Thu, Apr 25, 2024
Volume 8, Issue 2 (Spring 2022)
Caspian J Neurol Sci 2022, 8(2): 76-89 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaei S, Jahanbin E. Translation and Validation of the Persian Version of Mindful Eating Questionnaire. Caspian J Neurol Sci 2022; 8 (2) :76-89
URL: http://cjns.gums.ac.ir/article-1-517-en.html
URL: http://cjns.gums.ac.ir/article-1-517-en.html
1- Department of Psychology, Faculty of Literature and Humanities, University of Guilan, Rasht, Iran
Full-Text [PDF 2284 kb]
(476 Downloads)
| Abstract (HTML) (1071 Views)
Full-Text: (478 Views)
Introduction
Mindfulness is a quality of awareness, indicating purposeful and non-judgmental attention to the present moment [1]. Mindfulness reflects being in the moment, without judging and commenting on what is happening, i.e., the experience of pure reality without explanation [2]. Mindfulness helps individuals understand that, although negative emotions occur throughout life, they are not a fixed component of personality and life. Therefore, mindfulness causes the individual to choose thoughtful reactions instead of abnormal responses to these events [3, 4]. This state of mind is often learned through various methods of meditation. This approach was introduced by Jon Kabat‐Zinn (1970) after establishing a stress-reduction clinic at Massachusetts Medical Center [2]. A brief definition of mindfulness is accurate and non-judgmental awareness of the present moment [5]. Evidence indicated that mindfulness and its interventions have desirable effects on various fields. Increasing mindfulness reduces psychological distress and job stress and improves wellbeing and quality of life [6, 7, 8]. It also enhances adaptability and socio-emotional functioning [9].
Eating behavior is a part of nutritional psychology related to nutrition-related factors and normative eating patterns [10]. Eating behavior is a broad term that encompasses a wide range of eating behaviors, such as food choice, motive, diet, eating habits, and eating disorders [10, 11].
In nutrition, mindfulness can be used to describe a non-judgmental awareness of bio-emotional feelings towards eating or in a food-related environment; mindful eating is a skill to lose or maintain weight by creating an awareness of why a subject eats food. For example, mindful eating can help identify and respond to satiety or not respond to inappropriate eating clues such as advertising, fatigue, or anxiety. Mindfulness skills are cognitive abilities, i.e., often distinguished from weight management programs, such as meal planning, record keeping, and food portion control [5]. Today, it is widely accepted that healthy eating is the most critical tool for a healthier life, preventing diseases, and coping with existing conditions. Studies demonstrated that mindful eating is associated with healthier behaviors and less negative emotions [12, 13, 14, 15, 16]. It plays a significant role in maintaining weight in the long run [17].
Theoretically, three eating styles, including emotional eating, eating based on external cues, and restrained eating, are the main mechanisms associated with mindful eating and depression. Emotional eating is eating in response to negative emotions [18], i.e., an abnormal response to stress [19]. It occurs when individuals pay more attention to their emotions than hunger symptoms. This is because they encounter difficulty distinguishing the feeling of hunger from other states of physical arousal. [20]. Similarly, individuals have learned to use eating to respond to emotions to reduce emotional distress [19]. Eating in response to external stimuli includes the appearance of the food, its pleasant smell, and taste, regardless of the feeling of satiety and inner hunger [21]. Restrained eating includes food intake or diet restrictions and checking the amount of food received based on dietary rules instead of addressing the correct signs of hunger and satiety [22]. Restrained eating is associated with positive outcomes, such as weight loss management, and adverse outcomes, such as an increased risk of eating disorders. These results are based on applying the self-regulation methods [23]. Individuals with emotional eating, individuals who eat based on external cues, and restrained eaters ignore the signs of physical hunger and satiety to guide their eating behaviors [24]. Mindfulness is associated with reducing automatic behaviors and increased self-regulation in eating behaviors [25], reducing overeating and inappropriate eating behaviors [26, 27].
Mindful eating is described as a state of non-judgmental attention to emotional and bodily feelings when eating, i.e., suggested to help improve individuals’ eating behaviors and weight loss. By connecting the mind and body, mindful eating makes the individual aware of what they are eating and how they are feeling [28]. It requires a subject’s full awareness to distinguish between physical and emotional hunger. This differentiates the body’s needs and determines whether a subject has received enough food [29]. Awareness of the act of eating makes eating more enjoyable, which includes admiring the food’s shape, smell, and taste. A mindful individual is aware that external factors are not the leading cause of eating. Individuals who are less aware of their eating habits are usually overweight and anxious, have less control over their eating habits, and have higher negative affections. Moreover, these variables can predict eating disorders [29].
With the advancement of technology and lifestyle changes, individuals have become increasingly inactive, affecting their eating habits [30]. The main factors changing subjects’ eating habits include specific emotions, environment, and individual awareness [29]. Researchers hypothesize that yoga exercises may lead to less weight gain due to mindfulness skills learned in yoga teachings, such as focusing on breathing, awareness of movements while practicing it, and meditation. A valid and reliable measure of mindful eating was required to examine whether yoga increases mindfulness or mindful eating in practice [5]. There are several mindfulness scales; however, none focuses on mindful eating [31, 32, 33, 34].
Framson et al. [5] specifically developed a tool for measuring mindful eating that its psychometric properties were explored among pregnant women [35], women seeking weight reduction [36], and a sample of Malaysian overweight and obese adults [37]. According to previous studies, individuals with higher Body Mass Index (BMI) present less mindfulness than those who practice yoga and meditation. Besides, mindful eating is strongly associated with yoga and exercise [38, 39, 40].
Mindfulness plays an influential role in treating and assisting clinical and non-clinical groups. Mindfulness has been used in various interventions. Thus, it is necessary to prepare a valid and reliable tool to measure mindful eating. Having a valid tool to measure mindful eating can help nutrition and psychology researchers to examine whether mindful eating skills are effective and how these skills are acquired through practice and intervention. It also reveals how mindful eating is related to healthy eating behaviors and health consequences. Therefore, the present study intended to translate and determine the psychometric properties of the Mindful Eating Questionnaire (MEQ) in the Iranian population.
Materials and Methods
Design, translation, and procedure
The present descriptive cross-sectional study was based on translation and validation of the questionnaire. The first step to being assured of an admissible translation quality involves selecting the best method for translating the research tool. To translate the questionnaire, Wild et al.’s [41] 10-stage model was selected [41]. For cultural adaptation in the procedure of back translation, endeavors were practiced by the translation group to consider cultural equivalences (e.g. semantic, idiomatic, empirical, & perceptional). Pursuant to Wild et al. [41], the first translation procedure step involves obtaining permission from the instrument developer(s) to use it and selecting the key-in-country individuals. Thus, permission to use the MEQ was received from its developers (Celia Framson; Jeannette M. Schenk; Alyson Littman). By key-in-country individuals, we mean those principal coordinators who manage the procedure of translation in the target country (i.e., first & second authors). Based on the second stage of forwarding translation, the MEQ was independently translated by two translators who had university degrees in psychology. They were also familiar with psychological interventions for obesity, mindfulness, and yoga. Wild et al. [41] held that reconciliation is necessary following forwarding translation. Therefore, a panel including the members of the study team was formed. The translation copies were discussed compared, and their contradictions and differences were specified. Then, they were corrected and integrated into a single copy. The two translators were requested to cooperate with the research concerning back translation. The back translators were residents of Iran, held MA in English and Persian, with a university degree in translation studies. They were also familiar with the translation of psychological scales and questionnaires. Back translation review and harmonization were performed to ensure the conceptual equivalence. Therefore, the research team members identified the problematic items while studying the back translations.
Accordingly, the final Persian version of MEQ (P-MEQ) was provided to 10 MA psychology students to comment on the questions. Furthermore, possible changes were made to make the questions more understandable and to confirm the formal validity of the MEQ. Then, the final translation was reviewed by members of the research team. Eventually, all the procedures’ stages were written in a report, including the taken measures [41].
Next, to determine the reliability of the P-MEQ retest, it was completed by 50 students from two randomly selected classes. After three weeks, the same individuals filled the P-MEQ again. The variance obtained from the first implementation of P-MEQ was used to determine the sample size in the main study.
The participants in the main study included 384 college students of the University of Guilan, one of the largest universities in northern Iran (available at https://guilan.ac.ir/home). These participants were selected by the two-stage cluster sampling method in 2019-2020. Initially, 3 faculties at the main complex of the university (the faculties of Literature & Humanities, Agriculture, Engineering) were randomly selected. Then, the classes held on the even days were randomly sampled, and all male and female students of these classes were considered respondents. The inclusion criteria for the college student population included being a student at the University of Guilan and willingness to cooperate in the project. The exclusion criteria included reluctance to cooperate with the researcher and the incompletion of the inventory
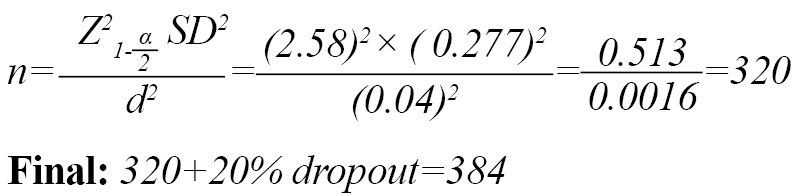
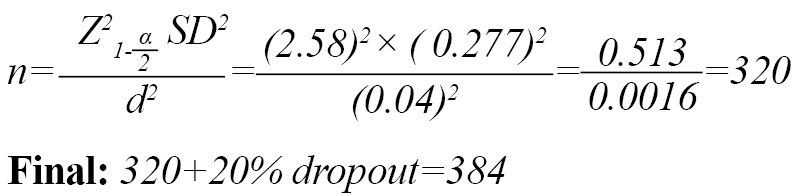
To meet the ethical requirements, the research participants were assured about their privacy and confidentiality of the information. Moreover, the psychological tests and physical measurements were performed anonymously. The study participants were also assured that the collected data would be published as the group average. To determine the sample size in the main study, the mean estimation formula in the population was used [42]. By placing the standard deviation obtained from the first stage of P-MEQ evaluation in students as 0.277 based on a pilot study of 50 subjects in the following sample volume formula [42]; considering 99% confidence level (z=2.58) and tolerable error (d) of 0.04 (about half a point away from the real average), the sample size was estimated as 320 people. The sample size was increased to 384 subjects for accuracy, managing missing data, and considering a 20% sample dropout.
Cronbach’s alpha coefficient was used to determine the internal consistency of P-MEQ and its subscales. The Confirmatory Factor Analysis (CFA) was used to evaluate the construct validity, confirm the dimensions introduced by Framson et al. [5], and fit it with data obtained from the Iranian population. The scores were correlated with the short form of the Freiburg Mindfulness Questionnaire (FMI) scores to determine the concurrent validity of P-MEQ. These two questionnaires were filled out by 60 randomly selected students simultaneously. Finally, to determine known-group validity, 23 very obese participants (BMI: over 35 kg/m2) in a sports club in Rasht City (northern Iran) for yoga and diet therapy were selected by convenient sampling. Besides, their P-MEQ scores were compared with the scores of healthy-weight individuals (BMI: 18.5:25 kg/m2) by the Independent Student t-test. All analyses were performed using SPSS and AMOS. The applied tools in this study are as follows:
Mindful Eating Questionnaire (MEQ): This questionnaire is designed by Framson et al. [5] and contains 28 self-report items with 5 dimensions of mindful eating (i.e., disinhibition, external cues, awareness, emotional response, & distraction). The options are scored based on a 4-point Likert-type scale, ranging from 1 (never/rarely) to 4 (usually/always). A higher score on the MEQ indicates better mindful eating. Framson et al. [5] reported the Cronbach’s alpha coefficient of this questionnaire between 0.64 and 0.83. The Cronbach’s alpha coefficient of the whole questionnaire equals 0.64, suggesting the acceptable reliability of the MEQ. Validity inspection revealed that the MEQ scores were inversely related to BMI greater than 30 kg/m2. Moreover, the scores of yoga practitioners were higher than non-practitioner groups.
The Freiburg Mindfulness Inventory-Short Form (FMI-SF): This 14-item inventory was developed by Walach et al. [43]. The study participants must answer questions based on a 4-point Likert-type scale, ranging from 1 (never/rarely) to 4 (usually/always). Question 13 is scored reversely. The minimum score in this questionnaire is 14, and the maximum is 56. A higher score indicates higher mindfulness. Walach et al. [43] reported the Cronbach’s alpha coefficient of this inventory as 0.86. Ghasemi Jobaneh et al. [44] reported Cronbach’s alpha and test-retest reliability coefficients of FMI-SF equal to 0.92 and 0.83, respectively. The CFA results also confirmed the construct validity and the fit of the data with the inventory structure.
Body Mass Index (BMI): BMI measures individuals’ weight proportionality to their height. This index is calculated by dividing the weight by the square of the person’s height. It is used as one of the most reliable scales to measure the likelihood of being overweight or underweight. The World Health Organization (WHO) considers BMI below 18.5 kg/m2 as being underweight or a sign of malnutrition. On the other hand, an index above 25 kg/m2 is considered overweight; over 30 kg/m2 indicates obesity, and higher than 35 kg/m2 indicates morbid obesity [45]. Since 2000, the BMI has been recognized by the Centers for Disease Control and Prevention in the USA as the best, simplest, and safest way to calculate weight and assess a subject’s health and nutrition status [46].
Results
First sub-study: test-retest reliability (n=50)
Thirty female and 20 male college students (N=50) with a mean±SD age of 20.62±4.20 years (age range: 18-43 years) participated in determining the reliability of the retest. Pearson correlation coefficients data indicated a moderate-to-strong relationship between the first and second-order implementation of the subscales and the total P-MEQ score with a 3-week interval (disinhibition=0.68, external cues=0.58, awareness=0.65, emotional response =0.79, distraction=0.64, & the total score of P-MEQ=0.59). All coefficients were significant at the P<0.0001. Moreover, the Paired Students t-test demonstrated no difference between the first- and second-time scores of P-MEQ (P>0.05). In other words, the P-MEQ scores remained stable after 3 weeks and re-evaluation.
Second sub-study: Confirmatory factor analysis and other psychometric indices (N=384)
The demographic characteristics of the study participants are listed in Table 1.
.jpg)
Three Hundred Forty-Eight students with a mean±SD age of 21.67±4.20 years participated in the study (age range: 18-58 years). Sixty-Six individuals were not interested in walking, and the average walking hours in those who were interested was 5.91±5.10, ranging from 1 to 30 hours per week.
Table 2 lists the matrix of correlation coefficients between demographic characteristics and the scores of P-MEQ subscales.
.jpg)
Notably, there was a positive and significant correlation between the total score of P-MEQ and its subscales (all at P<0.0001), and the most robust relationship is associated with the distraction subscale (r=0.554). The relationship between the total score of P-MEQ and other demographic variables was negligible.
The P-MEQ factors were extracted by the first- and second-order Confirmatory Factor Analysis (CFA) by Maximum odds estimation method and based on the goodness of fit indices in Structural Equation Modeling (SEM), including Chi-square (χ2), Chi-square/degree-of-freedom ratio (normalized Chi-square CMIN/DF), Adjusted Goodness-of-Fit Index (AGFI) >0.8, Parsimonious Comparative Fit Index (PCFI) >0.50, Comparative Fit Index (CFI) >0.90, Incremental Fit Index (IFI) >0.90, and Root Mean Square Error of Approximation (RMSEA) <0.05 using AMOS [47]. Hoelter’s index was used to evaluate the adequacy of the sample size at the levels of 0.05 and 0.01 [48]. Moreover, according to Kline [49], the minimum sample size for CFA is n=200, and 384 individuals were examined in this study. In the second-order factor analysis, it is assumed that the latent variables extracted in the first stage reflect a certain concept and can represent a more general concept at a secondary and higher level [50].
Convergent and divergent validity
The convergent and divergent validity of the MEQ construct was measured by Fornell and Larcker’s [51]approach using Average Variance Extracted (AVE), Maximum Shared Squared Variance (MSV), and Average Shared Square Variance (ASV). The AVE must be greater than 0.5 to establish convergent validity and to confirm divergent validity, MSV and ASV must be below AVE [52].
Reliability
To evaluate the internal consistency of the MEQ, Cronbach’s alpha, Omega McDonald, and Theta coefficients were estimated, and disinhibition and awareness components >0.7 were considered appropriate [53]. However, the other three components’ values were <0.7. There is a relationship between the number of items that make up a scale (the length of the scale) and the Cronbach’s alpha coefficient; thus, a possible reason for the low coefficient of internal consistency of external cues, emotional response, and distraction is the limited number of their constituent items. Therefore, following Cox and Ferguson [54], the mean inter-item correlation method is preferred [54]. According to them, an acceptable scale is the one that the internal correlation of its items varies between 0.20 and 0.40. The mean correlation between the constituent items of external cues, emotional response, and distraction was 0.36, 0.27, and 0.31, respectively. Accordingly, these components also have acceptable reliability. Construct Reliability (CR) was then calculated using CFA. Construct reliability or factor consistency is an alternative to Cronbach’s alpha coefficient in SEM analysis, and construct reliability greater than .7 was considered appropriate [52].
Univariate and multivariate data distributions were examined separately to investigate the normal distribution and outliers. The presence of multivariate outliers was investigated using the Mahalanobis d-squared method (P<0.001). Furthermore, Mardia’s coefficient assessed the multivariate normal distribution (>20).
Moreover, multicollinearity was tested by VIF [49, 55].
The improved first-order factor analysis data indicated that the goodness-of-fit index of chi-square was equal to χ2(261)=656.54 (P<0.001). Then, other indices were examined to evaluate the fitness of the model (RMSEA=0.067, PCFI=0.623, AGFI=0.835, IFI=0.924, & CFI=0.916); all indices confirmed the goodness of fit of the model (Table 3 & Figure 1) [49].
.jpg)
After examining the first-order CFA model and identifying the components of the MEQ construct, the second-order factor analysis was performed by SEM to measure the concept “if the number of components is in the general concept of MEQ”. The second-order CFA fitness indicators vs. the first-order CFA model are presented in Table 3. Figure 2 illustrates the SEM model and CFA of the MEQ construct in the factor loading mode with standardized coefficients.
.jpg)
The values of the obtained factor loadings were >0.4 and significant at the level of 0.001 for all MEQ items except items 4, 8, 14, and 25, i.e., removed from the analysis.
Convergent and divergent validity data
According to Table 4, in the first-order CFA analysis, the AVE of all factors is greater than 0.5, and the AVE per factor is greater than its ASV and MSV.
.jpg)
The results revealed that the MEQ construct has a good convergent and divergent validity. Moreover, in the second-order CFA, AVE is greater than 0.5, which confirms the convergent validity. Table 4 lists that the internal stability and CR (>0.7) of the four extracted P-MEQ factors are confirmed.
Third sub-study: Concurrent validity (n=56)
In the concurrent validity phase, 42 female and 14 male students (n=56) with a mean±SD age of 22.12±2.85 years were present (age range: 18-37 years). Pearson correlation coefficient results signified a poor correlation between the total score of P-MEQ and the total score of FMI-SF (r=0.24, P=0.07). After removing the identified items with poor factor loading in CFA (items 4, 8, 14, and 25,), the Pearson correlation analysis again revealed a weaker relationship between the revised P-MEQ and the total FMI-SF score (r=0.08, P=0.55).
Fourth sub-study: Validity of known groups
In this study, 30 participants (15 males & 15 females) with normal BMI (18.5 to <25) were compared with 23 very obese participants (18 females & 5 males; BMI: >35.0 kg/m2) concerning P-MEQ subscales. The independent student t-test (Table 5) reveals that the obese group had lower scores in distraction, disinhibition, and emotional response subscales than normal people. However, the same group achieved better awareness and external cues subscales scores than healthy subjects. However, these two groups were not different in the total P-MEQ scores (Table 5).
.jpg)
Discussion
The present study intended to translate and determine the psychometric features of the Persian version of MEQ in the Iranian population. The test-retest reliability of the total P-MEQ after 3 weeks was equal to 0.59, and that of the disinhibition, external cues, emotional response, and distraction was in the range of 0.58 to 0.79. This result is not comparable with Framson et al. [5] because their study did not calculate such an index. The results of this study were consistent with those of Abbaspoor et al. [36]on Iranian women who were seeking weight reduction. Test-Retest reliability was obtained as poor to fair in Malaysian adults with overweight and obese [37] for the MEQ dimensions (between 0.26 and 0.45); however, it was strong (r=0.85) in a sample of pregnant women [35]. The strong result in the Apolzan et al.’s study [35] was due to the evaluation of a more homogeneous sample, and obtaining weaker results in the Abdul Basir et al.’s study [37], compared to the present study was due to the 8-week interval to determine the stability over time. However, the result of this research in the Iranian population suggests that the repeatability of P-MEQ results can be trusted over time.
The construct validity of P-MEQ was evaluated through CFA. The analysis results showed that items 4, 8, and 14 from the external cues and item 25 of disinhibition had a weak factor loading and were excluded from the CFA. The possible justification for omitting these items is the particular structure of two-stage scoring, especially items 4 and 8, and the lack of conceptual commonalities of these four questions with the latent factor related to it in the Iranian population. After deleting these 4 questions and freeing some covariance errors terms in Figure 1, the 5-factor model of the first-order P-MEQ demonstrated a good fit with the factors introduced by Framson et al.
.jpg)
[5] (i.e., awareness, distraction, disinhibition, emotional response, & external cues). The second-order CFA also confirmed that the 5 factors of mindful eating in the Iranian population could be interpreted in terms of the general concept of MEQ (Figure 2). Consistent with this study, Abbaspoor et al. [36] among women seeking weight reduction through exploratory factor analysis indicated that MEQ is divisible to the same dimensions as Framson et al. [5] claim. However, a study among overweight and obese adults in Malaysia revealed that MEQ has 7 components. Cross-cultural and linguistic differences may influence achieving such discrepant results [37].
Cronbach, McDonald’s omega, and Theta alpha coefficients were suitable for the awareness and disinhibition factors after removing items with low factor loadings. However, this coefficient was <0.70 for other subscales. This result of reliability analysis may be due to the limited number of items within each factor. Therefore, following Cox and Ferguson [54], the mean correlation of the items was used to determine the P-MEQ reliability, which was obtained in the 0.20-0.40 range for distraction, emotional response, and external cue subscales. In previous studies, Cronbach’s alpha coefficient of 0.64 [37] and 0.56 [35] was reported for the MEQ total score. The same coefficient for MEQ components in women seeking weight reduction was measured as 0.73-0.81 [36]. In Framson et al.’s [5] study, the distraction factor had a Cronbach’s alpha coefficient below 0.70. However, the mean Cronbach’s alpha coefficients of the 5 subscales in their study (α=64) were interestingly consistent with the mean of the same coefficients in the present study (see Table 4). These results indicate that P-MEQ has good internal coherence. This tool’s internal consistency is at least acceptable [49], and each item measures a similar concept and structure.
The findings as to concurrent validity indicated that the total P-MEQ scores lacked an acceptable correlation with the total FMI-SF scores even after removing the items with low factor loading. Although the Persian version of FMI-SF acquired good psychometric properties in the Iranian population, it did not significantly correlate with P-MEQ in this study (r=0.24). Therefore, the concurrent validity of P-MEQ was not confirmed. In contrast to the present study, the results of Beshara et al. [12]in North Australia indicated that high mindfulness scores were associated with mindful eating, and more mindful eating was associated with choosing smaller portions of high-energy foods. In a student population, Jordan et al. [13] outlined that high levels of mindfulness are associated with a greater tendency to choose fruit instead of confections and adopt healthier eating behaviors. Moreover, Apolzan et al. [35] reported acceptable concurrent validity for MEQ through its correlation with Mindful Attention Awareness Scale (MAAS) scores in a sample of pregnant women.
To justify these disparities with the P-MEQ study, it is noted that the majority of the participants in this study had normal BMI; therefore, these individuals do not feel restrained in eating. Therefore, there may be no concurrence between mindfulness and mindful eating. Moreover, most Asian countries (including Iran) transition from traditional to Western and machine lifestyles. Accordingly, the interest in fast foods is growing [56, 57]. With the industrialization and development of societies, physical activities decline significantly, including occupational and interactive activities. Concurrently, there is a shift in eating habits from traditional vegetarian and carbohydrate diets to high-fat types. Lifestyle alternations in these communities have increased the prevalence of overweight and obesity [30]. Wrong eating habits can dominate rapid eating habits, and a person’s mindfulness may not be affected by wrong eating habits. Therefore, a mindful person may not be mindful of their eating behavior.
The evaluation results of the known group’s validity indicated that the group with normal BMI obtained better scores in distraction, disinhibition, and emotional response than the group with a BMI of ≥35 kg/m2 (very obese). Furthermore, the obese group acquired a better awareness and external cues than the normal BMI group. Some obtained findings are consistent with the Malaysian version [37]. These results reveal that obese people in the study who exercise to lose weight in the sports clubs are more aware of food’s taste, appearance, and psychological effects. They also recognize clues that encourage them to eat more. These mindfulness skills may have been developed through the mindful efforts of obese people and their coaches. However, comparisons between the two groups suggested that very obese populations had a busier mental space when eating than those with a healthy BMI. Their behavioral inhibitions are weaker when complete, and they stop eating later. They are more likely to be trapped by emotional factors that encourage more eating. These results suggest that implementing therapeutic interventions to reduce distraction and disinhibition and improve emotion regulation skills may help lose weight. The results highlighted that practicing yoga and meditation, which include components of mindfulness, constructively impact reducing fatigue, increasing body awareness, and managing patients’ stress [8]. It can also be associated with lower BMI [38, 39, 40].
The study population was mainly restricted to university students. Therefore, generalizing the obtained results to other critical clinical populations, such as patients with eating disorders, people at risk of overweight, and obesity, is not logical. There was no significant difference between the healthy and very obese groups regarding the total P-MEQ score. The collected results revealed no cut-off point for differentiating individuals with poorer mindful eating status. It is suggested to find a cut-off point by improving and rewriting the items and adding the cultural factors of West Asia in the Persian version of MEQ for screening groups at risk of obesity. Moreover, there may be gender differences in mindful eating and eating behaviors neglected in this study. Therefore, future studies can evaluate and compare the gender-wise invariance of structural and confirmatory models of the P-MEQ.
The third wave of psychological therapies is mainly focused on the concept of mindfulness [58]. Mindfulness is a process that reduces negative emotions and symptoms of various disorders, including obesity and eating disorders [14, 15, 16]. The results of this study are applicable in psychological wellbeing, treating eating disorders, obesity, and related problems. Undoubtedly, the development of efficient tools for evaluating clients and monitoring the process of therapeutic interventions is an essential step in recognizing and measuring mindful eating behavior in the clinical domain.
Conclusion
The Persian version of MEQ has appropriate face validity, test-retest reliability, and internal consistency. Four items were removed from the Persian version due to poor factor loadings. The first and second-order 5-factor structural model of the P-MEQ has a good fit in the Iranian population. However, the concurrent validity of this questionnaire was not confirmed.
Ethical Considerations
Compliance with ethical guidelines
All study procedures complied with the ethical standards outlined in the Helsinki Declaration (2013). Informed Consent Informed consent was obtained from all participants.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology, software, validation, formal analysis: Sajjad Rezaei; Investigation, resources: all author; Data curation, writing – original draft preparation: Elham Jahanbin; Writing – review & editing, visualization, supervision: Sajjad Rezaei; Project administration, and funding acquisition: Elham Jahanbin.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Hereby the authors express their gratitude towards the students at University of Guilan - Rasht and the applicants of yoga exercises in Mehr Clinic (in the north of Iran) for their participation in this research.
References
Mindfulness is a quality of awareness, indicating purposeful and non-judgmental attention to the present moment [1]. Mindfulness reflects being in the moment, without judging and commenting on what is happening, i.e., the experience of pure reality without explanation [2]. Mindfulness helps individuals understand that, although negative emotions occur throughout life, they are not a fixed component of personality and life. Therefore, mindfulness causes the individual to choose thoughtful reactions instead of abnormal responses to these events [3, 4]. This state of mind is often learned through various methods of meditation. This approach was introduced by Jon Kabat‐Zinn (1970) after establishing a stress-reduction clinic at Massachusetts Medical Center [2]. A brief definition of mindfulness is accurate and non-judgmental awareness of the present moment [5]. Evidence indicated that mindfulness and its interventions have desirable effects on various fields. Increasing mindfulness reduces psychological distress and job stress and improves wellbeing and quality of life [6, 7, 8]. It also enhances adaptability and socio-emotional functioning [9].
Eating behavior is a part of nutritional psychology related to nutrition-related factors and normative eating patterns [10]. Eating behavior is a broad term that encompasses a wide range of eating behaviors, such as food choice, motive, diet, eating habits, and eating disorders [10, 11].
In nutrition, mindfulness can be used to describe a non-judgmental awareness of bio-emotional feelings towards eating or in a food-related environment; mindful eating is a skill to lose or maintain weight by creating an awareness of why a subject eats food. For example, mindful eating can help identify and respond to satiety or not respond to inappropriate eating clues such as advertising, fatigue, or anxiety. Mindfulness skills are cognitive abilities, i.e., often distinguished from weight management programs, such as meal planning, record keeping, and food portion control [5]. Today, it is widely accepted that healthy eating is the most critical tool for a healthier life, preventing diseases, and coping with existing conditions. Studies demonstrated that mindful eating is associated with healthier behaviors and less negative emotions [12, 13, 14, 15, 16]. It plays a significant role in maintaining weight in the long run [17].
Theoretically, three eating styles, including emotional eating, eating based on external cues, and restrained eating, are the main mechanisms associated with mindful eating and depression. Emotional eating is eating in response to negative emotions [18], i.e., an abnormal response to stress [19]. It occurs when individuals pay more attention to their emotions than hunger symptoms. This is because they encounter difficulty distinguishing the feeling of hunger from other states of physical arousal. [20]. Similarly, individuals have learned to use eating to respond to emotions to reduce emotional distress [19]. Eating in response to external stimuli includes the appearance of the food, its pleasant smell, and taste, regardless of the feeling of satiety and inner hunger [21]. Restrained eating includes food intake or diet restrictions and checking the amount of food received based on dietary rules instead of addressing the correct signs of hunger and satiety [22]. Restrained eating is associated with positive outcomes, such as weight loss management, and adverse outcomes, such as an increased risk of eating disorders. These results are based on applying the self-regulation methods [23]. Individuals with emotional eating, individuals who eat based on external cues, and restrained eaters ignore the signs of physical hunger and satiety to guide their eating behaviors [24]. Mindfulness is associated with reducing automatic behaviors and increased self-regulation in eating behaviors [25], reducing overeating and inappropriate eating behaviors [26, 27].
Mindful eating is described as a state of non-judgmental attention to emotional and bodily feelings when eating, i.e., suggested to help improve individuals’ eating behaviors and weight loss. By connecting the mind and body, mindful eating makes the individual aware of what they are eating and how they are feeling [28]. It requires a subject’s full awareness to distinguish between physical and emotional hunger. This differentiates the body’s needs and determines whether a subject has received enough food [29]. Awareness of the act of eating makes eating more enjoyable, which includes admiring the food’s shape, smell, and taste. A mindful individual is aware that external factors are not the leading cause of eating. Individuals who are less aware of their eating habits are usually overweight and anxious, have less control over their eating habits, and have higher negative affections. Moreover, these variables can predict eating disorders [29].
With the advancement of technology and lifestyle changes, individuals have become increasingly inactive, affecting their eating habits [30]. The main factors changing subjects’ eating habits include specific emotions, environment, and individual awareness [29]. Researchers hypothesize that yoga exercises may lead to less weight gain due to mindfulness skills learned in yoga teachings, such as focusing on breathing, awareness of movements while practicing it, and meditation. A valid and reliable measure of mindful eating was required to examine whether yoga increases mindfulness or mindful eating in practice [5]. There are several mindfulness scales; however, none focuses on mindful eating [31, 32, 33, 34].
Framson et al. [5] specifically developed a tool for measuring mindful eating that its psychometric properties were explored among pregnant women [35], women seeking weight reduction [36], and a sample of Malaysian overweight and obese adults [37]. According to previous studies, individuals with higher Body Mass Index (BMI) present less mindfulness than those who practice yoga and meditation. Besides, mindful eating is strongly associated with yoga and exercise [38, 39, 40].
Mindfulness plays an influential role in treating and assisting clinical and non-clinical groups. Mindfulness has been used in various interventions. Thus, it is necessary to prepare a valid and reliable tool to measure mindful eating. Having a valid tool to measure mindful eating can help nutrition and psychology researchers to examine whether mindful eating skills are effective and how these skills are acquired through practice and intervention. It also reveals how mindful eating is related to healthy eating behaviors and health consequences. Therefore, the present study intended to translate and determine the psychometric properties of the Mindful Eating Questionnaire (MEQ) in the Iranian population.
Materials and Methods
Design, translation, and procedure
The present descriptive cross-sectional study was based on translation and validation of the questionnaire. The first step to being assured of an admissible translation quality involves selecting the best method for translating the research tool. To translate the questionnaire, Wild et al.’s [41] 10-stage model was selected [41]. For cultural adaptation in the procedure of back translation, endeavors were practiced by the translation group to consider cultural equivalences (e.g. semantic, idiomatic, empirical, & perceptional). Pursuant to Wild et al. [41], the first translation procedure step involves obtaining permission from the instrument developer(s) to use it and selecting the key-in-country individuals. Thus, permission to use the MEQ was received from its developers (Celia Framson; Jeannette M. Schenk; Alyson Littman). By key-in-country individuals, we mean those principal coordinators who manage the procedure of translation in the target country (i.e., first & second authors). Based on the second stage of forwarding translation, the MEQ was independently translated by two translators who had university degrees in psychology. They were also familiar with psychological interventions for obesity, mindfulness, and yoga. Wild et al. [41] held that reconciliation is necessary following forwarding translation. Therefore, a panel including the members of the study team was formed. The translation copies were discussed compared, and their contradictions and differences were specified. Then, they were corrected and integrated into a single copy. The two translators were requested to cooperate with the research concerning back translation. The back translators were residents of Iran, held MA in English and Persian, with a university degree in translation studies. They were also familiar with the translation of psychological scales and questionnaires. Back translation review and harmonization were performed to ensure the conceptual equivalence. Therefore, the research team members identified the problematic items while studying the back translations.
Accordingly, the final Persian version of MEQ (P-MEQ) was provided to 10 MA psychology students to comment on the questions. Furthermore, possible changes were made to make the questions more understandable and to confirm the formal validity of the MEQ. Then, the final translation was reviewed by members of the research team. Eventually, all the procedures’ stages were written in a report, including the taken measures [41].
Next, to determine the reliability of the P-MEQ retest, it was completed by 50 students from two randomly selected classes. After three weeks, the same individuals filled the P-MEQ again. The variance obtained from the first implementation of P-MEQ was used to determine the sample size in the main study.
The participants in the main study included 384 college students of the University of Guilan, one of the largest universities in northern Iran (available at https://guilan.ac.ir/home). These participants were selected by the two-stage cluster sampling method in 2019-2020. Initially, 3 faculties at the main complex of the university (the faculties of Literature & Humanities, Agriculture, Engineering) were randomly selected. Then, the classes held on the even days were randomly sampled, and all male and female students of these classes were considered respondents. The inclusion criteria for the college student population included being a student at the University of Guilan and willingness to cooperate in the project. The exclusion criteria included reluctance to cooperate with the researcher and the incompletion of the inventory
To meet the ethical requirements, the research participants were assured about their privacy and confidentiality of the information. Moreover, the psychological tests and physical measurements were performed anonymously. The study participants were also assured that the collected data would be published as the group average. To determine the sample size in the main study, the mean estimation formula in the population was used [42]. By placing the standard deviation obtained from the first stage of P-MEQ evaluation in students as 0.277 based on a pilot study of 50 subjects in the following sample volume formula [42]; considering 99% confidence level (z=2.58) and tolerable error (d) of 0.04 (about half a point away from the real average), the sample size was estimated as 320 people. The sample size was increased to 384 subjects for accuracy, managing missing data, and considering a 20% sample dropout.
Cronbach’s alpha coefficient was used to determine the internal consistency of P-MEQ and its subscales. The Confirmatory Factor Analysis (CFA) was used to evaluate the construct validity, confirm the dimensions introduced by Framson et al. [5], and fit it with data obtained from the Iranian population. The scores were correlated with the short form of the Freiburg Mindfulness Questionnaire (FMI) scores to determine the concurrent validity of P-MEQ. These two questionnaires were filled out by 60 randomly selected students simultaneously. Finally, to determine known-group validity, 23 very obese participants (BMI: over 35 kg/m2) in a sports club in Rasht City (northern Iran) for yoga and diet therapy were selected by convenient sampling. Besides, their P-MEQ scores were compared with the scores of healthy-weight individuals (BMI: 18.5:25 kg/m2) by the Independent Student t-test. All analyses were performed using SPSS and AMOS. The applied tools in this study are as follows:
Mindful Eating Questionnaire (MEQ): This questionnaire is designed by Framson et al. [5] and contains 28 self-report items with 5 dimensions of mindful eating (i.e., disinhibition, external cues, awareness, emotional response, & distraction). The options are scored based on a 4-point Likert-type scale, ranging from 1 (never/rarely) to 4 (usually/always). A higher score on the MEQ indicates better mindful eating. Framson et al. [5] reported the Cronbach’s alpha coefficient of this questionnaire between 0.64 and 0.83. The Cronbach’s alpha coefficient of the whole questionnaire equals 0.64, suggesting the acceptable reliability of the MEQ. Validity inspection revealed that the MEQ scores were inversely related to BMI greater than 30 kg/m2. Moreover, the scores of yoga practitioners were higher than non-practitioner groups.
The Freiburg Mindfulness Inventory-Short Form (FMI-SF): This 14-item inventory was developed by Walach et al. [43]. The study participants must answer questions based on a 4-point Likert-type scale, ranging from 1 (never/rarely) to 4 (usually/always). Question 13 is scored reversely. The minimum score in this questionnaire is 14, and the maximum is 56. A higher score indicates higher mindfulness. Walach et al. [43] reported the Cronbach’s alpha coefficient of this inventory as 0.86. Ghasemi Jobaneh et al. [44] reported Cronbach’s alpha and test-retest reliability coefficients of FMI-SF equal to 0.92 and 0.83, respectively. The CFA results also confirmed the construct validity and the fit of the data with the inventory structure.
Body Mass Index (BMI): BMI measures individuals’ weight proportionality to their height. This index is calculated by dividing the weight by the square of the person’s height. It is used as one of the most reliable scales to measure the likelihood of being overweight or underweight. The World Health Organization (WHO) considers BMI below 18.5 kg/m2 as being underweight or a sign of malnutrition. On the other hand, an index above 25 kg/m2 is considered overweight; over 30 kg/m2 indicates obesity, and higher than 35 kg/m2 indicates morbid obesity [45]. Since 2000, the BMI has been recognized by the Centers for Disease Control and Prevention in the USA as the best, simplest, and safest way to calculate weight and assess a subject’s health and nutrition status [46].
Results
First sub-study: test-retest reliability (n=50)
Thirty female and 20 male college students (N=50) with a mean±SD age of 20.62±4.20 years (age range: 18-43 years) participated in determining the reliability of the retest. Pearson correlation coefficients data indicated a moderate-to-strong relationship between the first and second-order implementation of the subscales and the total P-MEQ score with a 3-week interval (disinhibition=0.68, external cues=0.58, awareness=0.65, emotional response =0.79, distraction=0.64, & the total score of P-MEQ=0.59). All coefficients were significant at the P<0.0001. Moreover, the Paired Students t-test demonstrated no difference between the first- and second-time scores of P-MEQ (P>0.05). In other words, the P-MEQ scores remained stable after 3 weeks and re-evaluation.
Second sub-study: Confirmatory factor analysis and other psychometric indices (N=384)
The demographic characteristics of the study participants are listed in Table 1.
.jpg)
Three Hundred Forty-Eight students with a mean±SD age of 21.67±4.20 years participated in the study (age range: 18-58 years). Sixty-Six individuals were not interested in walking, and the average walking hours in those who were interested was 5.91±5.10, ranging from 1 to 30 hours per week.
Table 2 lists the matrix of correlation coefficients between demographic characteristics and the scores of P-MEQ subscales.
.jpg)
Notably, there was a positive and significant correlation between the total score of P-MEQ and its subscales (all at P<0.0001), and the most robust relationship is associated with the distraction subscale (r=0.554). The relationship between the total score of P-MEQ and other demographic variables was negligible.
The P-MEQ factors were extracted by the first- and second-order Confirmatory Factor Analysis (CFA) by Maximum odds estimation method and based on the goodness of fit indices in Structural Equation Modeling (SEM), including Chi-square (χ2), Chi-square/degree-of-freedom ratio (normalized Chi-square CMIN/DF), Adjusted Goodness-of-Fit Index (AGFI) >0.8, Parsimonious Comparative Fit Index (PCFI) >0.50, Comparative Fit Index (CFI) >0.90, Incremental Fit Index (IFI) >0.90, and Root Mean Square Error of Approximation (RMSEA) <0.05 using AMOS [47]. Hoelter’s index was used to evaluate the adequacy of the sample size at the levels of 0.05 and 0.01 [48]. Moreover, according to Kline [49], the minimum sample size for CFA is n=200, and 384 individuals were examined in this study. In the second-order factor analysis, it is assumed that the latent variables extracted in the first stage reflect a certain concept and can represent a more general concept at a secondary and higher level [50].
Convergent and divergent validity
The convergent and divergent validity of the MEQ construct was measured by Fornell and Larcker’s [51]approach using Average Variance Extracted (AVE), Maximum Shared Squared Variance (MSV), and Average Shared Square Variance (ASV). The AVE must be greater than 0.5 to establish convergent validity and to confirm divergent validity, MSV and ASV must be below AVE [52].
Reliability
To evaluate the internal consistency of the MEQ, Cronbach’s alpha, Omega McDonald, and Theta coefficients were estimated, and disinhibition and awareness components >0.7 were considered appropriate [53]. However, the other three components’ values were <0.7. There is a relationship between the number of items that make up a scale (the length of the scale) and the Cronbach’s alpha coefficient; thus, a possible reason for the low coefficient of internal consistency of external cues, emotional response, and distraction is the limited number of their constituent items. Therefore, following Cox and Ferguson [54], the mean inter-item correlation method is preferred [54]. According to them, an acceptable scale is the one that the internal correlation of its items varies between 0.20 and 0.40. The mean correlation between the constituent items of external cues, emotional response, and distraction was 0.36, 0.27, and 0.31, respectively. Accordingly, these components also have acceptable reliability. Construct Reliability (CR) was then calculated using CFA. Construct reliability or factor consistency is an alternative to Cronbach’s alpha coefficient in SEM analysis, and construct reliability greater than .7 was considered appropriate [52].
Univariate and multivariate data distributions were examined separately to investigate the normal distribution and outliers. The presence of multivariate outliers was investigated using the Mahalanobis d-squared method (P<0.001). Furthermore, Mardia’s coefficient assessed the multivariate normal distribution (>20).
Moreover, multicollinearity was tested by VIF [49, 55].
The improved first-order factor analysis data indicated that the goodness-of-fit index of chi-square was equal to χ2(261)=656.54 (P<0.001). Then, other indices were examined to evaluate the fitness of the model (RMSEA=0.067, PCFI=0.623, AGFI=0.835, IFI=0.924, & CFI=0.916); all indices confirmed the goodness of fit of the model (Table 3 & Figure 1) [49].
.jpg)
After examining the first-order CFA model and identifying the components of the MEQ construct, the second-order factor analysis was performed by SEM to measure the concept “if the number of components is in the general concept of MEQ”. The second-order CFA fitness indicators vs. the first-order CFA model are presented in Table 3. Figure 2 illustrates the SEM model and CFA of the MEQ construct in the factor loading mode with standardized coefficients.
.jpg)
The values of the obtained factor loadings were >0.4 and significant at the level of 0.001 for all MEQ items except items 4, 8, 14, and 25, i.e., removed from the analysis.
Convergent and divergent validity data
According to Table 4, in the first-order CFA analysis, the AVE of all factors is greater than 0.5, and the AVE per factor is greater than its ASV and MSV.
.jpg)
The results revealed that the MEQ construct has a good convergent and divergent validity. Moreover, in the second-order CFA, AVE is greater than 0.5, which confirms the convergent validity. Table 4 lists that the internal stability and CR (>0.7) of the four extracted P-MEQ factors are confirmed.
Third sub-study: Concurrent validity (n=56)
In the concurrent validity phase, 42 female and 14 male students (n=56) with a mean±SD age of 22.12±2.85 years were present (age range: 18-37 years). Pearson correlation coefficient results signified a poor correlation between the total score of P-MEQ and the total score of FMI-SF (r=0.24, P=0.07). After removing the identified items with poor factor loading in CFA (items 4, 8, 14, and 25,), the Pearson correlation analysis again revealed a weaker relationship between the revised P-MEQ and the total FMI-SF score (r=0.08, P=0.55).
Fourth sub-study: Validity of known groups
In this study, 30 participants (15 males & 15 females) with normal BMI (18.5 to <25) were compared with 23 very obese participants (18 females & 5 males; BMI: >35.0 kg/m2) concerning P-MEQ subscales. The independent student t-test (Table 5) reveals that the obese group had lower scores in distraction, disinhibition, and emotional response subscales than normal people. However, the same group achieved better awareness and external cues subscales scores than healthy subjects. However, these two groups were not different in the total P-MEQ scores (Table 5).
.jpg)
Discussion
The present study intended to translate and determine the psychometric features of the Persian version of MEQ in the Iranian population. The test-retest reliability of the total P-MEQ after 3 weeks was equal to 0.59, and that of the disinhibition, external cues, emotional response, and distraction was in the range of 0.58 to 0.79. This result is not comparable with Framson et al. [5] because their study did not calculate such an index. The results of this study were consistent with those of Abbaspoor et al. [36]on Iranian women who were seeking weight reduction. Test-Retest reliability was obtained as poor to fair in Malaysian adults with overweight and obese [37] for the MEQ dimensions (between 0.26 and 0.45); however, it was strong (r=0.85) in a sample of pregnant women [35]. The strong result in the Apolzan et al.’s study [35] was due to the evaluation of a more homogeneous sample, and obtaining weaker results in the Abdul Basir et al.’s study [37], compared to the present study was due to the 8-week interval to determine the stability over time. However, the result of this research in the Iranian population suggests that the repeatability of P-MEQ results can be trusted over time.
The construct validity of P-MEQ was evaluated through CFA. The analysis results showed that items 4, 8, and 14 from the external cues and item 25 of disinhibition had a weak factor loading and were excluded from the CFA. The possible justification for omitting these items is the particular structure of two-stage scoring, especially items 4 and 8, and the lack of conceptual commonalities of these four questions with the latent factor related to it in the Iranian population. After deleting these 4 questions and freeing some covariance errors terms in Figure 1, the 5-factor model of the first-order P-MEQ demonstrated a good fit with the factors introduced by Framson et al.
.jpg)
[5] (i.e., awareness, distraction, disinhibition, emotional response, & external cues). The second-order CFA also confirmed that the 5 factors of mindful eating in the Iranian population could be interpreted in terms of the general concept of MEQ (Figure 2). Consistent with this study, Abbaspoor et al. [36] among women seeking weight reduction through exploratory factor analysis indicated that MEQ is divisible to the same dimensions as Framson et al. [5] claim. However, a study among overweight and obese adults in Malaysia revealed that MEQ has 7 components. Cross-cultural and linguistic differences may influence achieving such discrepant results [37].
Cronbach, McDonald’s omega, and Theta alpha coefficients were suitable for the awareness and disinhibition factors after removing items with low factor loadings. However, this coefficient was <0.70 for other subscales. This result of reliability analysis may be due to the limited number of items within each factor. Therefore, following Cox and Ferguson [54], the mean correlation of the items was used to determine the P-MEQ reliability, which was obtained in the 0.20-0.40 range for distraction, emotional response, and external cue subscales. In previous studies, Cronbach’s alpha coefficient of 0.64 [37] and 0.56 [35] was reported for the MEQ total score. The same coefficient for MEQ components in women seeking weight reduction was measured as 0.73-0.81 [36]. In Framson et al.’s [5] study, the distraction factor had a Cronbach’s alpha coefficient below 0.70. However, the mean Cronbach’s alpha coefficients of the 5 subscales in their study (α=64) were interestingly consistent with the mean of the same coefficients in the present study (see Table 4). These results indicate that P-MEQ has good internal coherence. This tool’s internal consistency is at least acceptable [49], and each item measures a similar concept and structure.
The findings as to concurrent validity indicated that the total P-MEQ scores lacked an acceptable correlation with the total FMI-SF scores even after removing the items with low factor loading. Although the Persian version of FMI-SF acquired good psychometric properties in the Iranian population, it did not significantly correlate with P-MEQ in this study (r=0.24). Therefore, the concurrent validity of P-MEQ was not confirmed. In contrast to the present study, the results of Beshara et al. [12]in North Australia indicated that high mindfulness scores were associated with mindful eating, and more mindful eating was associated with choosing smaller portions of high-energy foods. In a student population, Jordan et al. [13] outlined that high levels of mindfulness are associated with a greater tendency to choose fruit instead of confections and adopt healthier eating behaviors. Moreover, Apolzan et al. [35] reported acceptable concurrent validity for MEQ through its correlation with Mindful Attention Awareness Scale (MAAS) scores in a sample of pregnant women.
To justify these disparities with the P-MEQ study, it is noted that the majority of the participants in this study had normal BMI; therefore, these individuals do not feel restrained in eating. Therefore, there may be no concurrence between mindfulness and mindful eating. Moreover, most Asian countries (including Iran) transition from traditional to Western and machine lifestyles. Accordingly, the interest in fast foods is growing [56, 57]. With the industrialization and development of societies, physical activities decline significantly, including occupational and interactive activities. Concurrently, there is a shift in eating habits from traditional vegetarian and carbohydrate diets to high-fat types. Lifestyle alternations in these communities have increased the prevalence of overweight and obesity [30]. Wrong eating habits can dominate rapid eating habits, and a person’s mindfulness may not be affected by wrong eating habits. Therefore, a mindful person may not be mindful of their eating behavior.
The evaluation results of the known group’s validity indicated that the group with normal BMI obtained better scores in distraction, disinhibition, and emotional response than the group with a BMI of ≥35 kg/m2 (very obese). Furthermore, the obese group acquired a better awareness and external cues than the normal BMI group. Some obtained findings are consistent with the Malaysian version [37]. These results reveal that obese people in the study who exercise to lose weight in the sports clubs are more aware of food’s taste, appearance, and psychological effects. They also recognize clues that encourage them to eat more. These mindfulness skills may have been developed through the mindful efforts of obese people and their coaches. However, comparisons between the two groups suggested that very obese populations had a busier mental space when eating than those with a healthy BMI. Their behavioral inhibitions are weaker when complete, and they stop eating later. They are more likely to be trapped by emotional factors that encourage more eating. These results suggest that implementing therapeutic interventions to reduce distraction and disinhibition and improve emotion regulation skills may help lose weight. The results highlighted that practicing yoga and meditation, which include components of mindfulness, constructively impact reducing fatigue, increasing body awareness, and managing patients’ stress [8]. It can also be associated with lower BMI [38, 39, 40].
The study population was mainly restricted to university students. Therefore, generalizing the obtained results to other critical clinical populations, such as patients with eating disorders, people at risk of overweight, and obesity, is not logical. There was no significant difference between the healthy and very obese groups regarding the total P-MEQ score. The collected results revealed no cut-off point for differentiating individuals with poorer mindful eating status. It is suggested to find a cut-off point by improving and rewriting the items and adding the cultural factors of West Asia in the Persian version of MEQ for screening groups at risk of obesity. Moreover, there may be gender differences in mindful eating and eating behaviors neglected in this study. Therefore, future studies can evaluate and compare the gender-wise invariance of structural and confirmatory models of the P-MEQ.
The third wave of psychological therapies is mainly focused on the concept of mindfulness [58]. Mindfulness is a process that reduces negative emotions and symptoms of various disorders, including obesity and eating disorders [14, 15, 16]. The results of this study are applicable in psychological wellbeing, treating eating disorders, obesity, and related problems. Undoubtedly, the development of efficient tools for evaluating clients and monitoring the process of therapeutic interventions is an essential step in recognizing and measuring mindful eating behavior in the clinical domain.
Conclusion
The Persian version of MEQ has appropriate face validity, test-retest reliability, and internal consistency. Four items were removed from the Persian version due to poor factor loadings. The first and second-order 5-factor structural model of the P-MEQ has a good fit in the Iranian population. However, the concurrent validity of this questionnaire was not confirmed.
Ethical Considerations
Compliance with ethical guidelines
All study procedures complied with the ethical standards outlined in the Helsinki Declaration (2013). Informed Consent Informed consent was obtained from all participants.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors contributions
Conceptualization, methodology, software, validation, formal analysis: Sajjad Rezaei; Investigation, resources: all author; Data curation, writing – original draft preparation: Elham Jahanbin; Writing – review & editing, visualization, supervision: Sajjad Rezaei; Project administration, and funding acquisition: Elham Jahanbin.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
Hereby the authors express their gratitude towards the students at University of Guilan - Rasht and the applicants of yoga exercises in Mehr Clinic (in the north of Iran) for their participation in this research.
References
- Crane B, Kabat-Zinn J. Full catastrophe living; using the wisdom of your body and mind to face stress, pain and illness. Spiritual Health Int. 2006; 3(2):52. [DOI:10.1002/shi.88]
- Segal ZV, Williams MG, Williams M, Teasdale JD. Mindfulness-based cognitive therapy for depression, second edition. New York: Guilford Publications; 2012. https://www.google.com/books/edition/Mindfulness_Based_Cognitive_Therapy_for/1_NcsDZ17icC?hl=en&gbpv=0
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: A proposed operational definition. Clin Psychol Sci Pract. 2004; 11(3):230-41. [DOI:10.1093/clipsy.bph077]
- Azadmarzabadi E. [The effectiveness of mindfulness training on psychological symptoms in veterans with post-traumatic stress disorder (Persian)]. Int J Behav Sci. 2013; 7(1):67-74. http://www.behavsci.ir/article_67813.html
- Framson C, Kristal AR, Schenk JM, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009; 109(8):1439-44. [DOI:10.1016/j.jada.2009.05.006] [PMID] [PMCID]
- Bostock S, Crosswell AD, Prather AA, Steptoe A. Mindfulness on-the-go: Effects of a mindfulness meditation app on work stress and well-being. J Occup Health Psychol. 2019; 24(1):127-38. [DOI:10.1037/ocp0000118] [PMID] [PMCID]
- Pagnini F, Bercovitz KE, Phillips D. Langerian mindfulness, quality of life and psychological symptoms in a sample of Italian students. Health Qual Life Outcomes. 2018; 16(1):29. [DOI:10.1186/s12955-018-0856-4] [PMID] [PMCID]
- DeBolt LS, McCubbin JA. The effects of home-based resistance exercise on balance, power, and mobility in adults with multiple sclerosis. Arch Phys Med Rehabil. 2004; 85(2):290-7. [DOI:10.1016/j.apmr.2003.06.003] [PMID]
- Alahari U. Supporting Socio-emotional competence and psychological well-being of school psychologists through mindfulness practice. Contemp Sch Psychol. 2017; 21(4):369-79. [DOI:10.1007/s40688-017-0154-x]
- LaCaille L. Eating behavior. In: Gellman MD, Turner JR, editors. Encyclopedia of behavioral medicine. New York: Springer; 2013. https://link.springer.com/referenceworkentry/10.1007/978-1-4419-1005-9_1613#howtocite
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? Int J Eat Disord. 2014; 47(3):310-4. [DOI:10.1002/eat.22189] [PMID] [PMCID]
- Beshara M, Hutchinson AD, Wilson C. Does mindfulness matter? Everyday mindfulness, mindful eating and self-reported serving size of energy dense foods among a sample of South Australian adults. Appetite. 2013; 67:25-9. [DOI:10.1016/j.appet.2013.03.012] [PMID]
- Jordan CH, Wang W, Donatoni L, Meier BP. Mindful eating: Trait and state mindfulness predict healthier eating behavior. Pers Individ Dif. 2014; 68:107-11. [DOI:10.1016/j.paid.2014.04.013]
- Miller RL, Lucas-Thompson RG, Sanchez N, Smith AD, Annameier SK, Casamassima M, et al. Effects of a mindfulness-induction on subjective and physiological stress response in adolescents at-risk for adult obesity. Eat Behav. 2021; 40:101467. [DOI:10.1016/j.eatbeh.2020.101467] [PMID] [PMCID]
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract. 2017; 11(5 Suppl 1):90-111. [DOI:10.1016/j.orcp.2016.09.002] [PMID]
- Atkinson MJ, Wade TD. Does mindfulness have potential in eating disorders prevention? A preliminary controlled trial with young adult women. Early Interv Psychiatry. 2016; 10(3):234-45. [DOI:10.1111/eip.12160] [PMID]
- Durukan A, Gül A. Mindful eating: Differences of generations and relationship of mindful eating with BMI. Int J Gastron Food Sci. 2019; 18:100172. [DOI:10.1016/j.ijgfs.2019.100172]
- van Strien T, Donker MH, Ouwens MA. Is desire to eat in response to positive emotions an “obese” eating style: Is Kummerspeck for some people a misnomer? Appetite. 2016; 100:225-35. [DOI:10.1016/j.appet.2016.02.035] [PMID]
- Heatherton TF, Herman CP, Polivy J. Effects of physical threat and ego threat on eating behavior. J Pers Soc Psychol. 1991; 60(1):138-43. [DOI:10.1037/0022-3514.60.1.138] [PMID]
- van Strien T, Ouwens MA. Counterregulation in female obese emotional eaters: Schachter, Goldman, and Gordon’s (1968) test of psychosomatic theory revisited. Eat Behav. 2003; 3(4):329-340. [DOI:10.1016/S1471-0153(02)00092-2]
- Schachter S, Goldman R, Gordon A. Effects of fear, food deprivation, and obesity on eating. J Pers Soc Psychol. 1968; 10(2):91-7. [DOI:10.1037/h0026284] [PMID]
- Stroebe W, van Koningsbruggen GM, Papies EK, Aarts H. Why most dieters fail but some succeed: A goal conflict model of eating behavior. Psychol Rev. 2013; 120(1):110-38. [DOI:10.1037/a0030849] [PMID]
- Schaumberg K, Anderson DA, Anderson LM, Reilly EE, Gorrell S. Dietary restraint: What’s the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clin Obes. 2016; 6(2):89-100. [DOI:10.1111/cob.12134] [PMID]
- Winkens LHH, van Strien T, Brouwer IA, Penninx BWJH, Visser M. Mindful eating and change in depressive symptoms: Mediation by psychological eating styles. Appetite. 2019; 133:204-11. [DOI:10.1016/j.appet.2018.11.009]
- Wolever RQ, Best JL. Mindfulness-based approaches to eating disorders. In: Didonna F, editor. Clinical handbook of mindfulness. New York: Springer; 2009. [DOI:10.1007/978-0-387-09593-6_15]
- Levesque C, Brown KW. Mindfulness as a moderator of the effect of implicit motivational self-concept on day-to-day behavioral motivation. Motiv Emot. 2007; 31(4):284-99. [DOI:10.1007/s11031-007-9075-8]
- Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003; 84(4):822-48. [DOI:10.1037/0022-3514.84.4.822]
- Hirschmann JR, Zaphiropoulos L. Kids, carrots, and candy: A practical, positive approach to raising children free of food and weight problems. California: Createspace Independent Pub; 2012. https://www.google.com/books/edition/Kids_Carrots_and_Candy/bUfdMgEACAAJ?hl=en
- Pintado-Cucarella S, Rodríguez-Salgado P. Mindful eating and its relationship with body mass index, binge eating, anxiety and negative affect. J Behav Health Soc Issues. 2016; 8(2):19-24. [DOI:10.1016/j.jbhsi.2016.11.003]
- Tian H, Xie H, Song G, Zhang H, Hu G. Prevalence of overweight and obesity among 2. 6 million rural Chinese adults. Prev Med. 2009; 48(1):59-63. [DOI:10.1016/j.ypmed.2008.10.020] [PMID]
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: The Kentucky inventory of mindfulness skills. Assessment. 2004; 11(3):191-206. [DOI:10.1177/1073191104268029] [PMID]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006; 13(1):27-45. [DOI:10.1177/1073191105283504] [PMID]
- Carlson LE, Brown KW. Validation of the Mindful Attention Awareness Scale in a cancer population. J Psychosom Res. 2005; 58(1):29-33. [DOI:10.1016/j.jpsychores.2004.04.366] [PMID]
- Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, Carlson L, et al. The Toronto Mindfulness Scale: Development and validation. J Clin Psychol. 2006; 62(12):1445-67. [DOI:10.1002/jclp.20326] [PMID]
- Apolzan JW, Myers CA, Cowley AD, Brady H, Hsia DS, Stewart TM, et al. Examination of the reliability and validity of the Mindful Eating Questionnaire in pregnant women. Appetite. 2016; 100:142-51. [DOI:10.1016/j.appet.2016.02.025] [PMID] [PMCID]
- Abbaspoor Z, Javadifar N, Miryan M, Abedi P. Psychometric properties of the Iranian version of mindful eating questionnaire in women who seeking weight reduction. J Eat Disord. 2018; 6:33. [DOI:10.1186/s40337-018-0220-4] [PMID] [PMCID]
- Abdul Basir SM, Abdul Manaf Z, Ahmad M, Abdul Kadir NB, Ismail WNK, Mat Ludin AF, et al. Reliability and validity of the Malay Mindful Eating Questionnaire (MEQ-M) among overweight and obese adults. Int J Environ Res Public Health. 2021, 18(3), 1021. [DOI:10.3390/ijerph18031021] [PMID] [PMCID]
- Daubenmier JJ. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q. 2005; 29(2):207-19. [DOI:10.1111/j.1471-6402.2005.00183.x]
- Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005; 11(4):28-33. [PMID]
- McIver S, O’Halloran P, McGartland M. Yoga as a treatment for binge eating disorder: A preliminary study. Complement Ther Med. 2009; 17(4):196-202. [DOI:10.1016/j.ctim.2009.05.002] [PMID]
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and Cultural Adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and Cultural Adaptation. Value Health. 2005; 8(2):94-104. [DOI:10.1111/j.1524-4733.2005.04054.x] [PMID]
- Lemeshow S, Lwanga SK, Hosmer DW, Klar J. Adequacy of sample size in health studies. New York: Wiley; 1990. https://www.google.com/books/edition/Adequacy_of_Sample_Size_in_Health_Studie/gUBjQgAACAAJ?hl=en
- Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S. Measuring mindfulness-the Freiburg mindfulness inventory (FMI). Pers Individ Dif. 2006; 40(8):1543-55. [DOI:10.1016/j.paid.2005.11.025]
- Ghasemi Jobaneh R, Arabzadeh M, Jalili Nikoo S, Alipour Z, Mohsenzadeh F. [Survey the validity and reliability of the Persian version of short form of freiburg mindfulness inventory (Persian)]. J Rafsanjan Univ Med Sci. 2015; 14(2):137-50. http://journal.rums.ac.ir/article-1-2293-fa.html
- Moreira-Silva I, Santos R, Abreu S, Mota J. Associations between body mass index and musculoskeletal pain and related symptoms in different body regions among workers. Sage Open. 2013; 3(2):1-6. [DOI:10.1177/2158244013491952]
- Yagnik PJ, McCormick DP, Ahmad N, Schecter AJ, Harris TR. Childhood and adolescent obesity and depression: A systematic literature review. Int Arch Integr Med. 2014; 1(2):23-33. http://iaimjournal.com/wp-content/uploads/2014/10/4-childhood-and-adolescent-obesity-and-depression.pdf
- Meyers LS, Gamst G, Guarino AJ. Applied multivariate research: Design and interpretation. New York: SAGE Publications; 2016. https://www.google.com/books/edition/Applied_Multivariate_Research/bm51DQAAQBAJ?hl=en
- Garson GD. Structural equation modeling from statnotes: Topics in multivariate analysis IInternet]. 2009 [Updated 2014 October 5th]. Avalble from: https://faculty.chass.ncsu.edu/garson/pa765/statnote.htm
- Kline RB. Data preparation and psychometrics review. In: Kline RB. Principles and practice of structural equation modeling. Fourth edition. New York: Guilford; 2015. https://www.google.com/books/edition/Principles_and_Practice_of_Structural_Eq/Q61ECgAAQBAJ?hl=en&gbpv=0
- Gatignon H. Statistical analysis of management data. New York: Springer; 2010. [DOI:10.1007/978-1-4419-1270-1]
- Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981; 18(1):39-50. [DOI:10.2307/3151312]
- Hair J, Anderson R, Black B, Babin B. Multivariate data analysis. London: Pearson Education; 2016. https://www.google.com/books/edition/Multivariate_Data_Analysis/LKOSAgAAQBAJ?hl=en
- Javali SB, Gudaganavar NV, Raj SM. Effect of varying sample size in estimation of coefficients of internal consistency. WebmedCentral Biostatistics. 2011; 2(2):WMC001572. http://www.webmedcentral.com/article_view/1572
- Cox T, Ferguson E. Measurement of the subjective work environment. Work Stress. 1994; 8(2):98-109. [DOI:10.1080/02678379408259983]
- Esposito Vinzi V, Chin WW, Henseler J, Wang H. Handbook of partial least squares: Concepts, methods and applications. In: Gentle JE, Härdle WK, Mori Y. Handbooks of computational statistics. Berlin: Springer; 2010. [DOI:10.1007/978-3-540-32827-8]
- Chehabi HE. The westernization of Iranian culinary culture. Iran Stud. 2003; 36(1):43-61. [DOI:10.1080/021086032000062875]
- Askari Majabadi H, Solhi M, Montazeri A, Shojaeizadeh D, Nejat S, Khalajabadi Farahani F, et al. Factors influencing fast-food consumption among adolescents in Tehran: A qualitative study. Iran Red Crescent Med J. 2016; 18(3):e23890. [PMID] [PMCID]
- Ost LG. Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behav Res Ther. 2008; 46(3):296-321. [DOI:10.1016/j.brat.2007.12.005] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2022/04/6 | Accepted: 2022/04/21 | Published: 2022/04/21
Received: 2022/04/6 | Accepted: 2022/04/21 | Published: 2022/04/21
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |