Thu, Apr 25, 2024
Volume 4, Issue 1 (Winter 2018)
Caspian J Neurol Sci 2018, 4(1): 1-5 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadianinejad S, Majidinasab N, Nejati A, Hatamian H, Mehramiri A, Sajedi S et al . Tapering Oral Steroid Treatment After IV Methylprednisolone Pulse Therapy in Demyelinating Optic Neuritis. Caspian J Neurol Sci 2018; 4 (1) :1-5
URL: http://cjns.gums.ac.ir/article-1-212-en.html
URL: http://cjns.gums.ac.ir/article-1-212-en.html
Seyed-Ehsan Mohammadianinejad1 
 , Nastaran Majidinasab1
, Nastaran Majidinasab1 
 , Adel Nejati *
, Adel Nejati * 
 2, Hamidreza Hatamian3
2, Hamidreza Hatamian3 
 , Asieh Mehramiri1
, Asieh Mehramiri1 
 , Seyed-Aidin Sajedi1
, Seyed-Aidin Sajedi1 
 , Saeed Hesam1
, Saeed Hesam1 


 , Nastaran Majidinasab1
, Nastaran Majidinasab1 
 , Adel Nejati *
, Adel Nejati * 
 2, Hamidreza Hatamian3
2, Hamidreza Hatamian3 
 , Asieh Mehramiri1
, Asieh Mehramiri1 
 , Seyed-Aidin Sajedi1
, Seyed-Aidin Sajedi1 
 , Saeed Hesam1
, Saeed Hesam1 

1- Golestan Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2- Golestan Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran , nejatiadel@gmail.com
3- Department of Neurology, Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
2- Golestan Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran , nejatiadel@gmail.com
3- Department of Neurology, Poursina Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
Full-Text [PDF 827 kb]
(3758 Downloads)
| Abstract (HTML) (3920 Views)
Full-Text: (2182 Views)
Introduction
Optic neuritis is an inflammation of the optic nerve. The most common cause is demyelinating optic neuritis which may occur in the form of Multiple Sclerosis (MS) and less likely Neuromyelitisoptica (NMO), connective tissue disorders and other immune mediated optic neuropathies [1-3]. It occurs more in women, typically young adults in the age group of 20-45 years [4]. There is often a concern of making a diagnosis of MS by patients and even physicians referring these patients to a neurologist. Typical optic neuritis is characterized by a unilateral painful visual impairment of variable severity evolved within 2 weeks with good and persistent response to high dose IV steroid therapy [5-7]. It is associated with a higher risk of conversion to MS according to Optic Neuritis Treatment Trial study (ONTT). This study as the largest prospective study among patients with optic neuritis, demonstrated that the risk of conversion to MS in the following years is particularly remarkable when associated with brain MRI lesions characteristic for demyelination of disease [1, 8-10].
ONTT showed that IV steroid treatment in patients presenting with the first attack of optic neuritis results in more rapid improvement associated with reducing the short term risk of developing MS in the following two years compared with controlled placebo group. An interesting and unexpected finding was that oral steroid treatment increased the risk of second relapse and developing MS in this time period. The beneficial effect of IV regimen in reducing the risk of MS was mostly manifested in the presence of abnormal brain MRI consisting of 2 or more characteristic demyelinating lesions. Patients in the IV steroid group in this study received 3 gram IV methylprednisolone followed by oral prednisone 1 mg/kg for 2 weeks while the oral steroid group received oral prednisolone 1 gr/kg for 2 weeks as the only treatment throughout the course. Studies have shown the efficacy of IV high dose steroid therapy in accelerating recovery and also improving the short term prognosis at 2 years regarding conversion to MS [11].
It is important to consider that most studies have not shown the positive effect of this therapy on the final outcome of patients with optic neuritis. IV methylprednisolone pulse therapy is now indicated in optic neuritis in the presence of white matter lesions, severe pain, significant impairment of vision (more than 50%), poor vision in the fellow eye and disabling scotoma [12-15].While oral steroid following IV pulse therapy has been mostly abandoned in adults with optic neuritis because it is considered as adding no benefit while putting the patient at greaterrisk of adverse effects, it is still used sometimes in adults with more severe optic neuritis. It is also known that adverse effects of steroid therapy including GI upset, flushing, sleep and mood disturbance, acne and more importantly serious events such as avascular bone necrosis and metabolic disturbances are dependent on the dose and duration of the steroid treatment [16, 17].
The aim of this study was to show if the tapering oral steroid treatment for a short course following IV pulse steroid therapy would affect the outcome in patients presenting with acute optic neuritis. Both the positive and negative results could help us to evaluate the risk/benefit assessment of introducing this strategy in this commonly encountered neurologic problem.
Materials and Methods
This randomized double-blind clinical trial study was performed during the period of 2015-2016. The research project was registered at www.irct.ir under the No: IRCT2015102724735N1 after the approval of the ethics committee of Ahvaz Jundishapur University of Medical Sciences. The patients who referred to a neurology clinic of an academic hospital in south-west of Iran included in this study. Inclusion criteria were as follows: Patients with first episode of acute demyelinating optic neuritis with decreased visual acuity (<5/10) and age between 15-50 years.
Exclusion criteria were as follows: history of diabetes mellitus, history of serious adverse effects during receiving IV methylprednisolone (such as gasterointestinal bleeding), known systemic disease other than multiple sclerosis or neuromyelitis optica that might be the cause of the optic neuritis.
Sixty patients randomized into two groups by block randomization with four block sizes. All of the patients received 1 gr IV methylprednisolone for 5 days; then group A received oral prednisolone 50 mg for 10 days and group B received placebo (consisted of mannitol and lactose) for the same time. During this study not only physician but also patients did not know whether the patient has received prednisolone or placebo after IV methylprednisolone. Visual acuity (was measured with Snellen chart) and color vision (was measured with Farnsworth D-15) checked before treatment, before oral tapering, 1 and 3 months after treatment.
All of the patients received pantoprazole 40 mg orally for prophylactic of stress ulcer during treatment [18].Each group consisted of 30 patients.
Systemic, neurological and ophthalmic examination was performed before treatment. Brain magnetic resonance imaging (almost all patients had multiple plaques conforming to multiple sclerosis according to McDonald criteria 2010), Visually Evoked Response (VER) and vasculitis tests were done for all patients. Visual acuity was assessed using Snellen (at a distance of 6 m) visual acuity charts. Color vision was recorded using Farnsworth D-15 color vision plates where the visual acuity permitted its assessment. Visual acuity and color vision were checked before treatment, before oral therapy, 1 and 3 months after treatment. SPSS software version 20 was used to analyze the data. Frequency and percent was used to description of qualitative variables, also mean and SD was used to description of quantitative variables. We compared two groups by using of independent test. P<0.05 was considered as the level of significance.
Results
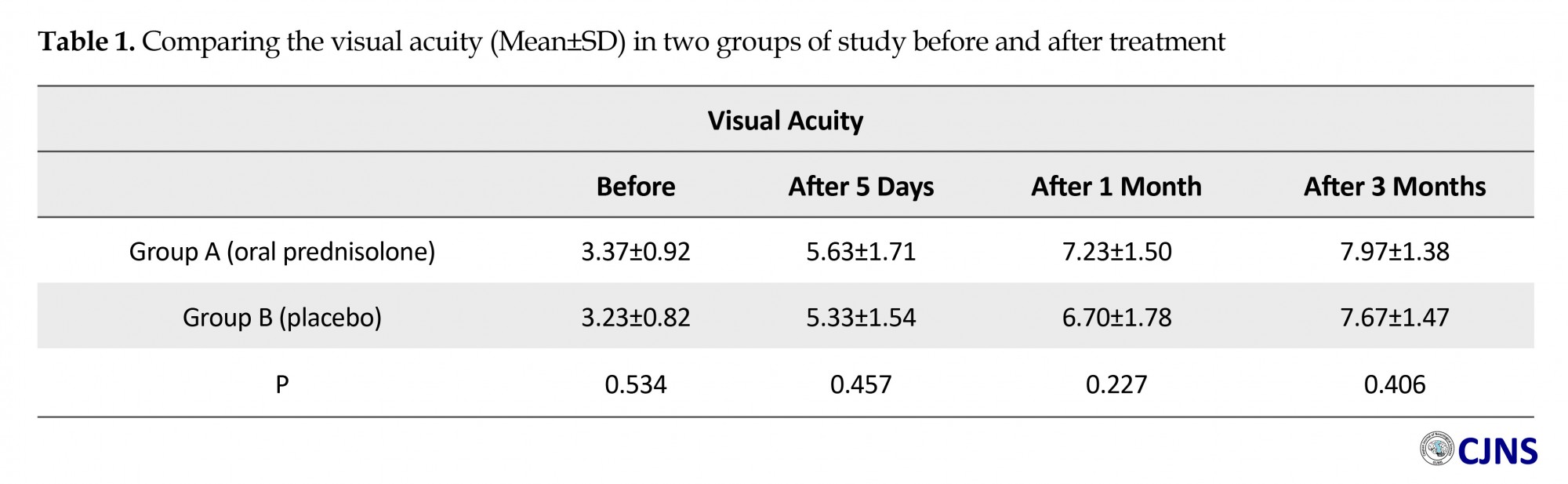
The mean age of patients in group A was 27.67±5.66 years and in Group B was 27.77±5.59 years. Group A consisted of 10 males and 20 females and Group B consisted of 11 males and 19 females. Mean±SD visual acuity in group A and B respectively were at baseline: 3.37±0.92 vs. 3.23±0.82 (P=0.534), before oral therapy: 5.63±1.71 vs. 5.33±1.54 (P=0.457), 1 month after treatment: 7.23±1.50 vs. 6.701±0.78 (P=0.227), 3 months after treatment: 7.97±1.38 vs. 7.671±47 (P=0.406) (Table 1).
ONTT showed that IV steroid treatment in patients presenting with the first attack of optic neuritis results in more rapid improvement associated with reducing the short term risk of developing MS in the following two years compared with controlled placebo group. An interesting and unexpected finding was that oral steroid treatment increased the risk of second relapse and developing MS in this time period. The beneficial effect of IV regimen in reducing the risk of MS was mostly manifested in the presence of abnormal brain MRI consisting of 2 or more characteristic demyelinating lesions. Patients in the IV steroid group in this study received 3 gram IV methylprednisolone followed by oral prednisone 1 mg/kg for 2 weeks while the oral steroid group received oral prednisolone 1 gr/kg for 2 weeks as the only treatment throughout the course. Studies have shown the efficacy of IV high dose steroid therapy in accelerating recovery and also improving the short term prognosis at 2 years regarding conversion to MS [11].
It is important to consider that most studies have not shown the positive effect of this therapy on the final outcome of patients with optic neuritis. IV methylprednisolone pulse therapy is now indicated in optic neuritis in the presence of white matter lesions, severe pain, significant impairment of vision (more than 50%), poor vision in the fellow eye and disabling scotoma [12-15].While oral steroid following IV pulse therapy has been mostly abandoned in adults with optic neuritis because it is considered as adding no benefit while putting the patient at greaterrisk of adverse effects, it is still used sometimes in adults with more severe optic neuritis. It is also known that adverse effects of steroid therapy including GI upset, flushing, sleep and mood disturbance, acne and more importantly serious events such as avascular bone necrosis and metabolic disturbances are dependent on the dose and duration of the steroid treatment [16, 17].
The aim of this study was to show if the tapering oral steroid treatment for a short course following IV pulse steroid therapy would affect the outcome in patients presenting with acute optic neuritis. Both the positive and negative results could help us to evaluate the risk/benefit assessment of introducing this strategy in this commonly encountered neurologic problem.
Materials and Methods
This randomized double-blind clinical trial study was performed during the period of 2015-2016. The research project was registered at www.irct.ir under the No: IRCT2015102724735N1 after the approval of the ethics committee of Ahvaz Jundishapur University of Medical Sciences. The patients who referred to a neurology clinic of an academic hospital in south-west of Iran included in this study. Inclusion criteria were as follows: Patients with first episode of acute demyelinating optic neuritis with decreased visual acuity (<5/10) and age between 15-50 years.
Exclusion criteria were as follows: history of diabetes mellitus, history of serious adverse effects during receiving IV methylprednisolone (such as gasterointestinal bleeding), known systemic disease other than multiple sclerosis or neuromyelitis optica that might be the cause of the optic neuritis.
Sixty patients randomized into two groups by block randomization with four block sizes. All of the patients received 1 gr IV methylprednisolone for 5 days; then group A received oral prednisolone 50 mg for 10 days and group B received placebo (consisted of mannitol and lactose) for the same time. During this study not only physician but also patients did not know whether the patient has received prednisolone or placebo after IV methylprednisolone. Visual acuity (was measured with Snellen chart) and color vision (was measured with Farnsworth D-15) checked before treatment, before oral tapering, 1 and 3 months after treatment.
All of the patients received pantoprazole 40 mg orally for prophylactic of stress ulcer during treatment [18].Each group consisted of 30 patients.
Systemic, neurological and ophthalmic examination was performed before treatment. Brain magnetic resonance imaging (almost all patients had multiple plaques conforming to multiple sclerosis according to McDonald criteria 2010), Visually Evoked Response (VER) and vasculitis tests were done for all patients. Visual acuity was assessed using Snellen (at a distance of 6 m) visual acuity charts. Color vision was recorded using Farnsworth D-15 color vision plates where the visual acuity permitted its assessment. Visual acuity and color vision were checked before treatment, before oral therapy, 1 and 3 months after treatment. SPSS software version 20 was used to analyze the data. Frequency and percent was used to description of qualitative variables, also mean and SD was used to description of quantitative variables. We compared two groups by using of independent test. P<0.05 was considered as the level of significance.
Results
The mean age of patients in group A was 27.67±5.66 years and in Group B was 27.77±5.59 years. Group A consisted of 10 males and 20 females and Group B consisted of 11 males and 19 females. Mean±SD visual acuity in group A and B respectively were at baseline: 3.37±0.92 vs. 3.23±0.82 (P=0.534), before oral therapy: 5.63±1.71 vs. 5.33±1.54 (P=0.457), 1 month after treatment: 7.23±1.50 vs. 6.701±0.78 (P=0.227), 3 months after treatment: 7.97±1.38 vs. 7.671±47 (P=0.406) (Table 1).
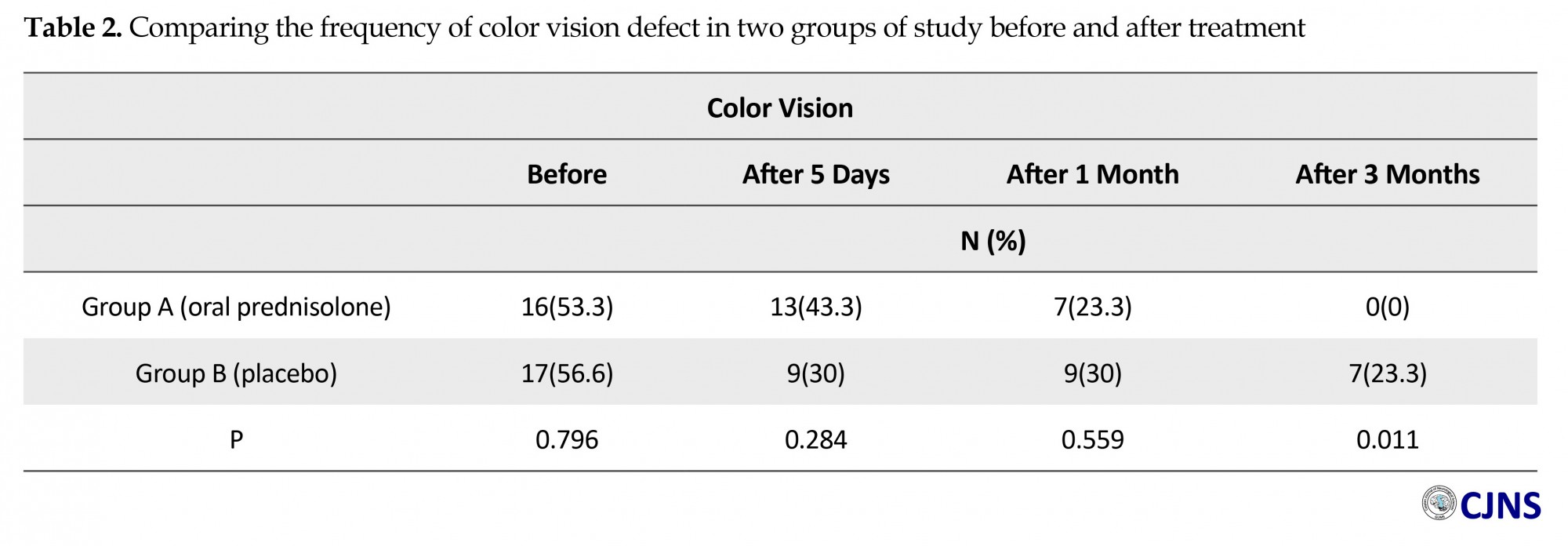
Frequency of color vision abnormality in group A and B respectively were at baseline: (53.3% vs. 56.6%, P=0.796), before oral tapering (43.3% vs. 30%, P=0.284), 1 month after treatment (23.3% vs. 30%, P=0.559), 3 months after treatment (0% vs. 23%, P=0.011) (Table 2). The study found that in all of the patients in two groups, partial recovery in visual acuity occurred before oral therapy, 1 and 3 months after treatment, although in group A (oral prednisolone) recovery was slightly better but it was not statistically significant. Color vision before oral therapy and 1 month after treatment was better in group A but it was not significant, contrary to the results of 3 months after treatment that found significant difference in 2 groups (no patient had color vision defect in group A).
Discussion
The present study assessed the outcome of two visual parameters after treatment with oral prednisolone after IV methylprednisolone in cases of optic neuritis. The mean age of our patients was (27.8 years) younger than of patients in Optic Neuritis Treatment Trial (ONTT) (32 years) and 65% of our patients were female which were less than that study (77%) [19]. In our study males and females were equally represented in both groups. ONTT was a multi-centric collaborative study, compared oral steroids, oral placebo and high-dose intravenous methyl-prednisolone in patients with optic neuritis.
The results of the study showed an early visual recovery in the intravenous methylprednisolone group but at the end of one year there was no difference in the visual functions between the three groups [20, 21]. The mean presenting visual acuity of our patients in tapered oral prednisolone group (A), 3 months after treatment was slightly better than group B (placebo) but it didn’t reach statistically significant. In our study following the treatment, both two parameters (visual acuity and color vision) recovered rapidly in both groups. On follow-up, the patients given oral prednisolone fared better in color vision 3 months after treatment (0%) compared with placebo group (23%), so the difference was statistically significant. Our results for color vision were better. Of course we measured color vision with Farnsworth D-15 but ONTT checked color vision with Ishihara color vision plates which is more sensitive than Farnsworth D-15.
Our study showed intravenous methylprednisolone with oral prednisolone was more effective compared to methylprednisolone. Patients on intravenous methylprednisolone with oral prednisolone responded well to therapy with prompt recovery of two visual parameters especially color vision in 3 months after treatment and no serious side-effects. So oral prednisolone can be considered as an adjunctive therapy to intravenous methylprednisolone for treatment of optic neuritis. However, larger studies with longer follow up period should be carried out to establish the efficacy of tapering oral prednisolone after IV methylprednisolone. Because our patients were followed only three months and if the follow up period would be elongated the results might be different.
Conclusion
Short term outcome, especially color vision of patients with demyelinating optic neuritis by oral steroid treatment after IV methylprednisolone pulse therapy is better than patients who did not receive oral steroid treatment.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors would like to express their gratitude to all the patients who participated in the project.
Conflict of Interest
The authors have no conflicts of interest.
References
The present study assessed the outcome of two visual parameters after treatment with oral prednisolone after IV methylprednisolone in cases of optic neuritis. The mean age of our patients was (27.8 years) younger than of patients in Optic Neuritis Treatment Trial (ONTT) (32 years) and 65% of our patients were female which were less than that study (77%) [19]. In our study males and females were equally represented in both groups. ONTT was a multi-centric collaborative study, compared oral steroids, oral placebo and high-dose intravenous methyl-prednisolone in patients with optic neuritis.
The results of the study showed an early visual recovery in the intravenous methylprednisolone group but at the end of one year there was no difference in the visual functions between the three groups [20, 21]. The mean presenting visual acuity of our patients in tapered oral prednisolone group (A), 3 months after treatment was slightly better than group B (placebo) but it didn’t reach statistically significant. In our study following the treatment, both two parameters (visual acuity and color vision) recovered rapidly in both groups. On follow-up, the patients given oral prednisolone fared better in color vision 3 months after treatment (0%) compared with placebo group (23%), so the difference was statistically significant. Our results for color vision were better. Of course we measured color vision with Farnsworth D-15 but ONTT checked color vision with Ishihara color vision plates which is more sensitive than Farnsworth D-15.
Our study showed intravenous methylprednisolone with oral prednisolone was more effective compared to methylprednisolone. Patients on intravenous methylprednisolone with oral prednisolone responded well to therapy with prompt recovery of two visual parameters especially color vision in 3 months after treatment and no serious side-effects. So oral prednisolone can be considered as an adjunctive therapy to intravenous methylprednisolone for treatment of optic neuritis. However, larger studies with longer follow up period should be carried out to establish the efficacy of tapering oral prednisolone after IV methylprednisolone. Because our patients were followed only three months and if the follow up period would be elongated the results might be different.
Conclusion
Short term outcome, especially color vision of patients with demyelinating optic neuritis by oral steroid treatment after IV methylprednisolone pulse therapy is better than patients who did not receive oral steroid treatment.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors would like to express their gratitude to all the patients who participated in the project.
Conflict of Interest
The authors have no conflicts of interest.
References
- Beck RW, Smith CH, Gal RL, Xing D, Bhatti MT, Brodsky MC, et al. Neurologic impairment 10 years after optic neuritis. Arch Neurol. 2004; 61(9):1386-9. doi: 10.1001/archneur.61.9.1386
- Beck RW, Trobe JD, Moke PS, Gal RL, Xing D, Bhatti MT, et al. High and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the optic neuritis treatment trial. Arch Ophthalmol. 2003; 121(7):944-9. doi: 10.1001/archopht.121.7.944
- Atkins EJ, Biousse V, Newman NJ. The natural history of optic neuritis. Rev Neurol Dis. 2006; 3(2):45-6. PMID: 16819420
- Flanagan P, Zele AJ. Chromatic and luminance losses with multiple sclerosis and optic neuritis measured using dynamic random luminance contrast noise. Ophthalmic Physiol Opt. 2004; 24(3):225–33. doi: 10.1111/j.1475-1313.2004.00191.x
- Levin LA, Lessell S. Optic neuritis and Multiple Sclerosis. Arch Ophthalmol. 2003; 121(7):1039-4. doi: 10.1001/archopht.121.7.1039
- Levin LA. Risk of Multiple Sclerosis after optic neuritis. JAMA. 2003; 290(3):403-4. doi: 10.1001/jama.290.3.403
- Osborne BJ, Volpe NJ. Optic Neuritis and Risk of MS: Differential Diagnosis and Management. Cleve Clin J Med. 2009; 76(3):181-90. doi: 10.3949/ccjm.76a.07268
- Warner JEA. Does optic disc appearance distinguish ischemic optic neuropathy from optic neuritis? Arch Ophthalmol. 1997; 115(11):1408. PMID: 9366671
- Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005; 202(4):473–7. doi: 10.1084/jem.20050304
- Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: Distinction from Multiple Sclerosis. Lancet. 2004; 364(9451):2106–12. doi: 10.1016/s0140-6736(04)17551-x
- Brodsky MC, Buckley EG, Chrousos GA, Corbett J, Eggenberger E, Goodwin JA, et al. Optic Neuritis Study Group. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol Case Rep. 2004; 137(1):77–83. PMID: 14700647
- Bee YS, Lin MC, Wang CC, Sheu SJ. Optic Neuritis: Clinical Analysis of 27 Cases. Gaoxiong Yi Xue Ke Xue Za Zhi. 2003; 19(3):105–11. doi: 10.1016/s1607-551x(09)70457-7
- Optic Neuritis Study Group. Long-term brain magnetic resonance imaging changes after optic neuritis in patients without clinically definite Multiple Sclerosis. Arch Neurol. 2004; 61(10):1538-41. doi: 10.1001/archneur.61.10.1538
- Optic Neuritis Study Group. The clinical profile of optic neuritis. Arch Ophthalmol. 1991; 109(12):1673-78. doi: 10.1001/archopht.1991.01080120057025
- Trobe JD, Sieving PC, Guire KE, Fendrick AM. The impact of the optic neuritis treatment trial on the practices of ophthalmologists and neurologists. Ophthalmology. 1999; 106(11):2047–53. doi: 10.1016/s0161-6420(99)90482-7
- Arnold AC. Evolving management of optic neuritis and Multiple Sclerosis. Am J Ophthalmol Case Rep. 2005; 139(6):1101–8. doi: 10.1016/j.ajo.2005.01.031
- Pham CQ, Regal RE, Bostwick TR, Knauf KS. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006; 40(7-8):1261–6. doi: 10.1345/aph.1g703
- Beck RW, Cleary PA, Anderson MM Jr, Keltner JL, Shults WT, Kaufman DI. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. N Engl J Med. 1992; 326(9):581-8. doi: 10.1056/NEJM199202273260901
- Mehrotra A, Saxena R, Jaffery N, Menon V. Comparative evaluation of megadose methylprednisolone with dexamethasone for treatment of primary typical optic neuritis. Indian J Ophthalmol. 2007; 55(5):355-9. doi: 10.4103/0301-4738.33821
- Optic Neuritis Study Group. The clinical profile of optic neuritis. Arch Ophthalmol. 1991; 109(12):1673-1678. doi: 10.1001/archopht.1991.01080120057025
- Chrousos GA, Kattah JC, Beck RW, Cleary PA. Side effects of glucocorticoid treatment. Experience of the Optic Neuritis Treatment Trial. JAMA. 1993; 269(16):2110-2.PMID: 8468765
Type of Study: Research |
Subject:
Special
Received: 2016/11/20 | Accepted: 2017/03/3 | Published: 2018/01/1
Received: 2016/11/20 | Accepted: 2017/03/3 | Published: 2018/01/1
References
1. Beck RW, Smith CH, Gal RL, Xing D, Bhatti MT, Brodsky MC, et al. Neurologic impairment 10 years after optic neuritis. Arch Neurol. 2004; 61(9):1386-9. doi: 10.1001/archneur.61.9.1386 [DOI:10.1001/archneur.61.9.1386]
2. Beck RW, Trobe JD, Moke PS, Gal RL, Xing D, Bhatti MT, et al. High and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the optic neuritis treatment trial. Arch Ophthalmol. 2003; 121(7):944-9. doi: 10.1001/archopht.121.7.944 [DOI:10.1001/archopht.121.7.944]
3. Atkins EJ, Biousse V, Newman NJ. The natural history of optic neuritis. Rev Neurol Dis. 2006; 3(2):45-6. PMID: 16819420 [PMID]
4. Flanagan P, Zele AJ. Chromatic and luminance losses with multiple sclerosis and optic neuritis measured using dynamic random luminance contrast noise. Ophthalmic Physiol Opt. 2004; 24(3):225–33. doi: 10.1111/j.1475-1313.2004.00191.x [DOI:10.1111/j.1475-1313.2004.00191.x]
5. Levin LA, Lessell S. Optic neuritis and Multiple Sclerosis. Arch Ophthalmol. 2003; 121(7):1039-4. doi: 10.1001/archopht.121.7.1039 [DOI:10.1001/archopht.121.7.1039]
6. Levin LA. Risk of Multiple Sclerosis after optic neuritis. JAMA. 2003; 290(3):403-4. doi: 10.1001/jama.290.3.403 [DOI:10.1001/jama.290.3.403]
7. Osborne BJ, Volpe NJ. Optic Neuritis and Risk of MS: Differential Diagnosis and Management. Cleve Clin J Med. 2009; 76(3):181-90. doi: 10.3949/ccjm.76a.07268 [DOI:10.3949/ccjm.76a.07268]
8. Warner JEA. Does optic disc appearance distinguish ischemic optic neuropathy from optic neuritis? Arch Ophthalmol. 1997; 115(11):1408. PMID: 9366671 [DOI:10.1001/archopht.1997.01100160578009] [PMID]
9. Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005; 202(4):473–7. doi: 10.1084/jem.20050304 [DOI:10.1084/jem.20050304]
10. Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: Distinction from Multiple Sclerosis. Lancet. 2004; 364(9451):2106–12. doi: 10.1016/s0140-6736(04)17551-x [DOI:10.1016/S0140-6736(04)17551-X]
11. Brodsky MC, Buckley EG, Chrousos GA, Corbett J, Eggenberger E, Goodwin JA, et al. Optic Neuritis Study Group. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol Case Rep. 2004; 137(1):77–83. PMID: 14700647 [DOI:10.1016/S0002-9394(03)00862-6]
12. Bee YS, Lin MC, Wang CC, Sheu SJ. Optic Neuritis: Clinical Analysis of 27 Cases. Gaoxiong Yi Xue Ke Xue Za Zhi. 2003; 19(3):105–11. doi: 10.1016/s1607-551x(09)70457-7 [DOI:10.1016/S1607-551X(09)70457-7]
13. Optic Neuritis Study Group. Long-term brain magnetic resonance imaging changes after optic neuritis in patients without clinically definite Multiple Sclerosis. Arch Neurol. 2004; 61(10):1538-41. doi: 10.1001/archneur.61.10.1538 [DOI:10.1001/archneur.61.10.1538]
14. Optic Neuritis Study Group. The clinical profile of optic neuritis. Arch Ophthalmol. 1991; 109(12):1673-78. doi: 10.1001/archopht.1991.01080120057025 [DOI:10.1001/archopht.1991.01080120057025]
15. Trobe JD, Sieving PC, Guire KE, Fendrick AM. The impact of the optic neuritis treatment trial on the practices of ophthalmologists and neurologists. Ophthalmology. 1999; 106(11):2047–53. doi: 10.1016/s0161-6420(99)90482-7 [DOI:10.1016/S0161-6420(99)90482-7]
16. Arnold AC. Evolving management of optic neuritis and Multiple Sclerosis. Am J Ophthalmol Case Rep. 2005; 139(6):1101–8. doi: 10.1016/j.ajo.2005.01.031 [DOI:10.1016/j.ajo.2005.01.031]
17. Pham CQ, Regal RE, Bostwick TR, Knauf KS. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006; 40(7-8):1261–6. doi: 10.1345/aph.1g703 [DOI:10.1345/aph.1G703]
18. Beck RW, Cleary PA, Anderson MM Jr, Keltner JL, Shults WT, Kaufman DI. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. N Engl J Med. 1992; 326(9):581-8. doi: 10.1056/NEJM199202273260901 [DOI:10.1056/NEJM199202273260901]
19. Mehrotra A, Saxena R, Jaffery N, Menon V. Comparative evaluation of megadose methylprednisolone with dexamethasone for treatment of primary typical optic neuritis. Indian J Ophthalmol. 2007; 55(5):355-9. doi: 10.4103/0301-4738.33821 [DOI:10.4103/0301-4738.33821]
20. Optic Neuritis Study Group. The clinical profile of optic neuritis. Arch Ophthalmol. 1991; 109(12):1673-1678. doi: 10.1001/archopht.1991.01080120057025 [DOI:10.1001/archopht.1991.01080120057025]
21. Chrousos GA, Kattah JC, Beck RW, Cleary PA. Side effects of glucocorticoid treatment. Experience of the Optic Neuritis Treatment Trial. JAMA. 1993; 269(16):2110-2.PMID: 8468765
https://doi.org/10.1001/jama.269.16.2110 [DOI:10.1001/jama.1993.03500160080036] [PMID]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |