one-month mortality, the results were somewhat different, with an increase in the year of the study (Reg Coef=0.025, P=0.260) and an increase in one unit of mean age (Reg Coef=0.030, P=0.232) and increased monthly mortality (Appendix 4). Publication bias
Ultimately, we utilized funnel plots to check the propagation bias for stroke mortality; the Egger test results did not confirm this bias (P=0.479). These studies were scattered almost on both sides of the horizontal line, indicating the absence of publication bias (Appendix 5). Discussion
Based on our findings, the stroke in-hospital mortality rate in Iran was estimated to be 18.71%. This is the first study to determine the in-hospital mortality rate in Iran, and it provides a baseline figure to evaluate the subsequent changes in the trend of stroke mortality rate. Our results were lower than the seven countries that reported their stroke mortality rates to World Health Organization (WHO): Russian Federation, Ukraine, Belarus, Turkmenistan, Kazakhstan, Seychelles, and Oman. Their rates varied from 26 in Oman to 233 per 100000 population in Russian Federation [47]. The rate of hospital mortality in Germany reported by the stroke registry system in 2000 was estimated to be 4.9% [48]. In Mashhad, a province in Iran, the in-hospital stroke mortality rate from March 2018 to March 2019 was 14.2% [49]. This case fatality rate was lower than reported in Tanzania, 33.3% [50]. Based on our data, age increased monthly mortality. The overall case fatality rate and reported case fatality rate in each gender demonstrated a non-significant increasing trend by age [51]. Furthermore, our study differed from a study in Tanzania, which described a significant increase of case fatality over the age of 65 [50].
Reedwong et al. [52] demonstrated that elderly patients have a higher mortality risk. This higher mortality risk is possibly due to transitional patients with medical emergencies and higher severity of stroke symptoms [53]. History of stroke, carotid stenosis, hypertension, dyslipidemia, and smoking are associated with low stroke mortality, probably because these risk factors are associated with non-cardioembolic stroke [54, 55]. Although significant studies have been published to predict stroke mortality, most have been convoyed when specific parts of stroke management and treatments have not yet been established or implemented on heterogeneous cohorts, such as ischemic and hemorrhagic strokes.
In the Middle East, the results of a recent systematic review revealed a significant positive correlation between age and mortality rate [56]. Age is an important risk factor for death, and each additional year in age is correlated with a 3% relative increase in in-hospital stroke mortality [49]. Age seems to be the most important predictor of the 1-year mortality of stroke. According to several previous studies [57], age ≥70 years is associated with stroke risk (P<0.05) [58]. Although many studies have mentioned that increasing age is an important risk factor for in-hospital death, some studies have considered the effect of age more, especially for the elderly (≥ 65 years). Also, it could not be independently correlated with poor outcomes (modified ranking scale ≥3) assessed through modified ranking scale at discharge [59, 60].
Based on our data, the 1-month stroke mortality rate in Iran was estimated to be 23.43%. The 30-day fatality rate in other demographic studies was estimated to be 23.43%, which was registered to be from 11.8% to 56.8% [61]. Recent studies have reported comparable results for 30-day lethality rates, such as ischemic stroke for 14.9% in Italy’s Lazio regions in 2011-2012 [59] and 7.9% in Scotland in 2013 [62]. Moreover, in a review, the 28-day-old lethality rate varied from 17% to 33% and was estimated to be 22.9% [63]. Kumral reported that the overall 30-day mortality rate was 19.7%, which was higher for hemorrhagic stroke patients (29%) compared to ischemic stroke (17%) [64]. The 28-day lethality rate for all types of stroke was 24%, while in the Oxfordshire Community Stroke project, the overall 30-day lethality rate was estimated at 19% [65]. Although in high-income countries, the lethality rate has decreased or remained steady for 28 days after stroke [66]. One of the reasons for this decline can be the improvement of care in the acute phase of the disease and management [67]. This finding might be relevant to Iran, which has undergone major political and socioeconomic changes after the Islamic revolution.
The 1-year mortality rate in Iran was 34.44%. In a separate study, independent predictors of stroke were considered age, pre-stroke functional status (MRS score more than 0), the severity of stroke (NIHSS), history of diabetes mellitus, heart disease, posterior circulation stroke syndrome (compared to anterior circulation stroke syndromes), and non-lacunar stroke causes [68]. In a population-based study in Greece on hemorrhagic patients, the 1-year mortality rate was estimated to be 36.8% [69]. The Danish MONICA study reported a 1-year mortality rate of 41% [70]. These mortality rates are considerably lower than those reported in previous older studies from Germany (58.3% between 1994 and 1996) [71] and New Zealand (57% between 1981-1982 and 1983) [72]. These differences may be associated with omitting cases that died before reaching the hospital.
Limitations of the study
Among the constraints of this study are the type and quality of studies included in our study, the sample size of studies, and the number of studies conducted in each province that can affect this study’s results. Another limitation of this review was that many studies had results based on critical variables such as gender, stroke typing, etc. Therefore, the researchers could not perform subgroup analysis and meta-regression based on these variables. These factors can also justify significant heterogeneity between studies. Moreover, it needs to be noted that the more distant cohort studies have higher mortality levels. It is inescapable to recognize the cohort effect and age in future research projects using demographic data and not look at cross-sectional data.
Study suggestions
Lastly, the quantity of mortality for a time period and type of stroke was not plausible. A few studies reported this rate; however, there is a necessity for more prospective studies in this field in the future. Besides, no study was published in numerous geographic areas, and more studies are necessary, especially in deprived provinces, to have a more accurate approximation in the country.
Conclusion
Our study’s findings revealed that the short-term mortality rate amongst stroke patients is about one-fifth in the hospital after death designation. This mortality rate increases in 1-month and 1-year periods, which increases by one-third in a 1-year mortality rate. Furthermore, it is essential to adjust programs to reduce mortality in short-term outcomes after stroke by performing specific primary treatments on these patients.
Ethical Considerations
Compliance with ethical guidelines
The research protocol was approved and supported by the Student Research Committee, Tabriz University of Medical Sciences (Code: IR.TBZMED.VCR.REC.1398.355).
Funding
The study was funded by Tabriz University of Medical Sciences, Tabriz, Iran. (Grant number: 1398.355).
Authors contributions
Study conception and design: Hossein-Ali Nikbakht, Soheil Hassanipour, and Saber Ghaffari-fam; Acquisition of data: Hassan Soleimanpour, Layla Shojaieand, and Sohrab Heidari; Statistical analysis: Hossein-Ali Nikbakht, Soheil Hassanipour, Sima Afrashteh, and Ehsan Sarbazi; Interpretation of results: Hossein-Ali Nikbakht, Soheil Hassanipour, Layla Shojaie, and Saber Ghaffari-fam; Drafting of manuscript, approval of the article’s final version, including the authorship list: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World Neurosurg. 2011; 76(6):S85-90. [DOI:10.1016/j.wneu.2011.07.023] [PMID]
- Kalkonde YV, Alladi S, Kaul S, Hachinski V. Stroke prevention strategies in the developing world. Stroke. 2018; 49(12):3092-7. [DOI:10.1161/STROKEAHA.118.017384] [PMID] [PMCID]
- Nouh AM, McCormick L, Modak J, Fortunato G, Staff I. High mortality among 30-day readmission after stroke: Predictors and etiologies of readmission. Front Neurol. 2017; 8:632. [DOI:10.3389/fneur.2017.00632] [PMID] [PMCID]
- Huang Y, Douiri A, Fahey M. A dynamic model for predicting survival up to 1 year after ischemic stroke. J Stroke Cerebrovasc Dis. 2020; 29(10):105133. [DOI:10.1016/j.jstrokecerebrovasdis.2020.105133] [PMID]
- Lindsay MP, Norrving B, Sacco RL, Brainin M, Hacke W, Martins S, et al. World stroke organization (WSO): Global stroke fact sheet. 2019. Int J Stroke. 2019; 14(8):806-17. [DOI:10.1177/1747493019881353] [PMID]
- Guzik A, Bushnell C. Stroke epidemiology and risk factor management. Continuum. 2017; 23(1):15-39. [DOI:10.1212/CON.0000000000000416] [PMID]
- Weber R, Krogias C, Eyding J, Bartig D, Meves SH, Katsanos AH, et al. Age and sex differences in ischemic stroke treatment in a nationwide analysis of 1.11 million hospitalized cases. Stroke. 2019; 50(12):3494-502. [DOI:10.1161/STROKEAHA.119.026723] [PMID]
- Qawasmeh MA, Aldabbour B, Momani A, Obiedat D, Alhayek K, Kofahi R, et al. Epidemiology, risk factors, and predictors of disability in a cohort of Jordanian patients with the first ischemic stroke. Stroke Res Treat. 2020; 2020:1920583. [DOI:10.1155/2020/1920583] [PMID] [PMCID]
- Johnson CO, Nguyen M, Roth GA, Nichols E, Alam T, Abate D, et al. Global, regional, and national burden of stroke, 1990-2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019; 18(5):439-58. [DOI:10.1016/S1474-4422(19)30034-1]
- Yousufuddin M, Young N. Aging and ischemic stroke. Aging (Albany NY). 2019; 11(9):2542-44. [DOI:10.18632/aging.101931] [PMID] [PMCID]
- Thrift AG, Arabshahi S. Is stroke incidence in low-to middle-income countries driven by economics? Int J Stroke. 2012; 7(4):307-8. [DOI:10.1111/j.1747-4949.2012.00819.x] [PMID]
- Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: Findings from the global burden of disease study 2010. Lancet. 2014; 383(9913):245-55. [DOI:10.1016/S0140-6736(13)61953-4] [PMID]
- Delbari A, Salman Roghani R, Tabatabaei SS, Rahgozar M, Lokk J. Stroke epidemiology and one-month fatality among an urban population in Iran. Int J Stroke. 2011; 6(3):195-200. [DOI:10.1111/j.1747-4949.2010.00562.x] [PMID]
- Shamshirgaran SM, Barzkar H, Savadi-Oskouei D, Marandi MY, Safaiyan A, Sarbazi E, et al. Predictors of short-term mortality after acute stroke in East Azerbaijan province, 2014. J Cardiovasc Thorac Res. 2018; 10(1):36. [DOI:10.15171/jcvtr.2018.06] [PMID] [PMCID]
- Borhani-Haghighi A, Safari R, Heydari ST, Soleimani F, Sharifian M, Kashkuli SY, et al. Hospital mortality associated with stroke in southern Iran. Iran J Med Sci. 2013; 333(Suplement 1):E184. [DOI:10.1016/j.jns.2013.07.750]
- Sarbazi E, Sarbakhsh P, Oskooei DS, Yazdchi M, Ghaffari-Fam S, Shamshirgaran SM. Factors related to 6-month mortality after the first-ever stroke. J Educ Health Promot. 2018; 7 :113. [DOI:10.4103/jehp.jehp_190_17] [PMID] [PMCID]
- Novbakht H, Shamshirgaran SM, Sarbakhsh P, Savadi-Oskouei D, Yazdchi MM, Ghorbani Z. Predictors of long-term mortality after first-ever stroke. J Educ Health Promot. 2020; 9:45. [DOI:10.4103/jehp.jehp_8_19] [PMID] [PMCID]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Sys Rev. 2015; 4(1):1. [DOI:10.1186/2046-4053-4-1]
- Harris RJ, Deeks JJ, Altman DG, Bradburn MJ, Harbord RM, Sterne JA. Metan: Fixed-and random-effects meta-analysis. Stata J. 2008; 8(1):3-28. [DOI:10.1177/1536867X0800800102]
- Bagos PG, Nikolopoulos GK. Mixed-effects poisson regression models for meta-analysis of follow-up studies with constant or varying durations. I J Biostat. 2009; 5(1). [DOI:10.2202/1557-4679.1168]
- Lin L, Chu H. Quantifying publication bias in meta‐analysis. Biometrics. 2018; 74(3):785-94. [DOI:10.1111/biom.12815] [PMID] [PMCID]
- Ghandehari K, Izadi Z. The Khorasan stroke registry: Results of a five-year hospital-based study. Cerebrovascular Diseases. 2007; 23(2-3):132-9. [DOI:10.1159/000097050] [PMID]
- Farzadfard MT, Thrift AG, Amiri A, Kapral MK, Hashemi P, Sposato LA, et al. Five-year case fatality following first-ever stroke in the Mashhad stroke incidence study: A population-based study of stroke in the Middle East. J Stroke Cerebrovasc Dis. 2018; 27(4):1085-9. [DOI:10.1016/j.jstrokecerebrovasdis.2017.11.018] [PMID]
- Amiri A, Kapral MK, Thrift AG, Sposato LA, Saber H, Behrouz R, et al. The incidence and characteristics of stroke in urban-dwelling Iranian women. J Stroke Cerebrovasc Dis. 2018; 27(3):547-54. [DOI:10.1016/j.jstrokecerebrovasdis.2017.09.050] [PMID]
- Morovatdar N, Thrift AG, Kapral MK, Behrouz R, Saber H, Amiri A, et al. Long-term outcomes of ischemic stroke of undetermined mechanism: A population-based prospective cohort. Neuroepidemiology. 2017; 49(3-4):160-4. [DOI:10.1159/000482019] [PMID]
- Shoeibi A, Salehi M, Thrift AG, Kapral MK, Farzadfard MT, Azarpazhooh A, et al. One‐year case fatality rate following stroke in the Mashhad stroke incidence study: A population‐based study of stroke in Iran. I J Stroke. 2015; 10:96-102. [DOI:10.1111/ijs.12611] [PMID]
- Salehi M, Amiri A, Thrift AG, Kapral MK, Sposato L, Behrouz R, et al. Five-year recurrence rate and the predictors following stroke in the Mashhad stroke incidence study: A population-based cohort study of stroke in the Middle East. Neuroepidemiology. 2018; 50(1-2):18-22. [DOI:10.1159/000485509] [PMID]
- Farhoudi M, Mehrvar K, Sadeghi-Bazargani H, Hashemilar M, Seyedi-Vafaee M, Sadeghi-Hokmabad E, et al. Stroke subtypes, risk factors and mortality rate in northwest of Iran. I J of Neurol. 2017; 16(3):112. [PMID] [PMCID]
- Deljavan R, Farhoudi M, Sadeghi-Bazargani H. Stroke in-hospital survival and its predictors: The first results from Tabriz stroke registry of Iran. Int J Gen Med. 2018; 11:233-40. [DOI:10.2147/IJGM.S158296] [PMID] [PMCID]
- Talebi M, Ghertasi M, Taheraghdam A, Andalib S, Sharifipour E. A comparison of risk factors and severity of ischemic stroke in female and male genders in North-West Iran: A cross-sectional study. Iran J Neurol. 2014; 13(4):215-9. [PMID] [PMCID]
- Oveisgharan S, Ghaemmaghami AB, Bahonar A, Sarrafzadegan N. Case fatality rate and disability of stroke in Isfahan, Iran: Isfahan stroke registry. Iran J Neurol. 2016; 15(1):9. [PMID] [PMCID]
- Tavahen H, Ghasemi M, Norouzi R, Memar H, Sharifkhah M. [Epidemiological and clinical characteristics of non-traumatic subarachnoid hemorrhage (Persian). J Isfahan Med Sch. 2013; 30(219). [Link]
- Oveisgharan S, Sarrafzadegan N, Shirani S, Hosseini S, Hasanzadeh P, Khosravi A. Stroke in Isfahan, Iran: Hospital admission and 28-day case fatality rate. Cerebrovasc Dis. 2007; 24(6):495-9. [DOI:10.1159/000110418] [PMID]
- Togha M, Bakhtavar K. Factors associated with in-hospital mortality following intracerebral hemorrhage: A three-year study in Tehran, Iran. BMC Neurol. 2004; 4(1):9. [DOI:10.1186/1471-2377-4-9] [PMID] [PMCID]
- Sabzghabaei A, Aeinechian S, Shojaee M, Kashani P, Manouchehrifar M. Epidemiological features of ischemic brain stroke; A cross-sectional hospital-based study. Arch Neurosci . 2019; 6(2). [DOI:10.5812/ans.74362]
- Delbari A, Roghani RS, Tabatabaei SS, Lökk J. A stroke study of an urban area of Iran: Risk factors, length of stay, case fatality, and discharge destination. J Stroke Cerebrovasc Dis. 2010; 19(2):104-9. [DOI:10.1016/j.jstrokecerebrovasdis.2009.06.003] [PMID]
- Amini Sani N, Savadi Oskouei D, Shamshirgaran SM, Dastgiri S, Hashemilar M , Jafariani M. [One-month mortality of stroke in Ardabil province, 2004 (Persian)]. J Ardabil Univ Med Sci. 2006; 7(4):353-6. [Link]
- Parniya R, Savadi Oskuei D, Mousavi S. Mortality rate in patients with intracranial hemorrhage and its risk factors at Alavi Hospital, Ardabil (Persian)]. J Ardabil Univ Med Sci. 2006; 6(4) :363-7. [Link]
- Bakhshayesh B, Hosseininezhad M, Saadat SMS, Hajmanuchehri M, Kazemnezhad E, Ghayeghran A-R. Predicting in-hospital mortality in Iranian patients with spontaneous intracerebral hemorrhage. I J Neurol. 2014; 13(4):231-6. [PMID] [PMCID]
- Razaazian N, Homaayoonfar H. [Mortality of stroke at Farabi hospital (Kermanshah, 1998-2000) (Persian)]. J Kermanshah Univ Med Sci. 2003; 6(4):e81164. [Link]
- Dehghani Firoozabadi M, Kazemi T, Sharifzadeh G, Dadbeh S, Dehghan P. Stroke in Birjand, Iran: A hospital-based study of acute stroke. Iran Red Crescent Med J. 2013; 15(3):264-8. [DOI:10.5812/ircmj.4282] [PMID] [PMCID]
- Ahangar AA, Ashraf Vaghefi SB, Ramaezani M. Epidemiological evaluation of stroke in Babol, northern Iran (2001-2003). Eur Neurol. 2005; 54(2):93-7. [DOI:10.1159/000088643] [PMID]
- Mehryar HR, Khaffafi B, Shadfar F, Khoshakhlagh H, Rezazadeh F, Choobianzali B. The Potential risk factors of Ischemic stroke incidence and mortality. Int J Res App Basic Med Sci. 2019; 5(1):50-68. [Link]
- Khosravi A, Amirifard H, Karami F. Frequency and causes of mortality in patients with stroke referred to Zahedan hospitals in 2016. Int J Res Med Sci. 2018; 6(3):743. [DOI:10.18203/2320-6012.ijrms20180588]
- Khosravi F, Salari H. One-year survival and related factors in patients with ischemic stroke. Int J Health Stud. 2016; 2(4):32-5. [Link]
- Zandieh A, Zeinali Kahaki Z, Sadeghian H, Fakhri M, Pourashraf M, Parviz S, et al. A simple risk score for early ischemic stroke mortality derived from national institutes of health stroke scale: A discriminant analysis. Clin Neurol Neurosurg. 2013; 115(7):1036-9. [DOI:10.1016/j.clineuro.2012.10.034] [PMID]
- Thrift AG, Howard G, Cadilhac DA, Howard VJ, Rothwell PM, Thayabaranathan T, et al. Global stroke statistics: An update of mortality data from countries using a broad code of "cerebrovascular diseases". Int J Stroke. 2017; 12(8):796-801. [DOI:10.1177/1747493017730782] [PMID]
- Heuschmann PU, Kolominsky-Rabas PL, Misselwitz B, Hermanek P, Leffmann C, Janzen R, et al. Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: The German stroke registers study group. Arch Intern Med. 2004; 164(16):1761-8. [DOI:10.1001/archinte.164.16.1761] [PMID]
- Shakeri MT, Nazar I, Saki A, Yousefi R, Hadianfar A, Sasannezhad P. Predictors of in-hospital mortality among suspected stroke patients, Mashhad, Iran: An application of autologistic regression model. 2021; 1-18(Unpublished). [DOI:10.21203/rs.3.rs-337328/v1]
- Okeng’o K, Chillo P, Gray WK, Walker RW, Matuja W. Early mortality and associated factors among patients with stroke admitted to a large teaching hospital in Tanzania. J Stroke Cerebrovasc Dis. 2017; 26(4):871-8. [DOI:10.1016/j.jstrokecerebrovasdis.2016.10.037] [PMID]
- Alhazzani AA, Mahfouz AA, Abolyazid AY, Awadalla NJ, Katramiz K, Faraheen A. In hospital stroke mortality: Rates and determinants in southwestern Saudi Arabia. Int J Environ Res Public Health. 2018; 15(5):927.[DOI:10.3390/ijerph15050927] [PMID] [PMCID]
- Wong K. Risk factors for early death in acute ischemic stroke and intracerebral hemorrhage: A prospective hospital-based study in Asia. Stroke. 1999; 30(11):2326-30. [DOI:10.1161/01.STR.30.11.2326] [PMID]
- Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, et al. Risk score for in-hospital ischemic stroke mortality derived and validated within the get with the guidelines-stroke program. Circulation. 2010; 122(15):1496-504. [DOI:10.1161/CIRCULATIONAHA.109.932822] [PMID]
- Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: Incidence, recurrence, and long-term survival in ischemic stroke subtypes: A population-based study. Stroke. 2001; 32(12):2735-40. [DOI:10.1161/hs1201.100209] [PMID]
- Upoyo AS, Setyopranoto I, Pangastuti HS. The modifiable risk factors of uncontrolled hypertension in stroke: A systematic review and meta-analysis. Stroke Res Treat. 2021; 2021 :6683256. [DOI:10.1155/2021/6683256] [PMID] [PMCID]
- El-Hajj M, Salameh P, Rachidi S, Hosseini H. The epidemiology of stroke in the Middle East. Eur Stroke J. 2016; 1(3):180-98. [DOI:10.1177/2396987316654338] [PMID] [PMCID]
- Anderson CS, Jamrozik KD, Broadhurst RJ, Stewart-Wynne EG. Predicting survival for 1 year among different subtypes of stroke. Results from the Perth Community Stroke Study. Stroke. 1994; 25(10):1935-44. [DOI:10.1161/01.STR.25.10.1935] [PMID]
- Habibi-Koolaee M, Shahmoradi L, Niakan Kalhori SR, Ghannadan H, Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in Gorgan: A retrospective hospital-based study-2015-2016. Neurol Res Int. 2018; 2018:2709654.[DOI:10.1155/2018/2709654] [PMID] [PMCID]
- Tong X, George MG, Yang Q, Gillespie C. Predictors of in-hospital death and symptomatic intracranial hemorrhage in patients with acute ischemic stroke treated with thrombolytic therapy: Paul Coverdell acute stroke registry 2008-2012. Int J Stroke. 2014; 9(6):728-34. [DOI:10.1111/ijs.12155] [PMID] [PMCID]
- Habibi-Koolaee M, Shahmoradi L, Niakan Kalhori SR, Ghannadan H, Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in Gorgan: a retrospective hospital-based study—2015-2016. Neurol Res Int. 2018; 2018. [DOI:10.1155/2018/2709654] [PMCID]
- Thrift AG, Thayabaranathan T, Howard G, Howard VJ, Rothwell PM, Feigin VL, et al. Global stroke statistics. Int J Stroke. 2017; 12(1):13-32. [DOI:10.1177/1747493016676285] [PMID]
- Read S, McAllister D, Colhoun H, Farran B, Fischbacher C, Kerssens J, et al. Incident ischaemic stroke and Type 2 diabetes: Trends in incidence and case fatality in Scotland 2004-2013. Diabet Med. 2018; 35(1):99-106. [DOI:10.1111/dme.13528] [PMID]
- Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003; 2(1):43-53. [DOI:10.1016/S1474-4422(03)00266-7]
- Kumral E, Özkaya B, Sagduyu A, Şirin H, Vardarli E, Pehlivan M. The ege stroke registry: A hospital-based study in the Aegean region, Izmir, Turkey. Cerebrovasc Dis. 1998; 8(5):278-88. [DOI:10.1159/000015866] [PMID]
- Anderson CS, Jamrozik KD, Broadhurst RJ, Stewart-Wynne EG. Predicting survival for 1 year among different subtypes of stroke. Results from the Perth community stroke study. Stroke. 1994; 25(10):1935-44. [DOI:10.1161/01.STR.25.10.1935] [PMID]
- Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. Lancet Neurol. 2009; 8(4):355-69. [DOI:10.1016/S1474-4422(09)70025-0]
- Vangen-Lønne AM, Wilsgaard T, Johnsen SH, Carlsson M, Mathiesen EB. Time trends in incidence and case fatality of ischemic stroke: The Tromsø study 1977-2010. Stroke. 2015; 46(5):1173-9. [DOI:10.1161/STROKEAHA.114.008387] [PMID]
- Gattringer T, Posekany A, Niederkorn K, Knoflach M, Poltrum B, Mutzenbach S, et al. Predicting early mortality of acute ischemic stroke: Score-based approach. Stroke. 2019; 50(2):349-56. [DOI:10.1161/STROKEAHA.118.022863] [PMID]
- Vemmos KN, Bots ML, Tsibouris PK, Zis VP, Grobbee DE, Stranjalis GS, et al. Stroke incidence and case fatality in southern Greece: The Arcadia stroke registry. Stroke. 1999; 30(2):363-70. [DOI:10.1161/01.STR.30.2.363] [PMID]
- Brønnum-Hansen H, Davidsen M, Thorvaldsen P. Long-term survival and causes of death after stroke. Stroke. 2001; 32(9):2131-6. [DOI:10.1161/hs0901.094253] [PMID]
- Kolominsky-Rabas PL, Sarti C, Heuschmann PU, Graf C, Siemonsen S, Neundoerfer B, et al. A prospective community-based study of stroke in Germany--the Erlangen stroke project (ESPro): Incidence and case fatality at 1, 3, and 12 months. Stroke. 1998; 29(12):2501-6. [DOI:10.1161/01.STR.29.12.2501] [PMID]
- Bonita R, Thomson S. Subarachnoid hemorrhage: Epidemiology, diagnosis, management, and outcome. Stroke. 1985; 16(4):591-4. [DOI:10.1161/01.STR.16.4.591] [PMID]
Type of Study: Review |
Subject:
Special
Received: 2022/09/14 | Accepted: 2022/09/28 | Published: 2022/09/28
Received: 2022/09/14 | Accepted: 2022/09/28 | Published: 2022/09/28
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


.jpg)

.jpg)
.jpg)
.jpg)