BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://cjns.gums.ac.ir/article-1-329-en.html
2- Otorhinolaryngology Research Center, Department of Otolaryngology, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
3- School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Introduction
Allergic Rhinitis (AR) is a common chronic disease with a prevalence of 15%-20% in adults and more than 42% in children. In recent decades, an increase in AR prevalence has been observed worldwide [1]. Recent studies have evaluated various psychological aspects of AR subjects, including the burden of the disease on the patients’ function and more importantly, quality of life [2, 3]. Personality traits develop early in life, playing basic roles in the behavioral and emotional functions of people, which remain almost constant throughout life. It is believed that some of these traits are associated with psychological or physical dysfunctions as some studies in psychosomatic medicine have found relationships between type one allergies (with elevated IgE levels) and psychological distresses, particularly with negative effects, including neuroticism, depression, social anxiety, and phobias [4-6].
Rodinkova et al. evaluated the presence of psychological profiles of 86 subjects with seasonal allergy using the Minnesota Multiphasic Personality Inventory (MMPI). Men with clinically diagnosed pollinosis had rigidity, paranoia, and schizophrenia. Also, pollen-sensitive women revealed a complex psychotype with increased depression, hysteria, psychopathy, paranoia, psychasthenia, and hypomania. The researchers advised a combination of two treatment regimens (pharmacotherapy and psychotherapeutic) as the main approach to treat patients with seasonal allergies [7]. Harter showed a positive association between generalized anxiety and seasonal allergies. Also, there was a positive association between depression and perennial allergies, as well as a negative association between anxiety and perennial allergies. This study supported the relevance of psychosocial factors in association with allergies [8].
Despite the approved roles of psychological factors and introducing various personality patterns in allergic disorders, no particular personality pattern associated with these disorders has yet been identified [9-11]. The aim of the present study was to evaluate the frequency of different personality patterns among Iranian patients with AR.
Material and Methods
A total of 100 subjects (50 subjects with persistent AR for at least one year and 50 normal controls) participated in this case-control prospective study from March 2013 to March 2014. Inclusion criteria were the age of more than 18 years, a minimum educational level of high school, and no history of psychiatric disorders. Cases were considered to have AR with the Score for Allergic Rhinitis (SFAR) ≥7 and positive nasal smear for eosinophilia. The sensitivity and specificity rates of the SAFAR as a diagnostic tool are 94.8% and 95.1%, respectively [12]. Annesi-Maesano et al. showed that a score of ≥7 optimally differentiates AR cases from those without AR [13]. For doing a nasal smear for tissue eosinophilia, the patients should stop their medications, such as antihistamine and/or nasal corticosteroids for at least five days before taking the nasal smears. A positive smear for eosinophilia was considered when there were 5% eosinophils of total leukocytes. Nasal smear cytology is a useful diagnostic test with moderately high sensitivity and a high specificity [14]. The control group was selected randomly from age- and sex-matched subjects seeking medical management services at the otolaryngology clinic, Amiralmomenin Hospital, Rasht, Iran and had no history of sinus problems.
To evaluate the personality traits of the subjects, the Persian translation and Persian norm scores of the MMPI-2 was used [15, 16]. MMPI-2 consists of 567 true/false self-report items for gathering a wide range of self-described characteristics and scoring them. MMPI test is the best known and widely used personality questionnaire that has been developed as an objective tool for the diagnosis of mental diseases. The MMPI-2 is generally used to screen abnormal people and particularly, determine the severity of the problems. This test has three validity scales and ten clinical scales. Validity scales provide information regarding the subject’s approach to the test and include Lie detection (L) scale, Infrequency (F), and Defensiveness (K) as a correction or inhibition scale. The L scale measures the tendency to present oneself in a favorable light. The K score is an indicator of more subtle attempts to deny psychopathology. The F score is an indicator of emotional distress and atypical experiences. It may reflect high levels of emotional distress and inadequate ego control [17].
The clinical scales of the MMPI-2 include Hypochondriasis (Hs), Depression (D), Hysteria (Hy), Psychopathic deviate (Pd), Masculinity/femininity (Mf), Paranoia (Pa), Psychasthenia (Pt), Schizophrenia (Sc), Hypomania (Ma), and Social introversion (Si). Raw scores were coded into T-score, based on a normative sample of the Iranian population. Higher scores indicate less functioning. A T score of 65 or higher is interpreted as a score in the clinical range [15]. For MMPI profile interpretation, the MMPI profile was classified into the high-point codes, which were bases on the elevations of the highest one, two, or three clinical scales. Dehghani et al. showed satisfactory reliability and validity of the MMPI-2 in the Iranian population. This study disclosed the validity of 0.49-0.89 for the MMPI subscales. Also, the readability score of subscales was 0.42-0.76 [18].
The study protocol was approved by the Ethical Committee of Guilan University of Medical Sciences, Iran, and complied with the principles outlined in the Helsinki Declaration. All subjects signed informed consent forms prior to participation in the study.
Statistical analysis
Assuming the alpha error of 0.05 and the power of 0.90, we calculated the total sample size of 70 subjects based on the Gauci et al. [19] study. Regarding the possibility of incomplete questionnaires, the number of samples in each group was increased to 50 cases. We presented frequencies for categorical variables and means and standard deviation for continuous variables. We also applied the independent t-test to compare the mean scores of the psychiatric features between the allergic and control groups. One-way Multivariate Analysis of Covariance (MANCOVA) test was used to compare the mean T-scores for 13 MMPI-2 scales (3 validity and 10 clinical scales) for 50 AR and 50 normal cases with valid profiles. This tested the main effect of the group using all MMPI-2 scales as outcome measures after adjusting for the potential confounder (sex). We used the Bonferroni’s correction to protect against type I error. All data were analyzed using SPSS V. 19. (IBM, SPSS, Inc., Chicago, IL, USA). Statistical significance was set at P<0.05.
Results
Of the 50 AR subjects analyzed, 20 cases were male and 30 cases were female. The age range of patients was 19 to 49 years, with a Mean±SD age of 29.1±8.6 years. The duration of symptoms ranged 1-9 years, with a mean duration of 3.2 years. In the control group, there were 22 males and 28 females with the Mean±SD age of 28.1±7.8 years.
Validity scale patterns showed no significant difference between the two groups. The validity profiles of about one-fourth of the AR subjects were characterized by increases in defensiveness, which was two times more than this profile in normal controls (Figure 1).
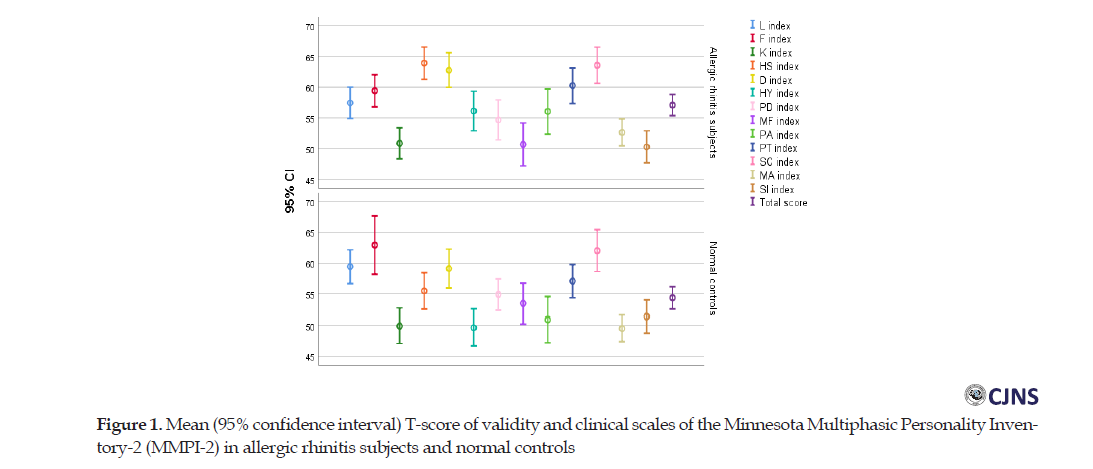
Before running MANCOVA, we checked homogeneity of the variances between the groups for each dependent variable. In addition, we calculated the regression slope of the dependent variables covariate for each group (clinical scales). None of the comparisons were statistically significant (P>0.05), which indicates that the statistical assumptions were not violated. Therefore, MANCOVA was carried out. The results of MANCOVA showed no significant difference between the two groups in the validity scales of the MMPI-2 test (F(3,96)=1.10, P=0.29). Then, validity scales showed no significant difference in over- or under-reporting symptoms.
The validity scale patterns were checked to determine whether the decreased L scale scores and the increased K scale scores were truly reflective of the changes in self-presentation style. The three validity scales were clustered into three specific categories: positive self-presentation (a V shape with L or K scale scores >65 T and both higher than F), negative self-presentation (a carat shape with F scale score >65 and F at least 10 T above L or K), and a neutral self-presentation (L, F, and K scores <65 T). The modal presentation style of AR subjects was to either make very critical self-appraisals (34%) or neutral ones (46%). In contrast, neutral ones (26%) were the most common modal validity configuration of the normal controls. Distributions of the three validity patterns between the two groups showed no significant difference (Chi-square=2.87, df=2, P=0.26).
Table 1 presents the mean and standard deviation of the clinical scales of the MMPI-2 in two groups.
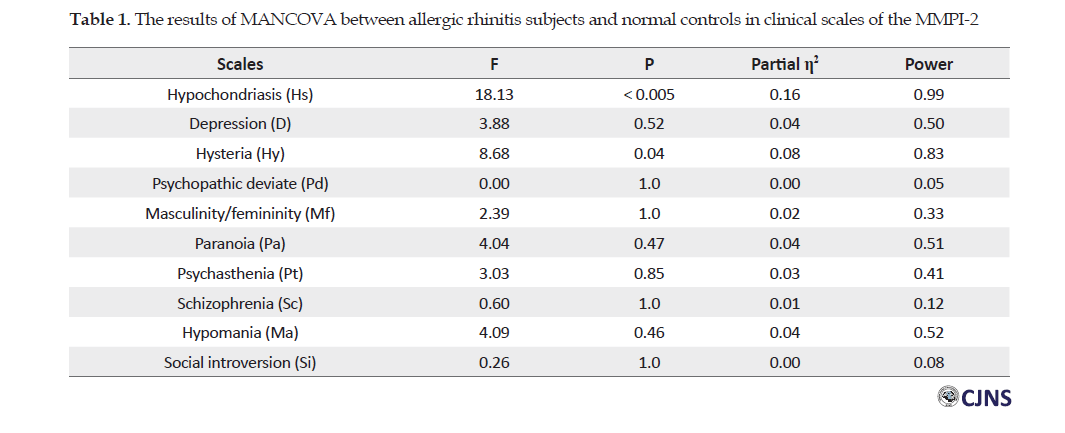
There was a statistically significant difference between two groups in the combined clinical scales after adjusting for sex (F (10, 88)=2.19, P=0.03, Wilks’ Λ=0.80, partial η2=0.20). The MANCOVA results showed a significantly high hypochondriasis scale score in AR subjects compared with normal controls (50% vs. 26%, F (1, 97)=18.13; P<0.005; partial η2=0.16) It was the highest score in 26% of the cases and 8% of controls. Another important difference of profiles among two groups was observed in hysteria scale (T-score > 65, 20% vs. 10%, F (1, 97)=8.68; adjusted P=0.04; partial η2=0.08). The statistical analysis showed that females obtained five out of the ten high T-scores in the hysteria scale (16.7% of females in the case group). In contrast, 25% of males in the case group achieved Hy scores >65 T-score. About 50% of the AR subjects showed a conversion V pattern (3-1-2 pattern), which means the tendency to be optimistic about their physical symptoms.
Characterization was performed using the MMPI-2 in the case and control groups and based on the Chi-square test (Table 2).
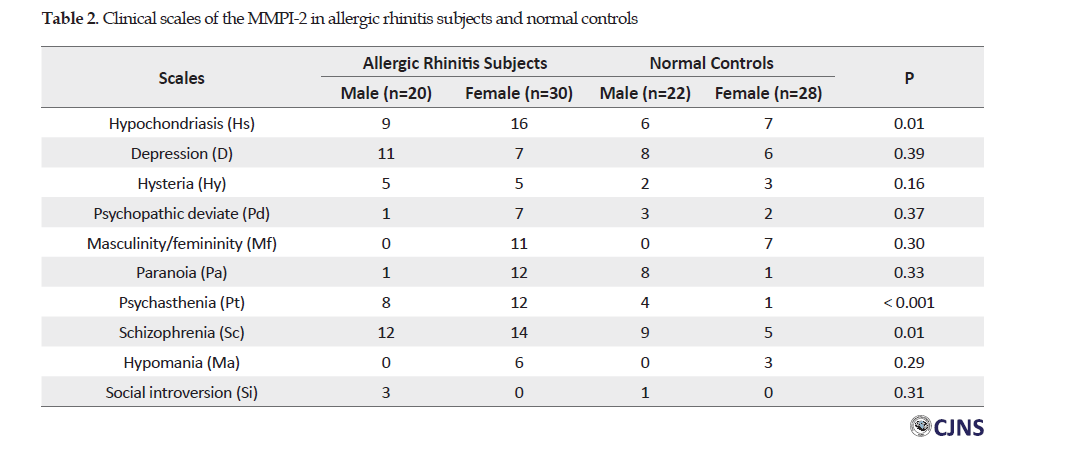
Forty-eight percent of the normal controls did not have elevated scores in clinical scales (45.5% of males and 50.0% females). In the allergic group, T-scores of clinical scales in only 16% of subjects were <65 (15% of males and 16.7% females). The most common profiles with elevated scores in the case group were schizophrenia (52%) and hypochondriasis (50%), whereas they were contained schizophrenia (28%) and depression (28%) in the control group. Also, the frequency of psychasthenia scale was significantly different between two groups (40% in AR subjects vs. 10% in normal controls, Chi-square=12.0, df=1, odds ratio=6 [95%CI 1.9-22.3], P<0.001). In 9 out of 20 AR subjects, this scale was elevated with schizophrenia scale, which mainly T-score of the Sc scale was higher than the Pt scale. In 11 out of 20 cases, this scale was associated with depression.
Table 3 depicted 1-point, 2-point, and 3-point codes of AR subjects and normal controls based on the decreasing frequency.

The most frequent 2-point code in AR subjects was the 28/82 pattern and it was seen exclusively in men. The most frequent 2-point code in women was the 26/62 pattern. In normal controls, the most frequent code pattern was the 68/86 pattern.
Discussion
Many epidemiologic studies have shown that AR is a multifactorial disease and is associated with psychological factors. The aim of this study was to use MMPI-2 scores in Iranian patients with AR and evaluate the psychological aspects of AR people. MMPI-2 scores are useful for measuring the emotional and physical aspects of patients with chronic diseases.
The present study indicated a significantly higher T-score on the hypochondriasis in AR subjects, which means these subjects had a high degree of distress about bodily functions. According to Graham, common characteristics among high scorers on the Hs scale include chronic weakness, lack of energy, fatigue, and sleep disturbance [20]. Many allergic people suffer from sleep disorders, fatigue, and sexual dysfunction [21]. Therefore, it is not surprising that people with chronic illness may use real or fictional bodily complaints to avoid emotional distress and displacement as an anxiety-coping mechanism [16, 19]. We examined personality traits between AR subjects and normal controls of either sex. The frequency of AR subjects who scored high on the Hs scale showed no significant difference. This finding was in contrast to previous studies [10, 19], in which hypochondriasis was more frequent in women. This discrepancy could be due to our small sample size.
Other significant high T-scores in cases were related to the hysteria scale. This scale measures the amount and type of denial as a defense mechanism. Patients with high levels of hysteria accept physical problems but reject their distress. They try to deal with their concerns by confining their problems to their physical body. These people inflate clinical symptoms of their disease and use this method to affect others [16]. Allergic people usually expect more attention and have more physical complaints. As a result, they gain higher scores in the hysteria scale [9]. When we considered T-score >65 as the cutoff point, abnormal MMPI profiles in AR and normal subjects were observed about 85% and 50%, respectively.
Although the mean Hs, D, and Hy T-scores for the allergic group were significantly higher than the control group, in the majority of cases, it was within the common scoring range and did not indicate a clinically important issue. Our results were in line with previous studies. Lv et al. revealed that women with AR scored higher than controls on Hs, D, Hy, Pt, and Sc clinical scales [9]. Also, Gauci et al. exhibited that women with AR scored significantly higher on the hypochondriasis (Hs) and social introversion (Si) scales [19]. Pasaoglu et al. revealed that patients with chronic idiopathic urticaria had higher scores on Hs, D, Hy, Pd, Pa, Pt, Sc, and Si scales compared with the control group. However, there was no significant difference between the two case and control groups [22].
The most frequent clinical scale in both groups was schizophrenia. It can be expected that allergic people feel social isolation and discomfort. However, the frequency of the psychasthenia scale showed a significant difference than other clinical scales. This scale measures long-lasting anxiety. We found that 18% of AR subjects had high scores on the Pt and Sc scales that can be explained as follows: mental confusion keeps the person away from focusing on solutions to solve the problems. Similar to this finding, elevations in Pt clinical scale indicate that allergic people experience psychological distress and discomfort [20]. On the other hand, 22% of AR subjects showed high scores on Pt and D scales; mean depression and indecisiveness are associated with worry and anxiety. It has been shown that the frequency of depression, anxiety, and sleep disorders in allergic subjects is higher than in the general population and vice versa; the frequency of allergy is higher in patients with depression [23].
The most frequent code pattern in AR subjects included a combination of scales 2 and 8, indicating the feeling of worthlessness, severe depression with anxiety and agitation, and fear of loss of control. Interestingly, the profile of normal controls revealed elevations of the MMPI-2 clinical scales 6 and 8, which are representative of marginal psychological adjustment. Twenty-four percent of AR subjects and 48% of normal controls displayed profiles without increasing clinical scale, suggesting that there w no apparent psychological maladjustment.
This study showed an increase in global psychopathology indices, especially on the neurosis-related scales (Hs, D, and Hy). Several possible mechanisms for the association between psychological indices and AR were suggested: 1) immunologic mechanism via the hypothalamic-pituitary-adrenal axis and 2) releasing mediators in the nose and plasma during an allergic reaction, which may travel to the central nervous system [19]. Also, some medications used to treat allergy can worsen psychiatric problems, perhaps by their effects on neurotransmitters and glucocorticoids [16].
This study had several limitations, which need to be addressed. The small sample size restricts the generalization of our findings. The results of MANCOVA showed low power for some clinical scales. The possible reason for this finding is that the covariate uses a degree of freedom that had been assigned to the error term that can result in an increase in the mean square error (reducing power). Second, the individuals’ personality is so complex that its different aspects cannot be explained even by the MMPI-2. Third, this study had a cross-sectional design. Thus, we could not determine which factors constitute stable personality characteristics due to AR. Fourth, we did not explore whether severity is a potentially important variable in assessing the MMPI-2 profiles of AR subjects. Finally, only subjects who had a minimum high school education level were included in this study. It is possible that the personality traits of AR subjects are different in other groups.
Conclusions
In summary, the results of the MMPI-2 indicated that AR patients suffer not only from physical discomfort but also from psychological distress. Allergic subjects are more sensitive to psychopathological features and these features, such as hypochondriasis, hysteria, and psychasthenia are more common in these people than in the general population. Therefore, these disorders could affect these patients’ quality of life and psychological treatment is important for these patients.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (No.: 3.132.599). All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki 2013.
Funding
This research received no specific grant from any funding agency, commercial, or non-profit sectors.
Authors' contributions
Methodology: Mir Mohammad Jalali; Investigation, writing-review & editing: All authors. Supervision, Writing-original draft: Robabeh Soleimani, Mir Mohammad Jalali; Funding acquisition, Resources: Robabeh Soleimani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
The authors are grateful to the Vice Chancellorship of Research and Technology of Guilan University of Medical Sciences.
References
1.Chen MH, Su TP, Chen YS, Hsu JW, Huang KL, Chang WH, et al. Allergic rhinitis in adolescence increases the risk of depression in later life: A nationwide population-based prospective cohort study. J Affect Disord. 2013; 145(1):49-53. [DOI:10.1016/j.jad.2012.07.011] [PMID]
2.Meltzer EO, Blaiss MS, Jennifer Derebery M, Mahr TA, Gordon BR, Sheth KK, et al. Burden of allergic rhinitis: Results from the Pediatric Allergies in America survey. J Allergy Clin Immunol. 2009; 124(3 Suppl):S43-S70. [DOI:10.1016/j.jaci.2009.05.013] [PMID]
3.Postolache TT, Lapidus M, Sander ER, Langenberg P, Hamilton RG, Soriano JJ, et al. Changes in allergy symptoms and depression scores are positively correlated in patients with recurrent mood disorders exposed to seasonal peaks in aeroallergens. Sci World J. 2007; 7:732129. [DOI:10.1100/tsw.2007.286] [PMID] [PMCID]
4.Buske-Kirschbaum A, Ebrecht M, Kern S, Gierens A, Hellhammer DH. Personality characteristics in chronic and non-chronic allergic conditions. Brain Behav Immun. 2008; 22(5):762-8. [DOI:10.1016/j.bbi.2007.12.002] [PMID]
5.Chang HY, Seo JH, Kim HY, Kwon JW, Kim BJ, Kim HB, et al. Allergic diseases in preschoolers are associated with psychological and behavioural problems. Allergy Asthma Immunol Res. 2013; 5(5):315-21. [DOI:10.4168/aair.2013.5.5.315] [PMID] [PMCID]
6.Mehrinejad SA, Rajabi Moghadam S. [Comparison of the personality characteristics of the patients suffering from allergic rhinitis with those of normal people (Persian)]. Sci J Kurdistan Univ Med Sci. 2012; 17(4):53-60. http://sjku.muk.ac.ir/article-1-924-en.html
7.Rodinkova V, Kondratyuk A, Bondarchuk O, Korytska I, Kyrychenko L, Kryvonos T, et al. Psychological Profiles of Seasonal Allergy Patients in Vinnytsya, Ukraine. J Allergy Clin Immunol. 2019; 143(2):AB237. [DOI:10.1016/j.jaci.2018.12.722]
8.Harter K, Hammel G, Krabiell L, Linkohr B, Peters A, Schwettmann L, et al. Different psychosocial factors are associated with seasonal and perennial allergies in adults: cross-sectional results of the KORA FF4 Study. Int Arch Allergy Immunol. 2019; 179(4):262-72. [DOI:10.1159/000499042] [PMID]
9.Lv X, Han D, Xi L, Zhang L. Psychological aspects of female patients with moderate-to-severe persistent allergic rhinitis. ORL J Otorhinolaryngol Relat Spec. 2010; 72(5):235-41. [DOI:10.1159/000314884] [PMID]
10.Muluk NB, Oğuztürk O, Koç C, Ekici A. Minnesota multiphasic personality inventory profile of patients with allergic rhinitis. J Otolaryngol. 2003; 32(3):198-202. [DOI:10.2310/7070.2003.40380] [PMID]
11.Vamanshankar H, Hegde KS, Chaturvedi J, Pratibha CB, Ross A, Nayar RC, et al. Do patients with allergic rhinitis have a particular personality trait? J Laryngol Otol. 2013; 127(4):378-82. [DOI:10.1017/S0022215113000170] [PMID]
12.Ologe FE, Adebola SO, Dunmade AD, Adeniji KA, Oyejola BA. Symptom score for allergic rhinitis. Otolaryngol Head Neck Surg. 2013; 148(4):557-63. [DOI:10.1177/0194599813477605] [PMID]
13.Annesi‐Maesano I, Didier A, Klossek M, Chanal I, Moreau D, Bousquet J. The Score for Allergic Rhinitis (SFAR): A simple and valid assessment method in population studies. Allergy. 2002; 57(2):107-14. [DOI:10.1034/j.1398-9995.2002.1o3170.x] [PMID]
14.Sood A. Diagnostic significance of nasal eosinophilia in allergic rhinitis. Indian J Otolaryngol Head Neck Surg. 2005; 57(1):13-6. [DOI:10.1007/BF02907618] [PMID] [PMCID]
15.Dehghani M, Ashori A, Askarabad MH, Khatibi M. Standardization and psychometric properties of Minnesota Multiphasic Personality Inventory (MMPI-2). J Psychol. 2010; 14(3):299-318. https://psycnet.apa.org/record/2012-03139-005
16.Mehrinejad SA, Jalili M, Ghaffari J. Comparison between psychological traits of patients with various atopic allergic diseases and healthy volunteers: A case-control study. Indian J Allergy Asthma Immunol. 2013; 27(1):42-6. [DOI:10.4103/0972-6691.116613]
17.Rademaker AR, Kleber RJ, Meijer ME, Vermetten E. Investigating the MMPI-2 trauma profile in treatment-seeking peacekeepers. J Pers Assess. 2009; 91(6):593-600. [DOI:10.1080/00223890903230899] [PMID]
18.Munley PH, Germain JM, Tovar-Murray D, Borgman AL. MMPI-2 profile code types and measurement error. J Pers Assess. 2004; 82(2):179-88. [DOI:10.1207/s15327752jpa8202_6] [PMID]
19.Gauci M, King MG, Saxarra H, Tulloch BJ, Husband AJ. A Minnesota Multiphasic Personality Inventory profile of women with allergic rhinitis. Psychosom Med. 1993; 55(6):533-40. [DOI:10.1097/00006842-199311000-00009] [PMID]
20.Graham JR. MMPI-2: Assessing personality and psychopathology. New York: Oxford University Press; 2011. https://books.google.com/books?id=FyWBuQAACAAJ&dq
21.Jalali MM, Gerami H, Soleimani R, Alizadeh P. Quality of life in patients with allergic rhinitis in the North of Iran. J Clin Diagn Res. 2018; 12(6):MC1-MC4. [DOI:10.7860/JCDR/2018/32872.11694]
22.Pasaoglu G, Bavbek S, Tugcu H, Abadoglu O, Misirligil Z. Psychological status of patients with chronic urticaria. J Dermatol. 2006; 33(11):765-71. [DOI:10.1111/j.1346-8138.2006.00178.x] [PMID]
23.Postolache TT, Komarow H, Tonelli LH. Allergy: A risk factor for suicide? Curr Treat Options Neurol. 2008; 10(5):363-76. [DOI:10.1007/s11940-008-0039-4] [PMID] [PMCID]
Received: 2020/08/25 | Accepted: 2020/06/12 | Published: 2020/06/12
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |