BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://cjns.gums.ac.ir/article-1-363-en.html
Introduction
Cognitive impairment is a common symptom in Schizophrenia (SZ) [1]. Bipolar Disorder (BD) has also been associated with problems in some cognitive domains [2]. Although these deficits are more severe in patients with SZ, there is a significant overlap between the two diseases in cognitive problems [1]. Cognition is an essential part and an important determinant of quality of life in patients with SZ and BD that affects not only the individual but also the family, community, and health system. There has been a great deal of research on cognition in SZ in the last 4 decades. The results have shown that cognitive impairment might lead to daily dysfunction in patients with this disorder even may be greater than the severity of other symptoms [3]. This impairment in people with SZ is moderate to severe, compared to healthy individuals [4, 5], and it is even seen in the early stages of SZ and is independent of the symptoms and side effects of medications [6, 7].
The subtypes of cognitive impairment that are involved in SZ include processing speed, attention, working memory, verbal and visual learning, executive functioning, verbal comprehension, and social cognition [7-10]. Various studies have emphasized memory impairment in patients with SZ. Severe levels of cognitive impairment might be observed in patients with SZ, such as memory impairment, and the function of the dorsolateral prefrontal cortex plays an important role in the performance of several cognitive domains [11, 12].
Evidence has also shown that patients with BD have persistent cognitive impairment [13], and this impairment and functional limitations are observed in half of the bipolar patients even in the absence of psychotic and mood symptoms [14]. Numerous studies have shown that patients with BD have difficulty with executive function, verbal memory, psychomotor, and continuity of attention [2, 15-17]. These impairments with different severity might be seen during periods of normal mood [18], although the severity is more remarkable in the acute phase of the disease [19].
The results of a recent meta-analysis on BP patients during normal mood and on healthy individuals showed that bipolar patients had moderate to severe impairment in verbal memory, working memory, visual learning, and visual memory, while their hypervigilance, reasoning ability, problem-solving, and processing speed were not significantly different [20]. In another study, the cognitive function of bipolar patients during the normal mood period was weaker than that in normal individuals. The results of this study showed that cognitive impairment could persist even after the acute phase of the disease [21]. Also, according to the results of other studies, cognitive impairment during the manic period of bipolar disorder is worse than in the period of depressive illness [22, 23].
In various studies, different findings are reported about variances in cognitive impairment between BD patients with and without a history of psychotic symptoms. Some studies have reported poorer cognitive function in patients with BD with psychotic symptoms compared to the patients without psychiatric symptoms, while others have shown no such difference or just a moderate difference [24]. For example, in a cross-sectional study by Bowie et al. among patients with SZ, BD with psychosis, and without psychosis, patients with SZ and BD with psychosis had poorer cognitive function compared to the group of bipolar patients without psychosis [14], while in another study by Achalia et al., there was no significant difference between bipolar patients with and without psychosis [24]. According to the contradictory results of previous studies, we performed the present study to compare the memory impairment of three groups of patients with each other and with the severity of psychiatric symptoms.
Materials and Methods
This analytical cross-sectional study was performed on 42 outpatients included three groups (14 patients with SZ, 14 bipolar patients with psychosis, and 14 bipolar patients without psychosis) referred to Shafa Hospital in Rasht, Iran, in 2018-2019. Assuming the alpha error of 0.05 and the power of 0.20, we calculated a sample size of 42 patients with G power software based on the Barch and Sheffield study [3].
The study was approved by the Ethics Committee at the Research Center of Guilan University of Medical Sciences (Ethics Code: IR.GUMS.REC.1397.497). In this study, the patients in the three groups were diagnosed based on DSM-V criteria and clinical interviews. The inclusion criteria included at least literate and being mentally and behaviorally stable and without alcohol and substance abuse. We excluded the patients with severe medical and mental disorders that could not complete questionnaires. All participants completed a demographic information questionnaire, a Brief Psychiatric Rating Scale (BPRS), and Wechsler’s Memory Scale (WMS) for adults. After fully explaining the objectives of the study, all patients gave written informed consent to participate in the study. Then, questionnaires were used to collect research data.
Study tools
Demographic Information Questionnaire
We used a demographic questionnaire to gather data, such as age, gender, educational level, and place of residence, occupation, type of psychiatric disorder, number of hospitalizations, duration of psychiatric disorder, and history of medical illnesses and other drug use.
Wechsler’s Memory Scale (WMS)
WMS was created by Wechsler in 1945 and is the result of 10 years of research to build a simple, immediate, and practical tool for assessing memory [25]. The scale consists of 7 subscales; personal and current information (score 0-6), orientation to time and place (score 0-5), mental control (score 0-9), logical memory (score 0-21), memory span/digits span (score 0-8), visual memory (score 0-14), and associative learning (score 0-21). For this scale, the corrected score is estimated of total subscales’ scores by adding the fixed score of different age groups. Finally, the memory score is determined based on the corrected score. In the study of Ryan et al., the Cronbach alpha reliability coefficient of this scale was 0.75 for normal individuals and 0.89 for patients with psychiatric disorders [26]. In Iran, standardization of this scale was performed and reliability was estimated 0.85 by calculating the Cronbach alpha coefficient [27].
Brief Psychiatric Rating Scale (BPRS)
BPRS is an 18-item questionnaire that was developed in 1962 by Overall and Gorham. It is an easy and comprehensive test in assessing the symptoms of illness and mental health problems [28]. This scale has been used in most studies that have examined the symptoms of psychopathology, and especially in research on SZ and its symptoms, and its validity and reliability have been proven in various studies [29]. It is scored on the Likert-type scale from 1 (not present) to 7 (very severe) and the total score is between 18 and 126. A higher score on this scale indicates the severity of the disease. For the total scale, reliability by intra-class correlation and validity were reported as R=0.78 (P<0.001), and R=0.66 (P<0.01), respectively [30]. For the Iranian version of this scale, the agreement coefficient and the Cronbach alpha reliability coefficient was reported as R=0.72 and R=0.8, respectively [31].
Statistical analysis
We presented frequencies for demographic variables and Mean±SD for continuous variables. The one-way analysis of variance (ANOVA) was used to compare mean scores and Tukey’s test for post hoc analysis. All data were analyzed by SPSS v. 21. A P-value of less than 0.05 is considered statistically significant.
Results
In this study, 42 patients participated in 3 groups of 14 patients each (14 patients with SZ, 14 ones with BD with psychosis, and 14 ones with BD without psychosis). Table 1 presents the demographic characteristics of patients into three groups of patients with SZ, BD with psychosis, and BD without psychosis.
.png)
The Mean±SD ages of SZ, BD with psychosis, and BD without psychosis groups were 39.07 (9.82), 43.57 (8.80), and 46.57 (13.19) years, respectively. Also, the Mean±SD numbers of hospitalizations were 3.00 (5.08), 4.36 (4.16), and 1.50 (1.40) for three groups, respectively, and the Mean±SD duration of a psychiatric disorder for three groups was 14.86 (10.85), 13.71 (10.73), and 11.07 (7.48) years, respectively.
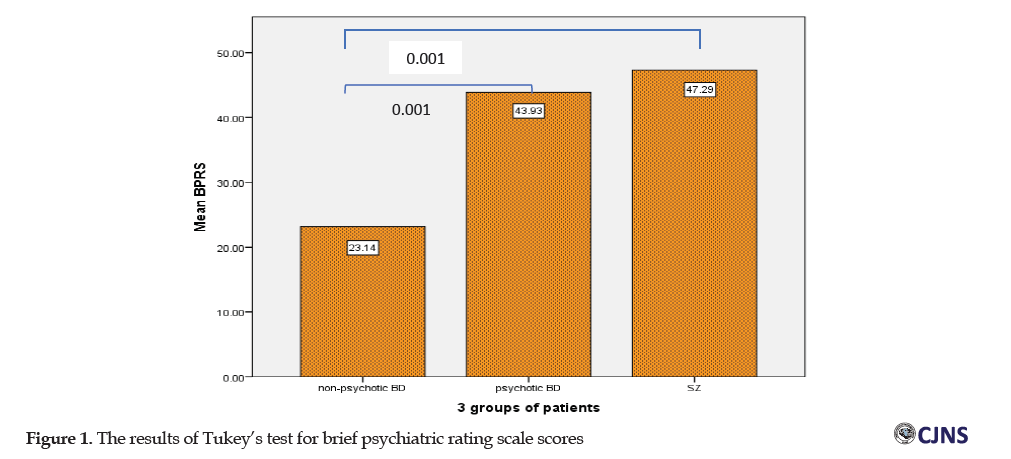
The Mean±SD BPRS total scores in three groups of SZ, BD with psychosis, and BD without psychosis were 47.28 (14.83), 43.93 (11.07), 23.14 (4.09), respectively, and there was a statistically significant difference between the three groups of patients (F=19.19, P=0.001).
According to the results of Tukey’s test (post hoc analysis) in Figure 1, there was no statistically significant difference between BPRS scores of patients with SZ and BD with psychosis, while the difference between scores of patients with SZ and BD without psychosis (24.14) (P=0.001), and between the two groups of patients with BD (20.78) were statistically significant (P=0.001).
The results of ANOVA showed that the Mean±SD of the WMS sores in three groups of SZ, BD with psychosis, and BD without psychosis patients were 62.07 (10.75), 76.57 (12.62), 73.5 (13.31), respectively. Based on the results, there was a statistically significant difference between the mean of the WMS scores in the three groups of patients (F=5.42, P=0.008).
Based on the results of Tukey’s test in Figure 2, the difference between WMS scores of patients with SZ and BD with psychosis (-14.5) and the scores of patients with SZ and BD without psychosis (-11.42) were statistically significant (P=0.009, P=0.047, respectively), but the difference between patients with BD with psychosis and BD without psychosis [3] was not significant.
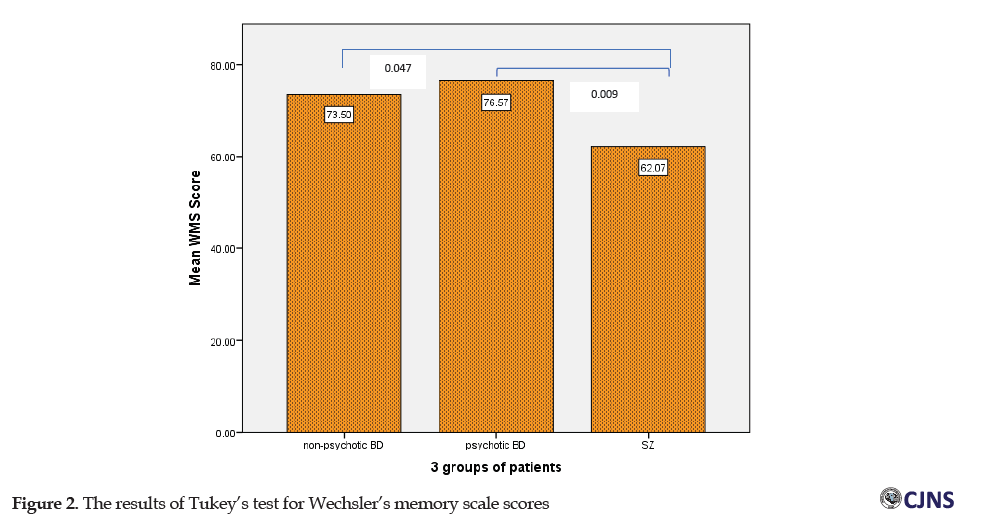
Table 2 presents the subscales’ scores of WMS. In the subscale of orientation, the score of people with BD without psychosis was significantly higher than those in the BD with psychosis groups and SZ (P=0.002).
.png)
According to the results of the Pearson correlation coefficient, there was a negative correlation between the scores of WMS and the scores of BPRS in the groups of patients with SZ (r=0.668, P=0.009) and patients with BD without psychosis (r=0.753, P=0.002), while no significant correlation was observed between the WMS and BPRS scores in patients with BD with psychosis (r=0.423, P=0.132).
Discussion
The results of the present study showed significant differences between the mean BPRS total scores of patients with SZ and BD without psychosis and between BD patients with psychosis and BD without psychosis. SZ patients obtained higher scores than BD with psychosis and BD without psychosis, respectively. In the study of Zhu et al. on 716 participants, the BPRS scores of 216 patients with SZ were also significantly higher than the scores of patients with mood disorders [32]. Thus, the presence of psychosis has a significant relationship with the BPRS scores, being more remarkable in patients with SZ. Comparison between memory scores of the three groups of patients showed that the scores of patients with SZ were lower than bipolar patients with psychosis and BD without psychosis, which was statistically significant (P=0.008).
The present findings were consistent with the results of several studies [14, 15, 33-35]. According to the finding of the study of Mazinani et al., the mean total scores of MMSE (The Mini-Mental State Examination) in patients with SZ was lower than BD type I and, in most questions, SZ patients obtained lower scores than bipolar patients [35]. Also, in another study by Simonsen et al. [36], the cognitive performance of psychotic individuals was reported to be lower compared to non-psychotic individuals. In another research by Achalia et al., the cognitive function of healthy and bipolar individuals was significantly different, but there was no difference between BD patients with and without psychosis [24]. However, in subscales of memory, our findings were a little different. According to the results, SZ patients obtained lower scores than BD patients with psychosis and BD without psychosis in all subscales of memory (personal information, orientation, mental control, logical memory, number repetition, visual memory, learning associations), but this difference was only remarkable in the orientation subscale (P=0.002). These inconsistent findings could be attributed to differences in illness duration or stage.
Comparing the correlation between BPRS and memory scores among individuals in each group, a negative correlation is observed between patients with SZ and BD without psychosis, meaning that the more severe psychotic symptoms in SZ are associated with poorer memory and bipolar patients without psychosis with weaker symptoms of psychopathology experienced considerably less memory impairment. Thus, it seems that the psychotic features of SZ and increasing symptoms of disorders are associated with weaker memory. These findings were compatible with the results of Zhu et al. [32] and Lewandowski [37] that certain domains of psychopathology were positively correlated with cognitive impairment.
Because cognitive processes play the most important role in the social relationships and lives of people with SZ and BD and even have a significant impact on morbidity and mortality, trying to prevent cognitive deficits can have a dramatic impact on the lives of these people and reduce hospitalization cases and consequently reduce the costs of the health system. One of the limitations of this study was the lack of consideration of patients’ initial IQ for accurate assessment of memory. Moreover, another limitation was the wide age range of patients in the study. It is suggested that future studies be undertaken with a larger sample size with a control group and longitudinal studies for more accurate results. It is also suggested that non-drug therapies, such as cognitive-behavioral therapy and psychosocial rehabilitation be performed in these patients, and memory scores and cognition before and after these interventions be compared to evaluate the effect of such therapies on patients. Then, if these methods had been effective, they would be used to help rehabilitation and better life and reduce individual and social pressure on these patients, their families, community, and health care system.
Conclusion
The results of the present study showed that SZ patients obtained higher mean BPRS scores than BD with psychosis and BD without psychosis, respectively. Memory scores of patients with SZ were lower than bipolar patients with psychosis and BD without psychosis. Also, SZ patients obtained lower scores than bipolar patients with psychosis and BD without psychosis in all subscales of memory (personal information, orientation, mental control, logical memory, number repetition, visual memory, learning associations), but this difference was only remarkable in the orientation subscale. Furthermore, a negative correlation between BPRS and memory scores observed in patients with SZ and BD without psychosis, but no in BD with the psychosis group.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Research Ethics Committee of the GUMS (IR.GUMS.REC.1397.497) The subjects signed a written informed consent. All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki, 2013.
Funding
This article is extracted from a dissertation with registration (Code: 2170). The researchers did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and investigation: All authors; Methodology: Robabeh Soleimani, Fatemeh Eslamdoust-Siahestalkhi; Data collection: Mohammadreza Akhzari; Data analysis: Fatemeh Eslamdoust-Siahestalkhi; Writing - original draft, Writing – review & editing: Robabeh Soleimani, Fatemeh Eslamdoust-Siahestalkhi; Supervision: Robabeh Soleimani.
Conflict of interest
The authors declared no conflicts of interest.
Acknowledgements
The authors would like to express their sincere thanks to Dr. Ali Imani (psychiatrist) and the volunteers participated in this research.
References
1.Bora E, Pantelis C. Social cognition in schizophrenia in comparison to bipolar disorder: A meta-analysis. Schizophr Res. 2016; 175(1-3):72-8. [DOI:10.1016/j.schres.2016.04.018] [PMID]
2.Bora E, Yucel M, Pantelis C. Cognitive endophenotypes of bipolar disorder: A meta-analysis of neuropsychological deficits in euthymic patients and their first-degree relatives. J Affect Disord. 2009; 113(1-2):1-20. [DOI:10.1016/j.jad.2008.06.009] [PMID]
3.Barch DM, Sheffield JM. Cognitive impairments in psychotic disorders: Common mechanisms and measurement. World Psychiatry. 2014; 13(3):224-32. [DOI:10.1002/wps.20145] [PMID] [PMCID]
4.Fioravanti M, Bianchi V, Cinti ME. Cognitive deficits in schizophrenia: an updated metanalysis of the scientific evidence. BMC Psychiatry. 2012; 12(1):64. [DOI:10.1186/1471-244X-12-64] [PMID] [PMCID]
5.Moritz S, Klein J, Desler T, Lill H, Gallinat J, Schneider BC. Neurocognitive deficits in schizophrenia. Are we making mountains out of molehills? Psychol Med. 2017; 47(15):2602-12. [DOI:10.1017/S0033291717000939] [PMID]
6.Joyce E, Huddy V. Defining the cognitive impairment in schizophrenia. Psychol Med. 2004; 34(7):1151-5. [DOI:10.1017/S0033291704003472] [PMID]
7.Tripathi A, Kar SK, Shukla R. Cognitive deficits in schizophrenia: Understanding the biological correlates and remediation strategies. Clin Psychopharmacol Neurosci. 2018; 16(1):7-17. [DOI:10.9758/cpn.2018.16.1.7] [PMID] [PMCID]
8.Dickinson D, Iannone VN, Wilk CM, et al. General and specific cognitive deficits in schizophrenia. Biol Psychiatry. 2004; 55(8):826-33. [DOI:10.1016/j.biopsych.2003.12.010] [PMID]
9.Gold JM, Hahn B, Strauss GP, et al. Turning it upside down: Areas of preserved cognitive function in schizophrenia. Neuropsychol Rev. 2009; 19(3):294-311. [DOI:10.1007/s11065-009-9098-x] [PMID] [PMCID]
10.Kraus MS, Keefe RS. Cognition as an outcome measure in schizophrenia. Br J Psychiatry Suppl. 2007; 191(S50):s46-51. [DOI:10.1192/bjp.191.50.s46] [PMID]
11.Guo JY, Ragland JD, Carter CS. Memory and cognition in schizophrenia. Mol Psychiatry. 2019; 24(5):633-42. [DOI:10.1038/s41380-018-0231-1] [PMID] [PMCID]
12.Kraguljac NV, Srivastava A, Lahti AC. Memory deficits in schizophrenia: A selective review of Functional Magnetic Resonance Imaging (FMRI) studies. Behav Sci (Basel). 2013; 3(3):330-47. [DOI:10.3390/bs3030330] [PMID] [PMCID]
13.Demant KM, Almer GM, Vinberg M, Kessing LV, Miskowiak KW. Effects of cognitive remediation on cognitive dysfunction in partially or fully remitted patients with bipolar disorder: Study protocol for a randomized controlled trial. Trials. 2013; 14:378. [DOI:10.1186/1745-6215-14-378] [PMID] [PMCID]
14.Bowie CR, Best MW, Depp C, Mausbach BT, Patterson TL, Pulver AE, et al. Cognitive and functional deficits in bipolar disorder and schizophrenia as a function of the presence and history of psychosis. Bipolar Disord. 2018; 20(7):604-13. [DOI:10.1111/bdi.12654] [PMID]
15.Bora E, Pantelis C. Meta-analysis of cognitive impairment in first-episode bipolar disorder: Comparison with first-episode schizophrenia and healthy controls. Schizophr Bull. 2015; 41(5):1095-104. [DOI:10.1093/schbul/sbu198] [PMID] [PMCID]
16.Bora E, Yücel M, Pantelis C. Neurocognitive markers of psychosis in bipolar disorder: A meta-analytic study. J Affect Disord. 2010; 127(1-3):1-9. [DOI:10.1016/j.jad.2010.02.117] [PMID]
17.Quraishi S, Frangou S. Neuropsychology of bipolar disorder: A review. J Affect Disord. 2002; 72(3):209-26. [DOI:10.1016/S0165-0327(02)00091-5] [PMID]
18.Kurtz MM, Gerraty RT. A meta-analytic investigation of neurocognitive deficits in bipolar illness: Profile and effects of clinical state. Neuropsychology. 2009; 23(5):551-62. [DOI:10.1037/a0016277] [PMID] [PMCID]
19.Bortolato B, Miskowiak KW, Köhler CA, Vieta E, Carvalho AF. Cognitive dysfunction in bipolar disorder and schizophrenia: A systematic review of meta-analyses. Neuropsychiatr Dis Treat. 2015; 11:3111-25. [DOI:10.2147/NDT.S76700] [PMID] [PMCID]
20.Elias LR, Miskowiak KW, Vale AM, Köhler CA, Kjærstad HL, Stubbs B, et al. Cognitive impairment in euthymic pediatric bipolar disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017; 56(4):286-96. [DOI:10.1016/j.jaac.2017.01.008] [PMID]
21.Palazzo MC, Arici C, Cremaschi L, Cristoffanini M, Dobrea C, Dell'Osso B, et al. Cognitive performance in euthymic patients with bipolar disorder vs healthy controls: A neuropsychological investigation. Clin Pract Epidemiol Ment Health. 2017; 13:71-81. [DOI:10.2174/1745017901713010071] [PMID] [PMCID]
22.Sanches M, Bauer IE, Galvez JF, Zunta-Soares GB, Soares JC. The management of cognitive impairment in bipolar disorder: Current status and perspectives. Am J Ther. 2015; 22(6):477-86. [DOI:10.1097/MJT.0000000000000120] [PMID] [PMCID]
23.Vrabie M, Marinescu V, Talaşman A, Tăutu O, Drima E, Micluţia I. Cognitive impairment in manic bipolar patients: important, understated, significant aspects. Ann Gen Psychiatry. 2015; 14(1):41. [DOI:10.1186/s12991-015-0080-0] [PMID] [PMCID]
24.Achalia RM, Nagendra B, Achalia G, Chopade M, Sable A, Venkatasubramanian G, et al. Effect of psychotic symptoms on cognitive impairment in patients with bipolar disorder. Ind Psychiatry J. 2019; 28(1):115-22. [DOI:10.4103/ipj.ipj_1_19] [PMID] [PMCID]
25.Wechsler D. A standardized memory scale for clinical use. J Psychol. 1945; 19(1):87-95. [DOI:10.1080/00223980.1945.9917223]
26.Ryan JJ, Morris J, Yaffa S, et al. Test‐retest reliability of the Wechsler Memory Scale, Form I. J Clin Psychol. 1981; 37(4):847-8. [DOI:10.1002/1097-4679(198110)37:43.0.CO; 2-K] [PMID]
27.Sarrami G. Standardization Wechsler Memory Scale on the population living in Tehran. Tarbiyat. 1993; 83:25-30. http://noo.rs/sbQZJ
28.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962; 10(3):799-812. [DOI:10.2466/pr0.1962.10.3.799]
29.Shafer A. Meta-analysis of the Brief Psychiatric Rating Scale factor structure. Psychol Assess. 2005; 17(3):324-35. [DOI:10.1037/1040-3590.17.3.324] [PMID]
30.Andersen J, Larsen JK, Kørner A, Nielsen BM, Schultz V, Behnke K, et al. The Brief Psychiatric Rating Scale: Schizophrenia, reliability and validity studies. Nord Psykiatr Tidsskr. 1986; 40(2):135-8. [DOI:10.3109/08039488609096456]
31.Fallahi Khoshknab M. [Effectiveness of psychiatric nursing home care services for psychiatric status in Schizophrenics (Persian)]. Iran Rehabilit J. 2007; 8(29):75-9. www.sid.ir/fa/journal/ViewPaper.aspx?id=65029
32.Zhu Y, Womer FY, Leng H, Chang M, Yin Z, Wei Y, et al. The relationship between cognitive dysfunction and symptom dimensions across Schizophrenia, Bipolar Disorder, and major depressive disorder. Front Psychiatry. 2019; 10:253. [DOI:10.3389/fpsyt.2019.00253] [PMID] [PMCID]
33.Bora E. Differences in cognitive impairment between schizophrenia and bipolar disorder: Considering the role of heterogeneity. Psychiatry Clin Neurosci. 2016; 70(10):424-33. [DOI:10.1111/pcn.12410] [PMID]
34.Fujino H, Sumiyoshi C, Yasuda Y, Yamamori H, Fujimoto M, Fukunaga M, et al. Estimated cognitive decline in patients with schizophrenia: A multicenter study. Psychiatry Clin Neurosci. 2017; 71(5):294-300. [DOI:10.1111/pcn.12474] [PMID]
35.Mazinani R, Haj Seyed Javadi A, Afshari R, Eslami L. [The cognitive state of hospitalized men with Schizophrenia and Bipolar I Disorder (Persian)]. Iran Psychiatry Clin Psychol. 2005; 11(3):298-303. www.sid.ir/en/journal/ViewPaper.aspx?ID=47953
36.Simonsen C, Sundet K, Vaskinn A, Birkenaes AB, Engh JA, Faerden A, et al. Neurocognitive dysfunction in bipolar and schizophrenia spectrum disorders depends on history of psychosis rather than diagnostic group. Schizophr Bull. 2011; 37(1):73-83. [DOI:10.1093/schbul/sbp034] [PMID] [PMCID]
37.Lewandowski KE, Cohen BM, Keshavan MS, Ongür D. Relationship of neurocognitive deficits to diagnosis and symptoms across affective and non-affective psychoses. Schizophr Res. 2011; 133(1-3):212-7. [DOI:10.1016/j.schres.2011.09.004] [PMID] [PMCID
Received: 2020/12/22 | Accepted: 2020/12/20 | Published: 2020/12/20
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






