Tue, Apr 23, 2024
Volume 4, Issue 4 (Autumn 2018)
Caspian J Neurol Sci 2018, 4(4): 152-158 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ezzati K, Sarrafzadeh J, Ebrahimi Takamjani I, Khani S. The Efficacy of Superficial and Deep Dry Needling Techniques on Functional Parameters in Subjects With Upper Trapezius Myofascial Pain Syndrome. Caspian J Neurol Sci 2018; 4 (4) :152-158
URL: http://cjns.gums.ac.ir/article-1-191-en.html
URL: http://cjns.gums.ac.ir/article-1-191-en.html
1- Neuroscience Research Center, Poorsina Hospital, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Physiotherapy, School of Medicine, Iran University of Medical Sciences, Tehran, Iran , j.sarrafzadeh@gmail.com
3- Department of Physiotherapy, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
2- Department of Physiotherapy, School of Medicine, Iran University of Medical Sciences, Tehran, Iran , j.sarrafzadeh@gmail.com
3- Department of Physiotherapy, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 1089 kb]
(911 Downloads)
| Abstract (HTML) (2952 Views)
Rock and Rainey reported that two sessions of dry needling with intramuscular electrical stimulation on thoracic spine can reduce pain and improve ROM of patients with MPS of multifidus muscle, but they did not provide any explanation for the cause of the change in these parameters [17]. In their study, changes were measured in a short period and there was no control group and dry needling was not the only used method, and an electrical stimulation with a frequency level of 1.5 Hz was also used. Therefore, pain reduction can be attributed to the simultaneous use of dry needling and electrical stimulation.
Ceccherelli et al. by comparing superficial and deep acupuncture, found out that at the end of the treatment there was no evidence of significant statistical differences between two methods; however, pain reduction was greater in the group treated with deep acupuncture. But, there was a significant difference between the two groups after the 3-month follow up, with a better result in the deeply stimulated group [9]. It seems that changes in the ROM using SDN method are less compared to DDN technique [10].
One of the reasons is that in the SDN, no changes in muscle fiber density of TrPs or local twitch response occurs. Although the pain may be reduced, but due to the lack of change in the density and structure of TrPs fibers, the change in ROM using SDN method is not very evident. On the other hand, in our study, the group treated with DDN had no significant difference with SDN group after treatment, probably due to muscle soreness. However, in the follow-up periods of 7 and 15 days, due to the decrease in inflammation and wounds in fibers, the increase in the ROM was significantly different from that of the SDN group before and after the treatment. Hence, the ROM in the SDN group was not significantly changed at different times after treatment and in the 7- and 15-day follow up periods, but in the DDN group these changes increased significantly over time. Neck disability gradually decreased in both groups over time, where it was higher in the DDN. The NDI change in DDN group was 8, and in SDN group 2 (Mean difference=6.2). The MDC for NDI score has been reported as 5 [18].
In studies that compare the effects of deep and superficial DN, the intensity of pain has been mostly measured. In most studies, higher pain reduction has been reported in patients treated with DDN [9, 10]. Few studies have measured NDI changes [7]. In the present study, the effect of SDN technique on NDI was not significant, whereas in the DDN group these changes were higher and significant. Improvement of functional ability with DDN method in patients with chronic low back pain has also been reported due to the reduction of pain and mechanical sensitivity [19]. Koppenhaver et al. reported 25% improvement in functional ability of low back pain patients with MPS of multifidus muscle following one session of dry needling [20]. Arendt-Nielsen and Graven-Nielsen stated that the TrPs in the muscle can cause movement changes (such as reduced ROM of weak areas and reduced concurrent contraction) as well as sensory changes (such as pain and tenderness) [21].
In most studies, the method of DDP technique has shown significant effects on functional ability of the neck during even one treatment session [20]. Ziaeifar showed that two sessions of DDN on upper trapezius muscle can improve the disability of arm, although this improvement was not much in comparison with compression technique [22]. They used DASH (the Disability of Arm, Hand, and Shoulder) instrument which is mainly used to measure the functional ability of the upper limb. As previously mentioned, the pain of the upper trapezius muscle is toward the back of neck, head and jaw. The use of NDI questionnaire (used in the present study) may report different results.
Conclusion
The changes in the range of motion and the functional ability of the neck were observed over time when superficial and deep dry needling techniques were used. However, these changes were more significant and prominent in patients treated with deep dry needling, especially in the follow-up periods.
Ethical Considerations
Compliance with ethical guidelines
This study was examined in physiotherapy clinic of Iran University of Medical Sciences during 2016-2017 (Code: IR.IUMS.REC.1395.9413340001).
Funding
This paper was prepared from analyzing part of Saeme Khani’s MSc. Thesis which has been approved by Iran University of Medical Sciences (Registration number: IR.IUMS.REC.1395.9413340001).
Authors contributions
All authors contributed in preparing this article.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Department of Physiotherapy, School of Rehabilitation Sciences at Iran University of Medical Sciences and all patients participated in this study.
References
Full-Text: (1356 Views)
Introduction
Neck pain is a common disorder in people with chronic pain. Among many causes of pain and disability in this area, Myofascial Pain Syndrome (MPS) of upper trapezius muscle is one of the most important ones [1]. MPS is a common, non-joint, and musculoskeletal disorder characterized by the presence of trigger points [2]. Other symptoms of this disease are twitch response during pressure, Reduced Range of Motion (ROM), and other signs of autonomic system [3]. Active trigger points are the main cause of pain in 85% of patients with musculoskeletal pain [2, 3].
According to the European ::::union:::: consisting of 15 European countries, about 25% and 15% of workers, reported shoulder/neck pains and arm pain with myofascial origin, respectively [4]. So far, several kind of therapies have been used for MPS [5]. Dry needling is one of the most important therapeutic approaches in individuals with MPS and its clinical effectiveness has recently been studied [2, 4, 5].
Dry needling is performed by different methods such as superficial, deep, and fascia [3, 5]. In many studies, the effects of these methods on the treatment of MPS have been reported and in some studies, these methods have been compared with each other [5, 6]. Although many studies have been conducted on dry needling methods, but in a few studies, superficial and deep dry needling techniques have been compared to each other [7]. However they have not considered the effects of each of these two methods on MPS. Moreover, most of them are related to the Chinese acupuncture methods [8-10]. Considering this limitation, this study attempts to compare the effects of superficial and deep dry needling techniques on the clinical factors of cervical ROM and neck disability, which naturally highlights important points in the superiority of therapeutic approaches that are very important from a clinical point of view.
Materials and Methods
Study design and population
The present study is a quasi-experimental study where 50 patients with MPS of upper trapezius muscle were randomly divided into two groups of 25 treated with Superficial Dry Needling (SDN) and Deep Dry Needling (DDN). Study variables were Range of Motion (ROM) and Neck Disability Index (NDI). The study inclusion criteria were as follows: Being 2 to 40 years old and having a chronic neck pain that started at least 3 months. Also, the diagnosis of active Trigger Points (TrPs) in the main site of the upper trapezius muscle (the midpoint of the line between the 7th cervical vertebra and acromion process) was performed by a physiotherapist based on Travell and Simons’ criteria: 1. The presence of a taut band in the muscle; 2. Presence of tender nodule in the muscle; and 3. The reproduction of pain during compression of TrPs (in the back and sides of the neck, around the temple, above the eye area, and on the jaw in the affected side) [1].
The study exclusion criteria were as follows: having fibromyalgia based on the criteria of the American College of Rheumatology (1990) with the following symptoms in at least 11 points out of 18 tender point sites: attachment area of suboccipital muscles, low neck area, trapezius, supraspinatus, second rib, lateral epicondyle, gluteal, greater trochanter, and knee; having trigeminal neuralgia, rheumatoid arthritis, rheumatic diseases, degenerative diseases, fracture, dislocation, inflammation, bursitis, and severe dryness of the joints, shoulder and neck myopathy, neuropathy, myelopathy and torticollis; having a history of operation in neck and shoulder and in other areas of the body; having history of injection or acupuncture in the trigger points of upper trapezius muscle; having cancer, infection, pulmonary pain and disease, and acquired immunodeficiency virus; doing athletic exercises (because athletes may differ in terms of muscle stiffness, muscle thickness and fascias as well as the quality of exercise); having substance abuse or taking corticosteroids; being pregnant; having continuous physical therapy or exercise during the last two weeks; taking sedative medications or drinking alcohol one week before the evaluation; having mental and cognitive impairment as well as uncorrected vision impairment; and having history of neck injury or whiplash in the last three months.
Study procedure
The subjects first completed the consent form and then the demographic form as well as the NDI questionnaire. At the first session, they were evaluated, and then received 3 sessions of dry needling treatment every other day. After treatment and two on the 7th and 15th day of follow-up, they were re-evaluated. Since the group with no treatment was not ethically possible, there was no control group. Medications used by the subjects in the two groups of SDN and DDN were the same.
After the evaluation, the patients were asked to lie in prone position with hands placed under the forehead. To maintain the location of TrPs during the treatment session, non-muscular sites such as spinous process of 7th cervical vertebra, clavicle and scapula spine were used. An alcohol solution was used to disinfect the area, and the examiner used sterilized latex gloves. In DDN group, the used needle had 50 mm length and 0.25 mm diameter, while in the SDN group, the used needle with a length of 20 mm and a diameter of 0.25 mm, penetrated only up to 5 mm (equal to the distance between the catheter tip and needle tip). It should be noted that the type and country of manufacture and the length of needles used in the two groups as well as the sites of needling (the midline between the 7th cervical vertebra and acromion process that had already checked with regard to presence of active trigger point there) were the same. The subject would enter the study if he had at least one active trigger point at that site.
After detecting the location of TrPs by touching the mentioned site, the therapist’s second and third fingers of nondominant hand were kept in place. Then, the therapist by his dominant hand pierced the needle into the skin to reach the TrPs (one group superficial penetration and another group deep penetration). Signs of reaching the TrPs was the presence of local twitch response or the recognition of pain. From this moment, the needle was inserted the treated TrP eight times with a fast-in and fast-out technique in a cone pattern. After the final movement, the needle was left in place for 5 minutes based on the suggestions of previous studies [2, 5, 6] and then removed.
In SDN method, the length of needle insertion was also based on the distance between the catheter tip and needle tip, and inserted at the point with active TrP which was already detected. Post-treatment evaluations included: 1. Measurement of disability using NDI tool: Persian version of NDI was used to assess the neck pain affected by performing daily activities, which included following subscales: pain intensity, personal activities, lifting objects, reading, headaches, concentration, work, driving, sleeping, and recreation activities [11]; 2. Measurement of ROM of lateral flexion of neck with a goniometer: Forward head angle was measured while the patient was in an upright seated position, actively moving his neck to one side without turning, bringing the ear toward the shoulder until pain elicitation. The fixed arm of the goniometer was placed perpendicular to the ground, the axis on the spinous process of the 7th cervical vertebra, and the removable arm in the midline of the cervical spine [12].
Results
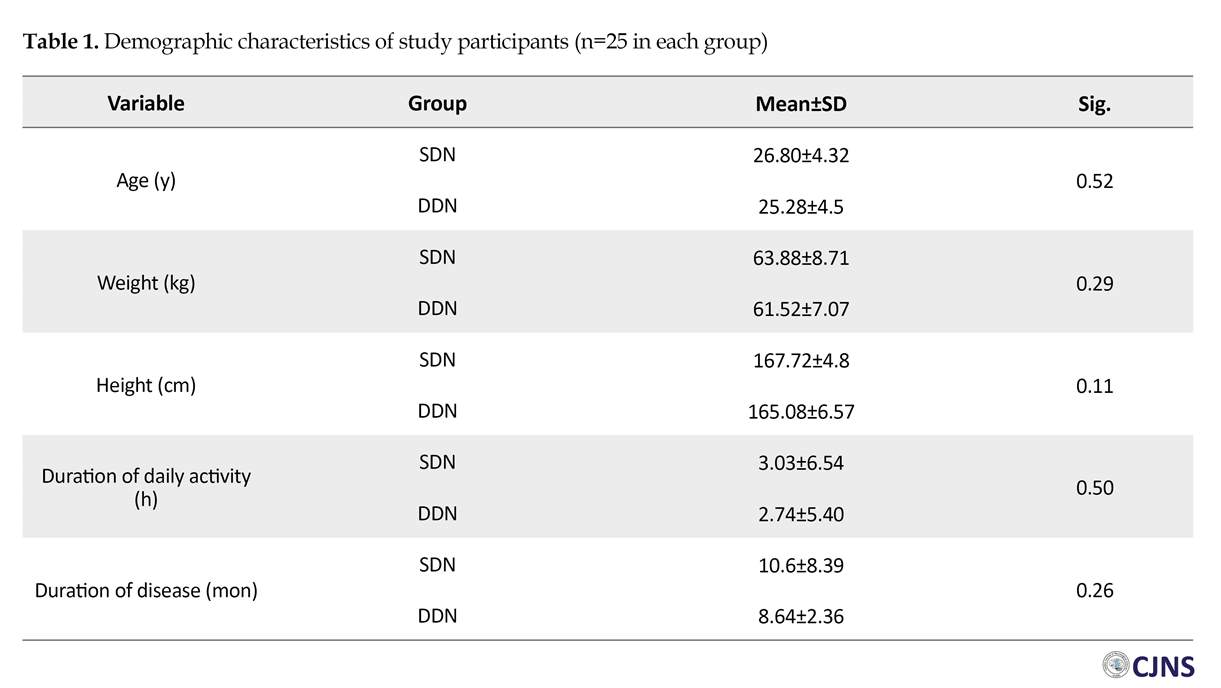
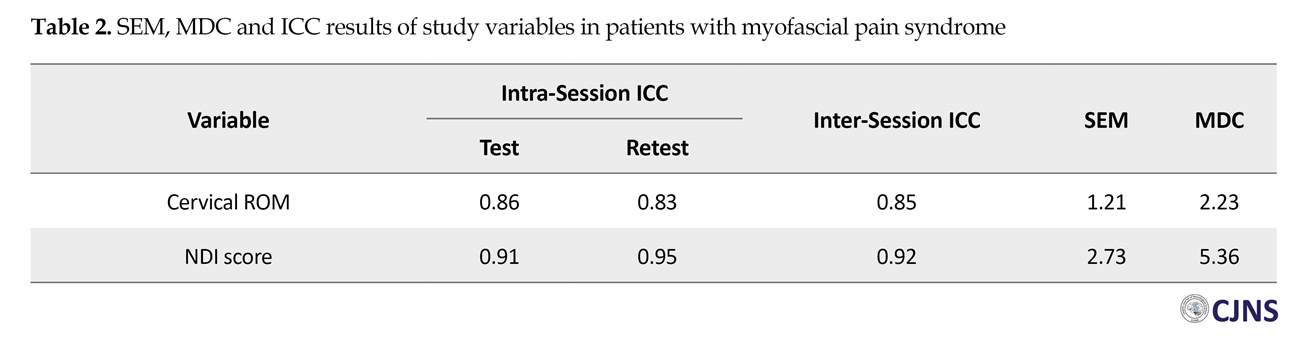
Demographic characteristics of participants are shown in Table 1. All patients participated in the treatment sessions and in both evaluation stages (the rate of sample drop was zero). The results of Kolmogorov-Smirnov (K-S) Test showed that variables of age, weight and height were normally distributed (P>0.05). Standard Error of Measurement (SEM), Intra-class Correlation Coefficients (ICC), and Minimal Detectable Changes (MDC) related to the study variables obtained from 12 patients are presented in Table 2.
Neck pain is a common disorder in people with chronic pain. Among many causes of pain and disability in this area, Myofascial Pain Syndrome (MPS) of upper trapezius muscle is one of the most important ones [1]. MPS is a common, non-joint, and musculoskeletal disorder characterized by the presence of trigger points [2]. Other symptoms of this disease are twitch response during pressure, Reduced Range of Motion (ROM), and other signs of autonomic system [3]. Active trigger points are the main cause of pain in 85% of patients with musculoskeletal pain [2, 3].
According to the European ::::union:::: consisting of 15 European countries, about 25% and 15% of workers, reported shoulder/neck pains and arm pain with myofascial origin, respectively [4]. So far, several kind of therapies have been used for MPS [5]. Dry needling is one of the most important therapeutic approaches in individuals with MPS and its clinical effectiveness has recently been studied [2, 4, 5].
Dry needling is performed by different methods such as superficial, deep, and fascia [3, 5]. In many studies, the effects of these methods on the treatment of MPS have been reported and in some studies, these methods have been compared with each other [5, 6]. Although many studies have been conducted on dry needling methods, but in a few studies, superficial and deep dry needling techniques have been compared to each other [7]. However they have not considered the effects of each of these two methods on MPS. Moreover, most of them are related to the Chinese acupuncture methods [8-10]. Considering this limitation, this study attempts to compare the effects of superficial and deep dry needling techniques on the clinical factors of cervical ROM and neck disability, which naturally highlights important points in the superiority of therapeutic approaches that are very important from a clinical point of view.
Materials and Methods
Study design and population
The present study is a quasi-experimental study where 50 patients with MPS of upper trapezius muscle were randomly divided into two groups of 25 treated with Superficial Dry Needling (SDN) and Deep Dry Needling (DDN). Study variables were Range of Motion (ROM) and Neck Disability Index (NDI). The study inclusion criteria were as follows: Being 2 to 40 years old and having a chronic neck pain that started at least 3 months. Also, the diagnosis of active Trigger Points (TrPs) in the main site of the upper trapezius muscle (the midpoint of the line between the 7th cervical vertebra and acromion process) was performed by a physiotherapist based on Travell and Simons’ criteria: 1. The presence of a taut band in the muscle; 2. Presence of tender nodule in the muscle; and 3. The reproduction of pain during compression of TrPs (in the back and sides of the neck, around the temple, above the eye area, and on the jaw in the affected side) [1].
The study exclusion criteria were as follows: having fibromyalgia based on the criteria of the American College of Rheumatology (1990) with the following symptoms in at least 11 points out of 18 tender point sites: attachment area of suboccipital muscles, low neck area, trapezius, supraspinatus, second rib, lateral epicondyle, gluteal, greater trochanter, and knee; having trigeminal neuralgia, rheumatoid arthritis, rheumatic diseases, degenerative diseases, fracture, dislocation, inflammation, bursitis, and severe dryness of the joints, shoulder and neck myopathy, neuropathy, myelopathy and torticollis; having a history of operation in neck and shoulder and in other areas of the body; having history of injection or acupuncture in the trigger points of upper trapezius muscle; having cancer, infection, pulmonary pain and disease, and acquired immunodeficiency virus; doing athletic exercises (because athletes may differ in terms of muscle stiffness, muscle thickness and fascias as well as the quality of exercise); having substance abuse or taking corticosteroids; being pregnant; having continuous physical therapy or exercise during the last two weeks; taking sedative medications or drinking alcohol one week before the evaluation; having mental and cognitive impairment as well as uncorrected vision impairment; and having history of neck injury or whiplash in the last three months.
Study procedure
The subjects first completed the consent form and then the demographic form as well as the NDI questionnaire. At the first session, they were evaluated, and then received 3 sessions of dry needling treatment every other day. After treatment and two on the 7th and 15th day of follow-up, they were re-evaluated. Since the group with no treatment was not ethically possible, there was no control group. Medications used by the subjects in the two groups of SDN and DDN were the same.
After the evaluation, the patients were asked to lie in prone position with hands placed under the forehead. To maintain the location of TrPs during the treatment session, non-muscular sites such as spinous process of 7th cervical vertebra, clavicle and scapula spine were used. An alcohol solution was used to disinfect the area, and the examiner used sterilized latex gloves. In DDN group, the used needle had 50 mm length and 0.25 mm diameter, while in the SDN group, the used needle with a length of 20 mm and a diameter of 0.25 mm, penetrated only up to 5 mm (equal to the distance between the catheter tip and needle tip). It should be noted that the type and country of manufacture and the length of needles used in the two groups as well as the sites of needling (the midline between the 7th cervical vertebra and acromion process that had already checked with regard to presence of active trigger point there) were the same. The subject would enter the study if he had at least one active trigger point at that site.
After detecting the location of TrPs by touching the mentioned site, the therapist’s second and third fingers of nondominant hand were kept in place. Then, the therapist by his dominant hand pierced the needle into the skin to reach the TrPs (one group superficial penetration and another group deep penetration). Signs of reaching the TrPs was the presence of local twitch response or the recognition of pain. From this moment, the needle was inserted the treated TrP eight times with a fast-in and fast-out technique in a cone pattern. After the final movement, the needle was left in place for 5 minutes based on the suggestions of previous studies [2, 5, 6] and then removed.
In SDN method, the length of needle insertion was also based on the distance between the catheter tip and needle tip, and inserted at the point with active TrP which was already detected. Post-treatment evaluations included: 1. Measurement of disability using NDI tool: Persian version of NDI was used to assess the neck pain affected by performing daily activities, which included following subscales: pain intensity, personal activities, lifting objects, reading, headaches, concentration, work, driving, sleeping, and recreation activities [11]; 2. Measurement of ROM of lateral flexion of neck with a goniometer: Forward head angle was measured while the patient was in an upright seated position, actively moving his neck to one side without turning, bringing the ear toward the shoulder until pain elicitation. The fixed arm of the goniometer was placed perpendicular to the ground, the axis on the spinous process of the 7th cervical vertebra, and the removable arm in the midline of the cervical spine [12].
Results
Demographic characteristics of participants are shown in Table 1. All patients participated in the treatment sessions and in both evaluation stages (the rate of sample drop was zero). The results of Kolmogorov-Smirnov (K-S) Test showed that variables of age, weight and height were normally distributed (P>0.05). Standard Error of Measurement (SEM), Intra-class Correlation Coefficients (ICC), and Minimal Detectable Changes (MDC) related to the study variables obtained from 12 patients are presented in Table 2.
The Independent t-test was used to assess the homogeneity of quantitative variables between the two groups before the treatment, and the results showed that the studied variables were not significantly different in both groups before the treatment. Hence, two groups were homogenous in terms of study variables (Table 3). Table 3 presents Standard Error of Measurement (SEM), Intra-class Correlation Coefficients (ICC), and Minimal Detectable Changes (MDC) of the study variables obtained from 12 patients.
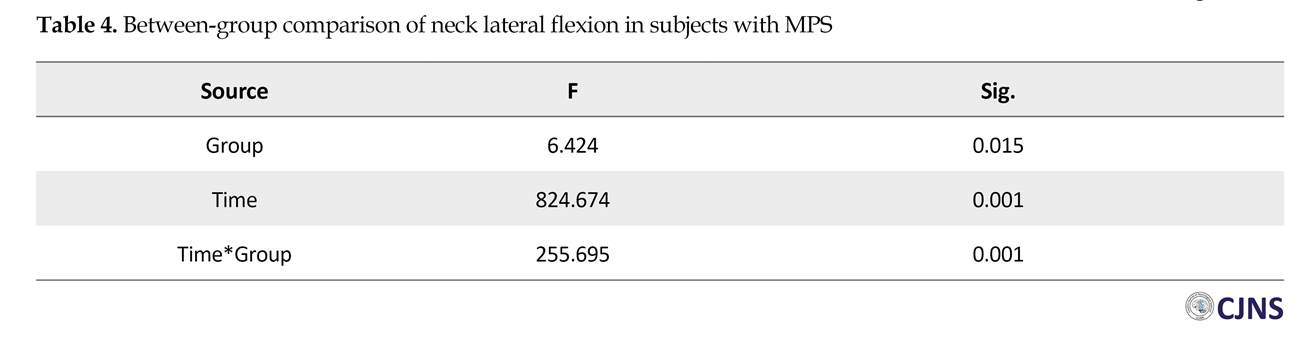
According to the ANOVA results in Table 4, it can be seen that the interaction effect between group and time on the lateral flexion of neck toward the non-affected side is significant (P<0.001). This indicates that the changes in the cervical ROM before and after treatment and in the follow-up periods of 7 and 15 days are different between the two groups. The simple main effect of group on the lateral flexion ROM of neck in patients after treatment (P=0.001), and in the follow-up period (P<0.001) was statistically significant. The simple main effect of time on the lateral flexion of neck was also significant (P<0.001) which indicates that the change in the cervical ROM before and after treatment and in the follow-up periods was significantly different.
ANOVA results also showed that the interaction effect of group and time on NDI was significant (P<0.001). This indicates that the changes in the NDI before and after treatment and in the follow-up periods of 7 and 15 days are different between the two groups. The simple main effect of time and group on NDI were significant (P<0.001) which shows that the change in the NDI before and after the treatment and in the follow-up periods was significantly different (Table 5).
Discussion
The results of the current study showed that the cervical ROM of patients with MPS had progressively increased in both treatment groups over time. MPS reduces the ROM, although this reduction may not be too much [13]. This may lead to pain, fiber contraction, reduced distance between cervical vertebrae, and muscle spasm [14]. Therefore, attention to measuring the ROM is important not only in the neck but also in the further regions such as shoulder and wrist [15]. Pavkovich reported that dry needling of TrPs in the upper trapezius, levator scapula, supraspinatus, and infraspinatus does not affect ROM of neck and shoulder. He blamed the fusion of cervical vertebrae as the reason for this outcome [16].
According to the ANOVA results in Table 4, it can be seen that the interaction effect between group and time on the lateral flexion of neck toward the non-affected side is significant (P<0.001). This indicates that the changes in the cervical ROM before and after treatment and in the follow-up periods of 7 and 15 days are different between the two groups. The simple main effect of group on the lateral flexion ROM of neck in patients after treatment (P=0.001), and in the follow-up period (P<0.001) was statistically significant. The simple main effect of time on the lateral flexion of neck was also significant (P<0.001) which indicates that the change in the cervical ROM before and after treatment and in the follow-up periods was significantly different.
ANOVA results also showed that the interaction effect of group and time on NDI was significant (P<0.001). This indicates that the changes in the NDI before and after treatment and in the follow-up periods of 7 and 15 days are different between the two groups. The simple main effect of time and group on NDI were significant (P<0.001) which shows that the change in the NDI before and after the treatment and in the follow-up periods was significantly different (Table 5).
Discussion
The results of the current study showed that the cervical ROM of patients with MPS had progressively increased in both treatment groups over time. MPS reduces the ROM, although this reduction may not be too much [13]. This may lead to pain, fiber contraction, reduced distance between cervical vertebrae, and muscle spasm [14]. Therefore, attention to measuring the ROM is important not only in the neck but also in the further regions such as shoulder and wrist [15]. Pavkovich reported that dry needling of TrPs in the upper trapezius, levator scapula, supraspinatus, and infraspinatus does not affect ROM of neck and shoulder. He blamed the fusion of cervical vertebrae as the reason for this outcome [16].
Rock and Rainey reported that two sessions of dry needling with intramuscular electrical stimulation on thoracic spine can reduce pain and improve ROM of patients with MPS of multifidus muscle, but they did not provide any explanation for the cause of the change in these parameters [17]. In their study, changes were measured in a short period and there was no control group and dry needling was not the only used method, and an electrical stimulation with a frequency level of 1.5 Hz was also used. Therefore, pain reduction can be attributed to the simultaneous use of dry needling and electrical stimulation.
Ceccherelli et al. by comparing superficial and deep acupuncture, found out that at the end of the treatment there was no evidence of significant statistical differences between two methods; however, pain reduction was greater in the group treated with deep acupuncture. But, there was a significant difference between the two groups after the 3-month follow up, with a better result in the deeply stimulated group [9]. It seems that changes in the ROM using SDN method are less compared to DDN technique [10].
One of the reasons is that in the SDN, no changes in muscle fiber density of TrPs or local twitch response occurs. Although the pain may be reduced, but due to the lack of change in the density and structure of TrPs fibers, the change in ROM using SDN method is not very evident. On the other hand, in our study, the group treated with DDN had no significant difference with SDN group after treatment, probably due to muscle soreness. However, in the follow-up periods of 7 and 15 days, due to the decrease in inflammation and wounds in fibers, the increase in the ROM was significantly different from that of the SDN group before and after the treatment. Hence, the ROM in the SDN group was not significantly changed at different times after treatment and in the 7- and 15-day follow up periods, but in the DDN group these changes increased significantly over time. Neck disability gradually decreased in both groups over time, where it was higher in the DDN. The NDI change in DDN group was 8, and in SDN group 2 (Mean difference=6.2). The MDC for NDI score has been reported as 5 [18].
In studies that compare the effects of deep and superficial DN, the intensity of pain has been mostly measured. In most studies, higher pain reduction has been reported in patients treated with DDN [9, 10]. Few studies have measured NDI changes [7]. In the present study, the effect of SDN technique on NDI was not significant, whereas in the DDN group these changes were higher and significant. Improvement of functional ability with DDN method in patients with chronic low back pain has also been reported due to the reduction of pain and mechanical sensitivity [19]. Koppenhaver et al. reported 25% improvement in functional ability of low back pain patients with MPS of multifidus muscle following one session of dry needling [20]. Arendt-Nielsen and Graven-Nielsen stated that the TrPs in the muscle can cause movement changes (such as reduced ROM of weak areas and reduced concurrent contraction) as well as sensory changes (such as pain and tenderness) [21].
In most studies, the method of DDP technique has shown significant effects on functional ability of the neck during even one treatment session [20]. Ziaeifar showed that two sessions of DDN on upper trapezius muscle can improve the disability of arm, although this improvement was not much in comparison with compression technique [22]. They used DASH (the Disability of Arm, Hand, and Shoulder) instrument which is mainly used to measure the functional ability of the upper limb. As previously mentioned, the pain of the upper trapezius muscle is toward the back of neck, head and jaw. The use of NDI questionnaire (used in the present study) may report different results.
Conclusion
The changes in the range of motion and the functional ability of the neck were observed over time when superficial and deep dry needling techniques were used. However, these changes were more significant and prominent in patients treated with deep dry needling, especially in the follow-up periods.
Ethical Considerations
Compliance with ethical guidelines
This study was examined in physiotherapy clinic of Iran University of Medical Sciences during 2016-2017 (Code: IR.IUMS.REC.1395.9413340001).
Funding
This paper was prepared from analyzing part of Saeme Khani’s MSc. Thesis which has been approved by Iran University of Medical Sciences (Registration number: IR.IUMS.REC.1395.9413340001).
Authors contributions
All authors contributed in preparing this article.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Department of Physiotherapy, School of Rehabilitation Sciences at Iran University of Medical Sciences and all patients participated in this study.
References
- Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: Upper half of body. Philadelphia: Williams and Wilkins; 1999.
- Fernández-de-Las-Peñas C, Alonso Blanco C, Miangolarra JC. Myofascial trigger points in subjects presenting with mechanical neck pain: A blinded, controlled study. Man Ther. 2007; 12(1):29-33. [DOI:10.1016/j.math.2006.02.002]
- Dommerholt J, Huijbregts P. Myofascial trigger points: Pathophysiology and evidence-informed diagnosis and management. Burlington: Jones & Bartlett Learning; 2010.
- Niel Asher S. The concise book of trigger points: A professional and self-help manual. Berkeley: North Atlantic Books; 2014.
- Behnam A, Mahyar S, Ezzati K, Rad SM. The use of dry needling and myofascial meridians in a case of plantar fasciitis. J Chiropr Med. 2014; 13(1):43-8. [DOI:10.1016/j.jcm.2014.01.006] [PMID] [PMCID]
- Baldry P. Superficial versus deep dry needling. Acupunct Med. 2002; 20(2-3):78-81. [DOI:10.1136/aim.20.2-3.78] [PMID]
- Edwards J, Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain: A randomised controlled trial. Acupunct Med. 2003; 21(3):80-6. [DOI:10.1136/aim.21.3.80] [PMID]
- Haker E, Lundeberg T. Acupuncture treatment in epicondylalgia: A comparative study of two acupuncture techniques. Clin J Pain. 1990; 6(3):221-6.
- Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: A double-blind randomized controlled study. Clin J Pain. 2002; 18(3):149-53. [DOI:10.1097/00002508-200205000-00003] [PMID]
- Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients–a blinded RCT. Acupunct Med. 2004; 22(4):170-7. [DOI:10.1136/aim.22.4.170] [PMID]
- Mousavi SJ, Parnianpour M, Montazeri A, Mehdian H, Karimi A, Abedi M, et al. Translation and validation study of the Iranian versions of the neck disability index and the neck pain and disability dcale. Spine. 2007; 32(26):E825-31. [DOI:10.1097/BRS.0b013e31815ce6dd] [PMID]
- Reese NB, Bandy W. Joint range of motion and muscle length testing. Philadelphia: Saunders; 2002.
- Sedighi A, Ansari NN, Naghdi S. Comparison of acute effects of superficial and deep dry needling into trigger points of suboccipital and upper trapezius muscles in patients with cervicogenic headache. J Bodyw Mov Ther. 2017; 21(4):810-4. [DOI:10.1016/j.jbmt.2017.01.002] [PMID]
- Pecos Martín D, Montañez Aguilera FJ, Gallego Izquierdo T, Urraca Gesto A, Gómez Conesa A, Romero Franco N, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: A randomized controlled trial. Arch Phys Med Rehabil. 2015; 96(5):775-81. [DOI:10.1016/j.apmr.2014.12.016]
- Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine. 2004; 29(1):33-40. [DOI:10.1097/01.BRS.0000103944.10408.BA] [PMID]
- Pavkovich R. The use of dry needling for a subject with acute onset of neck pain: A case report. Int J Sports Phys Ther. 2015; 10(1):104-13. [PMID] [PMCID]
- Rock JM, Rainey CE. Treatment of nonspecific thoracic spine pain with trigger point dry needling and intramuscular electrical stimulation: a case series. Int J Sports Phys Ther. 2014; 9(5):699-711. [PMID] [PMCID]
- Ailliet L, Rubinstein SM, De Vet HC, Van Tulder MW, Terwee CB. Reliability, responsiveness and interpretability of the neck disability index-Dutch version in primary care. Eur Spine J. 2015; 24(1):88-93.
- Kubo K, Yajima H, Takayama M, Ikebukuro T, Mizoguchi H, Takakura N. Effects of acupuncture and heating on blood volume and oxygen saturation of human Achilles tendon in vivo. Eur J Appl Physiol. 2010; 109(3):545-50. [DOI:10.1007/s00421-010-1368-z] [PMID]
- Koppenhaver SL, Walker MJ, Su J, McGowen JM, Umlauf L, Harris KD, et al. Changes in lumbar multifidus muscle function and nociceptive sensitivity in low back pain patient responders versus non-responders after dry needling treatment. Man Ther. 2015; 20(6):769-76. [DOI:10.1016/j.math.2015.03.003]
- Arendt Nielsen L, Graven Nielsen T. Muscle pain: Sensory implications and interaction with motor control. Clin J Pain. 2008; 24(4):291-8. [DOI:10.1097/AJP.0b013e31815b608f] [PMID]
- Ziaeifar M, Arab AM, Karimi N, Nourbakhsh MR. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014; 18(2):298-305. [DOI:10.1016/j.jbmt.2013.11.004] [PMID]
Type of Study: Research |
Subject:
Special
Received: 2018/02/23 | Accepted: 2018/07/21 | Published: 2018/10/1
Received: 2018/02/23 | Accepted: 2018/07/21 | Published: 2018/10/1
References
1. Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: Upper half of body. Philadelphia: Williams and Wilkins; 1999.
2. Fernández-de-Las-Pe-as C, Alonso Blanco C, Miangolarra JC. Myofascial trigger points in subjects presenting with mechanical neck pain: A blinded, controlled study. Man Ther. 2007; 12(1):29-33. [DOI:10.1016/j.math.2006.02.002] [DOI:10.1016/j.math.2006.02.002]
3. Dommerholt J, Huijbregts P. Myofascial trigger points: Pathophysiology and evidence-informed diagnosis and management. Burlington: Jones & Bartlett Learning; 2010.
4. Niel Asher S. The concise book of trigger points: A professional and self-help manual. Berkeley: North Atlantic Books; 2014.
5. Behnam A, Mahyar S, Ezzati K, Rad SM. The use of dry needling and myofascial meridians in a case of plantar fasciitis. J Chiropr Med. 2014; 13(1):43-8. [DOI:10.1016/j.jcm.2014.01.006] [PMID] [PMCID] [DOI:10.1016/j.jcm.2014.01.006]
6. Baldry P. Superficial versus deep dry needling. Acupunct Med. 2002; 20(2-3):78-81. [DOI:10.1136/aim.20.2-3.78] [PMID] [DOI:10.1136/aim.20.2-3.78]
7. Edwards J, Knowles N. Superficial dry needling and active stretching in the treatment of myofascial pain: A randomised controlled trial. Acupunct Med. 2003; 21(3):80-6. [DOI:10.1136/aim.21.3.80] [PMID] [DOI:10.1136/aim.21.3.80]
8. Haker E, Lundeberg T. Acupuncture treatment in epicondylalgia: A comparative study of two acupuncture techniques. Clin J Pain. 1990; 6(3):221-6. [DOI:10.1097/00002508-199009000-00009] [PMID]
9. Ceccherelli F, Rigoni MT, Gagliardi G, Ruzzante L. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: A double-blind randomized controlled study. Clin J Pain. 2002; 18(3):149-53. [DOI:10.1097/00002508-200205000-00003] [PMID] [DOI:10.1097/00002508-200205000-00003]
10. Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients–a blinded RCT. Acupunct Med. 2004; 22(4):170-7. [DOI:10.1136/aim.22.4.170] [PMID] [DOI:10.1136/aim.22.4.170]
11. Mousavi SJ, Parnianpour M, Montazeri A, Mehdian H, Karimi A, Abedi M, et al. Translation and validation study of the Iranian versions of the neck disability index and the neck pain and disability dcale. Spine. 2007; 32(26):E825-31. [DOI:10.1097/BRS.0b013e31815ce6dd] [PMID] [DOI:10.1097/BRS.0b013e31815ce6dd]
12. Reese NB, Bandy W. Joint range of motion and muscle length testing. Philadelphia: Saunders; 2002.
13. Sedighi A, Ansari NN, Naghdi S. Comparison of acute effects of superficial and deep dry needling into trigger points of suboccipital and upper trapezius muscles in patients with cervicogenic headache. J Bodyw Mov Ther. 2017; 21(4):810-4. [DOI:10.1016/j.jbmt.2017.01.002] [PMID] [DOI:10.1016/j.jbmt.2017.01.002]
14. Pecos Martín D, Monta-ez Aguilera FJ, Gallego Izquierdo T, Urraca Gesto A, Gómez Conesa A, Romero Franco N, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: A randomized controlled trial. Arch Phys Med Rehabil. 2015; 96(5):775-81. [DOI:10.1016/j.apmr.2014.12.016] [DOI:10.1016/j.apmr.2014.12.016]
15. Lee H, Nicholson LL, Adams RD. Cervical range of motion associations with subclinical neck pain. Spine. 2004; 29(1):33-40. [DOI:10.1097/01.BRS.0000103944.10408.BA] [PMID] [DOI:10.1097/01.BRS.0000103944.10408.BA]
16. Pavkovich R. The use of dry needling for a subject with acute onset of neck pain: A case report. Int J Sports Phys Ther. 2015; 10(1):104-13. [PMID] [PMCID] [PMID] [PMCID]
17. Rock JM, Rainey CE. Treatment of nonspecific thoracic spine pain with trigger point dry needling and intramuscular electrical stimulation: a case series. Int J Sports Phys Ther. 2014; 9(5):699-711. [PMID] [PMCID] [PMID] [PMCID]
18. Ailliet L, Rubinstein SM, De Vet HC, Van Tulder MW, Terwee CB. Reliability, responsiveness and interpretability of the neck disability index-Dutch version in primary care. Eur Spine J. 2015; 24(1):88-93. [DOI:10.1007/s00586-014-3359-y] [PMID]
19. Kubo K, Yajima H, Takayama M, Ikebukuro T, Mizoguchi H, Takakura N. Effects of acupuncture and heating on blood volume and oxygen saturation of human Achilles tendon in vivo. Eur J Appl Physiol. 2010; 109(3):545-50. [DOI:10.1007/s00421-010-1368-z] [PMID] [DOI:10.1007/s00421-010-1368-z]
20. Koppenhaver SL, Walker MJ, Su J, McGowen JM, Umlauf L, Harris KD, et al. Changes in lumbar multifidus muscle function and nociceptive sensitivity in low back pain patient responders versus non-responders after dry needling treatment. Man Ther. 2015; 20(6):769-76. [DOI:10.1016/j.math.2015.03.003] [DOI:10.1016/j.math.2015.03.003]
21. Arendt Nielsen L, Graven Nielsen T. Muscle pain: Sensory implications and interaction with motor control. Clin J Pain. 2008; 24(4):291-8. [DOI:10.1097/AJP.0b013e31815b608f] [PMID] [DOI:10.1097/AJP.0b013e31815b608f]
22. Ziaeifar M, Arab AM, Karimi N, Nourbakhsh MR. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014; 18(2):298-305. [DOI:10.1016/j.jbmt.2013.11.004] [PMID] [DOI:10.1016/j.jbmt.2013.11.004]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |