BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://cjns.gums.ac.ir/article-1-326-en.html


 , Robabeh Soleimani2
, Robabeh Soleimani2 

 , Hossein Khoshrang1
, Hossein Khoshrang1 

 , Cyrus Emir Alavi3
, Cyrus Emir Alavi3 
 , Gelareh Biazar *
, Gelareh Biazar * 

 1, Mohadese Ahmadi1
1, Mohadese Ahmadi1 

 , Mahin Tayefeh Ashrafiyeh3
, Mahin Tayefeh Ashrafiyeh3 

 , Shamin Zakariapour4
, Shamin Zakariapour4 

2- Department of Psychiatry, Kavosh Behavioral, Cognitive and Addiction Research Center, Shafa Hospital, Guilan University of Medical Sciences, Rasht, Iran
3- Razi Clinical Research Development Center, Guilan University of Medical Sciences, Rasht, Iran
4- Student Research Committee, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
Introduction
Electroconvulsive Therapy (ECT) is used to manage a wide variety of psychiatric diseases, including major depression, mania, and schizophrenia [1-5]. It is also surviving for patients who cannot tolerate drug side effects, treatment-resistant cases, and emergency conditions such as suicide, catatonia, and neuroleptic malignant syndrome when a prompt therapeutic response is crucial [2, 6]. It is a safe and effective treatment modality in both inpatients and outpatients settings. The mortality rate of ECT is low and reported as two deaths per 100000 cases [7]. Since ECT is performed under general anesthesia, it is more easily acceptable [8]. However, ECT-related side effects should be considered. Studies have shown that these patients might be affected by hemodynamic fluctuations due to vagal tone activity before the seizure and increased sympatric tone after the seizure, which results in bradycardia followed by tachycardia and hypertension [9, 10]. Other side effects include headache, myalgia, memory loss, delirium, nausea, dizziness, confusion, fatigue, dry mouth, numbness, and falling among old patients (frequency reported) [10, 11].
Succinylcholine-related complications should be considered as well. However, it is thought that the majority of these symptoms might not be due to ECT, rather to their medications or underlying diseases [12, 13]. Although most of these side effects are transient and minor, if not controlled well, they may affect the patient’s tolerance to continue and finish the treatment course [14, 15]. Despite several advantages, side effects, stigma, poor knowledge, and attitude around ECT are the main barriers to the use and acceptance of ECT [14]. For example, patients who experience a severe headache following the ECT administration may refuse to follow and complete all ECT sessions [15]. Therefore to reduce patients’ suffering and help them better accept this procedure, besides improving their general view toward ECT and promoting public information, its side effects must be well identified and managed as well. A few studies have focused on this topic, but their results could not be generalized due to the study differences in patients’ characteristics, anesthesia methods, and so on. This survey was conducted to identify and focus on the major ECT side effects among our psychiatric patients in Shafa Hospital as an academic, referral, and the main center for all types of psychiatric diseases.
Materials and Methods
This cross-sectional study took place in Shafa Academic Hospital affiliated to Guilan University of Medical Sciences (GUMS). The inclusion criterion was the patients referred in Spring and Autumn 2019 on 235 patients who were referred in that period for ECT. ECT was administrated in a dedicated suite and under the supervision of the ECT team consisting of a psychiatric, an anesthesiologist, and a trained nurse. All patients underwent anesthesia visits before scheduling for ECT. This evaluation included a medical history and laboratory tests review, and a physical examination. The energy levels for ECT administration were selected based on seizure threshold which was related to age, gender, and underlying disease, so it varied from one patient to another [14].
After the permission, informed written consent was obtained and admitted cases for ECT were enrolled in the survey. If patients had the insight to give the informed consent it would be obtained from them otherwise like psychotic cases a relative who could legally give it was asked for. During the procedure, the patients underwent standard monitoring by electrocardiography, pulse oximetry, and non-invasive blood pressure measurements. Then propofol 1-1.5 mg/kg followed by succinylcholine 0.5 mg/kg as a muscle relaxant was administrated. Airway control was maintained by mask ventilation. After a short period of hyperventilation, an electrical current was delivered to the brain through two electrodes placed bilaterally over the temporal region resulting in a seizure that lasted between 20 to 60 seconds.
A questionnaire consists of demographic data and complications in the recovery ward was filled out by a nurse who was not engaged in the survey process. Data were analyzed an reported by frequency reporting and T-test in SPSS software V. 20.
Results
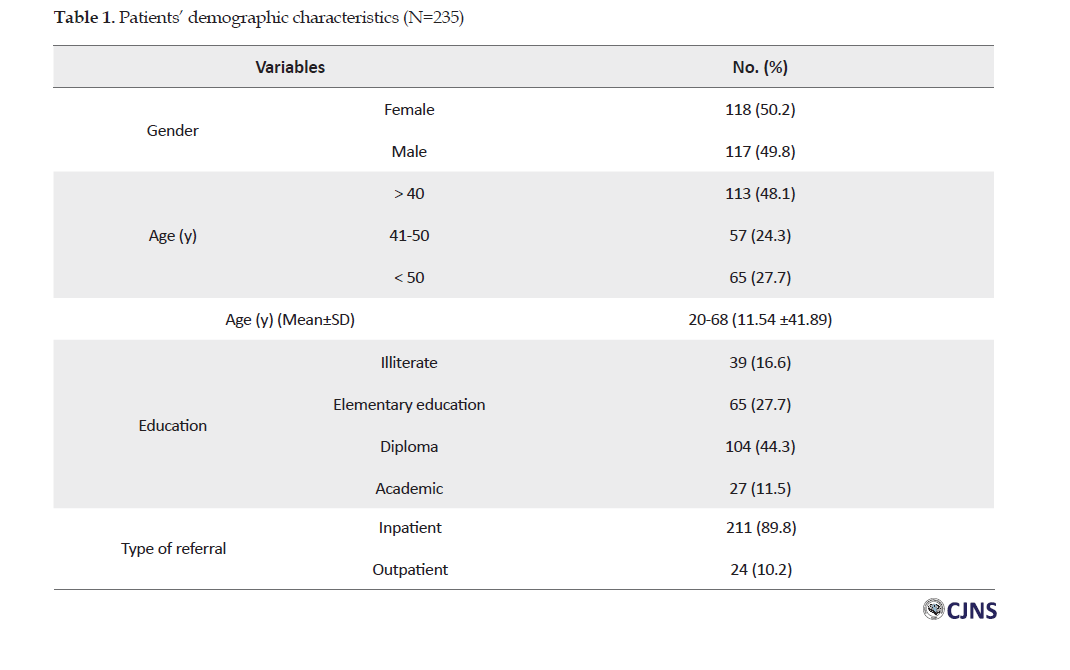
During the study period, a total of 235 patients were evaluated. Patients’ demographic data are presented in Table 1.
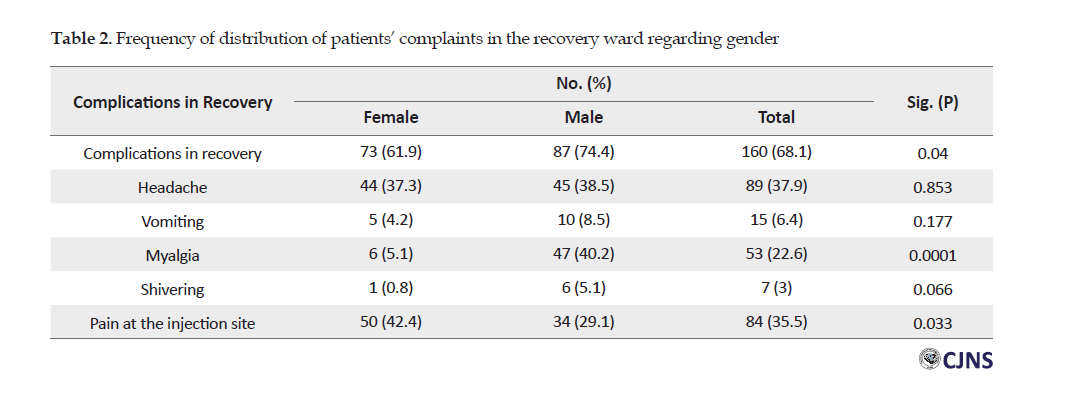
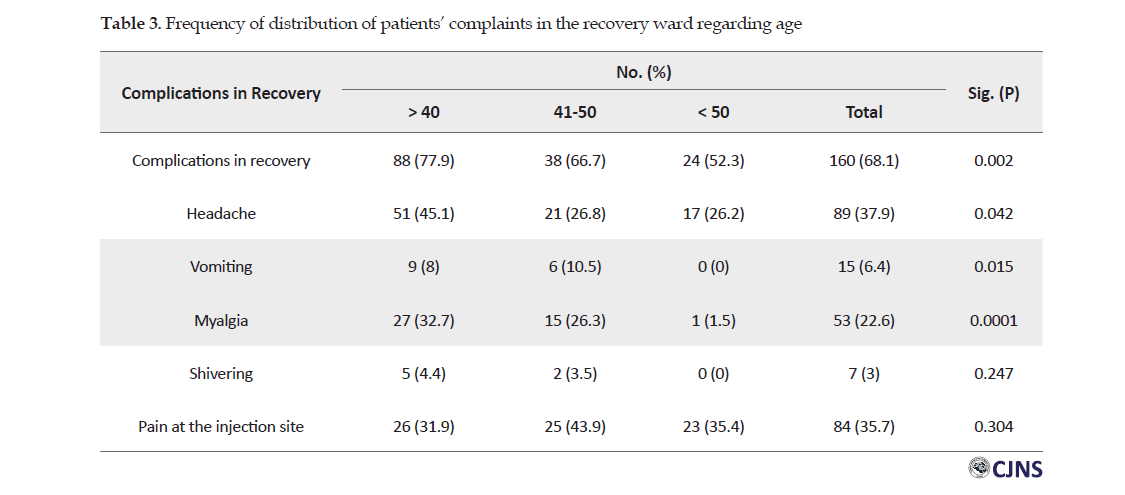
The underlying psychiatric disease was heterogeneous, including bipolar, psychosis, major depression, and anxiety disorders. Among them, 160 (68.1%) had at least one complication. A total of 53 patients (22.6%) reported myalgia. Also, 89 patients (37.9%) had a headache, 15 (6.4%) nausea, 7 (3%) shivering, and 84 (35.5%) pain in the injection site. Male gender and younger people were more prone to myalgia. The correlation between age, gender, and patients complaints in the recovery ward is presented in Tables 2 and 3.
Discussion
This study revealed that headache, myalgia, and propofol injection pain were the main side effects of ECT during the recovery period. In line with this paper, studies have reported that 48% to 85% of patients experience post ECT headache [16]. The pathophysiological mechanism is not well known, but it is postulated that vasodilation contraction of temporalis and masseter muscles, alternations of serotonergic neurotransmission in the brain, trigger this kind of headache [17, 18]. The incidence of headache seems to be different among studies. This may be explained by different times of pain assessment. Sometimes this symptom is not experienced in the recovery ward [14]. It is indicated that these undesirable side effects are presented within the first hours after ECT [19]. Haghighi et al. reported that 21.6% of the patients complained of headaches after 6 hours [20] while Isura et al. reported it as 71.4% during the first 2 hours [21]. Confirming the importance of the time of patients’ evaluation, in Saricicek et al. study, the incidence of headache and myalgia significantly diminished 12 and 24 hours post ECT comparing to the first 2 hours as the first measurement time point [22].
The case selection pattern was also different among studies, our cases were heterogeneous which was different from Rajapakse et al. who only selected patients with major depression [21]. In our study, male gender and younger age were identified as predictors for myalgia. However, this correlation was not found for underlying diseases and medical comorbidities. Besides, the headache was significantly more common among people under 45 years old. Myalgia was identified as the second patients’ complaint after ECT. We suppose that it was underreported in this studybecause the patients were assessed in the recovery ward immediately after regaining consciousness. They may have complained of myalgia during the next hours.
A positive correlation was found regarding myalgia and male gender and age under 45. Dinwiddie et al. indicated that myalgia was more common among patients younger than 45 years old which was similar to our results [14]. Post ECT myalgia is a well-known adverse effect of the procedure. There is not enough evidence to know the real prevalence of myalgia. Its occurrence and severity depend on the used anesthetic agents and the technique. Limited literature has focused on the subject. As clinical evidence indicates that post ECT myalgia is partly due to succinylcholine, it is claimed that myalgia is the result of muscle damage due to succinylcholine fasciculation [23].
In contrast to available literature, Markowitz et al. reported that the major patients’ complaints were nausea and headache (as high as 45%) [24]. On the whole, ECT side effects are among the main barriers for patients to complete the ECT sessions. On the other hand, simple, safe, and effective strategies are available to manage these complications. For example, post-ECT headache can be treated by ketorolac acetaminophen, ibuprofen. Moreover, studies have reported promising results by prophylactic use of ibuprofen 600 mg, and also intranasal sumatriptan [21]. Furthermore, to reduce or prevent myalgia, simple and safe strategies such as a low dose of succinylcholine before the main dosage can reduce the fasciculation severity. Low doses of non-depolarizing muscle relaxants could also be effective. Pain on the injection site as the other major side effect can make anesthesia an unpleasant experience. However, it could also be easily prevented by several modalities. Even low doses of propofol before administrating the main dose could alleviate the pain by desensitization mechanism which was well discussed in the current literature [25]. So it is strongly recommended that ECT guidelines be revised, to control these adverse effects with a preventive approach.
The strength of our study was that we evaluated more side effects among ECT patients, while current literature has only focused on two common adverse effects such as headache and myalgia. Although our results confirmed the same two main ECT side effects as well. The significant finding of this work was that in spite of the available studies indicating these adverse side effects, they still remain as suffering conditions for these patients. In other words, as a big concern, the clinical usage of the findings of previous studies is not promising considering that the mentioned side effects still frequently occur in an academic and referral hospital. It is crucial that more attention be paid to the practical aspect of our research.
Conclusion
Supporting the findings of some previous studies, headache, myalgia, and pain in the injection site were the main complaints reported by the ECT patients. However, the disappointing conclusion could be the fact that enough attention has not been paid to the practical aspect of the previous research in routine clinical practice. It is strongly recommended that ECT guidelines be revised to control these adverse effects with a preventive approach. Preventive strategies for headache, myalgia, and propofol injection pain are recommended for routine practice. As the next steps, we welcome future well-planned clinical trials with larger sample size and longer follow up durations to develop the optimal therapeutic and preventive strategies to solve these complaints and help the patients to have a better attitude toward ECT and complete the subsequent sessions.
Our evaluation was restricted to the recovery ward, so we missed the possible incidence of complications during the next hours. Furthermore, it was a single-center study with small sample size.
Ethical Considerations
Compliance with ethical guidelines
The study protocol was approved by the Research Ethics Committee of the GUMS (Ref: IR.GUMS.REC.1397.356) and subjects gave written informed consent. All study procedures were in compliance with the ethical guidelines of the Declaration of Helsinki, 2013.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Drafting the original paper: Siamak Rimaz and Gelareh Biazar; Writing, reviewing, and editing: Mohadese Ahmadi and Mahin Tayefeh Ashrafiyeh; Collecting resources: Hossein Khoshrang and Cyrus Emir Alavi; Supervision: Robabeh Soleimani; Data collection: Shamin Zakariapour.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgements
We thanks all patients and stuffs who have cooperated in ECT ward of Shafa Hospital.
References
1.Tess AV, Smetana GW. Medical evaluation of patients undergoing electroconvulsive therapy. N Engl J Med. 2009; 360(14):1437-44. [DOI:10.1056/NEJMra0707755] [PMID]
2.Liu CC, Qian XY, An JX, Yu ZL, Wu JP, Wen H, et al. Electroconvulsive therapy under general anesthesia with cisatracurium, laryngeal mask airways, and Bispectral index. J ECT. 2016; 32(1):17-9. [DOI:10.1097/YCT.0000000000000251] [PMID]
3.Mashayekhi A, Ghayoumi AR. Catatonia development in a patient with bipolar disorder following electroconvulsive therapy: A case report. Iran J Psychiatry. 2019; 14(1):109-12. [DOI:10.18502/ijps.v14i1.429] [PMID] [PMCID]
4.Roshanaei-Moghaddam B, Pauly MC. Treatment of methamphetamine dependence with Electroconvulsive Therapy (ECT) in Iran: A critical note. Iran J Psychiatry. 2014; 9(3):184-7. [PMID] [PMCID]
5.Hekmatara S, Ghorishizadeh MA, Amiri S. Comparison of bifrontal and bitemporal electroconvulsive therapy in patients with major depressive disorder. Iran J Psychiatry. 2009; 4(1):13-6. https://ijps.tums.ac.ir/index.php/ijps/article/view/492
6.Ding Z, White PF. Anesthesia for electroconvulsive therapy. Anesth Analg. 2002; 94(5):1351-64. [DOI:10.1097/00000539-200205000-00057] [PMID]
7.Kayalha H, Khezri M, Rastak Sh, Mehdi Pour H, Sofiabadi M. [Comparison of the hemodynamic effects of two anesthetics; sodium thiopental and propofol in patients undergoing electroconvulsive therapy (Persian)]. J Ardabil Univ Med Sci. 2018; 18(3):357-66. [DOI:10.29252/jarums.18.3.357]
8.Rashmi P, Singh PV. Anesthesia for electroconvulsive therapy: A Noble approach. Int J Med Res Health Sci. 2015; 4(4):890-5. [DOI:10.5958/2319-5886.2015.00179.4]
9.Uppal V, Dourish J, Macfarlane A. Anaesthesia for electroconvulsive therapy. Contin Educ Anaesth Crit Care Pain. 2010; 10(6):192-6. [DOI:10.1093/bjaceaccp/mkq039]
10.Wajima Z. Anesthesia management of special patient populations undergoing electroconvulsive therapy: A review. Journal of Nippon Medical School. 2019; 86(2):70-80. [DOI:10.1272/jnms.JNMS.2019_86-202]
11.Bhagat P, Waghmare H, Gandhi P. A study of common side effects of Electro Convulsive Therapy and their predictors. Glob J Res Anal. 2017; 6(6):318-9. https://bit.ly/3fBONkc
12.Nazemroaya B, Moradi Farsani D, Sadeghi-Vaghfi A. [Comparison of cisatracurium and succinylcholine on hemodynamic changes during and after electroconvulsive therapy (Persian)]. J Isfahan Med Sch. 2016; 34(395):963-70. https://www.researchgate.net/publication/316557614
13.Nazemroaya B, Hashemi ST, Pourreza A, Mirzakhani F. Comparison of seizure duration and hemodynamic changes with cisatracurium versus succinylcholine in electroconvulsive therapy. Arch Anesth Crit Care. 2018; 4(1):417-22. [DOI:10.15761/PD.1000182]
14.Dinwiddie SH, Huo D, Gottlieb O. The course of myalgia and headache after electroconvulsive therapy. J ECT. 2010; 26(2):116-20. [DOI:10.1097/YCT.0b013e3181b07c0a] [PMID]
15.Rasmussen KG, Petersen KN, Sticka JL, Wieme LJ, Zosel JH, Marienau MES, et al. Correlates of myalgia in electroconvulsive therapy. J ECT. 2008; 24(1):84-7. [DOI:10.1097/YCT.0b013e31814b17e6] [PMID]
16.Isuru A, Rodrigo A, Wijesinghe C, Ediriweera D, Premadasa Sh, Wijesekara C, et al. A randomized, double-blind, placebo-controlled trial on the role of preemptive analgesia with acetaminophen [paracetamol] in reducing headache following Electroconvulsive Therapy [ECT]. BMC Psychiatry. 2017; 17(1):275. [DOI:10.1186/s12888-017-1444-6] [PMID] [PMCID]
17.Roth LS. Acetaminophen preferable to ibuprofen for pretreatment of electroconvulsive therapy-induced headache. J Clin Psychiatry. 2004; 65(5):726. [DOI:10.4088/JCP.v65n0520g] [PMID]
18.Waite J, Easton A, editors. The ECT handbook. 3rd edition. London: RCPsych Publications; 2013. https://books.google.com/books?id=haSlvJlOXC0C&dq
19.American Psychiatric Association. Task Force on Electroconvulsive Therapy. The practice of ECT: Recommendations for treatment, training and privileging. Convuls Ther. 1990; 6(2):85-120. [PMID]
20.Haghighi M, Sedighinejad A, Naderi Nabi B, Emiralavi C, Biazar G, Mirmozaffari K, et al. The incidence and predictors of headache and myalgia in patients after Electroconvulsive Therapy (ECT). Anesth Pain Med. 2016; 6(3):e33724. [DOI:10.5812/aapm.33724]
21.Rajapakse T, Sivapalasingam A. Patients presenting with depression to a psychiatry clinic: A descriptive survey. Sri Lanka J Psychiatry. 2011; 2(1):36-8. [DOI:10.4038/sljpsyc.v2i1.3166]
22.Saricicek V, Sahin L, Bulbul F, Ucar S, Sahin M. Does rocuronium-sugammadex reduce myalgia and headache after electroconvulsive therapy in patients with major depression? J ECT. 2014; 30(1):30-4. [DOI:10.1097/YCT.0b013e3182972bd2] [PMID]
23.Wong SF, Chung F. Succinylcholine‐associated postoperative myalgia. Anaesthesia. 2000; 55(2):144-52. [DOI:10.1046/j.1365-2044.2000.055002144.x] [PMID]
24.Markowitz JS, Kellner CH, DeVane CL, Beale MD, Folk J, Burns C, et al. Intranasal sumatriptan in post-ECT headache: Results of an open-label trial. J ECT. 2001; 17(4):280-3. [DOI:10.1097/00124509-200112000-00008] [PMID]
25.Sedighinejad A, Naderi Nabi B, Haghighi M, Biazar G, Imantalab V, Rimaz S, et al. Comparison of the effects of low-dose midazolam, magnesium sulfate, remifentanil and low-dose etomidate on prevention of etomidate-induced myoclonus in orthopedic surgeries. Anesth Pain Med. 2016; 6(2):e35333. [DOI:10.5812/aapm.35333]
Received: 2020/08/25 | Accepted: 2020/06/12 | Published: 2020/06/12
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



